Urinary tract surgery - investigation of UT dx
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
45 Terms
Where are the kidneys located?
Sit in the retroperitoneal space
R more cranial than left
Both covered by thin capsule
What history would you take when investigating urinary disease?
Complete history incl. signalment & prev. tx
Onset/duration of clinical signs
Progression of clinical signs
Drinking and urination changes
Previous therapy (response)
What are the clinical manifestations of urinary disease?
Haematuria
PU/PD
Dysuria (pain on urination)
Pollakiuria (multiple frequent urination)
Stranguria (straining to urinate)
Oliguria (reduced urine output)
Anuria (absence of urine)
Nocturia (getting up in the night to urinate)
Incontinence
Lethargy
Collapse
Pyrexia
Weight loss
Vomiting or diarrhoea
Abdominal or lumbar pain
What imaging techniques can you use when investigating urinary disease?
Radiography
Contrast radiographic studies (using air / radiopaque contrasts)
Ultrasound
Advanced Imaging
CT, MRI
Cystoscopy
What is assessed in plain radiography?
2 orthogonal views —> R or L lateral + ventrodorsal
Size
Shape
Location
Number
Margination
Opacity
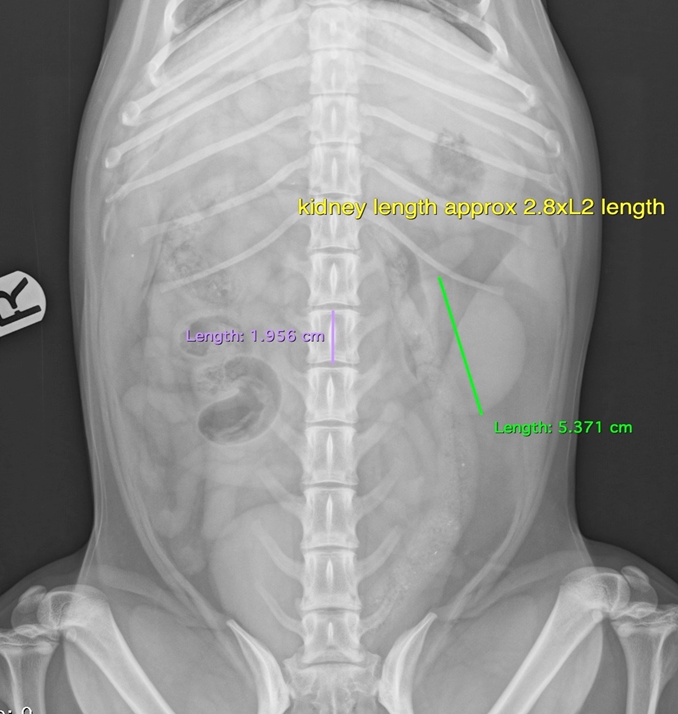
Describe the features of the kidney in survey radiography
Retroperitoneal
R more cranially (cranial pole T13)
L L1-L3
Length
Dogs —> 2.5-3.5 x L2 length
Cats —> 2.4-3 x L2 length
Describe the features of the bladder in a dog or cat in survey radiography
Dogs
Entirely intraabdominal, or intrapelvic neck (females may be more likely to have urinary incontinane)
Os penis present
Cats
Consistently intrabdominal neck
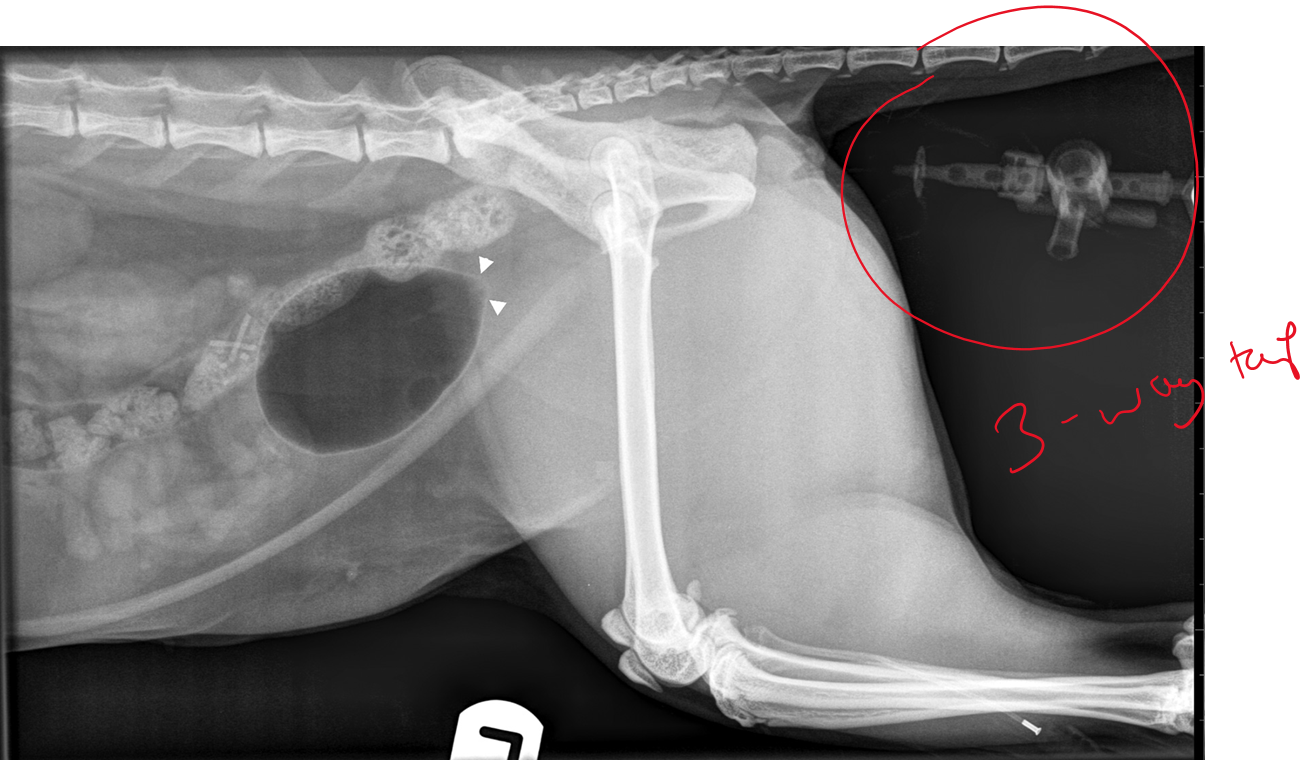
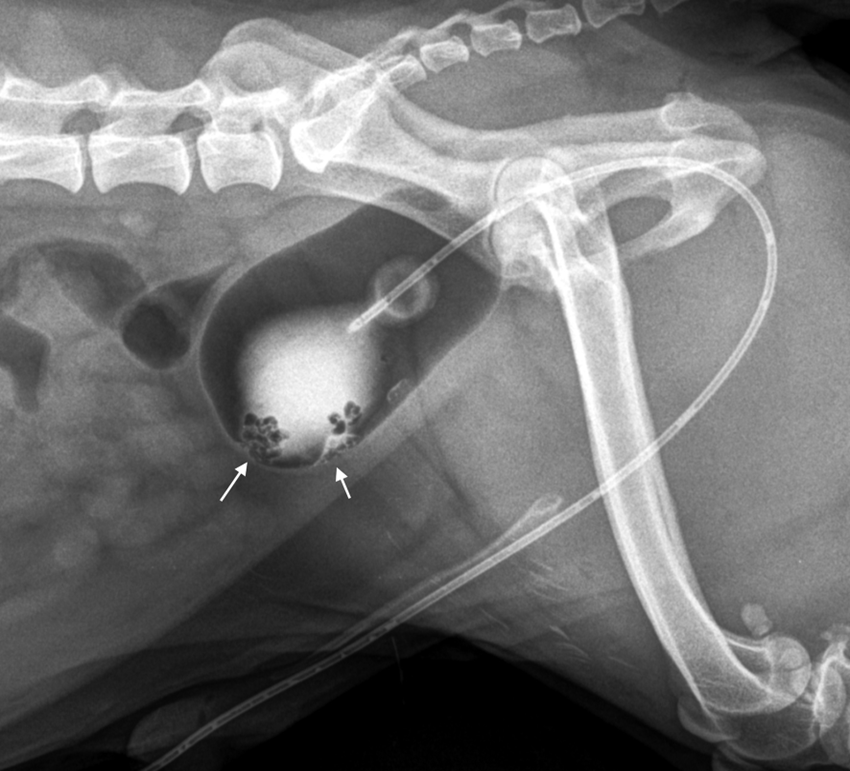
What is being shown in this radiograph and what are the possible causes?
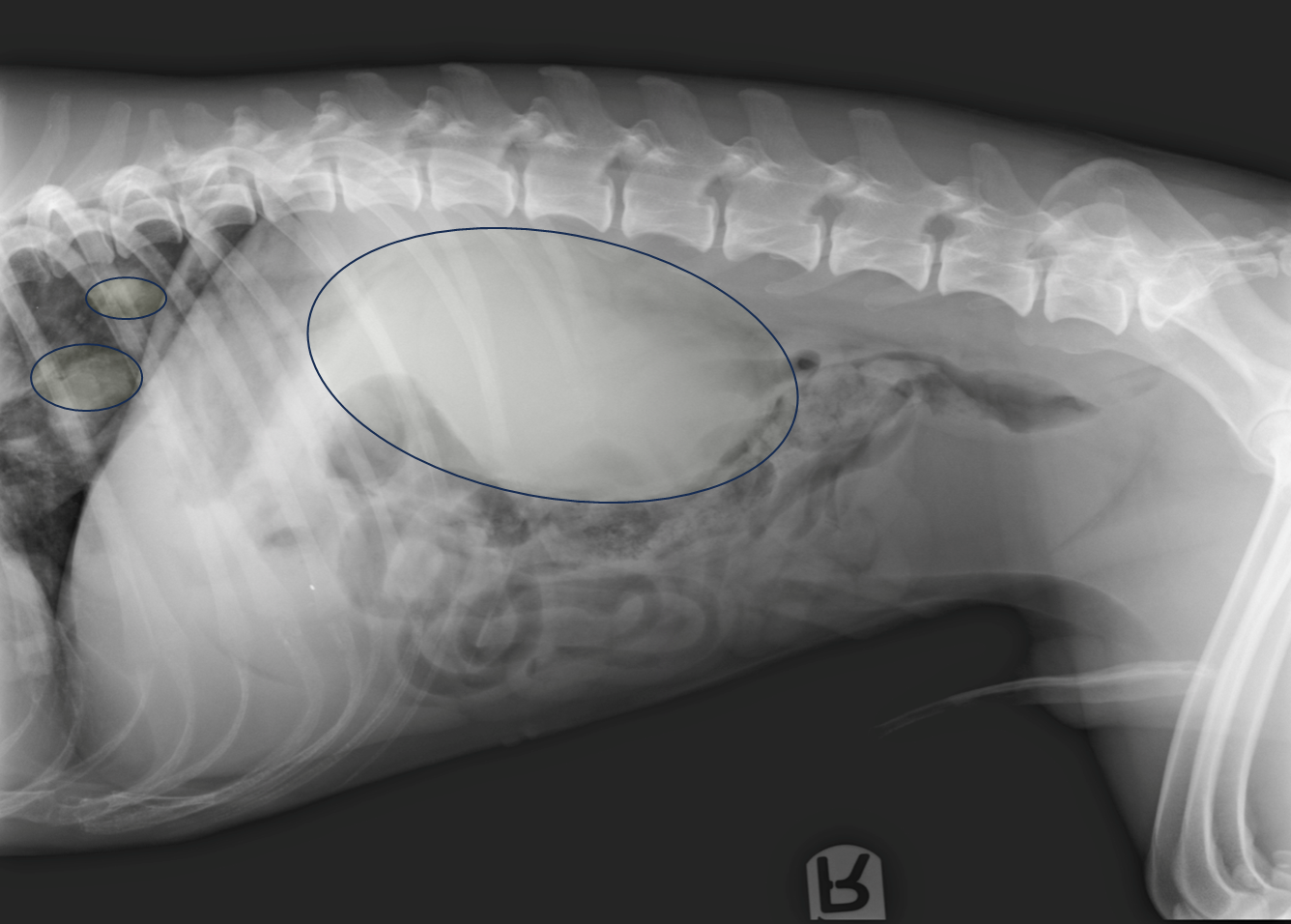
Enlarged kidney —> increased soft tissue opacity in kidney
DDX = Cysts, haemorrage, abscess, neoplasia, granulomatous inflam, hydronephrosis
Metastasis of neoplasia (smaller circles)
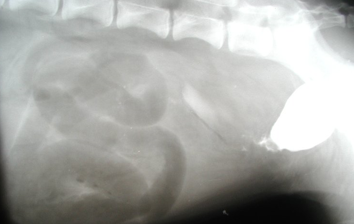
What is being shown on this radiograph?

Mineralised calculi opacities present within the bladder lumen
Urethra has been collimated out of the radiograph —> retake radiograph to see if mineralised calculi is along length of urethra
What is being shown on this radiograph?
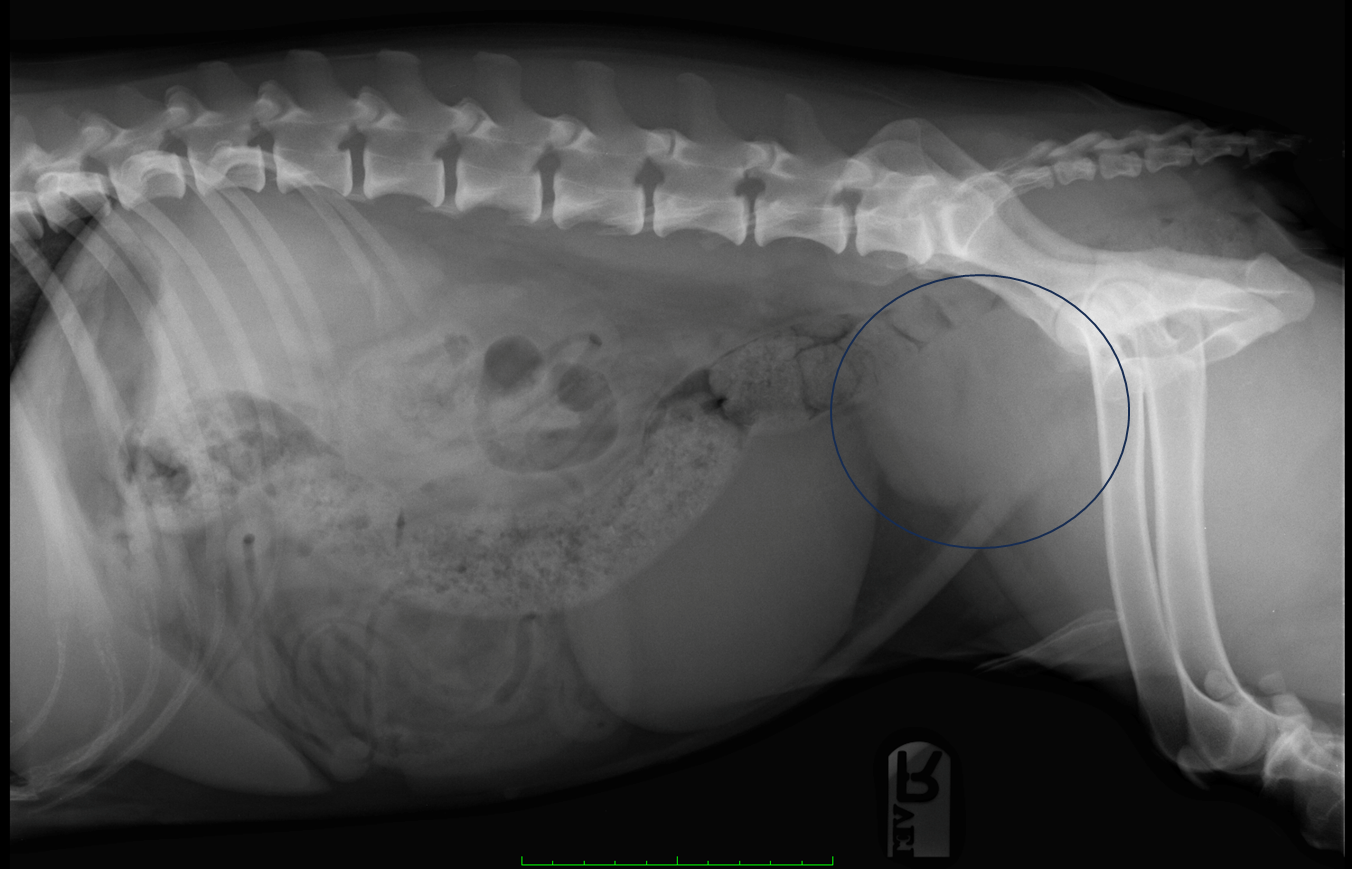
Enlarged prostate (benign prostatic hyperplasia?)
What are examples of negative contrast agents?
Make things more black
Room air
Carbon dioxide (ideally —> don't cause an embolism)
What are examples of positive contrast agents?
Make things more radiopaque
Iodine-based
When carrying out retrograde urethrography/vaginourethrography, why do you need to collect the urine sample first?
What else should you do prior?
Will change urine results otherwise
(starve patient and give enema 2-3hrs before)
When would you carry out intravenous urography?
Evaluation of kidneys and ureters
Indirect assessment of renal function
Investigation of uroabdomen
Investigation of urinary incontinence
Investigations of upper tract haematuria
What is the process of intravenous urography and when would you not use it?
Inject contrast agent through cannula and take radiographs sequentially (would go into kidney first)
Renal failure
Dehydration
Hypotension
Hypovolaemia
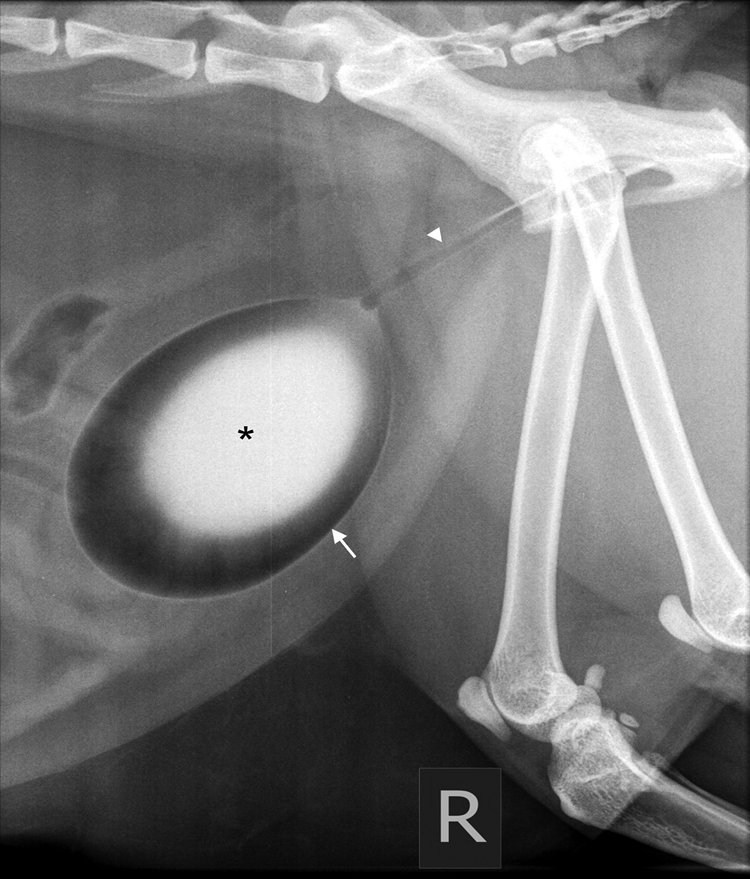
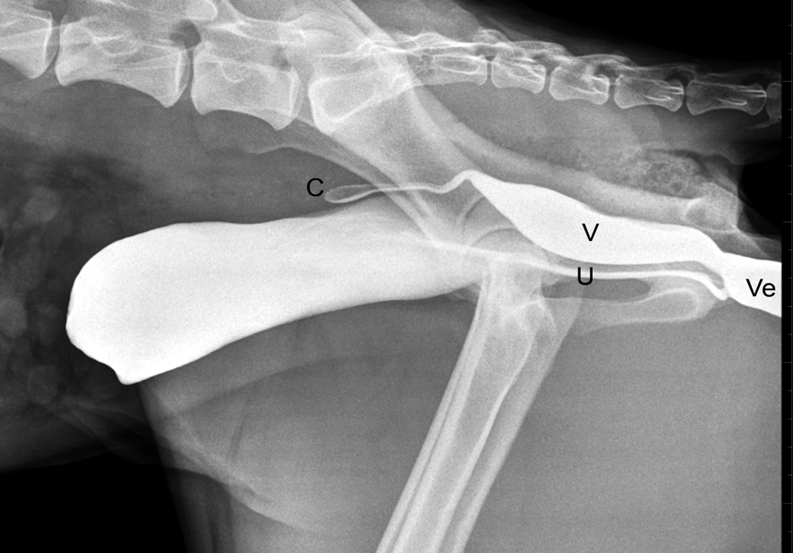
What is being shown here after the use of Intravenous Urography?
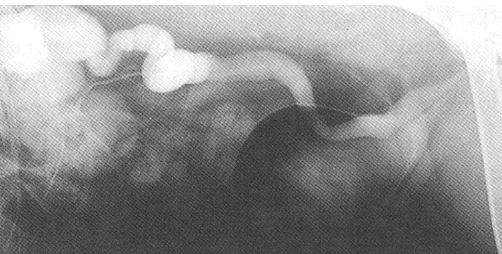
Ectopic ureter —> the ureter is dilated and is inserting into the urethra rather than the trigone of the bladder
When would you utilise contrast cystography?
Haematuria
Dysuria
Urine retention
Incontinence
What information does contrast cystography tell you?
Bladder location and integrity
Assessment of bladder wall and mucosa (only if double contrast)
Presence of calculi (depending on opacity)
How is pneumocystography carried out?
Urinary catheter placement
Room air or Carbon dioxide injected into the bladder (5-10ml/kg in dogs, 25ml in cats)
Left lateral recum
Gently palpate bladder while injecting, stop injecting when bladder feels moderately distended, obtain radiograph —> don’t over-distend bladder!
When should you NOT perform a pneumocystography?
If bladder is ruptured, mucosal trauma or haemorrhage —> use positive contrast as more definitive to see
What is being shown here?

Intrapelvic bladder —> irregularly shaped due to surrounding tissues compressing
What is being shown here?

There is a thickened irregular wall —> the bladder hasn’t distended evenly due to fibrosis and chronic cystitis.
When and how would you carry out Positive contrast cystography?
To localize the bladder and assess integrity (obscures caliculi and we cannot see mucosal detail)
Place urinary catheter and inject 5-10ml/kg of contrast medium
Conc. of contrast medium = 150mg/ml, dilute with saline
Reflux of contrast into ureters due to pressure = normal finding
What is being shown in this Positive contrast cystography radiograph?
Bladder is small and is caudally positioned
Mineralised opacity of contrast medium
Contrast leaking into the abdomen (rupture)
What is being shown in this positive contrast cystography radiograph?
You can see that bladder is abnormally positioned —> due to perineal hernia and the bladder had herniated through the pelvic diaphragm
How do you carry out double contrast cystography?
Urinary catheter placement
Empty bladder
2-5ml (small patient) 10-20 ml (large patient) of diluted contrast medium (150mg/ml) - important not to inject too much
Inject gas as for pneumocystography
Highlights mucosal detail —> can recognise lesions not seen with gas or contrast medium alone
Why would you carry out double contrast cystography?
Assessment of mucosal lining and looking for radiolucent calculi
Best assessment of mucosal detail, can recognise lesions not seen with gas or contrast medium alone
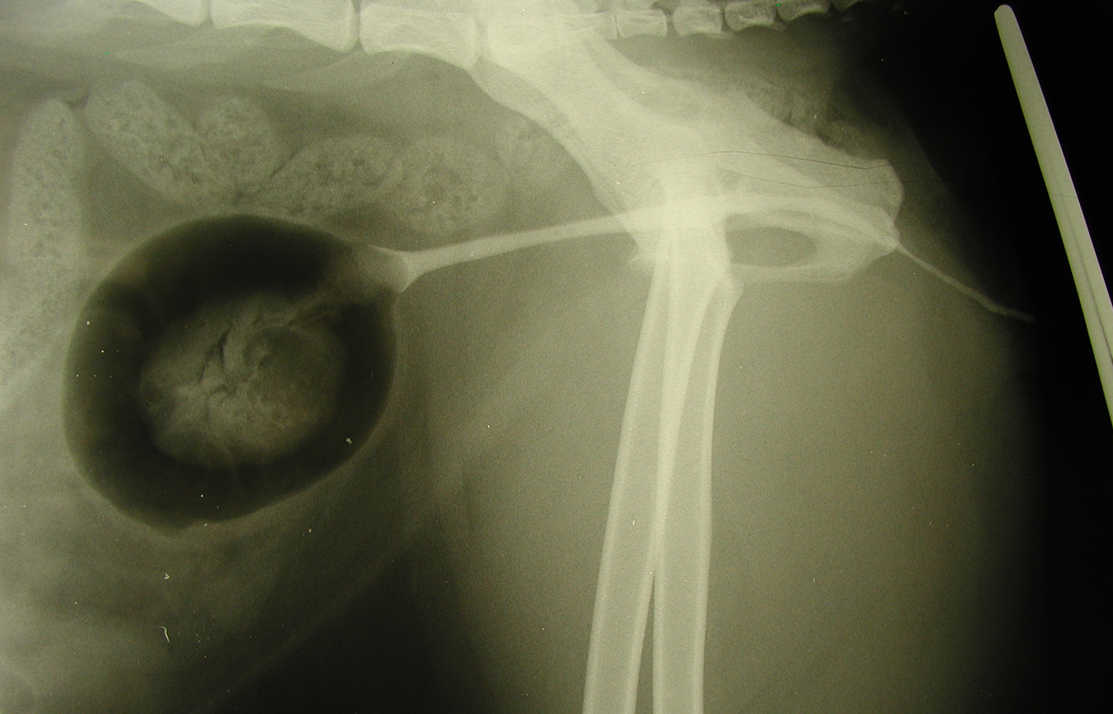
What is the double contrast cystography showing here?
Growth of polyps from bladder wall —> polypoid cystitis
Soft tissue of polyps outlined by contrast
Using folley urinary catheter —> has balloon on end, stops catheter dislodging from UT —> gets stuck @ neck of bladder
What is retrograde urethrography used to investigate?
Urethral, prostatic, vaginal and penile disease
Stranguria or dysuria
calculi in urethra?
narrowing of urethra? = stricture
Urinary obstraction / RTA? —> urethra damaged
How do you carry out retrograde urethrography?
Catheterise urethra and empty bladder (if possible)
Pneumocystogram should ideally be performed first. This aids with retention of the contrast in the urethra.
Prefilled urinary cath with contrast medium, tto remove air bubbles (will look like false filling defect)
Tip of the foley catheter in the penile urethra
Take radiographs while injecting (5-10ml, 150mg/ml)
Take radiographs while injecting
Describe this retrograde urethrography radiograph (dog)?

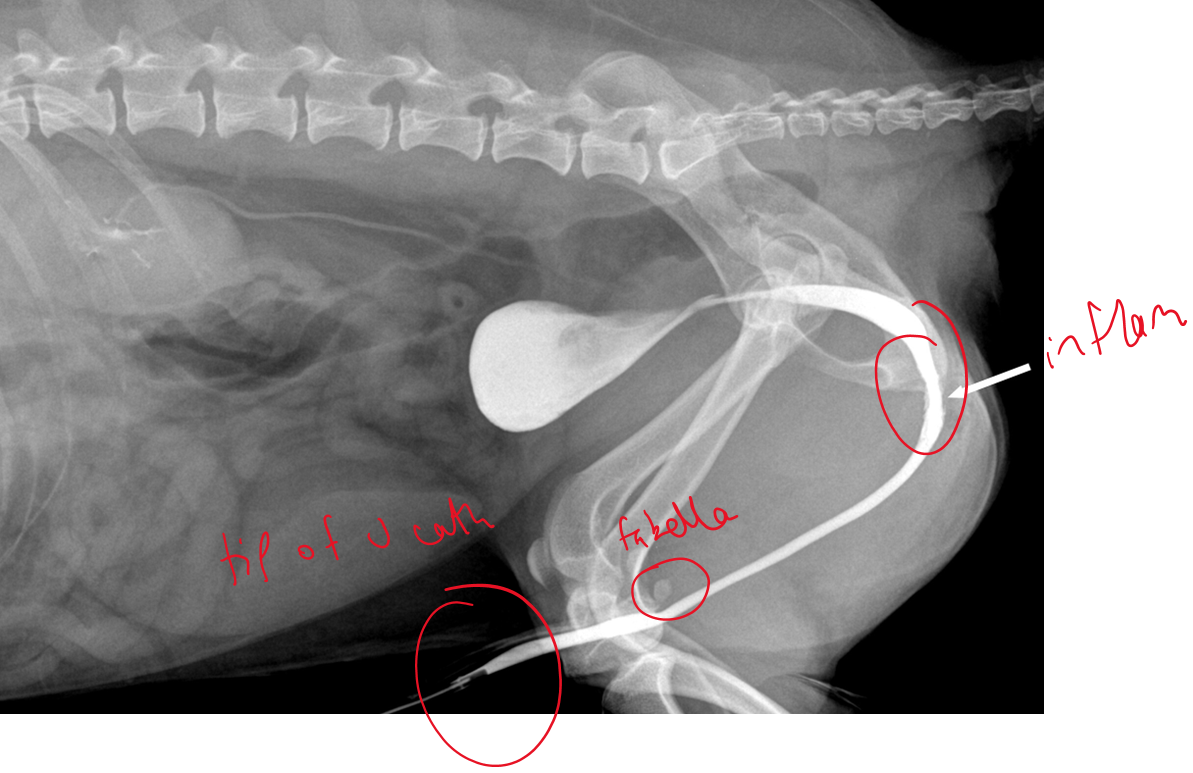
Membranous urethra is wider (normal)
Fabella of femur can look like caliculi so pull legs forward
No contrast leakage
Describe this retrograde urethrography radiograph (cat)?
Narrowing
Strong hollow contrast leading to bladder
Ureters would have been clearer with IVU
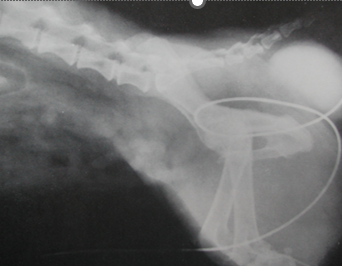
What is being shown here?

RTA —> femoral #
Bladder rupture —> leakage of urine into the peripheral tissues
cannot see clear bladder outline
gas obacity in abdomen, consistent with ruptured ureter
What would you use retrograde vaginourethrogram to investigate?
Used for females as difficult to catheterise
Stranguria (e.g. neoplasia, proliferative urethritis)
Mass lesions within pelvis or vagina
Urinary incontinence
Ectopic ureters
How do you perform a vaginourethrogram?
Insert a Foley catheter into the vulva and dilate the balloon
Clamp the lips of the vulva using atraumatic forceps
Inject radiographic contrast material
Take the radiograph as injecting contrast
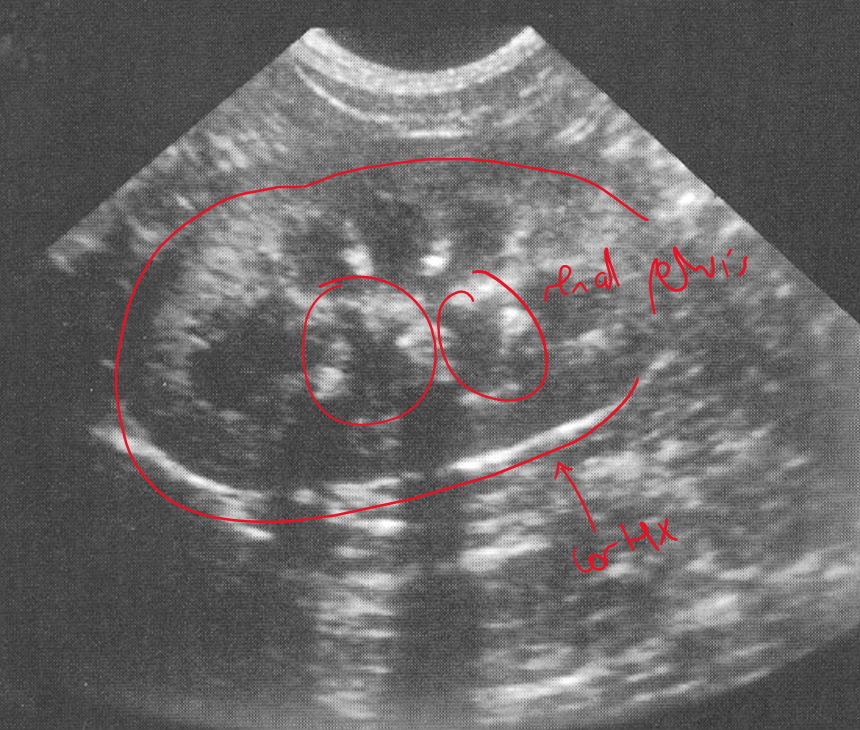
What do you identify about the kidneys in an ultrasound?
Size, shape, internal architecture, renal perfusion (doppler —> highlights blood flow)
Clear demarcation between cortex and medulla (normal)
(ureters not normally identified)
(urethra challenging due to intrapelvic location)
What do you identify about the bladder in an ultrasound?
Wall thickness and layering
Presence of mass lesions
Calculi
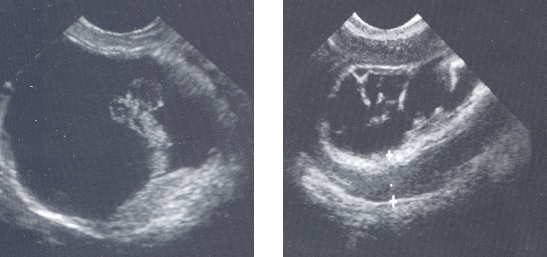
What is being shown here?
R = Dilated renal pelvis
Bottom = dilalted proximal ureter
L = ureters dilated by couple mms —> obstruction of urinary outflow
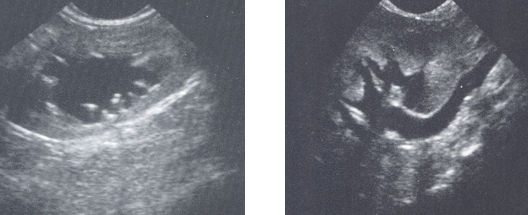
What is being shown in this bladder?
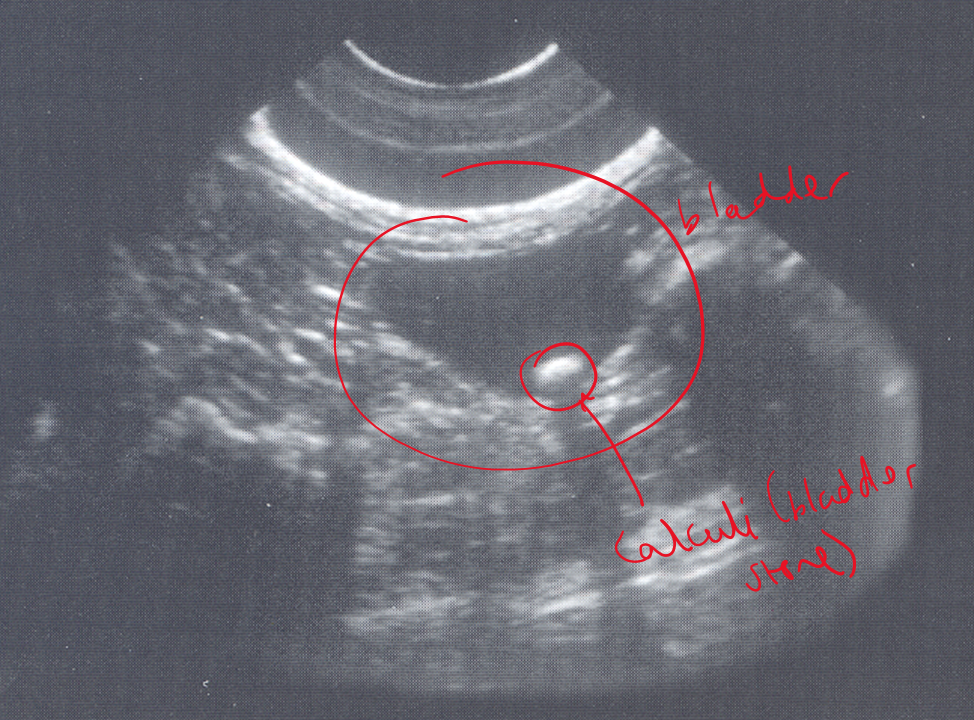
Cystolith (bladder stone) —> casting acoustic shadow
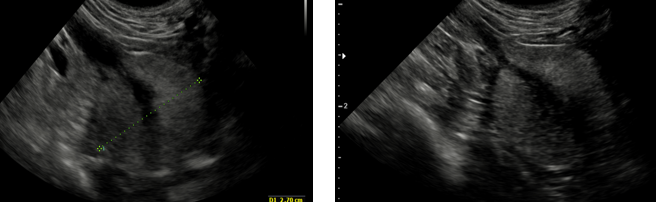
What is being shown in these bladders?
L —> thickened wall with a hyperechoic lesion arising from the wall —> consistent with a bladder wall mass
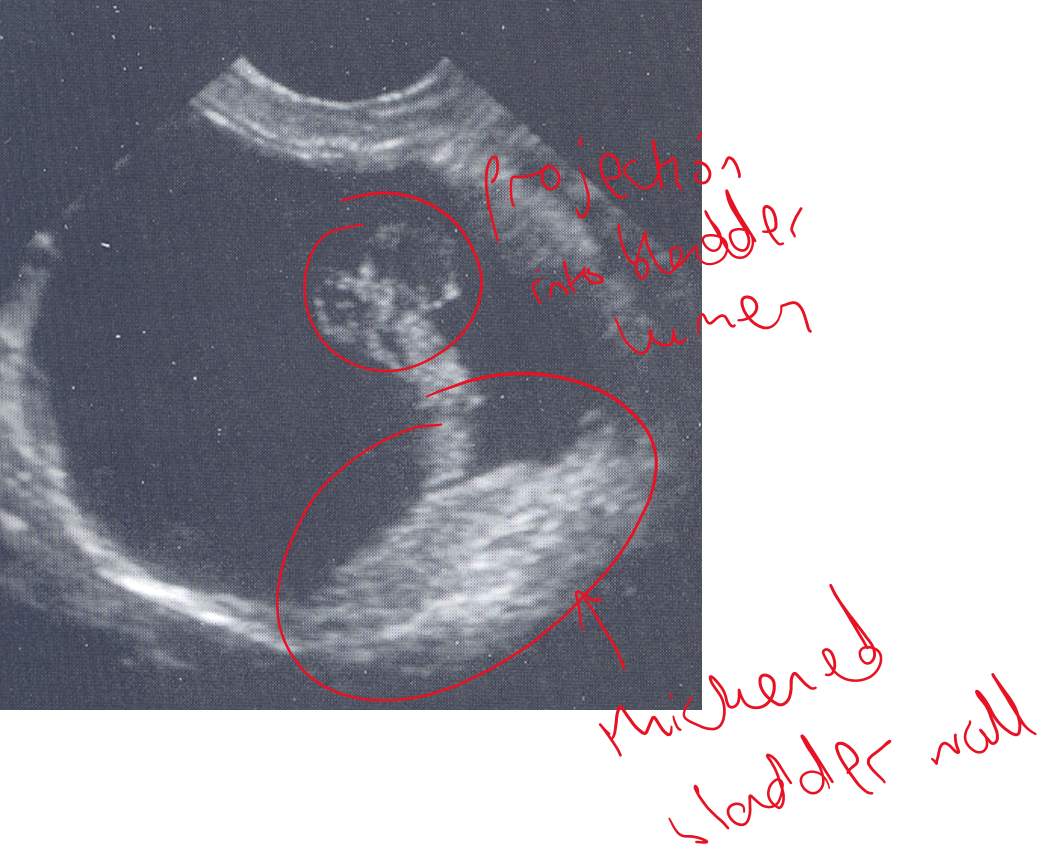
R —> thickened and within the lumen we can see hyperechoic areas which may be a mass or could be blood clots.
How do you use a doppler to tell the difference between a blood clot vs a tumour?
Blood clot has no blood flow, tumour does
What is being shown on this ultrasound?
Normal prostate
What can cystoscopy be used for?
Diagnosis and treatment of ectopic ureters and other developmental conditions
Can also be used for removal of bladder stones or to acquire biopsies
What are the advantages and disadvantages of cystoscopy?
+
Minimally invasive —> patient can go home same day (no surgery required)
Excellent visualization of urethra and bladder
Allows simultaneous treatment
-
Requires additional equipment
Requires advanced skill —> could overfill bladder or camera could go through bladder
What are the options for biopsies?
Fine needle aspirates with or without U/S guidance
avoid for masses → could leave trail of neoplastic cells in abdomen when needle withdrawn
Catheter suction samples from the bladder, urethra or prostate
Surgical —> incisional (part of lesion) or excisional (whole thing)