Ch19: Blood, 19.2 Erythrocytes and Oxygen Transport
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
What is the significance of erythrocyte structure?
Shape and components facilitate their transport of oxygen and carbon dioxide through blood
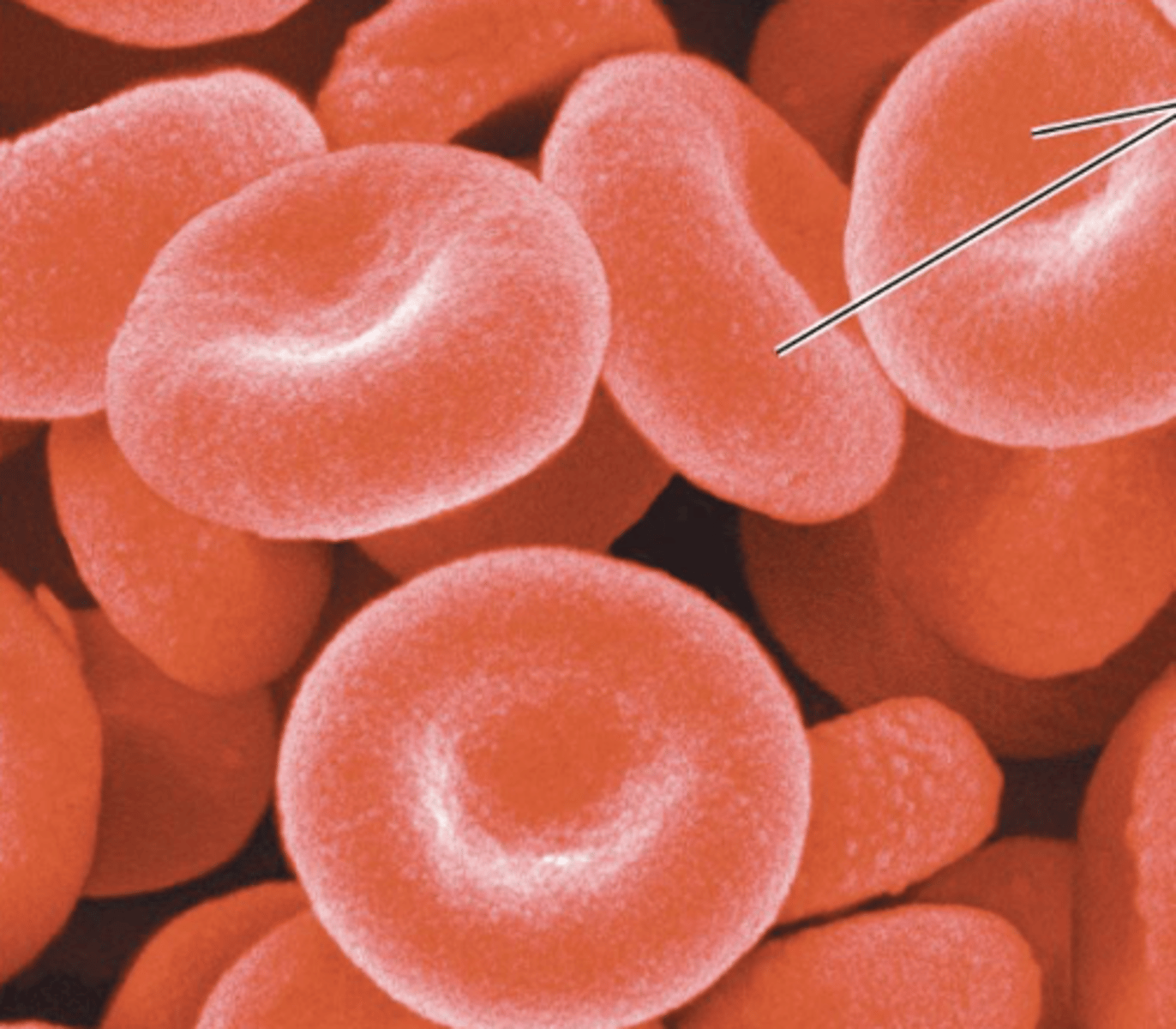
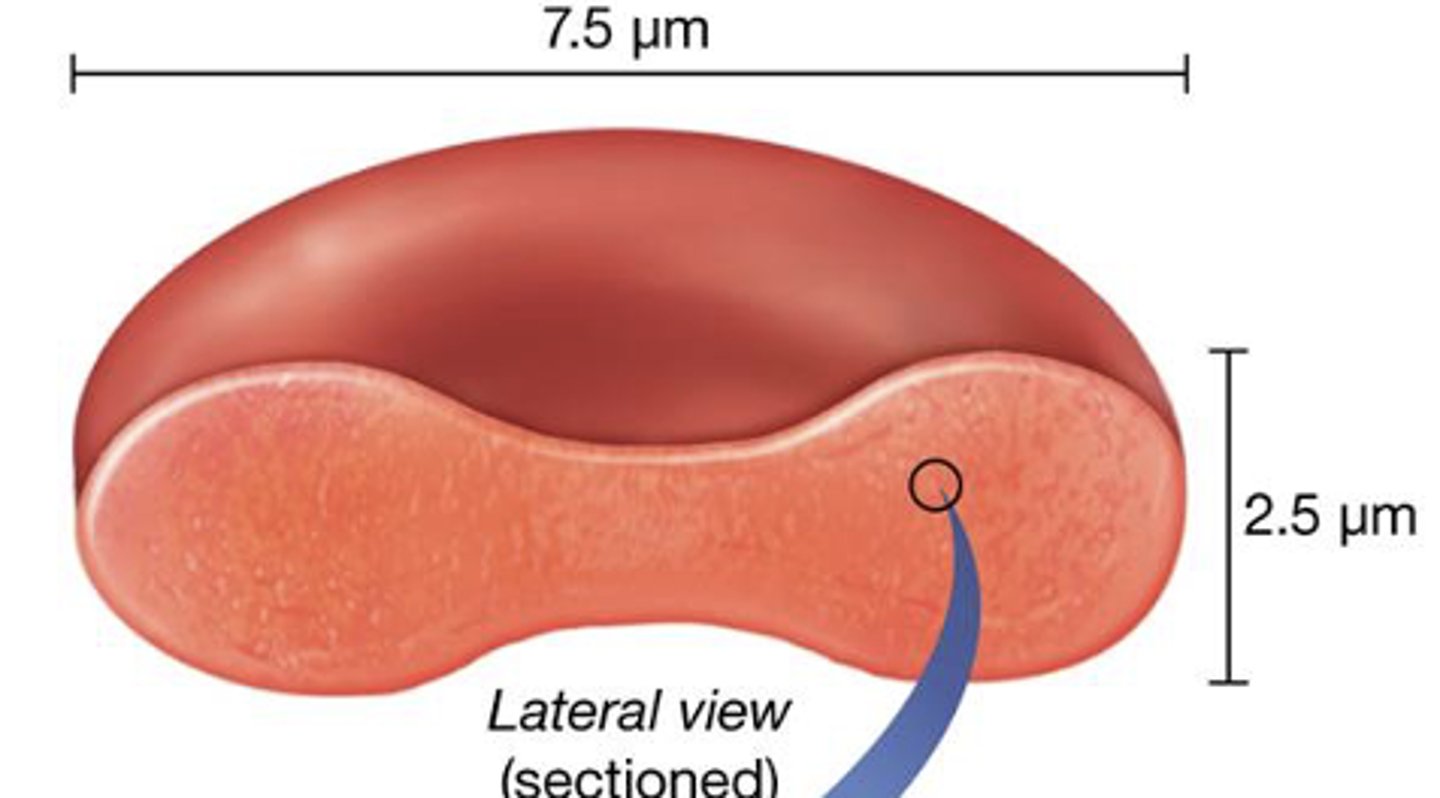
What is the significance of erythrocyte shape?
increases surface area of cell; vital to role in gas exchange
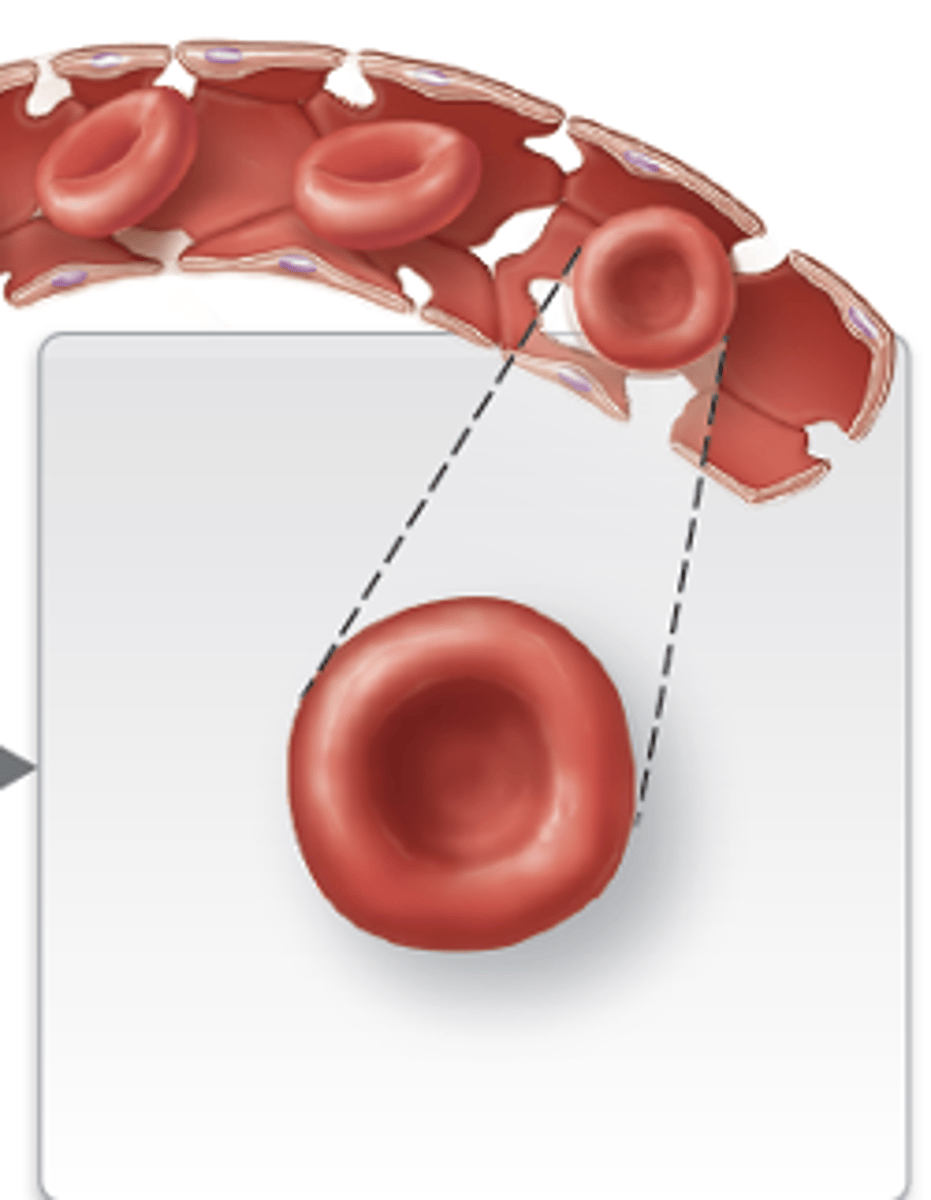
What is different about mature RBCs?
they are anucleate, lost nucleus during maturation; also lack most other cellular organelles
Describe erythrocyte structure
biconcave disc containing cytosol, enzymes, and hemoglobin
What is the effect of anucleate, mature RBCs?
Creates room in cytosol for enzymes and nearly 1 billion oxygen-binding hemoglobin (Hb) proteins
What is hemoglobin?
large protein that consists of four polypeptide subunits: two alpha (a) chains and two beta (b) chains
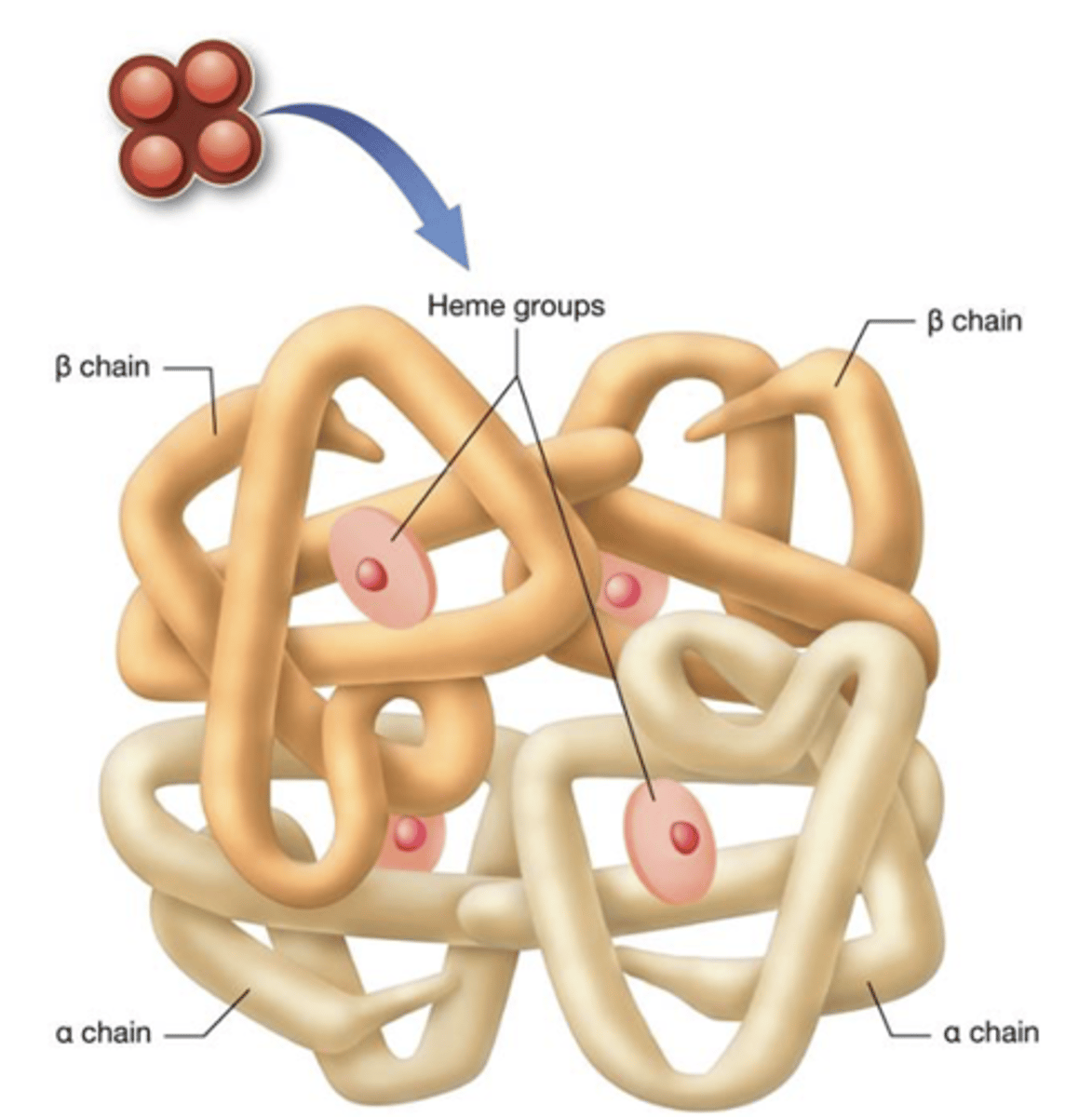
What is a heme group?
iron-containing compound that each polypeptide is bound to
What is oxyhemoglobin (HbO2)?
red molecule; hemoglobin bound to oxygen
When are iron ions in the heme group oxidized?
when it binds to oxygen in regions of high oxygen concentration; oxyhemoglobin forms as a result
Where does hemoglobin release oxygen?
tissues surrounding systemic capillary beds; where oxygen concentration is low
What is the result when hemoglobin binds to carbon dioxide?
carbaminohemoglobin
Where does carbaminohemoglobin form?
where oxygen levels are low
What percent of carbaminohemoglobin is the CO2 transported in the blood?
23%
When is carboxyhemoglobin formed? What does it bind to?
when hemoglobin binds to carbon monoxide; binds more strongly to iron ion than oxygen
What is the problem with carboxyhemoglobin?
Changes shape of Hb making it unable to unload oxygen into oxygen-deprived tissues; can lead to death
What is the lifespan of erythrocytes?
relatively short, ranging from 100–120 days
Why is the lifespan of erythrocytes so short?
Due to damage incurred by harsh environment in which they exist
Why can't erythrocytes repair themselves?
they lose most of their parts (organelles) when they mature and fill up with hemoglobin
Why does the body have to continuously make new erthyrocytes?
because they cannot repair themselves
What is hematopoiesis? Where does it take place?
process of making all blood cells (RBCs, WBCs, and platelets) from hematopoietic stem cells (HSCs); in the red bone marrow
What is erythropoiesis?
specific hematopoietic process that produces erythrocytes from HSCs
What are the steps of erythropoiesis?
1.) Hematopoietic stem cell
2.) Erythrocyte-CFU
3.) Proerythroblast
4.) Early erythroblast
5.) Last erythroblast
6.) Reticulocyte
7.) Erythrocyte
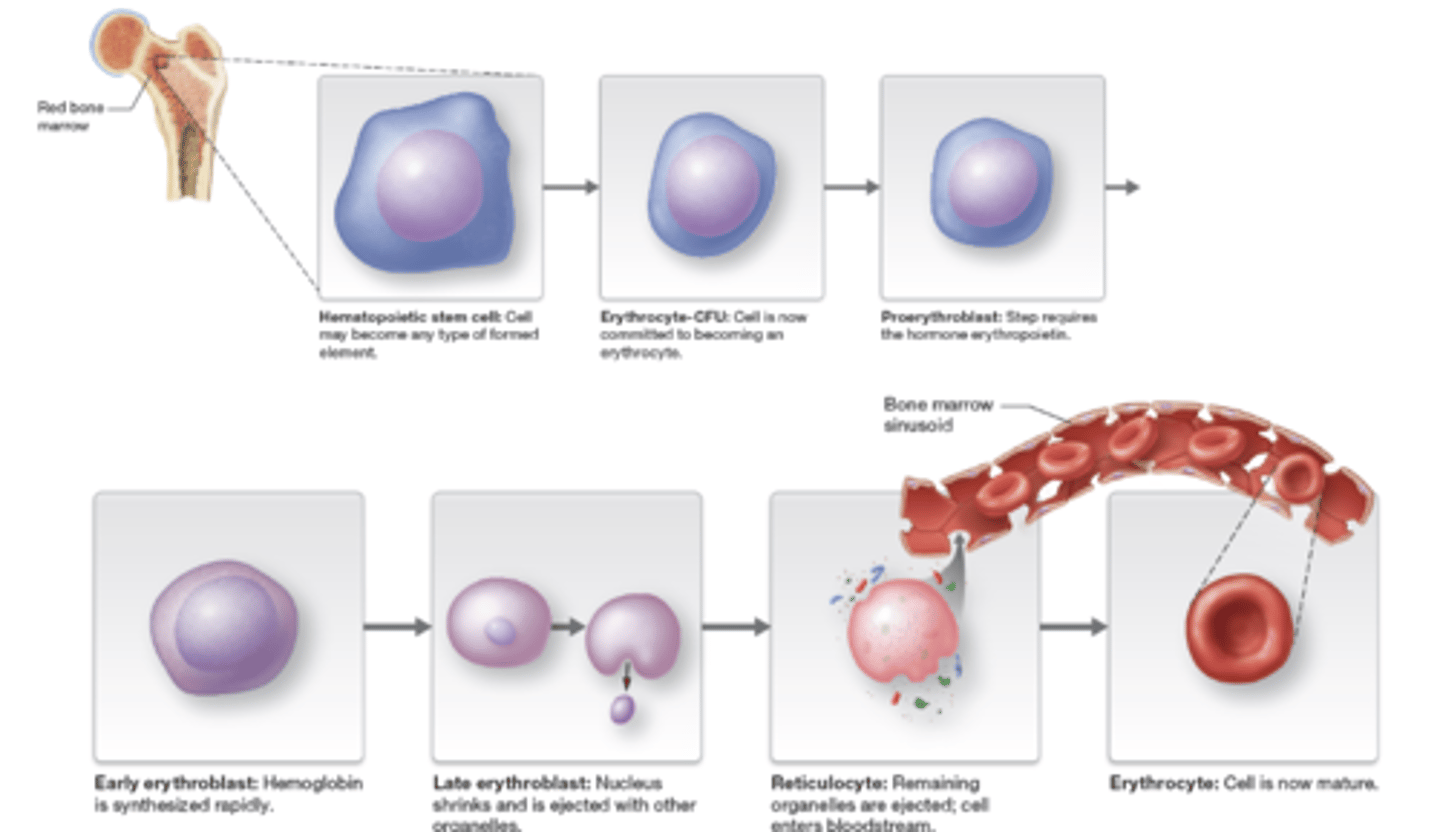
What occurs during the hematopoietic stem cell?
cell can become any type of formed element
What occurs during the erythrocyte-CFU?
cell commits to becoming a erythrocyte
What occurs during the proerythroblast?
requires hormone erythropoietin
What occurs during the early erythroblast?
hemoglobin synthesized rapidly

What occurs during the late erythroblast?
nucleus shrink and is ejected with other organelles
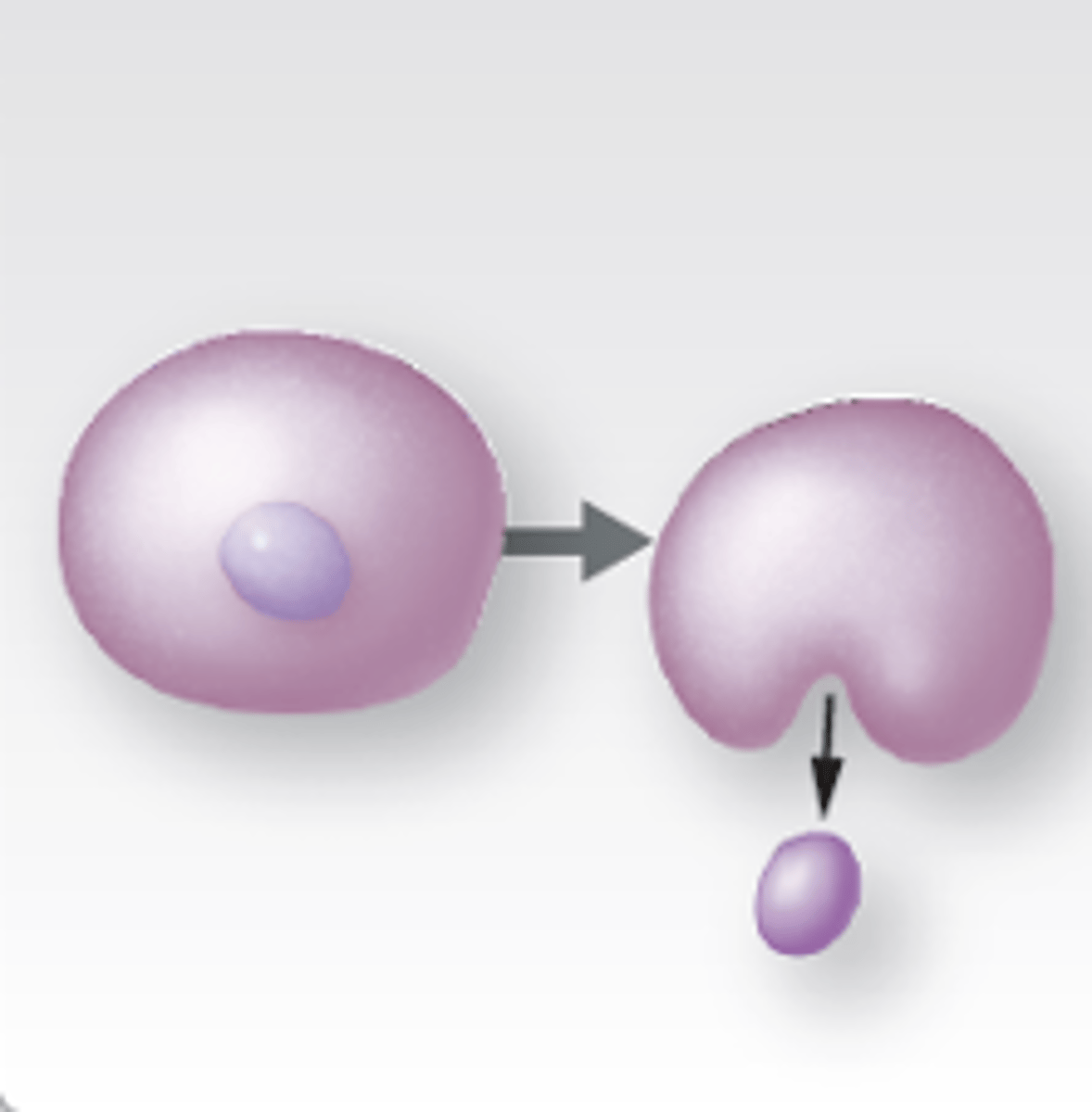
What occurs during the reticulocyte?
remaining organelles ejected; cell enters bloodstream
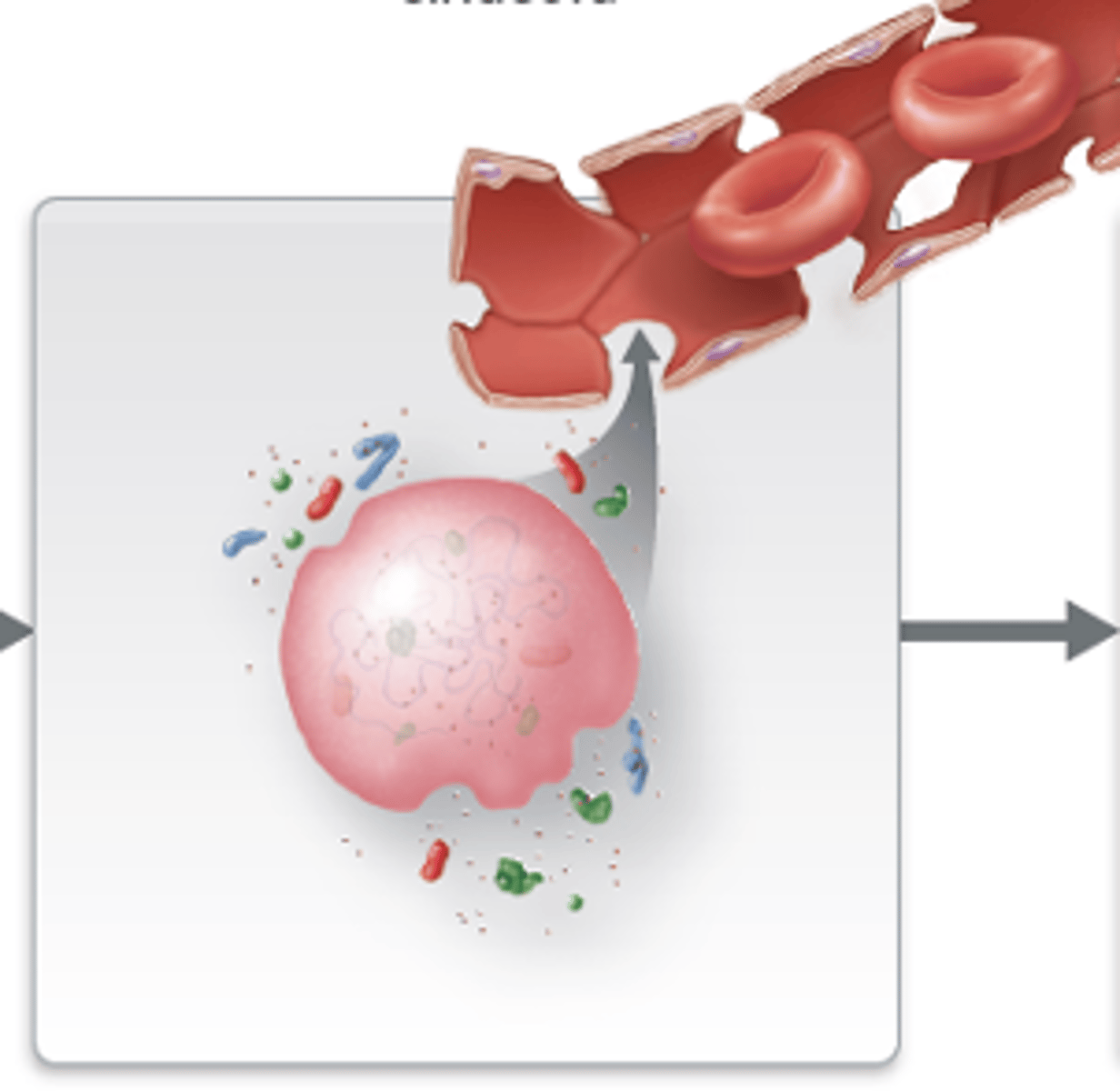
What occurs during the erythrocyte?
cell mature
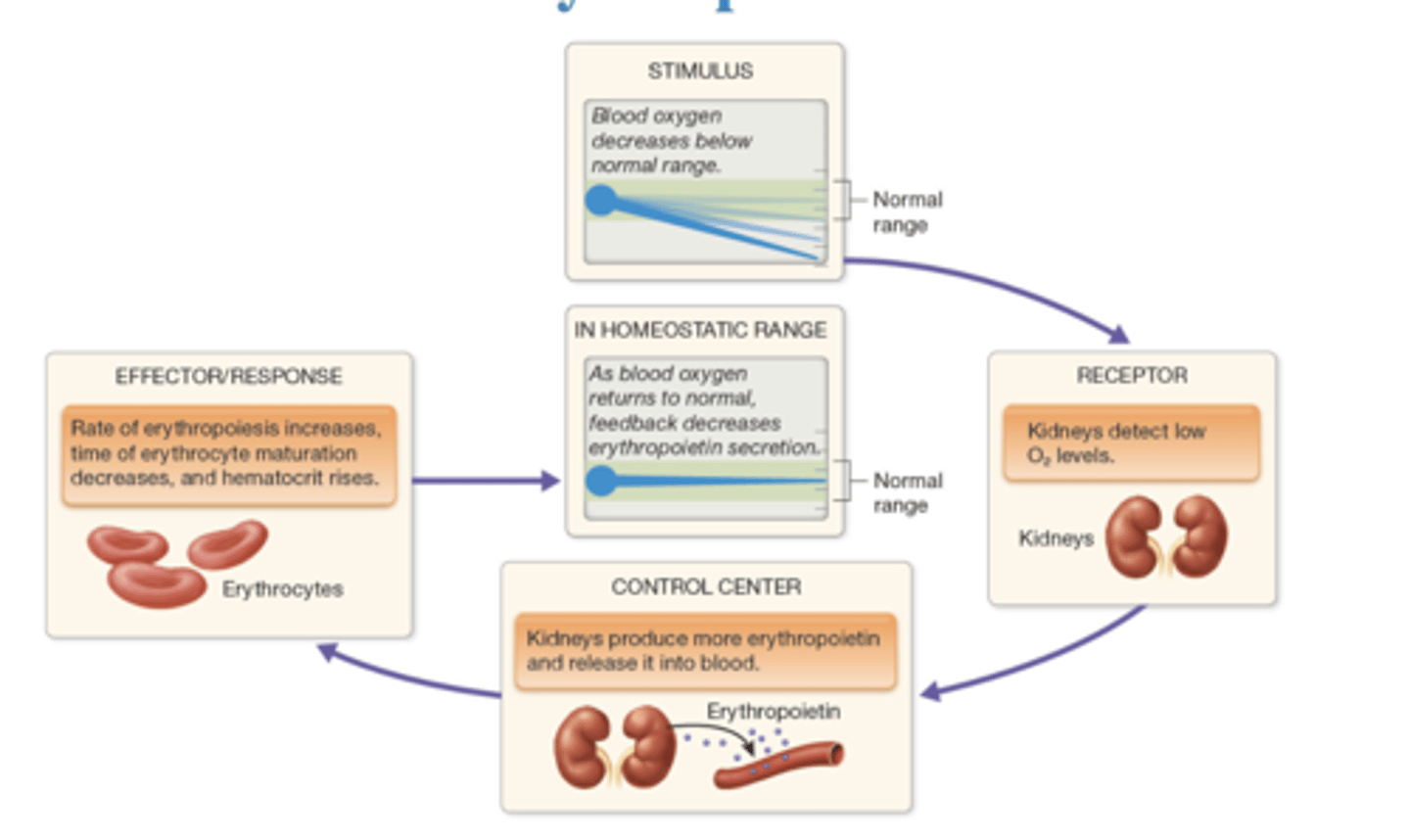
How is erythropoiesis regulated?
blood oxygen is below range, kidneys detect low O2 and produce more erythropoietin for erythropoiesis to raise hematocrit
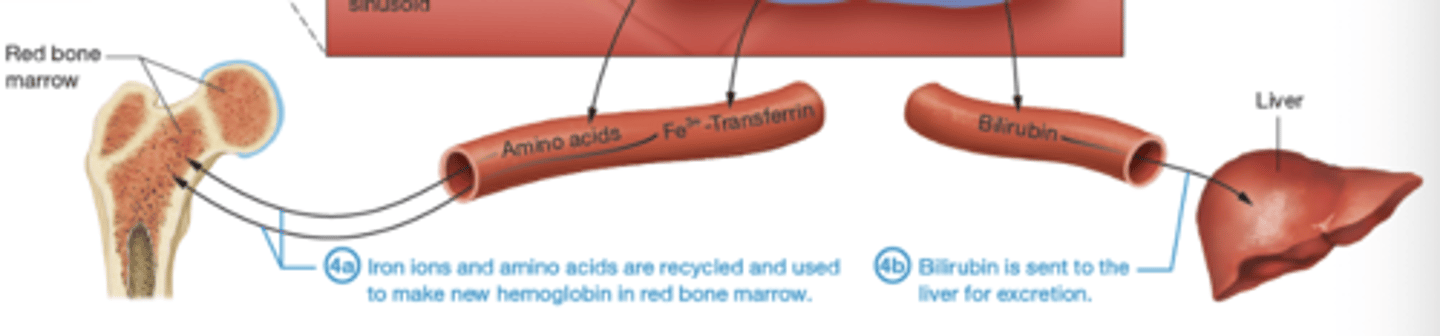
How does erythrocyte death occur?
erythrocytes are trapped in the sinusoids of the spleen so they are digested by macrophages and broken down
What happens to the broken down erythrocytes after death?
iron ions and amino acids recycled for new hemoglobin; bilirubin sent to liver for excretion
What is anemia?
decreased oxygen-carrying capacity of blood
What are the primary causes of anemia?
decreased hemoglobin, decreased hematocrit, and abnormal hemoglobin
What the the symptoms of anemia?
pallor (pale skin), fatigue, weakness, and shortness of breath
How does anemia affect circulating reticulocytes?
elevates it
What are circulating reticulocytes?
immature RBC
What happens to the body in response to diminished oxygen-carrying capacity?
body boosts EPO production
What are the symptoms of severe anemia?
elevated heart rate; body attempts to increase cardiac output to match demand for oxygen from oxygen-deprived tissues
What is the most common form of anemia?
iron deficiency anemia
What is iron deficiency anemia caused by?
inadequate dietary iron intake, reduced intestinal absorption of iron, or slow blood loss
What is decreased hemoglobin Anemia of chronic disease?
interferes with iron transportation from liver to red bone marrow
How does decreased hemoglobin Anemia of chronic disease develop?
result of another underlying disease state, such as cancer
What can cause a decrease of hemoglobin levels?
Vitamin B6 deficiency, malnutrition, poisoning with certain drugs or heavy metals (like lead), and pregnancy can all decrease hemoglobin levels
What factors reduce number of erythrocytes in blood?
blood loss, pernicious anemia, erythrocyte destruction, medication/radiation
How does blood loss reduce number of erythrocytes in blood?
due to number of causes from acute injury to stomach ulcers can lead to significant loss of circulating erythrocytes
How does pernicious anemia reduce number of erythrocytes in blood?
results from vitamin B12 deficiency; interferes with DNA synthesis of rapidly dividing cells, including hematopoietic cells in bone marrow
How does erythrocyte destruction reduce number of erythrocytes in blood?
caused by bacterial infections, diseases of immune system or liver, and lead poisoning; can result in hemolytic anemia
How does medication/ionizing radiation reduce number of erythrocytes in blood?
inhibit or stop production of erythrocytes in red bone marrow; condition called aplastic anemia; cause is often unknown
What is the most common example of abnormal hemoglobin?
sickle-cell disease
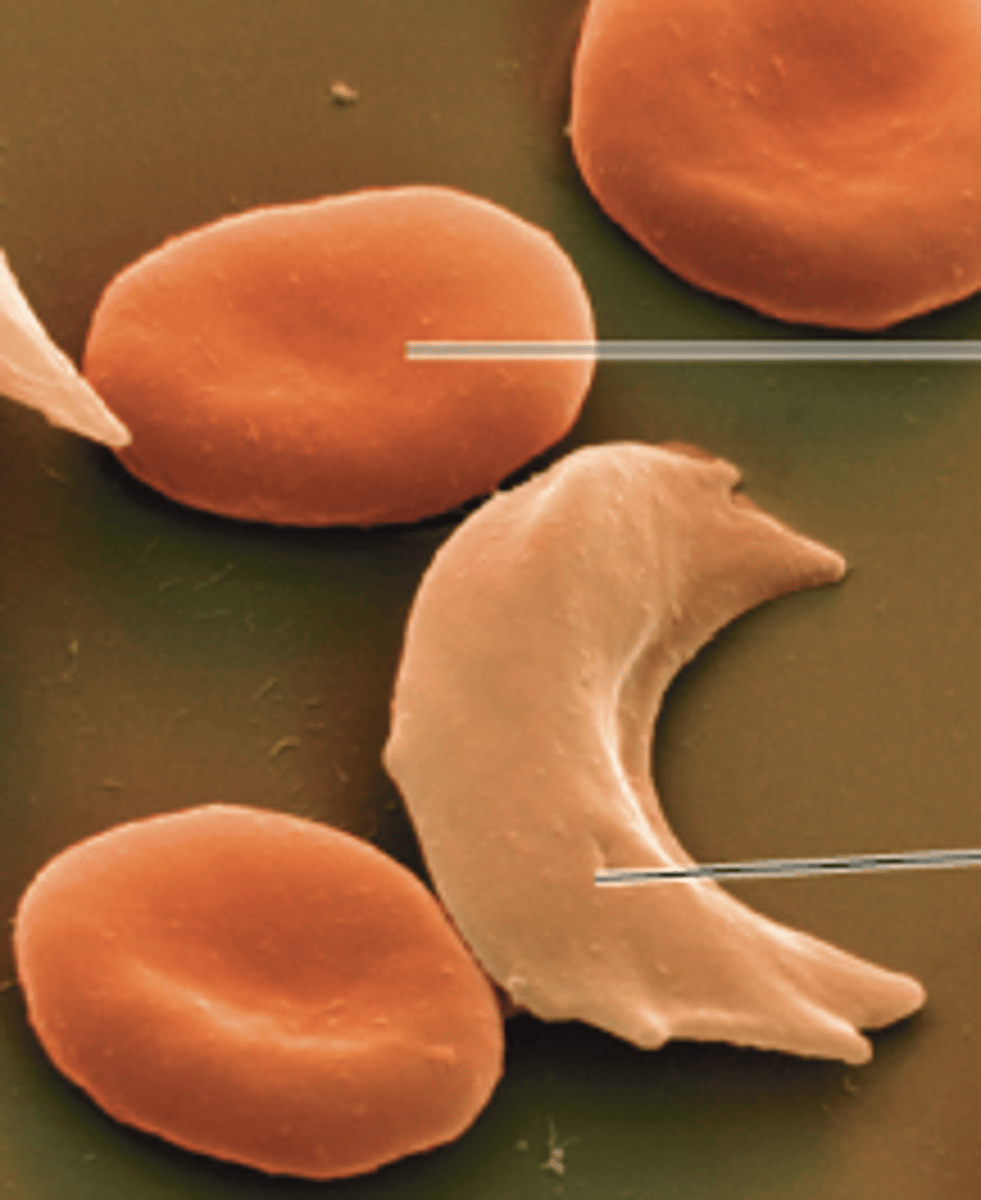
What occurs during sickle-cell disease?
oxygen levels are low, RBCs containing HbS change into sickle shape; leads to erythrocyte destruction in small blood vessels and reduction in circulating erythrocytes
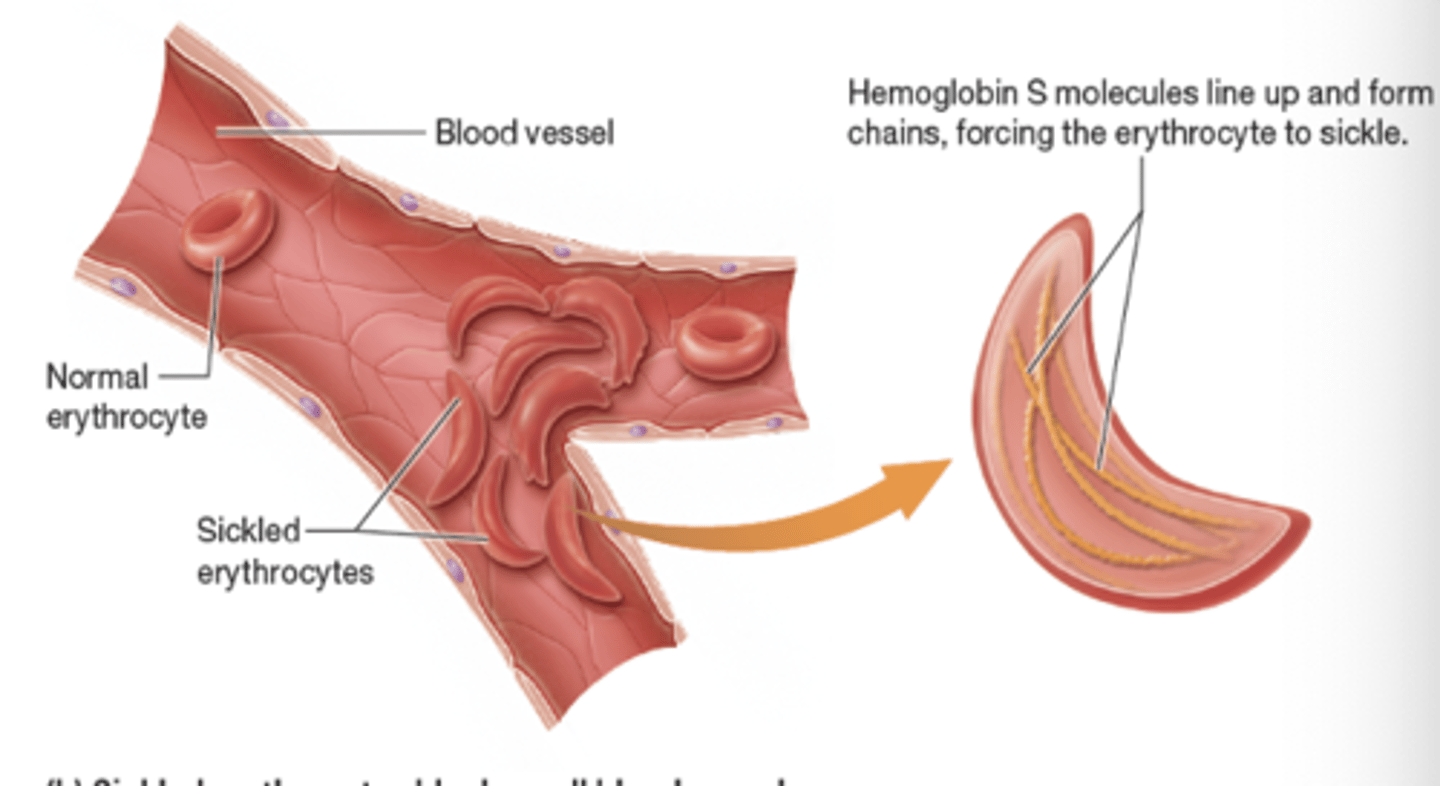
What does sickle-cell disease produce?
hemoglobin S (HbS); abnormal hemoglobin