Cardiology High-Yield Biomedical Sciences Flashcards
1/350
Earn XP
Description and Tags
Biomedical Sciences, Sourced from emma_dip on Quizlet
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
351 Terms
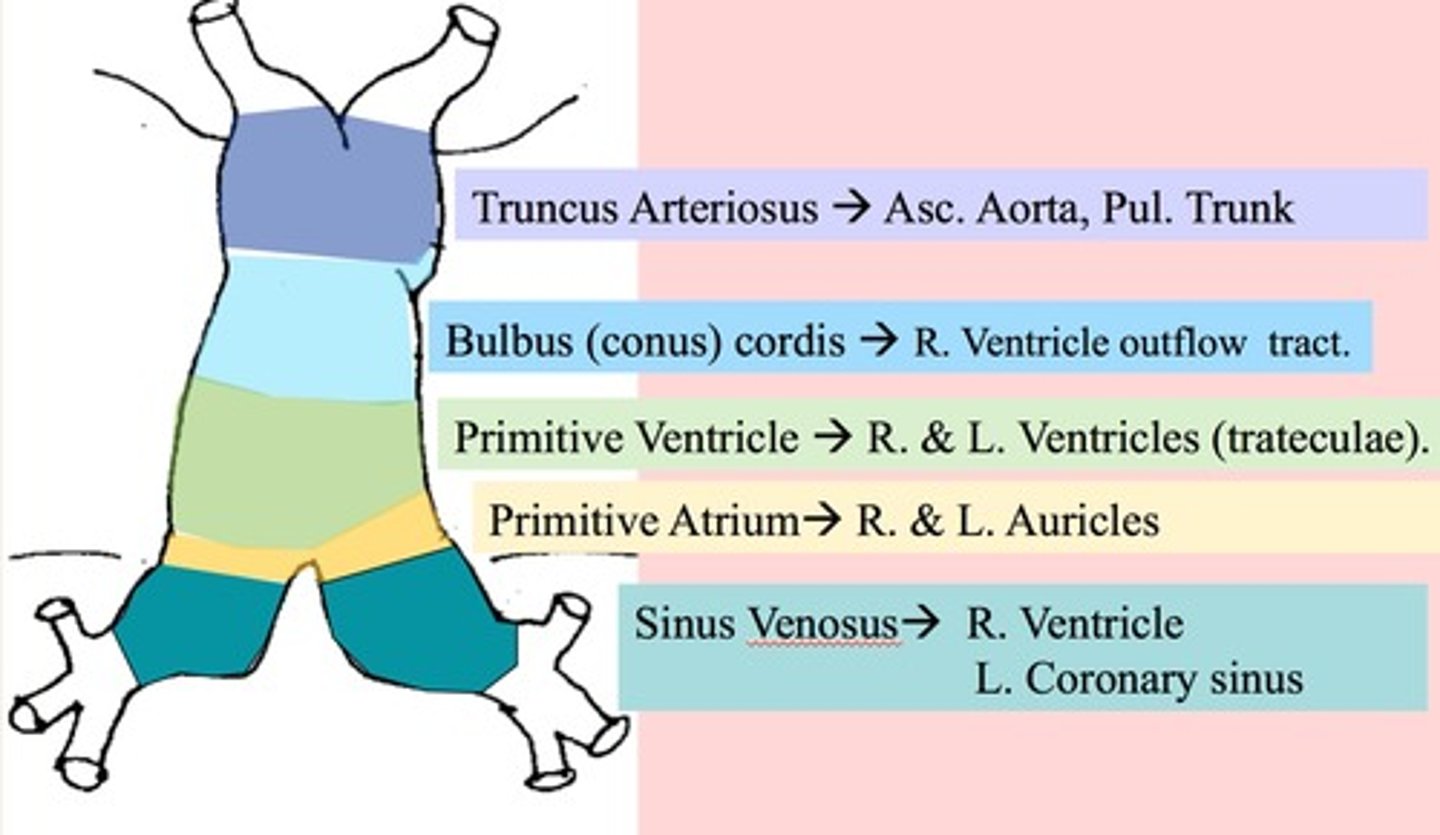
What is a Truncus Arteriosus?
Ascending Aorta and pulmonary Trunk
What is the Bulbus Cordis?
Smooth parts (outflow tract) of the the left and right ventricle
What is the Primitive Atrium is it/ consist of ?
trabeculated part of the left and right atrium
What is the primitive ventricle and what does it consist of?
trabeculated part of left and right ventricles
What does the primitive pulmonary vein form in the embryonic heart?
Smooth part of the left atrium
What does the Left horn of the Sinus Venosus form?
Coronary sinus
What does the Right horn of the sinus venosus form ?
smooth part of right atrium ( sinus venoum)
What 2 embryonic structures form the SVC?
R. Common Cardinal Vein
R. Anterior Cardinal Vein
When does the Heart start to beat in development? (time?)
4 week
Dextrocardia
- what defect is the cause of this?
L/R dynein arm
Dextrocardia
- associated with what syndrome ( cz of this syndrome?)
Kartagener syndrome ( primary ciliary dyskinesia)
-combination of situs inversus, chronic sinusitis, and bronchiectasis
Separation of the Chambers of the embryonic heart
- describe the development
1) Septum primum grows from roof down and in the middle of the foramen primum to form the foramen secundum on top and foramen premium on bottom.
2.) Septum secundum grows from up top down to cover the foramen secundum. The residual is the foramen oval. The Septum premum grows through the foramen primum to be the valve of the foramen oval
3.) septum secundum and primum fuse to form atrial septum
When/how does the foramen oval close in babies?
closes right after birth due to high LA pressures.
If your child has a Patent foramen ovale, what (platelet) risks can occur and how is this treated? Why didn't it close?
most of the time untreated: due to lack of fusion of septum premium and secundum.
- risk of paradoxical emboli
ventricle formation in Embryology
- what is the first thing to form?
- what is the opening called?
-how does this opening close?
- Muscular Ventricular septum forms
-interventricular septum
- The Aorticopulmonary septum will rotate and fuse with the musclar ventricular septum to form a membranous ventricular septum
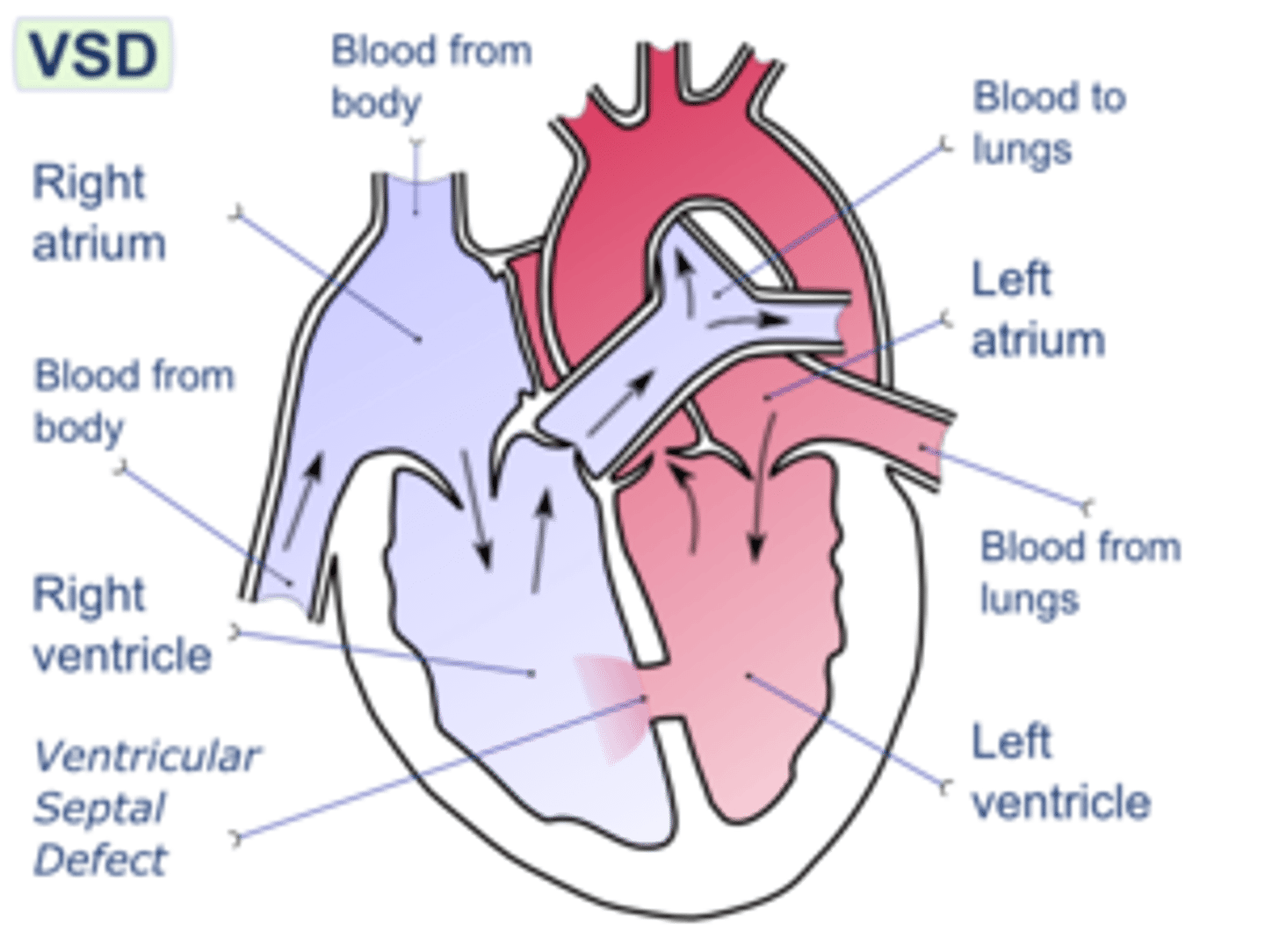
Where do VSDs most commonly occur in (L)?
membranous septum
How does the Outflow tract of the heart form?
Truncus Arteriosus is present then rotates with neural crest and endocardial cell migrations. aorticopulmonary septum formed to give ascending aorta and pulmonary trunk.
How do valves develop in the embryonic heart?
Aortic /pulmonary: from the endocardial cushions of the outflow tract
Mitral/Tricuspid: from fused endocardial cushions of the AV canal
What abnormalities could develop if the outflow tracts of the heart are not formed correctly? (3)
transposition of the great vessels
tetralogy of Fallot
persistent truncus arteriosus
What abnormalities could occur if the valves are not properly developed? (4)
(what syndrome associated with this?)
stenotic, regurgitant, atretic, displaced
( Ebstein anomaly)- ASD with tricuspid regurge
What is the mnemonic for remembering Fetal erythropoiesis site development?
Young Liver Synthesizes Blood
Yolk Sac
Liver
Spleen
Bone Marrow
What is the Fetal erythropoiesis site development?(time line)
Yolk Sac ( 3-8 weeks)
Liver (6 weeks- birth)
Spleen ( 10-28 weeks)
Bone Marrow (18 weeks-adult)
Hemoglobin development
-what type of globins does the Embyro have? (2)
- What type of globins does the Fetal hemoglobin have? (2)
embryo: zeta and epsilon
Fetal: alpha 2 and gamma 2
Hemoglobin development
- what type of Hg does the adult have?
- adults: alpha2 and Beta 2
Describe the binding and affinity of HgF
- what is the mneumonic for Fetal--> Adult hemoglobin?
HgF has a higher affinity for O2 due to less binding of 2,3-BPG.
-M: Alpha Always: Gamma Goes, Becomes Beta.
Describe the Fetal Circulation travel route?
What is present is the ductus arteriosus and the foramen ovale.
- From the aorta to the umbilical arteries to the placenta then umbilical veins to the ductus venosus.
- the umbilical vein: high O2
-the umbilical artery: low O2
What is the pressure of o2 in the umbilical vein? saturation?
30mmHg with 80% saturation
How does the foramen ovale and ductus arteriosus close at birth?
the infant takes a breath in and there is a decrease in Resistance in the pulmonary vasculature, increase in LA pressure which closes the Foramen ovale.
- the ductus arterioles closes after there is a increase in O2 which will decrease prostaglandins = closure
What medication will close the ductus arterioles if there is failure? What would keep it open?
indomethacin
-Prostaglandins
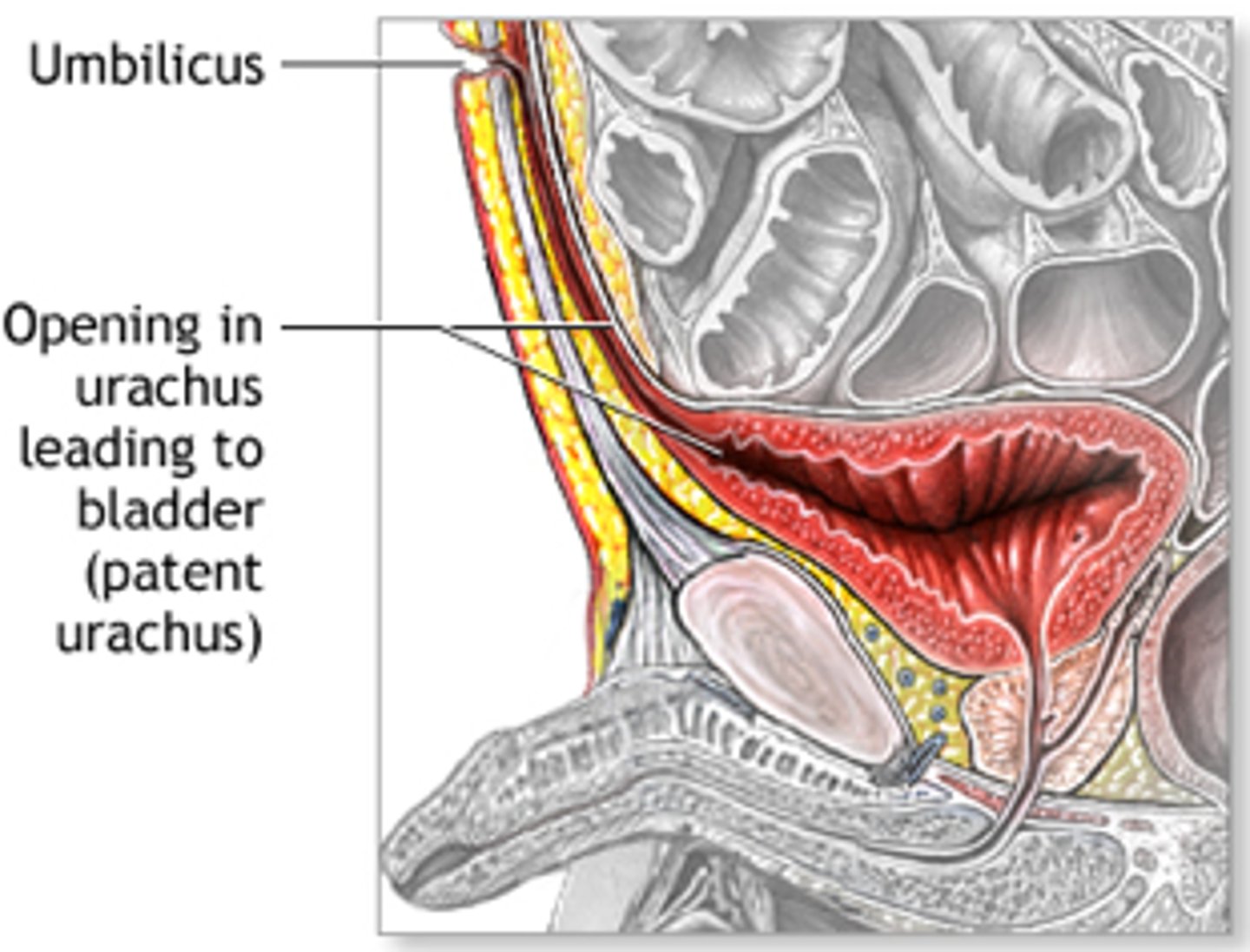
What does the Allantois become?
-> what remnant is left of this?
--> What is the urachus btw?
Allantois --> urachus
Median umbilical ligament
urachus is part of allantoic duct btw the bladder and umbilicus.
What does the Ductus Arteriosus leave as remnant?
Ligamentum Arteriosum
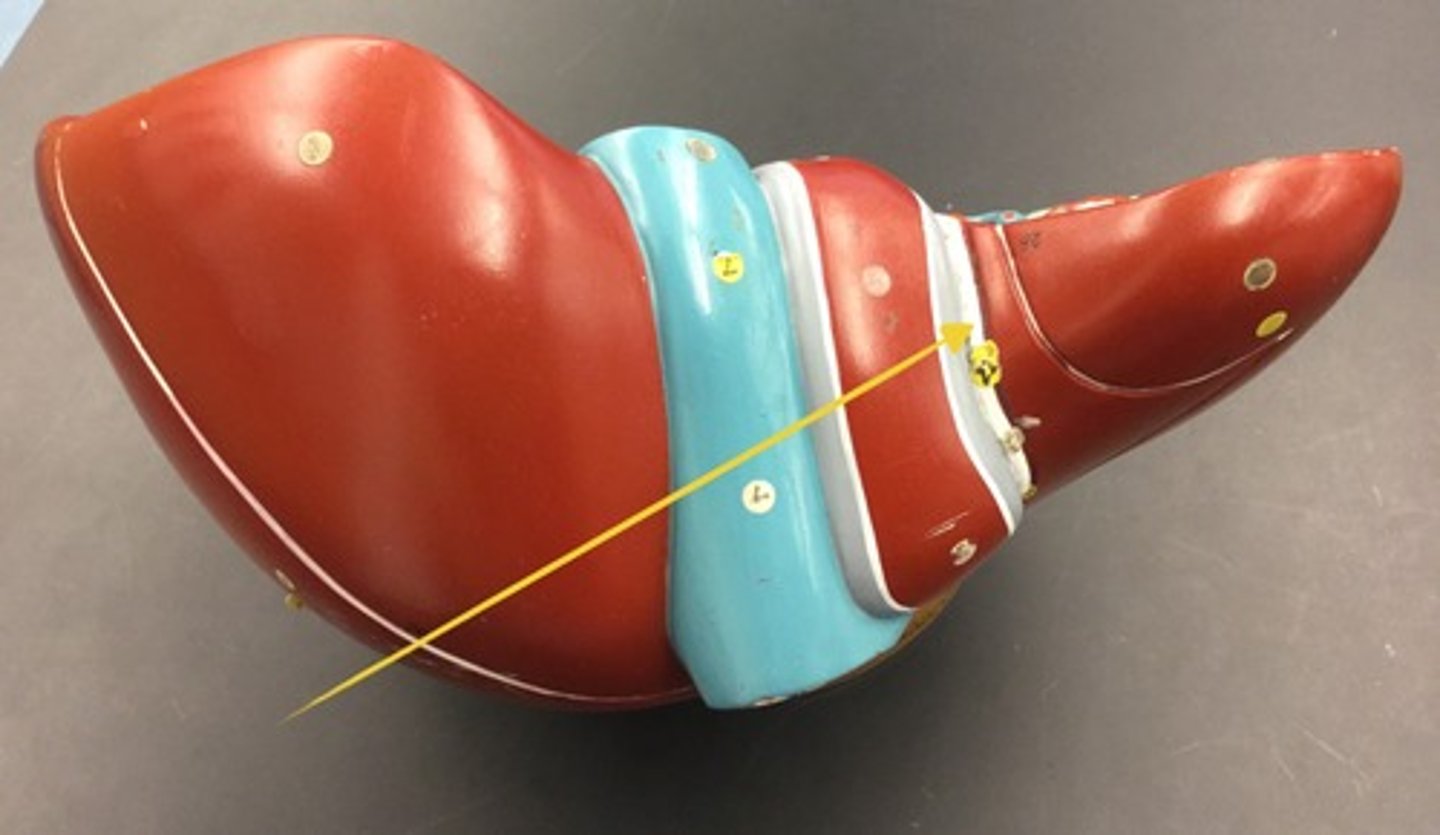
What is the Ligamentum venosus a remnant of ?
Ductus venosus
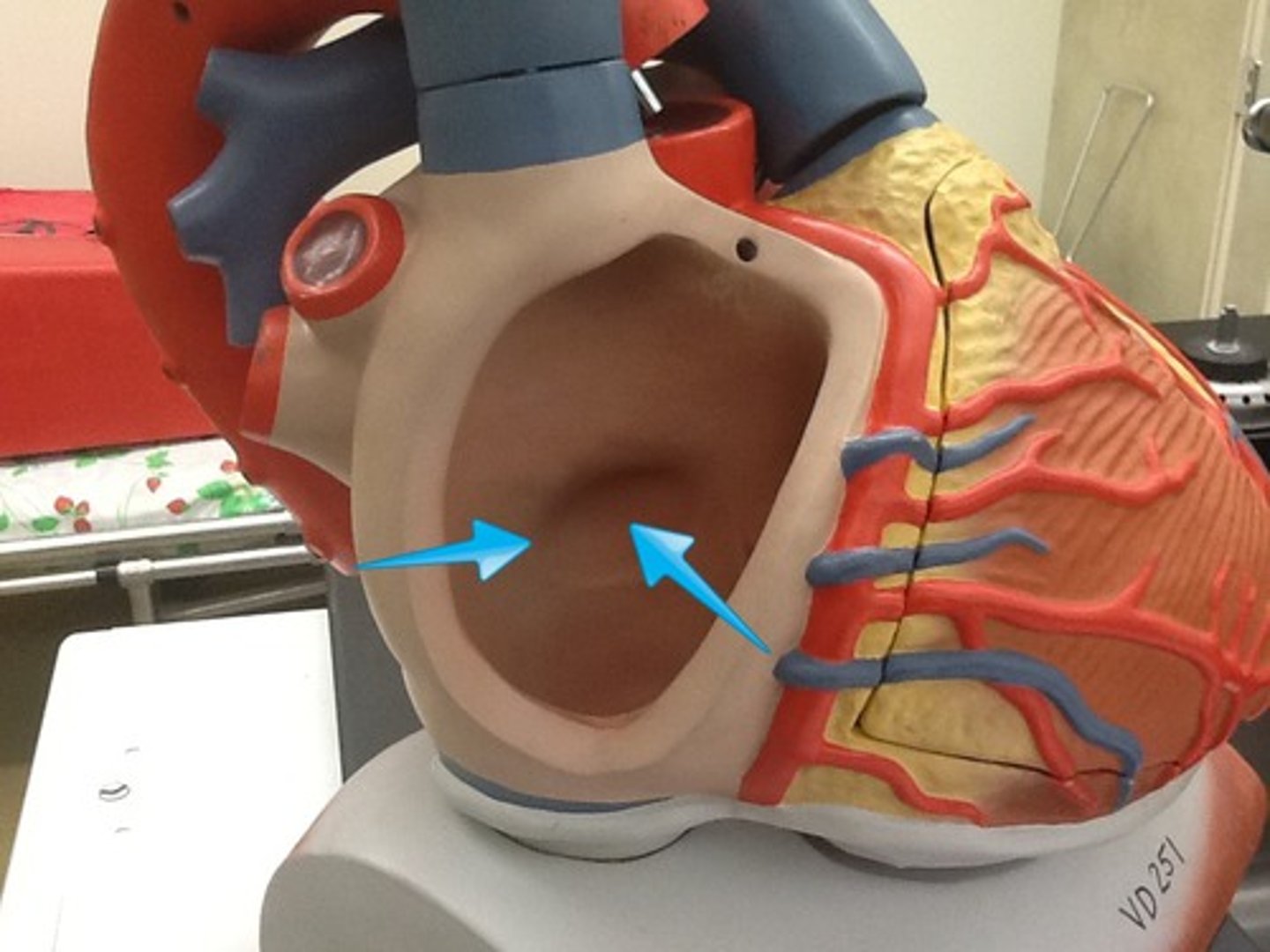
What remnant does the Foramen ovale leave?
Fossa ovalis
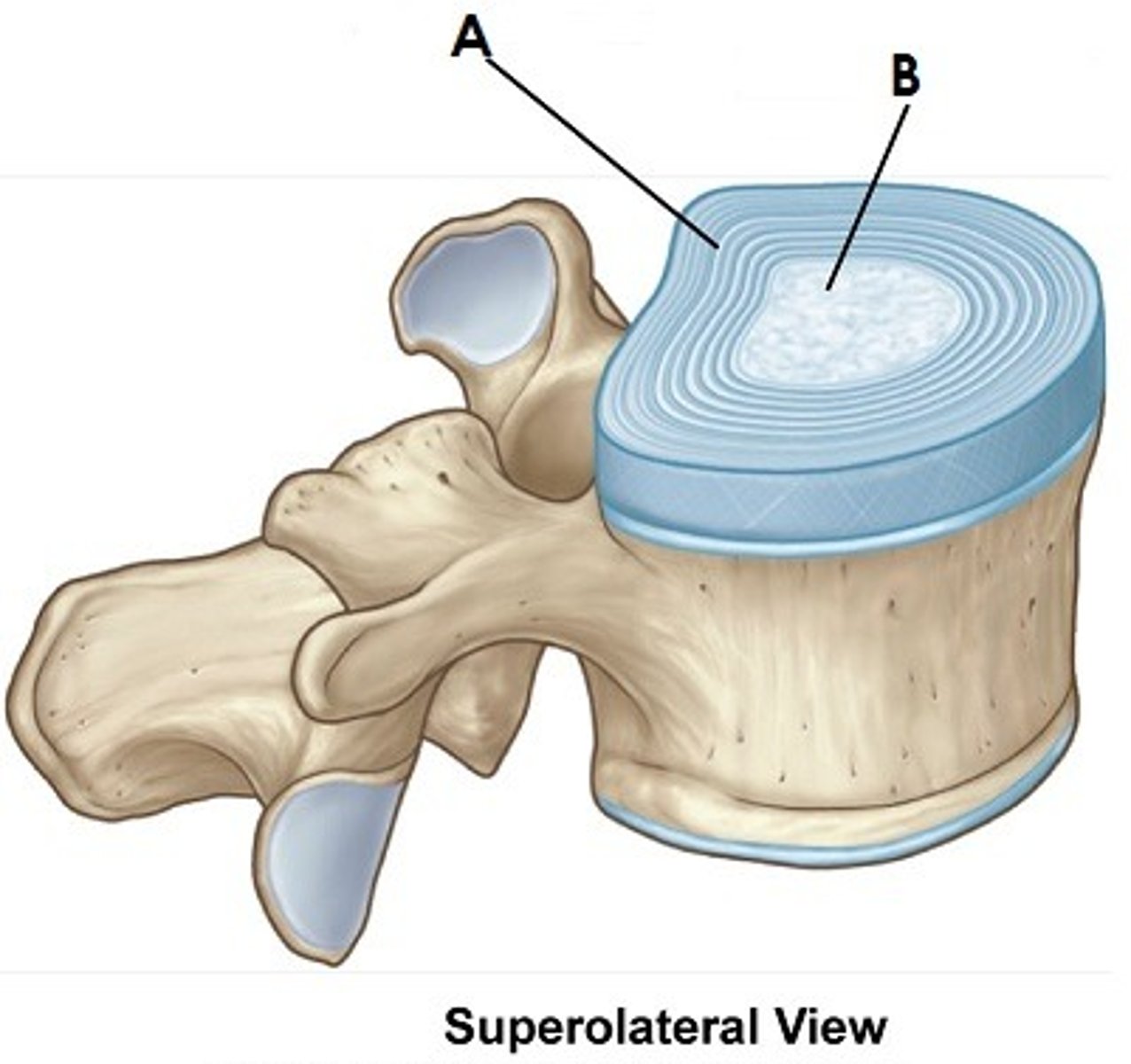
What remnant does the Notochord leave?
Nucleus pulposus
What is the Medial umbilical ligament a remnant of?
umbilical arteries ( L*)- (ligaments are tough and arteries are tougher than veins)
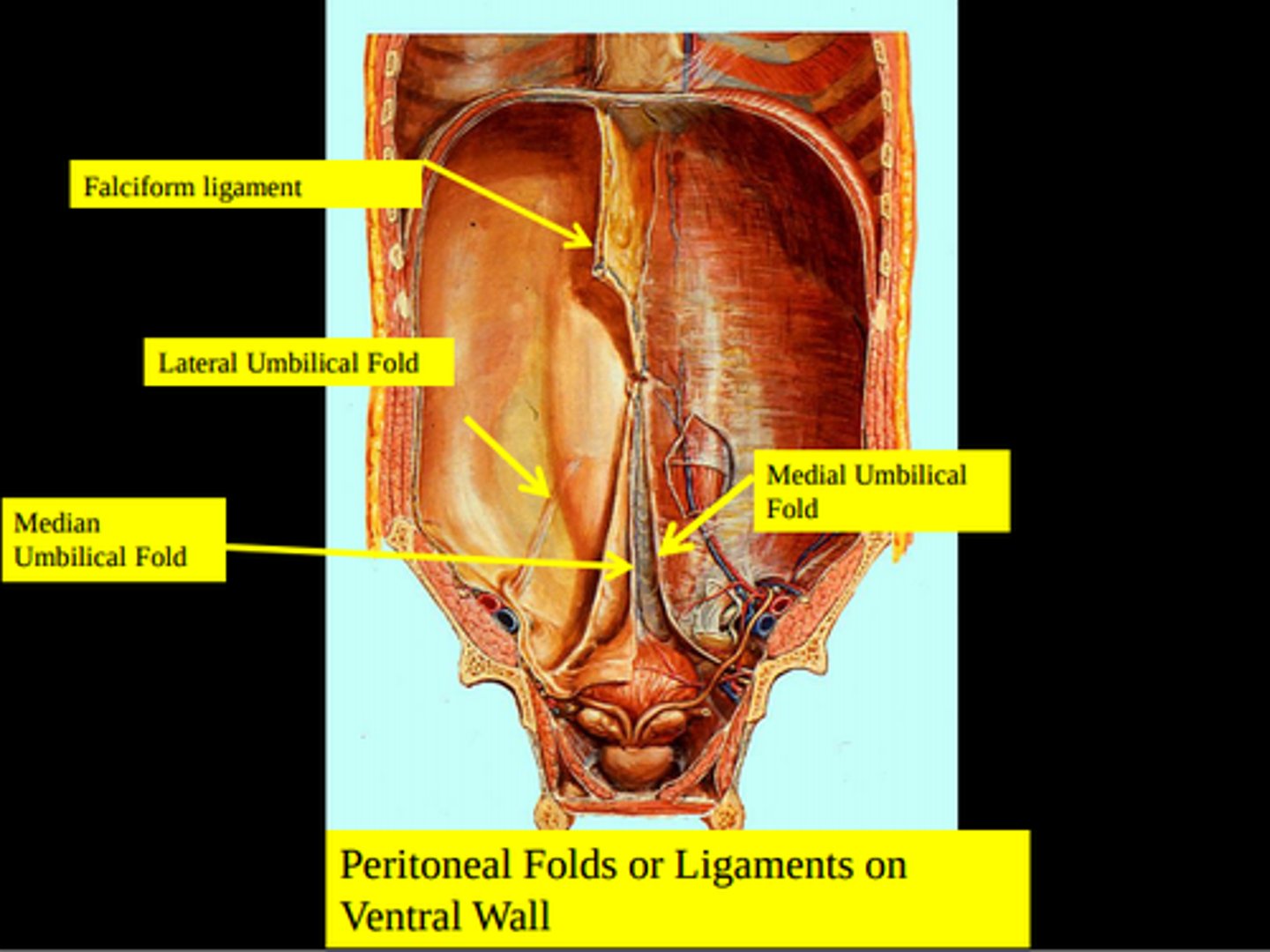
What does the Umbilical Vein form as a remnant?
Ligamentum teres hepatic within the falciform ligament
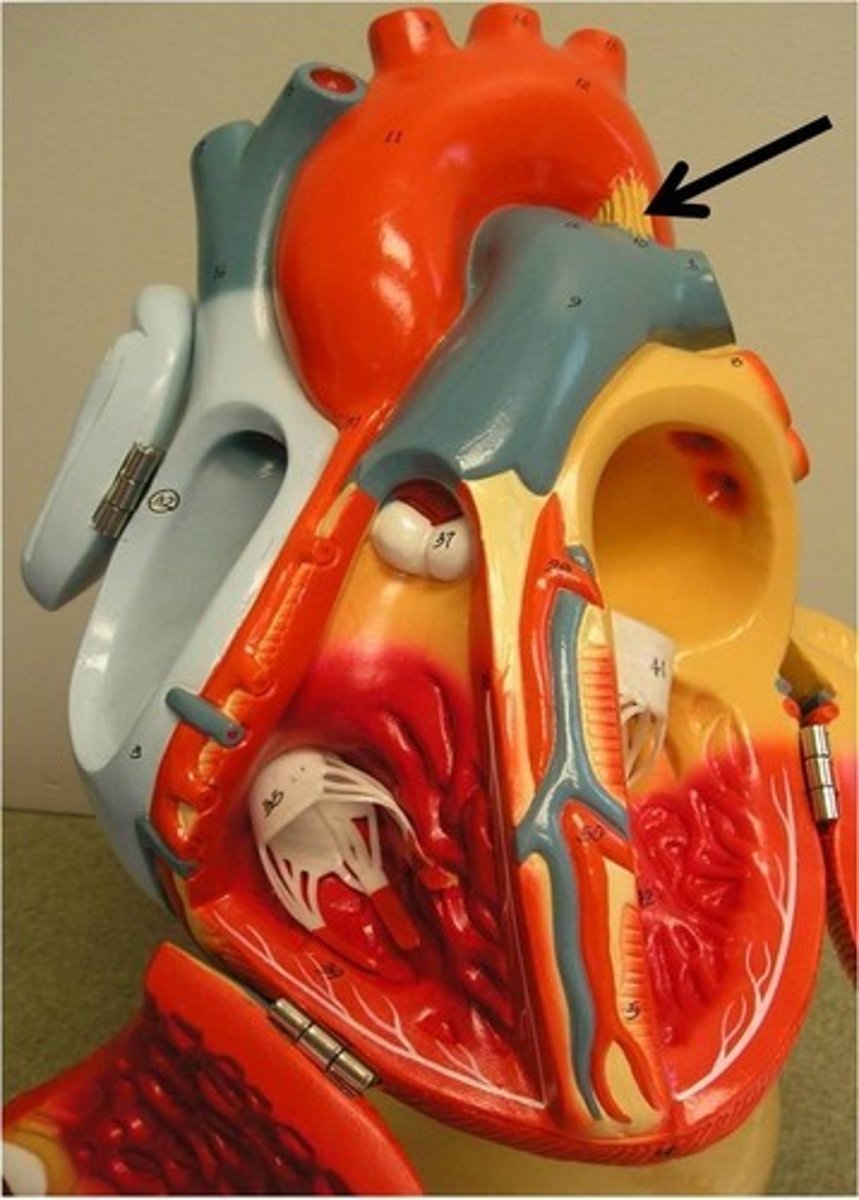
Blood supply of heart? - Coronary Arteries
Makes up capillary network
Lies directly beneath myocardial surface, and coronary veins
2 coronary arteries: originate from ascending aorta:
- Right Coronary Artery, from ant. aortic sinus
- Left Coronary Artery, post. aortic sinus
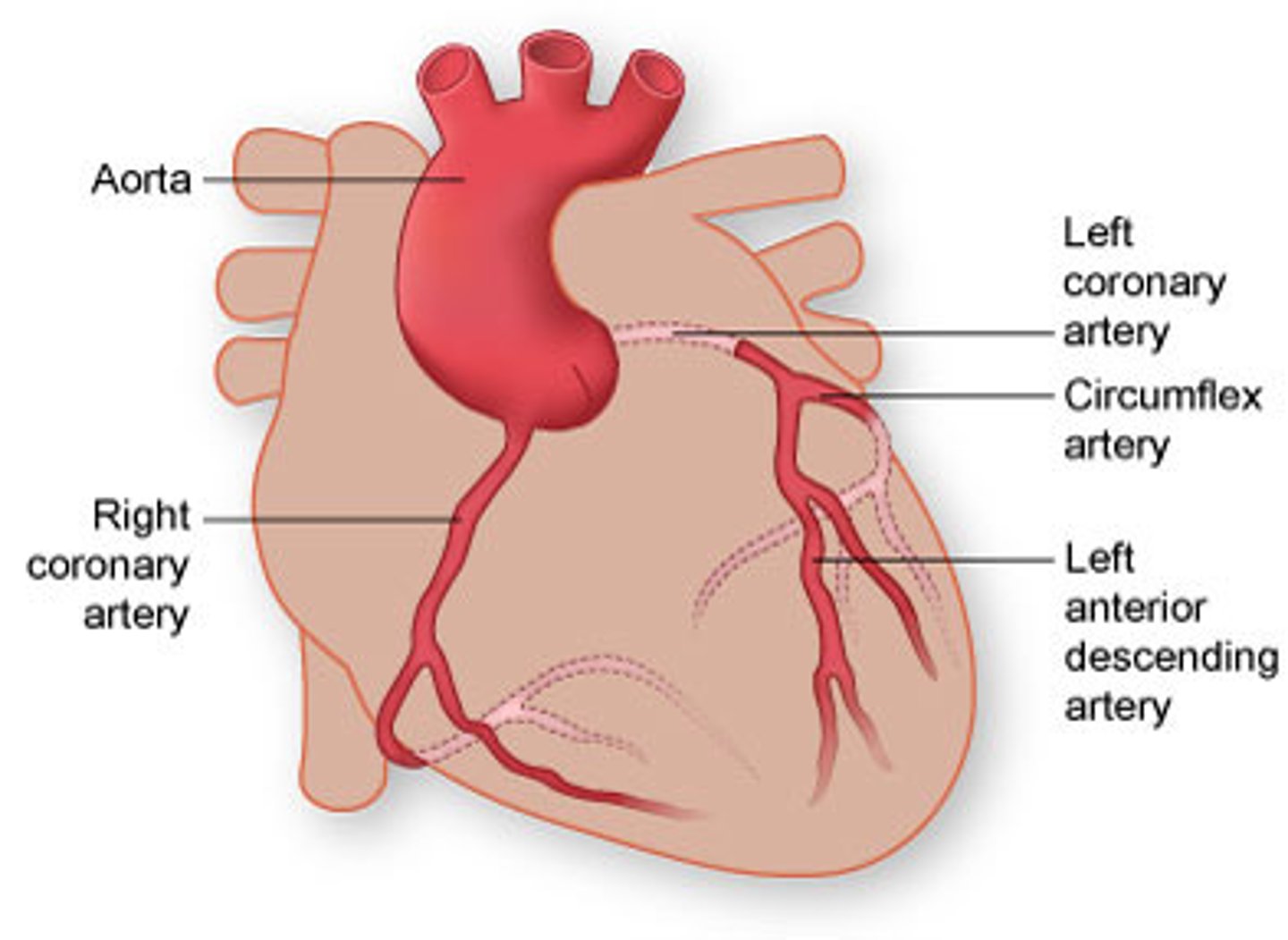
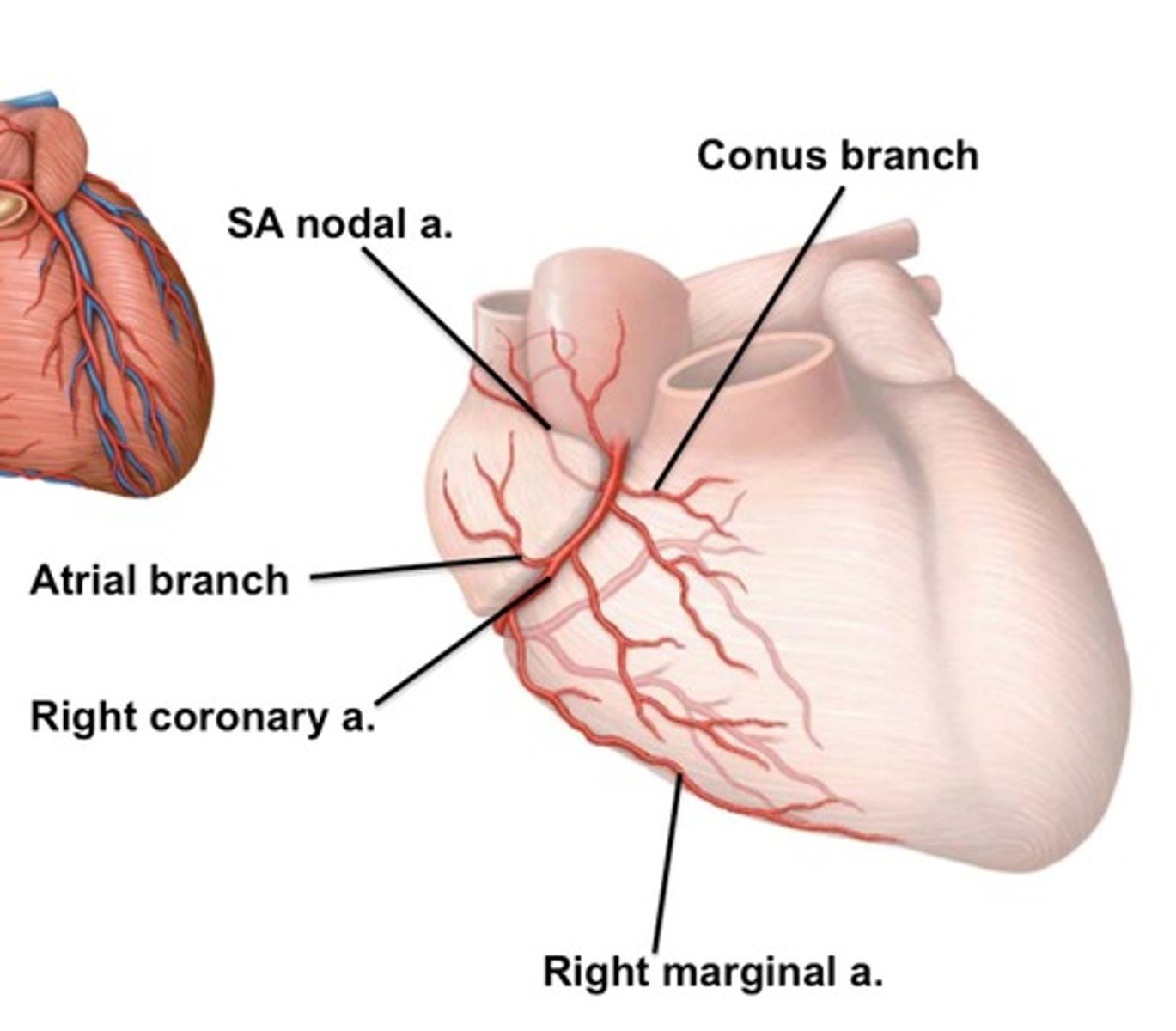
Blood supply of heart- Right Coronary Artery? - origin, pathway
Origin: above right cusp of aortic semilunar valve
Pathway: Runs in coronary sulcus next to right auricle downwards to the right turns to diaphragmatic surface.
Blood supply of heart- Right Coronary Artery? - branches and their supply
Right Conus Branch:
-ant. surface of infundibulum of pulmonary trunk
Anterior Ventricular Branches:
- ant. surface of right ventricle
Right marginal branch:
- a terminating branch
-lat. wall of right ventricle
Atrial branches:
- Right atrium
-> Sinoatrial Node Branch
Posterior Ventricular Branches:
- Diaphragmatic surface of right and left ventricles.
Posterior interventricular artery:
-Post. part of interventricular septum, AV-node, right (and left) ventricles
-a terminating branch
-> Atrioventricular nodal branch
Left Coronary Artery? - Origin, pathway, branches
Origin: above left cusp of aortic semilunar valve.
Pathway: Runs bellow left auricle. Splits into two main branches:
- Anterior Interventricular branch: in iv. sulcus to apex
-Circumflex Branch: in coronary sulcus to the left and downwards
Blood supply of heart - Left Coronary Artery? - Supply
Anterior interventricular artery/Left ant. descending a. (widow-maker):
-ant. part of interventricular septum
-left (and right) ventricle
-> diagonal artery
Circumflex artery
Left marginal artery:
-left ventricle
Left atrial branches:
-left atrium
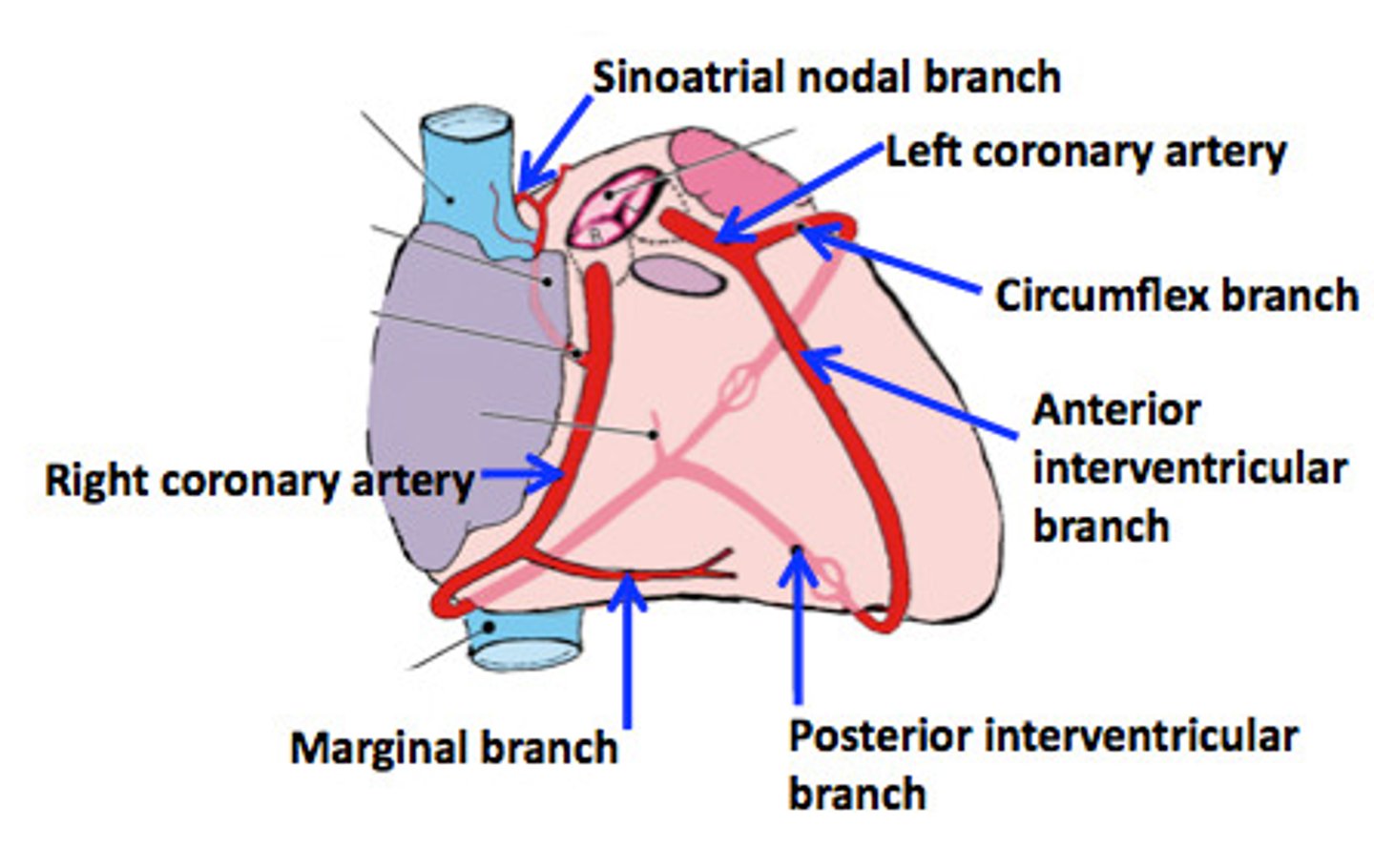
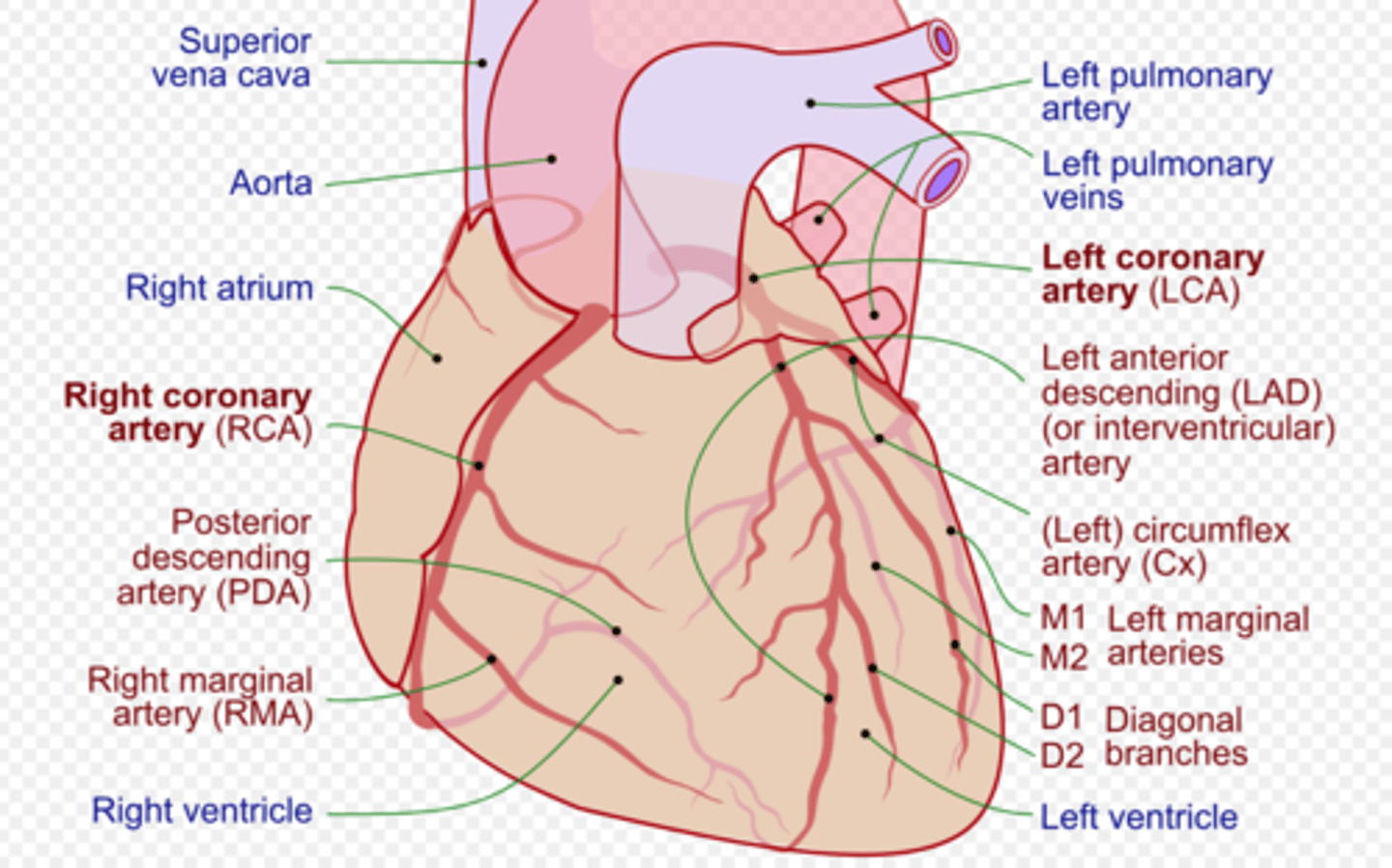
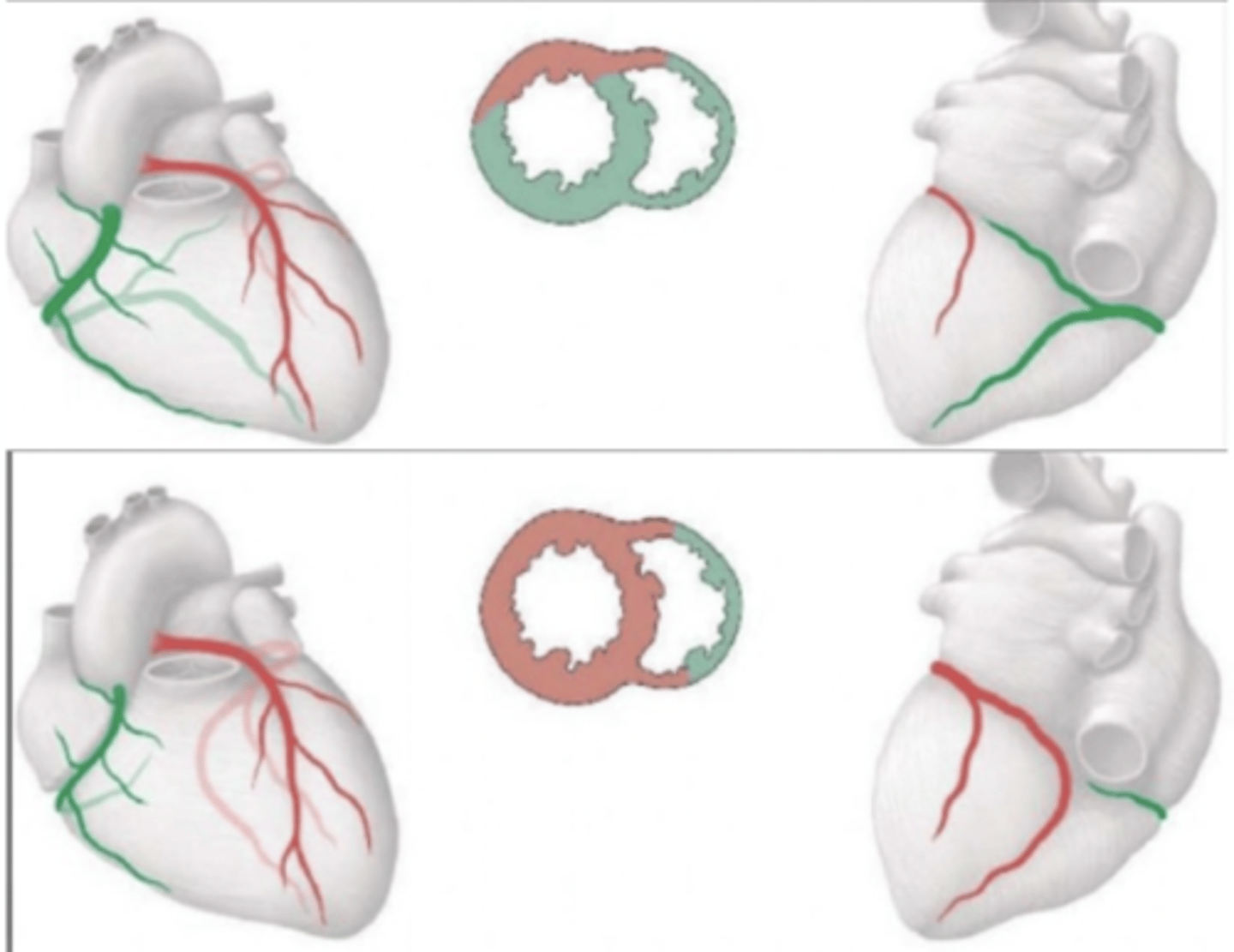
Right and left Coronary Dominance? Clinical importance
Every people has either the left- or the right interventrcular dominating the supply of the heart.
These arteries are anastomosing, so if one of them is blocked the other one cannot supply anyways
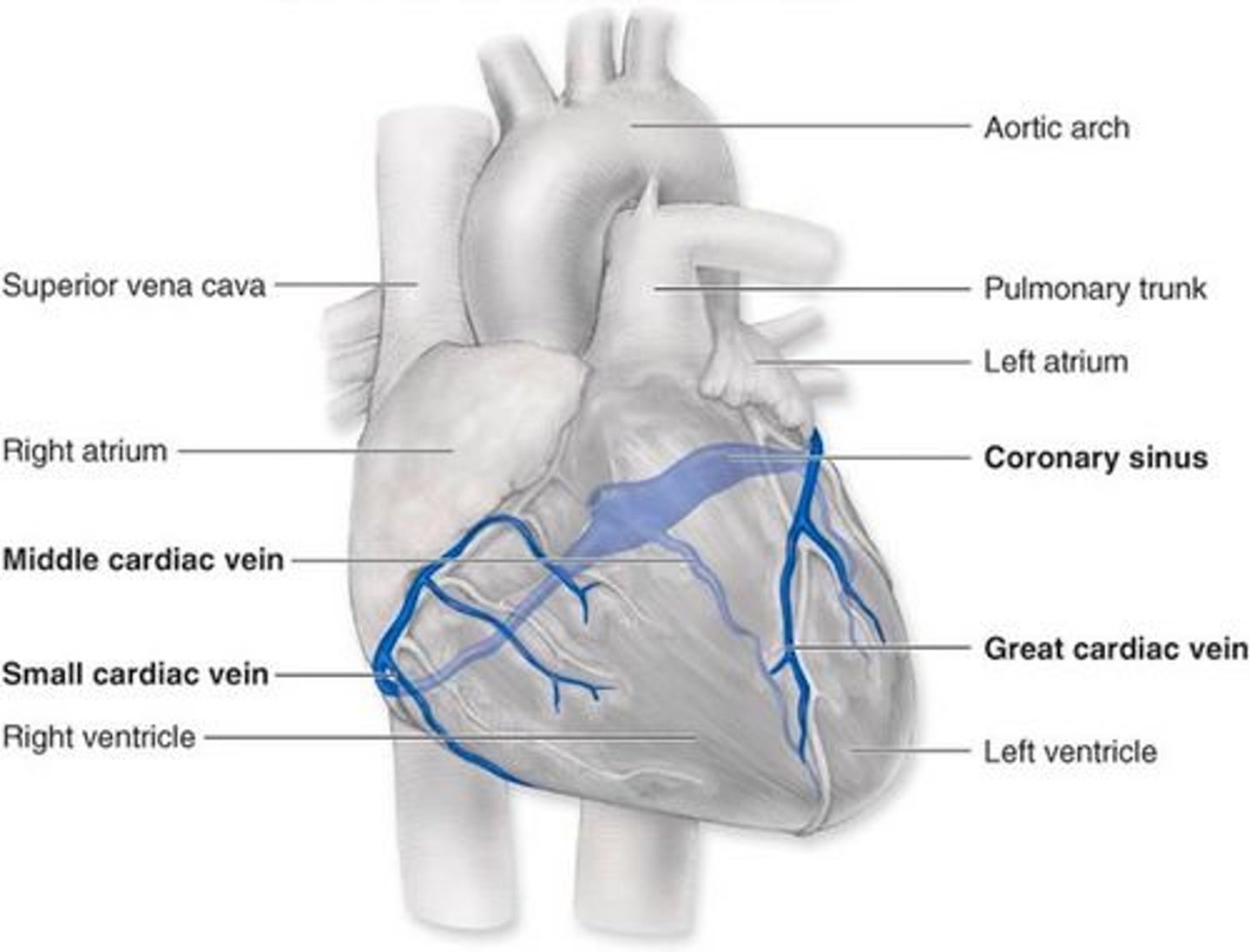
Venous Drainage of The Heart that empties in the coronary sinus? What area does it drain from? What artery does it accompany?
Great cardiac vein:
-Start: Apex
-Drains: Ant. of left atrium
- Joins: Ant. interventricular a. and circumflex a. in ant- iv. sulcus
-enters Cor. sinus on left side
-Olbique/Marshal vein of left atrium joins it
Middle cardiac vein:
-Start: Apex, post. iv. sulcus
-Drain: Post of right ventricle
-Accomp.: Post. iv. a.
-Joins: Small card. c.
-enters Cor. sinus on right side
Small cardiac vein:
-Drain: Right ventricle
-Accomp: Right ventricular a. in coronary sulcus
Posterior vein:
-Post. of Left ventricle
-On diaphr. surface (joins middle card. vein)
Right- and left marginal vein
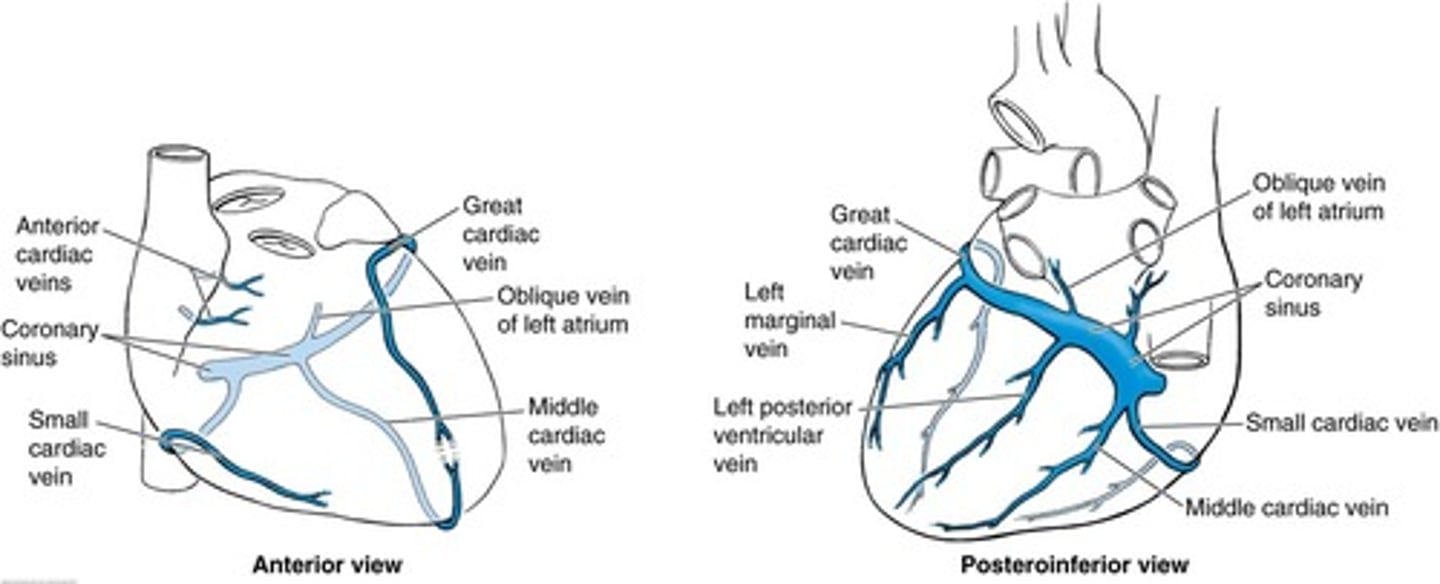
Small veins mainly from atrial walls that doesn't drain into coronary sinus (open directly into atrial cavities)?
Anterior Cardiac Veins:
-Small veins of right atrium and -ventricle
Smallest Cardiac Veins (Thebesian veins):
-Drain venous blood from walls into cardiac cavities (all chambers)
-responsible for minimal shunt circulation (venous blood mixed to oxygenated blood).
What does the left anterior descending artery supply? What does it branch from?
Branches from left coronary artery
Supplies:
-anterior 2/3 of intraventricular septum
-anterolateral papillary muscle
-anterior surface of LV
-m/c occluded
What does the posterior descending artery supply? What does it branch from?
Branches from right coronary artery
Supplies:
-AV node (depending on dominance)
-posterior 1/3 of intraventricular septum
-posterior 2/3 walls of ventricles
-posteromedial papillary muscle
What does the right coronary artery supply?
-SA node (independant of dominance)
-infarct may cause nodal dysfunction (bradycardia or heart block)
-right (acute) marginal artery (branches off RCA) supplies right ventricle
Describe the 3 different types of dominance in blood supply to the heart
1. Right dominant circulation
-85%
-PDA (posterior descending artery) arises from RCA (right coronary artery)
2. Left dominant circulation
-8%
-PDA arises from LCX (left circumflex artery - branches from left anterior descending artery (LAD))
3. Codominant circulation
-7%
-PDA arises from both RCA AND LCX
Source of oxygen and nutrients for fetus during gestation
- fetal lungs not in use
-fetus obtains nutrients from the mother via placenta & umbilical cord
-blood from placenta carried to fetus via umbilical vein ( attached to umbilical cord, attached to placenta)
umbilical cord
-contains 2 arteries & 1 vein
(umbilical vein, 2 umbilical arteries)
umbilical arteries function
-carry deoxygenated blood and waste products away from the fetus
umbilical vein function
-carries oxygenated blood and provides O2 and nutrients to the fetus
Placenta
-provides for exchange of nutrients and waste products between the fetus and the mother
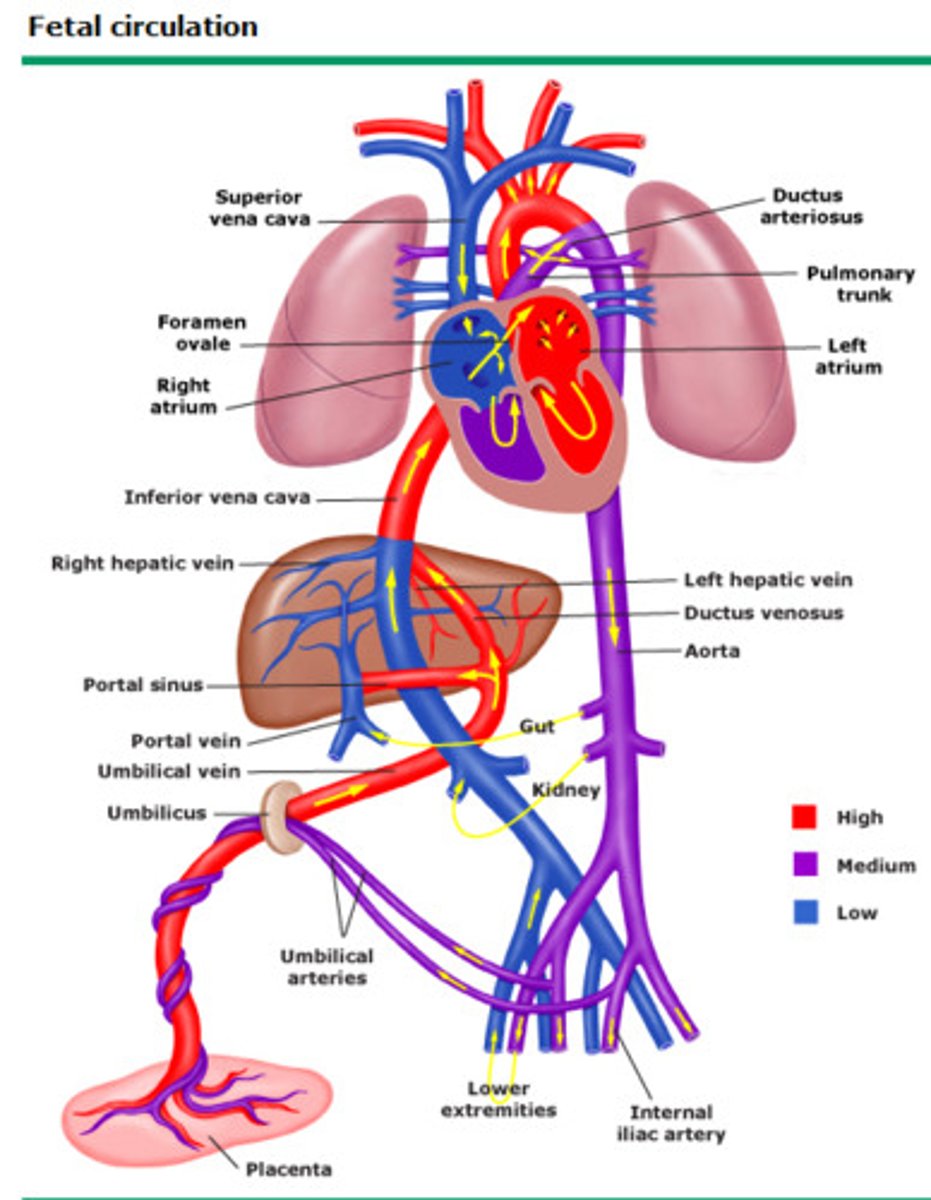
Veins that bring blood into fetal heart
-umbilical vein --> (via ductus venosus shortcut in liver) inferior vena cava --> right atrium
-superior vena cava
Arteries that take blood away from heart.
-pulmonary artery (via ductus arteriosus) --> aorta
-LV --> aorta
-aorta --> umbilical artery--> placenta
Where does the blood returning from lower limbs go
Inferior vena cava --> Right atrium --> foramen ovale --> left atrium --> left ventricle --> aorta -->
OR
RA--> RV --> Pulmonary artery --> ductus arteriosus --> aorta
Ductus venosus
connects the umbilical vein and the inferior vena cava, bypassing the liver
Foramen ovale
the opening between the right and left atria of the heart, bypassing the lungs
Ductus arteriosus
connects the pulmonary artery to the aorta, bypassing the lungs
5 fetal circulation adaptations prior to birth
1. umbilical vein
2. ductus venosus
3. foramen ovale
4. ductus arteriosus
5. umbilical artery
Trace the path of a red blood cell coming in from the placenta to the right atrium, and back to the placenta.
1. red blood cell absorbed from mom's blood pool by fetal capilaries in placenta
2. enters umbilical cord via umbilical vein
3. UV branches into inferior vena cava
4. RBC goes from IVC to right atrium
(can be squeezed to right ventricle
--> enters pulmonary artery-->blood approaches lungs *but does not go in & is shunted from Pulmonary artery to aorta) OR
5. from RA --> foramen ovale --> left atrium --> LV --> aorta
6. goes to legs & internal iliac arteries
7. major branch of iliac arteries RBC & most blood leaves via is the placental branch umbilical artery
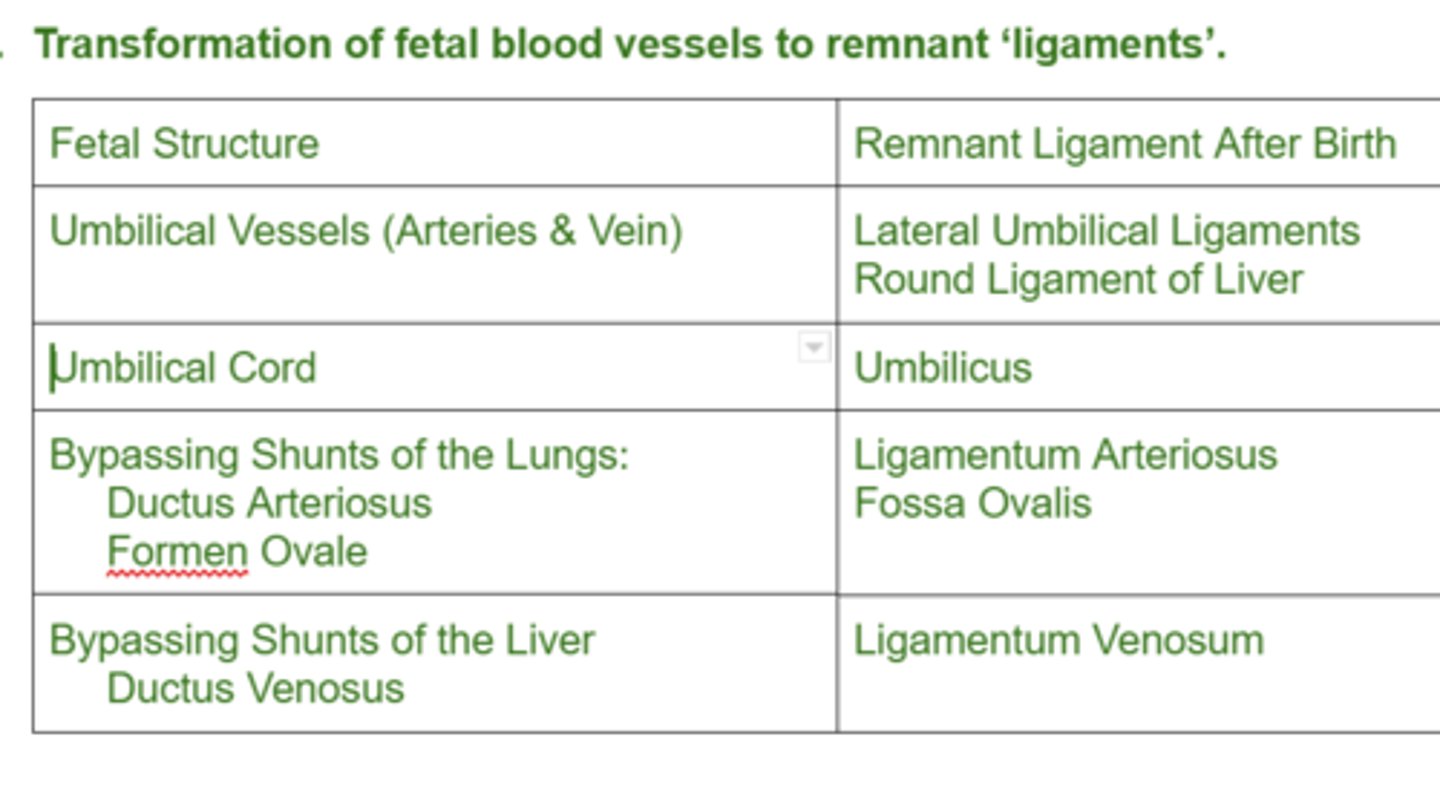
Key after birth changes
1. placenta removed from baby's circulation
2. lungs take in air
Changes in heart at birth.
-No blood coming from placenta
-Ductus arteriosus closes and becomes ligamentum arteriosum
-Foramen ovale closes & becomes fossa ovale
-Ductus venosus becomes ligamentum venosum
-Umbilical vein: ligamentum teres
-Umbilical arteries: medial umbilical ligament
Changes in blood circulation at birth.
1. umbilical vein
2. ductus venosus
(for the above 2: disuse in days, blood clotting off, leads to no blood flow)
3. foramen ovale
(flap of tissue closes off between atria d/t more pressure on left side than right, occurs in first few min s/p birth)
4. ductus arteriosus
(when prostaglandin lvls fall from removal of placenta, it closes via constriction, few hours s/p birth)
5. Umbilical arteries
(still get blood flowing to other internal illiac branches like bladder, but no blood flowing to umbilical artery, start constricting like DA, in hours)
Transformation of fetal blood vessels to remnant 'ligaments'.
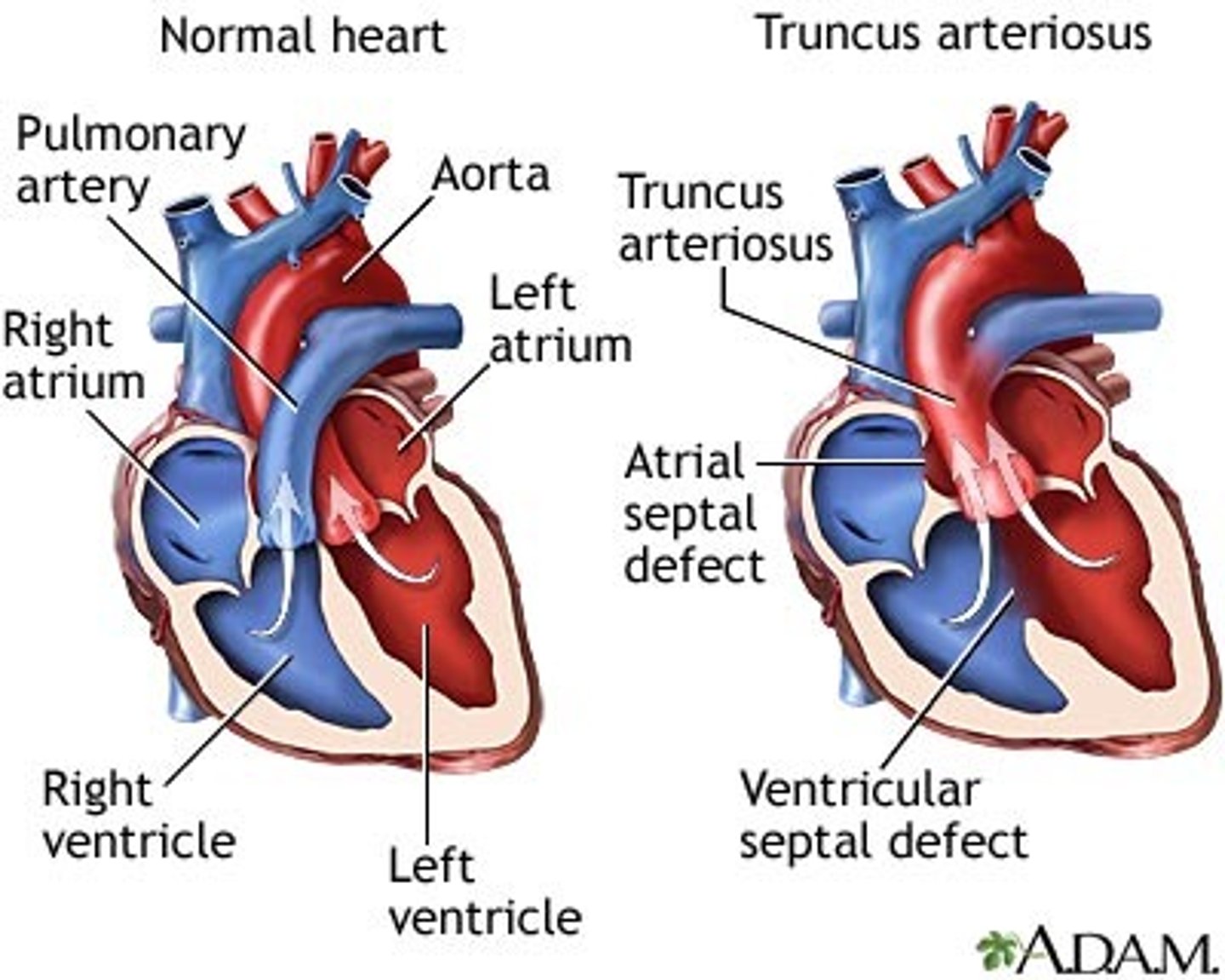
Most common defects seen in fetal heart at birth.
-Ventricular septal defect: (VSD)
-Atrial septal defect: (ASD)
-Persisting/Patent ductus arteriosus: (PDA)
-Pulmonary stenosis
-Persistent truncus arteriosus
-Transposition of great vessels
-Tetralogy of Fallot
-Coarctation of Aorta
Ventricular septal defect (VSD)
-Left to right shunting. Excessive fatigue on exertion and Pulmonary HTN.
Atrial septal defect: (ASD)
-Patent foramen ovale: Most common form of an Atrial Septal Defects.
-A small isolated patent foramen ovale causes no major problems, but if other defects present (e.g. pulmonary stenosis or atresia), blood is shunted through foramen ovale into L ventricle, producing cyanosis.
Persisting/Patent ductus arteriosus: (PDA)
-Left to right shunt of blood. Premi's. Associated with maternal rubella/prostaglandins
-baby still has ductus arteriosus open s/p birth
Persistent truncus arteriosus
Right to left shunt of blood--> cyanosis
Transposition of great vessels
Aorta from right, pulmonary trunk from left ventricle--> cyanosis
Tetralogy of Fallot
-Pulmonary stenosis
-Overriding aorta: Aorta emerges from both ventricles.
-Interventricular septal defect
-Right ventricular hypertrophy--> cyanosis
Coarctation of Aorta
Narrowing of Aorta
When does the cardiovascular system start to develop? When does blood start to circulate in it?
It starts to develop in the middle of the 3rd week, Blood circulates at the beginning of the 4th week
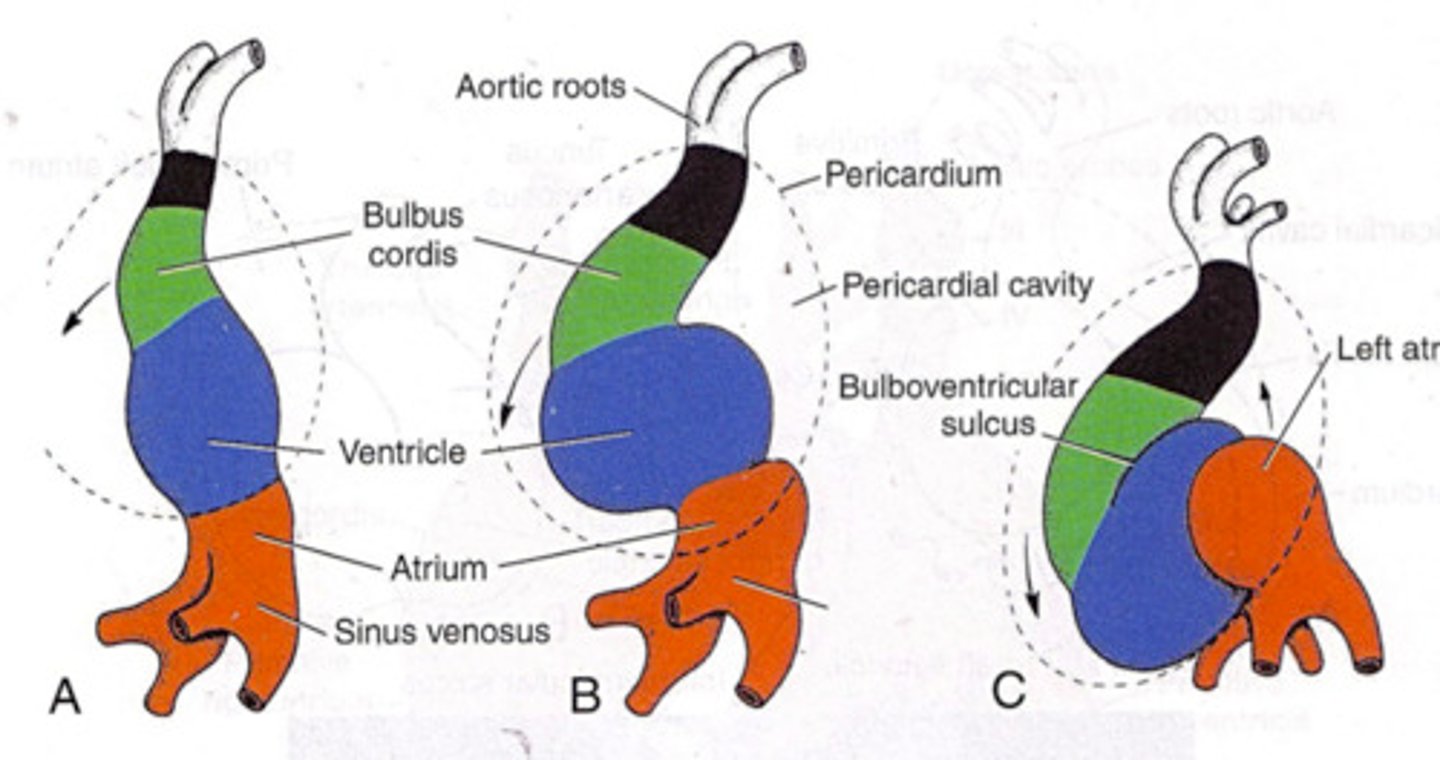
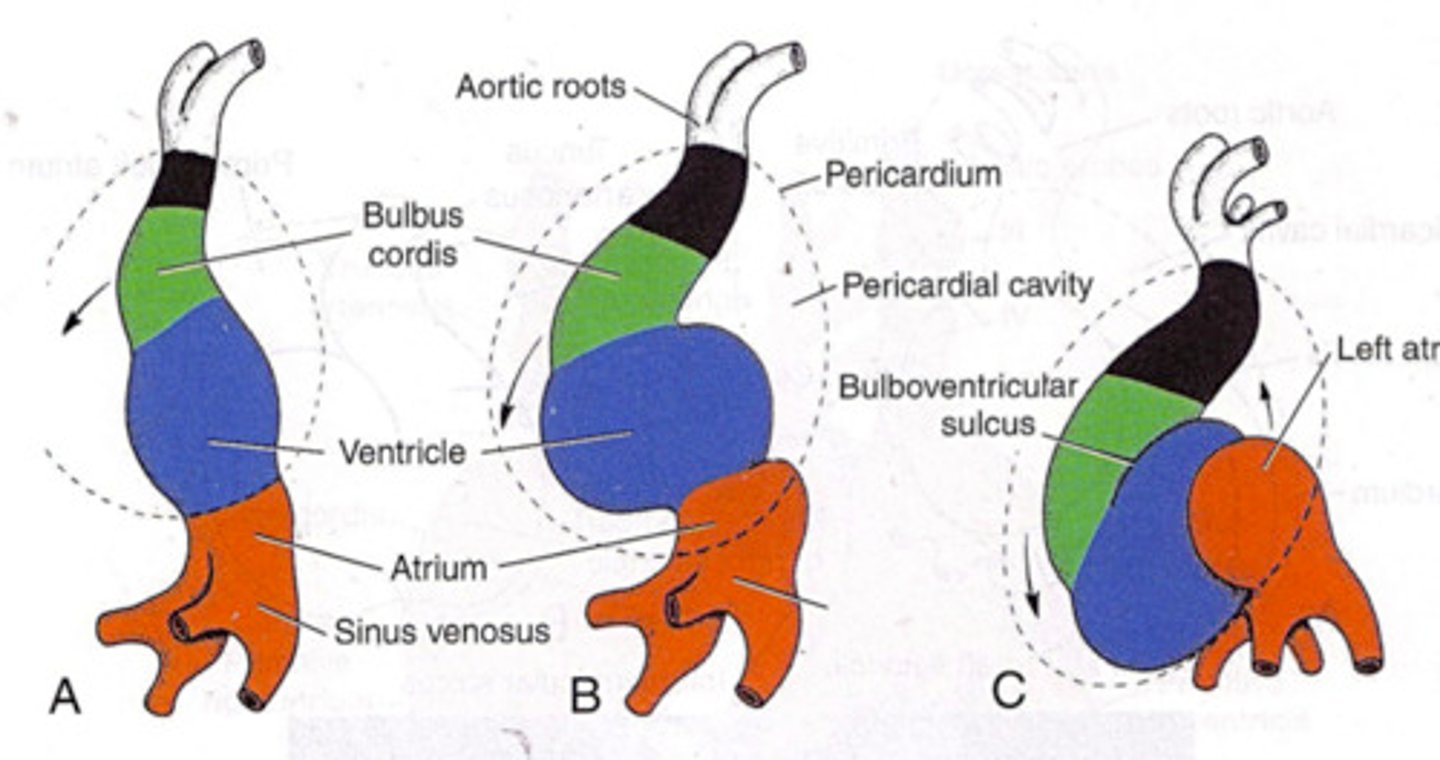
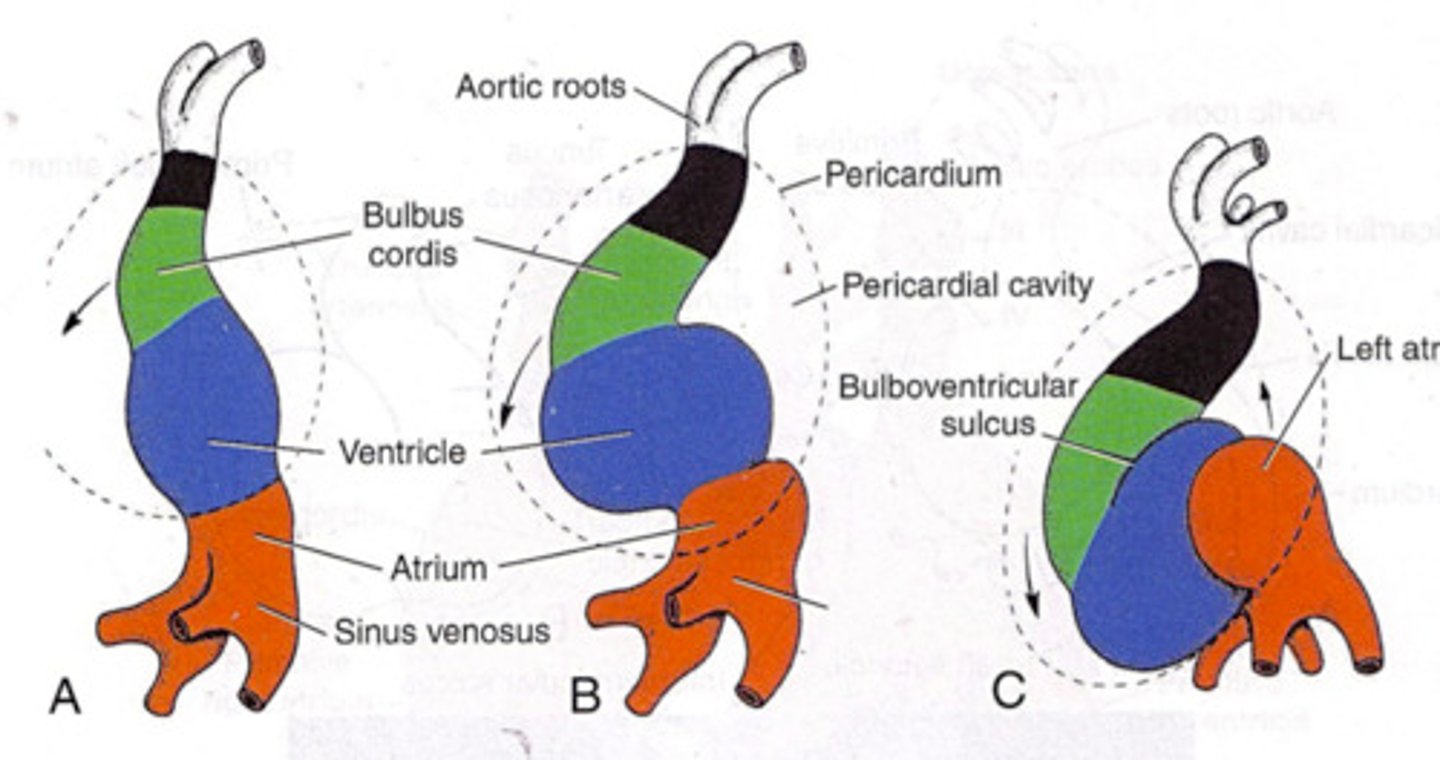
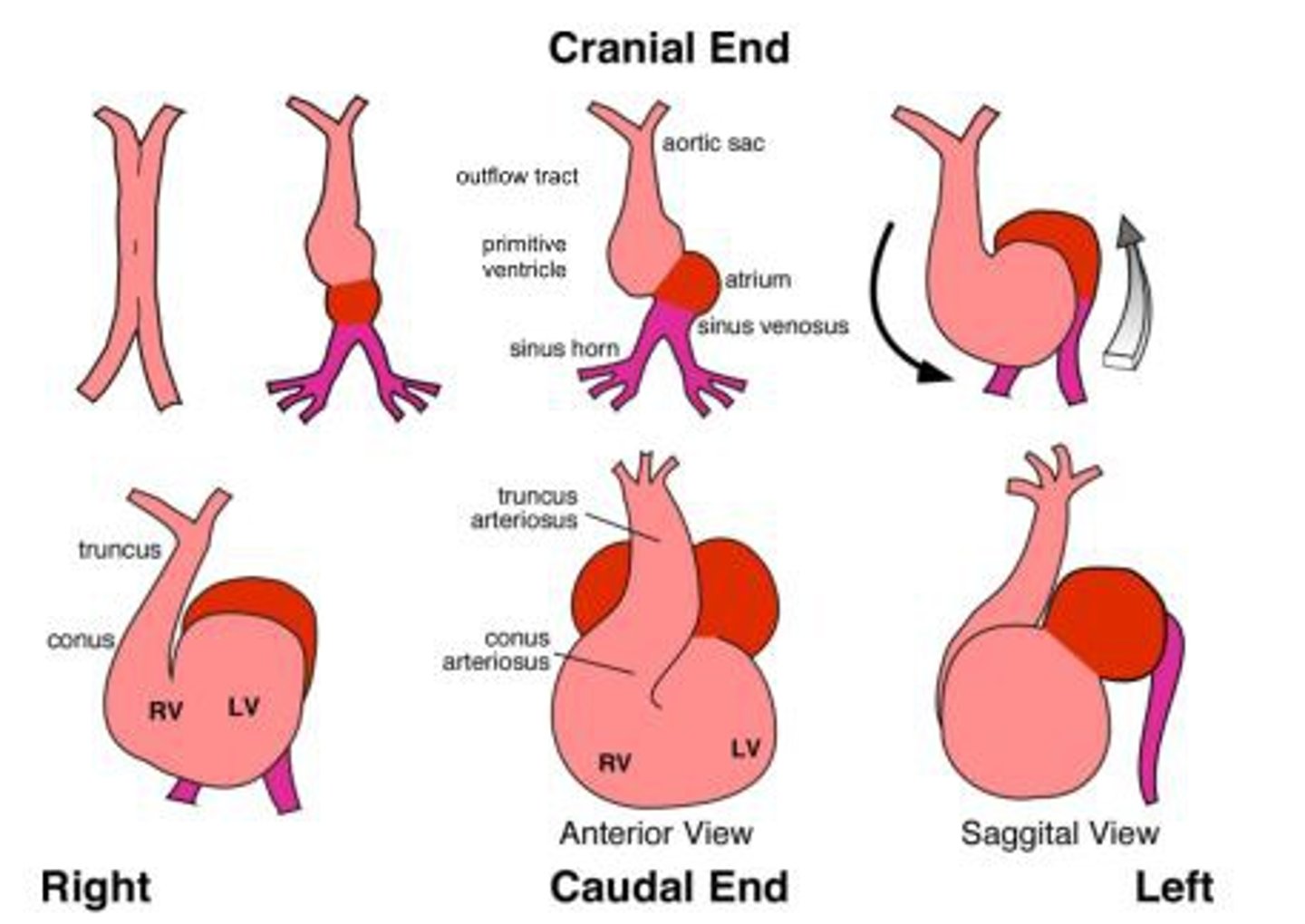
Describe the basic steps of heart development
1. Angioblastic cords in the cardiogenic area, cranial end of embryo.
2. Cords canalize to form Endocardial heart Tubes-late in third week.
3. Lateral folding of embryo brings the endocardial heart tubes together and they fuse to from a single heart tube with three layers-endocardium, myocardium and epicardium (visceral pericardium)
4. Head folding of the embryo brings the developing heart and the pericardial cavity ventral to the foregut and caudal to the oropharyngeal membrane.
5. Heart elongates and develops alternate dilations and constrictions: the bulbus cordis, ventricle, atrium and sinus venosus
6. Bulbus cordis and ventricle grow faster than other regions of the developing heart causing the heart to bend upon itself (forming a U shaped bulboventricular loop). The bend is down and to the right side of the embryo.
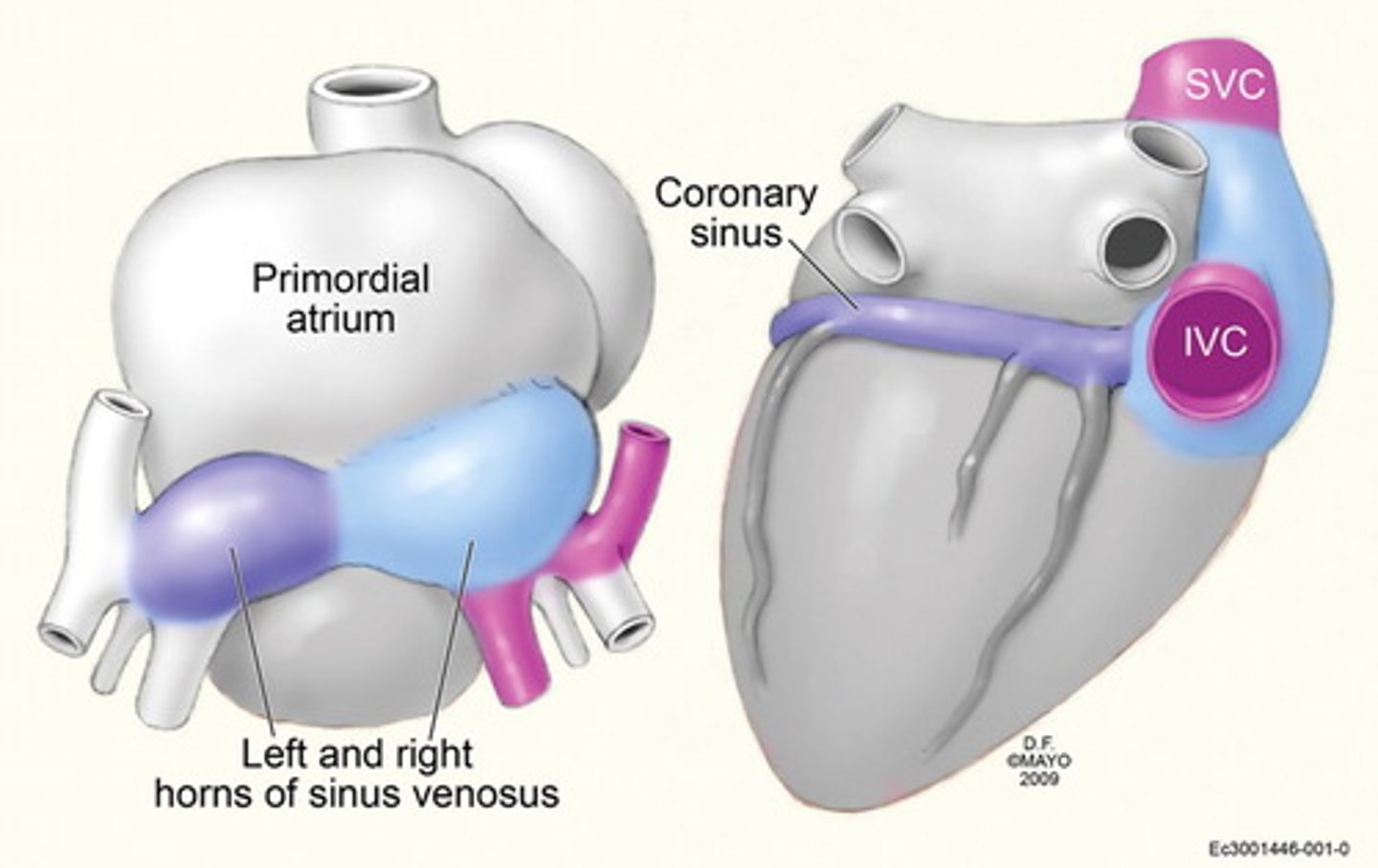
7. By this stage, the sinus venosus has developed lateral expansions, the right and left horns of the sinus venosus.
8. As heart develops, it gradually invaginates the pericardial cavity.
9. The heart is initally suspended from the dorsal wall by a mesentery, the dorsal mesocardium, however the central part of this mesentery degenrates froming a communcation-the transverse pericardial sinus between the right and left sides of the pericardial cavity.
Describe the bulbus cordis
outflow portion of he developing heart
together, the bulbus cordis and the primitive ventricle give rise to the ventricle of the formed heart. proximal to the truncus arteriosus.
The caudal end of the bulbus cordis gives rise to the smooth parts (outflow tract) of the left and right ventricles (aortic vestibule & conus arteriosus respectively).
The cranial end of the bulbus cordis (also known as the conus cordis) gives rise to the aorta and pulmonary trunk with the truncus arteriosus.
Tuncus Arteriosus
outflow portion of the developing heart
continuous with the aortic sac from which the aortic arches develop
The truncus arteriosus gives rise to the ascending aorta and the pulmonary trunk.
sinus venosus
receives venous blood from the chorion, yolk sac and embryo
develops right and left horns-due to the embryo shunting blood to the right side of the primitive heart
Bulboventricular loop
U shaped, as the primordial heart bends, the atrium and sinus venosus come to lie dorsal to the truncus arteriosus, bulbus cordis and ventricle, gives the adult position of the heart in the mediastinum, inflow of hte blood to heart is now on the posteiror aspect of the heart, where as the outflow of the blood with resepct to heart is situated anteriorly
When does the heart begin to beat?
22-23 days
Describe the circulation of the Primordial Heart
1. Blood enters the sinus venosus from a number of sites including: a. the embryo through the common cardinal veins, b. the placenta through the umbilical veins, c. the umbilical vesicle through the vitelline veins.
2. Blood from the sinus venosus enters the primordial atrium; flow from it is controlled by sinuatrial valves.
3. Blood passes through the atrioventricular canal into the primordial ventricle.
4. When the ventricle contracts, blood is pumped through the bulbus cordis and the truncus arteriosus into the aortic sac, from which it is distrubuted to the pharyngeal arch arteries in the pharyngeal arches.
5. Blood then passes into the dorsal aortas for distribution to the embryo, umbilical vesicle, and the placenta.
Before bulboventricular loop everything travels from inferior to superior, starting with the senous venous inferior. The bulbos cordis marks the begining of the outflow part.
Describe the blood flow thorugh primitive heart before partitioning in terms of location Posterior or Anterior, after the bulboventricular loop has fromed.
Posterior (Inflow):
1. Sinus venosus
2. Primordial Atrium
3. Atrioventricular Canal
4. Primordial Ventricle
Inferior Border of Adult -Bulboventricular Loop
Anterior (Starting inferiorly) (Outflow)
5. Bulbus Cordis
6. Truncus Arteriosus
7. Aortic Sac
8. Aortic Arches
When does the partitioning of the heart primordium begin?
Begins around the middle of the 4th week, and is completed by the end of the 5th week
Describe the development of the semilunar valves of the aorta nd the pulmonary trunk
Develops from three swellings of subendocardial tissue, swellings are restructured to form thin-walled cusps, position of the cusps after rotation is the normal anatomical way of naming cusps.
Anterior cups on the pulmonary trunk, posterior cusp on the aorta
Describe the development of the AV valves
proliferation of endocardial cushions around the AV canals.
Three cusps on the right side, two cusps on the left side.
endocardial cushions develop from the cardiac jelly
Describe the partitioning of the Primordial Atrium
The primordial atrium is divided into the right and left atria by the formation and fusion of the two sept: spetum primum and the spetum secundum.
Septum Primum
This is the first septum, as it grows inferiorly to the atrioventricular junction, it closes an opening between the primitve atrum called the foramen primum, this divides the primitive atrium into a right and left atria. This foramen will eventually close.
Before closure of the foramen primum, a second opening forms in the septum called the Foramen Secundum.
Septum Secundum
On the right side of the septum primum, this membrane grows inferiolry. It will grow only as much as to overlap the newly fomed foramen secundum.
This overlapping of the foramen secundum forms a flap valve over the foramen. This structure is called the Foramen Ovale.
Describe the Foramen Ovale
Before birth, the oval foramen allows most of the oxygenated blood entering the right atrium from the IVC to pass into the left atrium. It prevents the passage of blood in the opposite direction bc the septum primum closes against the relatively rigid septum secundum.
After birth, it functionally closes due ot higher pressure in the left atrium and the valve of the oval foramen fuses with the septum secundum forming the oval fossa.
In fetus, the highest pressure is in the right atrium, but once the lungs start working after birth, pressure decreases and increases in left side ot heart, closing the door.
Describe the formation of the Adult Right Atrium
Left horn of sinus venosus=coronary sinus
Right horn of sinus venosus-posterior wall of the right atrium, called sinus venarum (smooth portion of adult right atrium)
Primitive atrum form the rough anteiror wall of the adult right atrium (pectinate muscles)
Describe the Formation of the Adult Left Atrium
smooth walls formed from the incorporation into the left atrium of the primoridal pulmonary veins
Total Anomalous pulmonary Vein
a congential defect in which the primordial pulmonary vein may be incorporated to the right side of the developing interatrial septum therefore draining into the right atrium instead of the left atrium.
Describe the formation of the interventricular septum
1. Muscular portion: infolding of primitve ventricle growing superiorly to meet the membranous portion. Divides primitive ventricel into right and left side.
2. Membranous portion:
a. forms from the right side of fused endocardial cushions
b. fuses with aorticopulmonary septum and the muscular part of the intervetnricular septum.
Partitioning of the bulbus cordis and truncus arteriosus
during the 5th week, active proliferation of mesenchymal cells in the walls of the bulbus cordis results in the formation of the bulbar ridges.
Similar ridges from in the truncus arteriosus; these are continusous withe the bulbar ridges.
Bulbar and truncal ridges are derived mainly from the neural crest mesenchyme.
Together the bulbar and truncal ridges undergo 180 degree spiraling, possibly caused in part by the streaming of blood from the ventricles, results in the formation of a spiral aorticopulmonary septum.
This septum divides the bulbus cordis and the truncus arteriosus into the aorta nd the pulmonary trunk.
Aorticopulmonary septum
divides the bulbus cordis and the truncus arteriosus into the aorta nd the pulmonary trunk.
Because of the spiraling of the aorticopulonary septum the pulmonary trunk twists around the ascending aorta.
Bulbus cordis
Starts the outflow portion of the primitive heart
is incorporated inot the walls of the ventricles.
1. the right ventricle is represented by the conus arteriosus which gives rise to the pulmonary trunk.
2. the left ventricle, the bulbus cordis forms the walls of the aortic vestibule, the part of the ventricular cavity just inferior to the aortic valve.
Probe patent oval foramen
Atrial Septal Defect, not clincially significant, 25% of us have it, there is an overlap, pressure keeps it close, results from an incomplete adhesion between the flap of the valve of the oval foramen and the septum secundum after birth.
Secundum type of Atrail Septal defects
The secundum atrial septal defect usually arises from an enlarged foramen ovale, inadequate growth of the septum secundum, or excessive absorption of the septum primum.
If resorption occurs in abnormal locations, septum primum is fenestrated or net like of the septum primum and a large oval foramen.
Endocardial Cushion Defect with Primum Type
The ostium primum atrial septal defect (also known as an endocardial cushion defect) is a defect in the atrial septum at the level of the tricuspid and mitral valves. This is sometimes known as an endocardial cushion defect because it often involves the endocardial cushion, which is the portion of the heart where the atrial septum meets the ventricular septum and the mitral valve meets the tricuspid valve.
Endocardial cushion defects are associated with abnormalities of the atrioventricular valves (the mitral valve and the tricuspid valve). These include the cleft mitral valve, and the single atrioventricular valve (a single large, deformed valve that flows into both the right ventricle and the left ventricle).
Endocardial cushion defects are the most common congenital heart defect that is associated with Down's syndrome.
Sinus Venosus ASD
Located superior part of the interatrial septum, close to the SVC, defects result from abnormal developement of the septum secundum or incomplete absorption of the sinus venosus into the right atrium