APC EXAM 2- Gilmore
1/69
Earn XP
Description and Tags
5 lectures
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
What is a risk?
anything that threatens the ability of a person or organization to accomplish its mission—> associated with negative outcomes
What are the 2 types of risk? (from an insurance perspective)
speculative—> chance of gain OR loss
pure—> only a chance of loss (ex: fire, theft)
What is a way to help manage risk?
insurance (but must meet criteria)
A risk management process involves what 2 things?
identifying potential risks and assessing/managing those risks
What are the steps to the risk management process?
establish the context
identify/ analyze risks
evaluate and prioritize the risks
select an appropriate risk management strategy and implement the technique
monitor decisions and update risk management program
What are some techniques to manage risks?
risk avoidance
risk prevention/modification
risk absorption/retention
risk sharing or transfer
OBRA 90 required pharmacists to do what?
What did the learned intermediary doctrine do?
idk how imp
OBRA 90 requires prospective DUR, patient counseling, and to maintain pt. records
learned intermediary doctrine held that the duty to warn against ADRs and other problems was with the physician
What does HIPPA 1996 protect?
all individually identifiable health information
There are many risks associated with technology in the pharmacy including…
strategic risk
performance risk (technology might not work as intended)
operational risk (risks with day-to-day use)
psychosocial risk (stress/burnout from tech use)
Describe the factors that affect performance risk of an information technology system used in pharmacies:
system requirements (technical and operational needs the IT system must meet to function properly in a pharmacy setting)
modularity (how well different components of the system (e.g., inventory, EHR, billing) integrate and communicate)
Effective medication error prevention should focus on what factors that contribute to error?
a. blunt end/ latent end
b. front end/ active end
a. “blunt end” or “latent end” (blunt end is hidden systemic factors that create conditions for errors to occur vs. front/active end is immediate actions by frontline staff where errors become visible—> should focus on blunt end)
Which approach to risk provides a better understanding of risks in terms of both cause and outcome?
a. qualitative
b. quantitative
a.
What is Just Culture?
a framework that supports a learning environment by balancing accountability with system design
“Just Culture” distinguishes between what 3 types of behaviors?
human-error: inadvertent actions, slips, lapses, mistakes
at-risk behavior: risky actions that are mistakenly believed to be justified
reckless behavior: conscious disregard of substantial risk
What is Pharmacoeconomics?
What does it identify, measure, and compare?
assessing the clinical effectiveness of any new health care intervention—> is a TOOL not the FINAL ANSWER
description and analysis of the costs of drug therapy to health care systems and soceity
identifies, measures, and compares COSTS and CONSEQUENCES of pharm products and services
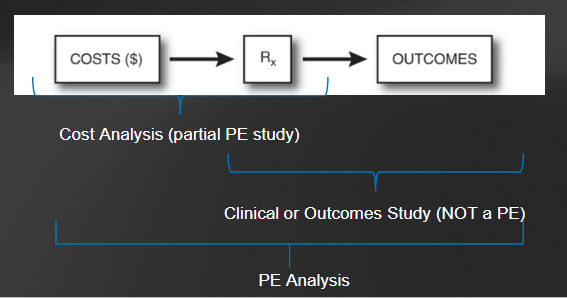
Based on the picture, which # is a cost analysis? which # is a clinical/outcomes study? which is a PE analysis?
cost analysis
clinical/outcomes study
PE analysis
PRACTICE:
A health services research plan to study the total cost burden of Type 2 Diabetes on society.
The costs will include:
Prevention
All treatments including medications
Losses from morbidity and mortality
Would this be a PE analysis?
No—> not a PE analysis… the study focuses on the disease NOT the intervention
a PE analysis requires measuring and comparing the cost of a pharm intervention and its resulting outcomes
Pharmacoeconomics can look at interventions made at the individual, hospital/health plan level, and societal level. What are examples of interventions made at each level?
individual
determine at patient-patient level what the best tx is
looks at demographics, clinical considerations, economics
health/health plan level
hospital systems create a formulary
insurance, creates formularies, tiers of coverage, copays
societal
federal government’s role in paying for health care services
some countries play a role in price negotiation, setting, and formulary management at national level
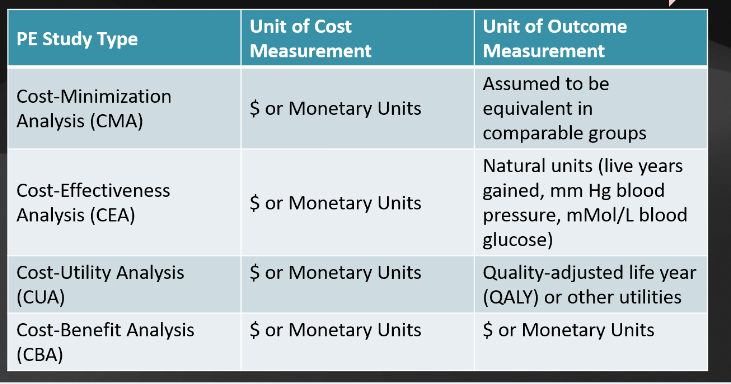
What are the 4 basic types of pharmacoeconomic studies?
Cost-minimization analysis (CMA)
cost-effectiveness analysis (CEA
cost-utility analysis (CUA)
cost-benefit analysis (CBA)
What is the similarity between all 4 types of pharmacoeconomic studies? difference?
each measure costs in $ but differ in how they measure/compare health outcomes
Which PE study type is easiest to conduct, but cannot be used when outcomes of each intervention are different?
a. CUA
b. CBA
c. CEA
d. CMA
d.
Answer the following about a cost-minimization analysis:
How does a CMA measure outcomes?
costs of what are compared?
cannot be used when?
examples/applications?
outcomes assumed to be equivalent
only costs of interventions are compared—> can’t be used when outcomes are different or for comparing different classes of medications
ex:
comparing 2 generic medications that are rated FDA equivalent
comparing cost of 2 therapeutically equivalent products in the same class (lisinopril vs. ramipril)
cost comparison of the same drug in different settings (lisinopril in the ER vs. at a community pharm)
What is the most common type of PE analysis?
a. CUA
b. CBA
c. CEA
d. CMA
c. cost-effectiveness analysis
Answer the following about a cost-effectiveness analysis:
How does a CEA measure outcomes?
advantages?
disadvantages?
measures outcomes in natural units (ex: mmHG, cholesterol levels, symptom free days)
advantage: outcomes easier to quantify compared to a CBA or CUA
disadvantage:
can’t compare programs with different types of outcomes (ex: cost-effectiveness of opening a diabetes clinic vs. HIV clinic)
hard to combine differences in medications other than effectiveness (like ADRs) (ex: when comparing 1st and 2nd gen antihistamines one gen might be more effective in relieving allergy symptoms, but not accounting for ADRs like drowsiness)
What are the 2 methods of reporting in cost-effectiveness analysis’s (CEA)?
average cost effectiveness ratio (CER)
CER = Total Cost of Intervention / Total Effectiveness of Intervention
incremental cost-effective ratio (ICER)
ICER = (Cost of B – Cost of A) / (Effectiveness of B – Effectiveness of A)
Answer the following about a cost-utility analysis:
How does a CUA measure outcomes?
applications?
measures outcomes using Quality-adjust life year (QALY) or other utilities
basically takes into account length and quality of life
applications
useful when outcomes effect quality of life (ex: cancer tx might prolong life but with severe side effects)
advantages/disadvantages of CUAs?
advantages
combines morbidity (quality) + mortality (length of life)
compares unrelated interventions (e.g., diabetes drugs vs. knee surgeries).
Uses cost/QALY thresholds (e.g., $50,000 per QALY) for objective decisions.
disadvantages
Utility weights are subjective estimates (no consensus on calculation).
May oversimplify complex health states (e.g., mental health impacts).
Answer the following about a cost-benefit analysis:
How does a CBA measure outcomes?
why is it unique?
advantages?
disadvantages?
measures outcomes using $
unique bc looks at $ but also benefits
advantages:
measuring both costs and benefits allows clinicians/decision makers to compare multiple programs or interventions with similar or unrelated outcomes
can see if benefits > cost of implementation
disadvantages:
hard to put $ value on health outcomes
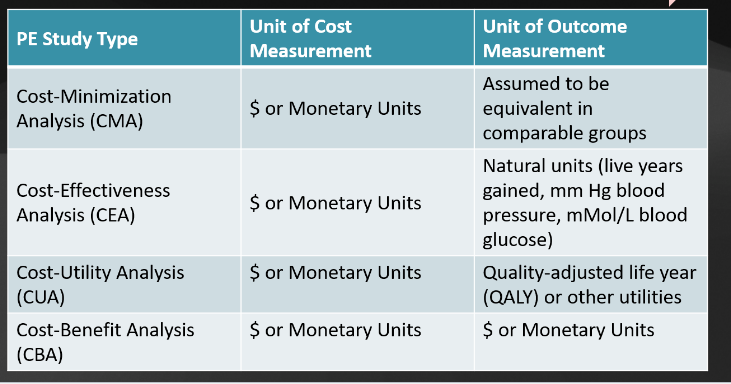
Review table of PE types:
Difference between direct medical and nonmedical costs?
idk how imp
direct medical—> cost of tx
direct nonmedical—> costs to pts./families associated with tx, but not medical
Define each of the following:
indirect costs
indirect benefits
intangible costs
intangible benefits
idk how imp
indirect costs- costs that involve the loss of productivity because of illness/death
indirect benefits- opposite of indirect costs
intangible costs- costs of pain, suffering, etc. from illness/tx
intangible benefits- avoidance of intangible costs
What are societal costs?
idk how imp
costs to insurance company, pt. provider/institution, and others based on loss of productivity
What is a sensitivity analysis used for?
to determine the effect of data uncertainty or assumptions on the conclusions of the study
aka—> uncertainty in the data= run a sens analysis
What are the 4 types of sensitivity analysis?
simple
threshold
analysis of extremes
monte carlo
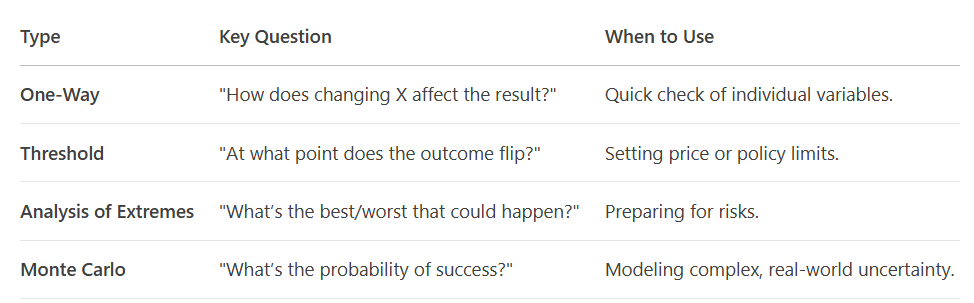
Describe the characteristics of each type of sensitivity analysis:
Type of Analysis | Characteristics |
Simple sensitivity | |
Threshold analysis | |
Analysis of extremes | |
Monte carlo simulation |
Type of Analysis | Characteristics |
Simple sensitivity |
|
Threshold analysis |
|
Analysis of extremes |
|
Monte carlo simulation |
|
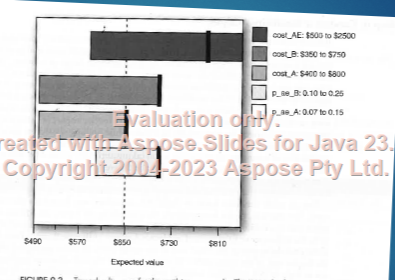
What is the use of a tornado diagram? What is it?
“graph of a one-way sensitivity analysis from the variables which change the answer the most to those variables that have the least impact on the answer”- gilmore
explained:
a visual tool ranking variables by their impact on an outcome
Widest bars = most influential factors.
Used in pharmacoeconomics to prioritize cost-effectiveness drivers
What is a decision analysis?
application of an analytical method for systemically comparing different decision options
graphical representation of allows calculation of values needed to compare different options
helps selecting the best/most cost-effective alternative
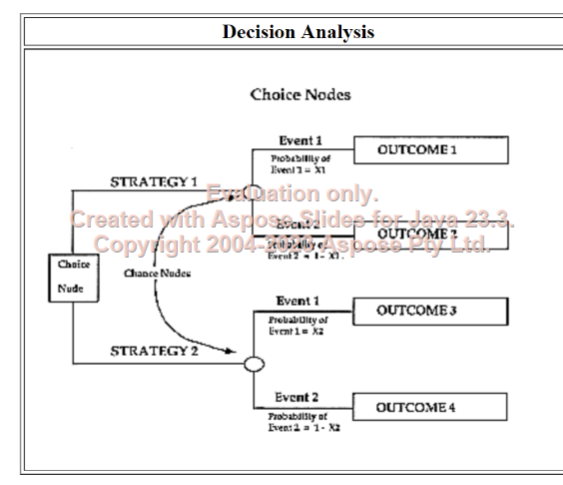
What are the steps to a decision analysis?
identify the specific decision (ex: should we include a new abx to our formulary?)
specify alternatives (ex: compare new abx to current standard of care)
draw the decision analysis structure (decision tree)
specify possible costs, outcomes, and probabilities
perform calculations
conduct a sensitivity analysis
Difference between choice, chance, and terminal nodes in a decision tree?
choice nodes: choice is allowed (ex: new abx vs. standard abx)
chance nodes: chance comes into equation (success vs. failure or ADR vs. no ADR)
terminal node: final outcome of interest for each option
In decision analysis, trees are simple and easy to use, but many diseases are very complex. What type of modeling can be used for a more accurate presentation of complex health scenarios that happen over a number of cycles or intervals?
Markov modeling
What are Markov states?
when we assume that a patient is in one of a finite number of health states
What are the components of a simple markov modeling process?
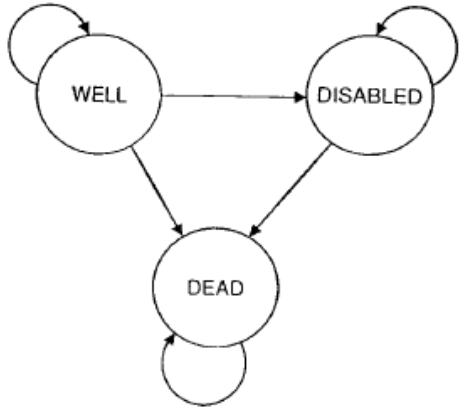
each state is represented by a circle
arrows between states are transitions
What’s the major difference between decision tree analysis and a markov modeling?
Decision analysis uses trees for simple comparisons and Markov models for complex, long-term scenarios
What is a managed care pharmacy and what are its 3 major goals?
managed care pharmacy—> focus is on drug therapy and pharm care
3 goals
contain costs
improve outcomes/QOL
improve quality/accessibility of healthcare
What is the value equation in pharmaceuticals?
define each component in the equation
VALUE= quality/cost
quality: defined as evidence-based medicine demonstrating measurable results in outcomes
cost: cost of drug
If quality remains constant, and cost increases, the value _____________.
a. increases
b. decreases
b.
If quality increases, and cost remains constant, the value _____________.
a. increases
b. decreases
a.
What are the 3 prime components in formulary development process in managed care?
clinical
financial (includes rebates)
other
What are rebates?
a discount provided by the pharm manufacturer to the insurer as part of a formulary status agreement
In managed care, negotiation is all about leverage.
What are some leverage opportunities?
drug uniqueness
organization size
shifts in clinical picture
generic availability
formulary type/restrictiveness
working relationship
product portfolio
What is the definition of off-label use?
use of a drug for indications, dosage forms or regimens, or others not stated in the product labeling approved by the FDA
What are the issues with off-label use?
compromises definitive clinical trial data, evidence-based medicine, safety/efficacy standards
off-label uses may be potentially harmful and/or lead to ineffective results
What are some areas where off-label products are used a lot?
pediatrics
oncology
What is the FDA’s policy regarding off-label use?
drug manufacturers the only ones that CANNOT discuss or provide material on off-label uses
prescribers can use off-label if appropriate
What is prior authorization?
protocols placed on meds to prevent prescribing unless defined and specific criteria are met (ex: high cost/potential for misuse)
What is a hospital chargemaster?
computerized, coded list of all items that will be charged in the hospital
problems: issues with connection to actual cost and raising pharm charges at same rate as other supplies
What are CPT codes?
type of billing terminology
describes complexity of the visit, type of visit
each code may require specific documentation
ex: 99211- physician not required or 90471- immunizations
What is CPT Code 99490?
chronic care management services can be reimbursed for 20 minutes of clinical staff type per calendar month
Can pharmacists become “providers” under the social security act? what does that mean?
no, as of now pharmacists cannot become a provider. being a provider means that you can participate in part B of Medicare and bill them for your services.
In a drug pricing hearing in 2019 where many CEOs of pharm companies testified, what did the pharma companies say? who did they blame?
pharma defends medical breakthroughs and needing room for further innovation
BLAME GOES TO PBMS AND INSURERS
potential HHS rebate reform rules earns pharm praise
need to move towards value-based arrangements, stronger biosimilar market
In a 2012 IPSOS global reputation center survey, what did consumers say pharm companies can do to better demonstrate their corporate citizenship?
develop innovative drugs to fight diseases
ensure the safety of drugs produced in other countries
develop assistance programs that provide less expensive drugs to low-income families
Each drug company has a public affairs office that is responsible for…
government relations
intelligence gathering
investor information
PACs supporting candidates
donates/support
unpredictable events—> bad pr, media relations
PHRMA code on interactions with healthcare professionals was introduced in 2009.
What are some codes drug companies have to follow when interacting with medical professionals and vice versa?
both risks and benefits are presented
provide modest meals-in office
gifts—> only educational items that are worth up to $100 are okay
not allowed to do recreational events as part of promotion
encourages practitioners to disclose financial relationships
elimination of company-sponsored pens, notepads, and other reminders bearing company logo
drug samples still okay
reps can’t TALK about off-label uses, but can give reprints of articles in many situations
The physicians payments sunshine act in the affordable care act require drug manufacturers to do what?
requires manufacturers of drugs, biologics, and devices to report transfers of value to physicians and teaching hospitals on a public website
In recent years marketing of drug makers has shifted from healthcare providers to _____.
direct to consumer advertising (DTCA)—> includes magazines, journals, television, social media
Does PhRMA spend more on marketing or research?
marketing (x3)
Is there any evidence that DTCA benefits healthcare quality?
no
What is the definition of disease mongering? disease awareness?
disease mongering: “The selling of sickness that widens the boundaries of illness and grows the markets for those who sell and deliver treatments”
disease awareness: industry term for disease mongering
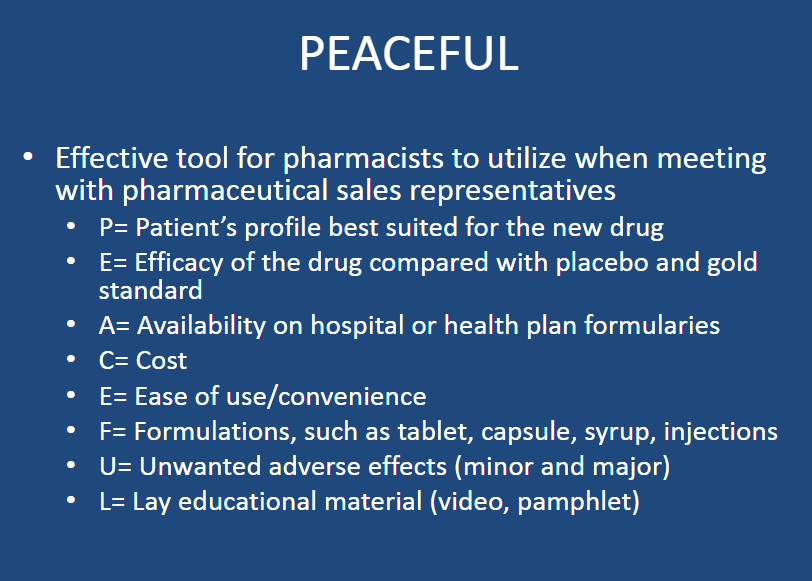
What is an effective tool for pharmacists to use when meeting with pharm sales reps?
“PEACEFUL”
Why do doctors and drug companies like drug samples?
What is the REAL purpose of samples?
Drug Companies |
|
Doctors |
|
REAL PURPOSE OF SAMPLES |
|