Module 5 Urinary & Reproductive System Exam Review
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
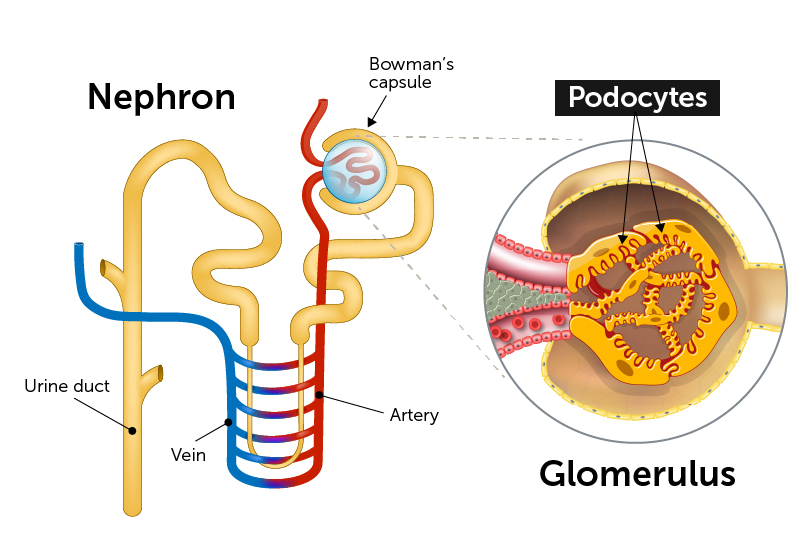
What is a nephron?
The functional unit of the kidney responsible for filtering blood and forming urine. Each kidney contains over 1 million nephrons.
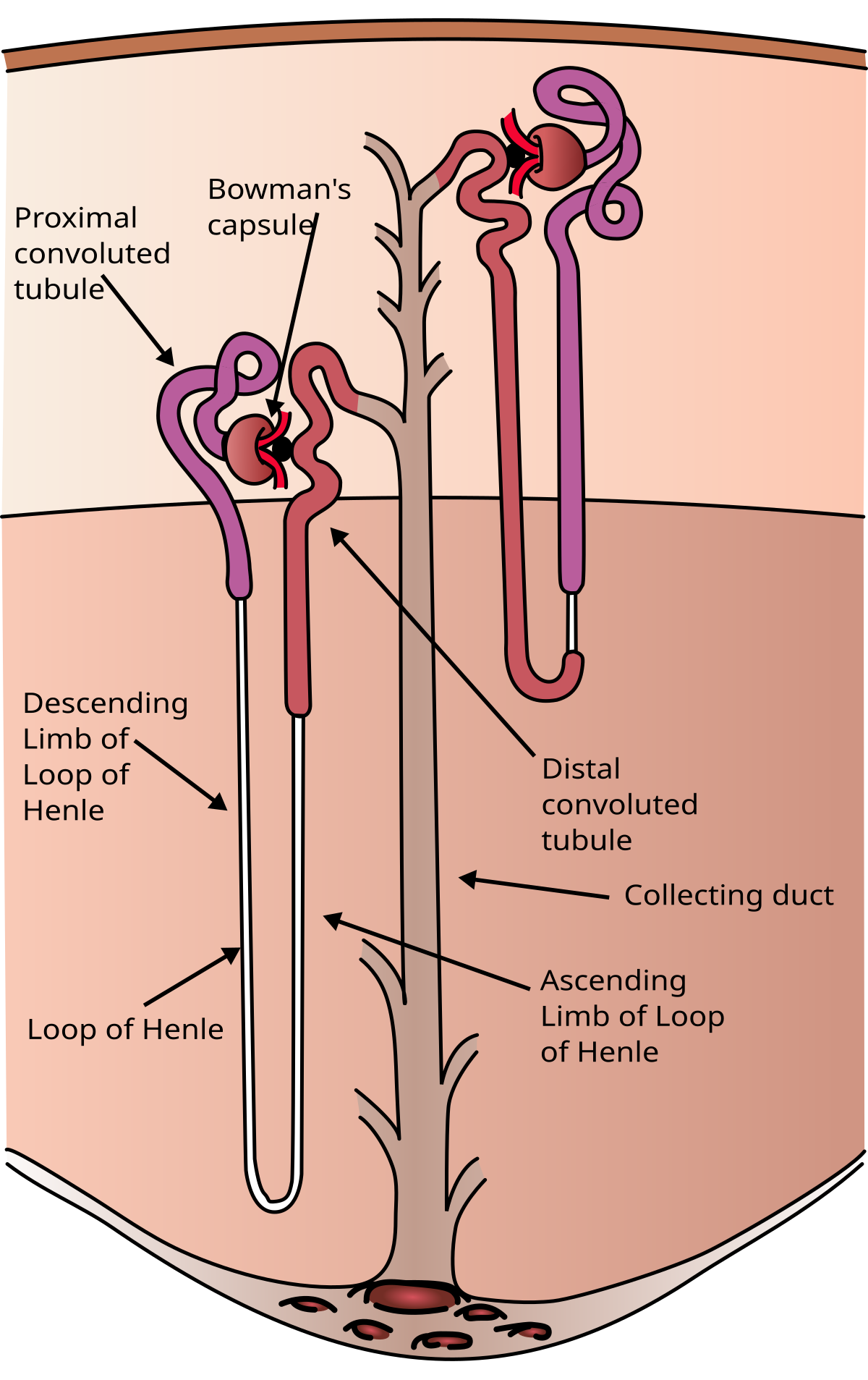
What are the two types of nephrons?
Cortical nephrons (~85%): Short loops, located mostly in the cortex.
Juxtamedullary nephrons: Long loops extending deep into the medulla, important for concentrating urine.
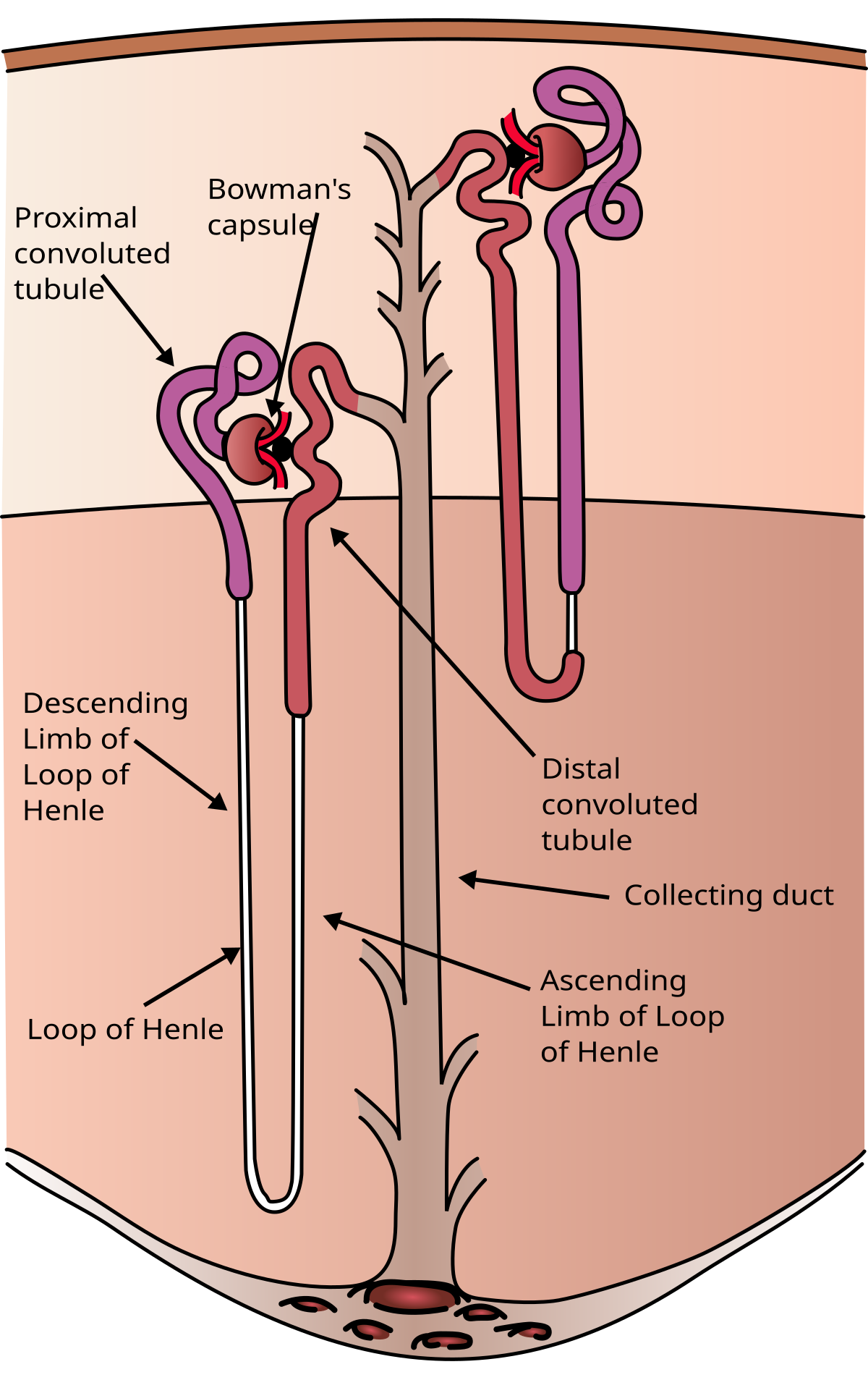
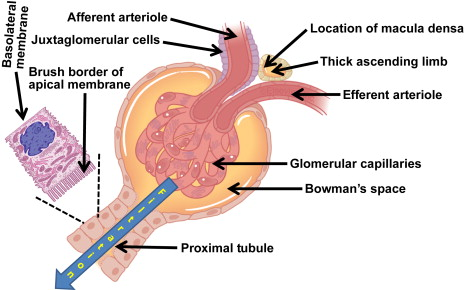
What is the renal corpuscle and its function?
The renal corpuscle consists of the glomerulus and Bowman’s capsule.
Its function is to perform filtration of blood plasma.
What happens in the proximal convoluted tubule (PCT)?
The PCT reabsorbs nutrients, water, and ions back into the bloodstream.
What is the function of the distal convoluted tubule (DCT)?
The DCT is involved in selective secretion and reabsorption of ions and helps with pH and electrolyte balance.
What is the role of the collecting duct?
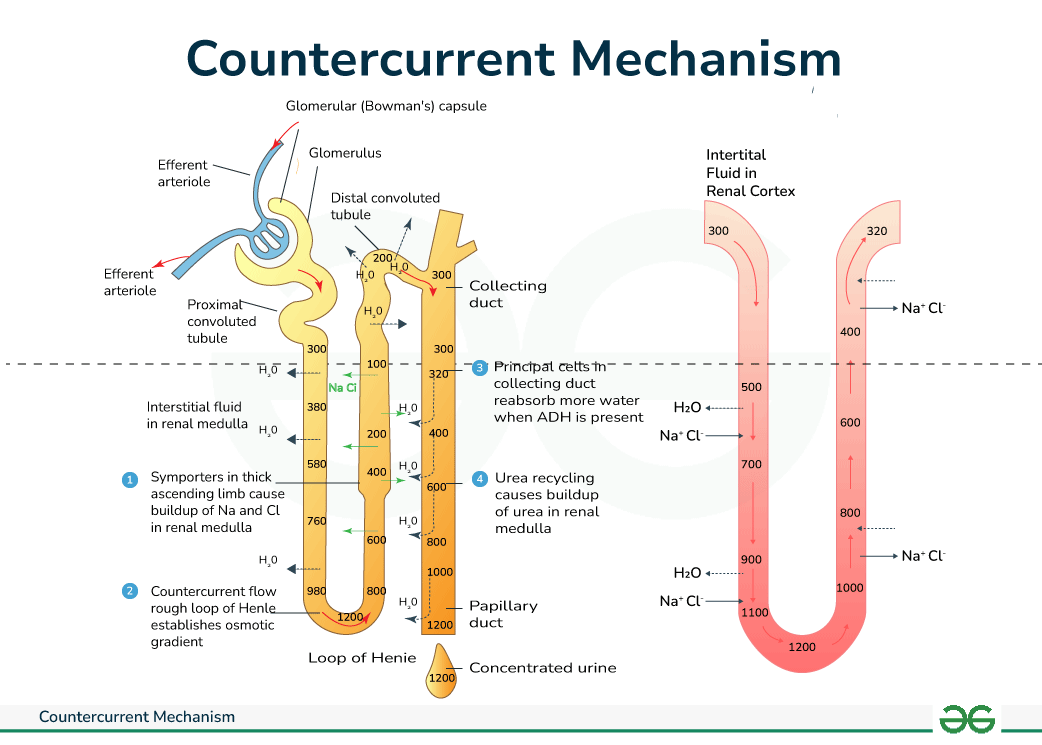
The collecting duct concentrates urine and responds to antidiuretic hormone (ADH) to control water reabsorption.
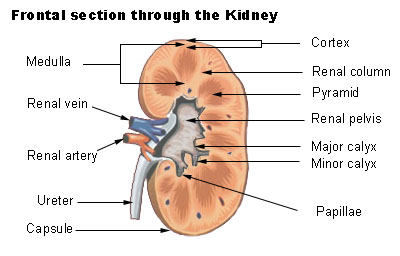
What is the renal pelvis?
A funnel-shaped structure that collects urine from the major calyces and channels it into the ureter.
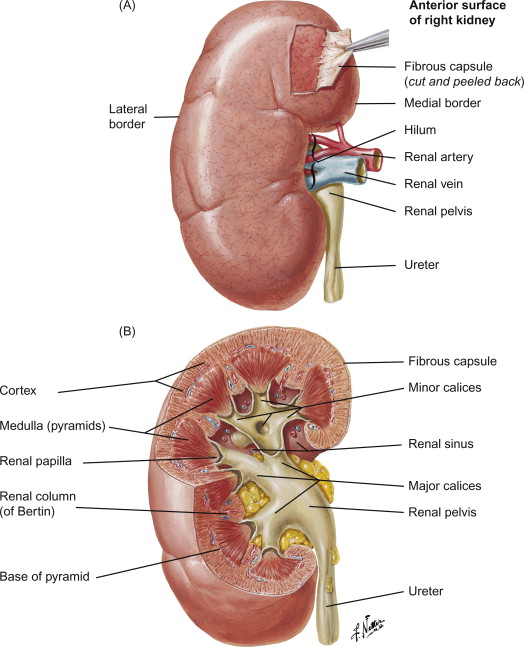
What is the fibrous capsule of the kidney?
The innermost protective layer directly surrounding the kidney.
What is perirenal (perinephric) fat?
A thick layer of adipose tissue that cushions the kidney and helps hold it in place within the abdominal cavity.
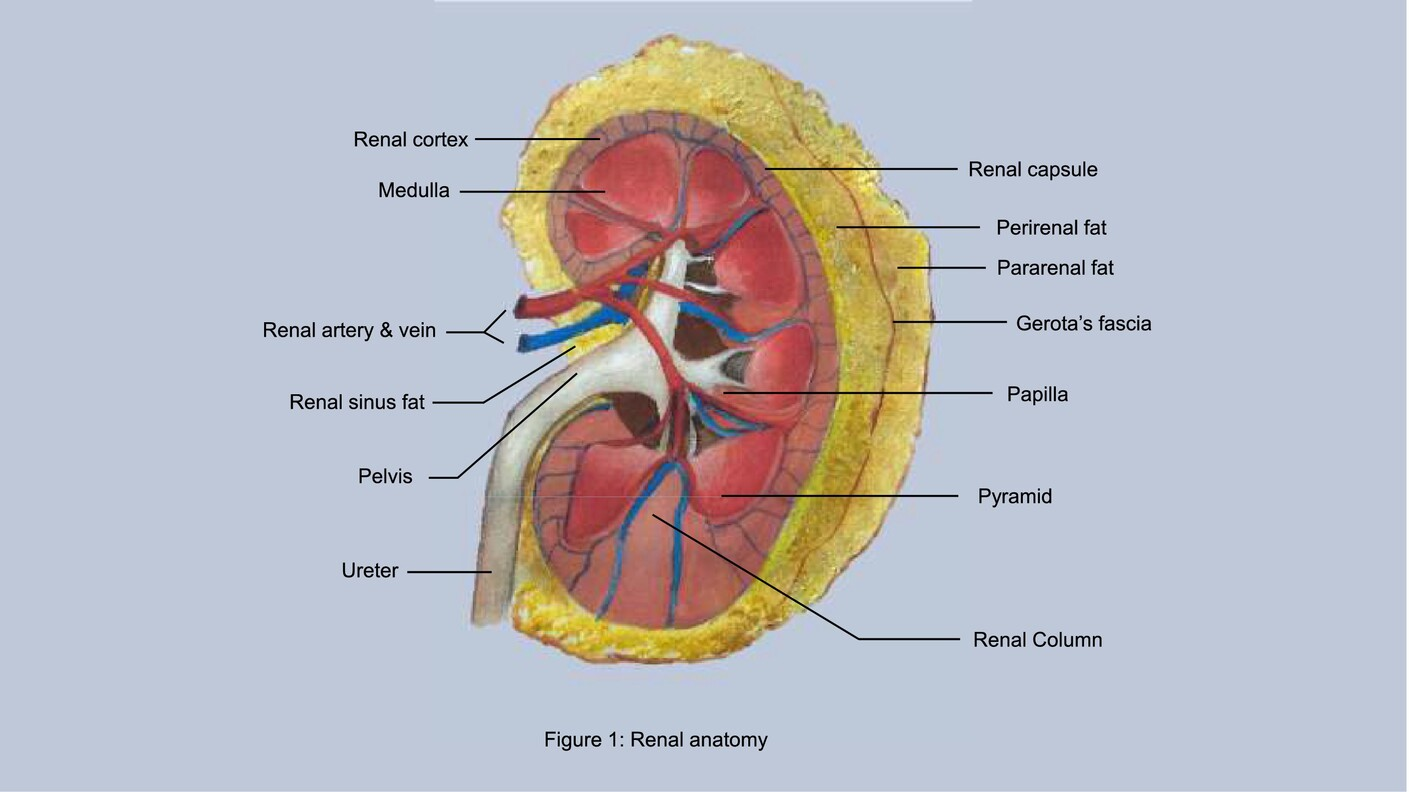
What are the three supportive tissue layers of the kidney (from deep to superficial)?
Fibrous capsule
Perirenal fat
Renal fascia
What are podocytes and where are they found?
Podocytes are specialized epithelial cells in the visceral layer of Bowman's capsule. They have foot processes (pedicels) that wrap around capillaries and form part of the filtration barrier via filtration slits.
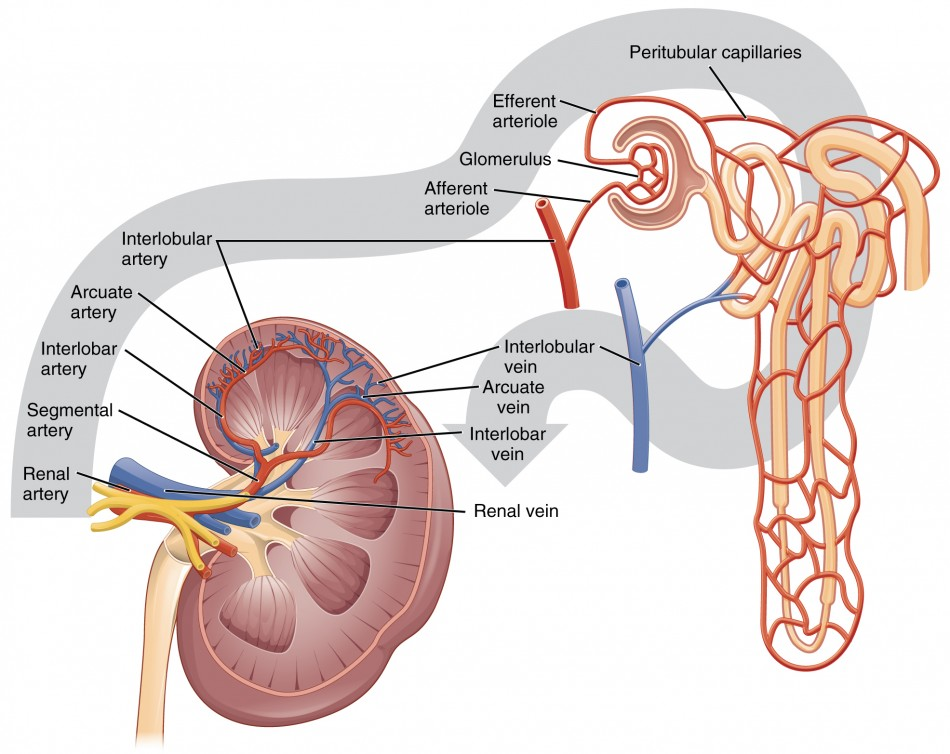
What is the correct order of arterial blood flow into the kidney?
Renal artery
Segmental arteries
Interlobar arteries (travel between renal pyramids)
Arcuate arteries (arch over base of pyramids)
Cortical radiate (interlobular) arteries
Afferent arterioles
Glomerulus (capillary bed for filtration)
Efferent arteriole
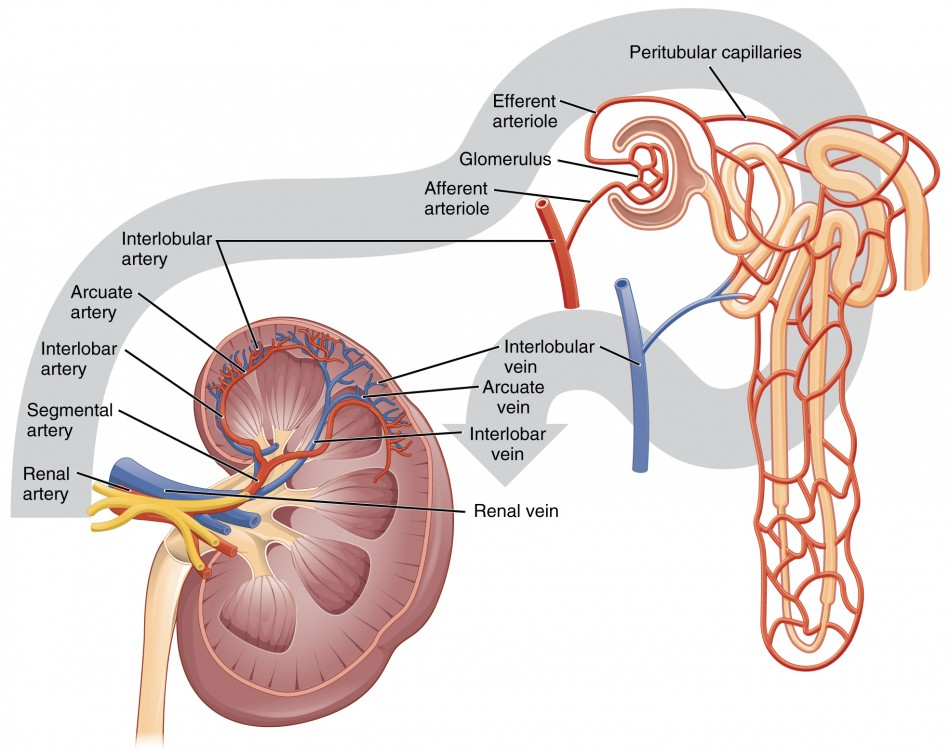
What happens after blood leaves the glomerulus through the efferent arteriole?
Blood flows to one of two capillary beds:
Peritubular capillaries (cortical nephrons) for reabsorption/secretion
Vasa recta (juxtamedullary nephrons) for maintaining medullary concentration gradient
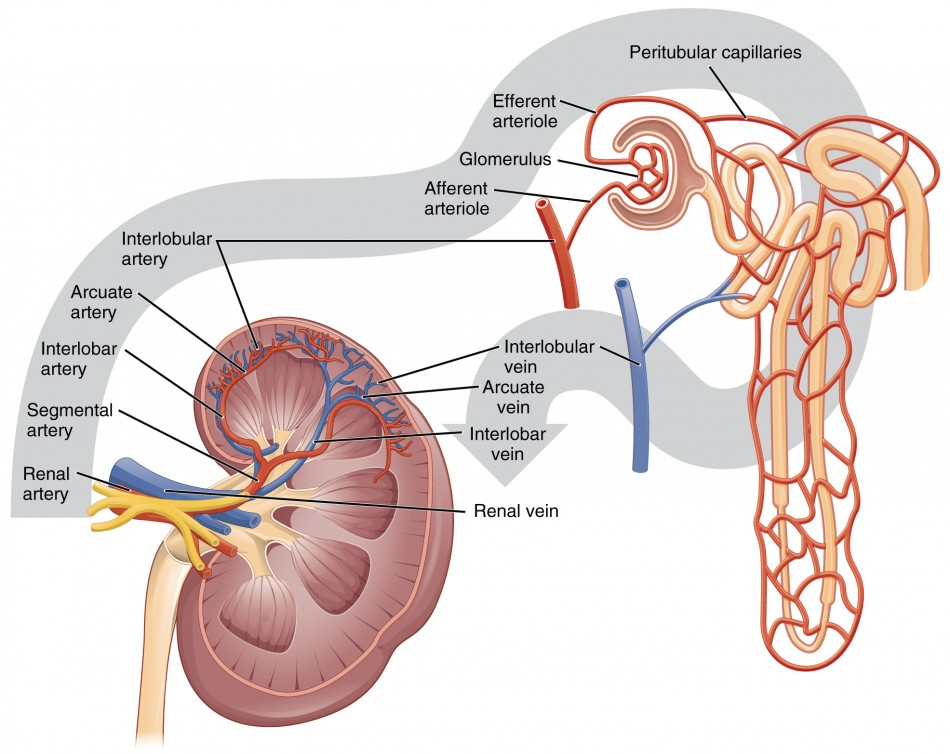
What is the correct order of venous blood flow out of the kidney?
Cortical radiate (interlobular) veins
Arcuate veins
Interlobar veins
Renal vein
→ Drains into the inferior vena cava
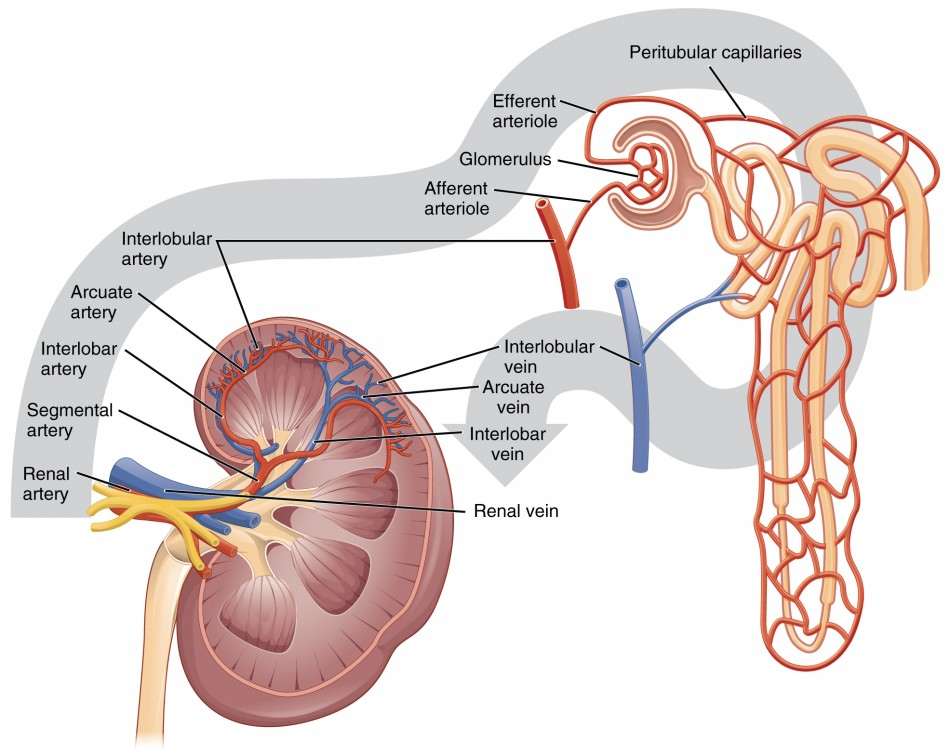
Which two vessels regulate blood flow to and from the glomerulus?
Afferent arteriole: Brings blood into the glomerulus
Efferent arteriole: Drains blood out of the glomerulus
→ Constriction/dilation of these arterioles helps regulate glomerular filtration rate (GFR).
What is glomerular filtration rate (GFR)?
The volume of filtrate formed by both kidneys per minute (about 125 mL/min). It indicates how well the kidneys are filtering blood.
What factors affect GFR?
Net filtration pressure (NFP)
Surface area of glomerular capillaries
Permeability of the filtration membrane
Afferent/efferent arteriole diameter
What is the countercurrent multiplier and where does it occur?
A process in the loop of Henle that establishes a concentration gradient in the medulla.
Descending limb: permeable to water
Ascending limb: pumps out Na⁺ and Cl⁻, not water
What is the countercurrent exchanger and where does it occur?
Occurs in the vasa recta (blood vessels of juxtamedullary nephrons).
Preserves the medullary gradient by removing water and solutes slowly, without disrupting the gradient.
What hormones regulate reabsorption in the distal nephron and collecting duct?
Aldosterone → ↑ Na⁺ reabsorption, ↑ K⁺ secretion
ADH (vasopressin) → ↑ water reabsorption
ANP → inhibits Na⁺ reabsorption, ↓ blood pressure
What part of the nephron is the major site of reabsorption?
The proximal convoluted tubule (PCT) — reabsorbs ~65% of filtrate
: What hormone regulates water reabsorption in the collecting duct?
Antidiuretic hormone (ADH) – it increases water reabsorption by making the collecting duct more permeable to water.
What happens in the collecting duct when ADH levels are low?
Water is not reabsorbed
Urine remains dilute
More water is lost in urine
What happens in the collecting duct when ADH levels are high?
Water is reabsorbed into the bloodstream
Urine becomes concentrated
Water loss is minimized
What type of urine is produced when ADH is high?
Concentrated urine – because more water is reabsorbed.
What type of urine is produced when ADH is low?
Dilute urine – because water stays in the filtrate and is excreted.
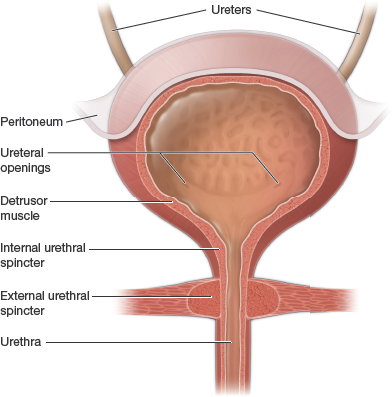
What triggers the micturition reflex?
Stretch receptors in the bladder wall are activated as the bladder fills.
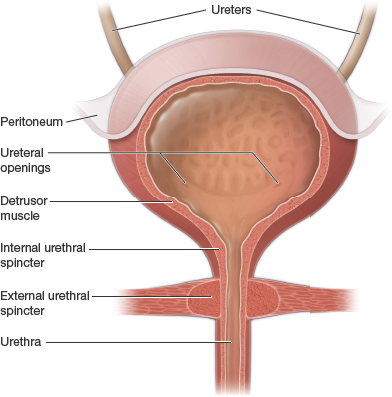
What part of the nervous system controls involuntary urination?
The parasympathetic nervous system, which contracts the detrusor muscle and relaxes the internal urethral sphincter.
What is the role of the detrusor muscle?
It is the smooth muscle in the bladder wall that contracts to expel urine during urination.
Where is the micturition center located in the CNS?
In the pons of the brainstem – coordinates voluntary and involuntary control.
What provides voluntary control over urination?
The external urethral sphincter, controlled by the pudendal nerve.