Exam 2 Pathology
1/206
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
207 Terms
what is chronic inflammation?
Inflammation of prolonged duration (weeks- years)
Chronic Inflammation is characterized by
• Lymphocytes, plasma cells, and macrophages
• Tissue destruction
• Repair
chronic inflammation arises in settings of:
persistant infections
immune-mediated disease
prolonged exposure to toxins
chronic inflammation arises in settings of persistant infections such as
• Treponema pallidum
• Mycobacterium
• Viruses
• Fungi
chronic inflammation arises in settings of prolonged exposure to toxins such as
silica and crystal
Fusion of activated macrophages forms
multinucleated giant cells
Mononuclear phagocyte system (reticuloendothelial system) includes cells scattered where?
in connective tissue, liver (Kupffer cells), spleen and lymph nodes (sinus histiocytes), CNS (microglial cells), and lungs (alveolar macrophages)
macrophages are activated by which pathway?
classical or alternative
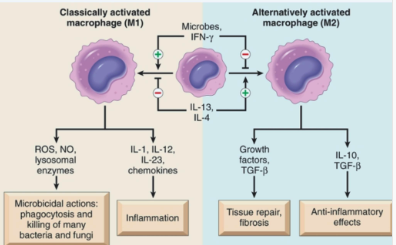
what roles do macrophages play in host defense and inflammatory response?
Phagocytosis
Tissue repair
Secretion of mediators
Proteases
Cytokines and eicosanoids
Antigen presentation
lymphocytes are mobilized in settings of
infections, necrosis, trauma
what cells are major drivers of autoimmune disease?
lymphocytes
what are the most prominent cells in chronic inflammation?
lymphocytes, monocyte-macrophages, and plasma cells
what is lymphocytosis?
Increased number of lymphocytes in the peripheral blood
what is lymphocytosis caused by?
most often → viral infections (Influenza, mumps, rubella, infectious mononucleosis)
but also certain bacterial infections (Whooping cough, tuberculosis)
what are the Predominant inflammatory cells in immune reactions and parasitic infections?
eosinophils
which inflammatory response do mast cells participate in?
both acute and chronic (by releasing histamine when exposed to antigens)
what is granuloma?
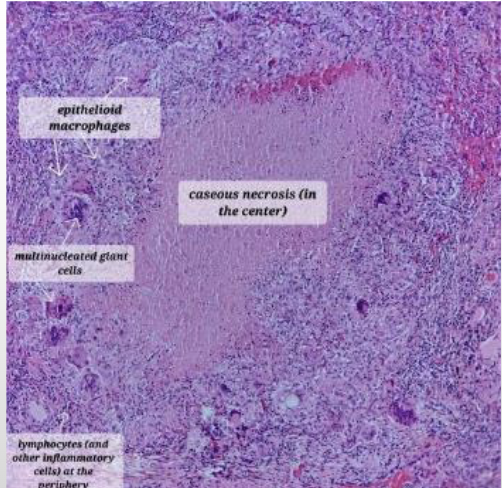
specific histopathologic pattern of chronic inflammation characterized by epithelioid histiocytes
what cells are often included in granulomatous inflammation?
multinucleated giant cells, lymphocytes, fibroblasts, and/or connective tissue
granulomatous inflammation may or may not exhibit
caseous necrosis
granulomas are caused by
Foreign body reactions
infections (Tuberculosis, tertiary syphilis, cat-scratch disease, leprosy, deep fungal infections)
immune-mediated diseases (Crohn disease, orofacial granulomatosis, granulomatosis with polyangiitis)
Idiopathic disorders (Sarcoidosis)

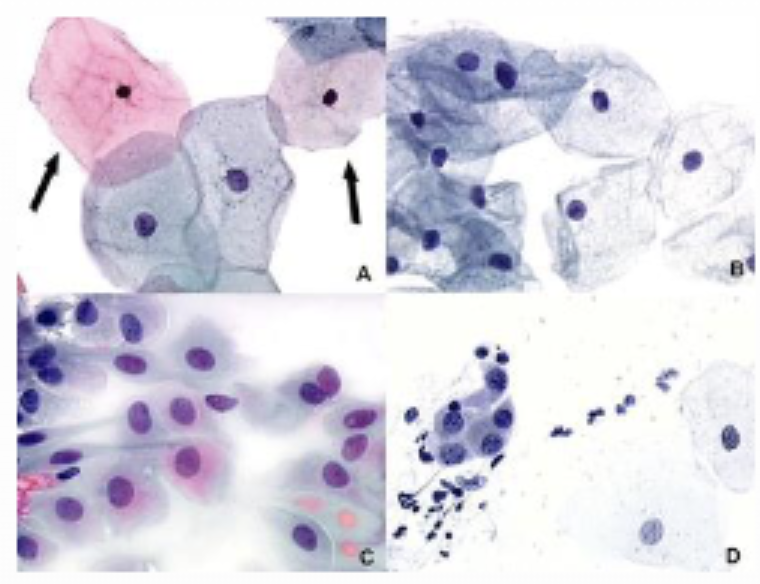
granulomas

subtle swelling of upper lip (granuloma inflammation due to Crohns disease)

granuloma inflammation due to Crohns diseaseCrohns disease
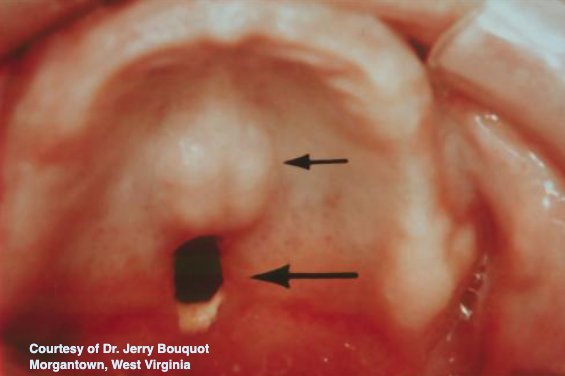
granuloma inflammation due to palatal preforation (drugs)
granuloma (w multi-nucleated cells)
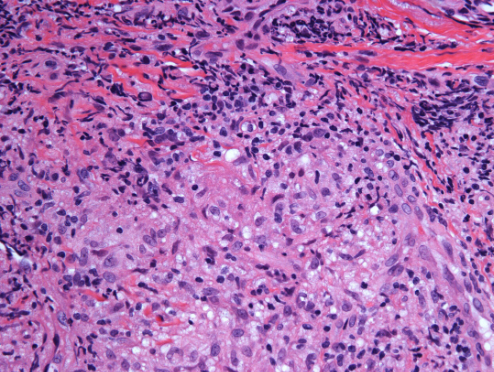
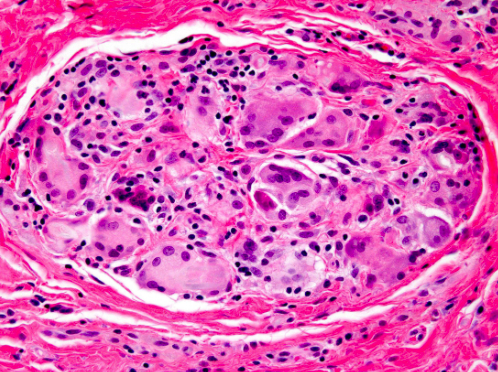
granuloma (w multi-nucleated giant cells)
what is the most common cause of granulomas in the oral cavity is
foreign body reaction
Granulomatous Disorders are caused by
foreign material (organic or inorganic) that cannot be phagocytosed by neutrophils
what endogenous foreign material examples that may cause granulomatous disorders?
Keratin, urate crystals, degenerated altered collagen, degenerated altered elastin (artery walls)
what exogenous foreign material examples that may cause granulomatous disorders?
Sutures, talcum powder, vegetable matter
what kind of reaction is tuberculosis?
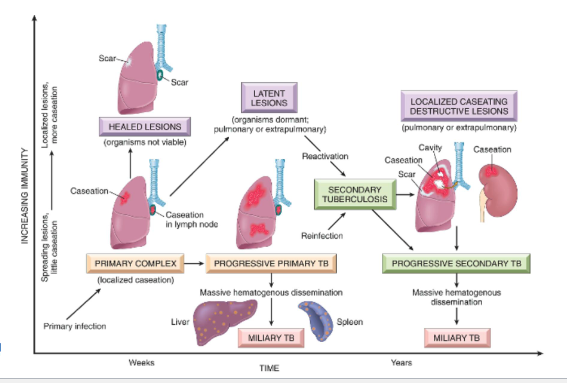
Type IV hypersensitivity reaction
how does tuberculosis start?
M. tuberculosis inhaled into alveolar spaces of lung, other tissues
Neutrophils cannot degrade cell wall; acute inflammation persists and becomes chronic granulomatous inflammation
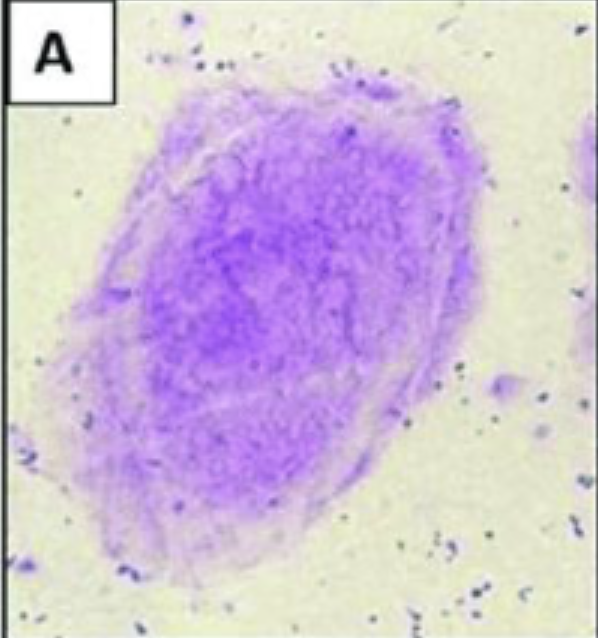
what are the large multinucleated cells seen in granulomatous diseases called?
Langhans giant cell
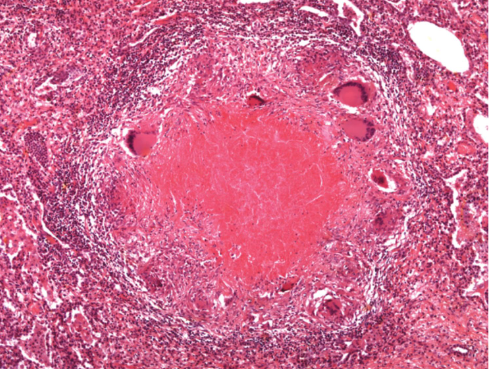
in tuberculosis, Central caseous necrosis is surrounded by
collection of
activated epithelioid histiocytes
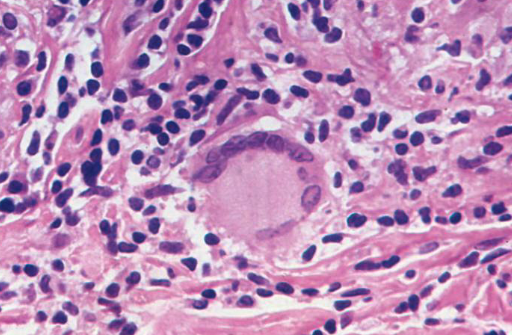
Langhans giant cell w nuclei arranged on periphery of abundant cytoplasm
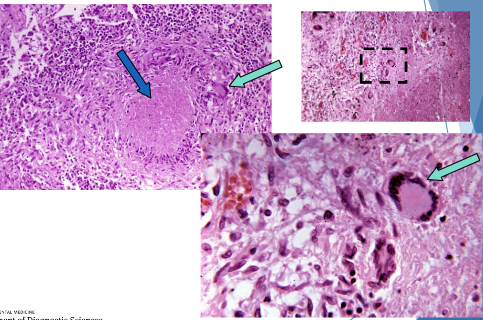
blue = Central caseous necrosis
green = Langhans giant cell
tuberculosis typically involves what organs?
lungs (but may affect other organs)
what are factors that favor extension in tuberculosis?
• Large numbers of highly-virulent organisms
• Poor immune response (malnutrition, extreme youth or old age, disease, immunosuppression)
what are factors that favor continment/eradication in tuberculosis?
• Small numbers of poorly-virulent organisms
• Good immune response (health, immunization)
• Antibiotic administration
tuberculosis infection leads to what reaction?
delayed hypersensitivity reaction (PPD test)
what is primary tubercuosis?
Disease in unsensitized patients
• Bacteria inhaled and proliferate
• Bacterial organism not destroyed
in primary tuberculosis, Once immune system is exposed to organism, the patient is sensitized and no disease progression occurs BUT what can happen?
latent tuberculosis (Viable organisms may remain walled off within
the healed primary complex)
Caseating TB in a peribronchial lymph node
what is progressive primary tuberculosis?
• Patient unable to mount sufficient immune response
• Continuing enlargement of caseating granulomas in lymph nodes
• More common in immunocompromised and Inuit populations
what is secondary tuberculosis?
• May follow soon after primary TB but more commonly after reactivation of dormant organisms
• Classically localized to apices
• Cavitation often seen
• Outcome varies
secondary tuberculosis is the Pattern of disease arising in what population?
5% of previously sensitized host
what is miliary tuberculosis?
Organisms disseminate through vascular system to heart and
pulmonary arteries, liver, bone marrow, spleen, and other organs
what are outcomes of tuberculosis?
vigorous immune response
Healing of apical lesion
Containment of the infection; no further spread of organism
fibrous wall breaks down
reactivated fibrocaseous TB
tuberculosis diagnosis is done how?
Active disease confirmed with culture and special mycobacterial stains (like Mantoux or PPD skin test)
how does Mantoux or PPD skin test diagnose tuberuclosis?
Detects cell-mediated hypersensitivity reaction after initial exposure (indicates infection, not active disease)

Mantoux or PPD skin test
what is the treatmenet and prognosis of tuberculosis?
BCG (Bacille Calmette Guérin) vaccination
BCG (Bacille Calmette Guérin) vaccination is made from?
Made from live weakened strain of Mycobacterium
bovis
• 50% effective in reducing likelihood and severity in
infants and young children
• Used in countries with high prevalence of tuberculosis
tuberculosis is caused by what bacteria?
mycobacterium tuberculosis
what are other mycobacterial diseases that cause cC=hronic inflammatory granulomatous response with minimal acute inflammation?
M. leprae → Leprosy
M. scrofulaceum → Scrofula and Enlarged lymph nodes of the neck
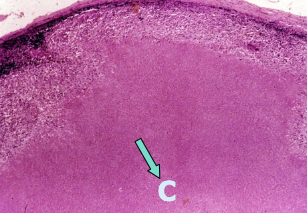
what is sarcoidosis?
Idiopathic multisystem disorder that causes lungs and lymph node enlargement (may result in pulmonary fibrosis)
discrete granulomas caused by sarcoidosis are mainly located where?
lymph nodes, lungs, liver, spleen and skin (rarely brain, bone)
giant cells in sarcoidosis may have what?
• Schaumann bodies- laminated calcific spherical concretions
• Asteroid bodies- stellate shapes

sarcoidosis
what is pathology?
The study of understanding the cause of disease and the changes in cells, tissues, and organs that are associated with disease
what is etiology?
Underlying causes and modifying factors that are responsible for initiation and progression of disease
what is pathogenesis?
Mechanisms of development and progression of disease, which account for the cellular and molecular changes that give rise to the specific abnormalities that characterize any particular disease
what is homeostasis?
• Steady state of normal cells
• Equilibrium between the cells and their environment
• Cells actively interact with their environment, constantly adjusting their structure and function to accommodate changing demands and extracellular stresses
what happens when homeostasis is disturbed?
If disturbed, the cell can be predisposed for onset of pathology
what are adaptations to environmental stress?
reversible changes in the number, size, phenotype, and metabolic activity cellular functions in response to change in their environment
Cell injury within limits is reversible. If the stressor is severe, persistent, or rapid in onset it
will result in …?
irreversible injury and death of the affected cell
what are causes of cell injury?
• Hypoxia and ischemia
• Toxins
• Infectious agents
• Immunologic reactions
• Genetic abnormalities
• Nutritional imbalances
• Physical agents
• Aging
what is reversible cell injury?
The deranged function and morphology of the injured cells can return to normal if the
damaging stimulus is remove
what are the 2 main morphologic correlates of reversible cell injury?
cellular swelling
fatty change
what is cellular swelling?
Injury associated with increased permeability of the plasma membrane
Cells and organelles take in water due to failure of the energy dependent ion pumps
Pallor due to compression of capillaries
Increased organ weight
what is fatty change?
Appearance of triglyceride containing lipid vacuoles in the cytoplasm
Nucleus is displaced and the cell swells
Seen frequently in liver, heart, and kidney
Ex: secondary to alcoholism, diabetes mellitus, malnutrition, obesity, and poisoning
Imbalance among uptake, utilization, and secretion of fat
what are the 2 pathways of irreversible injury?
apoptosis
necrosis
what is apoptosis?
programmed cell death (How we eliminate potentially harmful cells or cells that have outlived their usefulness (physiologic apoptosis)
No inflammatory cell response
Eliminates cells damaged beyond repair (apoptosis in pathologic conditions)
Ex: exposed to radiation, cytotoxic drugs, certain infections or viruses
what is necrosis?
accidental cell death (Cell death in which cellular membranes fall apart, and cellular enzymes leak out and ultimately digest the cell)
inflammatory cell response
Due to severe disturbances like loss of oxygen or nutrients
Rapid and uncontrollable
how does apoptosis work?
Fragments of the apoptotic cells break off (“apoptotic bodies”)
Apoptotic bodies are consumed by phagocytes
plasma membrane remains intact = liitle leakage of cellular contents so no inflammatory process
what is physiologic apoptosis?
During normal development, some cells die and are replaced by new ones
In these situations, cell death is always via apoptosis
Unwanted cells are eliminated without eliciting potentially harmful inflammation
In the immune system, apoptosis eliminates excess leukocytes and lymphocytes left at the end of an immune response
what is pathologic apoptosis?
Cells damaged beyond repair
Ex: DNA damage after radiation or cytotoxic drugs
Misfolded proteins
Certain infectious agents like viruses elicit apoptosis
what are morphologic characteristics of apoptosis?
Cells shrink
Chromatin condensation and aggregation
Fragmentation of DNA
Cells form cytoplasmic buds and fragment into apoptotic bodies
Composed of membrane bound pieces of cytosol and organelles
Rapid extrusion of fragments and phagocytosis
No inflammatory response
necrosis involves nuclear changes resulting from…?
breakdown of DNA and chromatin
Pyknosis- shrinkage of nucleus into a basophilic (darker) mass due to DNA condensing
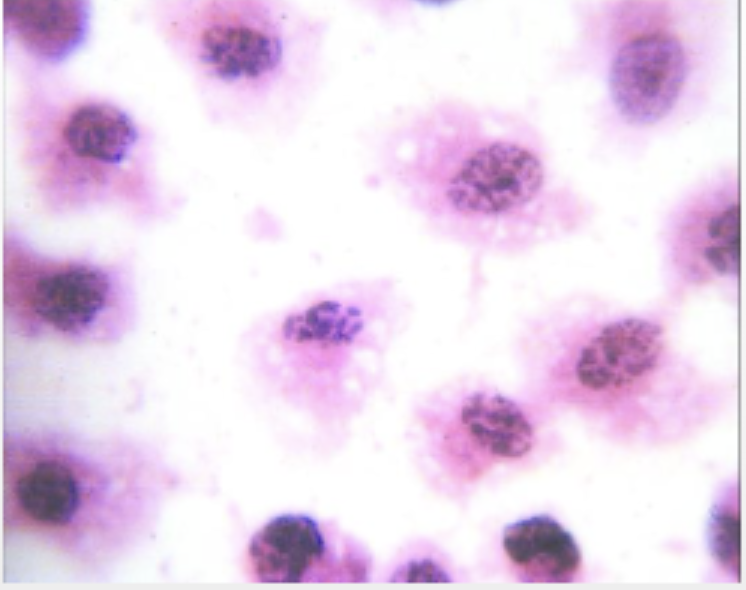
Karyorrhexis- fragmentation of nucleus into multiple small pieces
Karyolysis- fading of nucleus, less and less basophilic as DNA is digested
what are some cytoplasmic changes that occur during necrosis?
Increased pink cytoplasm – eosin dye binding to denatured proteins
Glassy, homogenous appearance
Vacuolated or “moth eaten” once the organelles have been digested by enzymes
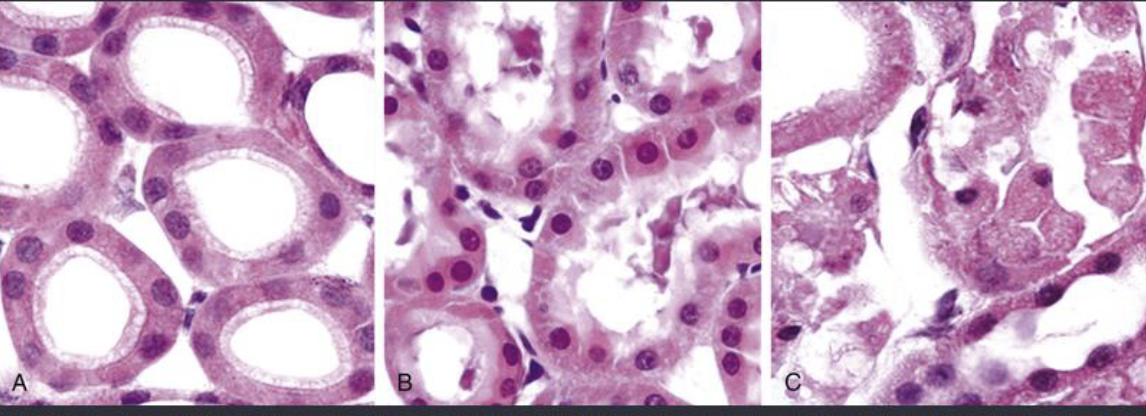
normal
early necrosis
necrosis (irreversible)
what are types of necrosis?
• Coagulative
• Liquefactive
• Gangrenous
• Caseous
• Fat
• Fibrinoid
what is the most common type of necrosis?
COAGULATIVE NECROSIS
what is COAGULATIVE NECROSIS?
Sudden loss of blood supply to an organ (ischemia)
Does not occur in the brain
Denaturation of proteins and enzymes resulting in blockage of proteolysis of
dead cellsUnderlying tissue architecture is preserved for a few days after death of the cells in the tissue
what is liquefactive necrosis?
Seen in focal bacterial and occasional fungal infections
Microbes stimulate rapid accumulation of inflammatory cells
Enzymes of the leukocytes digest (“liquefy”) the tissue
Hypoxic death of cells in the CNS
If initiated by acute inflammation like in bacterial infection the liquid will be pus

liquefactive necrosis
what is GANGRENOUS NECROSIS?
A clinical descriptor, not a distinct pattern of necrosis
Usually refers to a limb that has undergone coagulative necrosis involving multiple
tissue layers
what is “dry” gangrene?
Coagulative necrosis without liquefaction
what is “wet” gangrene?
Bacterial infection superimposed
Results in liquefactive necrosis
CASEOUS NECROSIS is most often seen in?
tuberculosis
CASEOUS NECROSIS
what is the histopathology of CASEOUS NECROSIS?
architecture is not preserved
Fragmented or lysed cells
Amorphous pink and granular
Often surrounded by a collection of macrophages and other inflammatory cells (granuloma)
describe the histopathology of fat necrosis
Shadowy outlines of necrotic fat cells
Basophilic calcium deposits
Inflammatory reaction
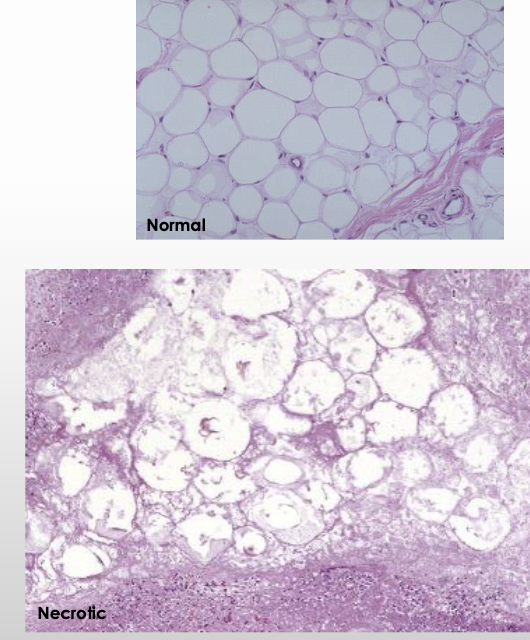
FAT NECROSIS
what is traumatic FAT NECROSIS?
severe injury to areas with high fat content
• Breast- post-cancer procedures and radiation
• Thigh and buttock- following medical and cosmetic procedures
what is enzymatic FAT NECROSIS?
complication of acute pancreatitis
• Pancreatic enzymes leak out of pancreas and destroy fat cells in peritoneum
• Triglyceride esters within the fat are split releasing fatty acids
• Fatty acids combine with calcium to produce chalky white areas (fat saponification)