Intrinsic Muscles of Larynx
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
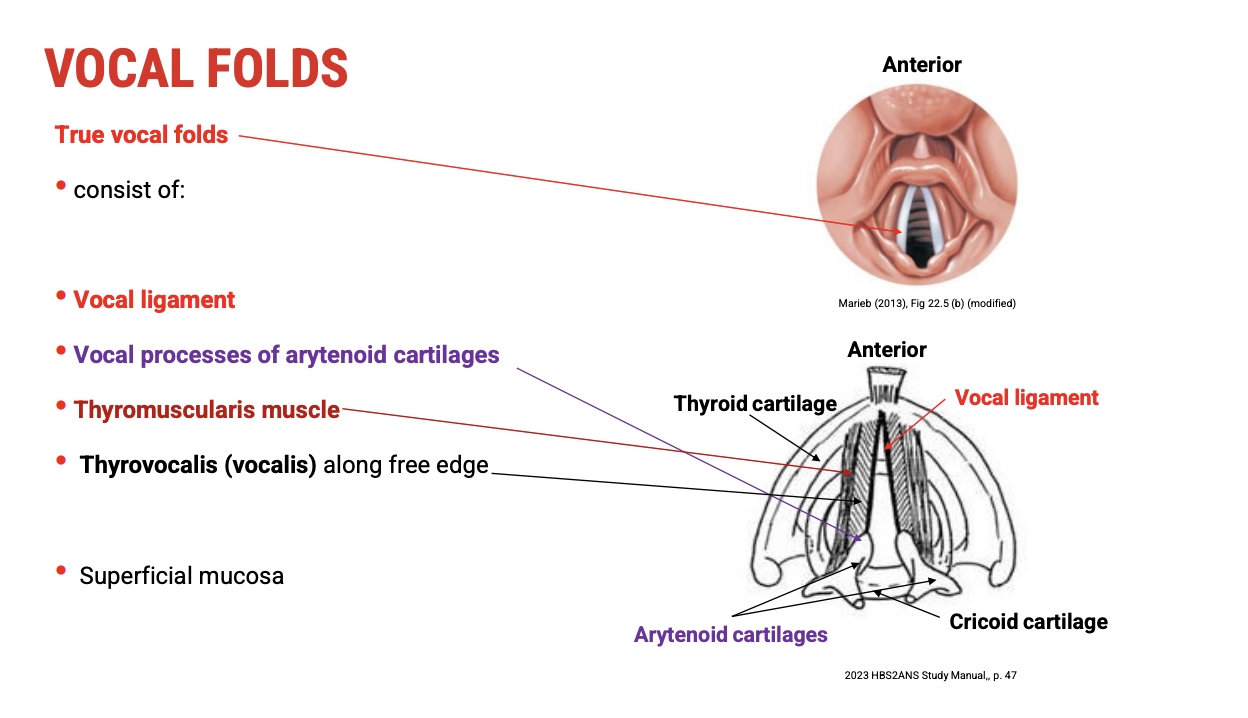
Anatomy of the Vocal Folds
🔹 Key Structures of the Vocal Folds (from medial to lateral)
Vocal Ligament (Most Medial)
Attached to the vocal process of the arytenoid cartilage
Provides tensile support and elastic recoil essential for vibration
Thyroarytenoid Muscle Group
Divided into two parts:
Thyrovocalis (Vocalis) Muscle (immediately lateral to the vocal ligament)
Fine-tunes vocal fold tension and pitch
Thyromuscularis Muscle (lateral to the thyrovocalis)
Controls vocal fold position and adduction
Superficial Mucosa
Covers all these internal structures
Provides smooth gliding surface for vibration
Contains stratified squamous epithelium to withstand mechanical stress
🧠 Functional Summary
The vocal ligament and vocalis muscle together form the vibratory core of the true vocal fold.
The thyromuscularis acts more on adduction and relaxation.
The mucosal covering is essential for efficient vibration and protection.
Coronal Section of the True Vocal Folds: Anatomical & Histological Overview
Structures Visible in Coronal View (Posterior to Anterior)
Surface Layer:
Epithelium / Mucosa
Stratified squamous epithelium covers the vocal folds, providing protection against mechanical stress during vibration.
Vocal Ligament:
Fibroelastic structure composed of collagen and elastin fibers
Provides tensile strength and elasticity for phonation.
Thyrovocalis Muscle (Medial portion of thyroarytenoid muscle):
Adjacent and lateral to the vocal ligament
Controls fine tension adjustments of the vocal folds for pitch modulation.
Thyromuscularis Muscle (Lateral portion of thyroarytenoid muscle):
Lateral to thyrovocalis
Functions in vocal fold adduction and relaxation.
Lateral Arytenoid Muscle:
Located posterior-laterally
Important for adduction of the vocal folds.
Cartilages:
Inferiorly: Cricoid cartilage, covered by the conus elasticus (fibroelastic membrane)
Superiorly: Thyroid cartilage
🧫 Histological Importance
The conus elasticus forms the inferior lining and contributes to the vocal ligament.
Stratified squamous epithelium allows the vocal folds to resist trauma from vibration and airflow.
Underlying muscle and ligament provide structure and dynamic movement essential for phonation.
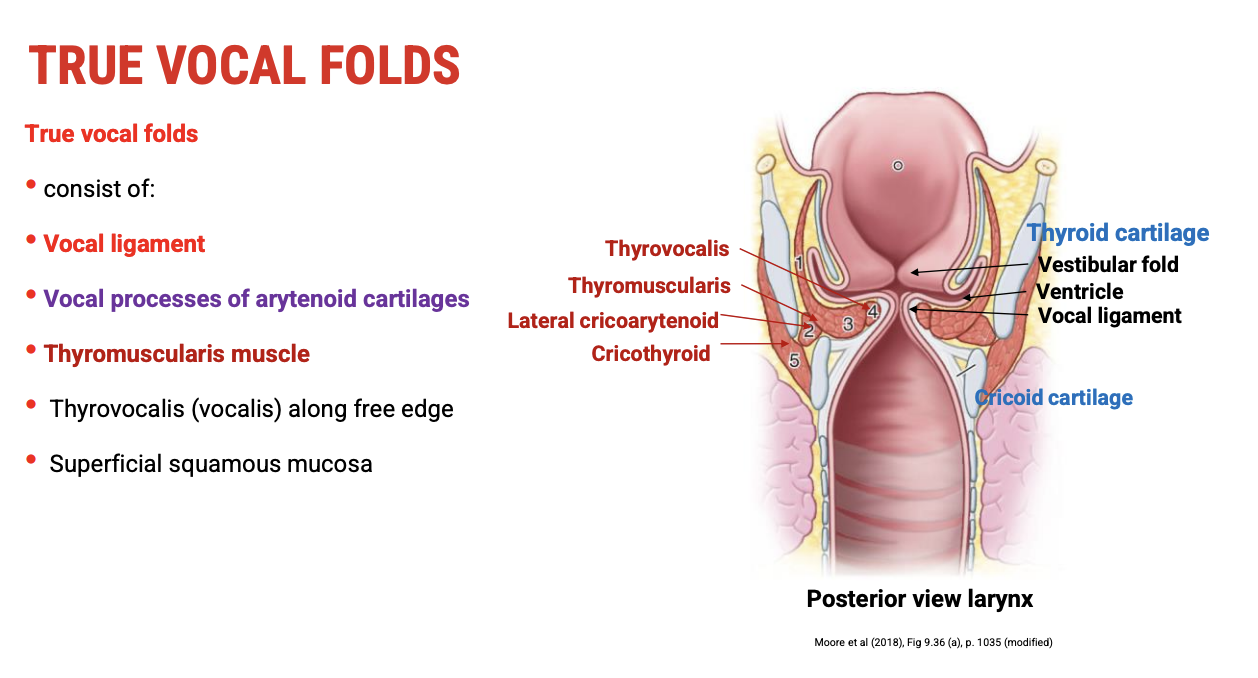
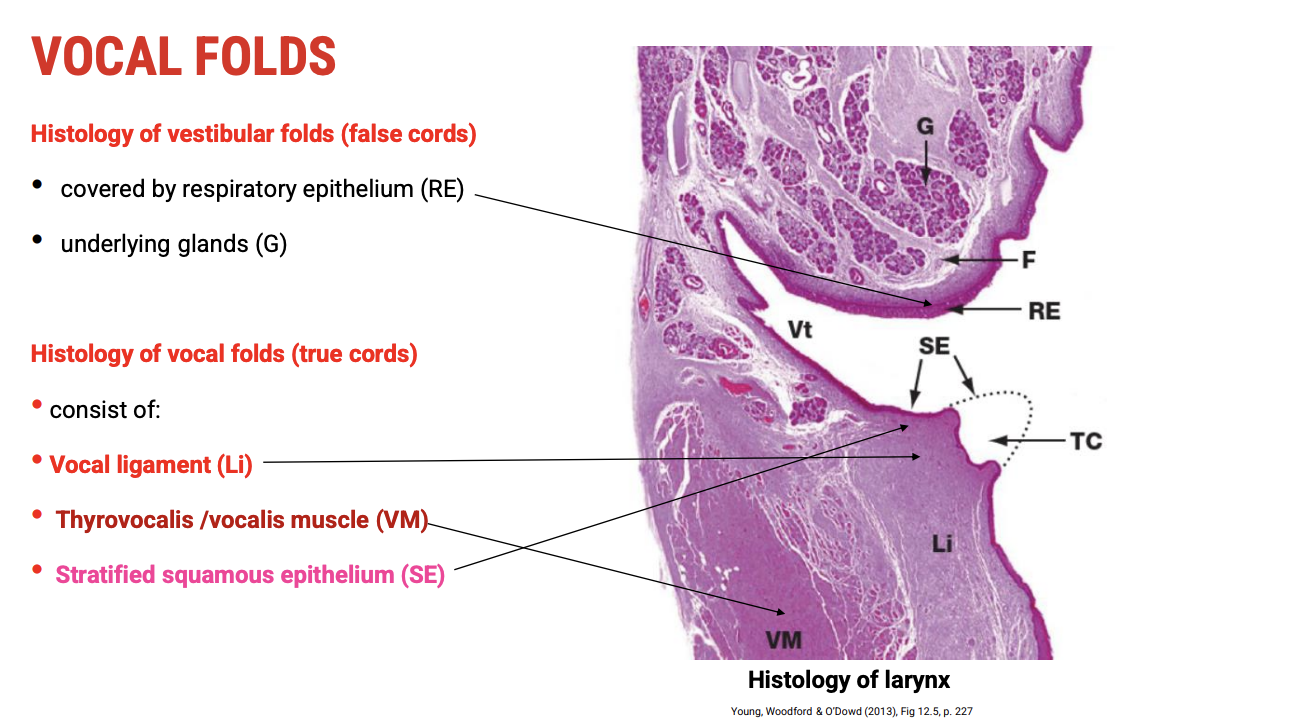
Coronal Section: False Vocal Fold vs True Vocal Fold
🔹 False Vocal Fold (Vestibular Fold) — Superior
Epithelium:
Covered by respiratory epithelium — pseudostratified columnar epithelium
This type contains cilia and mucus-secreting glands
Underlying Structures:
Contains glands to keep the mucosa moist and protected
Function:
Primarily protective, helps close the airway during swallowing
Anatomical Landmark:
Ventricle — the space (gap) between false and true vocal folds
🔸 True Vocal Fold (Vocal Cord) — Inferior
Central Core:
Vocal ligament — composed of elastic and collagen fibers, providing structural support and elasticity
Deep to Ligament:
Thyrovocalis muscle — controls tension of the vocal fold for phonation
Epithelium Covering:
Stratified squamous epithelium (denoted as SE)
Provides durability against mechanical stress from vibration and airflow during phonation
Function:
Primary structure for sound production (phonation)
🧠 Summary
Structure | Epithelium Type | Function |
False Vocal Fold | Pseudostratified columnar | Protective, mucus secretion |
Ventricle (gap) | — | Space between folds |
True Vocal Fold | Stratified squamous | Sound production |
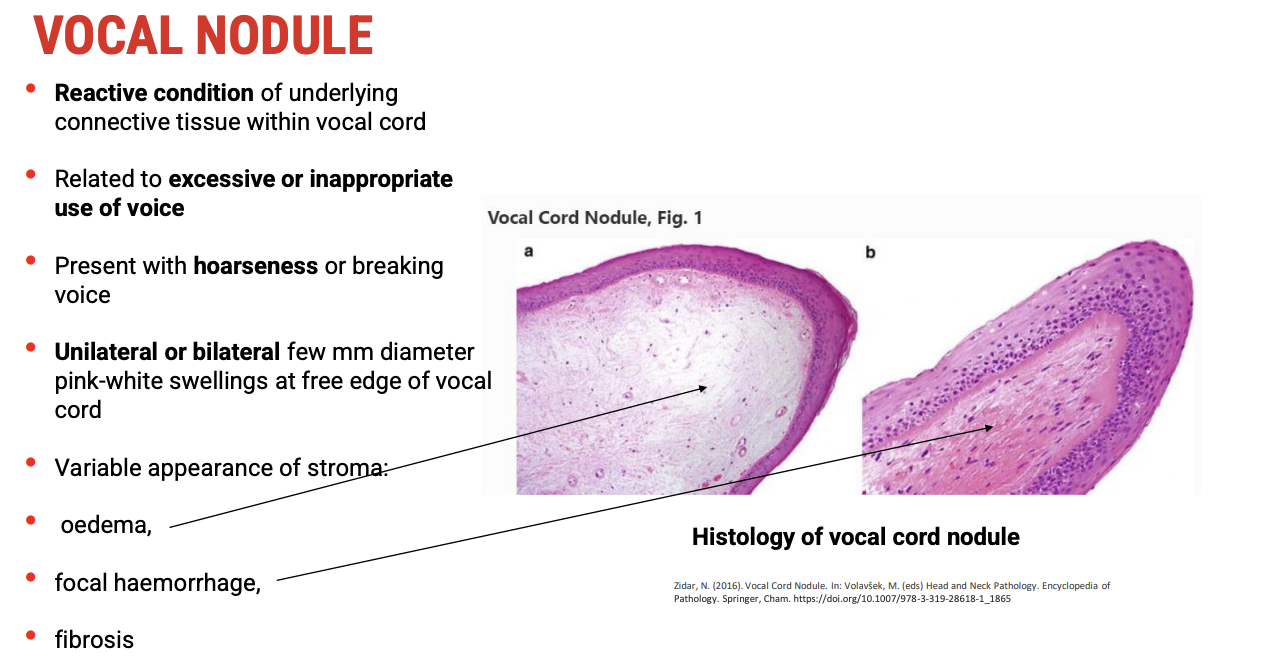
Vocal Nodules: Pathology and Clinical Features
🔍 Histology & Pathophysiology
Vocal nodules are a reactive lesion of the underlying connective tissue (stromal layer) of the true vocal folds.
They result from excessive or inappropriate voice use (voice abuse or misuse).
Histological changes include:
Edema (fluid accumulation in the stroma)
Focal haemorrhage (small bleeding spots)
Fibrosis (scarring and thickening of connective tissue)
Nodules do not involve malignant transformation or epithelial dysplasia—there is no cancer risk.
👁 Macroscopic Appearance (Laryngoscopy)
Small, pink-white swellings located at the free edge of the vocal folds.
Can be:
Unilateral or bilateral
Bilateral nodules may create an hourglass shape of the glottis during phonation.
🗣 Clinical Presentation
Common symptoms include:
Hoarseness
Voice breaks or instability
Vocal fatigue
🧠 Summary
Feature | Description |
Cause | Excessive/inappropriate voice use |
Histology | Reactive stromal changes (edema, haemorrhage, fibrosis) |
Macroscopic Appearance | Small pink-white nodules at free vocal fold edge |
Malignancy Risk | None |
Symptoms | Hoarseness, voice breaks, vocal fatigue |
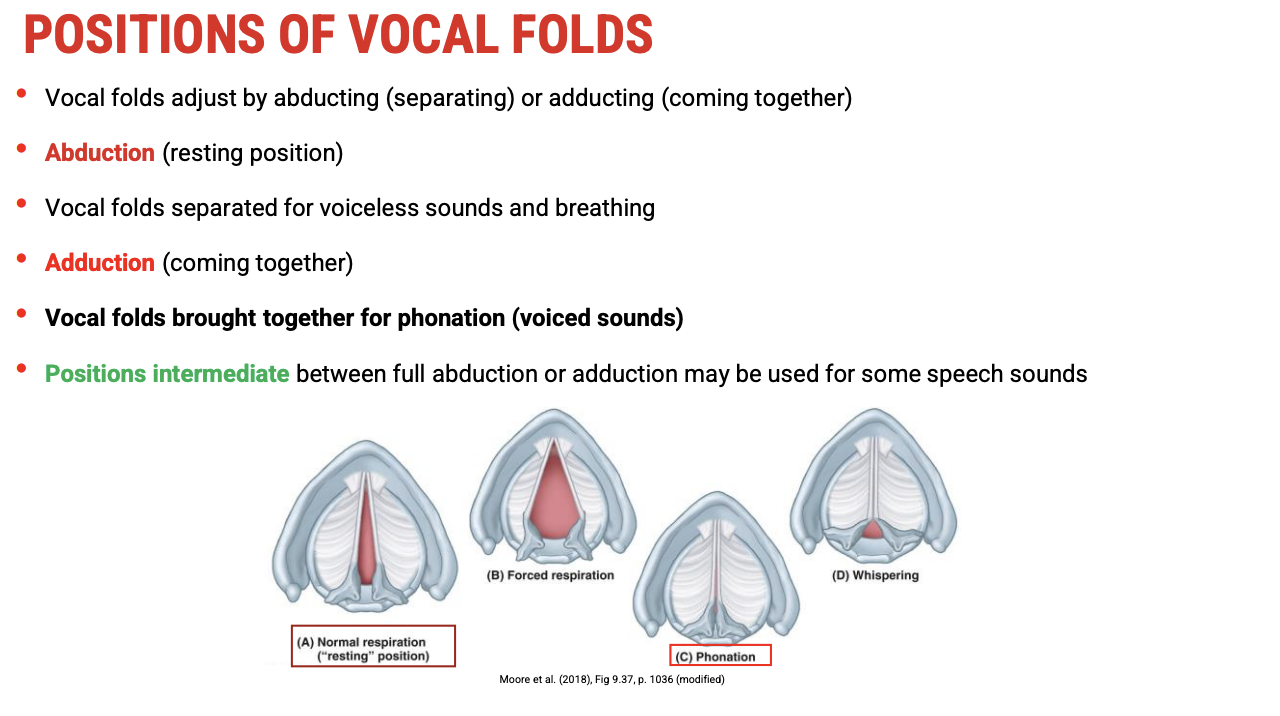
Positions and Movements of the Vocal Folds
🔹 Key Positions
Resting Position:
Slight abduction (vocal folds slightly apart)
Allows for quiet breathing and voiceless speech sounds.
Forced Abduction:
Vocal folds are widely separated
Occurs during heavy respiration or deep breathing (e.g., during exercise).
Adduction:
Vocal folds are brought together
Necessary for phonation (voiced sounds) and whispering.
In whispering, the vocal folds are adducted but the cartilaginous portions remain slightly apart, allowing air to pass.
Intermediate Positions:
Between full abduction and adduction for producing various speech sounds requiring precise control.
🔄 Functional Summary
Position | Description | Function |
Slight Abduction | Vocal folds slightly apart | Quiet breathing, voiceless sounds |
Forced Abduction | Vocal folds widely separated | Heavy respiration |
Adduction | Vocal folds closed | Phonation, voiced sounds, whispering |
Intermediate | Partial opening/closing | Fine speech sound modulation |
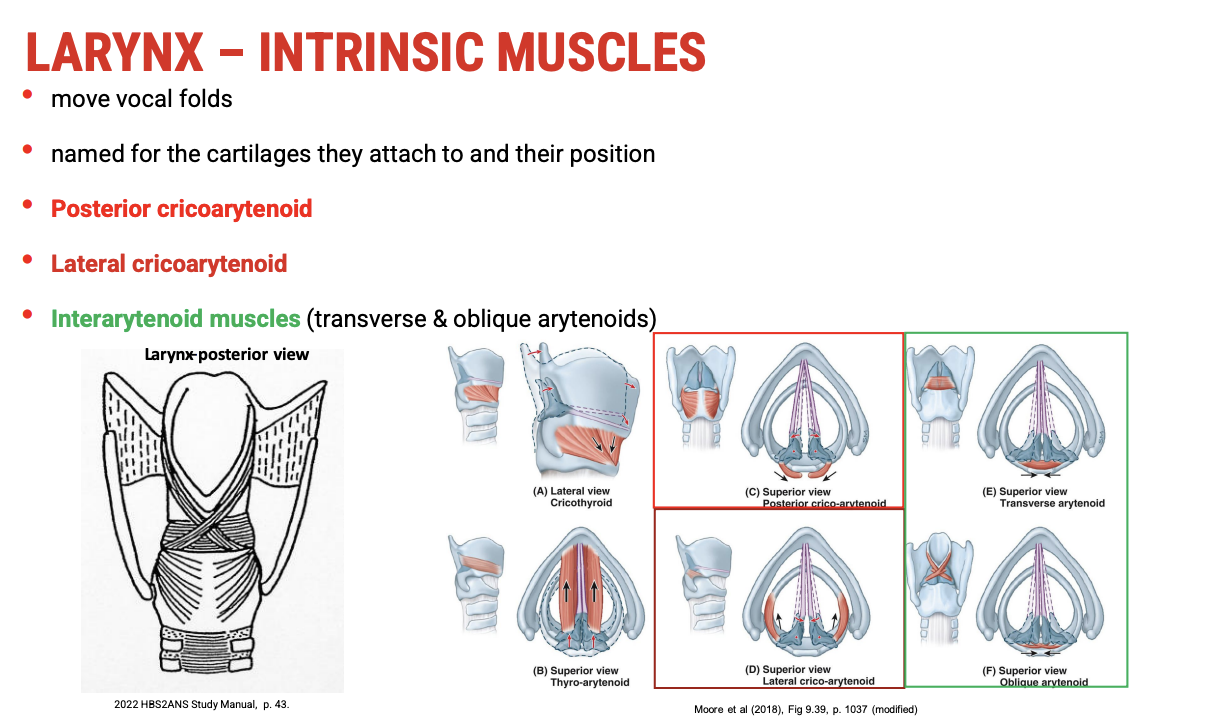
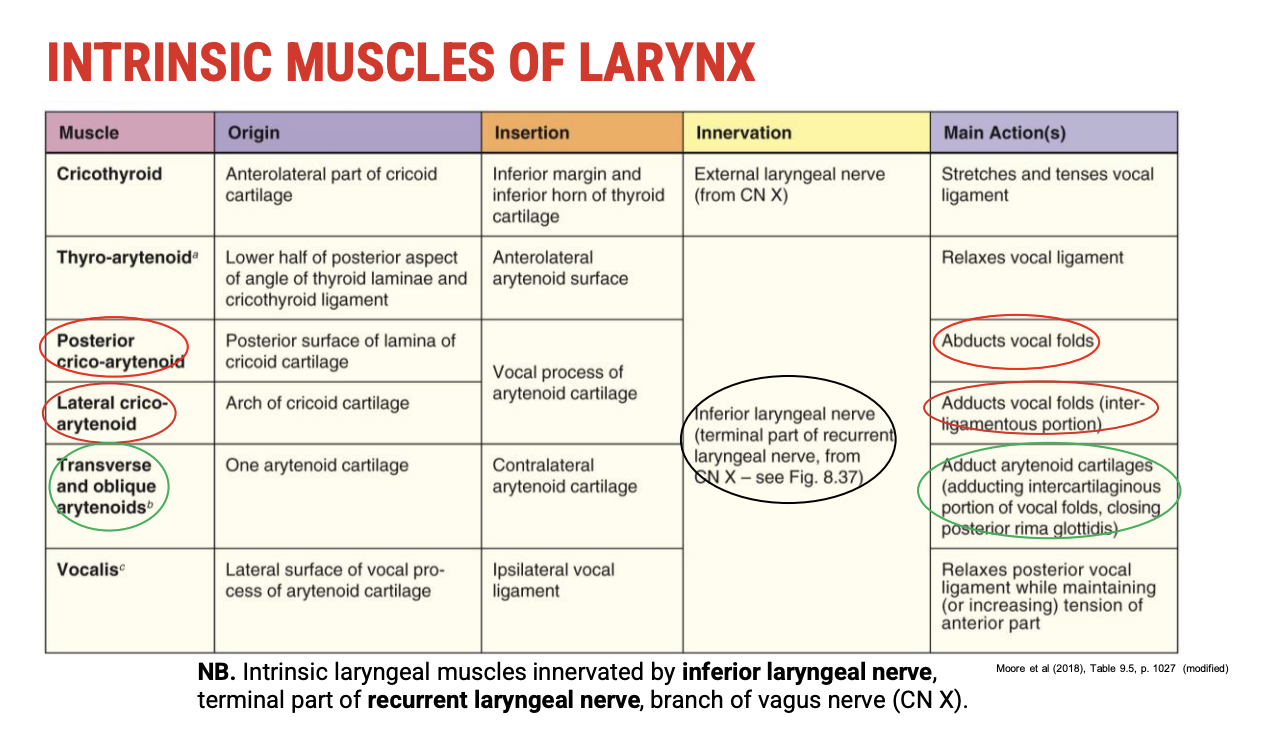
Intrinsic Muscles of the Larynx: Overview and Naming
🔹 Muscle Naming Principles
Named based on:
Cartilages they attach to (e.g., cricoid, arytenoid)
Position relative to the arytenoid cartilages (posterior, lateral, or between)
🔸 Intrinsic Muscles Attached to Cricoid & Arytenoid Cartilages
Muscle Name | Location/Position | Function Summary |
Posterior Cricoarytenoid | Posterior, between cricoid & arytenoid | Only abductor of vocal folds; opens glottis for breathing |
Lateral Cricoarytenoid | Lateral, between cricoid & arytenoid | Adductor; closes vocal folds for phonation |
Interarytenoid | Between arytenoids (transverse and oblique fibers) | Adducts arytenoid cartilages, closing posterior glottis |
🧠 Functional Highlights
Posterior cricoarytenoid is key for opening the vocal folds (abduction).
Lateral cricoarytenoid and interarytenoid muscles work to close the vocal folds (adduction), essential for voice production.
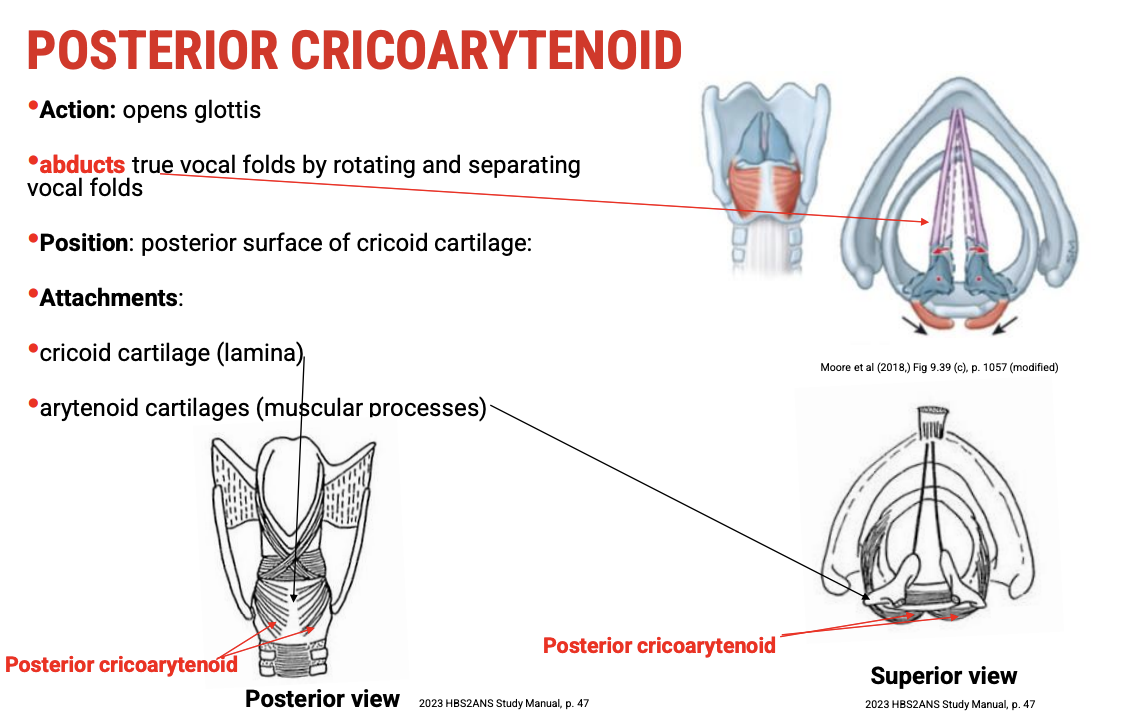
Posterior Cricoarytenoid Muscles
🦴 Anatomical Location
Located on the posterior surface of the cricoid cartilage (hence the name).
Origin: Posterior cricoid lamina
Insertion: Muscular process of the arytenoid cartilage
🔄 Function
Abducts the vocal folds by rotating the arytenoid cartilages laterally.
This action opens the glottis, allowing air passage for breathing.
The only intrinsic laryngeal muscle responsible for vocal fold abduction (opening).
👨🏫 Clinical/Workshop Tip
Movement can be visualised by rotating arytenoids away from the midline on larynx models, showing how vocal folds separate.
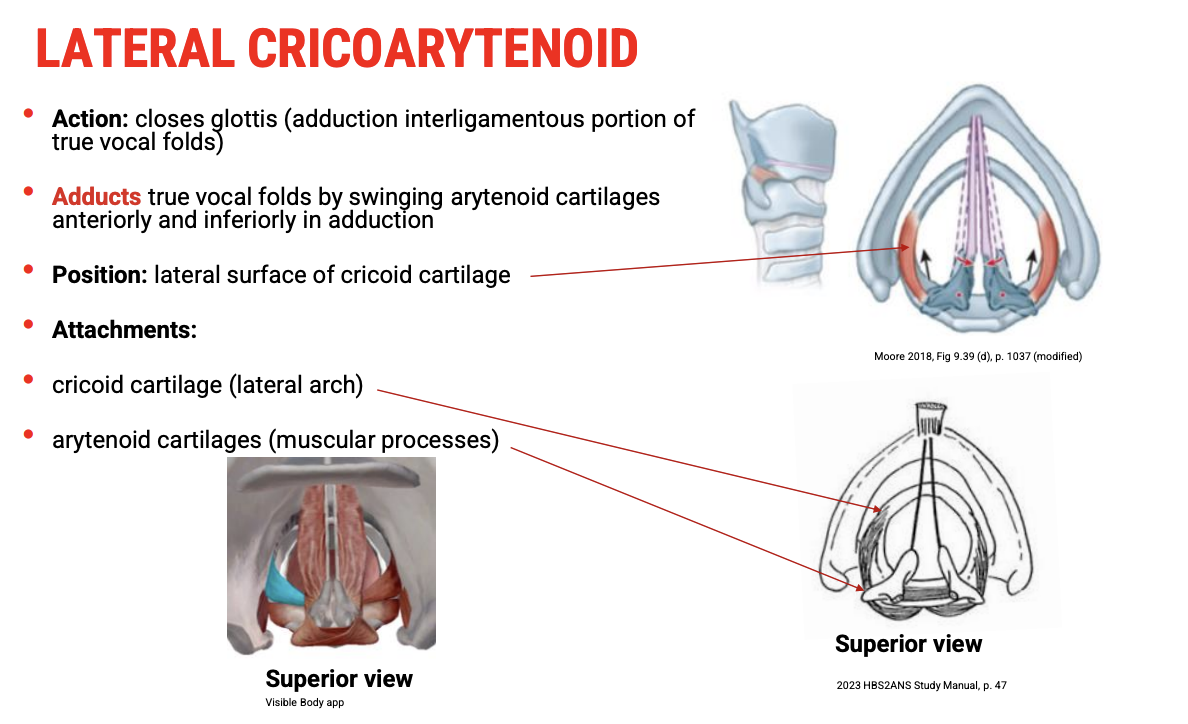
Lateral Cricoarytenoid Muscles
🦴 Anatomical Location
Positioned on the lateral surface of the cricoid cartilage, mainly on the arch.
Origin: Lateral cricoid cartilage (arch)
Insertion: Muscular process of the arytenoid cartilage
🔄 Function
Adducts the vocal folds by swinging the arytenoid cartilages anteriorly and inferiorly.
This movement closes the glottis, particularly the interligamentous (vocal fold) portion.
Responsible for bringing the true vocal folds together for phonation.
👁 Visualisation Tip
You can see their location and action clearly in anatomical apps like the Visible Body app, highlighting their role in vocal fold closure.
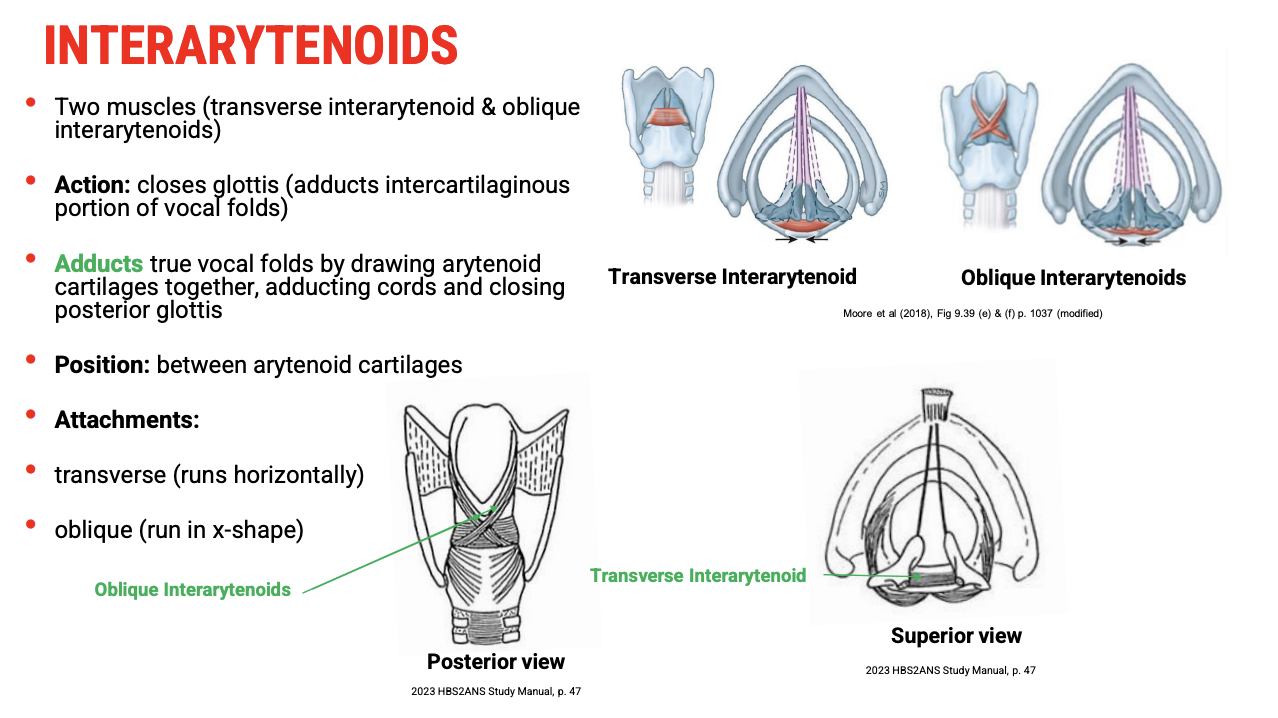
Interarytenoid Muscles
🦴 Anatomical Location
Located between the arytenoid cartilages.
Composed of two parts:
Transverse interarytenoid (runs horizontally)
Oblique interarytenoids (run diagonally in an X shape)
🔄 Function
Adduct the arytenoid cartilages, effectively closing the posterior (intercartilaginous) part of the glottis.
This action complements the lateral cricoarytenoid muscles to fully close the vocal folds.
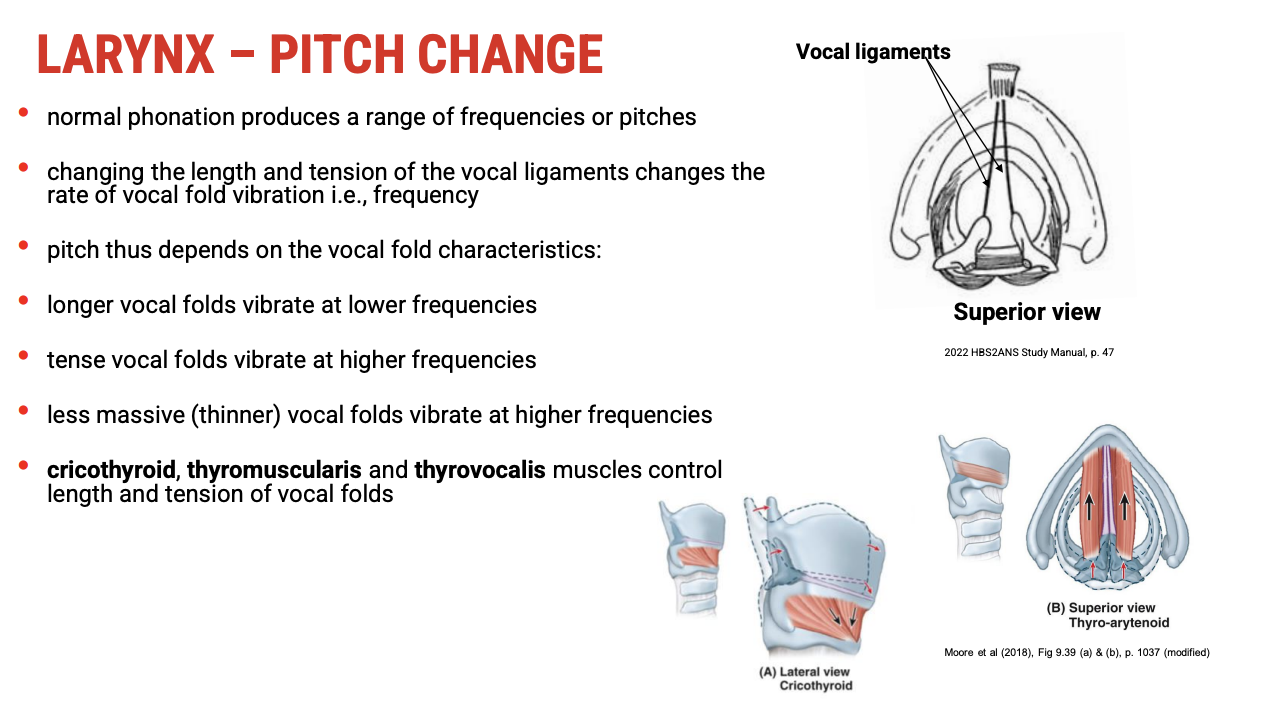
How Pitch Is Changed in the Larynx
🔑 Key Principles of Pitch Variation
Pitch depends on the length, tension, and thickness of the vocal folds — similar to strings on a musical instrument:
Longer vocal folds → lower frequency → lower pitch
Tense vocal folds → higher frequency → higher pitch
Thinner vocal folds → higher frequency → higher pitch
🦾 Muscles Controlling Length and Tension
Muscle | Role in Pitch Control |
Cricothyroid | Increases tension and lengthens vocal folds → raises pitch |
Thyrovocalis | Adjusts tension (fine control of vocal fold tension) |
Thyromuscularis | Can relax vocal folds, reducing tension → lowers pitch |
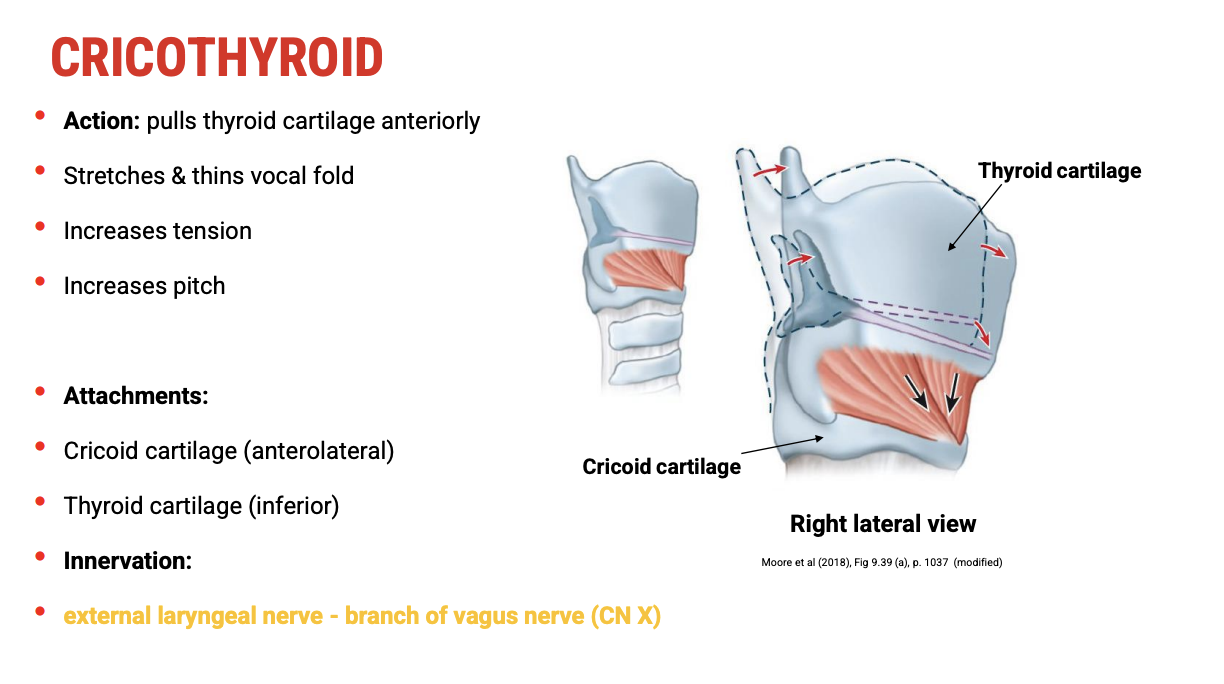
Cricothyroid Muscle
🦾 Action
Pulls the thyroid cartilage anteriorly and downward (rocks it forward on the cricoid cartilage).
This movement stretches and thins the vocal folds, increasing their tension.
Result: Raises pitch by increasing the frequency of vocal fold vibration.
🦴 Attachments
Origin: Anterolateral aspect of the cricoid cartilage
Insertion: Inferior border and inferior horn of the thyroid cartilage
⚡ Innervation
Innervated by the external branch of the superior laryngeal nerve (branch of the vagus nerve).
This is unique compared to other intrinsic laryngeal muscles, which are mostly innervated by the recurrent laryngeal nerve.
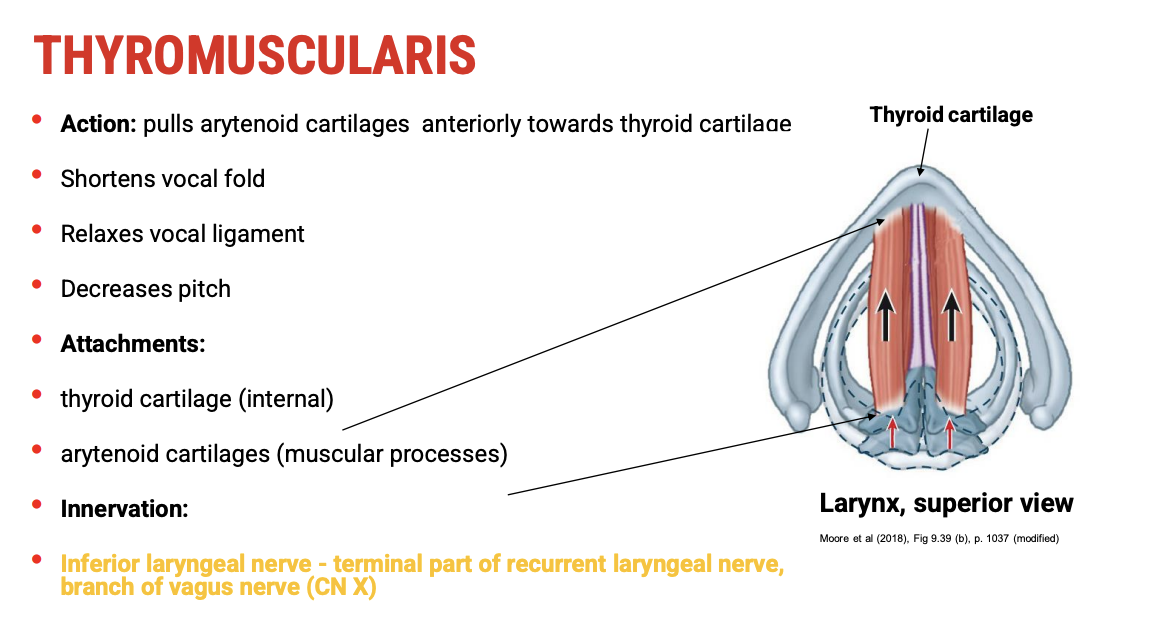
Thyromuscularis Muscle
🦾 Action
Pulls the arytenoid cartilages anteriorly toward the thyroid cartilage.
This shortens the vocal folds, relaxes the vocal ligament, and decreases pitch.
🦴 Attachments
Origin: Internal surface of the thyroid cartilage
Insertion: Muscular process of the arytenoid cartilage
⚡ Innervation
Innervated by the inferior laryngeal nerve (terminal branch of the recurrent laryngeal nerve, itself a branch of the vagus nerve).
This innervation is common to most intrinsic muscles of the larynx, except the cricothyroid.
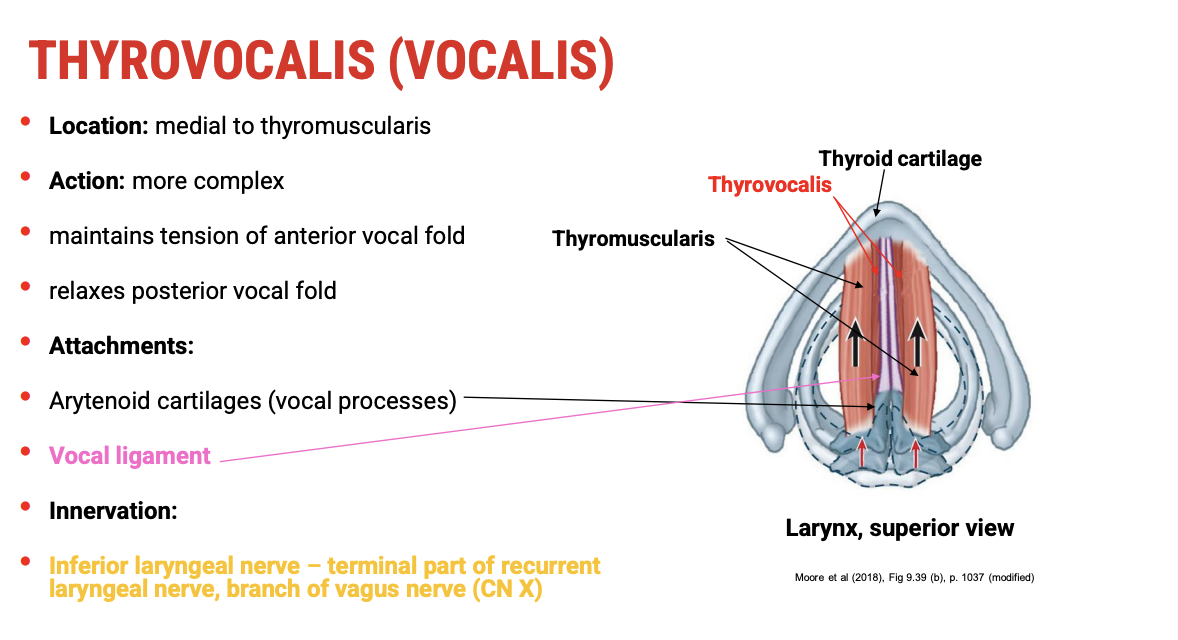
Thyrovocalis
🦾 Action
Located medial to the thyromuscularis within the vocal fold.
Has complex actions:
Maintains tension in the anterior part of the vocal fold (helps control fine tension for phonation).
Can relax the posterior part of the vocal fold, allowing subtle modulation of vocal fold stiffness.
🦴 Attachments
Origin: Vocal processes of the arytenoid cartilage
Insertion: Vocal ligament
⚡ Innervation
Innervated by the inferior laryngeal nerve (terminal part of the recurrent laryngeal nerve, branch of the vagus nerve), similar to the thyromuscularis
Intrinsic Muscles of the Larynx
Muscle | Action | Innervation |
Posterior cricoarytenoid | Abducts (opens) vocal folds (glottis) | Inferior laryngeal nerve (branch of recurrent laryngeal nerve, CN X) |
Lateral cricoarytenoid | Adducts (closes) vocal folds (interligamentous part) | Inferior laryngeal nerve (branch of recurrent laryngeal nerve, CN X) |
Transverse and oblique arytenoids | Adducts (closes) vocal folds (intercartilaginous part) | Inferior laryngeal nerve (branch of recurrent laryngeal nerve, CN X) |
🔹 Key Points
Posterior cricoarytenoid is the only abductor of the vocal folds.
Lateral cricoarytenoid and transverse/oblique arytenoids are adductors, with different focus areas of the vocal folds.
All three muscles are innervated by the inferior laryngeal nerve, which is the terminal branch of the recurrent laryngeal nerve, itself a branch of the vagus nerve (cranial nerve X).
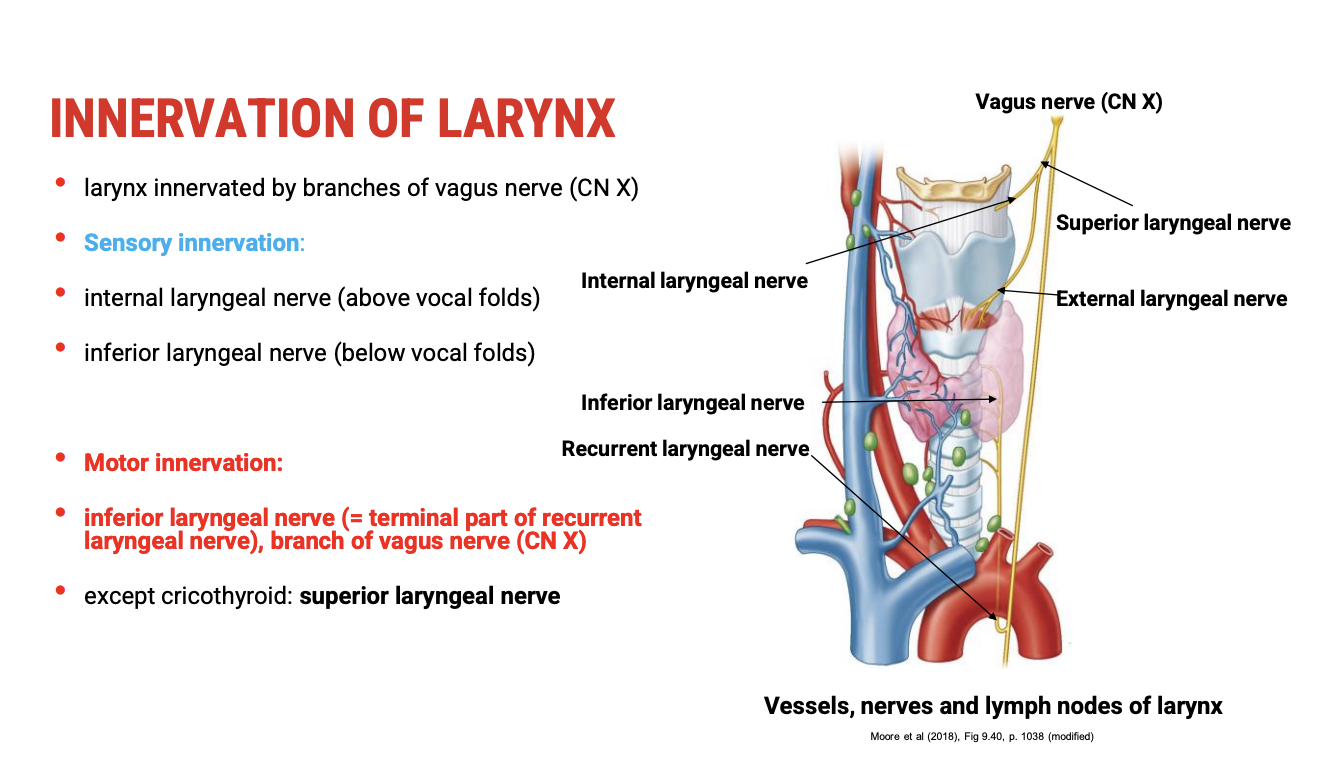
Pathway of the Vagus Nerve & Laryngeal Branches
Vagus Nerve (CN X) Pathway in the Neck:
Main trunk of the vagus nerve runs within the neurovascular bundle alongside the common carotid artery and internal jugular vein.
Branches relevant to the larynx:
Superior Laryngeal Nerve (SLN):
Internal branch:
Provides sensory innervation to the larynx above the vocal folds (supraglottic region).
External branch:
Provides motor innervation to the cricothyroid muscle, which controls tension and pitch.
Recurrent Laryngeal Nerve (RLN):
Branches off the vagus nerve inferiorly in the neck (right loops under right subclavian artery; left loops under the aortic arch).
Runs back upwards (recurrent) to enter the larynx from below.
Its terminal part is called the inferior laryngeal nerve.
Provides motor innervation to all intrinsic muscles of the larynx except the cricothyroid.
Also provides sensory innervation below the vocal folds (infraglottic region).
🔹 Summary
Nerve Branch | Function | Target Structures |
Internal branch of SLN | Sensory | Larynx above vocal folds |
External branch of SLN | Motor | Cricothyroid muscle |
Recurrent laryngeal nerve | Motor & sensory (via inferior laryngeal nerve) | All intrinsic muscles except cricothyroid; larynx below vocal folds |
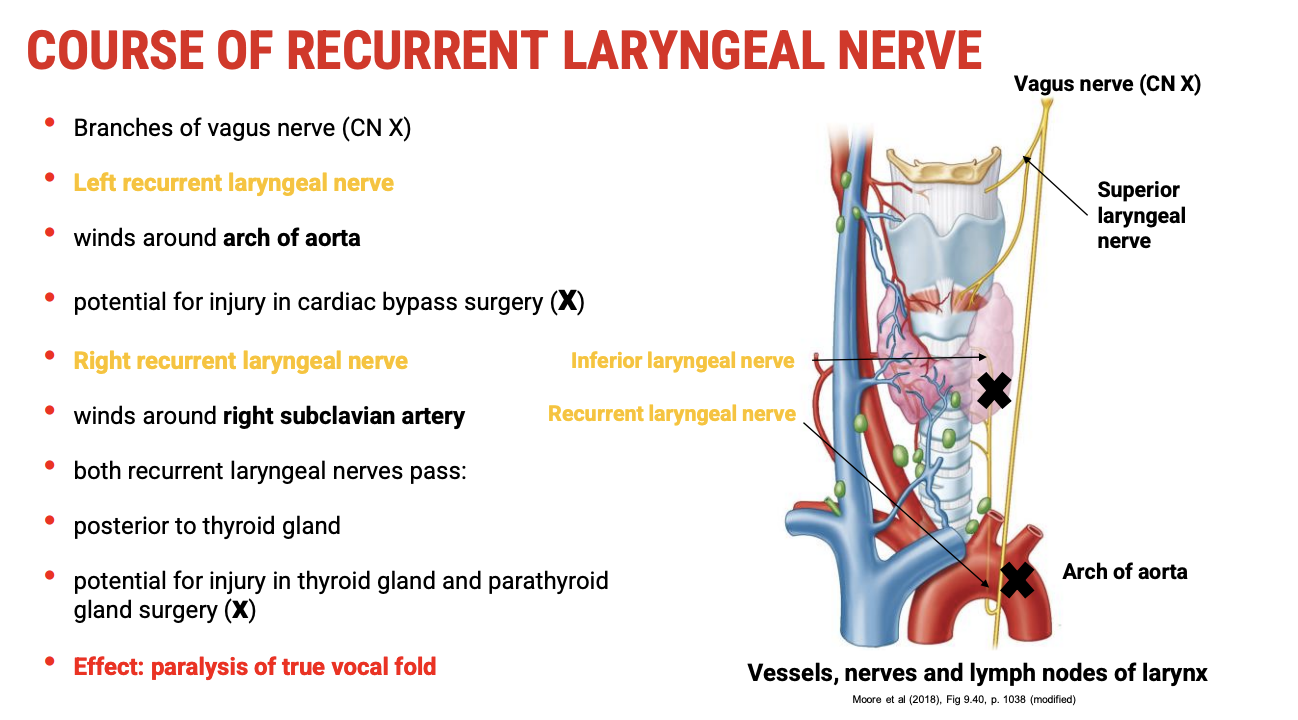
Course of the Recurrent Laryngeal Nerve (RLN) & Clinical Importance
Pathway Differences:
Left RLN:
Loops under the arch of the aorta.
Runs upward in the tracheoesophageal groove.
Because of its course around the aortic arch, it is at risk of injury during cardiac surgeries, especially cardiac bypass or aortic arch procedures.
Right RLN:
Loops under the right subclavian artery.
Travels upward similarly in the neck.
Common Course and Surgical Risk:
Both RLNs pass posterior to the thyroid gland.
They are at risk of injury during:
Thyroid surgery
Parathyroid surgery
Clinical Consequences of RLN Injury:
Paralysis of the true vocal fold on the affected side.
This can cause:
Hoarseness or breathy voice.
Possible aspiration risk due to incomplete glottic closure.
Breathing difficulties if bilateral injury occurs (rare but serious).
🔹 Summary
Side | Nerve Course | Surgical Risk Area | Potential Injury Consequence |
Left | Loops under aortic arch | Cardiac surgery; thyroid/parathyroid surgery | Ipsilateral vocal fold paralysis |
Right | Loops under right subclavian artery | Thyroid/parathyroid surgery | Ipsilateral vocal fold paralysis |
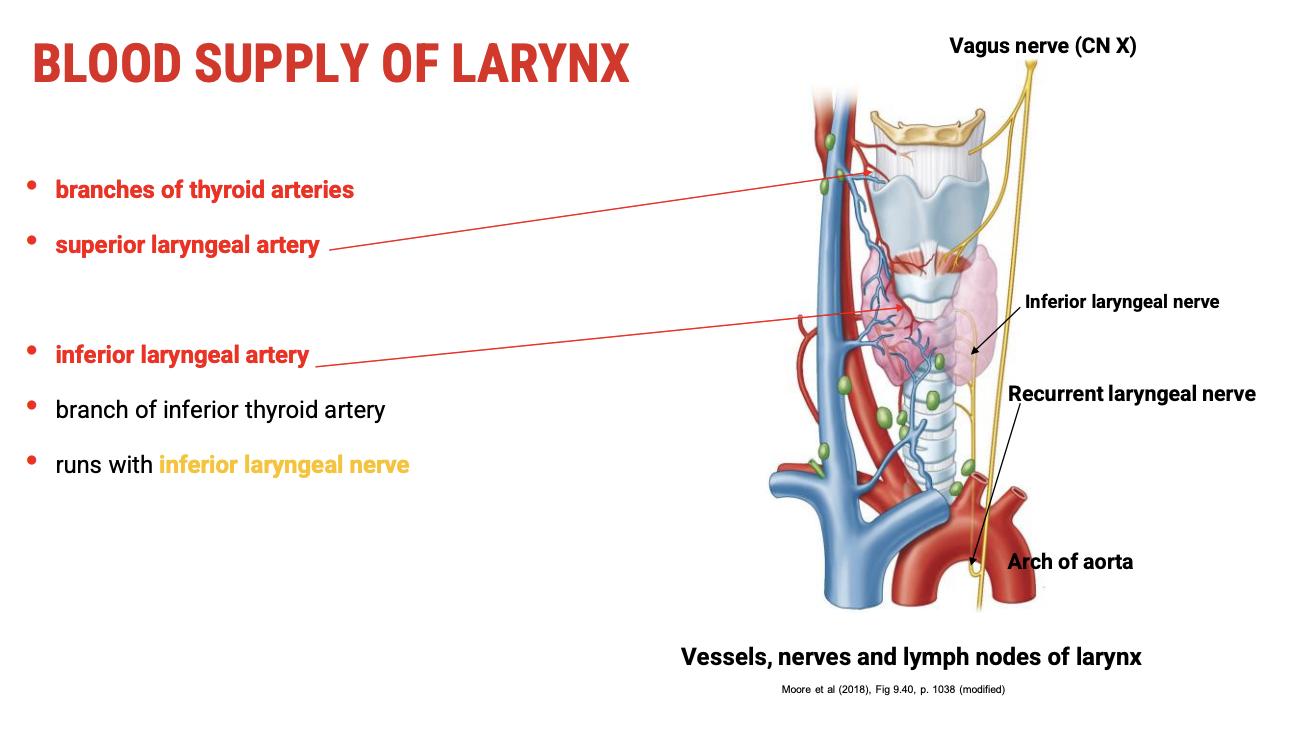
Blood Supply of the Larynx
Main Arterial Sources:
Superior laryngeal artery
Branches from the superior thyroid artery (which itself branches from the external carotid artery).
Supplies the upper part of the larynx including the supraglottic region.
Inferior laryngeal artery
Branches from the inferior thyroid artery.
The inferior thyroid artery runs with the inferior laryngeal nerve.
Supplies the infraglottic region and lower parts of the larynx.
Additional Notes:
These arteries are closely associated with thyroid vasculature.
Rich blood supply ensures good oxygenation for the vocal folds and laryngeal muscles critical for voice production and airway protection