10/2 Host-Microbe Interactions during Immune Development & Homeostasis
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
Learning Objectives
Appreciate the importance of the microbiota in human development and homeostasis
Describe how the microbiome evolves over time and which intrinsic and extrinsic factors shape it
Outline the mechanisms by which humans and the microbiome cooperate to maintain healthy mucosal barriers
Explain general mechanisms by which the microbiome contributes to homeostasis and disease
List some disorders that can result from microbial dysbiosis
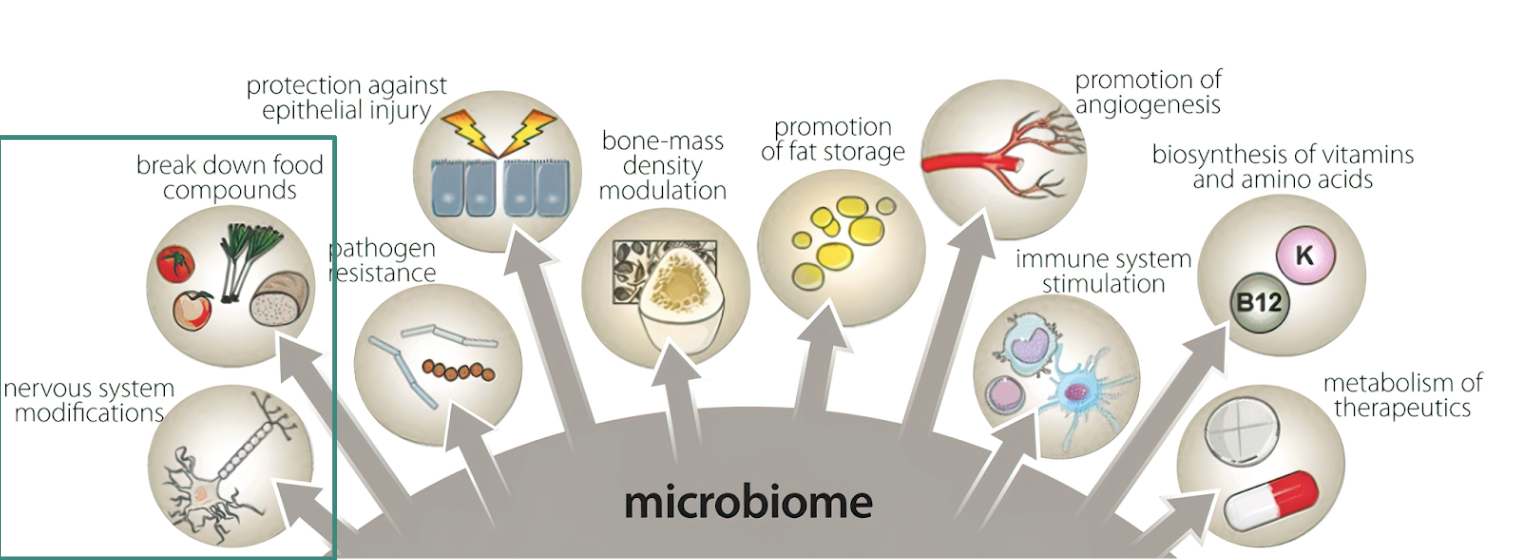
The human body is comprised of ?
a > 1:1 ratio of human cells and microbial cells
The microbiome …
is in constant communication with mucosal epithelial cells, immune cells, and the peripheral nervous system. these cells can then direct systemic changes in response to microbes
produces factors (NTs, hormones, vitamins, dietary metabolites, etc.) that directly impact the function of our organ systems
is required for human health and development
can be considered its own human organ system
What could happen without exposure to a microbiome?
variety of problems socially, internally, and physically
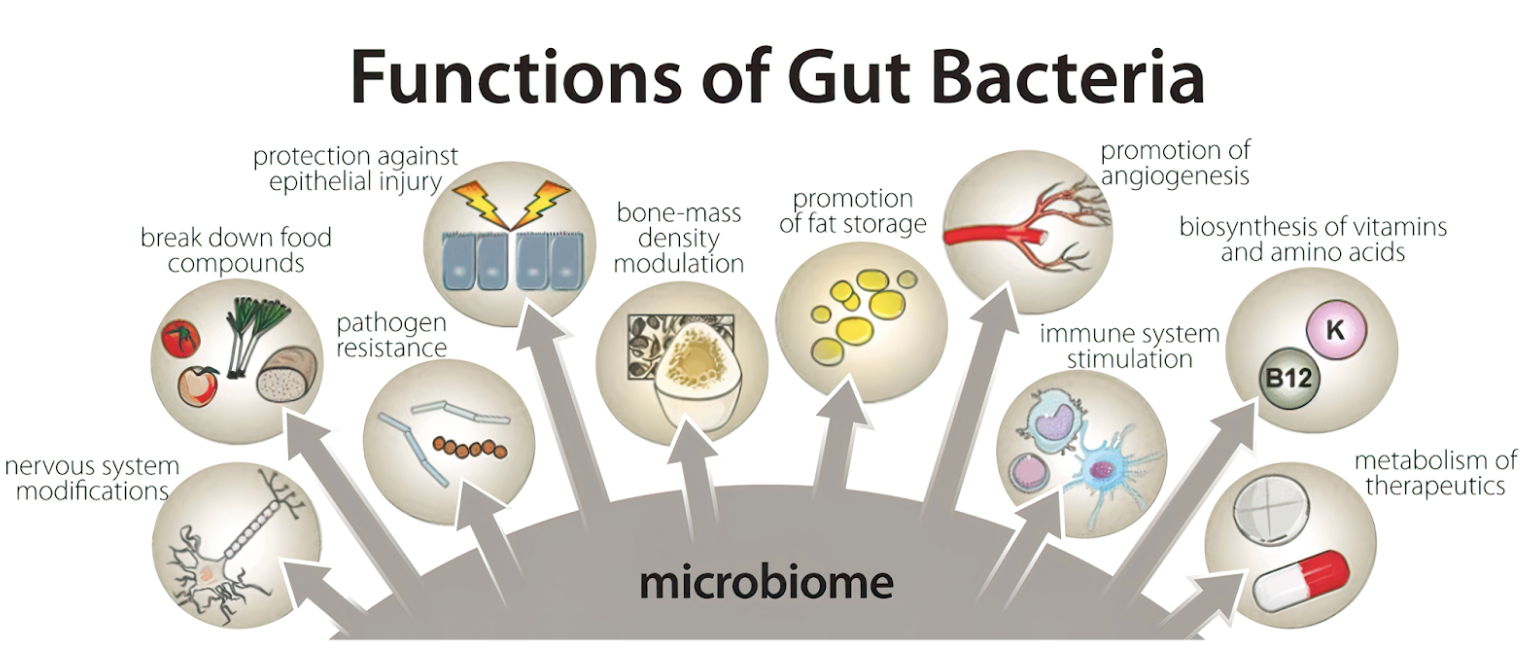
What are some functions of gut bacteria?
tell our NS what to do
maintain the epithelial barrier
promote blood vessel growth
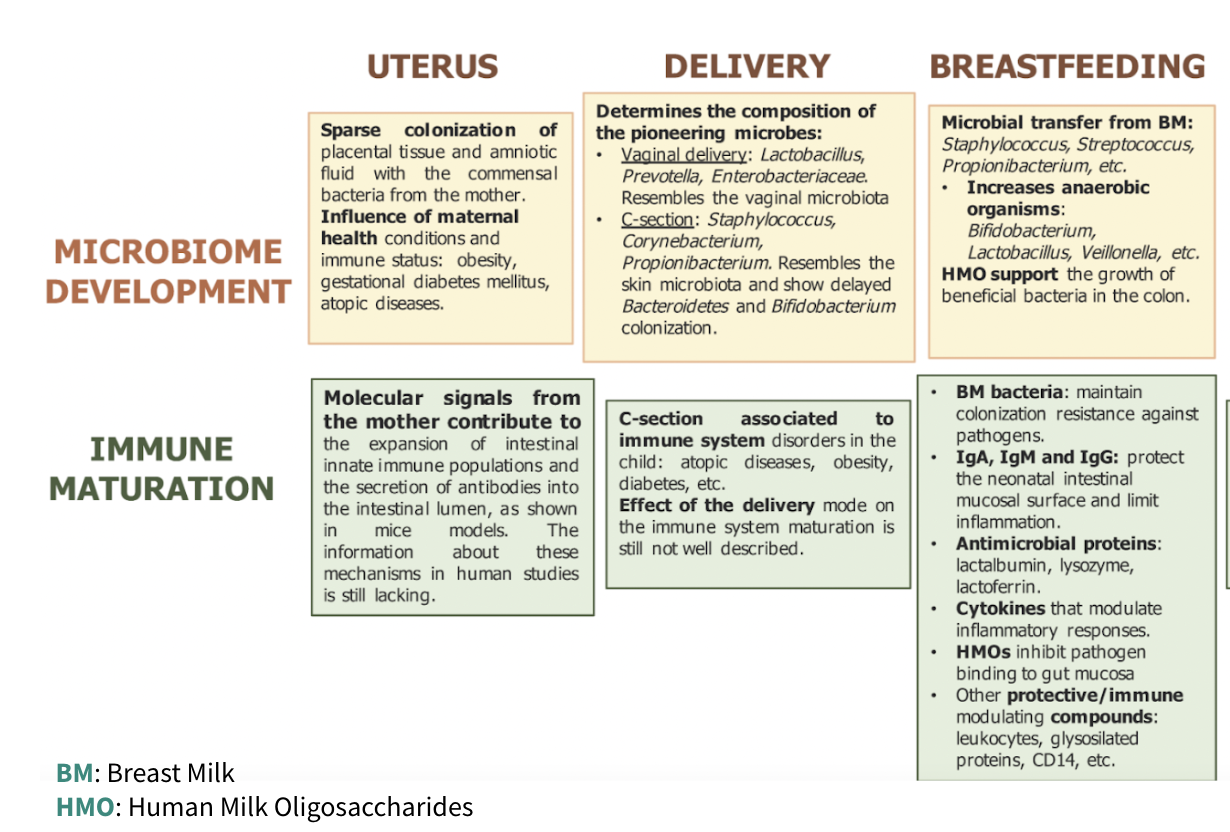
Where do we inherit our microbiome? When is our microbiome formed?
from our parents
microbiome is formed when we are born and is exposed to the outside world
in the womb, it is a sterile environment
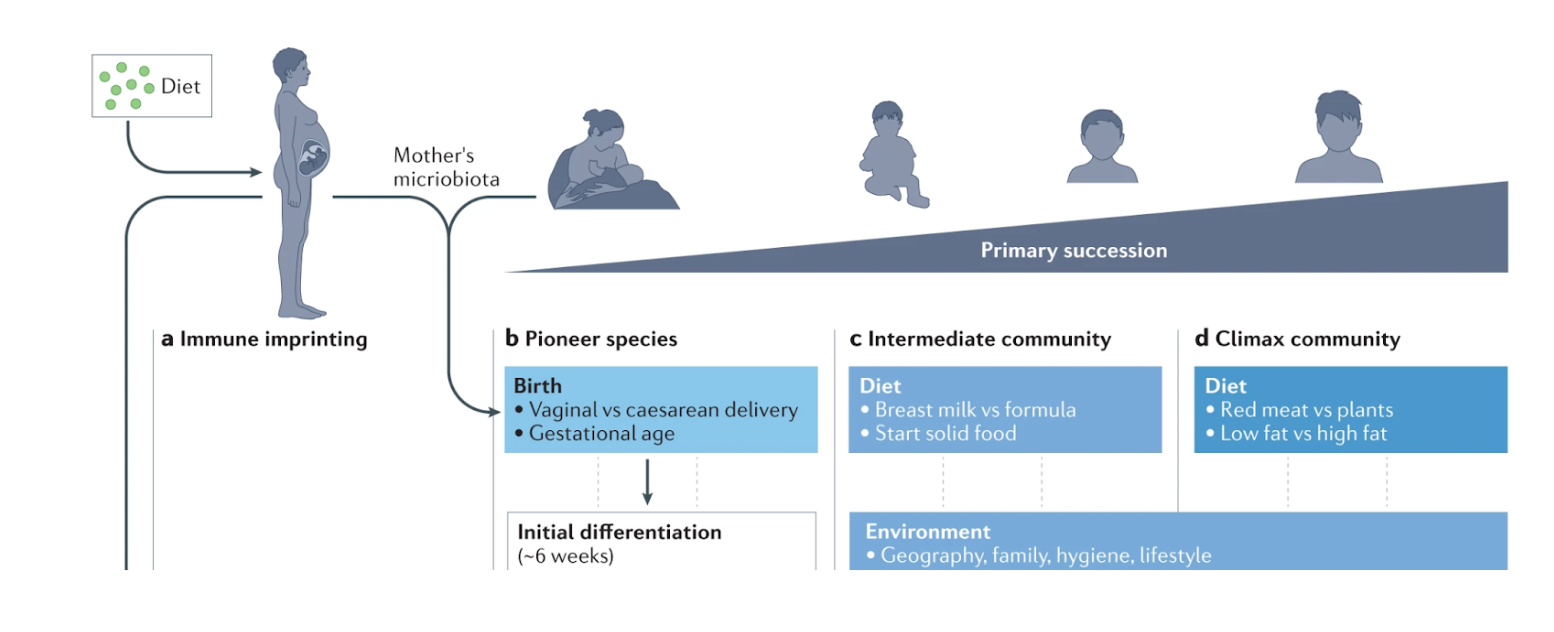
How can different birth deliveries result in different microbiomes?
from a vaginal birth: the microbiome is exposed to vaginal secretions
from a C-section birth: the microbiome is exposed to only the parent’s skin
this can lead to allergies, asthma, etc.
the solution is to try and swab newborn with vaginal secretion to try and mimic a vaginal birth’s benefits
What is important that an environment should have to promote microbiome development?
good for the baby/child to be exposed to more people outside of the home (such as at a daycare) because our body favors bacterial diversity
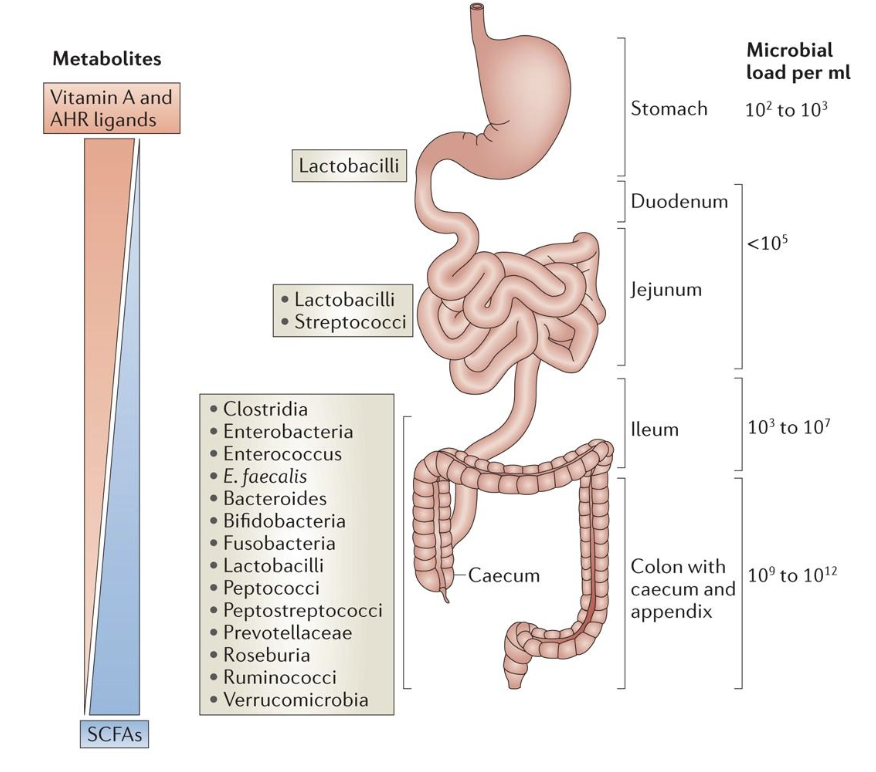
Mucosal tissues have what to support what?
mucosal tissues have distinct microbiomes specialized to supporting that tissue
for example, the lungs and guts are exposed to different things. dust/airborne toxins are more exposed to the lungs than the guts, so we want a microbiome in the lungs that is more able to combat dust
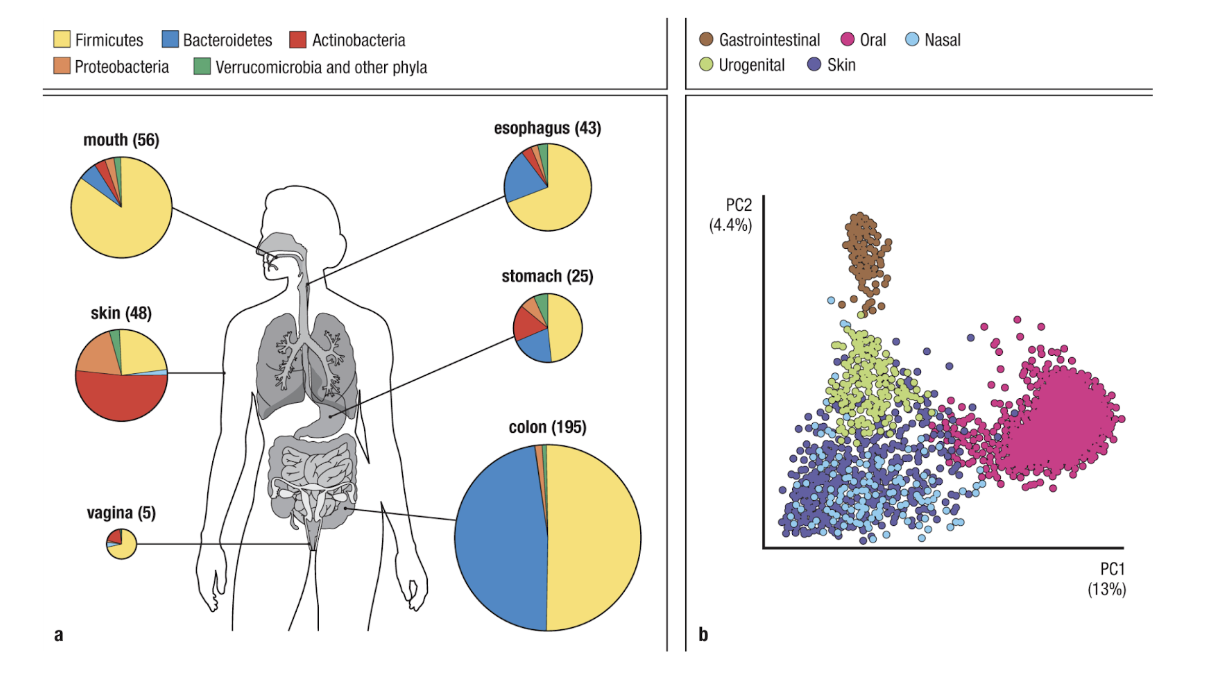
While microbes at all tissues play a key role in maintaining homeostasis, what are essential for what?
while microbes at all tissues play a key role in maintaining homeostasis, gastrointestinal microbes are essential for development and maintaining systemic homeostasis
What is regional specialization?
different microbiomes in different parts of the organ (such as the GI tract)
pH differences
access to nutrients (mucus, undigested fiber, etc.)
majority of species are obligate anaerobes (organisms that are unable to survive in presence of oxygen)
antigen content, gut-associated lymphoid tissue (GALT), and leukocyte populations vary throughout the gut
What are the different parts in maintaining the barrier in the gut?
mucus: first line of defense
antimicrobial peptides: maintain barrier between epithelium and gut lumen
macrophages: phagocytose invading commensals or pathogens
DC: capture mucosal antigens, traffic to mesenteric lymph nodes & Peyer’s patches, induce commensal-specific T & B cell responses
lymphocytes: traffic to gut lamina propria & Peyer’s patches promote B cell IgA class switching
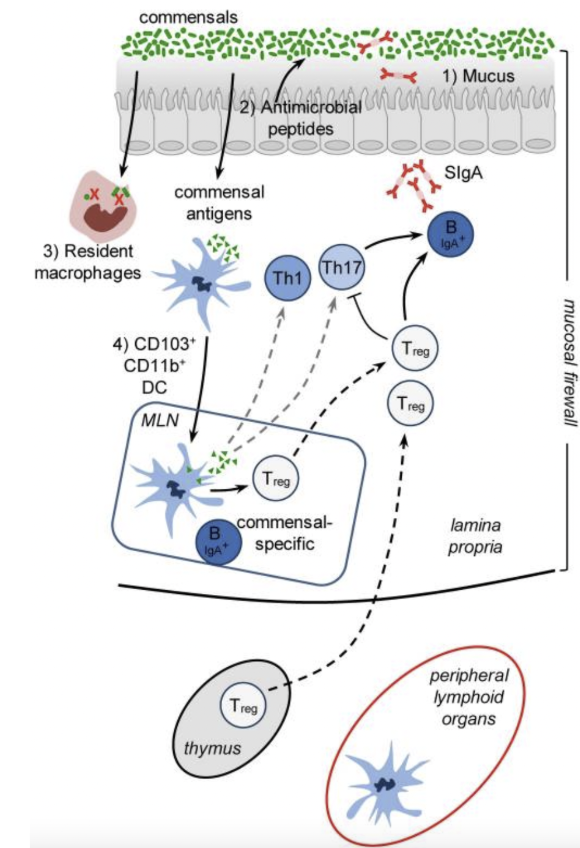
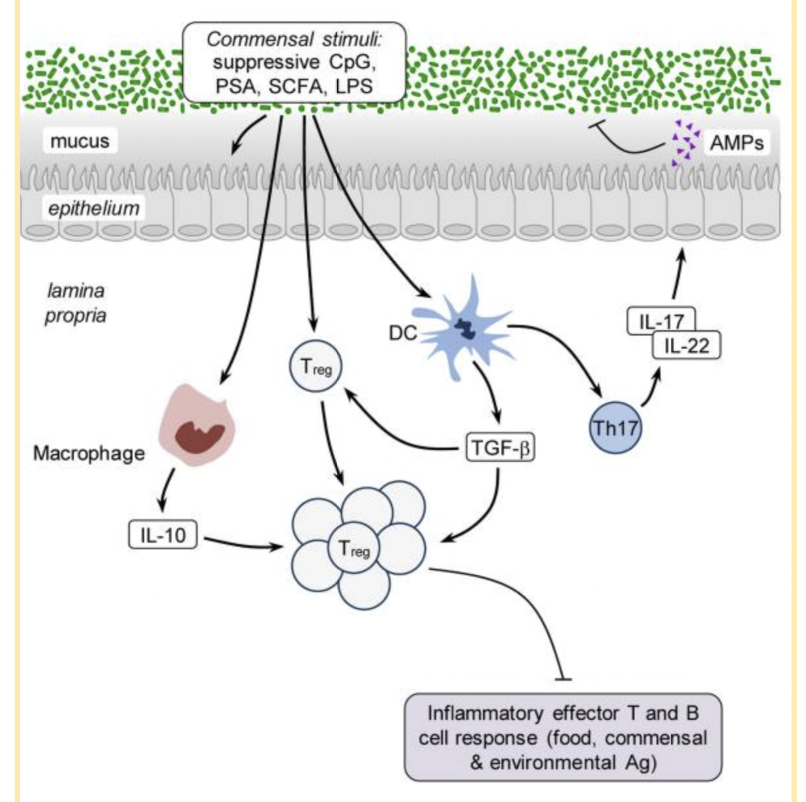
What and how do microbes regulate homeostatic barrier? What is commensal stimuli?
number of different commensal products participate in barrier regulation
delicate balance between regulatory (Treg) and inflammatory (Th17) tissue environment supports healthy barrier function
commensal stimuli are healthy microbes telling the immune cells to upregulate in order to maintain the barrier
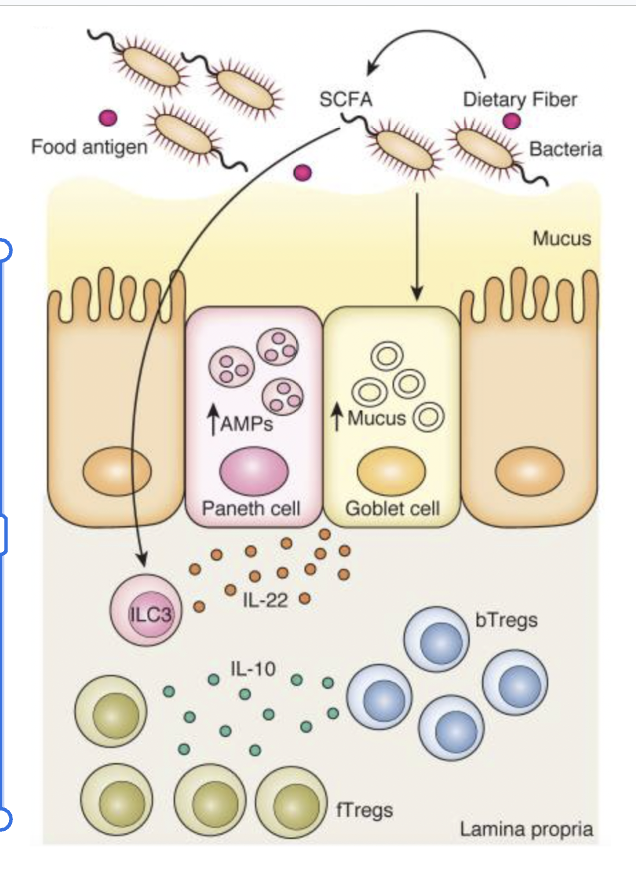
What further helps maintain homeostatic barrier regulation by microbes through fiber? Why is this beneficial for us?
our body is unable to digest fiber, so our healthy microbiota digests fiber into short-chain fatty acids (SCFAs)
SCFAs stimulate paneth cells which increases antimicrobial peptides, and also stimulate goblet cells which increases mucus secretion
these all help maintain the barrier
SCFAs contribute to dendritic cell tolerogenic polarization where DCs induce Treg differentiation, and Tregs produce IL-10 (this makes our environment more immunosuppressive)
IL-10 maintains immune tolerance
induction of a tolerogenic (anti-inflammatory) environment by microbes also protects us from attacking our food
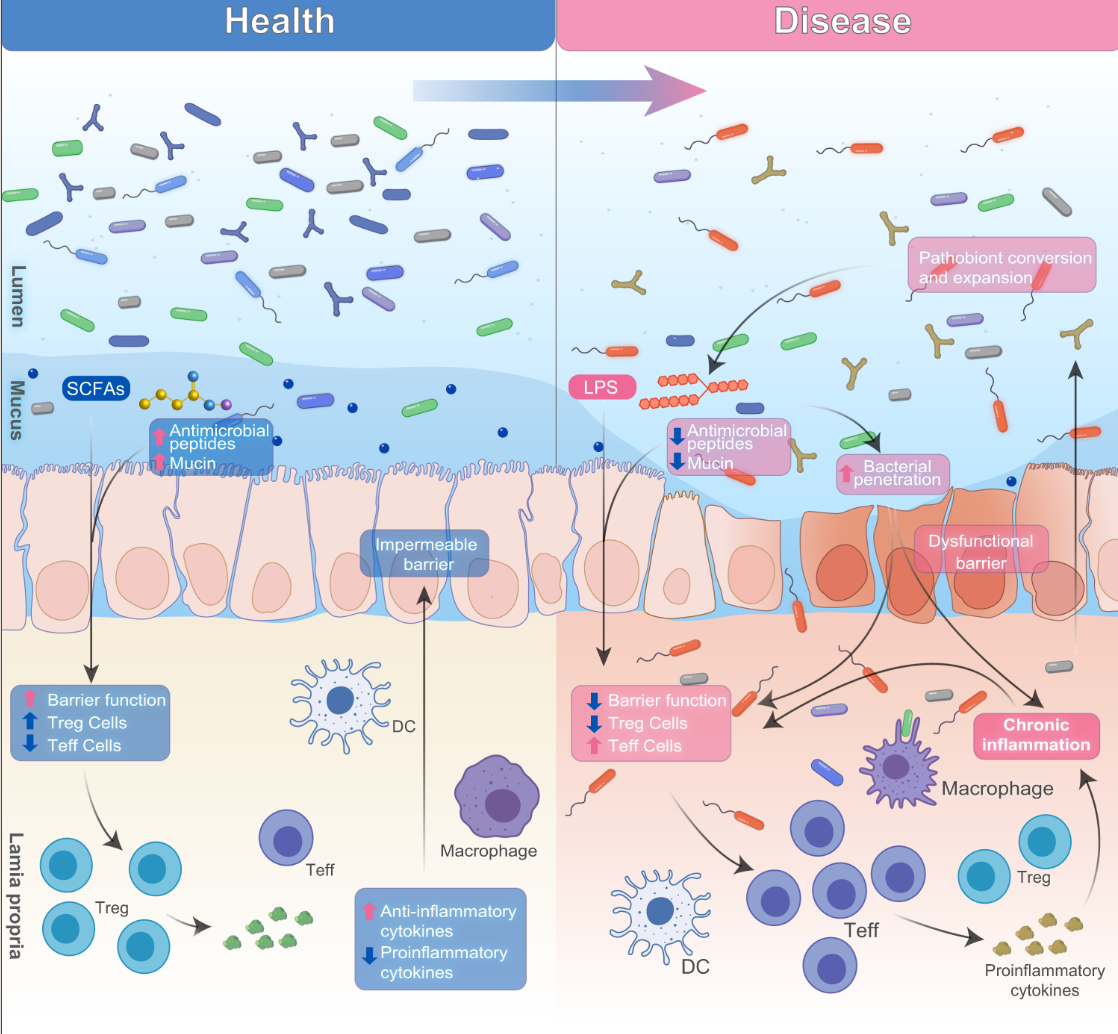
What can lead to a leaky gut?
microbial homeostasis is key for systemic homeostasis, and microbial dysbiosis (bad changes in the microbome community) can be a precursor to a number of health conditions
microbial dysbiosis → impaired epithelial barrier → translocation of food particles, toxins, microbes, etc. into lamina propria (gut) → immune activation → pathology
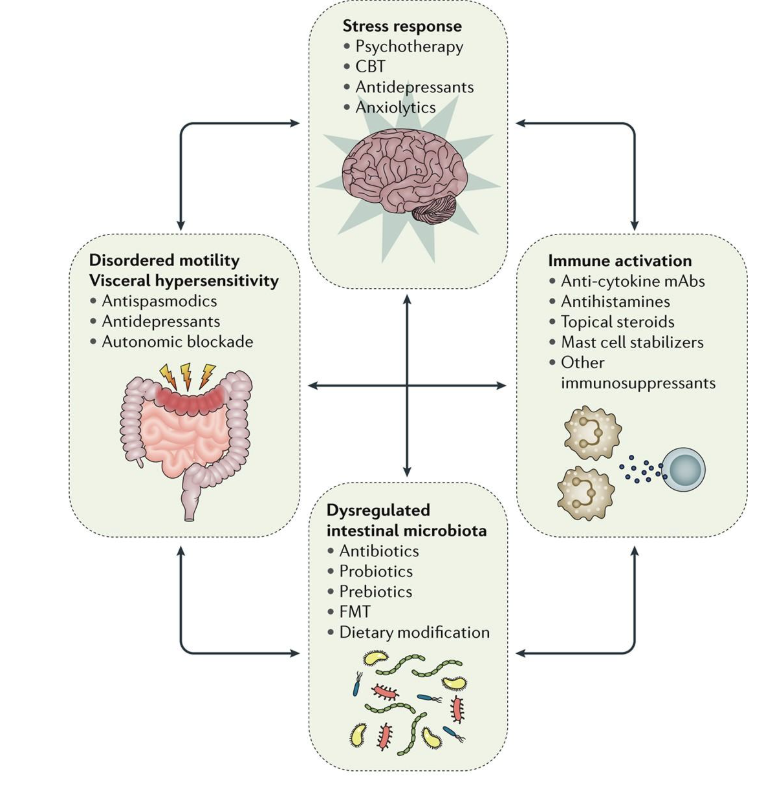
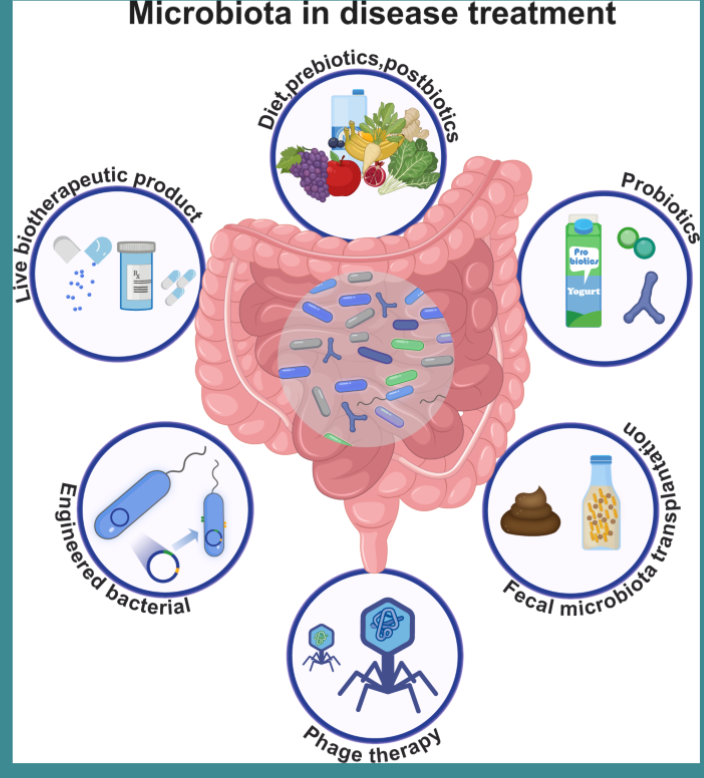
Treating gut dysbiosis may prove an effective therapy for a number of pathologies. What are some treatments?
diet, prebiotics, & postbiotics
help maintain healthy microbes
probiotics, fecal transplant (isolate microbes from one’s healthy feces and put it into pill form), engineered bacteria, & biotherapeutics
supplement with healthy microbes
Microbial products also?
microbial products also directly impact other organ systems independently of their immunomodulatory functions
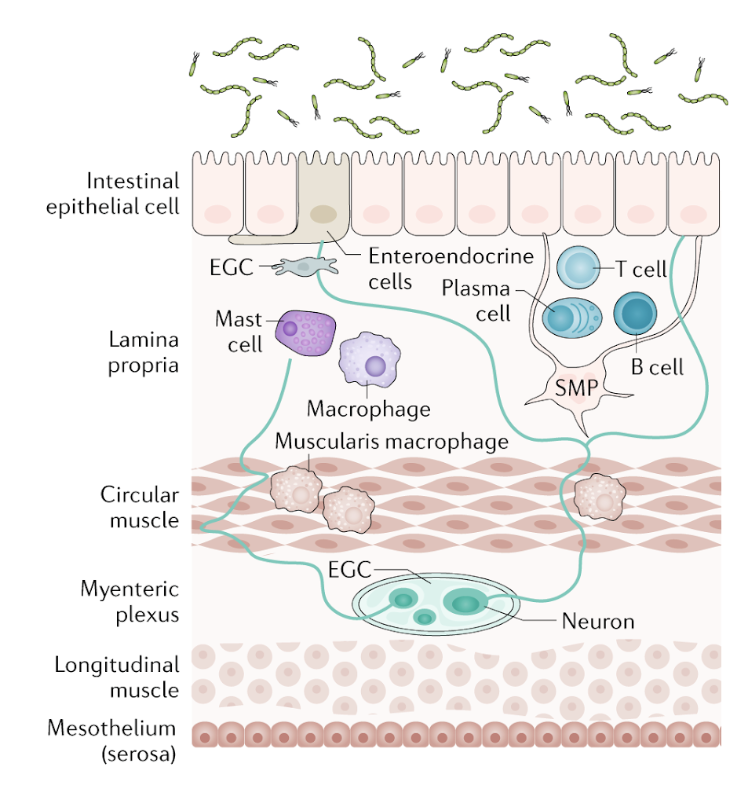
What is the enteric nervous system?
second brain that still communicates with the PNS
enteric glial cells (EGC) regulate the epithelial barrier and neuroendocrine communication
submucosal plexus (SMP) regulates enterocyte secretion and absorption and is in close proximity to intestinal microbes
macrophages of the muscularis are in close proximity with the myenteric plexus
How does microbial-mediated NT release work?
microbiota produces NT precursors and/or catalyze synthesis of NT through dietary metabolism
some signal on enteroendocrine cells to cause NT synthesis
NTs enter bloodstream and cross blood-brain barrier (BBB)
NT precursors enter bloodstrem, cross BBB, and are converted to NTs
Neuropod cells: intestinal epithelial cells that synthesize NTs that signal via vagus nerve
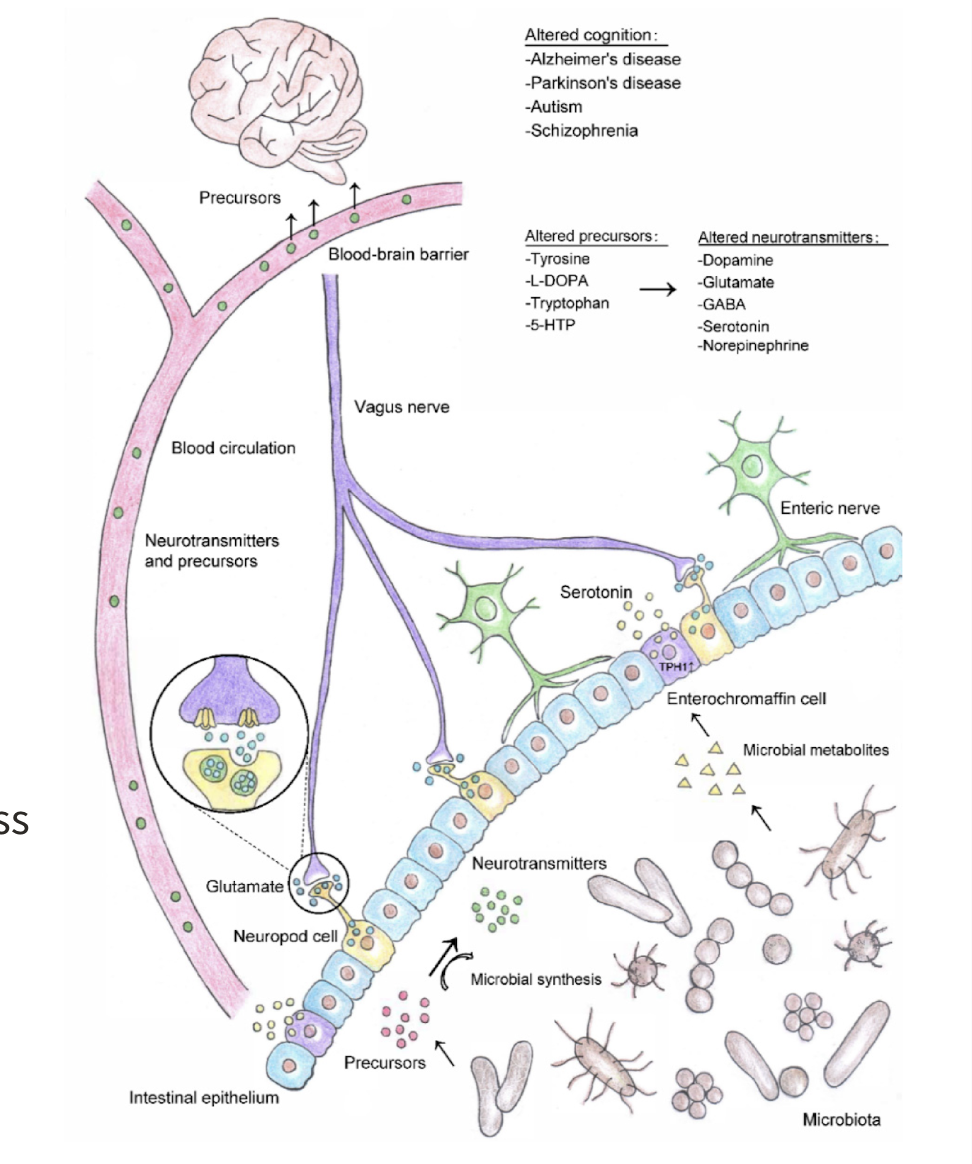
Microbial metabolites also affect where?
CNS Function
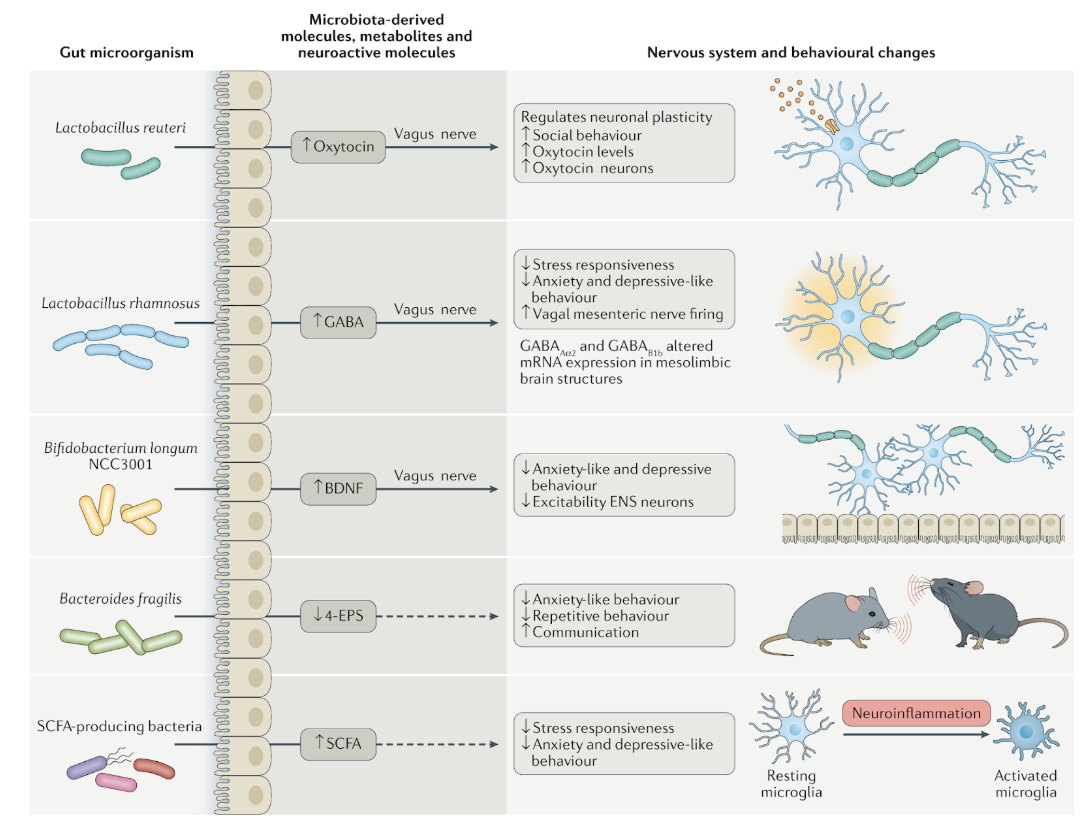
What is the microbiota-brain-immune axis?
bidirectional communication via autonomic nervous system (ENS & vagus nerve), neuroendocrine system, hypothalamic-pituitary-adrenal (HPA) axis, microbiota, and immune system
microbiota produces immunomodulatory & neuroactive metabolites (including NTs) and impact gut permeability (passage of nutrients & signaling molecules)
The microbiome direct changes in what, which affects what?
the microbiome directs changes in the immune system, which affects CNS function
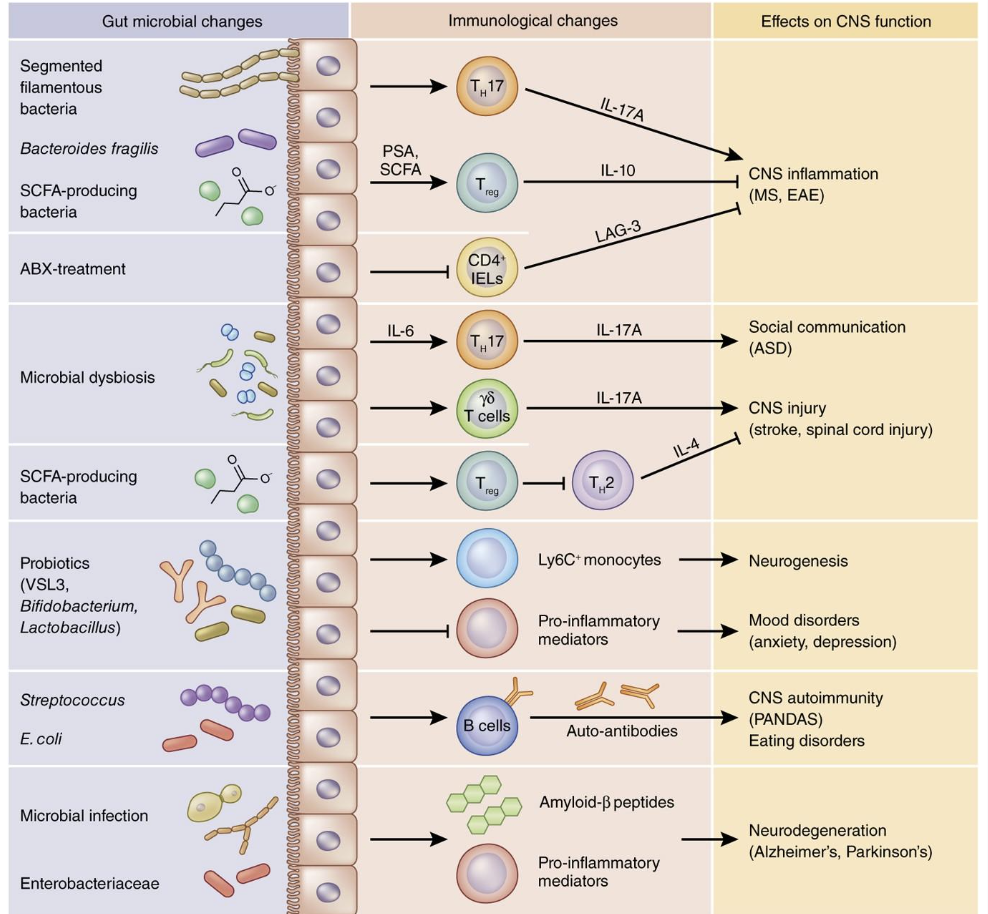
What can gut dysbiosis lead to? So what do we need to target?
neurological diseases
targeting the microbiome may prove helpful in treating neurological disorders