Respiratory Papers
1/156
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
157 Terms
Raidal et al, 2021
Bi-Level Positive Airway Pressure for Non-invasive Respiratory Support of Foals
Objective: To investigate the use of a commercial bi-level positive airway pressure (BiPAP) ventilator, designed for home care of people with obstructive respiratory conditions, for respiratory support of healthy foals with pharmacologically induced respiratory insufficiency
Results:
Administration of supplementary oxygen alone or with BiPAP was associated with significantly increased PaO2 in comparison to results at all other sampling times and results following BiPAP were significantly greater than after O2 administration
BiPAP was associated with significantly lower RR and significantly longer inspiratory and expiratory times at T2 than observed following O2 administration at this time
FiO2 was higher during BiPAP than during O2 administration to foals
Gas exchange and mechanics of breathing (increased tidal volume, decreased respiratory rate, and increased peak inspiratory flow) were improved during BiPAP relative to administration of supplementary oxygen alone or prior studies using continuous positive airway pressure, but modest hypercapnia was observed
Hypercapnia may be due to reduced respiratory drive, increased metabolic rate, hypoventilation due to sedation, or effects of equipment dead space
In this study, mask administration of O2 was likely associated with CO2 retention
Use of lower expiratory pressures did not prevent hypercapnia
Results suggest that monitoring of alveolar ventilation, pressure-volume curves, and PEEPi might be important for effective NIV of foals and to better characterize the response of foals to respiratory support
Conclusion: BiPAP was an effective respiratory support strategy for healthy foals with pharmacologically induced respiratory insufficiency. BiPAP was associated with increased PaO2, more efficient gas exchange and changes in respiratory mechanics including increased tidal volume, decreased respiratory rate, and increased peak inspiratory flow. The technique preserved minute ventilation in the face of reduced ventilation observed at other times associated with sedation and recumbency, but was associated with modest increase in PaCO2. Clinical observations, pulse oximetry and monitoring of expired carbon dioxide was of limited benefit in identification of foals responding inappropriately to BiPAP and improved methods to assess and monitor respiratory function are required in foals
Floyd et al, 2021
Nasal high flow oxygen therapy in hospitalized neonatal foals
Objective: To describe the use of high flow oxygen therapy (HFOT) in hospitalized neonatal foals
Results:
14 foals
Target starting respiratory gas flow rate of 40 L/min
Could not be achieved with 20 FR chest tubes initially used, limited to 25-35 L/min
Changed to 24 FR chest tubes to achieve a maximum flow rate of 60 L/min
Ensured chest tubes did not obstruct more than 50% of the nasal diameter to prevent obstruction to expiratory flow
Oxygen flow rate and oxygen concentration in the respiratory gas mix were based on arterial blood gas analysis
Specific FiO2 was not targeted
Median duration of use was 43 hours (range 2-93 hours)
Median flow rate of 0.7 L/kg/min (range 0.42-1.67)
10/14 foals survived to discharge
2 foals died
2 foals were euthanized
Treatment was discontinued in two foals due to excessive activity
Mechanical ventilation was used in two foals following the use of HFOT
No significant complications associated with the technique recorded
Optiflow system used
HFOT did not significantly improve oxygenation but not all foals were hypoxemic at the initiation of HFOT and the majority had received traditional oxygen therapy prior to switching to HFOT
Conclusion: This study provides preliminary information about the clinical use of HFOT in neonatal foals. This technique was well tolerated and no significant adverse effects were noted. Further study is required to evaluate efficacy and exact indications. HFOT shows promise as an intermediate means of providing respiratory support which may allow improved care for a wider group of neonatal foals
Harvey et al, 2021
Opsonization but not pretreatment of equine macrophages with hyperimmune plasma nonspecifically enhances phagocytosis and intracellular killing of Rhodococcus equi
Objective: To compare the effects of hyperimmune plasma (HIP) and normal plasma (NP) on phagocytosis and intracellular survival of virulent R. equi either as a pretreatment of alveolar macrophages (in the absence of opsonization) or when used as opsonins
Results:
Concentrations of R. equi at T0 were significantly lower for AMs treated with HIP than those treated with media only but concentrations of R. equi for HIP did not differ significantly from NP
Opsonization with either HIP or NP increased phagoyctosis by AMs and decreased intracellular survival or organisms in AMs
Pretreating AMs with either HIP or NP without opsonizing R. equi had no effects on phagocytosis or intracellular replications
Conclusion: Opsonizing R. equi with either NP or HIP decreases intracellular survival of organisms in AMs, but the effect does not appear to be enhanced by using HIP. Mechanisms other than effects on AMs must explain any clinical benefits of using HIP over NP to decrease the incidence of R. equi pneumonia in foals
Berman et al, 2021
Comparison of thoracic ultrasonography and thoracic radiography to detect active infectious bronchopneumonia in hospitalized dairy calves
Objective: To estimate performances of thoracic ultrasonography (TUS) and thoracic radiography (TR) to detect active infectious bronchopneumonia (BP) in hospitalized dairy calves and to determine the best strategy for using these tests based on a panel diagnosis method (PDM). Performances of TUS and TR were hypothesized to be equivalent
Results:
Interexpert agreement was moderate at 0.58
Diagnosis of active BP was consensual between 2 experts for 80% of the study sample
Lung consolidation on TUS and presence of an alveolar pattern on TR were the most prevalent thoracic lesions and were both detected in calves with and without active BP
TUS and TR failed to identify thoracic lesions in 3 and 2 calves with active BP, respectively
Out of 19 calves with active BP, TUS and TR were positive for 16 and 17 calves, respectively
The Se and Sp of TUS were 0.84 and 0.74, respectively
The Se and Sp or TR were 0.89 and 0.58, respectively
No significant difference was found in the Se and Sp of TUS and TR when analyzed alone, in series or in parallel
Conclusion: Thoracic ultrasonography or TR alone equally detected active BP in hospitalized dairy calves. Series or parallel analysis provided no additional benefits. Its ease of use and widespread accessibility support using TUS as a first-line test to detect active BP in hospitalized dairy calves
Sacks et al, 2021
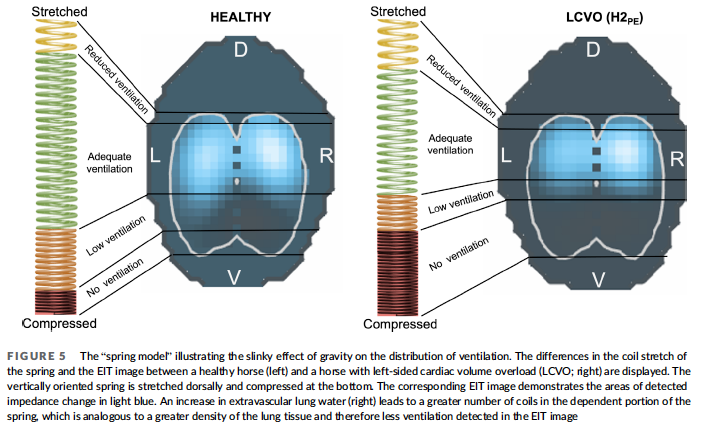
Electrical impedance tomography to measure lung ventilation distribution in healthy horses and horses with left-sided cardiac volume overload
Objective: To describe and compare electrical impedance tomography (EIT) variables in horses with naturally occurring compensated and decompensated left-sided cardiac volume overload (LCVO) and compare them to a healthy cohort
Results:
Compared to the healthy horses, the LCVO cohort had significantly less ventilated left (VAL) lung area, more ventilated right (VAR) lung area, smaller avg-max VdeltaZLLine and VdeltaZLLine
Ventilation was observed to be estimated lower in the ventral and central-ventral lung regions and higher in the most dorsal lung regions in the horses with clinical signs of alveolar PE than in the horses with compensated LCVO
Observation of EIT alterations were reflected by clinical signs in horses with decompensated LCVO and after administration of furosemide
Observation that the left lung was more affected by LCVO was unexpected
in horses reversal flow might favor venous congestion and edema location in the left lung
Also may be due to the position of the heart, sitting cranio-ventrally and slightly left-sided within the thorax
Enlarged left atrium of horses with LCVO might compress the left mainstem bronchus, restricting the airway lumen and redirecting the gas toward the right lung
Less likely due to lack of inhomogeneity in inflation of the right and left lung units
When assessing only the horses with decompensated LCVO, changes in accordance with the proposed slinky effect were observed
Less ventilation was detected in the ventral and central-ventral ROIs and more in the most dorsal ROI when compared to horses with compensated LCVO
Conclusion: EIT measurements of ventilation distribution showed less ventilation in the left lung of horses with LCVO and might be useful as an objective assessment of the ventilation effects of cardiogenic pulmonary disease in horses
Cohen et al, 2022
Association of pneumonia with concentrations of virulent Rhodococcus equi in fecal swabs of foals before and after intrabronchial infection with virulent R. equi
Hypothesis: Fecal concentration of virulent R. equi before IB infection with R. equi is positively associated with protection from pneumonia in foals
Results:
Fecal concentrations of virulent R. equi (vapA) before IB infection were significantly lower in control foals that developed pneumonia than in healthy control foals or those gavaged with live virulent R. equi (LVRE)
Two weeks after infection, fecal concentrations increased for pneumonic foals
The foals that were gavaged with R. equi had a marked decrease in their fecal concentrations of virulent R. equi after IB infection
Don’t know if this was from enhanced clearance of R. equi from both the respiratory and intestinal tracts
Conclusion: Greater natural ingestion of LVRE might contribute to protection against pneumonia among foals
Cohen et al, 2022
Fecal concentration of Rhodococcus equi determined by quantitative polymerase chain reaction of rectal swab samples to differentiate foals with pneumonia from healthy foals
Objective: To evaluate the accuracy of qPCR of rectal swab samples to differentiate foals with pneumonia from healthy foals of similar age from the same environment
Results:
The area under the ROC curve for qPCR of fecal swabs was 83.7%
At a threshold of 14,883 copies of vapA per 100 ng fecal DNA, specificity of the assay was 83.0% and sensitivity was 79.5%
Conclusion: Although fecal concentrations of virulent R. equi are significantly higher in pneumonic foals than healthy foals of similar age in the same environment, qPCR of rectal swabs as reported here lacks adequate diagnostic accuracy for clinical use
Migliorisi et al, 2022
Hyponatremia in horses with septic pneumopathy
Objective: Describe admission plasma sodium concentration ([Na]) in horses with septic pneumopathy and evaluate any association of plasma [Na] with markers of systemic inflammtion
Results:
20/35 (57%) horses had hyponatremia
14 had mild hyponatreima, 4 had moderate hyponatremia, and 2 had severe hyponatremia
When accounting for horses without pleural effusion, hyponatremia was present in 44% of cases
Loss of water into a third-space results in ADH release, water retention, and dilutional hyponatremia
A higher proportion of horses with SIRS had hyponatremia
Hyponatremia in SIRS associated with altered expression of ion channels in nephrons under the influence of pro-inflammatory cytokines as well as nonosmotic ADH release, secondary to the action of pro-inflammatory mediators
Hyponatremic patients had higher mean plasma fibrionogen concentration and higher rectal temperature than normonatremic horses
Fever and endogenous pyrogens are thought to induce nonosmotic release of ADH as a protective mechanism to retain more water and counteract insensible losses caused by the increased body temperature
Fibrinogen synthesized during inflammation after stimulation by IL-6 which has been linked to development of hyponatremia because of influence on ADH release
Negative correlations were found between plasma [Na] and fibrinogen concentrations and between plasma [Na] and rectal temperature
Presence of absence of pleural effusion did not influence severity of hyponatremia
No difference was found in white blood cell or neutrophil counts between hyponatremic and normonatremic horses
No association between prior usage of NSAIDs and frequency of hyponatremia at admission
No association between albumin and sodium concentration
Mean duration of hospitalization was longer in hyponatremic horses
Most common aerobic isolates were Actinobacillus spp (31%), Streptococcus equi ssp zooepidemicus (31%), alpha-Streptococcus spp (25%), and R. equi (14%)
Anaerobes were isolated from (17%) and comprised Bacteroides spp, Fusobacterium necrophorum, Clostridium sordelli, and Prevotella spp
One horse was diagnosed with EMPF at necropsy
Of the 35 horses in the study, 29 were discharged alive, 4 were euthanized, and 2 died in hospital
Both horses that died and 3 that were euthanized were hyponatremic at admission
When evaluating [Na], direct ion selective electrode (dISE) methodology should be used to avoid interference from increased plasma protein or triglyceride concentrations
Conclusion: Hyponatremia at admission is associated with the presence of inflammation, SIRS, and with longer duration of hospitalization
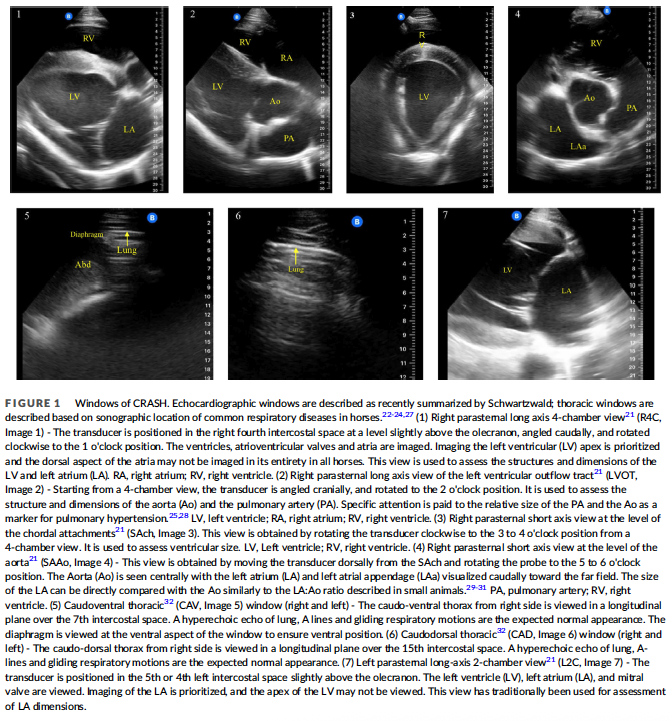
Bevevino et al, 2023
Feasibility of a point-of-care ultrasound protocol for cardiorespiratory evaluation of horses in different clinical settings
Objective: a. Describe the windows of a POCUS protocol for cardiorespiratory assessment of horses (CRASH) b. Estimate the number of acoustic windows that can be acquired by a sonographer in training c. Estimate the time required to complete the protocol for specific groups of horses d. Describe the sonographic abnormalities detected in horses presented with cardiovascular, respiratory, or systemic disease
Results:
The CRASH protocol could be performed in healthy and diseased horses in hospital, barn, and competition settings between 5.5 min (athletic horses) and 6.9 min (horses with clinical disease)
Thoracic windows were obtained most consistently, followed by right parasternal long-axis echocardiographic windows
For the cardiac windows, the 4-chamber long axis window was most consistently of good quality (92.5%) and the short axis at the level of the aorta had the lowest percentage of acceptable quality images in the normal (74.1%) and hospitalized (60%) groups
For the athletic horses, the short axis at the level of the chordal attachments had the lowest percentage of acceptable quality images (78.7%) and the 2 chamber long axis window was most consistently of acceptable quality
Frequently detected abnormalities were pleural fluid, lung consolidation, B-lines, and moderate-to-severe left-sided heart disease
Conclusion: The CRASH protocol was feasible using a pocket-sized ultrasound device in various groups of horses, could be completed rapidly in a variety of settings, and frequently identified sonographic abnormalities when evaluated by an expert sonographer. The diagnostic accuracy, observer agreement, and utility of the CRASH protocol merit further evaluation
Hepworth-Warren et al, 2023
Utility of serum amyloid A in monitoring clinical response to antimicrobial treatment in horses with bacterial pneumonia
Objective: To monitor SAA concentration in response to treatment and identify associations among SAA concentration, WBC and neutrophil counts, and fibrinogen in bacterial pneumonia in adult horses
Results:
Geometric mean SAA concentration on day 0 was 537 ug/mL
Geometric mean SAA concentration decreased significantly over time, peaking at day 2 and decreasing until discharge
SAA was normal (0 ug/mL) at the time or discharge in 40% of horses and decreased from admission in 94% of horses
Plasma concentration of fibrinogen, neutrophil count, and WBC count did not change significantly over time
Hyperfibrinogenemia was present in 35% of horses on day 0
Conclusion: SAA concentration decreased significantly over the course of treatment and correlated with clinical improvement of pneumonia, whereas fibrinogen, neutrophil, and WBC counts did not
Boccardo et al, 2024
Blood gases, acid-base, and metabolic alterations in calves with bronchopneumonia diagnosed via clinical signs and thoracic ultrasonography: A cross-sectional study
Objective: To describe metabolic, arterial blood gas, and acid-base disorders in calves with bronchopneumonia (BP) diagnosed by thoracic ultrasound (TUS), Wisconsin score (WISC), and combinations of WISC and TUS
Results:
WISC5: 71.9% healthy calves and 28.1% BP calves
TUS1cm: 30.7% healthy calves and 69.3% BP calves
TUS3cm: 51.1% healthy calves and 48.9% BP calves
WISC5/TUS1cm: 26% healthy calves, 4.8% upper respiratory tract infection calves, 45.8% subclinical BP calves, 23.4% clinical BP calves
WISC5/TUS3cm: 39.4% healthy calves, 11.7% upper respiratory tract infection calves, 32.5% subclinical BP calves, 16.5% clinical BP calves
Variables that exhibited statistically significant differences between healthy and sick calves as classified with WISC5 included, Na+, blood glucose, and blood urea
With TUS1cm, the statistically different variables included A-aO2, Na+, K+, blood glucose, blood creatinine, USI, and PON-1
With WISC5+TUS1cm, the variables that exhibited statistically significant differences were Na+, K+, AG, blood glucose, blood urea, USI, SIG, and PON-1
With WISC5+TUS3cm, only Na+, blood glucose, blood urea, and PON-1 showed statistically significant differences
Oxygenation and acid-base variables were unaffected
Glucose concentration in TUS-affected calves was significantly lower than in healthy calves
Paraoxonase-1 was significantly lower in TUS-affected calves
None of the variables highlighted clear distinctions in WISC-detected clinical and subclinical BP calves based on the combination of WISC and TUS
Suggest that metabolic changes during an episode of BP diagnosed with WISC score or TUS1 or 3cm were less critical than other disease conditions
Conclusion: Clinical signs indicate minor systemic disorders compared to TUS. The abnormalities detected by ultrasonographic examination were moderate and did not deviate from normal reference ranges
Hallowell et al, 2024
An updated description of bacterial pneumonia in adult horses and factors associated with death
Objective: To describe the clinical presentation and bacterial isolates of adult horses with bacterial pneumonia and identify factors associated with death
Results:
Historical risk factors were present for 60% of cases
History of travel (20%), general anesthesia (9.5%), esophageal obstruction (20%), other respiratory illness (12%)
Median duration of clinical signs before presentation was 10.5 days
Abnormal vital signs on intake were present for <50%
Fever present in 26%, tachycardia in 39%, and tachypnea in 44%
98% had one or more abnormality on ultrasound examination
Comet tails (68%), consolidation or abscessation (76%), pleural effusion (38%)
The most common clinicopathologic abnormalities were hyperglycemia (66%), band neutrophilia (64%), hyperfibrinogenemia (52%), lymphopenia (44%), and hypoalbuminemia (44%)
Most horses (58%) underwent at least 1 change of antimicrobial treatment and 67% received the highest priority critically important antimicrobials
For cases in which TTW and pleural effusion samples were both submitted, bacterial growth was identical between samples in 27%, in 45% there was growth from the TTW sample but none from the pleural fluid, and in 27% some but not all of the organisms identified on TTW were also identified on pleural effusion
One case had growth of an organism on pleural effusion culture that was not identified on TTW culture
Streptococcus zooepidemicus was the most isolated bacteria (44%), followed by E coli (19%), Kelbsiella spp (18%), other Streptococcus species (17%), and Bacillus spp (13%)
Fusobacterium spp were the most common anaerobic isolates (11%)
Antimicrobial susceptibility varied widely
Complications were reported in 12% of cases
Laminitis in 3.7%, antimicrobial associated diarrhea in 1.9%, pneumothorax in 0.94%, and thrombophlebitis in 0.94%
Survival to discharge was 73%
Heart rate at presentation and higher creatinine increased the risk of death
Higher lymphocyte count reduced risk
Could be that horses with higher lymphocyte counts have less circulating endotoxin and therefore less severe disease
Conclusion: Contrasting older literature, Fusobacterium spp. were the most common anaerobes. Streptococcus zoeepidemicus remained the most common isolate and was predictably susceptible to penicillin. Antimicrobial susceptibility was otherwise variable and broad applicability is limited as this was a single-center study. Increased risk of death associated with tachycardia and abnormally high serum creatinine concentration is consistent with previous studies
Raidal et al, 2024
Use of prototype bi-nasal prongs for noninvasive ventilation in foals
Objective: To compare bi-nasal prongs and masks for NIV in foals with pharmacologically induced respiratory insufficiency
Results:
Bi-nasal prongs were well tolerated and required less manual positioning or monitoring compared to the mask
The mask had to be held in place manually by an assistant to minimize leaks during NIV and spirometry
Partial pressure of carbon dioxide did not increase during NIV with bi-nasal prongs and was lower than observed with masks
Expiratory flow limitations may attenuate hypercapnia in foals during NIV and in this study expiratory flow limitations may have been ameliorated by the leaking of exhaled respiratory gases around the nasal prongs and reduced equipment dead space
The expiratory Vt was approximately 75% of the inspiratory value, suggesting there was substantive leakage around the prongs
This is likely clinically acceptable
Oxygenation and respiratory mechanics were improved in all foals and not different between device interfaces
Conclusion: Nasal prongs were well tolerated, had similar effects on respiratory function, and appeared to ameliorate hypercapnia observed previously during NIV in foals
What can high flow nasal oxygen deliver?
Heated and humidified medical gas at adjustable flow rates, up to 60 L/min, and FiO2, up to 100% via nasal cannulas
Proposed Benefits of High Flow Nasal Oxygen
Proposed that HFNOT improves pulmonary mechanics and reduces respiratory fatigue via reduction of anatomical dead space, provision of low-level PEEP, provision of constant FiO2 at rates corresponding to patient requirements and through improved patient tolerance
Reports in humans indicate that HFNOT decreases breathing frequency and work of breathing and reduces the need for escalation of respiratory support
Indications for High Flow Nasal Oxygen
Current indications in dogs include acute respiratory failure associated with pulmonary parenchymal disease, upper airway obstruction and carbon monoxide intoxication
Has also been advocated in certain conditions in cats and foals
Three Groups of Conditions that Can Result in Tissue Hypoxia
Those causing arterial hypoxemia
Those causing failure of the oxygen hemoglobin transport system without arterial hypoxemia
Those impairing the cells’ ability to utilize oxygen
Three Groups of Conditions that Can Result in Tissue Hypoxia - Those Causing Arterial Hypoxemia
Decreased FiO2
Alveolar hypoventilation
Gas diffusion impairment
V/Q mismatch
Cardiopulmonary shunt
Three Groups of Conditions that Can Result in Tissue Hypoxia - Those Causing Failure of the Oxygen Hemoglobin Transport System Without Arterial Hypoxemia
Anemia
Dyshemoglobinemia
Inadequate blood flow to tissues
Three Groups of Conditions that Can Result in Tissue Hypoxia - Those Impairing the Cells’ Ability to Utilize Oxygen
Cyanide toxicity
Low-Flow Oxygen
Deliver oxygen at a flow rate that is lower than the patient’s ventilatory requirements resulting in dilution of the concentration of inspired oxygen relative to the inspiratory flow
Conventional oxygen therapy (COT)
High-Flow Oxygen
Can provide gas at a rate to match minute ventilation and therefore a stable and predictable FiO2
Flow By FiO2
25-45%
Flow By Flow Rate
6-8 L/min
Flow By Advantages
Utilizes readily available equipment
Flow By Limitations
Not appropriate for prolonged therapy
Wasteful
Flow By Indications
Triage and procedures
Initial stabilization
Oxygen Cage FiO2
21-60%
Oxygen Cage Advantages
Well tolerated
Allows eating and drinking
Oxygen Cage Limitations
Reduced access to patients
FiO2 rapidly decreases when doors opened
Larger patients
Oxygen Cage Indications
Patients that will not tolerate nasal oxygen or in which nasal oxygen is contraindicated
Face Mask FiO2
35-55%
Face Mask Flow Rate
1-6 L/min
Face Mask Advantages
Utilizes readily available equipment
Rebreathing at low rates
Face Mask Limitations
Not appropriate for prolonged therapy
FiO2 depends on fit of mask
Face Mask Indications
Triage and procedures
Initial stabilization
Risk of rebreathing
Nasal Prongs Flow Rate
50-150 ml/kg/min
Nasal Prongs Advantages
Easy to place
Well tolerated
Nasal Prongs Limitations
Poor patient tolerance at high flow rates
Not suitable for some facial conformations
Nasal Prongs Indications
Ongoing oxygen support in hospital
Nasal Catheter FiO2
30-60%
Nasal Catheter Flow Rate
50-150 ml/kg/min
Nasal Catheter Advantages
Well tolerated
Nasal Catheter Limitations
Poor patient tolerance at high flow rates
Harder to place
Nasal Catheter Indications
Ongoing oxygen support in hospital
CPAP FiO2
21-100%
CPAP Advantages
Reliable FiO2
Delivers PPEEP
Humidifies inhaled gases
CPAP Limitations
Often requires heavy sedation
Specific equipment
CPAP Indications
Hypoxemia despite oxygen support
Upper airway obstruction
HFNOT FiO2
21-100%
HFNOT Flow Rate
10-60 L/min
HFNOT Advantages
Reliable FiO2
Delivers PEEP
Humidified inhaled gases
HFNOT Limitations
Specific equipment
HFNOT Indications
Hypoxemia despite conventional oxygen therapy
Increased work of breathing
Mechanical Ventilation FiO2
21-100%
Mechanical Ventilation Advantages
Reliable FiO2
Delivers PEEP
Humidifies inhaled gases
Mechanical Ventilation Limitations
Specific equipment
High complication rate
High cost
Mechanical Ventilation Indications
Hypoventilation
Hypoxemia despite oxygen support
Increased work of breathing (fatigue)
Non-Invasive Ventilation
Delivery of mechanical ventilation via techniques that do not require endotracheal intubation
Improve gas exchange and reduce inspiratory effort through the generation of positive pressure within the airways, reducing upper airway obstruction and recruitment of alveoli
What are the two main modalities of non-invasive ventilation?
Continuous positive airway pressure (CPAP)
Non-invasive pressure support ventilation
Continuous Positive Airway Pressure (CPAP)
May be performed using a tight-fitting mask or helmet with an expiratory valve connected to an oxygen source and gas blender or via a mechanical ventilator
Significant increases in PaO2 have been demonstrated after CPAP administered by helmet in dogs and anesthetized cats
Raidal et al compared the effect on respiration and ventilation in sedated foals treated with CPAP and mask oxygen
The effects of CPAP on arterial blood gas parameters were comparable to mask oxygen with modest increases in PaCO2 in almost all animals for both modalities
Clinical use in veterinary patients is effective in providing a known level of PEEP and improving oxygenation
Limited by the need for sedation or anesthesia to be tolerated in some patients and the high oxygen flow requirement to maintain PEEP
Non-Invasive Pressure Support Ventilation
Requires a ventilator triggered by the patient's inspiratory effort to deliver a decelerated gas flow in order to generate and maintain two different pre-set pressures during inspiration and expiration
Require nasal or oronasal (full face) masks which form an air seal
Invasive Mechanical Ventilation
Indicated in the management of severe hypoventilation, severe hypoxemia despite oxygen supplementation, when there is excessive work of breathing, and when long term endotracheal intubation is required
Provide oxygen support, conditioning of inspired gases, reduces the work of breathing, and can improve oxygenation via increasing airway and alveolar pressure and recruiting collapsed alveoli
Heavy sedation or a light plane of anesthesia generally required
Reported complications
Corneal and oral mucosal ulceration
Hypothermia
Positive fluid balance
Ventilator induced lung injury
Ventilator-associated pneumonia
Cardiovascular compromise
Patients ventilated for primary hypoventilation have a better prognosis than those being treated for primary pulmonary pathology, in particular ARDS
What three variables does high flow nasal oxygen therapy allow modification of?
Percentage of oxygen delivered
The flow rate of gas
Gas temperature
Components of HFNOT Devices
A high pressure source of oxygen and air
An air-oxygen blender or high flow Venturi system
A humidifying and heating system for conditioning the gas to optimal temperature and humidity
A sterile water reservoir
A non-condensing circuitry
An interface
Clinically Relevant Features of HFNOT
Provision of fixed concentrations of inspired gases
Delivery of heated and humidified gases
Generation of flow-dependent positive airway pressure
Flushing of anatomical dead space
Features result in increased patient comfort and compliance, provision of higher FiO2 compared to conventional oxygen therapy, maintenance of mucosal integrity and function, alveolar recruitment, and decreased work of breathing
FiO2 and Dead Space Washout with HFNOT
Flow rates provided during HFNOT are able to match the peak inspiratory flow of the patient and thus reliably provide the set FiO2
FiO2 approaching 100% are able to be achieved without the need for endotracheal intubation
Higher oxygen flow rates delivered during HFNOT compared to conventional oxygen therapy are proposed to "washout" CO2 from the anatomical dead space within the nasopharynx resulting in rebreathing
Results in improved FiO2, more efficient provision of minute ventilation, and decreased work of breathing
Positive Airway Pressure with HFNOT
PEEP aims to prevent alveolar collapse and recruit atelectic lung, improving alveolar ventilation
Providing higher flow rates to match intrinsic PEEP via CPAP reduces the work of breathing in patients with obstructive airway disease
A study of human cardiac surgery patients demonstrated a positive linear relationship between flow rate and mean airway pressure during HFNOT, with peep ranging from 3.0-4.8 cmH2O at flow rates of 30-50 L/min
Variations in the generation of airway pressure during HFNOT are due to patient differences, particularly the diameter of the nasal prongs relative to the patient's nares and whether or not the mouth is closed
Multiple prospective studies of adult humans treated with HFNOT have demonstrated that significant airway pressure generation only occurs when the patient's mouth is closed
Airway Resistance with HFNOT
Nasopharynx warms and humidifies inspired gases by contact with its large surface area
Results in significant resistance to inspiratory flow
By matching or exceeding rates of inspiratory flow, HFNOT likely attenuates his effect and further reduces the work of breathing
Pharyngeal distending pressure of up to 4 cm H2O can be achieved with HFNOT flow rates of 2 L/kg/min
Positive upper airway pressure may reduce airway resistance by stenting the soft palate and pharynx
Proposed that HFNOT stimulates airway stiffening and stenting by activation of the alae nasae muscle
Cool, dry air during respiratory support has been shown to decrease pulmonary compliance and conductance in infants
Demonstrated to be associated with a protective bronchoconstrictive response, secondary to stimulation of mucsarinic receptors in the nasal mucosa
In Saslow et al, pulmonary compliance was higher in patients receiving HFNOT compared to CPAP, despite the lower PEEP
Conditioning of inhaled gases by the nasal mucosa consumes energy
This energy is conceivably increased during supplementation of cool, dry gas during conventional oxygen therapy as well as during periods of respiratory distress and increased minute ventilation
Mucociliary Clearance with HFNOT
Slow, turbulent airflow in the nasopharynx allows inspired air to be warmed to ~34*C and humidified to 100%
Creates optimal conditions for the functioning of cilia and maintenance of mucus composition
Increased respiratory rates and open-mouth breathing in respiratory failure can affect airway humidification and conditioning of inspirated gas
HFNOT has been shown to reduce respiratory rates and effort and may be able to provide clinical improvement through the reduction in open mouth breathing
In a canine model, provision of heated and humidified gas improved mucociliary function
Patient Comfort with HFNOT
HFNOT is better tolerated and more comfortable than conventional oxygen therapy and non-invasive ventilation
Attributed to conditioning of inspired gas, correction of hypoxemia, increased alveolar recruitment, and the ability to eat and speak more readily
Conditioning of gas
Maintains conditioning of inspired air and hydration of the airway mucosa so nasal passages aren't desiccated
Device-patient interface
Non-invasive ventilation interfaces are associated with the development of skin lesions and patient discomfort
The interface of nasal CPAP requires secure fixing without leaks so the reported incidence of pressure ulcers ranges from 15-100%
Masks and helmets may interfere with eating and drinking
When compared to conventional nasal oxygen therapy patients, HFNOT patients experience decreased eye irritation and find it easier to eat
Indications for HFNOT in Human Medicine
Acute hypoxemic respiratory failure
Acute heart failure
Interstitial lung disease
Asthma
Carbon monoxide intoxication
Procedural sedation
Post-extubation
HFNOT for Acute Hypoxemic Respiratory Failure in People
HFNOT is becoming the first-line therapy for acute hypoxemic respiratory failure in patients that fail to show an adequate response to conventional oxygen therapy and for whom immediate intubation is not indicated
Cross-over study demonstrated that this modality significantly reduced discomfort in critically ill patients with respiratory failure compared to conventional therapy
FLORALI clinical trial
Compared conventional oxygen therapy (10 L/min or more via mask), HFNOT (50 L/min), and non invasive ventilation (8 hours or more/day with bilevel setting)
Included non-hypercapnic patients with acute hypoxemic respiratory failure (PaO2/FiO2 <300 mmHg), 84% of which had pneumonia
There was not significant difference in intubation rates between the 3 groups
Mortality was lower in the HFNOT group in the ICU and at 90 days
HFNOT was associated with a decreased intubation rate in a more severely affected subgroup of patients (PaO2/FiO2 <200 mmHg)
More than 75% of patients had thoracic radiographic changes consistent with a diagnosis of early ARDS
Observational study evaluated the effect of HFNOT in ARDS
45/51 patients who received HFNOT as a first line treatment had ARDS (PaO2/FiO2 137 mmHg) with 26/45 successfully treated with HFNOT alone
Patients who failed HFNOT had higher Simplified Acute Physiology Score II (SAPS II) scores in multivariate analysis
HOT-ER trial
Aimed to determine if HFNOT compared to conventional oxygen therapy reduced the need for non-invasive ventilation or intermittent positive pressure ventilation in patients with acute respiratory distress presenting to a hospital emergency department
Hypoxemic (SpO2 92% or less) and tachypneic (respiratory rate 22 bpm or greater) adult patients were randomized to receive HFNOT or conventional oxygen therapy with need for mechanical ventilation as the primary outcome
HFNOT did not reduce the need for ventilation in this population
Adverse events were infrequent but 1/12 patients did not tolerate HFNOT
HFNOT for Acute Heart Failure in People
HFNOT has been proposed to have hemodynamic effects that may aid in the management of acute heart failure and pulmonary edema
In particular, reducing pulmonary congestion via reductions in cardiac preload and afterload
Roca et al performed echos in patients with NYHA class II heart failure during HFNOT delivered at flow rates of 20 L/min and 40 L/min with 21% FiO2
Significant reductions in inspiratory collapse of the inferior vena cava occurred relative to flow rate during HFNOT and normalized following discontinuation of therapy
HFNOT may decrease afterload through the provision of PEEP and amelioration of sympathetic nervous system stimulation associated with hypoxia
Makdee et al
Assessed the efficacy of HFNOT in the management of acute heart failure by comparing respiratory rates following HFNOT with conventional oxygen therapy in patients presenting to an emergency room with pulmonary edema
Patients were included if they had SpO2 <95% and respiratory rate >25 breaths per minute
HFNOT was associated with lower respiratory rates at 60 minutes after initiation of therapy but there was not difference in mortality, non-invasive ventilation or intubation between groups
Prospective study compared HFNOT with conventional oxygen therapy in patients presenting to the emergency room with acute pulmonary edema
Conventional oxygen therapy group received oxygen via a nasal cannula at flow rates of >2 L/min while HFNOT was initiated at 45 L/min and FiO2 100%
Patients in both groups were treated to maintain SpO2 >93%
HFNOT resulted in greater improvement in respiratory rate, SpO2, lactate levels and arterial blood gas parameters compared with conventional therapy
Osman et al
Comparing HFNOT to helmet CPAP in adult patients presenting to the emergency room with acute cardiogenic pulmonary edema
CPAP more effective in the very short term in improving dyspnea, hemodynamics, and respiratory parameters
HFNOT for Interstitial Lung Disease in People
Group of pulmonary conditions that involve changes to the distal lung parenchyma
Subdivided into those with an identifiable etiology and those without
Acute respiratory failure can complicate interstitial lung disease and is associated with a poor prognosis and high mortality rate
Mechanical ventilation does not improve oxygenation in affected patients and is associated with a high incidence of barotrauma and a poor prognosis
Horio et al
Cases of acute respiratory failure associated with interstitial lung disease
Commenced on HFNOT (FiO2 70-100% ; flow rate 40 L/min) while additional medical management was initiated and took effect
HFNOT was well-tolerated and weaned in accordance with improving oxygenation parameters until discharge at 21-26 days
All of the subjects demonstrated immediate improvement with the commencement of HFNOT after failing to respond to conventional oxygen therapy
Retrospective study of patients with exacerbation of interstitial pneumonia
Grouped into pre-HFNOT and post-HFNOT cohorts based on the introduction of HFNOT at the hospital
Incorporation of HFNOT into the management of interstitial lung disease patients in this study resulted in lower in-hospital mortality, reduced requirement for sedation and analgesia and a lower incidence of discontinuation of oral intake
No difference in the incidence of complications
HFNOT for Asthma in People
The cold and dry air provided via conventional oxygen therapy modalities may potentially exacerbate bronchoconstriction, promote airway inflammation, and impair mucociliary function
Retrospective studies of pediatric status asthmaticus showed significant improvements in vital parameters, serum pH, and SpO2/FiO2 associated with HFNOT compared to conventional oxygen therapy
A pilot study supported these findings, demonstrating higher rates of pulmonary score improvement 2h after initiation of HFNOT compared to conventional oxygen therapy
HFNOT has been associated with decreased intubation rates for severe pediatric asthma
Improved patient outcomes have not been demonstrated
HFNOT for Carbon Monoxide Intoxication in People
Carbon monoxide competitively and reversibly binds to hemoglobin with 250 times greater affinity than oxygen resulting in a marked anemic hypoxia despite a normal PaO2
Treatment involves provision of high FiO2 to compete with carbon monoxide for hemoglobin binding sites and reduce the half-life of carboxyhemoglobin
Prospective study of adults with carbon monoxide intoxication
Primary objective was to determine the mean half-life of COHb after HFNOT (FiO2 100%, T 37*C, 60 L/min) which was found to be 36.8 mins
Another retrospective study identified a similar COHb half-life following HFNOT (41.1 min) but this was not found to be significantly different to that in patients receiving conventional oxygen therapy
There was a significant difference in COHb levels between treatment groups at 60 and 90 minutes
HFNOT for Procedural Sedation in People
Oxygen desaturation, airway obstruction, and apnea are the most prevalent adverse events during procedural sedation
Risk factors for hypoxemia during procedural sedation include high ASA physical status, reduced cardiopulmonary reserve, obesity, and prolonged procedural duration
Meta-analysis evaluating the effect of HFNOT and conventional oxygen therapy during procedural sedation in adults and children
HFNOT reduced the risk of hypoxemia and increased minimum oxygen saturation
Reduction in hypoxemia persisted regardless of the procedure, FiO2, risk-profile of the patient, and mode of propofol administration
HFNOT Post-Extubation in People
Post-extubation respiratory insufficiency is a known complication following weaning from invasive mechanical ventilation and may progress to acute respiratory failure which results in reintubation
Conditions associated with post-extubation respiratory insufficiency include upper airway obstruction, decreased respiratory muscle function, atelectasis and increased work of breathing, and hemodynamic stability
Zhu et al
Attempted to quantify the benefits of HFNOT for patients after planned extubation
HFNOT was associated with reduced post-extubation respiratory failure, decreased respiratory rates, and increased PaO2
No significant differences in reintubation rate, length of ICU and hospital stay, PaCO2, mortality, or severe adverse events were identified
Meta-analysis
Compared HFNOT and non-invasive ventilation in patients after extubation
Initial use of HFNOT in the post-extubation period was not inferior to non-invasive ventilation in regards to the probability of reintubation, treatment failure, or mortality and was associated with a reduced probability of complications including cutaneous lesions and respiratory failure
Multicenter randomized control trial comparing HFNOT to HFNOT in combination with non-invasive ventilation in patients at high risk of extubation failure
Included patients who successfully completed a spontaneous breathing trial after more than 24 hours intubation
Those in the combination group commenced non-invasive ventilation immediately after extubation with a minimum duration of 12h per day for the first 48h
HFNOT was administered between non-invasive ventilation sessions in the combined group and continuously in the HFNOT sole treatment group
Reintubation rate at day 7 was significantly higher in the HFNOT group compared to when the therapies were combined
Combination of HFNOT and non-invasive ventilation appeared to be more beneficial in patients with pre-exutubation hypercapnia, defined as PaCO2 > 45 mmHg
Complications and Considerations for HFNOT in People
Complications are rare
Complications include
Facial trauma
Abdominal distension
Aspiration
Epistaxis
Barotrauma
Risk is lower than other non-invasive ventilation modalities
Major concern during HFNOT is the risk of delayed intubation and mechanical ventilation in hypoxemic patients
Kang et al
Evaluated if delaying intubation until failure of HFNOT adversely affected patient outcome
Categorized patients based on time at which intubation occurred - before (early) and after (late) 48 hours of HFNOT
Patients intubated after 48 hours had higher overall ICU mortality
In a prospective observational study both patients and caregivers judged HFNOT to be more comfortable compared to conventional oxygen therapy
Patients report less mouth dryness and improved breathlessness with HFNOT compared with facemask oxygen
FLORALI trial reported higher patient discomfort after 1 h in patients failing HFNOT
Lower temperatures with full humidification was associated with lower discomfort regardless of flow rate
Cutaneous and mucosal ulceration of the nose, nasal septum, frenulum, and pinnae associated with friction between the skin and interface in prolonged HFNOT has been reported
Less significant than with NIV and CPAP
Retrospective study evaluating complications associated with HFNOT in a pediatric ICU over 1 year
Pneumothoraxes
Hodge and Prodhak
3 life threatening occurrences of air leak syndrome associated with HFNOT in pediatrics
Pneumothorax
Pneumomediatstium
Subcutaneous emphysema reported
Tension pneumocephalus rare but has been associated with HFNOT
Contraindications for HFNOT
Nasal, facial, and airway abnormalities that may affect nasal cannula fit and device function
Include epistaxis, basilar skull fractures, surgery to the nose and nasal obstruction
Predictors of HFNOT Treatment Failure in People
Current literature indicates that around 30% of patients will fail treatment and require mechanical ventilation
In patients with acute hypoxemic respiratory failure, an increased heart rate after 1 h of HFNOT was associated with intubation
Hemodynamic instability, elevated SOFA score, thoracoabdominal asynchrony, significantly increased respiratory rate, and poor oxygenation have been associated with HFNOT failure
ROX index was developed to predict success and failure of HFNOT
Index is the ratio of the pulse oximetry oxygen saturation over the fraction of inspired oxygen over the respiratory rate [(SpO2/FiO2/RR]
In a prospective study of 157 pneumonia patients treated with HFNOT, with FiO2 set to maintain SpO2 >92% and flow rate set at the clinician's discretion
Treatment failure was assessed based on respiration, oxygenation, and ventilatory parameters
Criteria for intubation and mechanical ventilation were decreased Glasgow Coma Scale score, hemodynamic instability, and persistent or worsening respiratory condition
A ROX index of 4.88 or greater measured after 12 hours of HFNOT was significantly associated with a lower risk of mechanical ventilation
In a multicenter prospective study ROX of 4.88 or greater measured at 2, 6, or 12h after HFNOT initiation was consistently associated with a lower risk of intubation
A ROX <2.85, <3.47, and <3.85 at 2, 6, and 12h of HFNOT initiation, respectively, were predictors of HFNOT failure
Patients who failed also demonstrated a lower increase in the values of the ROX index over the 12 h
HFNOT in Healthy Dogs
Precision Flow system vs conventional nasal oxygen cannula in healthy dogs
Significantly higher increase in baseline PaO2 between the delivery methods but no difference in PaO2 achieved with HFNOT at different flow rates
No differences in transpulmonary pressure between baseline and any of the treatment methods or between any of the treatments, suggesting negligible generation of positive airway pressure
Jagodich et al.
Optiflow/Airvo 2 system in a prospective randomized crossover study
Oxygen provided via conventional nasal cannula or HFNOT at a range of flow rates
Airway pressures generated by each system were comparable at equivalent flow rates
Only HFNOT at flow rates of 1-2 L/kg/min was able to maintain positive airway pressure and achieve CPAP in the majority of dogs
Both inspiratory and expiratory airway pressures significantly increased with increases in flow rate
Harduin et al
Evaluated the impact of gas flow rate and temperature on tolerance of dogs receiving HFNOT during recovery from anesthesia
No effect of flow rate or temperature on vital parameters or tolerance and overall good tolerance
HFNOT in Hypoxemic Respiratory Failure in Dogs
Keir et al
HFNOT in dogs with primary pulmonary hypoxemia
All dogs transitioned to HFNOT following failure of conventional oxygen therapy to maintain adequate oxygenation
A significant increase in mean PaO2 was achieved in association with a significant increase in oxygen flow rate
Four of the dogs had resolution of their hypoxemia following HFNOT
Prospective pilot study of effectiveness and tolerance of HFNOT therapy in 11 dyspneic dogs
After 60 minutes of treatment with 100% FiO2 at a flow rate calculated to match minute ventilation there was a significant increase in mean PaO2 and resolution of hypoxemia in 5/8 dogs with PaO2 <80 mmHg prior to initiation of HFNOT
6/11 dogs had a decrease in respiratory rate but only 2/11 were classified as not in respiratory distress base on the authors criteria
HFNOT was well tolerated
6/11 dogs died as a result of cardiac arrest or euthanasia due to deteriorating clinical condition
5/6 met criteria for intubation within 24h of admission
Prospective study evaluating HFNOT in acute hypoxemic respiratory failure in 22 dogs
Significant improvements in dyspnea score and oxygen saturation were identified at all times points compared to baseline with a moderate correlation between HFNOT flow rate and PaO2
There was no significant difference in PaCO2 between conventional oxygen therapy and HFNOT
There was a moderate correlation between PaCO2 and HFNOT flow rate
6/22 were intubated and ventilated after starting HFNOT and an additional 6/22 were euthanized due to required escalation of therapy
10/22 survived to discharge
8/22 avoided intubation and mechanical ventilation
HFNOT Post-Extubation in Dogs
Jagodich et al
Brachycephalic dogs with signs of upper airway obstruction in the immediate post-anesthetic period
Dyspnea scores and respiratory rates improved over time with stable normoxemia despite decreasing FiO2 and flow rates
HFNOT was able to be discontinued in <12h in 3 dogs and all survived to discharge without requirement of reintubation
HFNOT in Carbon Monoxide Poisoning in Dogs
Gazsi et al
Comparing mechanical ventilation and HFNOT in dogs with carbon monoxide poisoning following progression of clinical signs despite conventional oxygen therapy
The dog receiving HFNOT had marked improvement in FCOhb after 4 hours
The dog treated with mechanical ventilation had similar improvements in FCOHb and was weaned off the ventilator in the same time period
The calculated half-life of FCOHb was 167 min and 150 min in the dogs treated with HFNOT and IPPV, respectively
Complications of HFNOT in Dogs
Increase in PaCO2 has been identified in dogs receiving HFNOT
Aerophagia and gastric distension has been noted in dogs receiving HFNOT
No cases of air leak syndrome have been identified but there was one dog with pre-existing pneumothorax that did not resolve until discontinuation of HFNOT
HFNOT in Horses
Floyd et al
HFNOT in foals <36 hours old
No significant improvement in oxygenation with treatment was identified but not all foals were hypoxemic prior to initiation of HFNOT
Improvements in respiration pattern and decreased respiratory rates were observed
10/14 survived to discharge
HFNOT was well tolerated in all patients
No significant complications noted but two foals required escalation to mechanical ventilation and HFNOT had to be discontinued in two foals due to excessive activity
No significant increase in mean PaCO2 was observed
A mild but insignificant decrease in PaCO2 was observed in many foals
What % of the opening of the nares should the nasal prongs occlude in HFNOT
~50% to facilitate generation of desired airway pressures while minimizing resistance to exhalation
HFNOT Device Set Up
Patients should initially receive 100% FiO2 while stabilization occurs
This may then be titrated down based on patient oxygenation, aiming to maintain a SpO2 > 95% or PaO2 > 80 mmHg
Timely reduction of FiO2 to <60% is recommended due to concerns for oxygen toxicity associated with prolonged administration of high concentrations of oxygen
Flow rates should be commenced at 1-2 L/kg/min or calculated to match the patients minute ventilation (respiratory rate x VT)
A CPAP effect in dogs occurs at flow rates of 1-2 L/kg/min
A study assessing HFNOT protocol in human pediatric intensive care patients demonstrated more rapid weaning, decreased failure rates, and possibly decreased rate of escalation to positive pressure ventilation in patients initially treated with higher flow rates
These patients also received lower initial FiO2 and had a shorter length of stay in hospital despite longer duration of HFNOT
Higher flow rates may result in patient discomfort and aerophagia
Temperature is initially set at 37*C but may be adjusted based on patient body temperature and comfort
HFNOT Weaning
No weaning protocols available
Consider similar criteria as used for weaning from other methods of oxygen support
Improvement in underlying condition
Decreased device settings
High likelihood of coping with de-escalated therapy (e.g. conventional oxygen therapy)
Patients with stable respiration and oxygenation at <500 ml/kg/min FiO2 <40% will likely meet these criteria
FiO2 should be reduced prior to reducing the flow rate
Reduction of 5-10% FiO2, followed by reassessment in 1-2 h is recommended
In human adults, maintenance of stable respiratory parameters at 40% FiO2 should be achieved prior to flow weaning
In neonates, it has been recommended that FiO2 be reduced to 30% prior to reductions in flow rate
Respiratory rate, FiO2 and work of breathing should be stable for 12-24 h before commencing flow reduction
Escalation from HFNOT
Escalation of treatment is recommended when there is no clinical improvement in 1-2h despite high flow rates and FiO2
Failure to maintain adequate oxygenation despite HFNOT or persistent increased work of breathing are indication for positive pressure ventilation
Mechanical ventilation is also indicated in cases of severe or progressive hypoventilation
Long et al, 2024
Bilateral diaphragmatic paralysis in a weanling donkey jack
Case description: A 5 month old miniature donkey jack presented for fever, cough, and increased respiratory rate and effort initially unresponsive to treatment with antimicrobials and anti-inflammatories
Clinical findings:
No evidence of upper respiratory obstruction or bacterial pneumonia
Serial arterial blood gas evaluations revealed hypercapnia and hypoxemia
Diagnostic imaging was consistent with bilateral diaphragmatic paralysis
Nasal swab for equine influenza type A (subtype H3N8) was positive
Mildly decreased whole blood selenium concentration
Treatment and outcome:
Recovered after treatment with anti-inflammatories and supportive care
Clinical relevance: This case documents the first report of diaphragmatic paralysis in a donkey, with concurrent equine influenza infection offering a possible causal factor. Bilateral diaphragmatic paralysis should be considered as a differential diagnosis for respiratory distress in donkeys, particularly when diagnostic testing or treatment trials do not support more common causes of respiratory disease in adult animals, such as lower airway disease, asthma, and pulmonary fibrosis
What % of patients admitted to the ICU and mechanically ventilated patients had ARDS?
10% of all patients admitted to the ICU
23% of mechanically ventilated patients
What is the % mortality for patients with severe ARDS?
46%
Berlin Definition - Timing
Within 1 week of a known clinical insult or new or worsening respiratory symptoms
Berlin Definition - Origin of Edema/Diagnostics
Respiratory failure not fully explained by cardiac failure or fluid overload. Need objective assessment (e.g. echocardiography) to exclude hydrostatic edema if no risk factor present
Bilateral opacities - not fully explained by effusions, lobar/lung collapse, or nodules (chest radiograph or computed tomography)
Berlin Definition - Mild ARDS
PaO2/FiO2 >200 mmHg and less than or equal to 300 mmHg with PEEP or CPAP 5cm H2O or more
Berlin Definition - Moderate ARDS
PaO2/FiO2 > 100 mmHg and less than or equal to 200 mmHg with PEEP 5 cm H2O or more
Berlin Definition - Severe ARDS
PaO2/FiO2 100 mmHg or less with PEEP 5cm H2O or more
Vet ALI/ARDS Definition - Timing
Acute onset (<72 hours) of tachypnea and labored breathing at rest
Known risk factors