Endocrinology, GI Med, Repro and Dermatology
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
What is the endocrine system?
Autocrine = hormone signalling produced by a cell which binds back to itself
Paracrine = hormone signally between neighbouring cells
Endocrine = hormone signalling of one to far away cells
regulated by via negative feedback loops
hormones and cytokines act on gland directly to inhibit own production / downregulate → indirectly affecting hormone production
disease = when endocrine hormones are unbalanced and metabolic derangements occur
hypo = under functioning
hyper = over functioning
Pituitary Disease = Diabetes Insipidus and Acromegaly
Pituitary Gland
pedunculated gland (on a stalk) below midbrain
glandular and neurological tissue → produce many hormones
controls thyroid gland and adrenal glands directly
Diabetes Insipidus
decreased vasopressin = antidiuretic hormone, ADH
ADH normally maintains BP by constricting vessels (central pituitary gland) + resorption of water in distal tubules (nephrogenic)
caused = head trauma, neoplasia, cysts
Symptoms + Diagnostics
increased water intake + long term polyuria ad polydipsia (PU/PD)
urinalysis = USG
bloods = high urea/BUN, PCV, TP
water deprivation test (5% each day) to restore USG + normal hydration and body weight
Desmopressin = synthetic ADH to reduce water intake and ± USG
MRI to see if head trauma or cyst impeding pituitary gland
good prognosis with or without treatment, and can be asymptomatic
Acromegaly
increased excretion of growth hormone
also known as hypersomatotropism or “big face'“
common in cats - usually due to grown hormone pituitary tumours → insulin resistance + diabetes mellitus
rare in dogs = due to excessive progesterone (German shepards)
hard to treat → brain surgery to remove tumour
Parathyroid Disease = Hyperparathyroidism
Parathyroid Glands
x4 small glands embedded within the thyroid gland on ventral neck
regulates Ca and P via parathyroid hormone (increase Ca, decrease P)
parathyroid hormone is down-regulated by negative feedback from calcitriol in the renal tubules
Hyperparathyroidism
excessive production of parathyroid hormone
primary = functional tumour or adenoma
renal secondary = secondary to chronic kidney disease
nutritional secondary = secondary to diet (low Ca or high P)
Symptoms + Diagnostics
polyuria and polydipsia (PU/PD)
degenerative joint disease
bloods = high calcium
urinalysis = slightly low USG + crystals
ultrasounds + xray = enlarged or a mass on parathyroid glands
surgical removal of tumour
Thyroid Disease = Hyperthyroidism and Hypothyroidism
Thyroid Glands
butterfly shaped gland wrapping either side of trachea, below larynx
energy metabolism via production of thyroxine (T4)
hypothalamus produces thyrotropin-releasing hormone/TRH
pituitary gland produces thyroid stimulating hormone/ TSH
thyroid gland released thyroxine into blood
Hyperthyroidism = high thyroxine | Hypothyroidism = low thyroxine |
|
|
|
|
Bloods:
| Bloods:
|
Adrenal Disease = Hyperadrenocorticism and Hypoadrenocortism
Adrenal Glands
x2 adrenal glands (x1 w each kidney)
produce cortisol as a stress response
maintains blood pressure, but maintaining Na and K balance
central medulla = catecholamine production
peripheral cortex = steroid hormone production
Glomerulosa = aldosterone → H20 balance
Fasciculata = cortisol → sugar metabolism
Reticularis = androgen → sex hormones
adrenal glands controlled via hypothalamic pituitary adrenal axis
hypothalamus responds by producing corticotrophin releasing hormone (CRH)
Pituitary glands release adrenocorticotrophin (ACTH)
adrenal cortex produces cortisol via negative feedback loop of corticosteroid
Hyperadrenocorticism Cushing’s Disease | Hypoadrenocorticism Addison’s Disease |
|
|
|
|
Bloods
| Bloods
|
|
|
Pancreatic Disease = Diabetes mellitus
Pancreas
gland in abdomen near stomach and duodenum
Exocrine unit = produced digestive enzymes
Endocrine unit = produces insulin and glucagon
Insulin = made by beta cells to promote storage of energy/glucose
Glucagon = made by alpha cells to promote energy utilisation and ketone body formation, mobilise fat stores for energy
Insulin and glucagon antagonist each other, and usual controlled by diet, insulin/glucagon activity and energy expenditure
Diabetes Mellitus
unable to maintain glucose in a normal range → persistent hyperglycaemia and glucosuria
Dogs = beta cells destructive, not reversible. Middle aged, breed specific
Cats = beta cells functional, just lack insulin and sensitivity. Reversible if change obesity, diet and activity. Older male specific
Diabetic ketoacidosis = acutely decompensate → emergency
Symptoms + Diagnostics
normal HR
plantigrade stance
hair coat is dull and unkempt (inactive)
low muscle condition
bloods = high glucose and TP
Fructosamide assay = glycated protein average to help monitor
Ptyalism vs Dysphagia (define, symptoms and diagnostics)
Ptyalism | Dysphagia |
|
|
|
|
|
|
Regurgitations vs Vomiting (define, symptoms)
Regurgitation | Vomiting |
|
|
|
|
Diseases characterised by regurgitation
Obstructive = foreign body, stricture, vascular ring of oesophagus, neoplasia
Motility disorder
Megasophagus - dilation of oesophagus due to low peristaltic activity
Congenital (breed)
Acquired (neuromuscular disease or toxicity)
thoracic radiographs and endoscope → evaluate aspiration pneumonia, rule out foreign bodies or obstructions
blood test → autoimmune or disease related
treat underlying cause + nutritional support
gastrostomy tube
high caloric dense diet
small meals frequently to prevent regurgitation
hold dog upright or use Bailey chair whilst eating
no medications
Inflammatory = gastroesophageal reflux, oesophagitis , hernia
Oesophagitis - inflam of oesophageal lining
Due to: reflux, vomiting, foreign bodies, irritations, stricture formation
Signs: regurg, discomfort swallowing, anorexia, salivation
Diagnosis: history, radiographs or endoscopy
Treatment: analgesia, antacids, meds to increase sphincter tone
Explain acute vs chronic vomiting - causes + diagnostics
Organs = liver, pancreas, kidney, brain, chemoreceptor trigger zone
GI Causes
dietary problems - change, foreign material, intolerance, allergy
stomach, small intestine or large intestine disorders
obstruction, inflam, parasite, ulcer, neoplasia dilation
Acute Vomiting | Chronic Vomiting |
|
|
|
|
Small vs Large Intestine Diarrhoea
Small Intestinal | Large Intestinal |
|
|
Acute vs Chronic Diarrhoea
Acute | Chronic- Small Intestine | Chronic- Large Intestine |
|
|
|
|
|
|
|
| |
Acute Gastritis Acute pancreatitis = middle ages, obese female dogs Feline Pancreatitis = liver, GI inflam or necrotic → anorexia | Colitis Proctitis |
Constipation vs Obstipation
Constipation = infrequent, incomplete or difficult defaecation with passage of hard or dry faeces
Obstipation = intractable constipation cause by prolonged retention of hard, dry faeces (chronic)
Constipation signs, diagnostics + treatment
Symptoms
more common in cats than dogs
straining to defaecate with small volume produces
hard and dry but infrequent
mucoid stool or may have blood
occasional vomiting, inappetence and/or depression
Causes
dietary - excessive fibre
environment - low exercise, dirty litter box
drugs - opioids or diuretics
painful - perineal hernia, anal sac disease,
mechanical obstruction - prostatic enlargement, foreign body, stricture or narrow pelvic canal
general muscle weakness or dehydration or hypothyroidism
neuromuscular disease
Diagnostics
History and exam or rectum + neurological
Bloods - CBC, biochemistry, UQ
abdominal radiography, ultrasound or colonoscopy
Treatment
microlax enema or warm water with saline enema → monitor for defecation
IV fluids
deobstipation = manual removal of faeces under GA
endotracheal intubation = risk of aspiration
warm saline enema prior to assist with softening
manual breakdown by transabdominal massage
remove fragments via anus
radiograph to check progress
Dog vs Cat General Reproductive Cycle Time Periods
Dog | Cat |
|
|
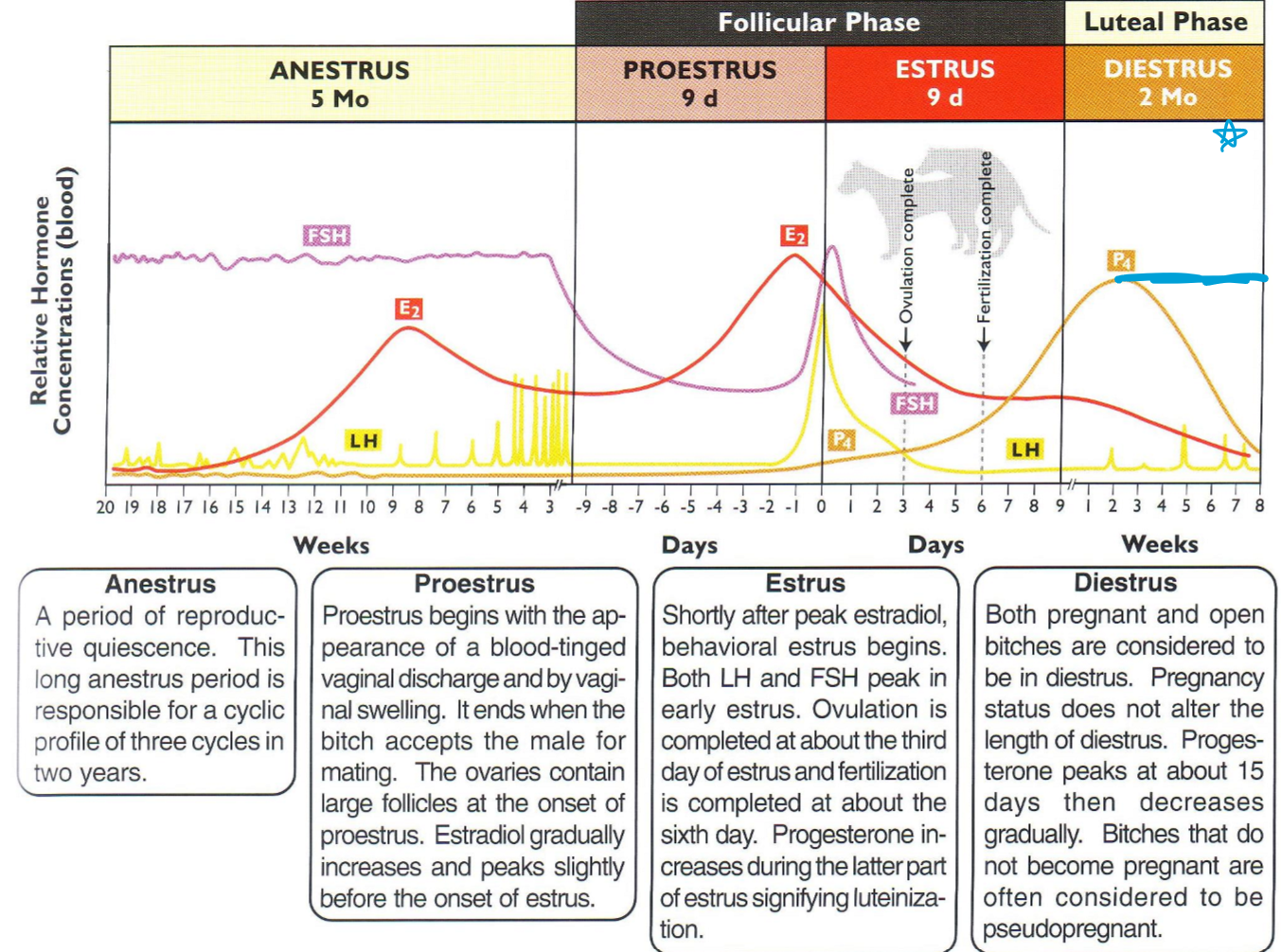
Explain the 4 Phases of the Canine Oestrus Cycle
Proestrus
9 days
changes in behaviour
swollen and turgid vulva
serosanguineous (bloody) vulva discharge
increased oestrogen
Oestrus
9 days
most receptive to mating behaviour
swollen but soft vulva
clear coloured vulva discharge
LH peak, increased progesterone, but decrease oestrogen
Dioestrus and Anoestrus
dioestrus = 60 days → then anoestrus = 120 days
normal behaviour
small vulva
no/sparse vulva discharge
high (dioestrus) or low (anoestrus) progesterone levels
Explain the 5 Phases of the Feline Oestrus Cycle
Pro-oestrus
0-2 days
changes in behaviour, head and neck rubbing
rise in oestradoil concentration
vaginal epithelium begins cornification
Oestrus
2-9 days
receptive to mating and oestrus behaviour
peak oestradoil concentration, and LH post mating
vaginal epithelium, cornification
induced ovulation 29-40 hrs after coitus
Post-oestrus
8-10 days
follow one oestus and precedes the next when ovulation has not been induced
no CL formation, low progesterone and oestradiol conc, no sex
Dioestrus
40-60 days
ovulation induced (pregnant = 60days, pesudopregnant = 40 days)
CL formation and high levels of progesterone
Anoestrus
30-90 days
seasonal absence of follicle activity in late fall and winter
oestradoil and progesterone levels are base line
Clinical Signs of Oestrus in the Canine
3 Sexual Reflexes
Upward tipping or winking of vulva in response to touching dorsal vulva (muscles preparing)
Ipsilateral curvature of rear legs in response to touching skin beside vulva (leg spread for stability when mounted)
Deviation or flagging of tail in response to touch skin beside vulva (tail up or to the side)
Other Key Signs
Vulva = swollen and edema
Discharge = serosanguineous
Behaviour = attract + interested in males, flagging tail + accept mating
Clinical sings of mating and oestrous in the feline
Females
crouching, w front legs on ground
hyperextension of back / lordosis
tail to side presenting vulva
vocal and restless
during coitus = steps with hind legs
post intromission = screaming, strike at male, rolling, licking vulva
Male
tom mounts the queen and bites her neck (5-50 seconds)
step and hold her with front legs and mouth (1-10 mins)
intromission and ejaculation (1-27 seconds)
jump away to avoid queen striking him
stay close to queen
repeat 4-5 times in 30 mins
Natural Mating and Insemination of the Canine
Natural Mating = 80-100%
dependant on heat period will change what day of cycle
14 day heat = mate on day 11-13
21 day heat = mate on day 18-20
28 day heat = mate on day 25-27
limited survival of oocytes (2 days) vs long survival of sperm in female (7-9 days)
use oestrous behaviour w caution
ideally vaginal cytology, speculum exam, changes in vaginal mucus, follicle growth (measure on US), serum hormone concentration (LH and progesterone)
Insemination = 55-75%
Intra-vaginal insemination = fresh semen
Intra-uterine insemination = frozen thawed semen
palpation (catheter), endoscope or laparoscopic (surgery)
Ovulation and Breeding of Felines
Induced Ovulation - Voitus
LH released from pituitary within minutes
ovulation induced 24-48 hours after coitus
factors affecting LH surge
oestrogen espoure
multiple mating copulations
fertility - 2-3 first days of oestrus
pheromones and experience of sexual partner
Natural Breeding
territorial = oesterous queen is brough to the tom
photoperiod = more than 14 hours of light per day
mating
active fertile male can service 15-20 at a time
sexual preferences
behavioural problems
Insemination
AI with fresh or frozen semen - intravaginal or interuterine
not common in felines as its hard to collect and induce
Pregnancy Diagnosis Methodology for Canine and Felines
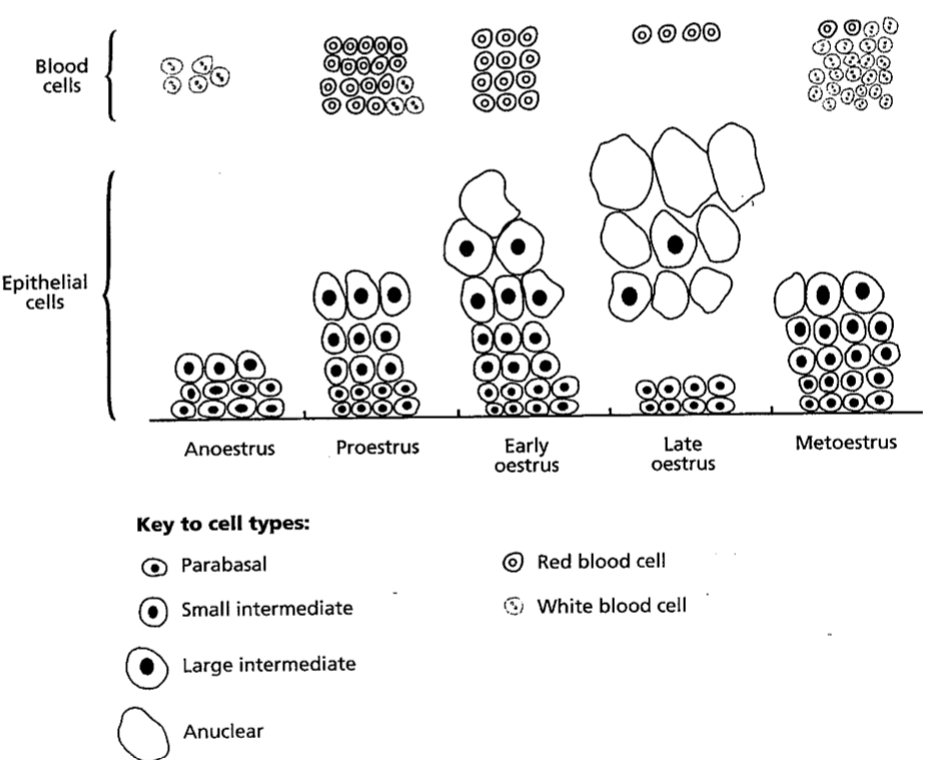
Vaginal Cytology (ideal)
increased oestrogen
proliferation/ increase/ thickening of epithelium in vagina (dark purple on histology)
pre-oestrus = more para basal, small intermediate and RBC
oestrus = more large intermediate + anuclear keratinised cell
anoestrus = more neutrophils to help clean out vagina
10-15 cm into vagina, hold down + point up to avoid urethra
roll swab over microscope slide 3-4 times, air dry → stain w Diff-quick or Wright-Giemsa → air dry
easy and cheap but needs to be repeated to monitor level of oestrogen (not ovulation) different for each bitch
Serum Hormone Concentrations (ideal)
LH peak duration <24 hrs
ovulation +2 → fertility max 0-5 days
measure 8-12 hours from proestrus until peak
Progesterone increase duration preovulatory and ongoing
ovulation 4-10 ng/ml → dioestrus >10 ng/ml
measure every day/second day in oestrus
Vaginoscopy
endoscopic observation - speculum, vaginoscope, optical endoscope
examination of vagina - profile/colour of mucosal folds + discharge
think but pale = oestrus vs thin, pink, moist = dioestrus
Follicle Growth
ultrasonography examination of right ovary - 5-7 mm
Explain the Copulation Tie in Canines
Intromission = 1-2 mins
ejaculation of 1st semen
engorgement of bulbus glandis and thrusting pelvic movement
ejaculation of 2nd semen (sperm rich)
The Turn = 2-5 seconds
the dog dismounts and turns (penis still inside)
Copulation Tie = 5-45 mins
bent penis = locking by the engorged bulbus
no drainage and high pressure
ejaculation of 3rd semen
flushes sperm rich into uterus (prevents falling out)
Gestation of Canine vs Feline
Canine Gestation
from LH peak = 64-66 days
from ovulation = 62-64 days
from cytologic dioestrus = 56-58 days
from mating to parturition = 57-72 days
hormones, progesterone (CL function) and relaxin (placenta function)
Feline Pregnancy
Pregnancy from mating = 63-65 days (53-74)
Implantation = 12-13 days after ovulation
Placenta will have brown boarders (not green from bile like canine)
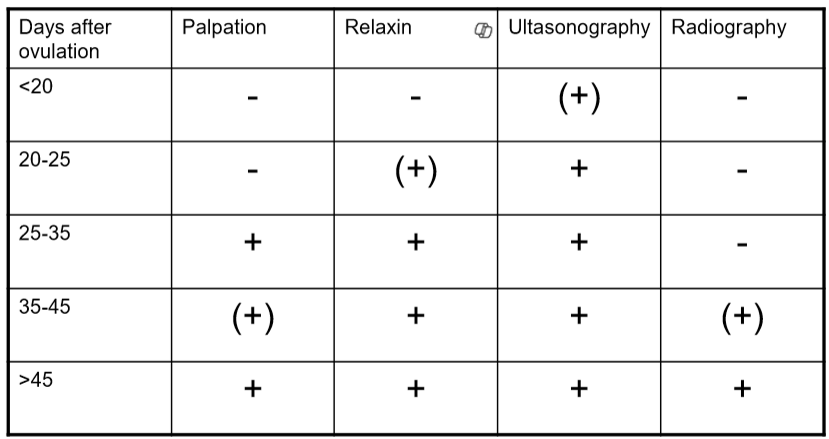
Determining a Pregnant Bitch or Queen
Detecting Pregnancy
Palpation + clinical signs
nipple enlarges + mammary develop
change body shape and weight
enlargement + palpate foetus
**from LH peak = 22-25 days
**from ovulation = 17-22 days
Hormone measurements
Relaxin assay (in house serology)
**from LH peak = 20-29 days
**from ovulation = 18-24 days
Ultrasonography
Embryonic vesicle D16, placenta D18 and embryo D22
**from LH peak = 19-22 days
**from ovulation = 18-19 days
Radiography
foetal skeletal D45 - number of foetuses and dystocia
only do x1 per litter
**from LH peak = 44-46 days
**from ovulation = 41-43 days
Explain normal parturition
Week Before
potential milk from mammary
dilation of vulva and pelvis ligament s
week inconsistent uterus contractions
Day Before
nesting behaviour
relaxing of cervix + loos cervix mucous
decrease temp
decreased progesterone
Stage 1 of Parturition
6-12 hours
cervical relaxation and dilation
restless, nervous, anorexia, shiver but panting
temp and progesterone rise
Stage 2 of Parturition
6-24 hours
birth of pups/kittens
cervix fully open, strong contractions, licking vulva
takes 1-2 mins per neonate, then 5-60 mins rest before next one
Stage 3 of Parturition
5-15 mins
expulsion of placentas
following each pup or every second (each uterine horn)
allow her to clean pups/kittens
Thermoregulation - unable to maintain temp
Carbohydrate regulation - hard to maintain blood glucose, so ensure feeding from mum or give formula
Parturition Differences Canine vs Feline
Canine | Feline |
|
|
|
|
Abnormal births and went to interfere
dependant on duration of birth
health of bitch
number of pups left in uterus
appearance of discharge (normal is green from bile / placenta)
maternal forces and contractions
straining due to pain or abnormal positions
no whelping
pausing for more than 2-4 hours between pups or kittens
symptoms of intoxication
What is the general approach to a skin case consult?
History
signalment
main concern - when? change over time? seasonal?
what treatments have been tried so far? did they help?
any current medications or parasite prevention?
what is the diet + environment? has this changed?
Physical Exam
Distant = itching? coat quality? obvious lesions? bilaterally symmetrical or are they focal?
methodical search over skin = face, neck, limps, dorsum, ventrum, peri-anal, tail
any parasites? use a flea comb to see fleas or flea dirt
Describe lesion morphology
location and distribution
number of lesions
size and appearance - colour, texture, shape
lumps - subcutaneous or cutaneous?
Diagnostic testing
skin cytology - impression, fine needle aspirate or trichogram
skin scraping - superficial or deep
wood’s lamp test - uses ultraviolent light to see ringworm
fungal culture
laboratory culture - fungal or bacterial
skin biopsy - histopathology or culture
referral for intradermal skin testing
Treatment
if diagnosis = target aetiology
no diagnosis = symptomatic management
Re-assesment
have clients concerns resolved?
is it improvement based on your judgement?
adjust treatment as required
What are the types of skin lesions?
Pruritus = itching, biting, licking, scratching or rubbing (30-40%)
Alopecia = absence of hair, localised, mutli-focal, symmetrical or generalised. May be due to self trauma or abnormal hair follicles
Wheals/hives/urticaria = small oedematous, raised lesions, allergy
Pigmentary change = disruption of melanin pigment, eg post shave, hypopigmentation (reduced) or hyperpigmentation (increased)
Rashes = erythema (red) or papules (pimple), localised inflammation
Scaling = superficial accumulation of loose skin on epidermis surface
Crusting = scales + exudate like blood, serum or pus on surface
Erosion = partial loss of epidermis, intact basement membrane, superficial
Ulceration = loss of epidermis, exposure of dermis, deep lesion
Lichenification = thickening of skin with chronic inflammation
Hyperkeratosis = keratin deposits on nose, paw pads, thick + hard
Masses = inflammatory papules pustules or abscesses or neoplastic
“People always wonder, please rescue cute elephants under large hazy mountains”
What is an allergic skin disease?
Type I Hypersensitivity reactions = foreign substance with IgE immunoglobulins
Type IV Hypersensitive reactions = contact allergies
History clues = breed, age (most star 1-3rs), duration/ seasonal, response to steroids
Clinical clues = pruritus (most common), recurrent secondary infections, lesion distribution
Describe common the x4 patterns of common cat allergies
Head and neck pruritus = localised, pruritic with erosive lesions
Miliary dermatitis = multi-focal pinpoint papules (can be felt), pruritic rash that spreads and becomes scabby
Eosinophilic granuloma complex
Plaque = well-defines, raised, red, on ventrum/thighs, itchy
Granuloma = raised, circular, yellow-pink, on head/thighs
Ulcer = well-defined, red skin ulcers, lip, not painful or itchy
Symmetrical / non-inflammatory alopecia = self trauma
Causes of common allergies
Flea Allergy Dermatitis
most common in dogs at base of tail
Diagnosis
wet paper towel or cotton wool → flea dirt will stain brown
intradermal testing - confirms reactivity to flea antigens
response to therapy
Treatment - compliance!
Insect Growth Regulatory = Sentinel
Adulticides (kills adults) = Nexgard, Bravecto, Seresto collar
Repellent to stop flea landing = Seresto collar
treat all animals in house
clean environment, wash bedding, remove organic debris
Mosquito Bite Hypersensitivity
most common in cats
scaling, crusting, alopecia on nose and ears
symptomatic treatment as for flea bite
Contact Allergy
most common in dogs, rare in cats
Type IV hypersensitivity response (cell mediated, not antibody mediated) due to direct contact w irritant, non-haired usually
Usually caused by plants, or chemicals
Diagnosis
contact elimination trial = eliminate for 10 days and observe for another 10 days
patch test = exposure in marked skin patches
Treatment
prevent contact with known irritants or remove asap
medical intervention - steroidal anti-inflammatories
Atopic Dermatitis
most common is pruritus and erythema on face, ears, perianal, paws, ventrum → saliva staining or secondary infections
genetically predisposed allergic dermatitis with complex interactions with enviro, microbes, genetics and immunological factors
Diagnosis
exclude parasites, infections, contact or food allergy
intradermal skin testing as blebs under skin → wheals
Treatment
modify patient response by managing secondary infections
need to cytology to diagnose organism → use antimicrobial
desensitisation treatment = subcut inj weekly then monthly
promoting skin barrier w Omega 5+6, regular baths/shampoo, prevent self-trauma
life long management
Food Allergy
immunological (true hypersensitivity) or non-immunological (food intolerance)
signs = pruritus and or gastrointestinal abnormalities, no seasonal
usually due to beef, chicken, wheat and lamb
elimination diet trial = novel protein and carbohydrate for 6-12 weeks
rechallenge trial = if symptoms improve, can reintroduce x1 protein at a time and monitor
long term commitment, takes time to see improvements
Causes of infectious skin disease?
Bacterial pyoderma
normal skin commensal bacteria in high numbers/overgrowth usually secondary to underlying allergy or disease
scales, epidermal collaretttes, pustule lesions and/or discharge
Diagnosis = cytology impression under microscope or swab to lab
Treatment = shampoo, amoxycalv antibiotic, caphalexin tablet or neocort anti-inflam cream
Fungal pyoderma
normal skin commensal fungal yeast in high numbers/overgrowth usually secondary to underlying disease
scales, greasy skin exudate, if chronic can be lichenified + discharge
Diagnosis = cytology impression under microscope
Treatment = shampoo, PMP ear suspension, fluconazole tablet, or fungafite cream
Dermatophytosis (ringworm)
fungal infection of the hair shaft creating round pruritic lesions
zoonotic infection
Diagnosis = trichogram (may show fungal spores), woods lamp (UV light) or fungal culture from hair plucked
Mites
Demodex cani and Demodex cati = non-contagious overgrowth due to immunocompromise
Sarcoptes scabei = infectious and zoonotic
Diagnosis = skin scrape (demodex = deep, scabies = superficial)
Treatment = parasite prevention and/or treat underlying immunocompromising disease
Otitis externa (bacterial or fungal)
many predisposing factors = conformation/genetics, moisture, parasites, allergy, foreign bodies, yeast and bacteria
Diagnose = cytology to see bacteria, vs yeast vs parasites OR otoscopic exam to see foreign material
Treatment = ear cleaning to reduce debris and biofilm, antimicrobials, reduce bacteria and fungal numbers
How to treat unknown ‘lumps and bumps’ in dermatology?
History
when first noticed? grown? appearance change?
every had a lump before? was it diagnosed?
is it bothering patient?
history of trauma like cuts or sun bath
Examination
location - cutaneous or subcutaneous
texture - soft/firm/hard, regular/irregular, mobile/non-mobile
surface - ulcerated or pigmented
number - singular or multiple
inflammation - local or systemic
lymph nodes - palpate for enlargement
Diagnosis
final needle aspirate to sample cells under microscope
biopsy = incisional (part of) or excisional (whole) mass → lab
inflammatory vs neoplastic
benign tumours = lipomas, sebaceous cyst, keratin cyst, histiocytoma
malignant tumours = mast cell, plasma cell or lymphoma