GI System
1/509
Earn XP
Description and Tags
Year 1 - Normal Animal
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
510 Terms
prehension
movement of food into the oral cavity so that digestion can begin
mastication
the process of chewing
excretion
getting rid of waste that has been absorbed into the body
egestion
getting rid of waste from ingested food before it is absorbed into the body
why is phosphate found in saliva in ruminants?
it acts as a buffer and provides a source of microbes
substances that can be found in saliva
mucin (lubrication), amylase, bicarbonate (neutralisation/buffering), phosphate, lysozyme and antibodies (reduce infection), protein-binding tannins, urea
2 types of salivary reflex pathways
congenital/innate and conditioned/learned
4 principle types of contraction of the GI tract
segmental, peristaltic, anti-peristaltic, mass movement
segmental contraction
mechanical contraction to break down and mix ingesta without moving it
peristaltic contraction
contractions which allow the movement of food in an aboral direction at a rate that allows sufficient time for digestion and absorption
anti-peristaltic contraction
contraction which allows movement of food in an oral direction to slow down transit of digesta or to alow rumination or vomiting
mass movement
more extended and stronger contraction to empty a certain part of the GI tract
layers of the abdominal wall
skin (often insulated with hair), superficial fascia of adipose and cutaneous trunci muscle, deep fascia (in ox & horse), muscles
muscles of the abdominal wall
external abdominal oblique, internal abdominal oblique, transverse abdominal, rectus abdominis
functions of the muscles of the abdominal wall
to enclose the abdominal cavity and its contents, contraction causes increase in intra-abdominal pressure, causes increase in intra-thoracic pressure if larynx is closed
micturition
urination
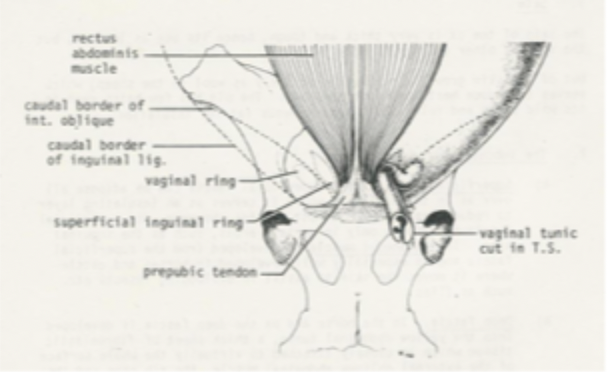
rectus abdominis muscle
straight abdominal muscle that originates on ventral surface of sternum and inserts on the cranial border of the pubis via the pre-pubic tendon, left and right sides are separated by the linea alba
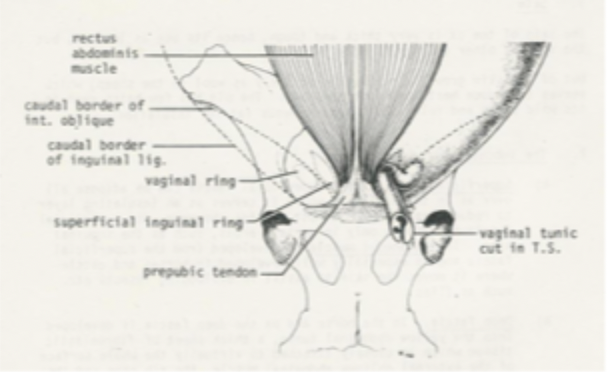

external abdominal oblique muscle
outermost lateral abdominal wall muscle which originates on lateral caudal surfaces of ribs and lumbodorsal fascia and inserts on linea alba and prepubic tendon, fibres run in a caudo-ventral direction
aponeurosis
very flat tendon
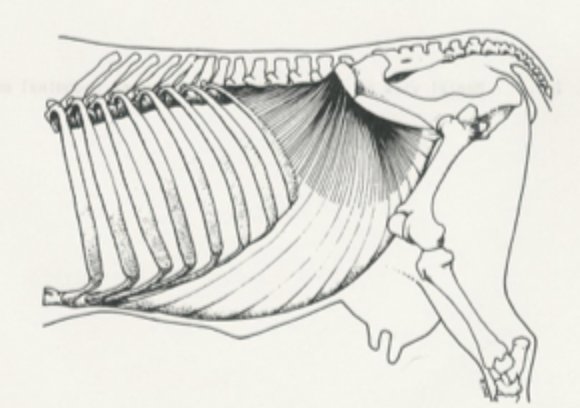
internal abdominal oblique muscle
middle lateral abdominal wall muscle which originates on coxal tuber and lumbodorsal fascia and inserts on linea alba, last rib and cartilages of caudal ribs, fibres run in a cranio-ventral direction
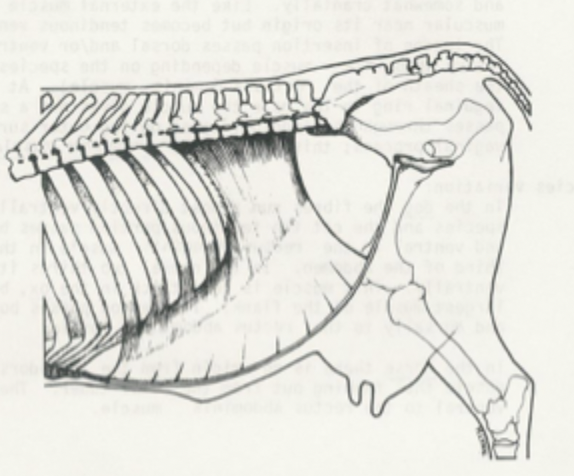
transverse abdominal muscle
innermost lateral abdominal wall muscle which originates on medial surfaces of ventral parts of caudal ribs and deep lumbodorsal fascia and inserts on linea alba, fibres run transversely
what is the sheath of rectus abdominis muscle formed of?
tendons of the lateral abdominal wall muscles
3 branches of ventral roots
medial, lateral, lateral cutaneous
inguinal canal
potential space between deep inguinal ring (gap in internal oblique muscle) and superficial inguinal ring (slit in external oblique muscle) which provides a pathway for the spermatic cord and round ligament from the abdomen to the external genitalia
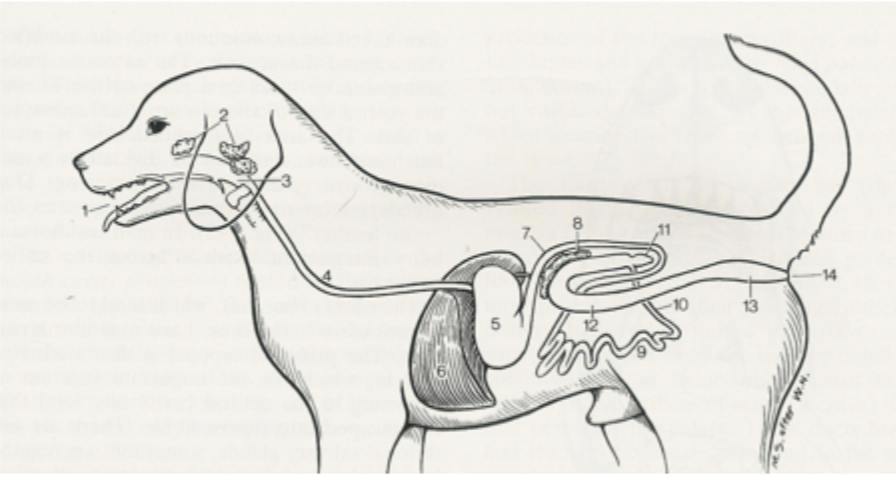
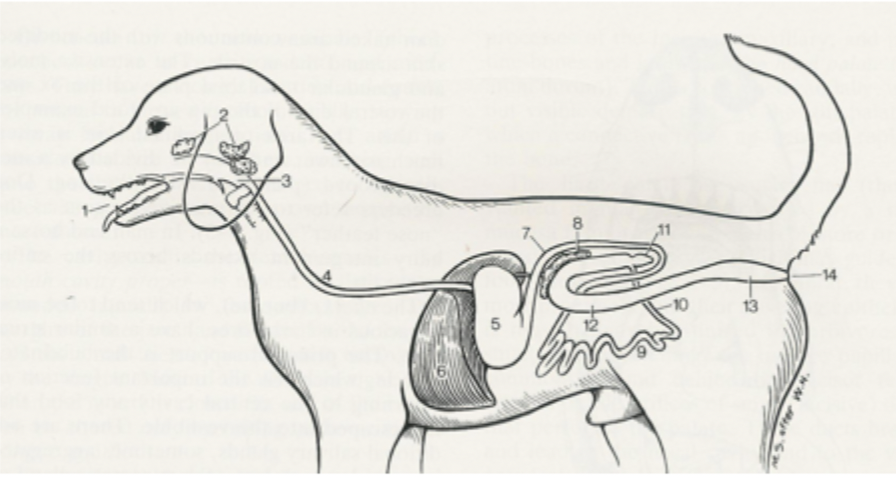
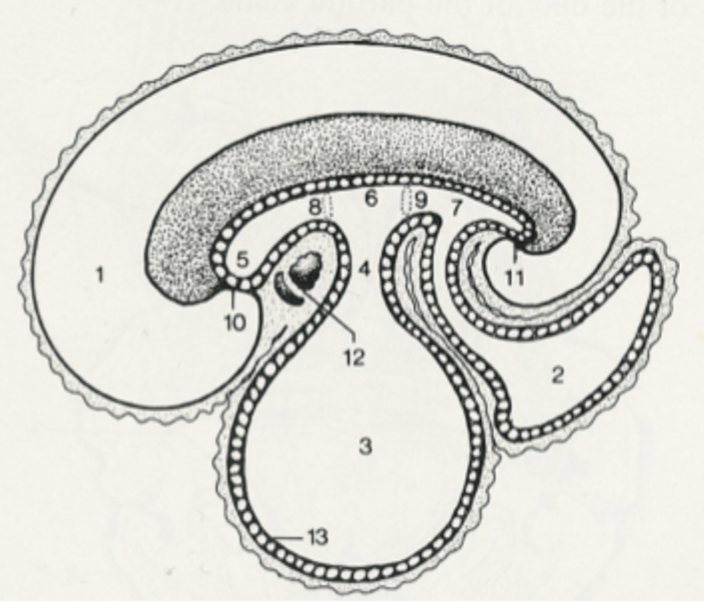
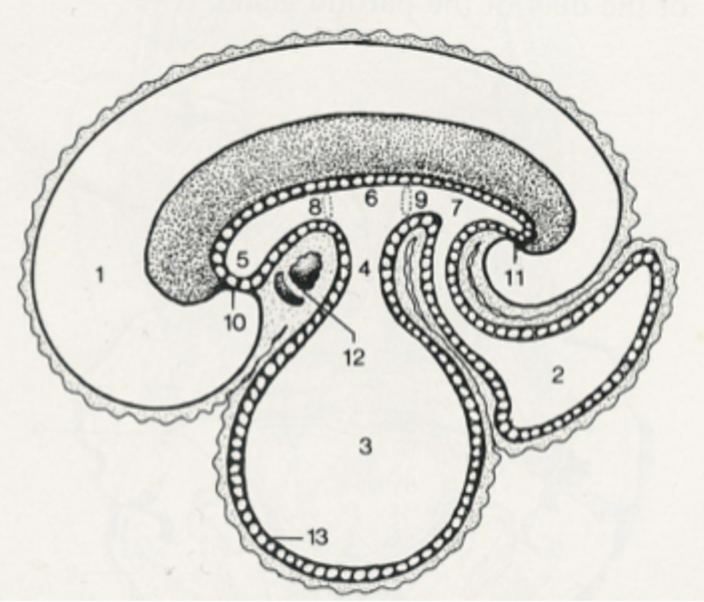
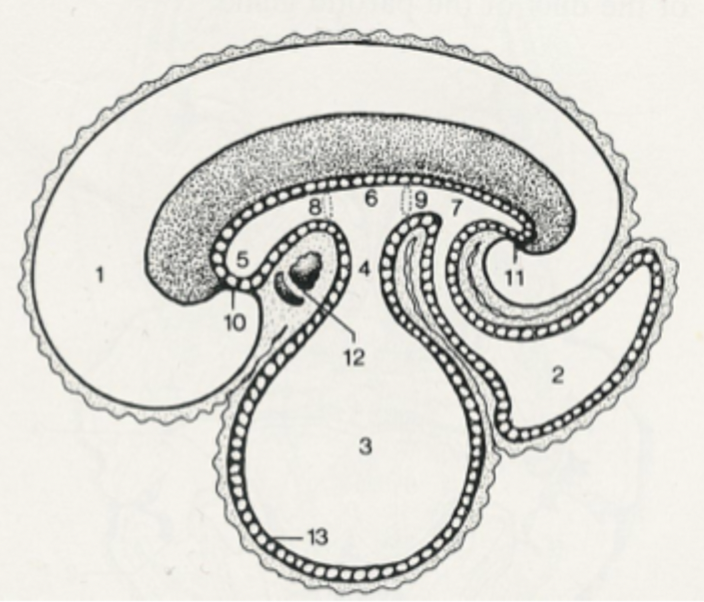
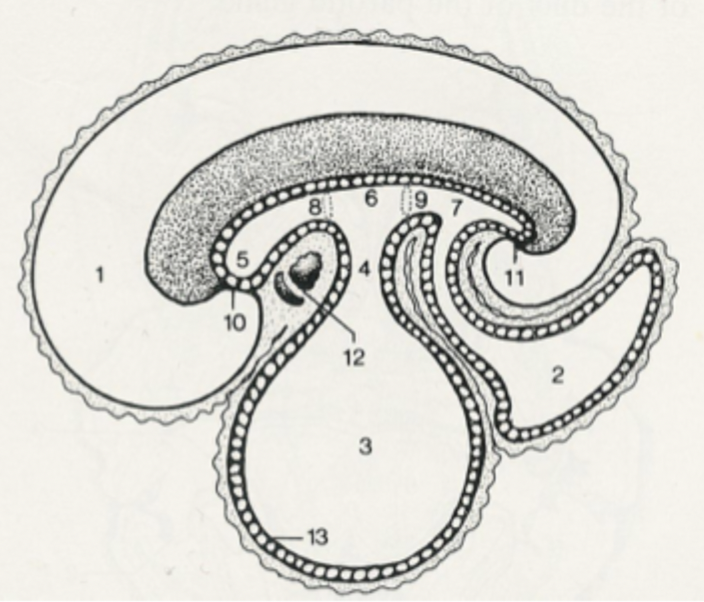
2
salivary glands
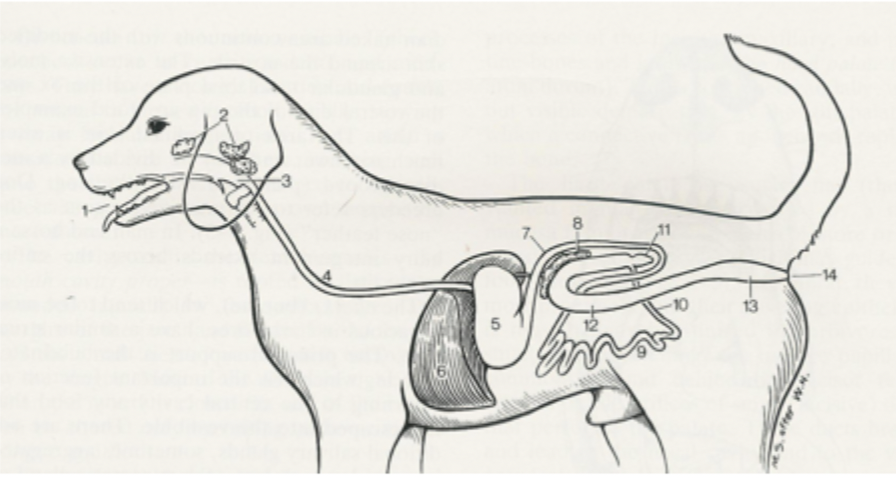
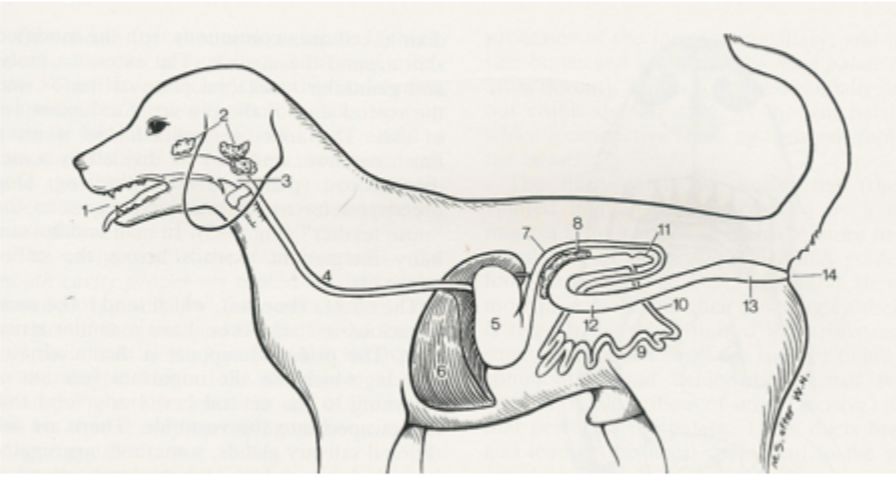
3
pharynx
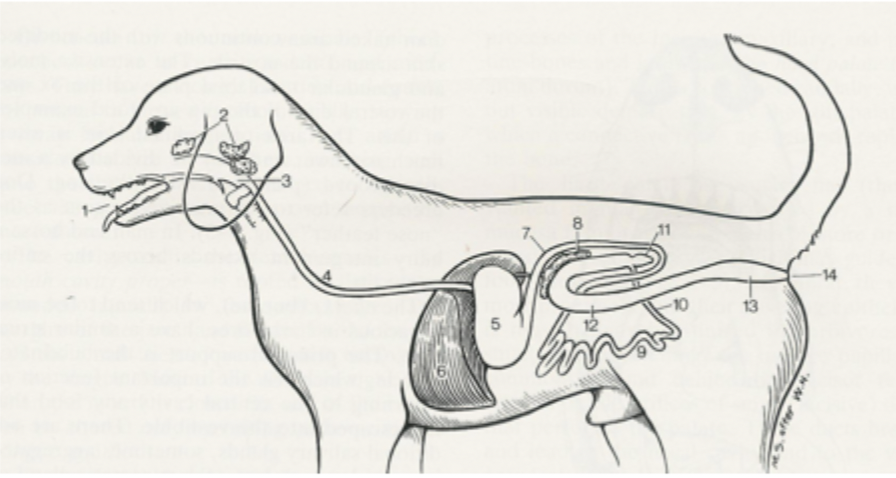
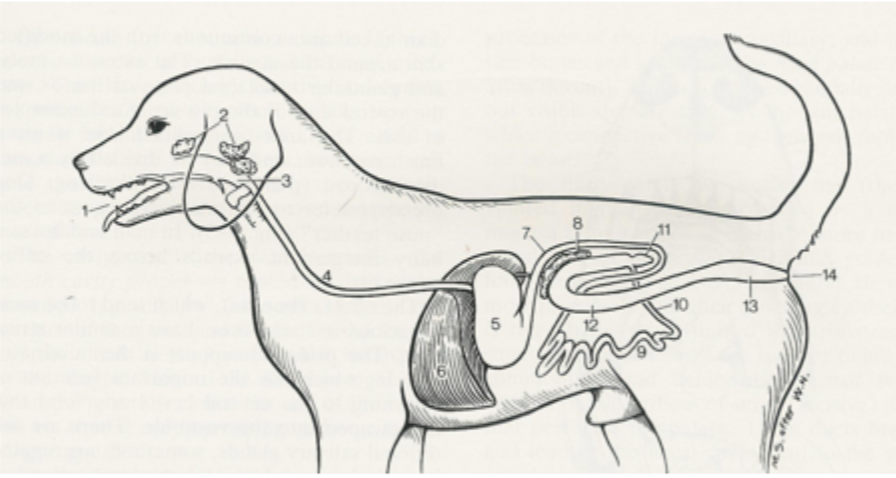
4
oesophagus
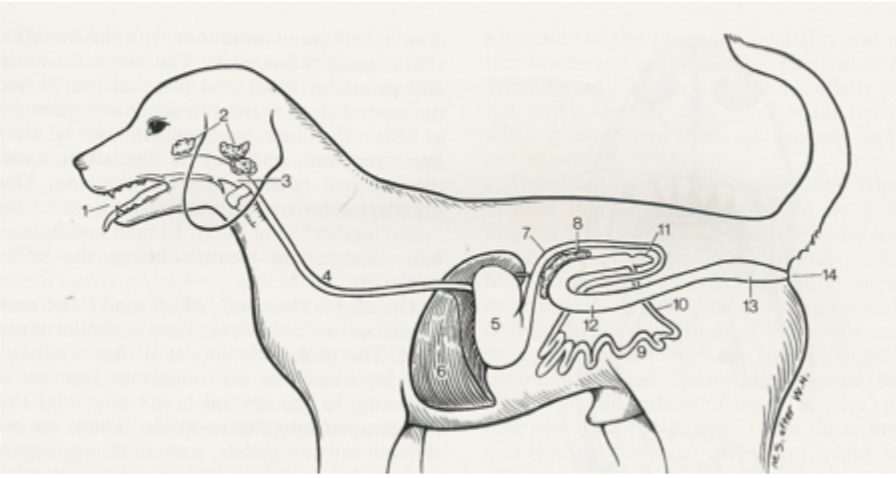
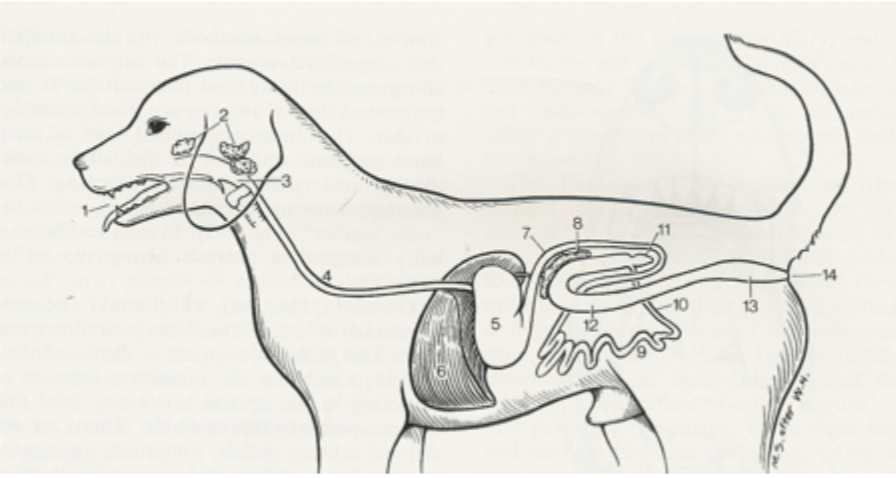
5
stomach
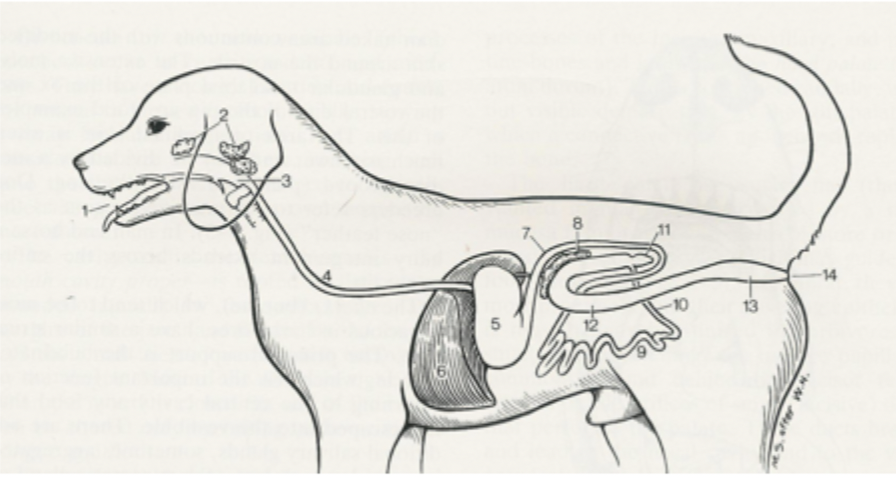
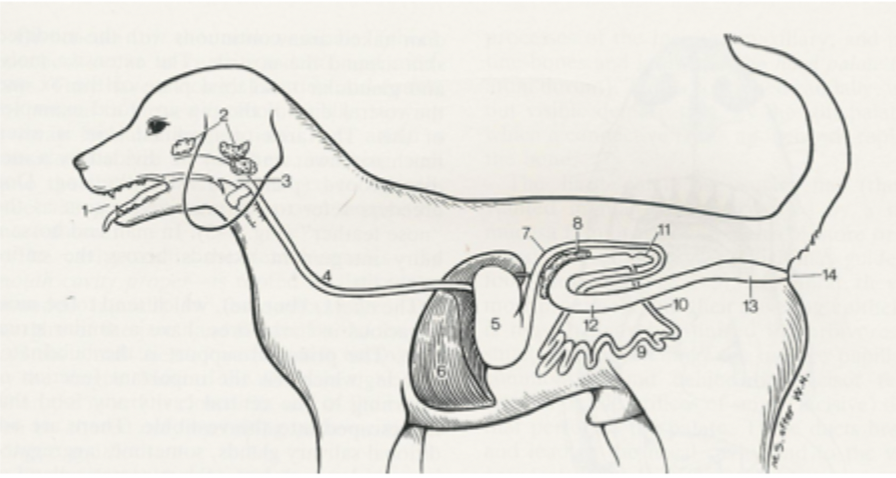
6
liver
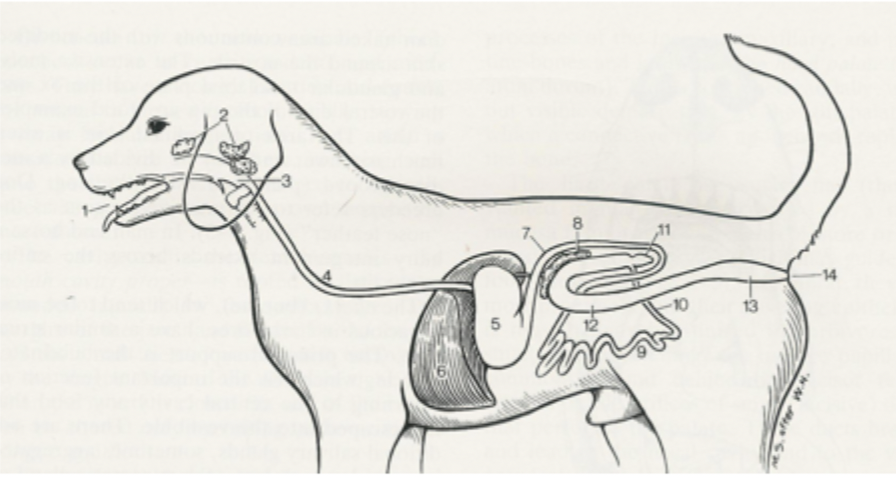

7
duodenum
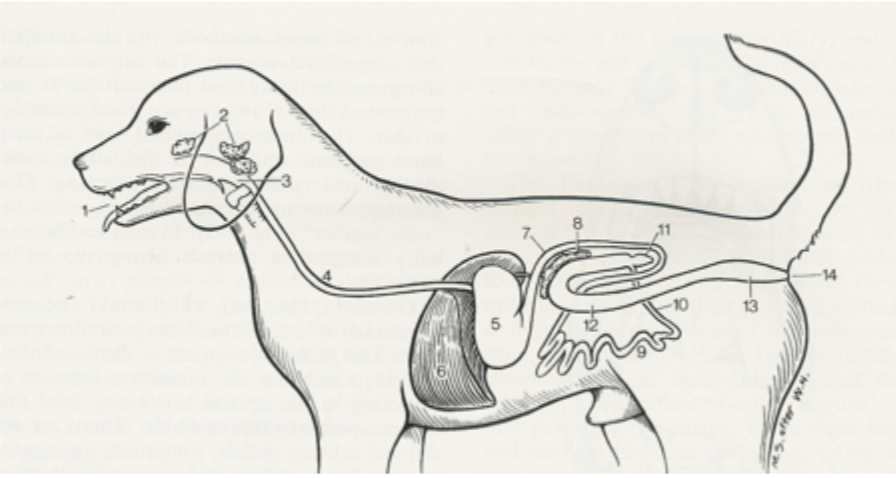
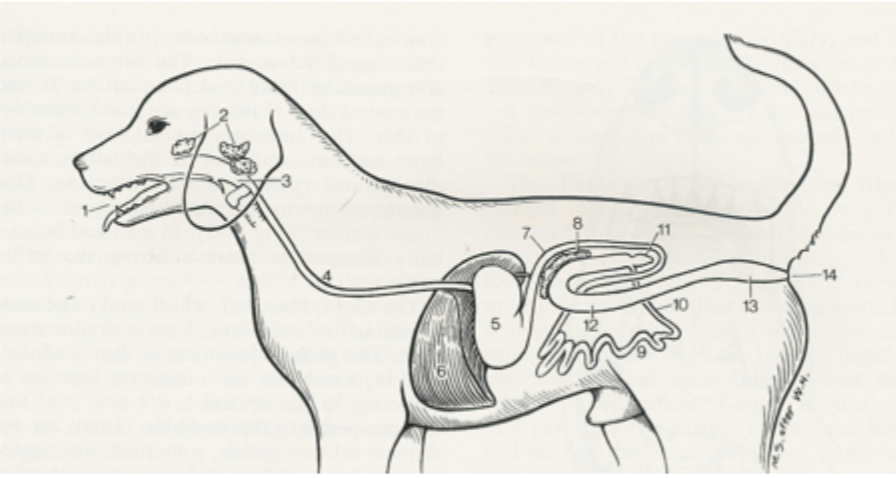
8
pancreas
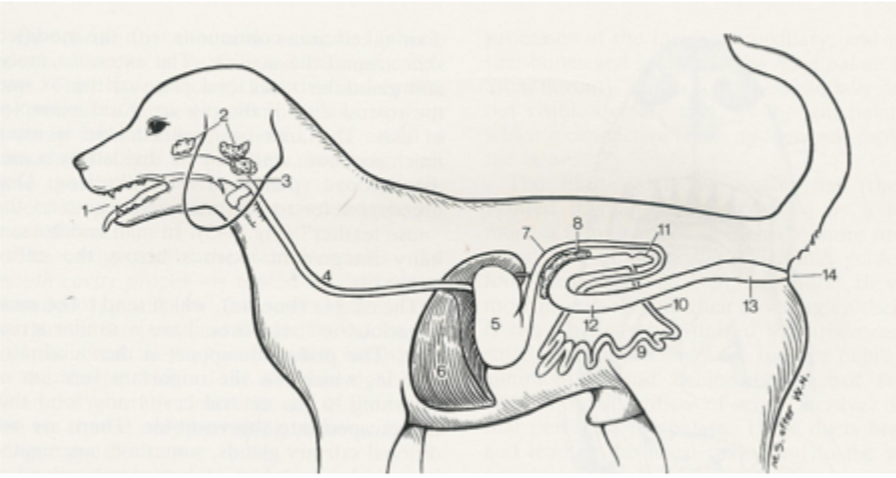

9
jejunum
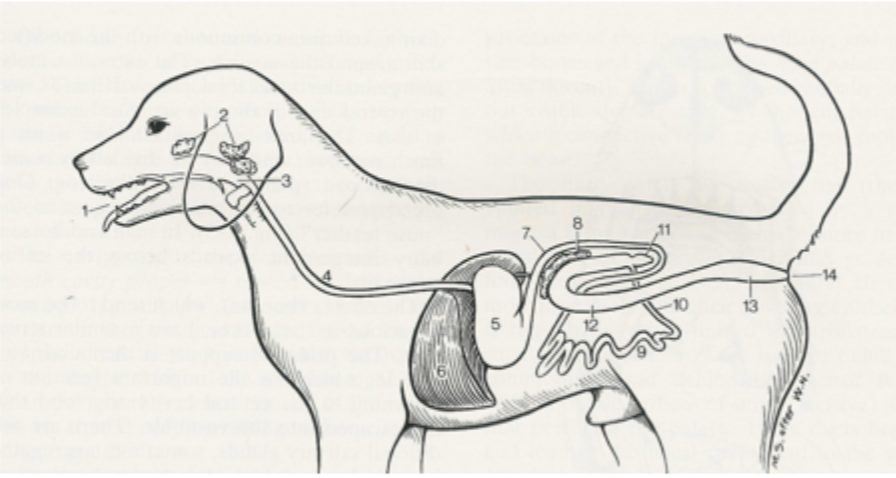
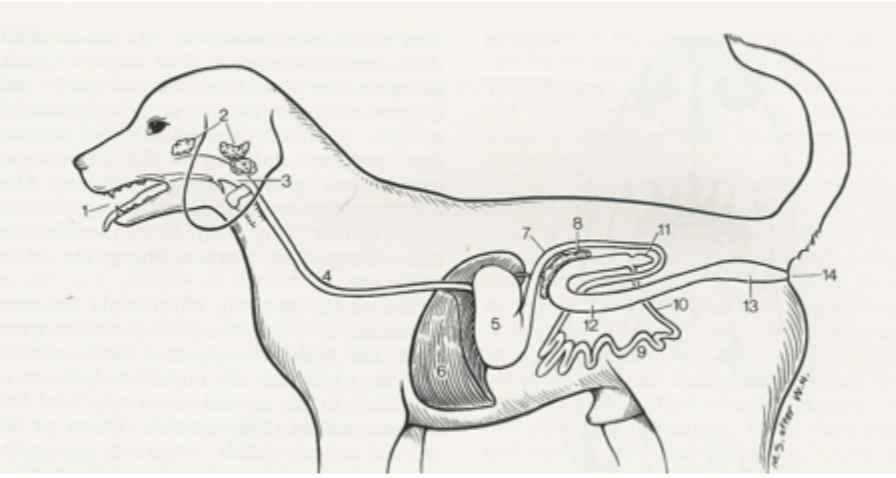
10
ileum
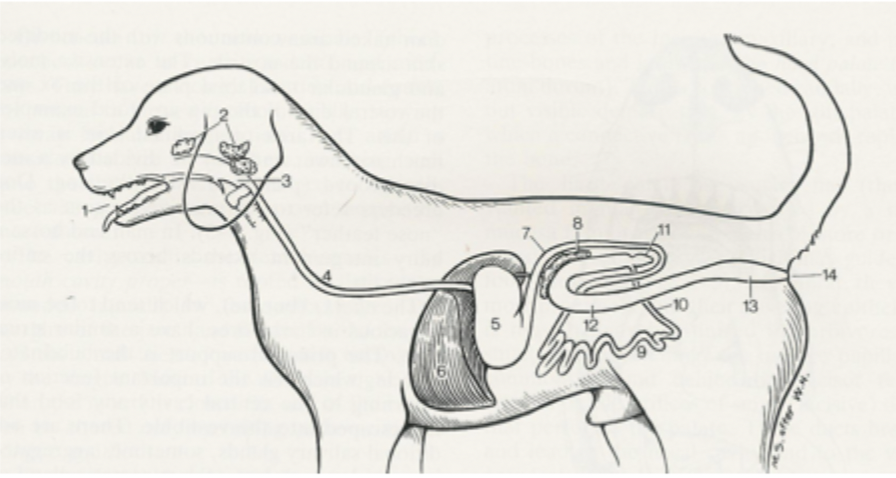

11
caecum

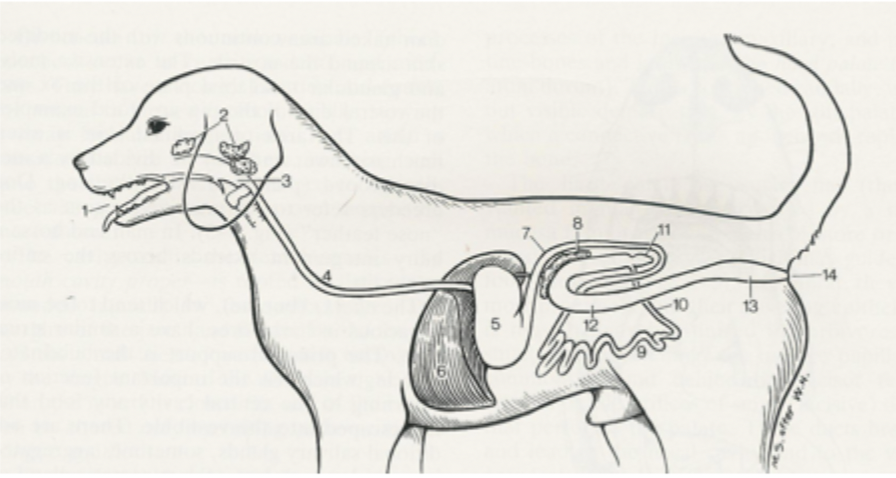
12
colon
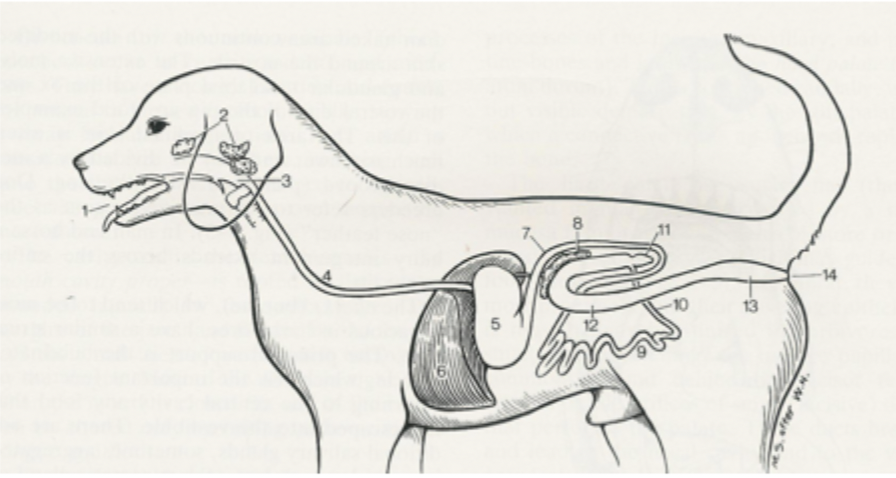
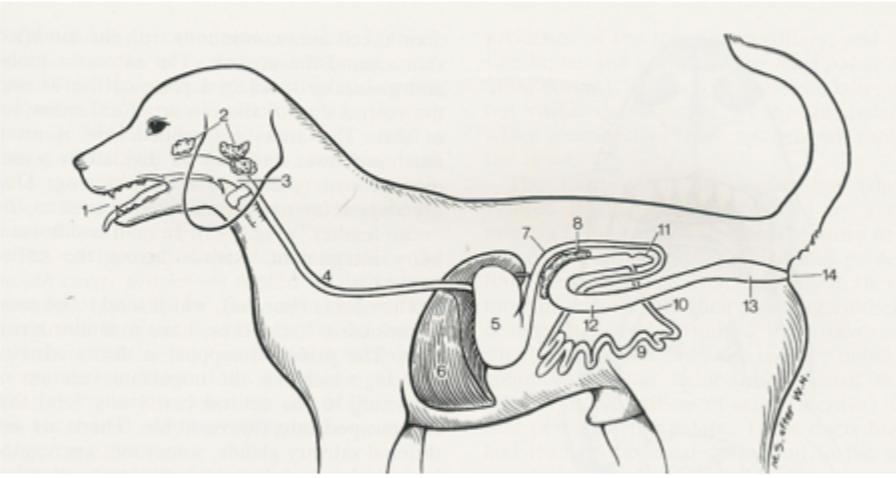
13
rectum

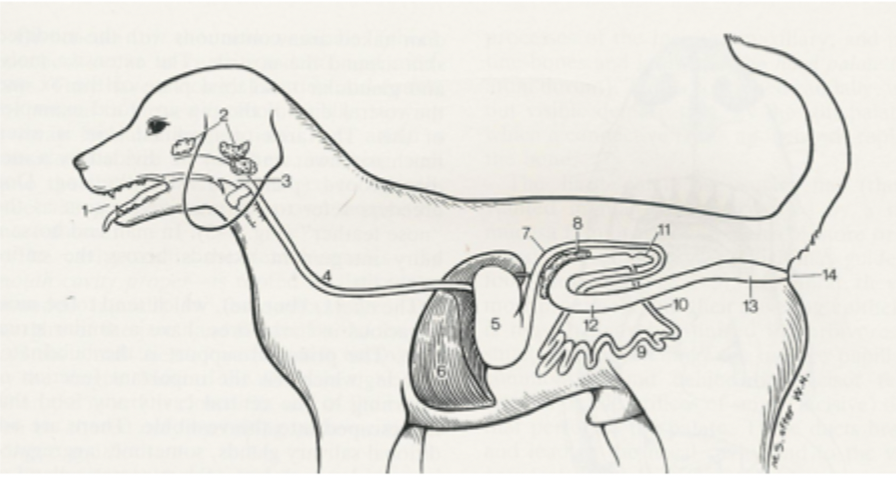
14
anus
endoderm of GI tract
epithelium lining GI tract and associated exocrine glands
splanchnic mesoderm
smooth muscle and connective tissue found in the GI tract
embryological development of GI tract
part of the yolk sac is taken into the body and goes on to form the gut
the midgut is separated from the foregut and hindgut by the cranial and caudal intestinal portals respectively
foregut ends blindly at oral plates and the hindgut ends blindly at cloacal plates
what does the foregut differentiate into?
pharynx, oesophagus, stomach, intial duodenum
what does the midgut differentiate into?
rest of duodenum, jejunum, ileum, caecum, ascending and transverse colon
what does the hindgut differentiate into?
descending colon and rectum
duodenum
first part of small intestine
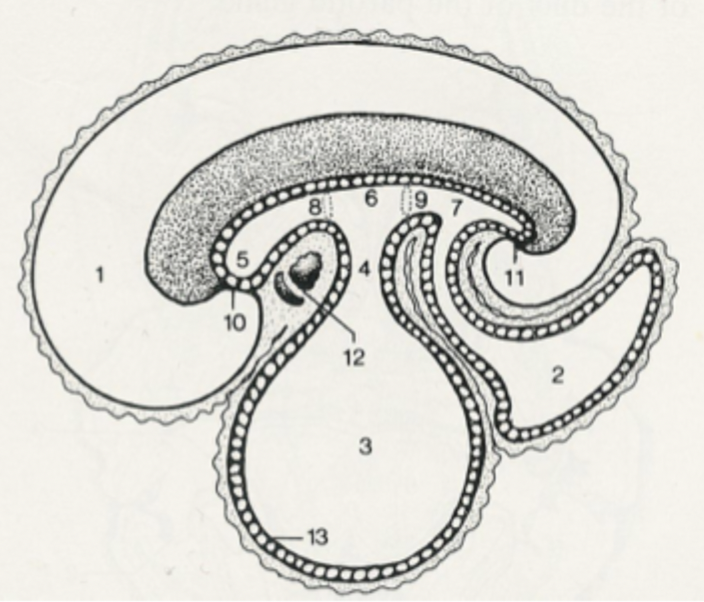
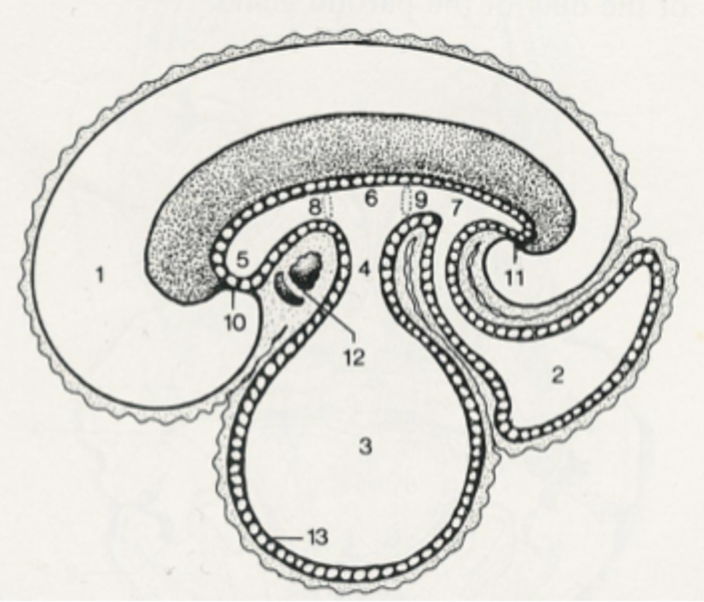
1
amniotic cavity
2
allantoic cavity
3
yolk sac

4
stalk of yolk sac
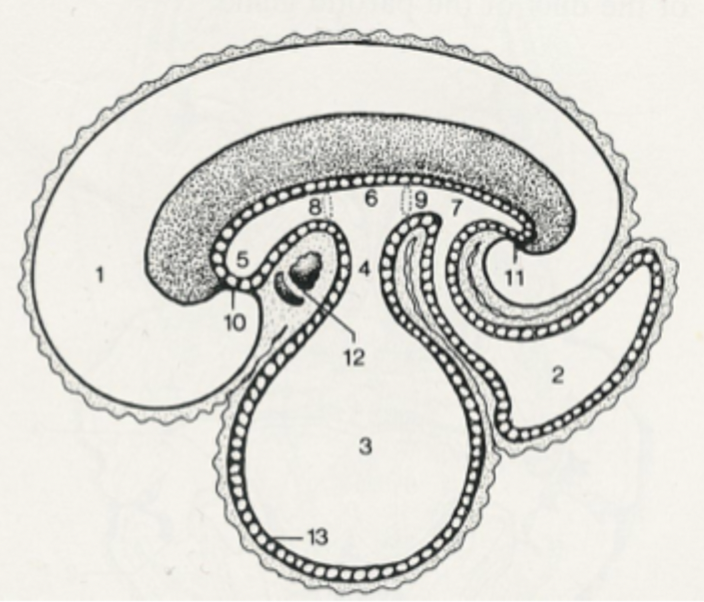
5
foregut
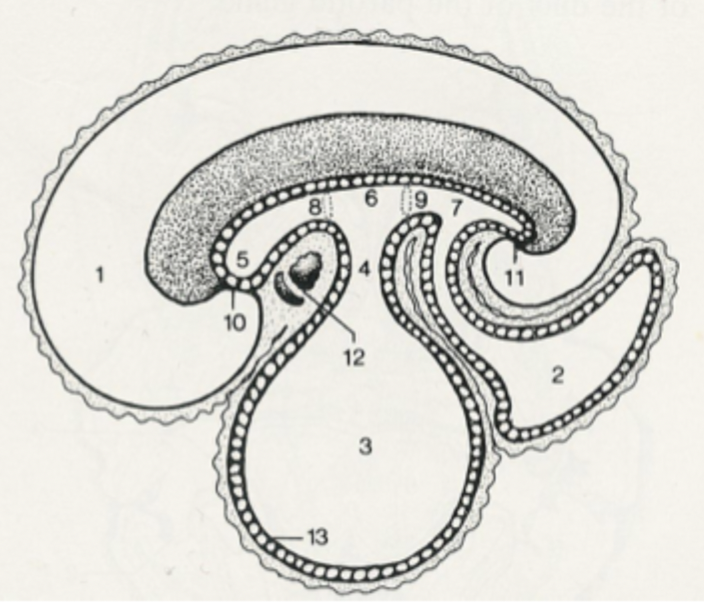
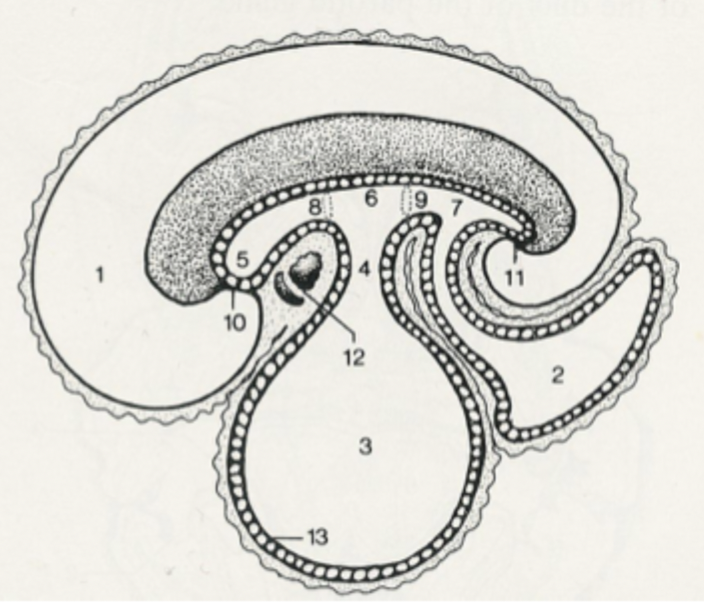
6
midgut
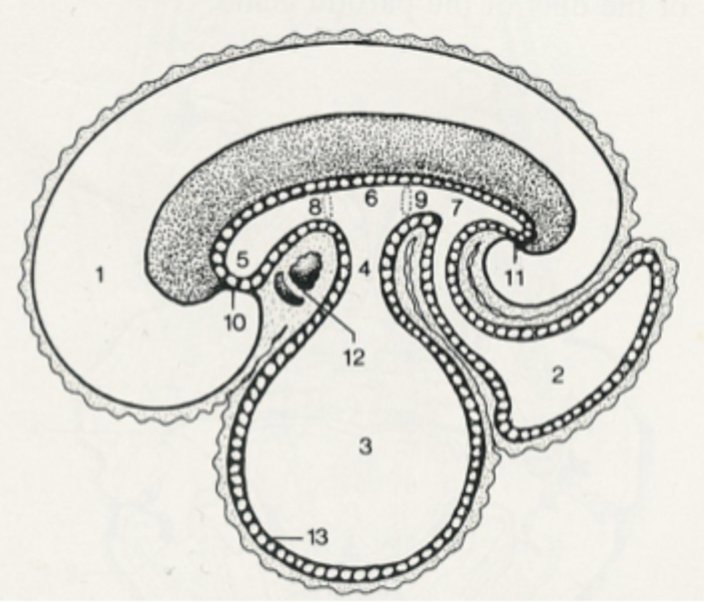
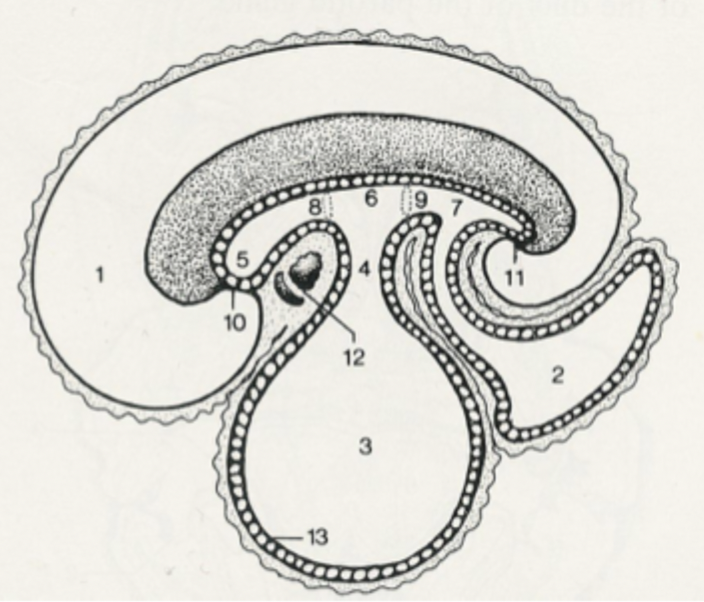
7
hindgut
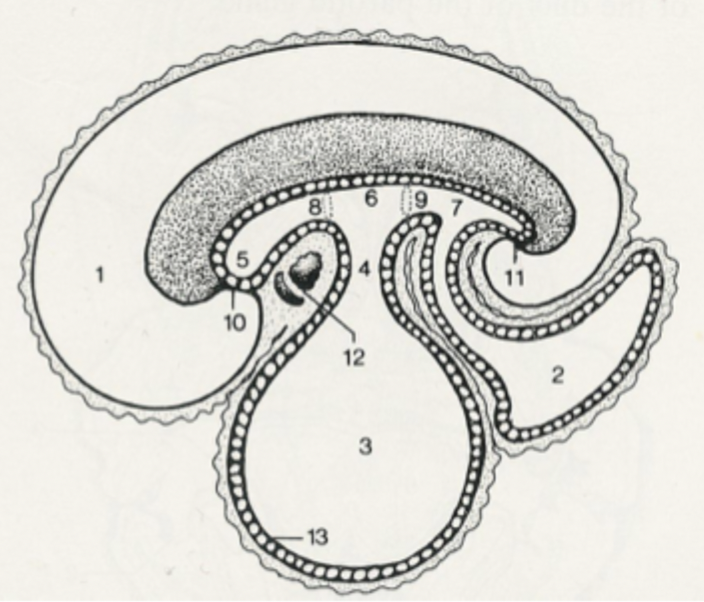
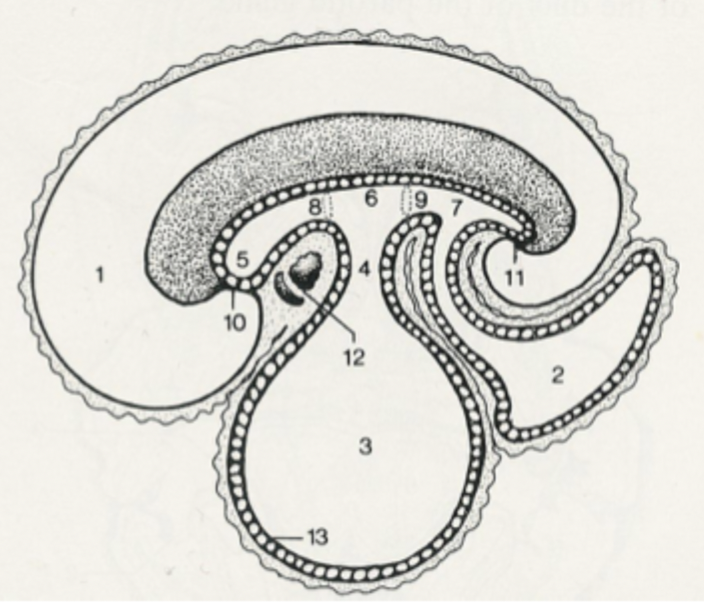
8
cranial intestinal portal
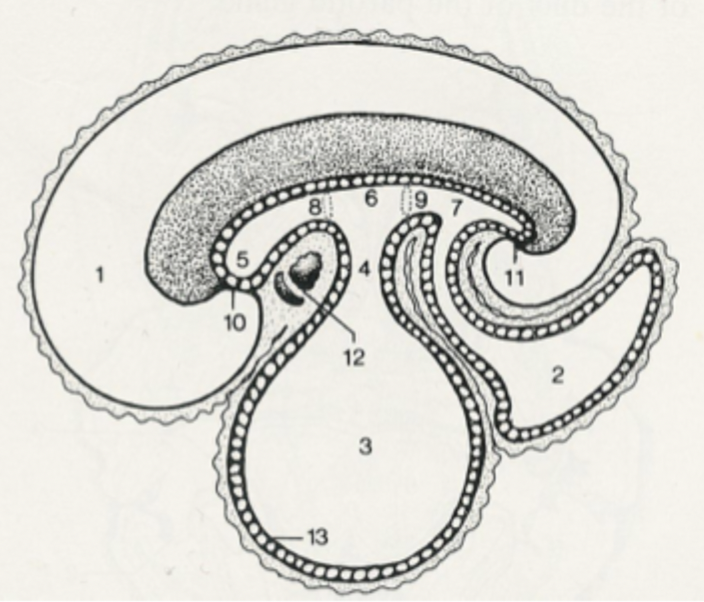
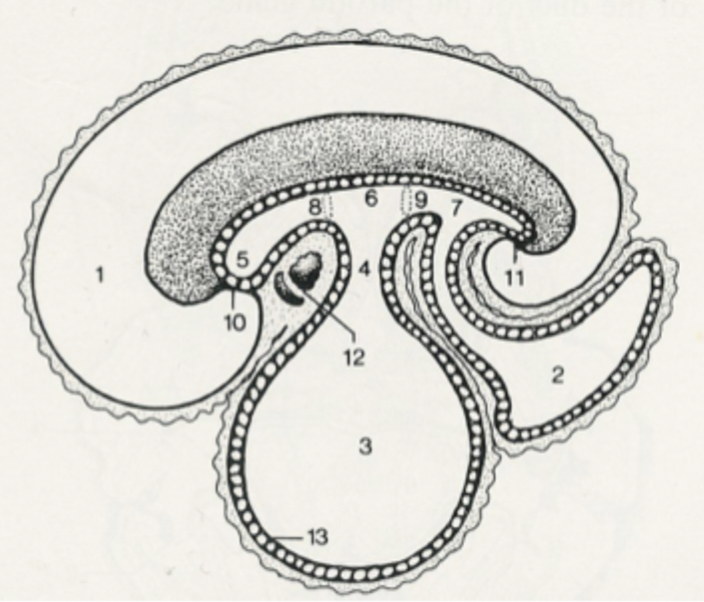
9
caudal intestinal portal
10
oral plate
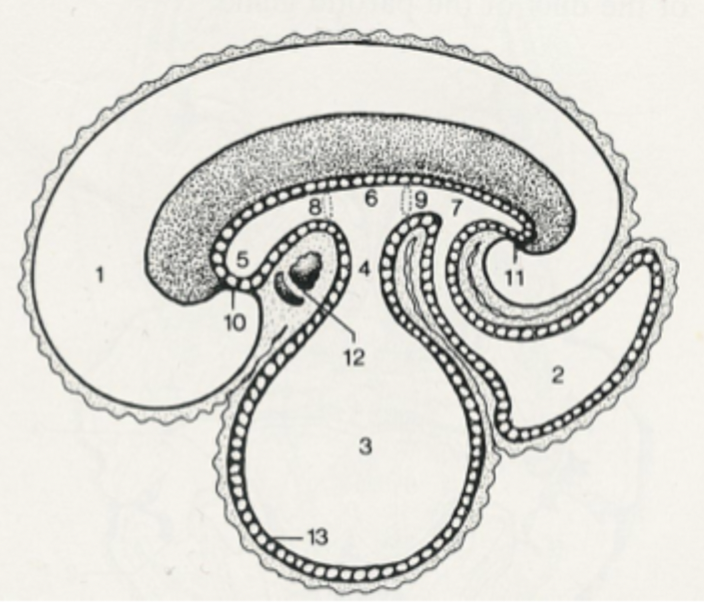
11
cloacal plate
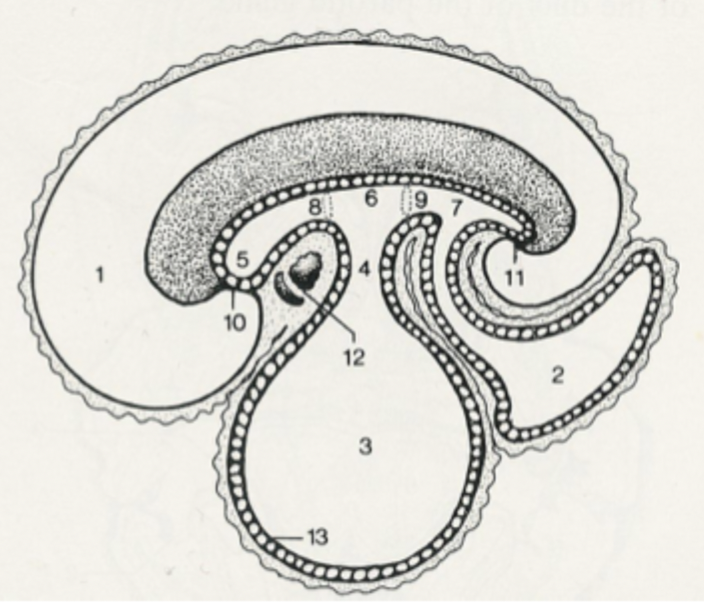
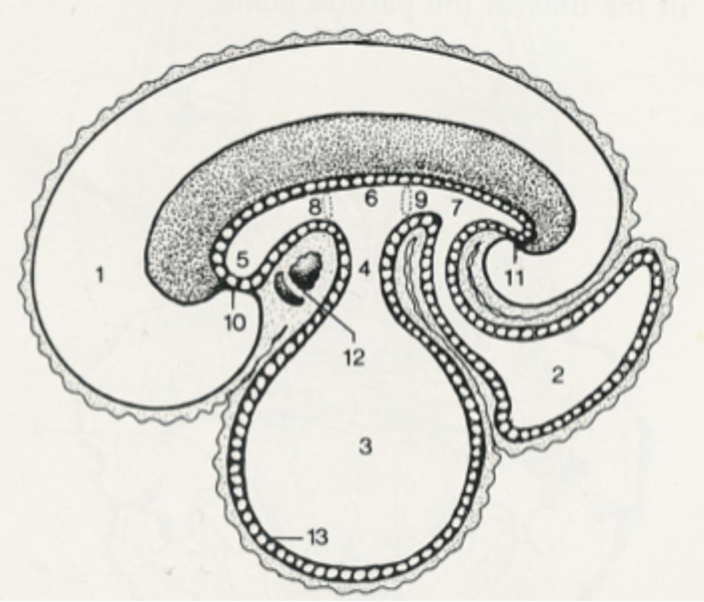
12
heart and pericardial cavity
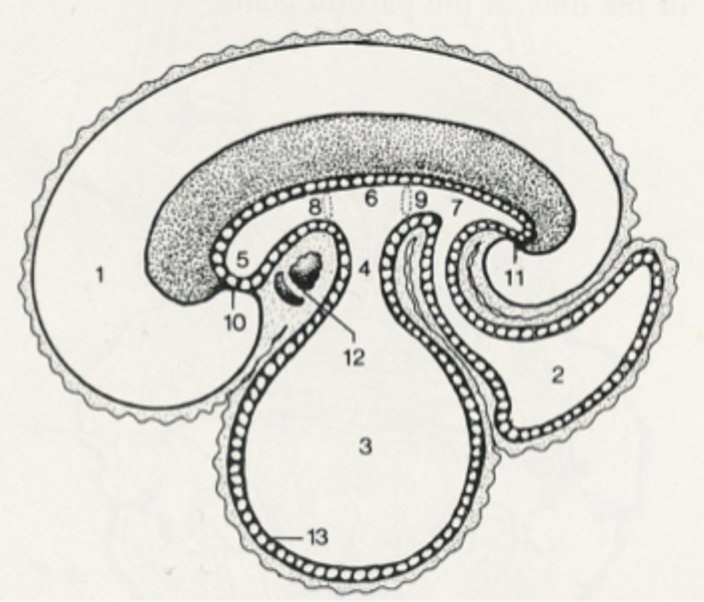

13
endoderm
process of development of the foregut
the caudal part of the foregut enlarges which identifies the stomach
the oesophagus develops from the gut tube
the stomach rotates along its longitudinal axis which brings the dorsal aspect to the left
the dorsal mesogastrium is pulled to the left
the stomach rotates along a dorsoventral axis which pulls the cranial extremity to the left and the caudal extremity to the right
part of the stomach to the left of the cardia enlarged to form the fundus
development of the liver
the endodermal diverticulum at the junction of the foregut and midgut becomes the liver which then expands caudally into the abdominal cavity
development of the pancreas
the dorsal primordia of the endodermal diverticulum becomes the left lobe of the pancreas and pancreatic duct and the ventral primordial becomes the right lobe of the pancreas and accessory pancreatic duct which eventually fuse
which vessels supply blood to the foregut?
branches of the celiac artery
development of the midgut
connection of the midgut to the yolk sac reduces to form the vitelline duct
the midgut grows rapidly causing it to hang in an elongated loop along with mesentery with extensive blood supply
rapid expansion of the liver pushes the midgut out of the abdominal cavity into the umbilical cord where it continues to develop (physiological herniation)
the cranial limb elongates rapidly to form the small intestine which rotates around its arterial axis
further rotation occurs which pulls caudal limb, caecum and ascending colon across abdomen to right side, transverse colon passes cranial to the cranial mesenteric artery
further enlargement of the abdominal cavity allows the developing midgut to return to the abdomen
development of the hindgut
rotation of the midgut brings the hindgut to the left side of the abdomen
the hindgut differentiates into the descending colon and rectum
a bud develops from the ventral part of the hindgut to form the allantois
the urorectal septum enlarges to meet the cloacal membrane which divides into 2 separate tubes
which blood vessels supply the midgut?
branches of the cranial mesenteric artery
which blood vessels supply the hindgut?
branches of the caudal mesenteric artery
peritoneum
a single continuous sheet of serous membrane that lines the abdominal cavity and envelops abdominal organs
function of the peritoneum
to support, protect and hold abdominal organs in place and provide a frictionless environment for the organs to move
layers of the peritoneum
parietal and visceral
peritoneal cavity
a potential space within the abdominal cavity located between the parietal and visceral layers of the peritoneum, which contains a lubricating fluid that allows organs to move freely
parietal peritoneum
a serous membrane that adheres to the abdominal wall
visceral peritoneum
a serous membrane with a shiny appearance that adheres to the surface of abdominal organs
mesentery connecting peritoneum location
between bowel and body wall
omentum
membrane that hangs down from the stomach, the lesser connects the stomach to the liver and the greater connects the stomach to the body wall
fold connecting peritoneum location
between bowel and bowel
topographical anatomy
the study of the relationship between organs within the abdomen
how many lobes are in the liver?
4
lobes of the liver
left and right (split into medial and lateral in dog), caudate (caudate and papillary process), quadrate
peritoneal attachments in the liver
coronary ligament, right and left triangular ligaments, falciform/round ligaments
location of coronary ligament in liver
between liver and caudal vena cava
location of triangular ligaments in the liver
between the liver and the diaphragm
location of falciform ligament in liver
between the liver and the anterior abdominal wall
round ligament
the fibrous cord remaining from the umbilical cord that runs within the free, lower edge of the falciform ligament
peritoneal attachments of the stomach
greatere and lesser momentum, gastro-splenic ligament
omental bursa
a cavity in the abdomen located behind the stomach and liver which allows the stomach to move freely and connects to the main peritoneal cavity through the epiploic foramen
peritoneal attachments of the spleen
gastro-splenic ligament (makes it quite mobile in the abdomen)
duodenum
the first part of the small intestine where the bile/pancreatic duct exits on the major duodenal papilla and the accessory duct exits on the mino duodenal papilla
peritoneal attachments of the duodenum
mesoduodenum, duodeno-colic fold, hepato-duodenal ligament
location of mesoduodenum
between the duodenum and the body wall
location of duodena-colic fold
between the duodenum and colon
location of hepato-duodenal ligament
between liver and duodenum
lobes of the pancreas
right lobe runs cranio-caudally and left lobe runs medio-laterally
peritoneal attachments of the pancreas
right lobe is within mesoduodenum and left lobe is within deep leaf of greater omentum
jejunum
the middle part of the small intestine which is covered by the greater omentum and should be empty most of the time
peritoneal attachment of the jejunum
meso-jejunum
ileum
the terminal portion of the small intestine which enters into the large intestine at the caeco-colic junction
peritoneal attachments of the ileum
ileo-caecal fold and meso-ileum
location of meso-ileum
between the ileum and the posterior wall of the abdominal cavity
caecum
the first part of the large intestine which is a blind-ending sac
peritoneal attachments of the caecum
ileo-caecal fold and caeco-colic fold
colon
the major part of the large intestine, consisting of the ascending colon which passes into the transverse colon at the right colic flexure followed by the descending colon at the left colic flexure which passes into the rectum