8. Acute coronary syndromes (myocardial infarction, unstable angina pectoris)
1/219
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
220 Terms
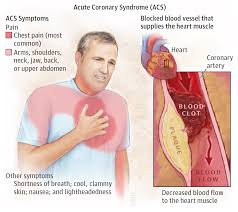
What is Acute Coronary Syndromes (ACS)
Acute Coronary Syndromes (ACS) refer to a spectrum of conditions resulting from decreased blood flow to the heart, including unstable angina and heart attacks. It is a medical emergency requiring prompt treatment.
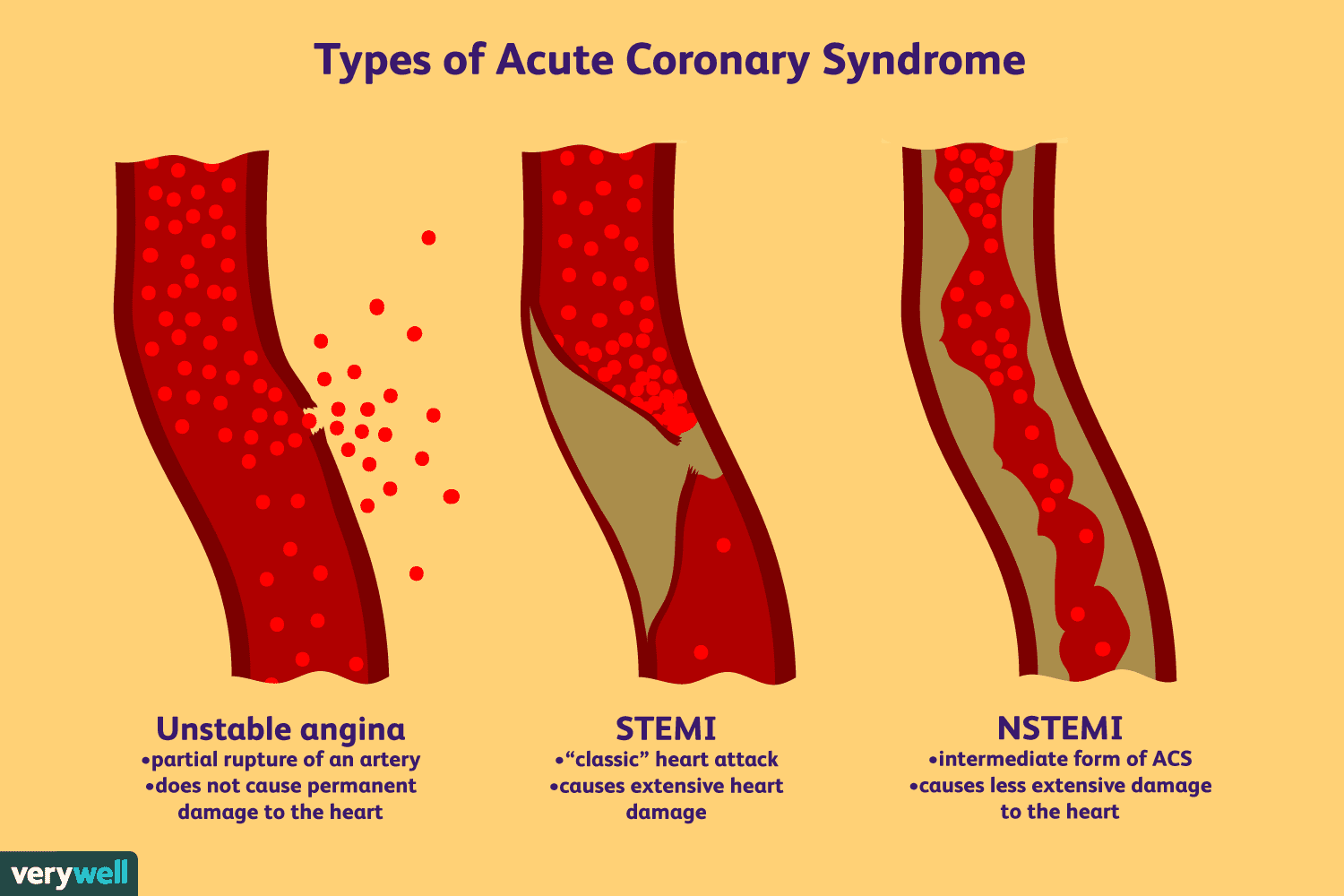
What are the three main types of Acute Coronary Syndromes (ACS)?
Unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI)
Unstable Angina: Chest pain at rest due to reduced blood flow to the heart.
NSTEMI: Partial blockage of a coronary artery causing heart muscle damage.
STEMI: Complete blockage of a coronary artery leading to significant heart muscle damage.
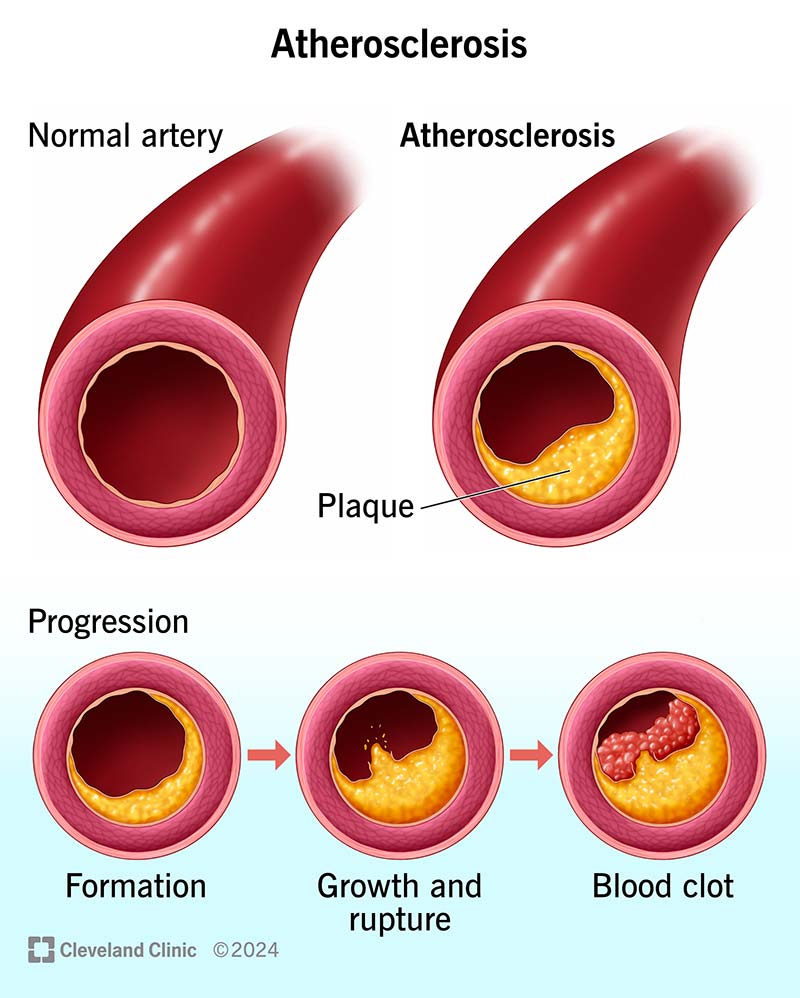
What is the pathophysiology behind Acute Co
ronary Syndromes (ACS)?
ACS typically results from the rupture of an atherosclerotic plaque and subsequent thrombus formation, leading to a sudden reduction or blockage of blood flow in a coronary artery.
The rupture of an atherosclerotic plaque exposes the underlying tissue to blood, causing platelet activation and aggregation, leading to thrombus formation.
What are common risk factors for developing ACS?
Increasing age, male gender, smoking, and a family history of coronary artery disease.
Which comorbidities significantly contribute to the risk of developing ACS?
Hypertension, diabetes mellitus, hyperlipidemia, and obesity significantly contribute to the risk of developing ACS.
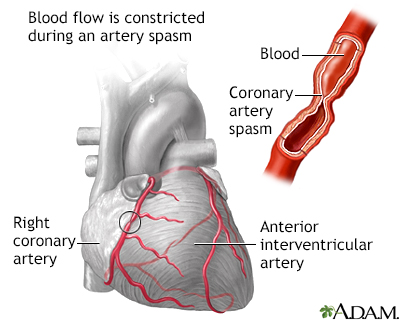
Alternate Causes of ACS
Coronary Artery Vasospasm
Coronary Artery Embolism
Takotsubo Cardiomyopathy
Myocarditis
Thrombophilia
Vasculitis
Myocardial Oxygen Supply-Demand Mismatch
What can cause transient episodes of chest pain in ACS?
Coronary Artery Vasospasm
What is Coronary Artery Vasospasm
Coronary Artery Vasospasm is a sudden constriction of the coronary arteries, leading to reduced blood flow to the heart muscle. It can cause chest pain (angina) or even a heart attack if severe.
What condition may result in Coronary Artery Embolism in ACS?
Atrial fibrillation or the presence of a prosthetic heart valve
Yes, Coronary Artery Embolism can lead to Acute Coronary Syndrome (ACS) by blocking blood flow to the heart, resulting in chest pain or heart attack.
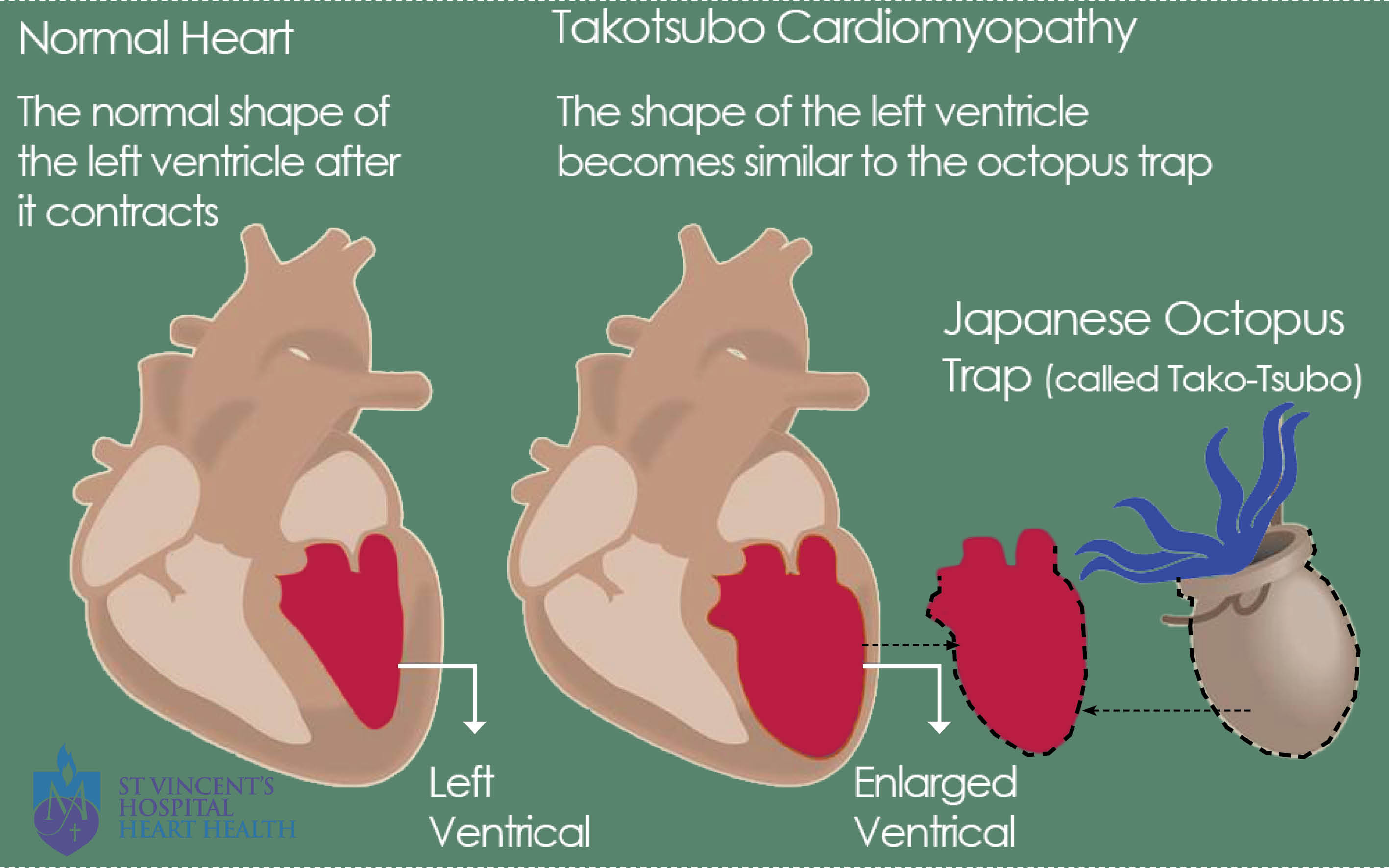
What is another name for stress-induced cardiomyopathy that mimics ACS
?
Takotsubo Cardiomyopathy
Also known as stress-induced cardiomyopathy, it mimics ACS but is typically precipitated by severe emotional or physical stress.
Takotsubo Cardiomyopathy is also known as stress-induced cardiomyopathy. It mimics ACS but is typically triggered by severe emotional or physical stress.
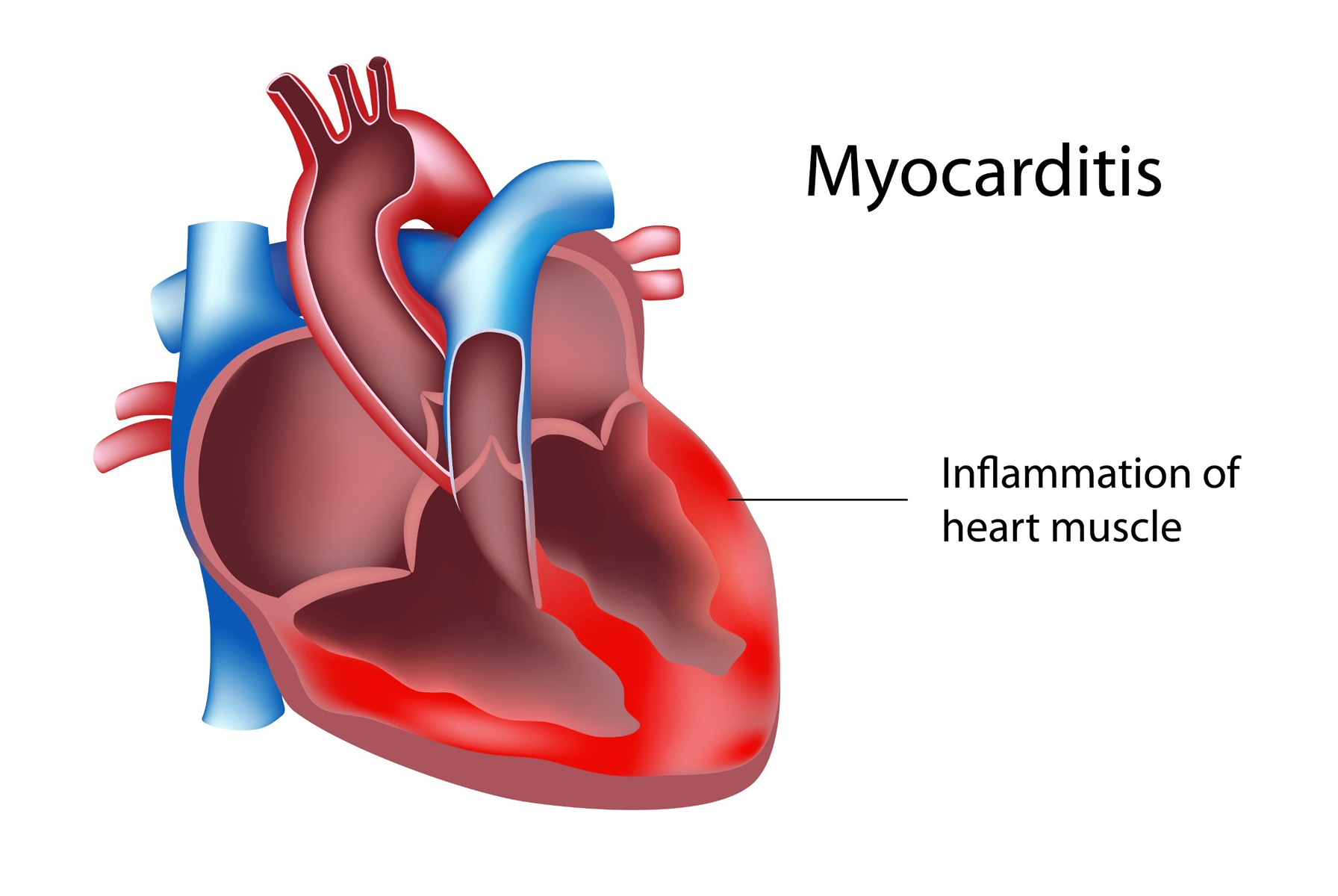
What is myocarditis
Inflammation of the heart muscle, often due to viral infections, which can impair myocardial function and mimic symptoms of ACS.
Yes, Myocarditis can mimic symptoms of Acute Coronary Syndrome (ACS) due to inflammation of the heart muscle, but it is not caused by blockages in the coronary arteries like ACS.
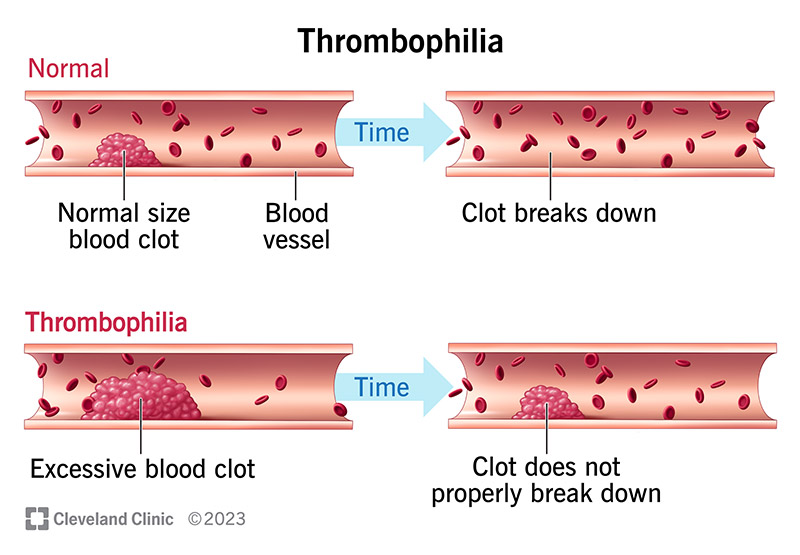
What is thrombophilia?
Increased tendency to form blood clots can lead to coronary thrombosis.
What is vasculitis?
Inflammatory destruction of blood vessels, which can include coronary arteries.
Yes, vasculitis can lead to acute coronary syndrome by causing inflammation and damage to the blood vessels supplying the heart, leading to reduced blood flow and potential heart complications.
What is Myocardial Oxygen Supply-Demand Mismatch?
Conditions like severe anemia, hypertrophic cardiomyopathy, or aortic stenosis can precipitate myocardial ischemia without coronary artery occlusion.
Pathophysiology of Acute Coronary Syndrome (ACS)
What is the primary cause of Acute Coronary Syndrome (ACS)?
The rupture of an unstable plaque.
How does the structure of an unstable plaque differ from a stable plaque?
Unstable plaques are lipid-rich and have a thin fibrous cap, while stable plaques contain fewer lipids and have a thicker fibrous capsule.
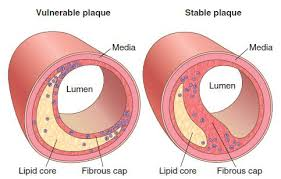
What role do Matrix Metalloproteinases play in plaque destabilization?
They degrade the structural integrity of the fibrous cap.
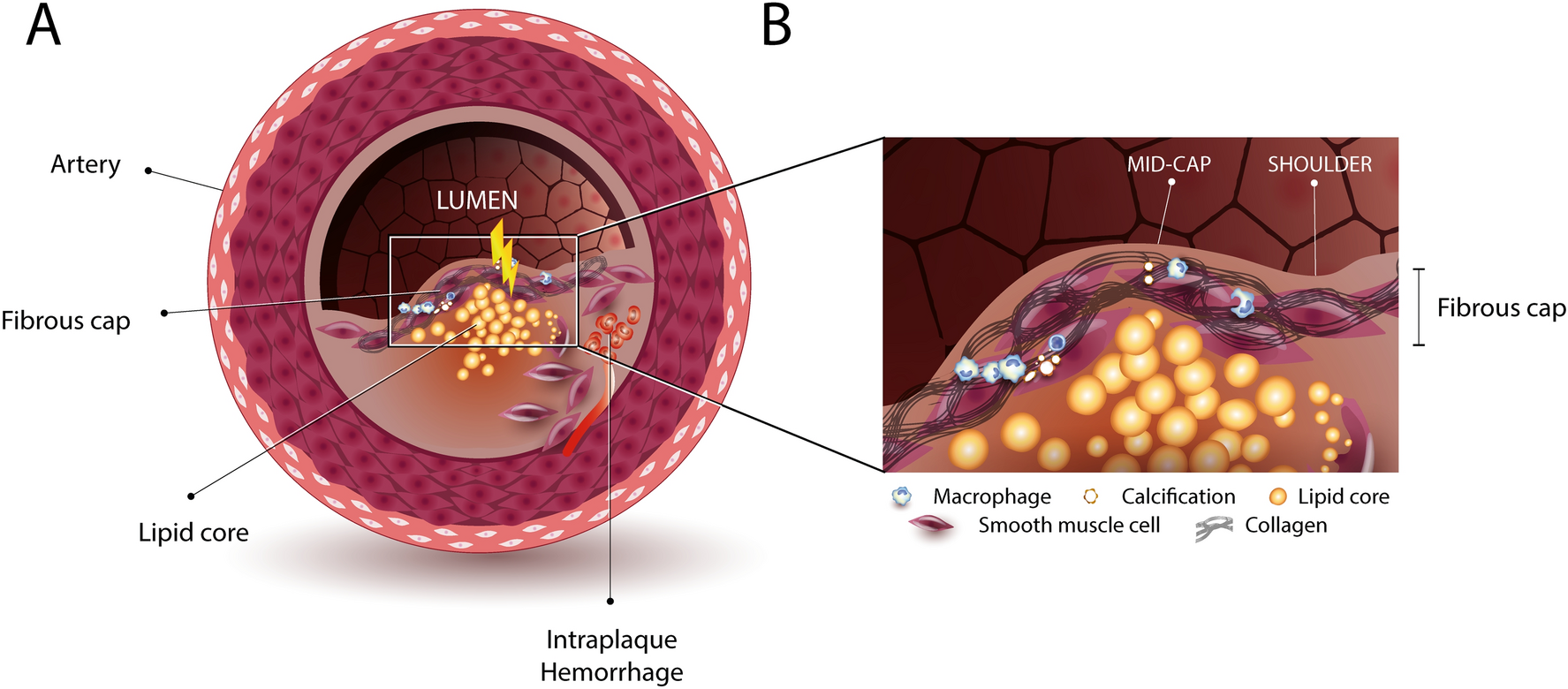
What happens when the plaque ruptures?
The underlying connective tissues are exposed to the bloodstream, triggering the thrombotic pathway.
Consequences of Plaque Rupture
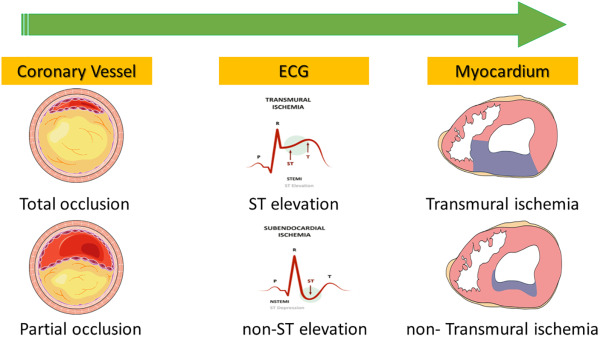
Partial Occlusion
Complete Occlusion
What conditions can partial occlusion due to plaque r
upture lead to?
Unstable angina or non-ST-elevation myocardial infarction (NSTEMI)
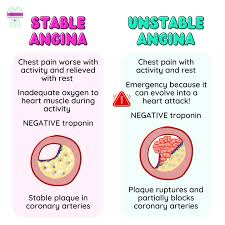
Stable angina is predictable chest pain that occurs with exertion and resolves with rest or medication. Unstable angina is unpredictable chest pain that can occur at rest or with minimal exertion and may signal an impending heart attack.
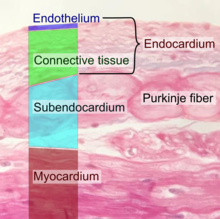
What layer of the myocardium is particularly affected by ischemia in conditions like unstable angina or NSTEMI?
Subendocardial layer
Complete Occlusion
What type of myocardial damage occurs in ST-elevation myocardial infarction (STEMI)?
Full thickness (transmural) myocardial damage
Complete Occlusion: Results in ST-elevation myocardial infarction (STEMI), where there is a full thickness (transmural) myocardial damage due to the complete interruption of blood supply.
What is the consequence of complete occlusion due to plaque rupture?
ST-elevation myocardial infarction (STEMI)
Clinical Presentation and Management of ACS
What is Unstable Angina?
A deterioration of previously stable angina where the pain becomes more severe, frequent, and may also occur at rest.
How long do episodes of Unstable Angina typically last?
Less than 20 minutes.
What happens to cardiac biomarkers in Unstable Angina?
They remain normal as myocardial necrosis does not occur.
Despite the severe symptoms, myocardial necrosis does not occur, so cardiac biomarkers remain normal.
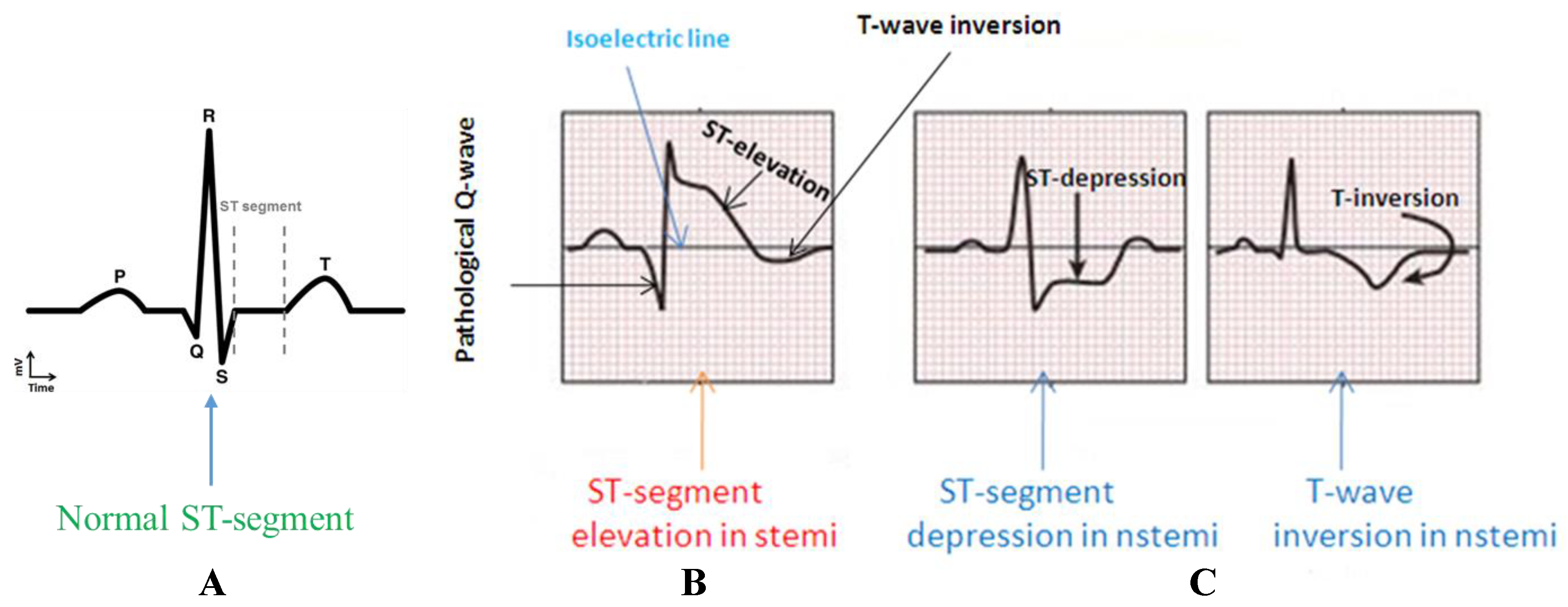
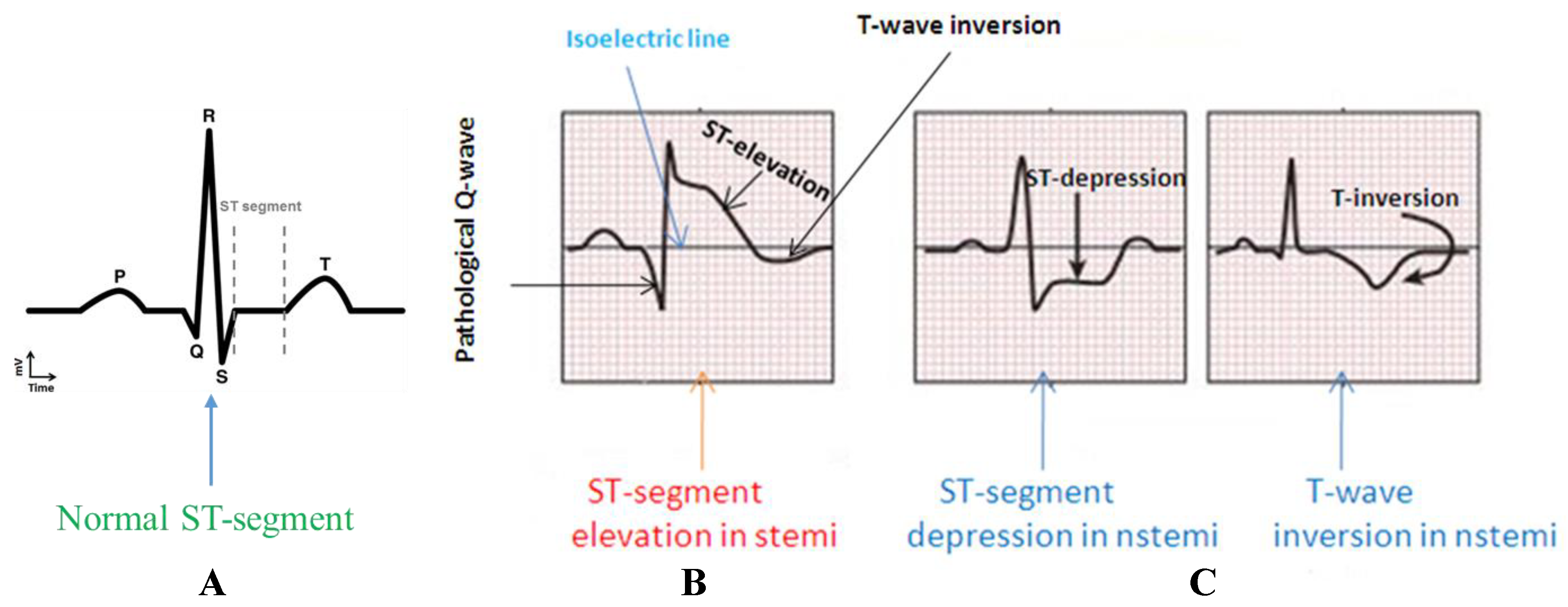
What can ECG findings show in Unstable Angina?
Can range from normal to showing ST-depression, reflecting myocardial strain rather than damage.
ECG findings in Unstable Angina: During unstable angina, ST-segment depression or T-wave inversion can occur due to myocardial ischemia, which affects the heart's electrical activity, leading to these ECG changes.
During stable angina, ECG may show transient ST-segment depression or T-wave inversion during episodes of chest pain, reflecting myocardial ischemia without permanent damage.
What is the treatment for Unstable Angina
?
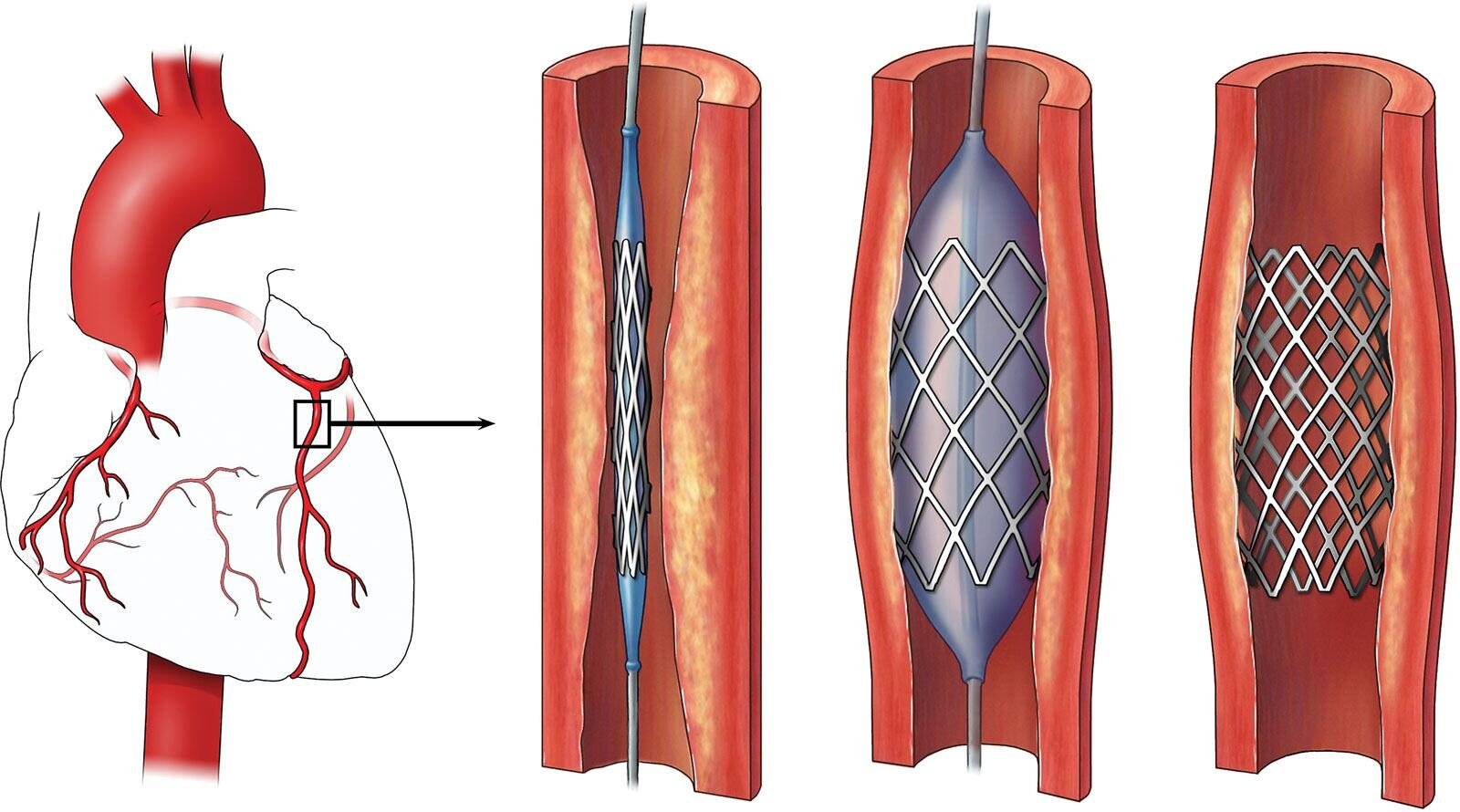
Includes antiplatelet therapy (aspirin, ticagrelor) and anticoagulation to prevent further thrombus formation. In high-risk cases, more invasive procedures like percutaneous coronary intervention (PCI) may be necessary.
Percutaneous Coronary Intervention (PCI): A procedure to open narrowed or blocked coronary arteries using a catheter with a balloon or stent to restore blood flow to the heart muscle.
NSTEMI
What does NSTEMI stand for?
Non-ST segment elevation myocardial infarction
How is NSTEMI characterized?
By acute myocardial ischemia that leads to myocardial injury, typically due to a partial occlusion of a coronary artery.
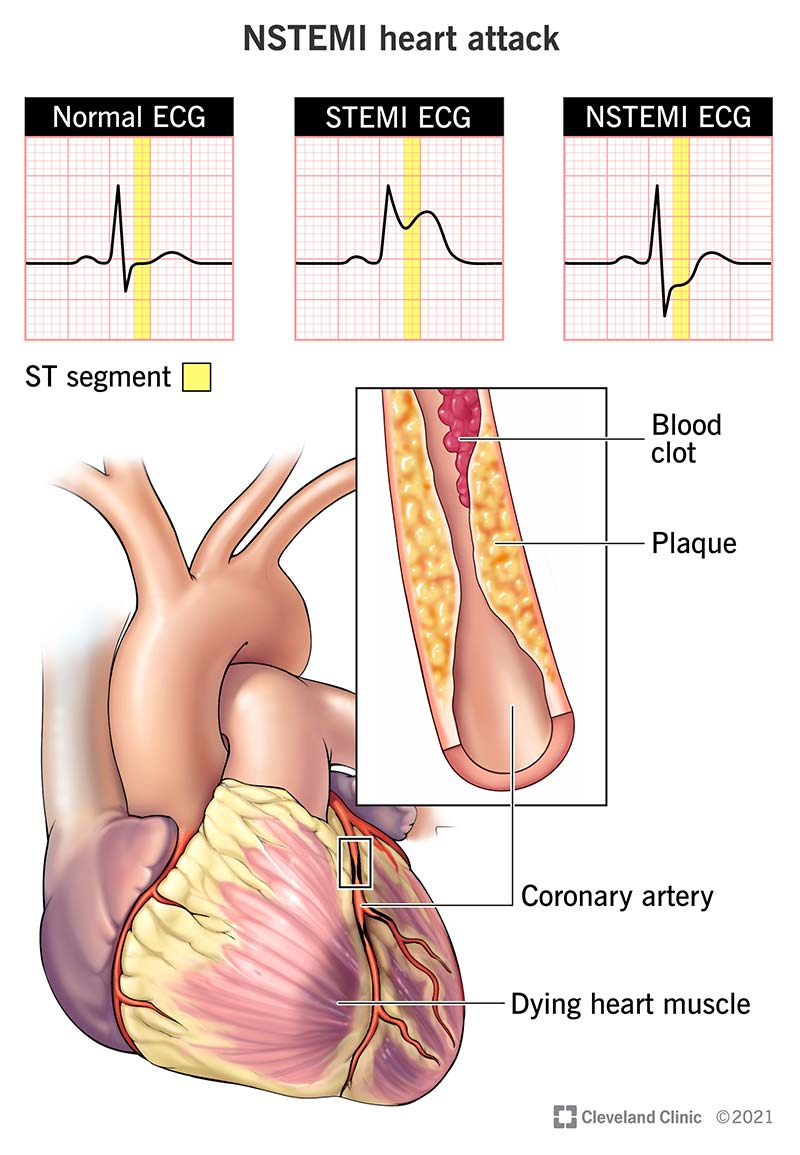
Which layer of the heart wall is particularly affected in NSTEMI?
The subendocardial layer
Diagnostic Criteria of NSTEMI
Cardiac Biomarkers
ECG Changes
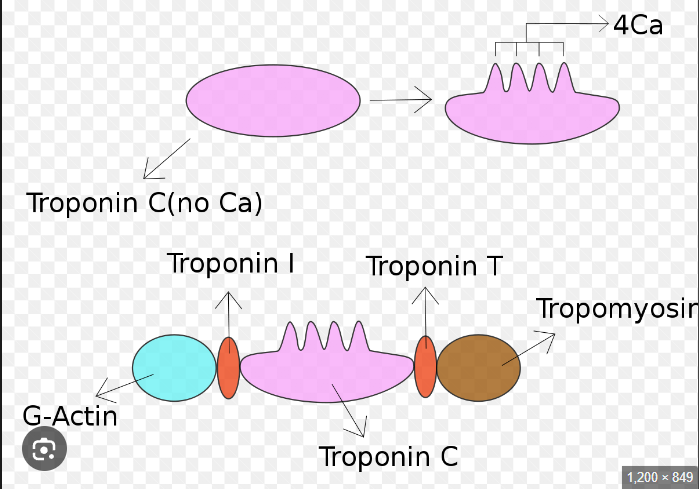
What are common cardiac biomarkers used in diagnosing NSTEMI
?
Troponins
Troponin I
Troponin T
Creatine Kinase-MB (CK-MB)
Troponins are proteins released when heart muscle is damaged. Troponin I and T are specific to heart muscle, while CK-MB is an enzyme also indicating heart damage.
What ECG changes may be see
n in NSTEMI?
ST-segment depression, T-wave inversion, or a loss of R-wave amplitude
ST-segment elevation is seen in STEMI, while ST-segment depression, T-wave inversion, or loss of R-wave amplitude are seen in NSTEMI. STEMI indicates complete blockage of a coronary artery, while NSTEMI indicates partial blockage.
Treatment of NSTEMI
Anticoagulation Therapy
Antiplatelet Therapy
Invasive Procedures
What is essential to prevent further clot formation in the treatment of NSTEMI?
Anticoagulation Therapy
What are the standard medications used to reduce the risk of further thrombotic events in NSTEMI?
Aspirin and P2Y12 inhibitors (e.g., ticagrelor)
What invasive procedure might high-risk NSTEMI patients require?
Coronary angiography followed by possible revascularization via percutaneous coronary intervention (PCI)
Coronary angiography is a medical procedure that uses X-ray imaging to visualize the blood vessels of the heart (coronary arteries) to diagnose blockages or other issues.
STEMI
What is the pathophysiology of STEMI?
Resulting from a complete occlusion of a coronary artery, leading to transmural infarction where the entire thickness of the heart muscle is affected.
Diagnostic Criteria
Cardiac Biomarkers
ECG Findings
How do the cardiac biomarkers in STEMI compare to NSTEMI?
Similarly elevated but typically to a higher extent due to more significant muscle damage.
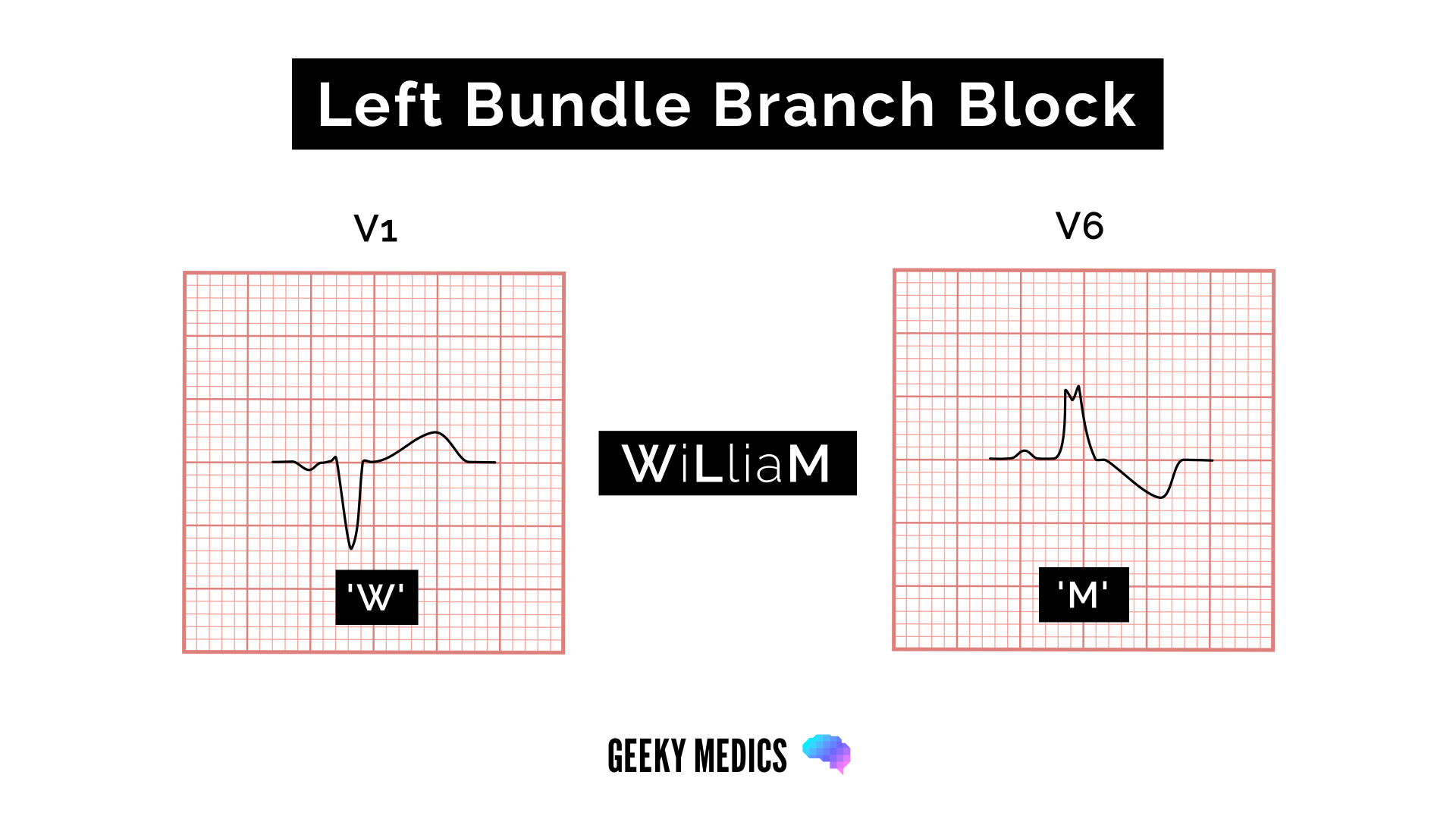
What are the ECG findings characteristic of STEMI?
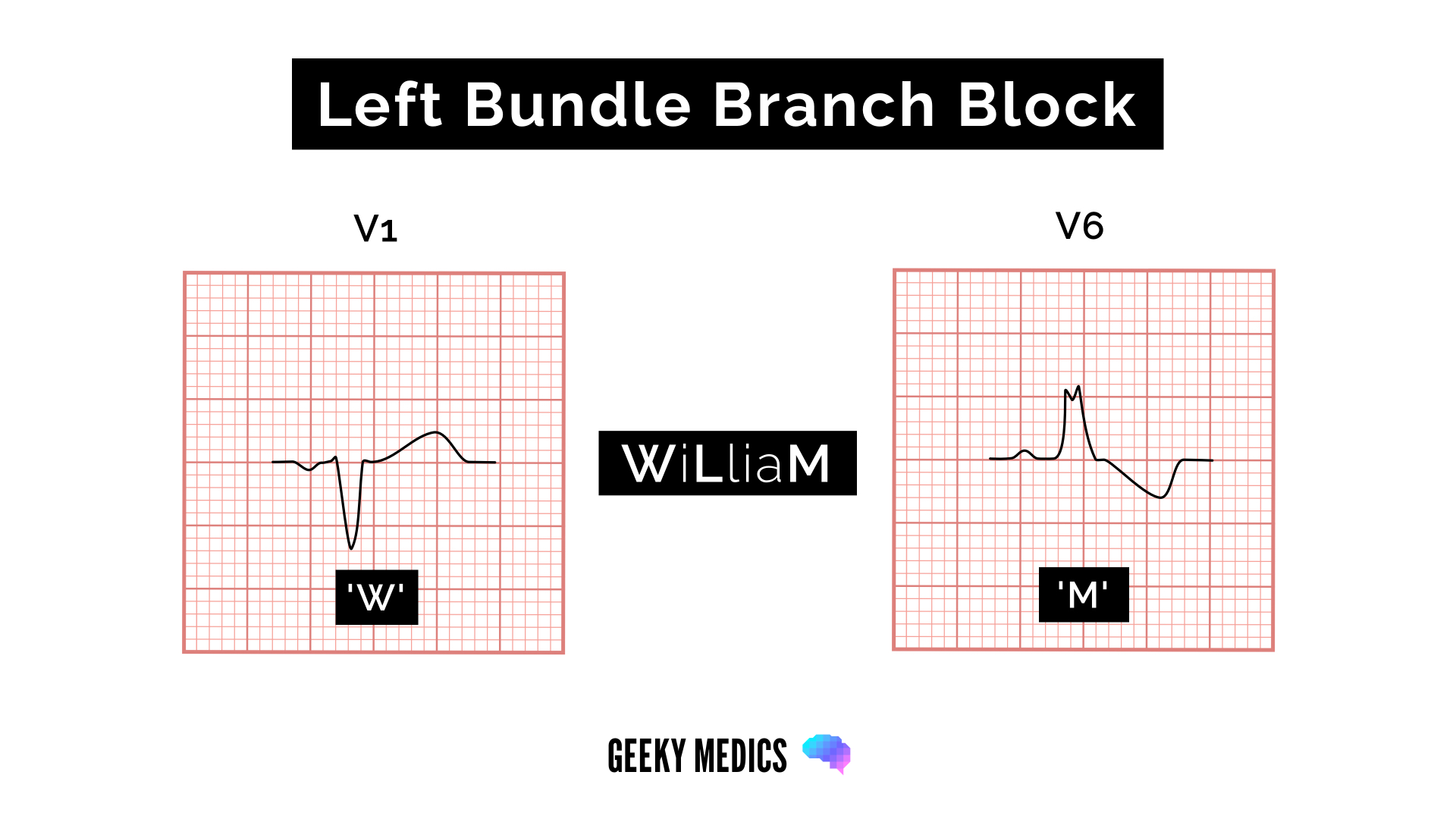
ST-segment elevations in two contiguous leads or the presence of a new left bundle branch block (LBBB), indicative of a widespread impact on cardiac electrical activity.
These ECG findings in STEMI are indicative of a significant myocardial infarction. ST-segment elevations in two contiguous leads or new LBBB suggest a widespread impact on cardiac electrical activity due to acute myocardial ischemia or infarction.
What is the preferred treatment for restoring blood flow in STEMI?
Urgent PCI, commonly known as angioplasty with stenting
Treatment of STEMI
Immediate Revascularization
Anticoagulation and Antiplatelet Therapy
Post-Revascularization Care
How are anticoagulation and antiplatelet therapies used in the treatment of STEMI?
To prevent further clots and stabilize existing ones
What medications are used in post-revascularization care for STEMI patients?
Beta-blockers, ACE inhibitors, or statins
Beta-blockers: Block beta-adrenergic receptors, reducing heart rate and blood pressure.
ACE inhibitors: Inhibit angiotensin-converting enzyme, lowering blood pressure.
Statins: Inhibit HMG-CoA reductase, reducing cholesterol synthesis.
Common Clinical Features of Acute Coronary Syndrome
Acute Retrosternal Chest Pain
Dyspnea
Pallor
Nausea and Vomiting
Diaphoresis and Anxiety
Dizziness or Syncope
What are the common descriptions of acute retrosternal chest pain in Acute Coronary Syndrome?
Dull, squeezing, or pressure-like sensation.
The pain in acute coronary syndrome is described as dull, squeezing, or pressure-like due to the heart muscle's lack of oxygen, leading to ischemia and the activation of pain receptors in the heart.
Where does the chest pain commonly radiate to in Acute Coronary Syndrome?
Left arm, shoulder, neck, jaw, back, or epigastrium.
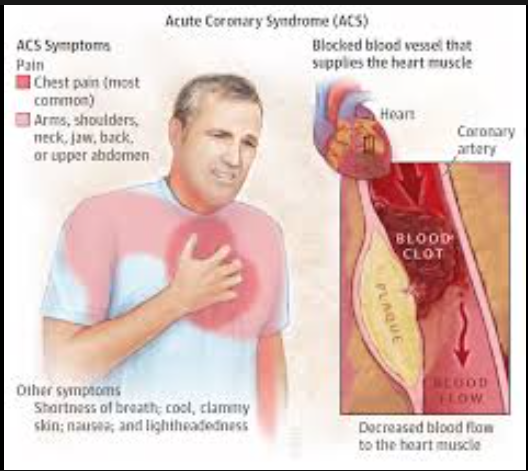
What are the typical triggers for chest pain in Acute Coronary Syndrome?
Exertion or stress.
When does chest pain frequently occur in Acute Coronary Syndrome?
Morning, due to circadian variations in blood pressure and coronary arterial tone.
What is dyspnea
?
Shortness of breath is a frequent symptom, reflecting either direct myocardial dysfunction or a consequence of the acute stress response.
What is pallor?
Paleness due to poor perfusion and the body's sympathetic response diverting blood to vital organs.
What may cause nausea and vomiting in Acute Coronary Syndrome?
These symptoms may be due to the visceral pain referral from the ischemic myocardium or a vagal response.
Why do patients with Acute Coronary Syndrome often experience diaphoresis and anxiety?
Sweating and feelings of anxiety are common and relate to adrenergic activation in the setting of pain and hypoxia.
What can cause dizziness or syncope in Acute Coronary Syndrome?
Reduced cardiac output and cerebral perfusion during acute events can lead to dizziness or syncope.
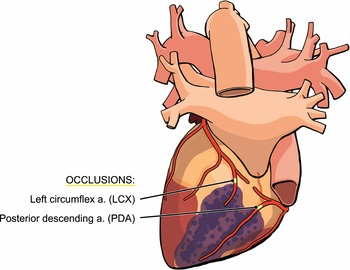
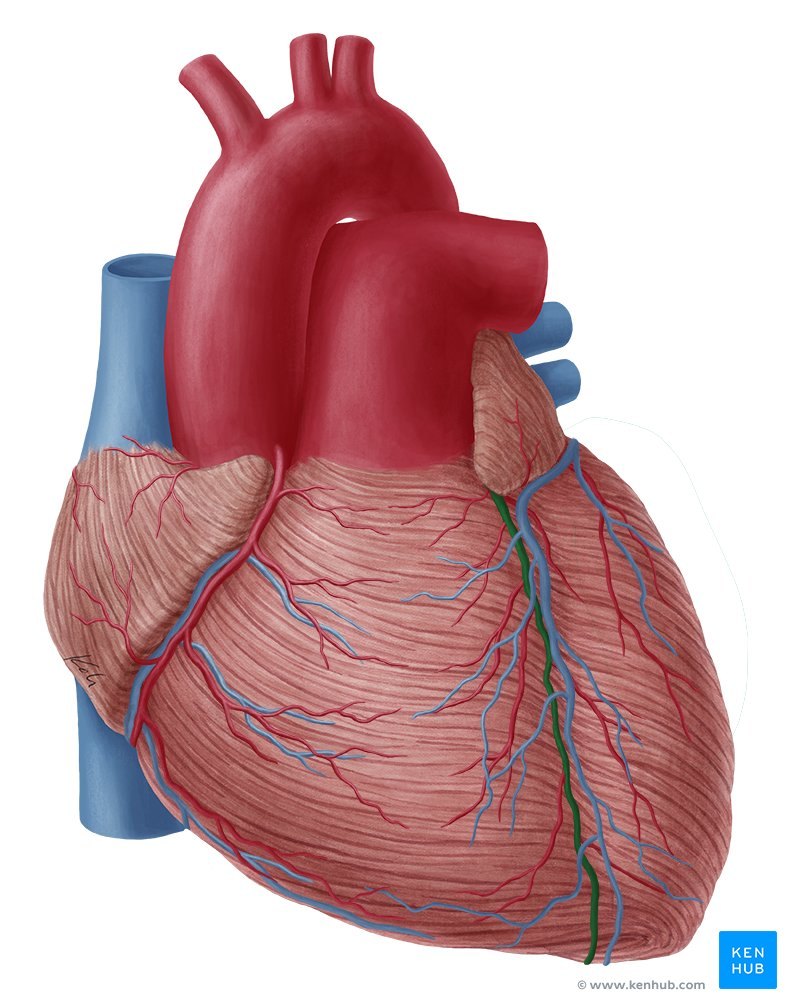
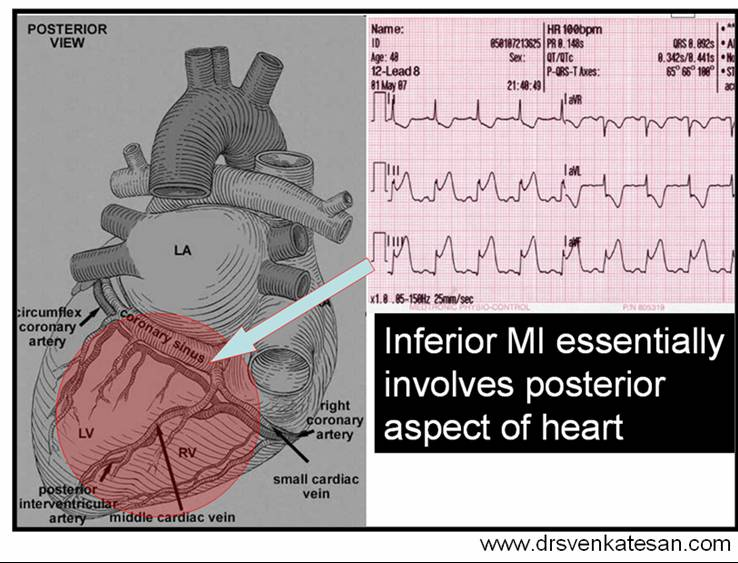
Specific Manifestations Based on Infarction Location
Inferior Wall Infarction
Right Ventricular Infarction
What is the cause of an inferior wall infarction?
Typically results from occlusion of the right coronary artery.
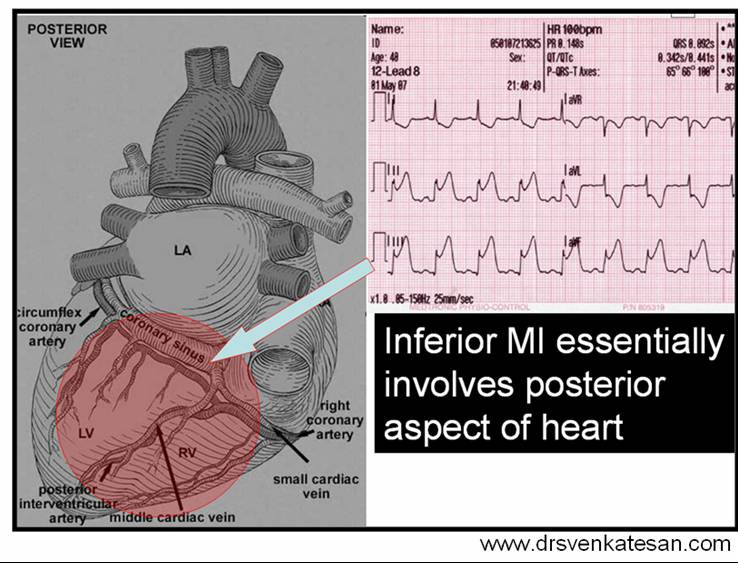
What symptoms can be seen in an inferior wall infarction?
Can include bradycardia due to involvement of the sinoatrial or atrioventricular nodes, and epigastric pain, often mistaken for indigestion or gastrointestinal issues.
What are the indicators of Right Ventricular Infarction?
Hypotension, elevated jugular venous pressure, and clear lung fields
Hypotension: Reduced cardiac output leads to decreased blood pressure.
Elevated jugular venous pressure: Indicates right heart failure.
Clear lung fields: Absence of pulmonary congestion due to right heart failure.
In right heart failure, there is an absence of pulmonary congestion because the right side of the heart is unable to effectively pump blood forward, leading to reduced pressure in the pulmonary circulation and preventing fluid accumulation in the lungs.
Pulmonary congestion is the accumulation of fluid in the lungs due to increased pressure in the pulmonary circulation, often caused by heart failure or other conditions affecting the heart's ability to pump blood effectively.
Why is it important to recognize right ventricular involv
ement in patients?
Recognizing right ventricular involvement is crucial as these patients may require specific management strategies, including maintenance of adequate right ventricular preload and cautious use of nitrates.
Nitrates are used cautiously in right heart failure to avoid reducing right ventricular preload excessively. They can affect systemic vascular resistance and may impact right ventricular function.
Atypical Presentations of Acute Coronary Syndrome
Minimal or No Chest Pain
Elderly and Women
What is meant by atypical presentations in the context of chest pain?
Presentations that do not follow the typical pattern of chest pain symptoms.
Why is minimal or no chest pain particularly common in patients with diabetes?
Due to diabetic neuropathy, which may mask typical chest pain sensations.
Who are more likely to present atypically with chest pain, the elderly or young individuals?
The elderly and women are more likely to present atypically with chest pain.
What are some symptoms that may be present in elderly and women as atypical chest pain presentations?
Symptoms may include fatigue, breathlessness, and general malaise rather than classic chest pain.
Initial Diagnostic Steps of Acute Coronary Syndrome
ECG
Cardiac Biomarkers
What is the importance of an immediate ECG in suspected Acute Coronary Syndrome (ACS) cases?
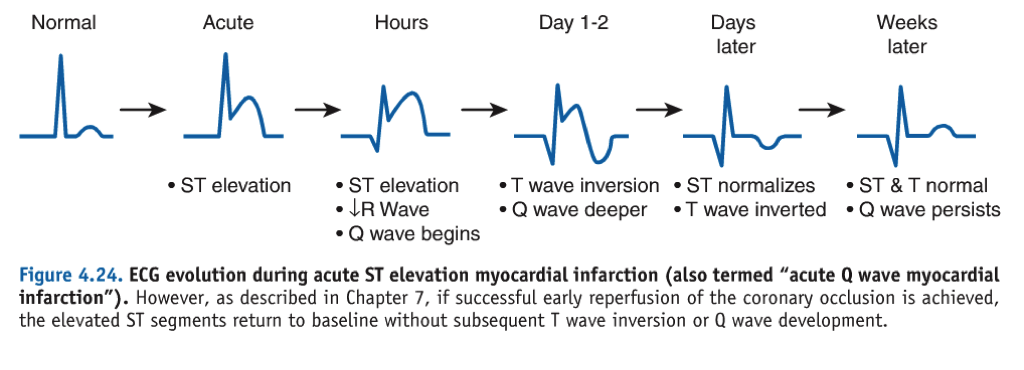
An immediate ECG is crucial to assess various changes depending on the stage and severity of the myocardial infarction.
An immediate ECG is crucial when ACS is suspected. The ECG can show various changes depending on the stage and severity of the myocardial infarction.
How do cardiac biomarkers like troponins help in diagnosing myocardial injury in ACS?
Cardiac biomarkers like troponins, released into the blood from the damaged heart muscle, confirm myocardial injury, with elevated levels indicating myocardial infarction.
ECG Changes in STEMI
Acute Stage
Intermediate Stage
Chronic Stage
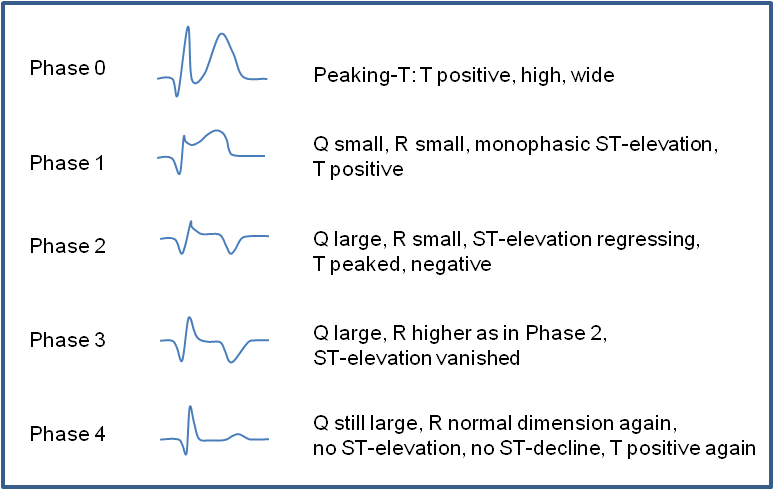
Acute Stage
Acute Stage ECG Changes in STEMI
Hyperacute T-waves
ST-Elevation
What are Hyperacute T-waves in the context of STEMI?
Peaked T-waves that are an early sign of ongoing myocardial infarction.
What does ST-Elevation in two contiguous leads with reciprocal ST-depressions indicate in STEMI?
Ongoing myocardial damage due to complete occlusion of a coronary artery.
Intermediate Stage
Necrosis Indicators
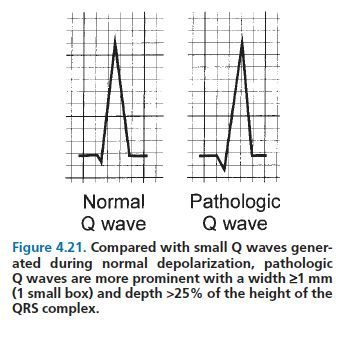
Pathological Q-Waves
What are Necrosis Indicators in the intermediate stage of STEMI?
Disappearance of R-wave, formation of pathological Q-waves, and T-wave inversions.
Pathological Q-waves in ST-elevation myocardial infarction (STEMI) are abnormal Q-waves that appear on an electrocardiogram (ECG) due to myocardial infarction. They indicate significant damage to the heart muscle and are a sign of a previous heart attack.
How are Pathological Q-Waves defined in the c
ontext of STEMI?
Duration >40 ms, amplitude >0.1 mV, or appearance in leads V1-V3, indicating myocardial necrosis.
What are the ECG changes seen in the acute stage of a STEMI?
Hyperacute T-waves and ST-elevation.
Hyperacute T-waves are an early sign of myocardial infarction (heart attack) characterized by tall, peaked T-waves on an electrocardiogram (ECG). They indicate severe ischemia and are often followed by ST-segment elevation.
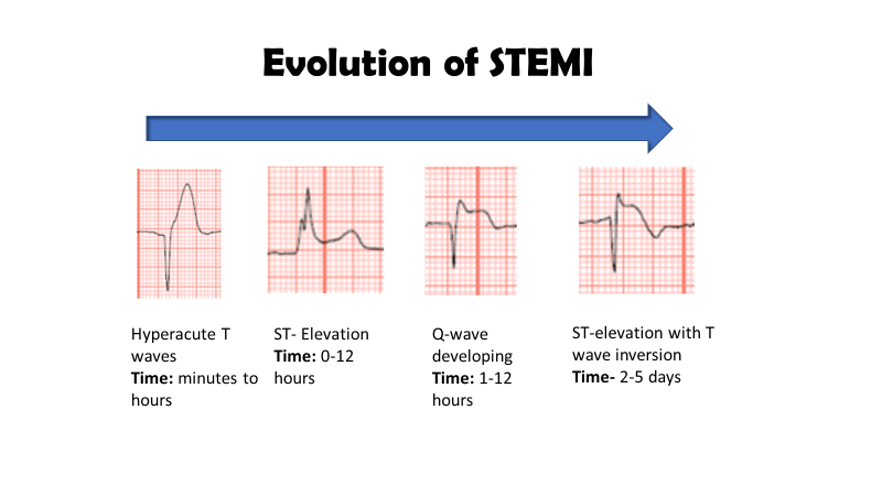
What are the ECG changes seen in the intermediate stage of a STEMI?
Necrosis indicators like disappearance of R-wave, formation of pathological Q-waves, and T-wave inversions.
The disappearance of R-wave in an electrocardiogram indicates myocardial infarction or necrosis of heart tissue.
photo: poor R wave
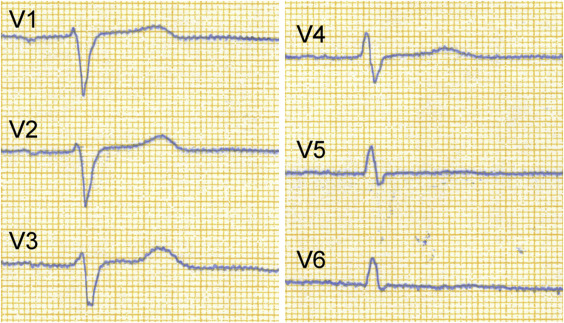
Chronic Stage
Scarring
ersistent, broad, and deep Q-waves indicate the formation of scar tissue where myocardial necrosis occurred. T-wave inversions may remain, and R-waves may not fully recover, showing incomplete healing.
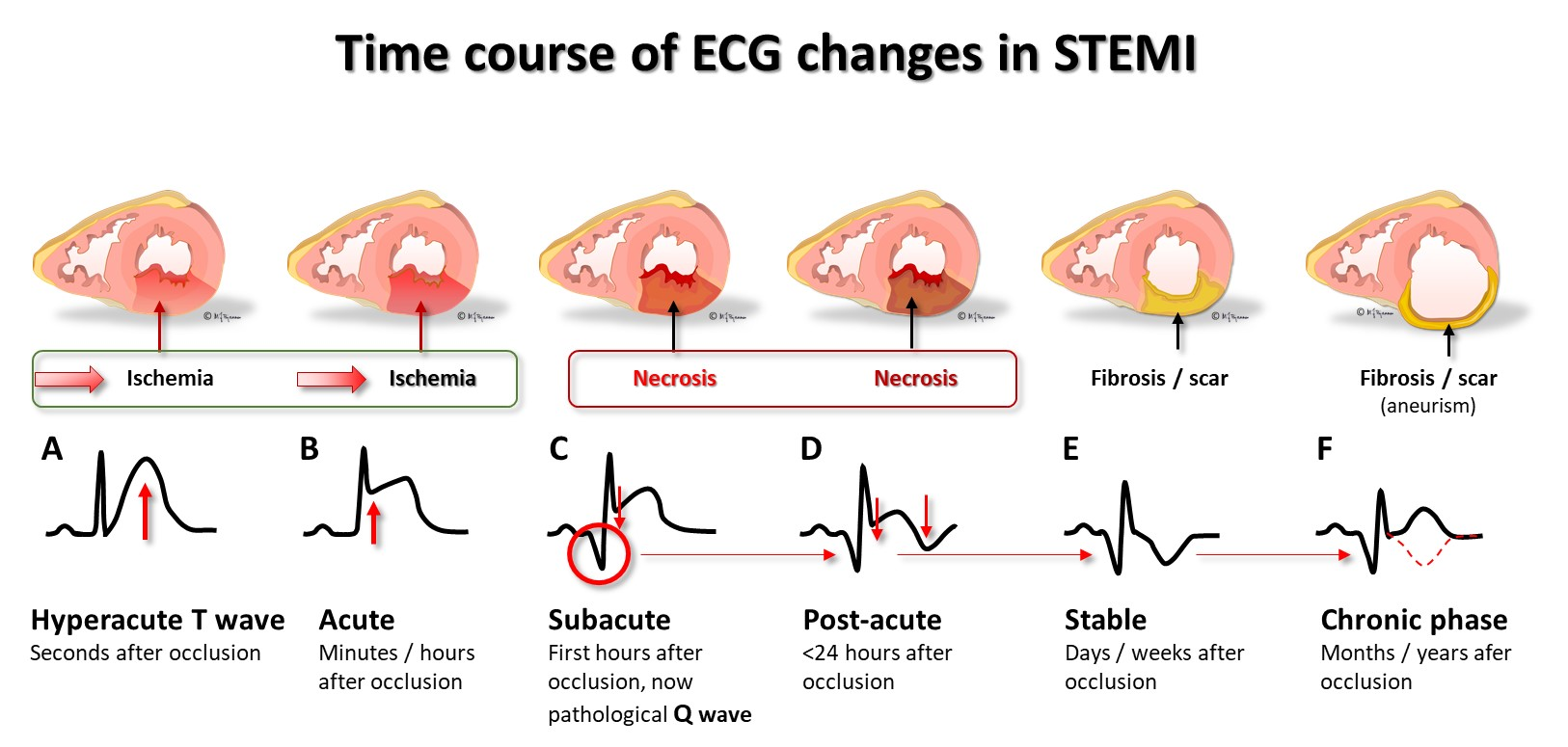
What ECG changes indicate the chronic stage of a STEMI?
Persistent Q-waves, incomplete recovery of R-waves, and T-wave inversions.
undefined
What is the typical sequence of ECG changes in a STEMI?
Hyperacute T-waves → ST-elevation → Pathological Q-wave formation → T-wave inversion → ST normalization → T-wave normalization.
undefined
What is the significance of Matrix Metalloproteinases in atherosclerosis?
Matrix Metalloproteinases, secreted by inflammatory cells within the plaque, degrade the fibrous cap's structural integrity, leading to its rupture.
Special Considerations
Left Bundle Branch Block (LBBB)
Why is Left Bundle Branch Block (LBBB) considered a STEMI equivalent in certain cases?
In patients with new or presumably new LBBB and symptoms suggestive of ACS, it is treated as a STEMI equivalent because it can mask typical ST-elevations due to underlying ventricular depolarization abnormalities.
Left Bundle Branch Block (LBBB):
LBBB is a cardiac conduction abnormality where the electrical impulse is delayed or blocked in the left bundle branch. This results in widened QRS complexes on ECG. It can indicate heart disease.
To recognise left bundle branch block, we use the name WiLLiaM and look at the first and last letters: W: complexes in V1 resemble the letter W: deep downward deflection (dominant S wave), which may be notched. M: complexes in V6 resemble the letter M: broad, notched or 'M' shaped R wave in V6
ECG Changes in NSTEMI
How do ECG changes in NSTEMI differ from those in STEMI?
NSTEMI does not typically show ST-elevation but may display non-specific changes like ST-depressions, T-wave inversions, or a loss of R-wave amplitude, reflecting less severe but significant myocardial injury.
Importance of Timely Diagnosis
Why is timely diagnosis crucial in cases of ACS?
Prompt identification and treatment are essential to minimize myocardial damage and improve outcomes, as management strategies differ between STEMI and NSTEMI based on the presence or absence of ST-elevation.
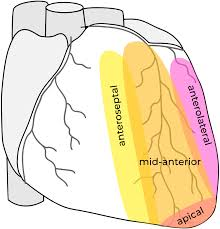
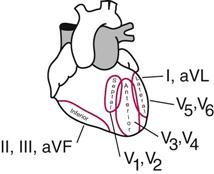
Localization of Myocardial Infarction by ECG Leads
V1-V6 (Chest Leads)
Limb Leads
Extended Leads for Posterior Wall
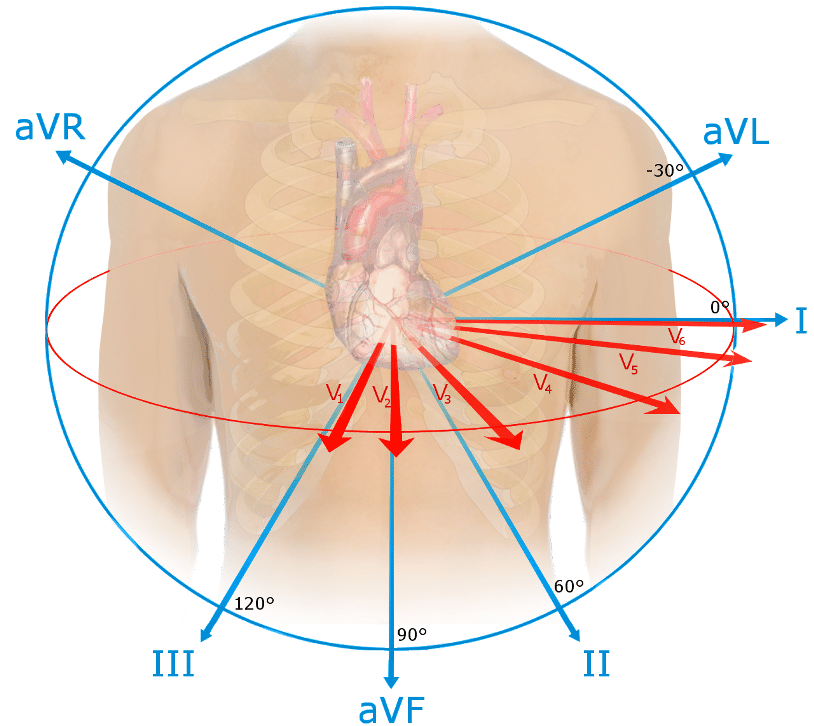
V1-V6 (Chest Leads)
V1-V6
V1-V2
V3-V4
V5-V6
What do V1-V6 chest leads indicate?
Extensive anterior infarct, typically due to occlusion of the proximal left anterior descending artery (LAD).
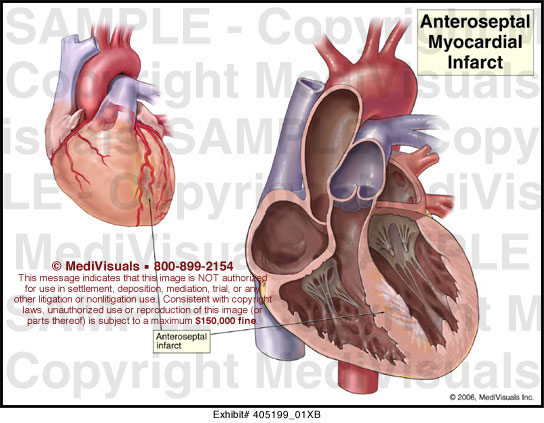
What does V1-V2 suggest?
Anteroseptal infarction, indicative of an left anterior descending artery (LAD) occlusion affecting the basal part of the septum.
What does V3-V4 point to in an ECG reading?
Anteroapical infarction, likely due to occlusion of the distal LAD, affecting the apex of the heart.
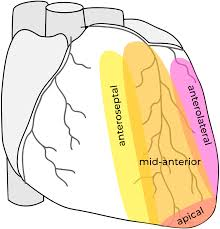
What does V5-V6 reflect in an ECG reading?
Anterolateral infarction, which can be caused by occlusion of the distal LAD, a diagonal branch of the LAD, or the left circumflex artery.
Limb Leads
I, aVL
II, III, aVF
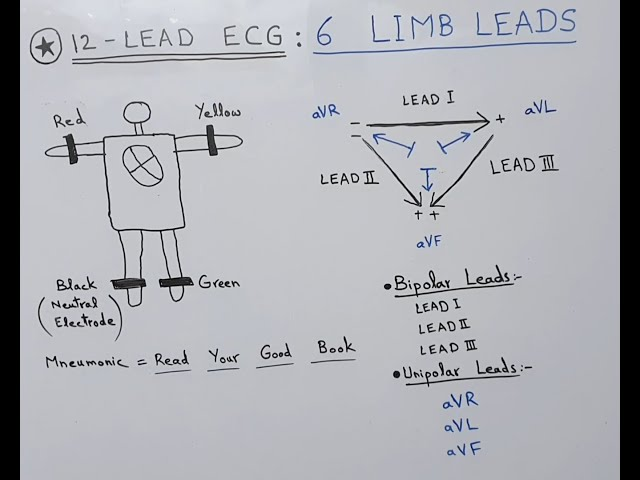
What do I, aVL leads indicate?
Lateral wall infarction, typically due to occlusion of the proximal left circumflex artery.
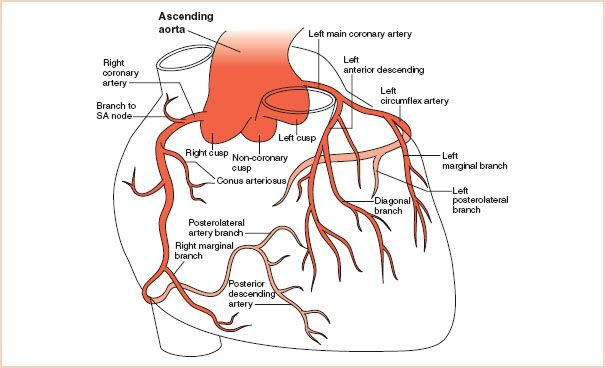
What do II, III, aVF leads show?
Inferior wall infarction, commonly caused by occlusion of the right coronary artery.
good picture
Extended Leads for Posterior Wall
V7-V9
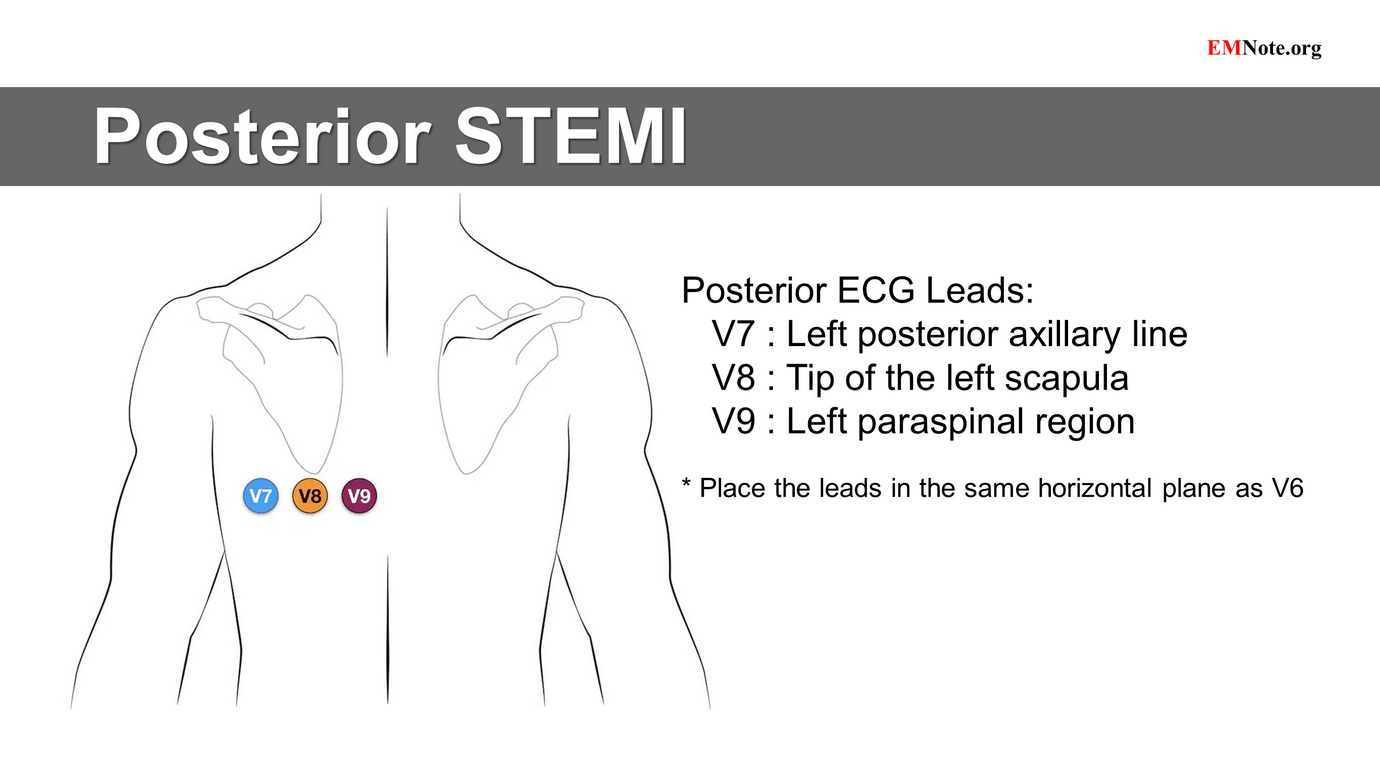
What are V7-V9 leads used to detect?
Posterior wall infarction
These leads are used to detect a posterior wall infarction, typically involving the posterior descending artery.