HN220 Lab Final
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
L7: What heart function produces each heart sound?
The first heart sound (S1, “LUB’) is produced by the closure of the atrioventricular (AV) valves (tricuspid and bicuspid/mitral) at the beginning of ventricular systole (ventricular contraction).
The second heart sound (S2, "DUB") is produced by the closure of the semilunar valves (aortic and pulmonary) at the end of ventricular systole making the beginning of ventricular diastole (ventricular relaxation).
L7: What do you observe about the location of the heart sounds with respect to the ECG wave?
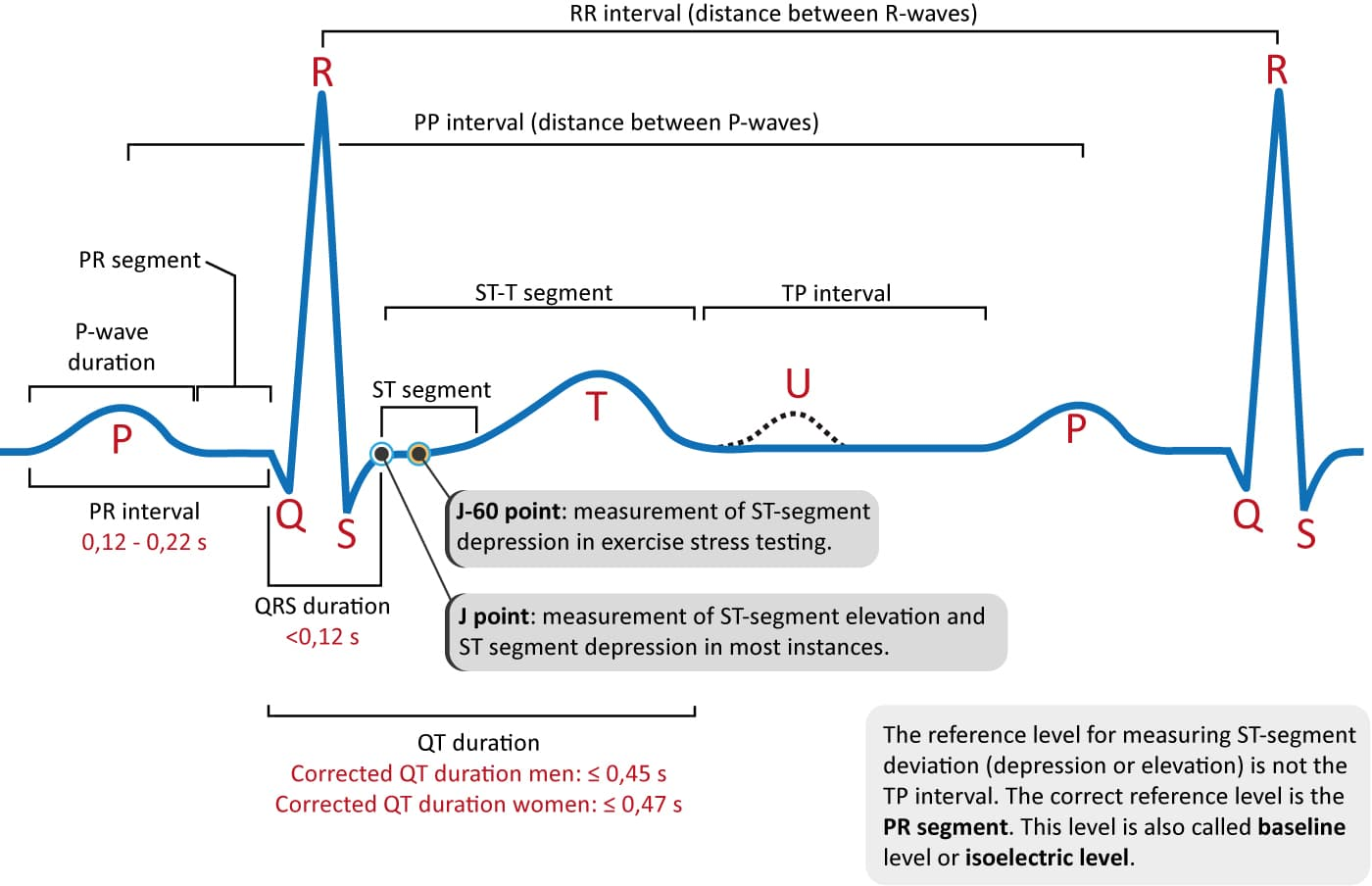
S1 occurs just after the QRS complex, when the ventricles contract and the AV valves close (ventricular depolarization/contraction).
S2 occurs just after the T wave, marking the end of the systole and the closure of the semilunar valves (ventricular repolarization/relaxation).
L7: Compare the above tracing to a healthy ECG tracing, what differences do you note?
In a healthy ECG, the rhythm is regular, and the spacing between each QRS complex is consistent.
In this ECG strip, the R-R intervals are not consistent / abnormal spacing– some are shorter, others longer – indicating an irregular rhythm.
However, P waves, QRS complexes, and T waves appear to be present and in the correct order.
Ex. of the irregular spacing:
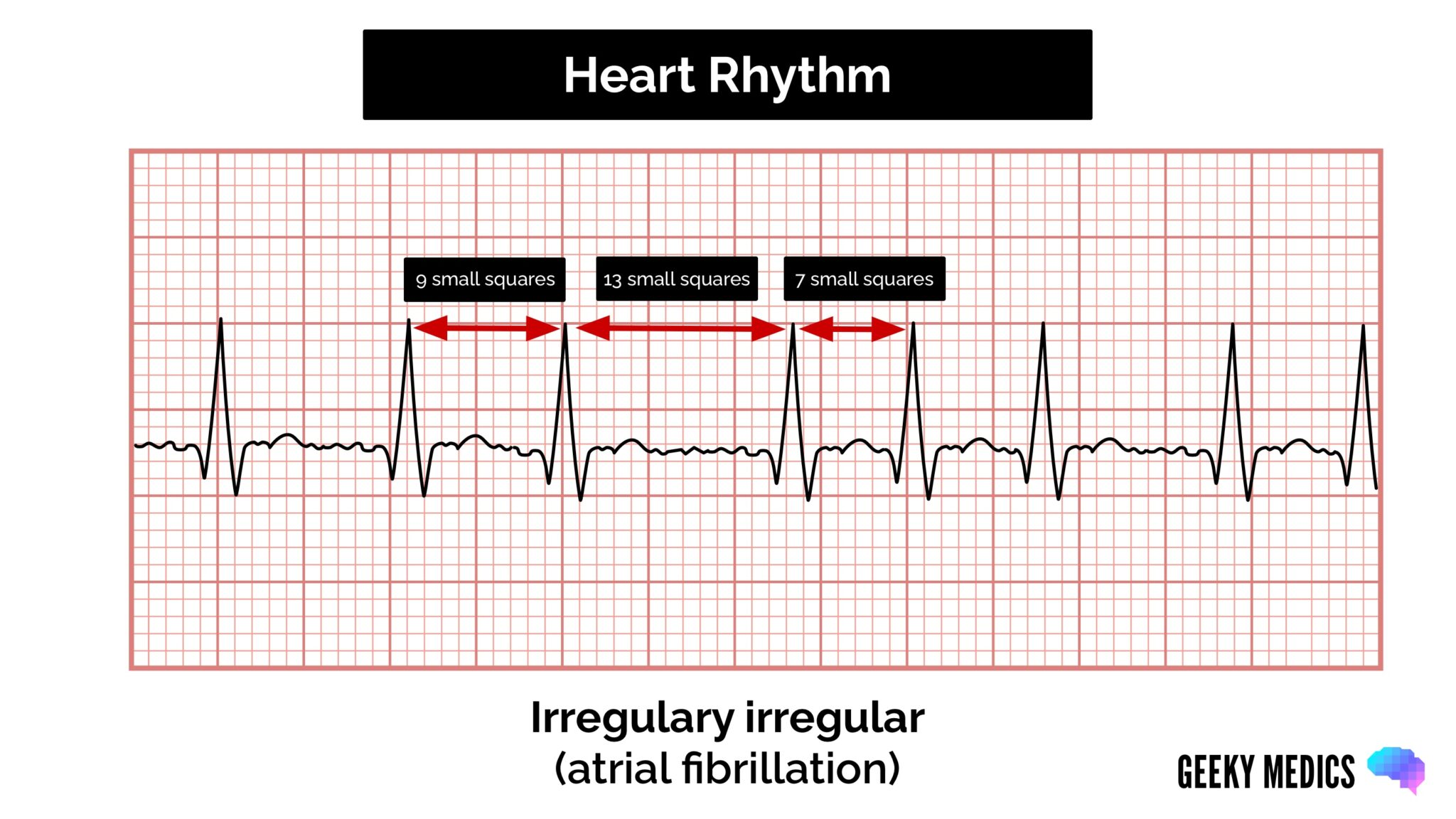
L7: What is causing the irregularities in the ECG wave you observed in question 3?
The irregular rhythm may suggest atrial fibrillation, sinus arrhythmia, or premature beats.
Since the P waves are hard to distinguish in some parts and the rhythm is irregular, atrial fibrillation is a possible cause.
Alternatively, it could be sinus arrhythmia, which is a normal variation in rhythm with breathing (especially in young people).
Premature beats: The P wave looks different or may be hidden. Followed by a normal-looking QRS complex.
L7: Based on your findings in question 3 and 4, what part of the heart is not functioning properly?
The atria, particularly the SA (sinoatrial) node, may not be functioning properly. Because the P wave represents atrial contraction/depolarization.
If atrial fibrillation is present, the atria are not contracting effectively, leading to erratic electrical activity.
L7: Based on questions 3 - 5, what effect is this impairment going to have on the functioning of the heart as a whole?
If the atria do not contract effectively → ventricular filling may be reduced → ↓stroke volume (less blood ejected per beat) → decreased cardiac output (CO=SV x HR)
This can lead to inadequate perfusion to tissues/organs, resulting in fatigue, dizziness, or shortness of breath.
Long-term, irregular rhythms can increase the risk of blood clots, stroke, and heart failure.
L7: In a numerical order state the flow of blood through all structures it passes, starting at the right atria and ending at the aorta, include the names of the valves it passes on its way.
Right atrium receives deoxygenated blood from the body via the superior and inferior vena cava.
Blood flows through the tricuspid valve into the right ventricle.
The right ventricle pumps blood through the pulmonary valve into the pulmonary arteries.
Blood travels to the lungs where it becomes oxygenated.
Oxygenated blood returns to heart via the pulmonary veins to the left atrium.
Blood flows through the bicuspid valve into the left ventricle.
The left ventricle pumps blood through the aortic valve.
Blood enters the aorta and is distributed to the rest of the body.
State the electrical conduction system of the heart. Where does the electrical signal travel to and where does it terminate?
Sinoatrial (SA) Node – Located in the right atrium, it is the heart’s natural pacemaker and initiates the electrical impulse, causing atrial contraction.
Atrioventricular (AV) Node – The signal is delayed to allow complete filling of the ventricles.
Bundle of His – Located in the interventricular septum. Conducts the electrical impulse from the AV node to the ventricles.
The Right and Left Bundle Branches – These branches split off the Bundle of His and travel down both sides of the septum. They conduct the signal toward the apex of the heart.
Purkinje Fibers – The impulse spreads through these fibers through the ventricular walls, causing ventricular contraction (systole).
So the electrical signal initiates at the SA node and terminates at the Purkinje fibers where it causes the ventricles to contract, pumping blood out of the heart.
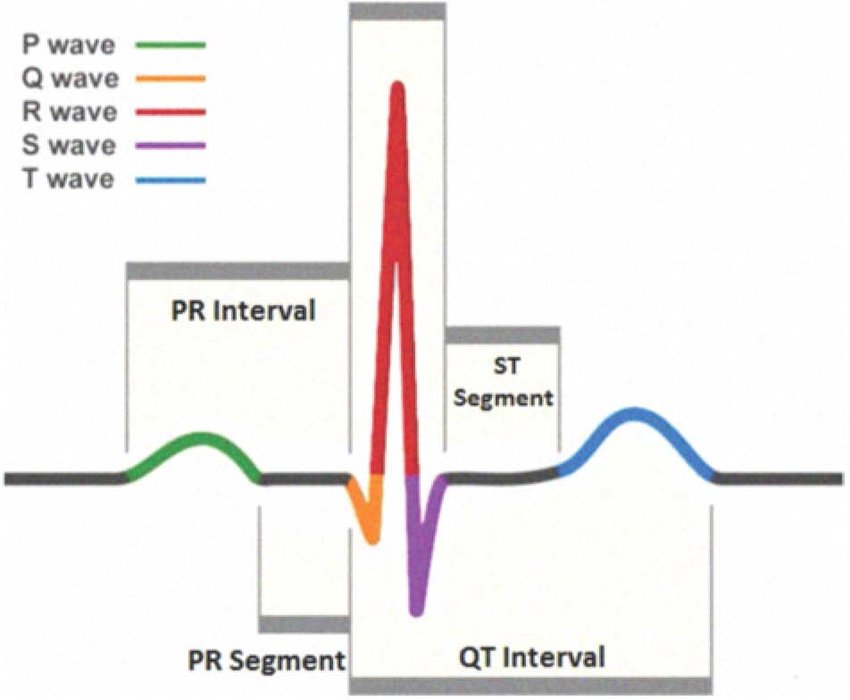
L7: Identify the nerve conduction and contractile phases of the heart for each interval listed below.
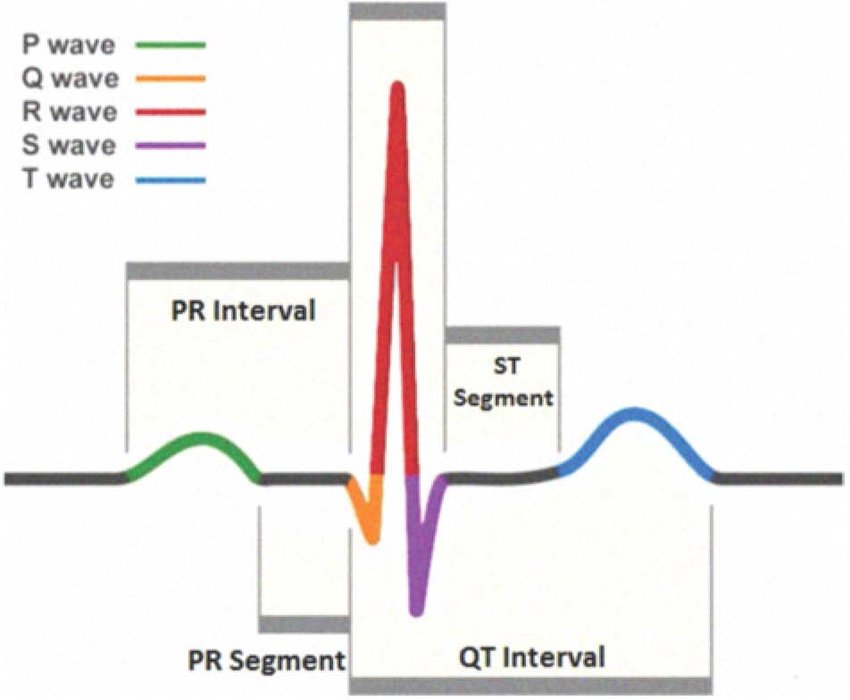
P-R* (start of P to start of QRS)
|
Q-T (start of QRS to end of T)
|
T-Q (end of T to start of QRS)
|
L8: Describe the differences in the type of blood flow at the brachial artery that allows for the determination of blood pressure.
When taking blood pressure, a cuff temporarily stops blood flow through the brachial artery (cuff pressure above systolic). As the cuff releases pressure, two types of blood flow are heard with a stethoscope:
Turbulent flow (Korotkoff sounds): As cuff deflates and falls just below systolic pressure but above diastolic pressure, turbulent flow occurs. This produces Korotkoff sounds, used to determine systolic BP (first sound heard).
Laminar flow (silent): When cuff pressure drops below diastolic pressure, the artery is fully open and blood flows smoothly again (laminar flow). When Korotkoff sounds disappear, this when diastolic pressure is measured.
L8: During the “Pre-immersion” or “Immersion after 5 seconds” intervals did your participant’s Heart Rate increase above resting? What would cause an increase?
Yes, heart rate often increases slightly right after immersion. This is caused by a stress response: cold shock response (sudden exposure to cold water triggers the sympathetic nervous system, causing immediate increase in HR and breathing rate.
Sudden immersion → adrenaline release → ↑ HR.
L8: As time immersed progressed, what did you observe regarding your participants Heart Rate? How might these changes be beneficial?
Heart rate decreased as time immersed increased due to activation of dive reflex. The dive reflex is controlled by the parasympathetic nervous system (via the vagus nerve).
What are the benefits of the reduction in HR?
Conserves oxygen by reducing cardiac workload, and redirects blood flow to essential organs like brain/heart.
Helpful in extending how long the body can go without oxygen like swimming.
As time immersed progressed, what did you observe about the participant’s pulse amplitude? What function does this change serve?
Pulse amplitude decreased over time, indicating vasoconstriction of peripheral blood vessels which decreases blood flow to peripheral tissues like limbs.
Redirects blood to the core and vital organs to conserve oxygen during the dive like heart/brain to prevent excessive heat loss in cold water.
L8: What is the overall goal of all the changes observed during the dive reflex?
The goal of the dive reflex is to conserve oxygen and protect vital organs (especially the brain and heart), help the body survive low oxygen conditions and to increase survival time during water submersion.
Achieved by:
Slowed heart rate (bradycardia),
Vasoconstriction (narrowing of vessels to limbs),
Reduced blood flow to extremities,
And increased blood flow to the brain and heart.
L9: Define Boyle’s law and relate it to pulmonary ventilation. Specifically, how does it apply to inspiration and expiration?
Boyle’s Law: P1V1 = P2V2
Gas law states that pressure and volume have an inverse relationship—when volume of space increases, the pressure within decreases (and vice versa).
During inspiration (breathing in), the diaphragm and intercostal muscles contract, expanding the thoracic cavity → thoracic volume increases → causing the pressure inside the lungs (alveolar pressure) to decrease → Alveolar pressure < Atmospheric pressure → air flows into the lungs because gases always move from high pressure to low pressure.
During expiration (breathing out), the diaphragm and intercostal muscles relax, decreasing the thoracic cavity volume → this volume reduction increases the pressure inside the lungs so that the alveolar pressure becomes higher than atmospheric pressure, forcing air out of the lungs → Alveolar pressure > Atmospheric pressure
**Breathing depends on changing lung volumes to create pressure gradients, as described by Boyle’s Law
L8: What differences do you observe between FVC, FEV1.0 and (FEV1.0/FVC) x 100 in comparison to exercise 2? What accounts for these differences?
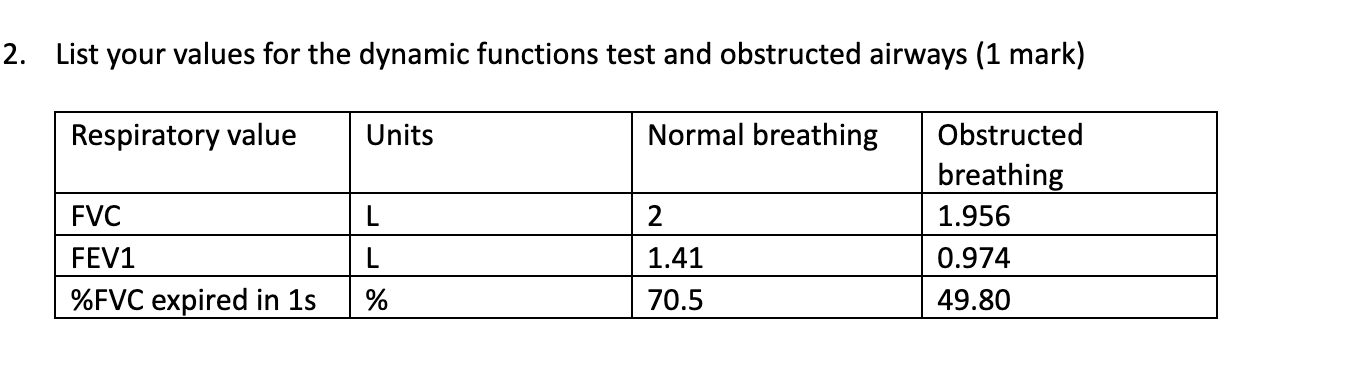
The FVC (force vital capacity) decreased in the obstructed condition, airflow restriction made it harder to exhale quickly.
The FEV 1.0 (force expiratory volume in 1 sec) dropped significantly as narrowed airways slow the rate of airflow.
The FEV1.0/FVC x 100 = %FVC expired in 1 second decreased dramatically due to the obstruction.
What accounts for these differences?
The FEV₁ and %FVC expired in 1 second are significantly reduced under obstructed breathing because in obstructive pulmonary conditions, airways narrow, increasing resistance and slowing expiration.
FVC is only slightly lower, which is expected because the total lung volume doesn't change much — just the rate of air movement is affected.
L8: What accounts for the differences (if any) between FVC in the two conditions?
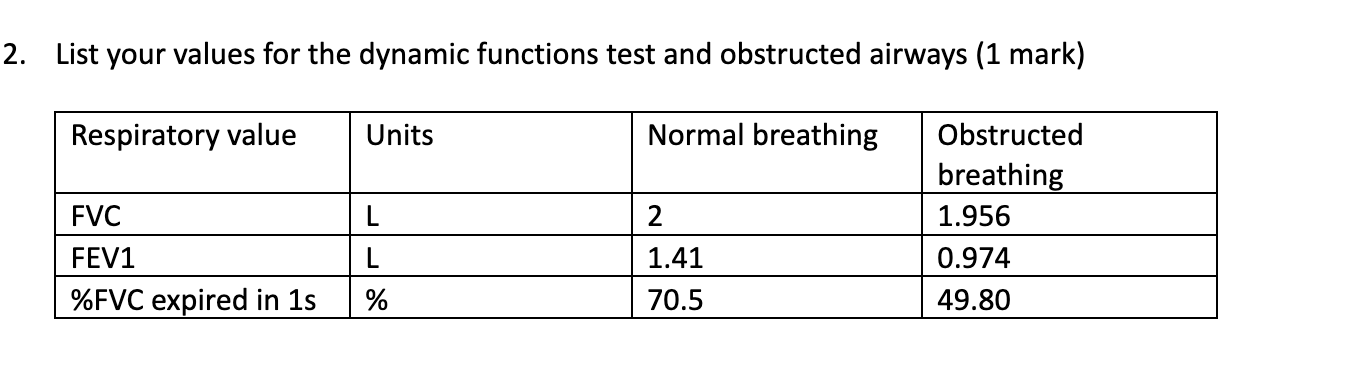
FVC is slightly lower in the obstructed condition (1.956 L vs 2.000 L).
This could be due to:
restrictive pulmonary diseases
Incomplete exhalation because of airway resistance.
Fatigue or discomfort during the obstructed test.
Slight air trapping in the lungs due to obstruction.
L8: What accounts for the differences of FEV₁ and %FVC expired in 1s between the two conditions?
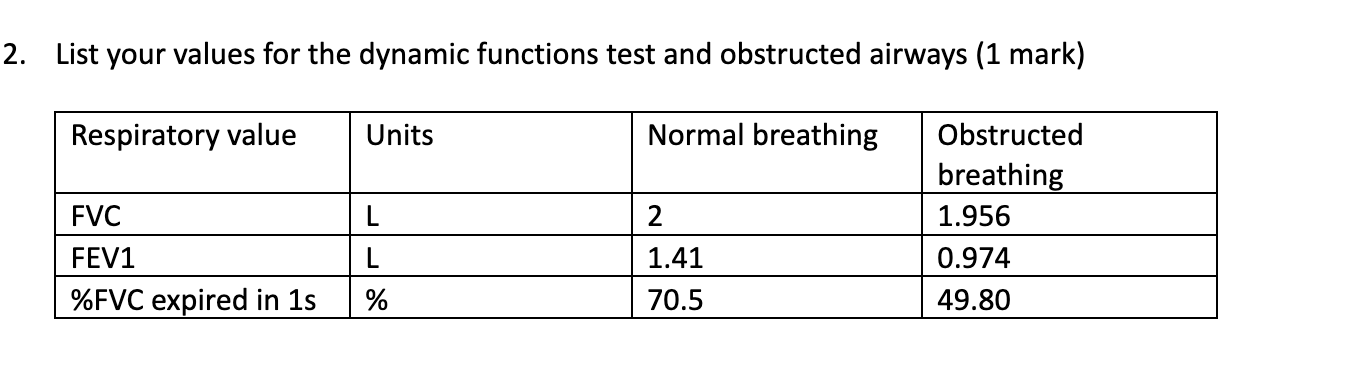
FEV₁ and %FVC in 1 second (FEV₁/FVC × 100) can be reduced due to:
obstructive pulmonary diseases
Obstructive conditions (e.g., asthma, COPD): Narrowed airways slow airflow → ↓FEV₁ and ↓ratio.
Fatigue, increased airway resistance, or poor technique can also reduce these values.
In healthy lungs, the %FVC expired in 1 sec is typically ~80% or more.
L10:
Calculate the clearance of inulin given the following values:
Concentration of inulin in plasma (P) = 0.1 mg/L
Concentration of inulin in urine (U) = 6 mg/L
Urine flow rate (V) = 2 mL/min
L10: If inulin is filtered, but neither reabsorbed nor secreted, what physiological variable that pertains to renal function is approximately equal to the clearance of inulin?
Glomerular Filtration Rate (GFR)
Because inulin is freely filtered by the glomerulus, and neither reabsorbed nor secreted by the nephron, its clearance is equal to the Glomerular Filtration Rate (GFR) — making it a gold standard for measuring it.
GFR ≈ Clearance of inulin
L10: List the pathway of filtrate/urine from the Bowman’s capsule until it leaves the nephron.
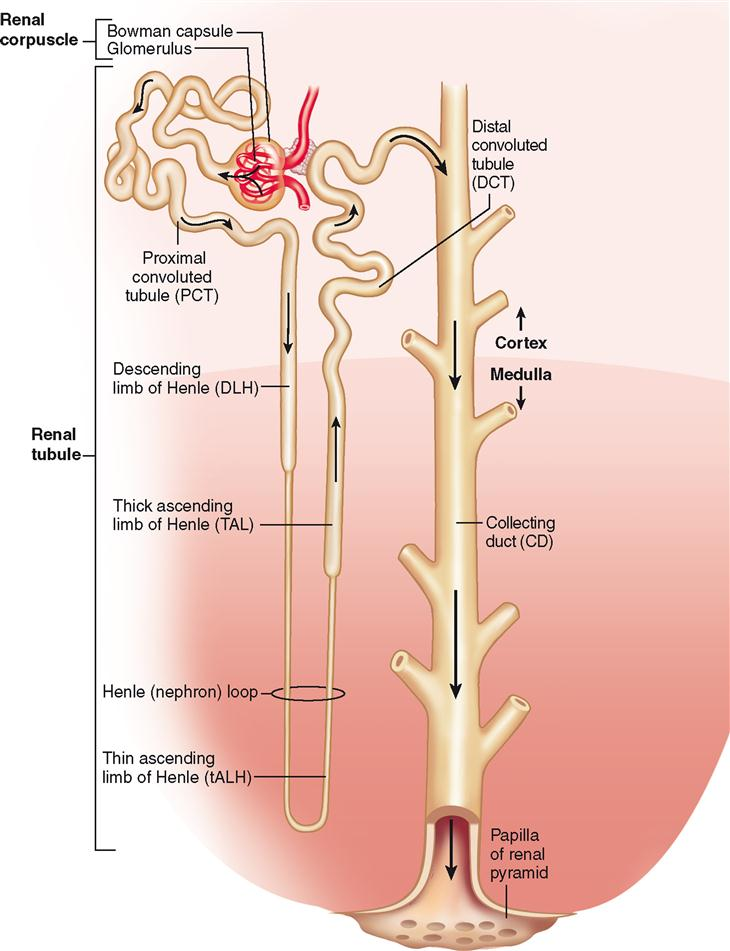
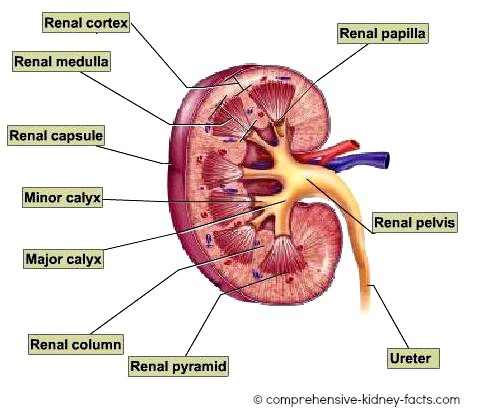
Bowman's capsule - filtration occurs here.
Proximal convoluted tubule - reabsorption of water, ions, and nutrients.
Loop of henle - descending limp is responsible for water reabsorption while the ascending loop is responsible for ion reabsorption.
Distal convoluted tubule - further ion and water reabsorption.
Collecting duct - final water reabsorption and ion reabsorption.
Renal papilla - urine leaves the collecting ducts here.
Minor/major calyx - collects urine from the renal papilla.
Renal pelvis - funnel -like structure that directs urine out of the kidney.
Ureter - urine travels to the bladder.
Bladder - stores urine until elimination.
Urethra - where urine exits the body.