Module 6.4: Physiology of Respiration @ High Altitudes
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
As altitude increases
The barometric pressure falls exponentially
-Barometric pressure drops by ½ for every 5,000 m or 18,000 ft of ascent
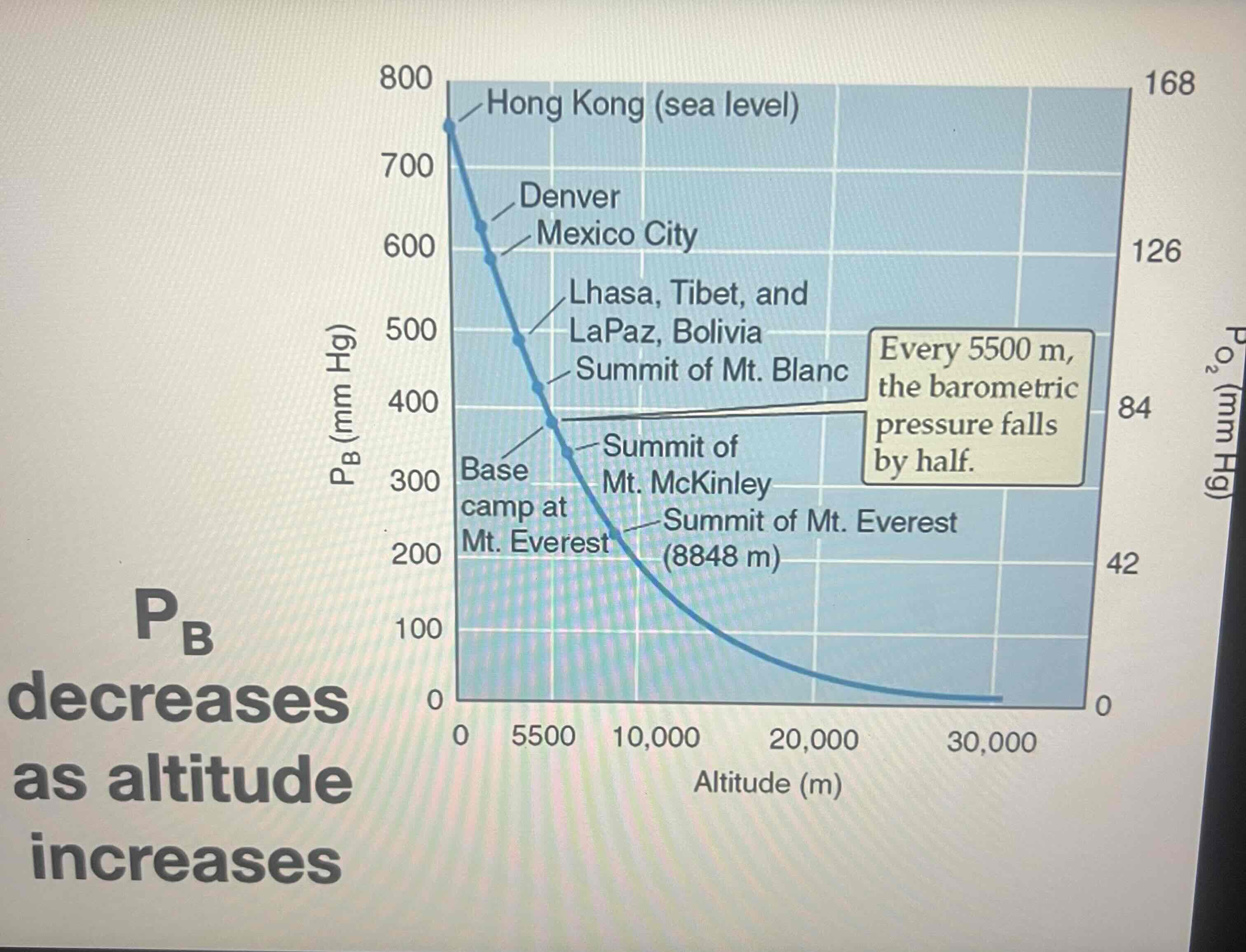
Left y axis shows
Barometric pressure
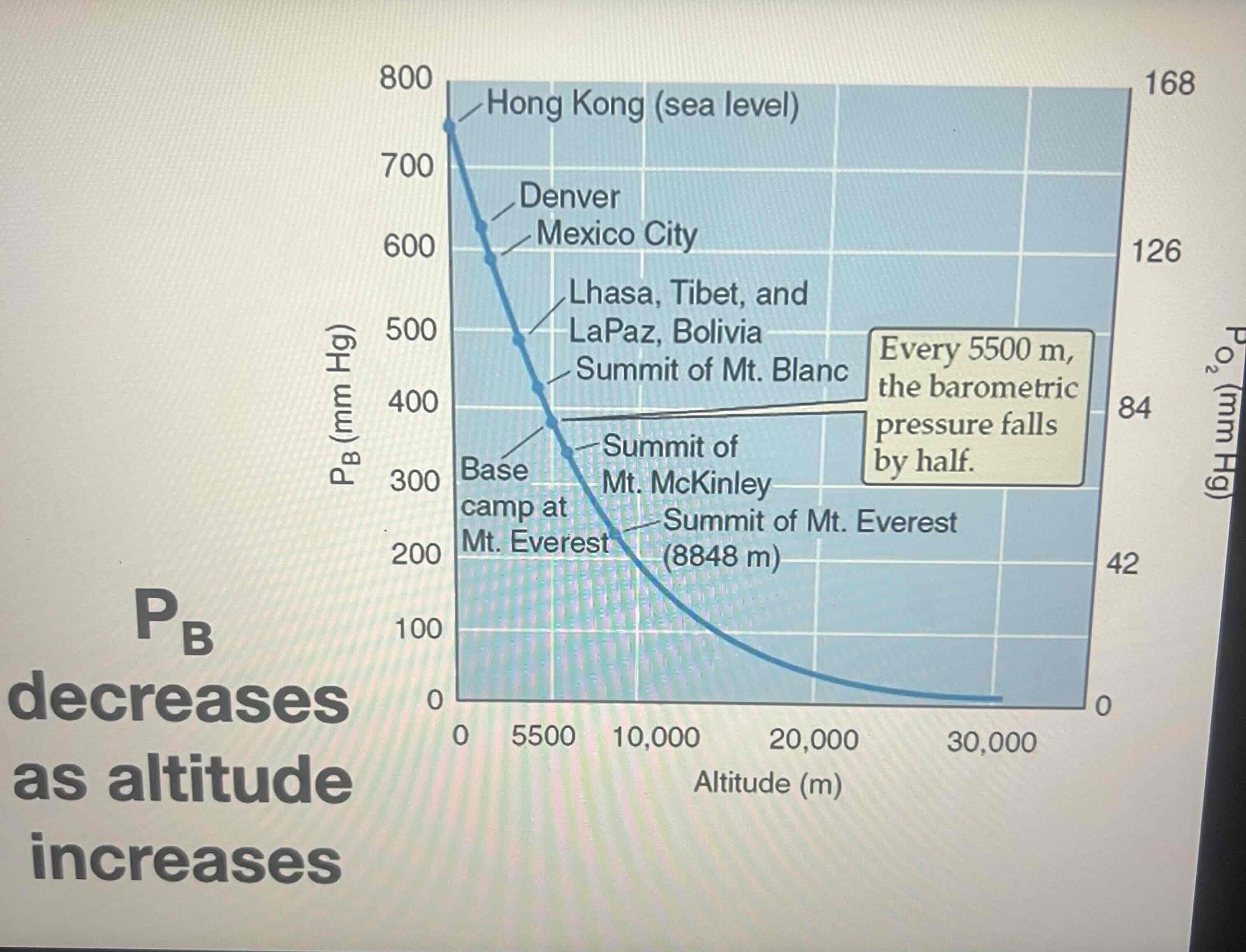
Right y axis shows
Partial pressure of O2
the Fraction of air is made up by
A gas that does NOT change
Fraction for O2
0.21 no matter where you’re on Earth
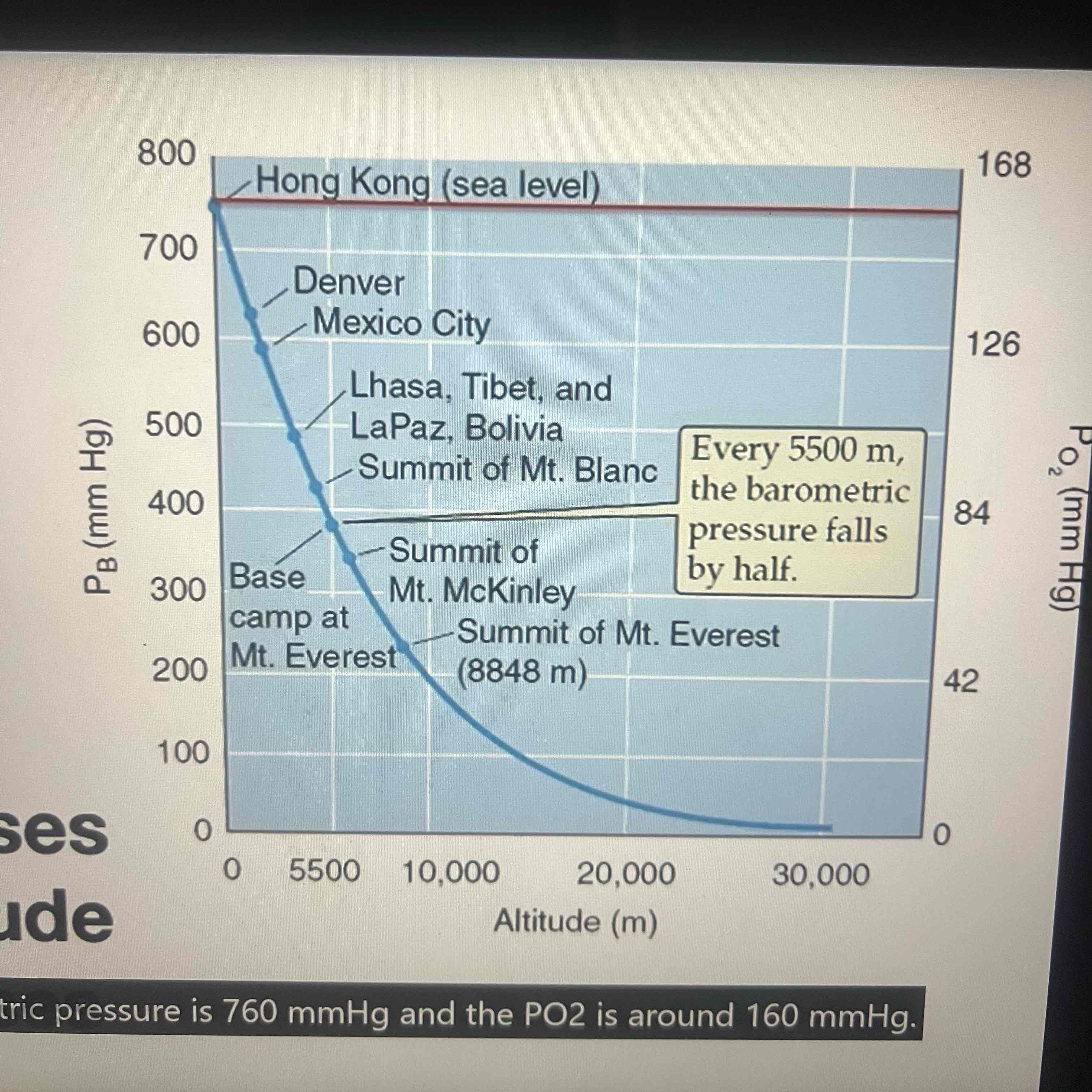
Ex: Hong Kong @ sea lvl
Barometric pressure is 760 mmHg
PO2 is 160 mmHg
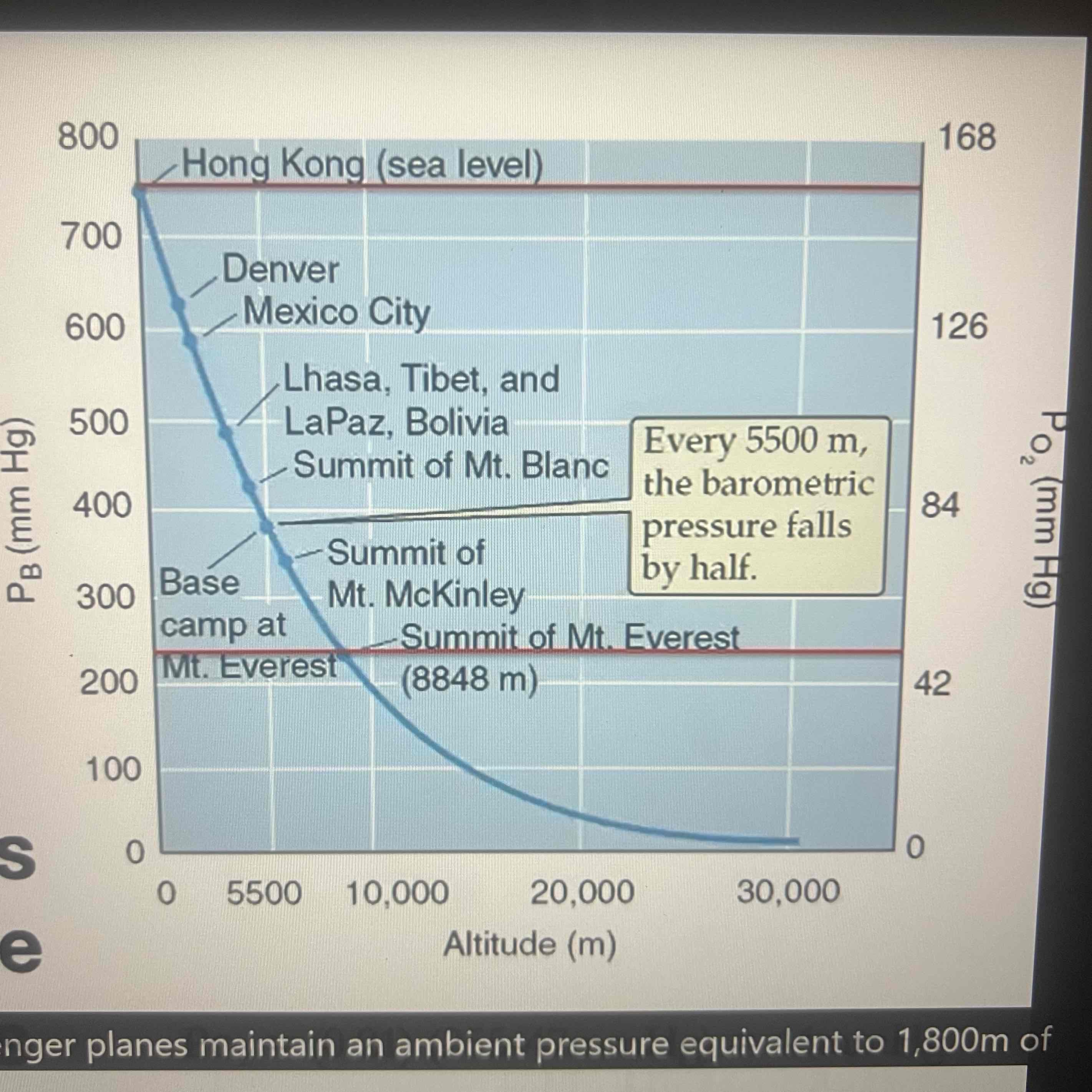
Ex: Summit of Mount Everest
Barometric pressure is 255mmHg
PO2 is 44 mmHg
must subtract partial pressure of water vapor from
barometric pressure before applying fraction
Inspire air is warmed & humidified &
@ 37C: the saturated water vapor pressure in the lungs is 47 mmHg regardless of altitude
Pressurized cabins in passenger planes
Maintain an ambient pressure equivalent to 1,800 m of altitude in cross continental flights or 2,400 m of altitude in transoceanic flights
Most don’t need supplemental oxygen in the inspired air @ Denver or other ski resorts SO
Most passengers are NOT bothered by the slight reduction in arterial oxygen saturation that’s associated w/ these cabin pressures
-89% @ 3,000m
Passengers w/ COPD
May need to carry supplemental oxygen on a plane even if they don’t require it @ sea level
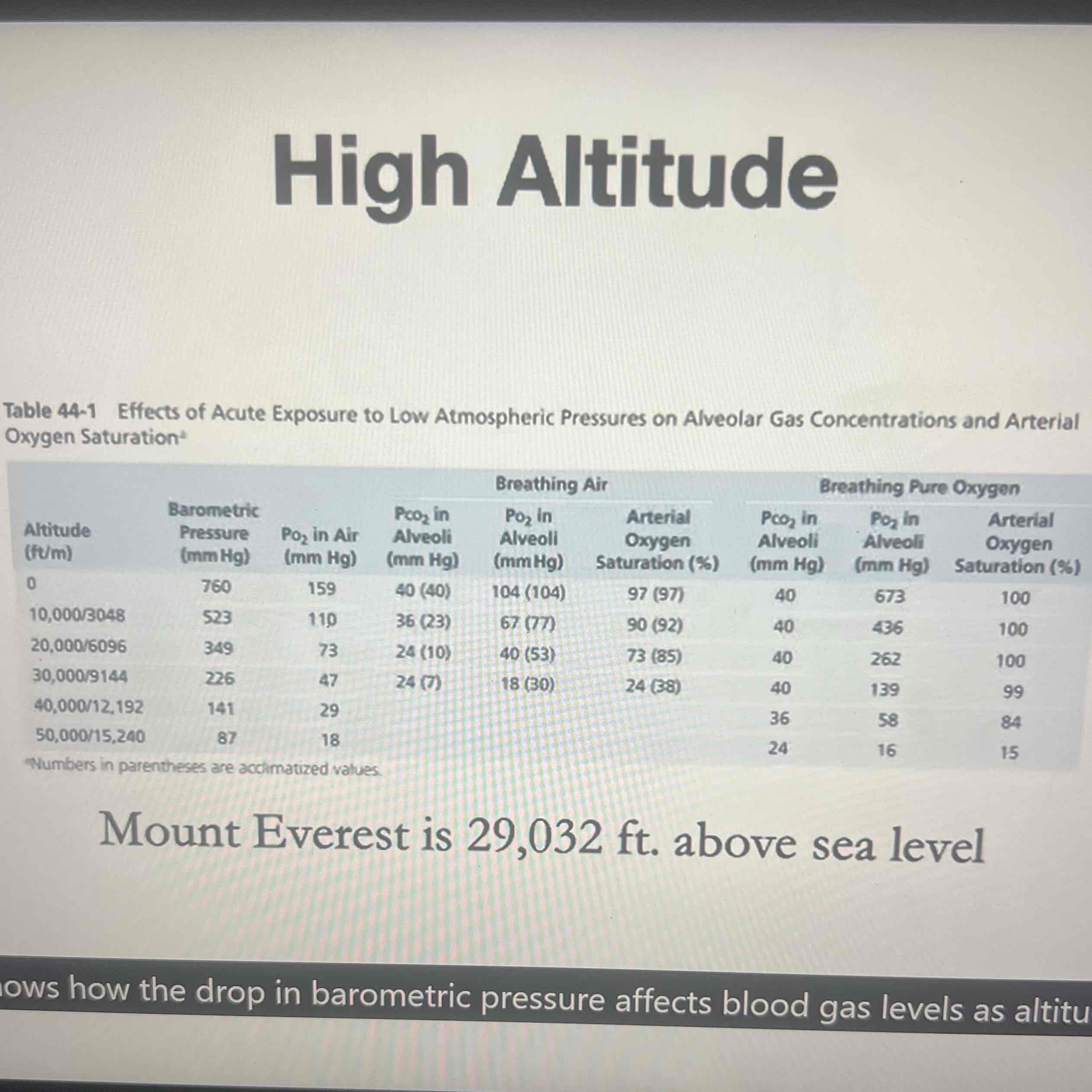
The drop in barometric pressure affects blood gas levels as altitude increases
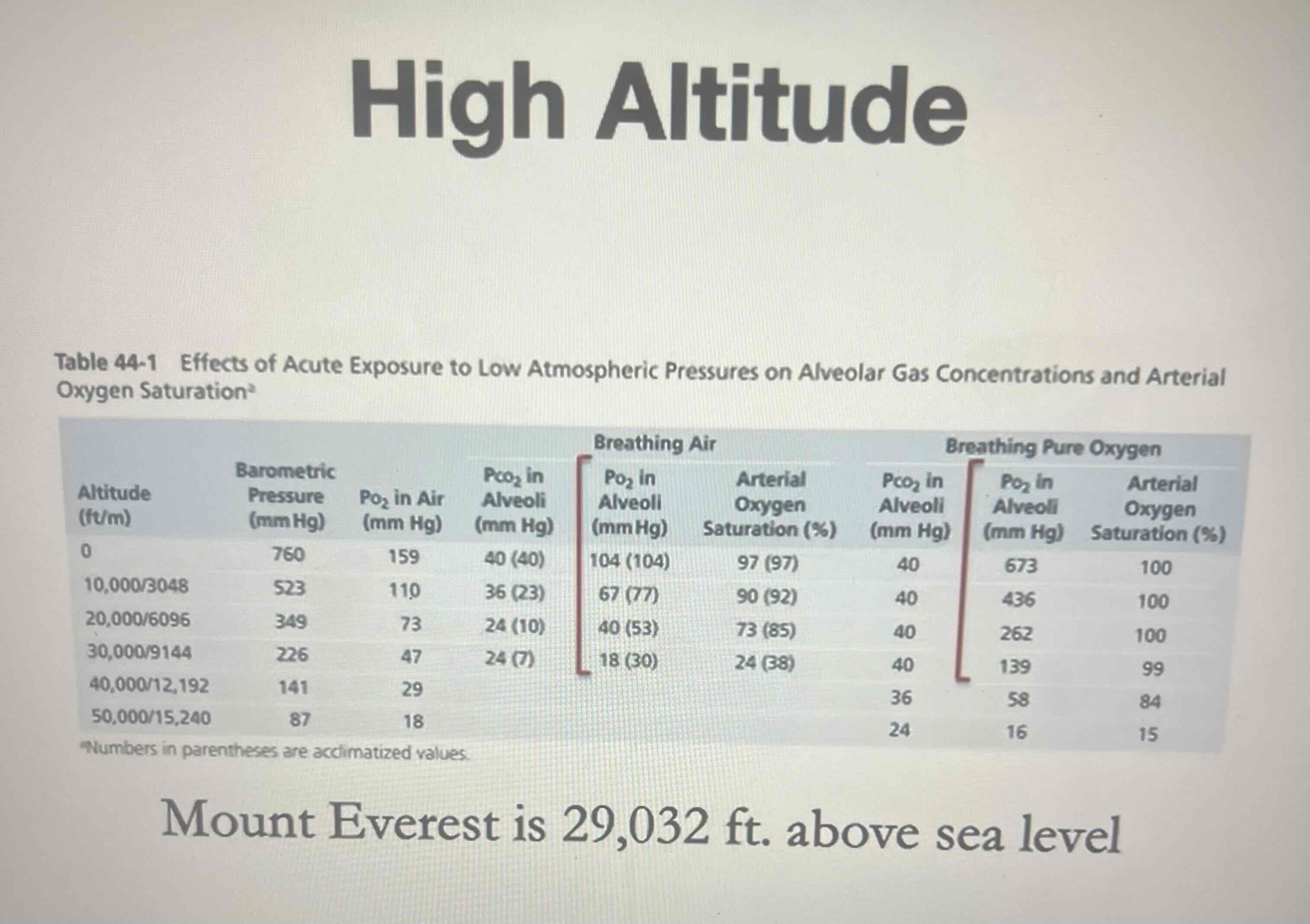
Partial pressure drops
In proportion to the decrease in barometric pressure
-Occurs whether a person is breathing in the air or whether they’re breathing pure oxygen
Benefit of utilizing oxygen @ very high altitudes as an aviator would
Is that near a normal partial pressure of O2 can still be achieved @ 30, 000 feet above seal level
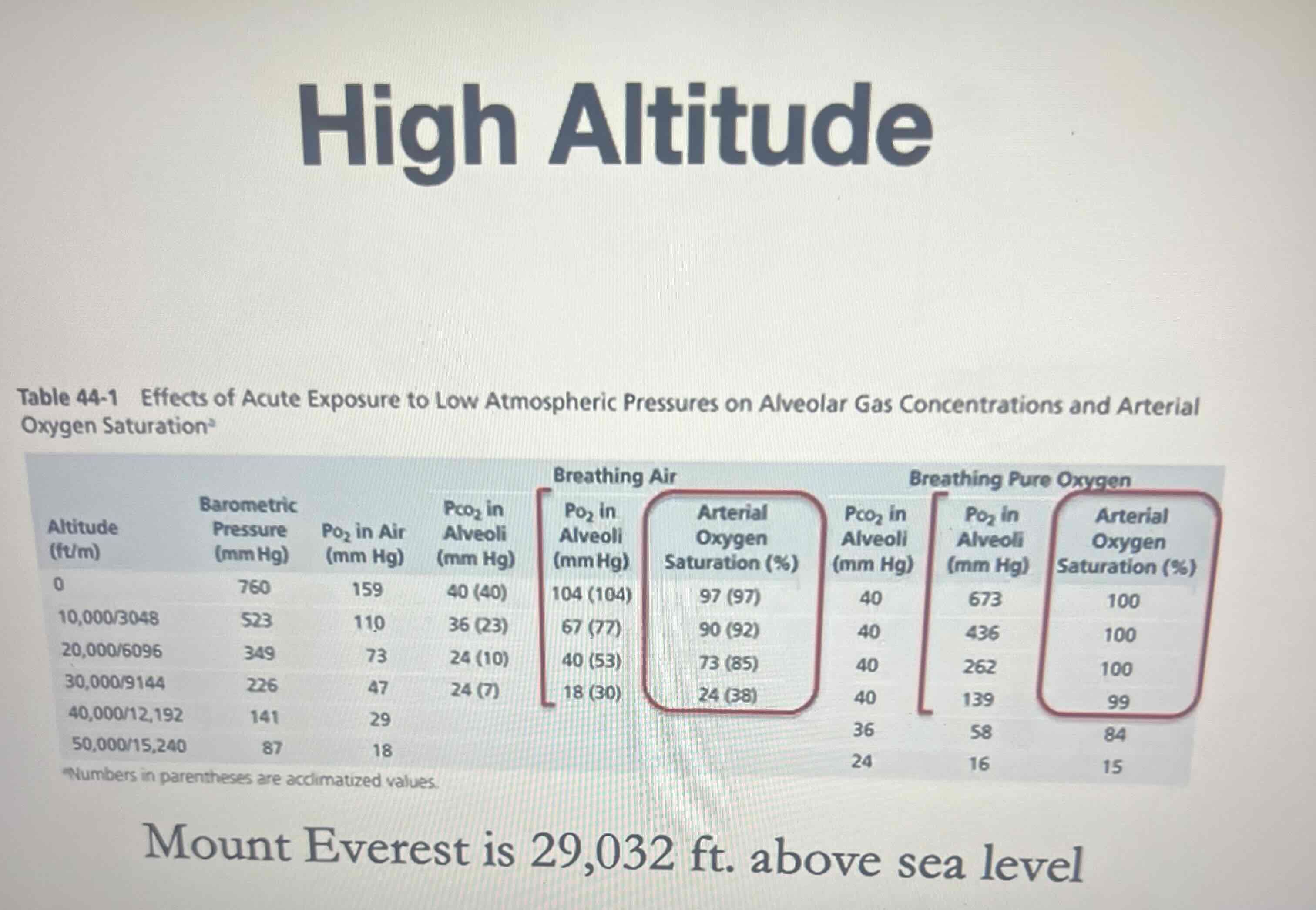
Most notable is the difference in arterial oxygen saturation levels
Which is a measure of oxygen carried by hemoglobin
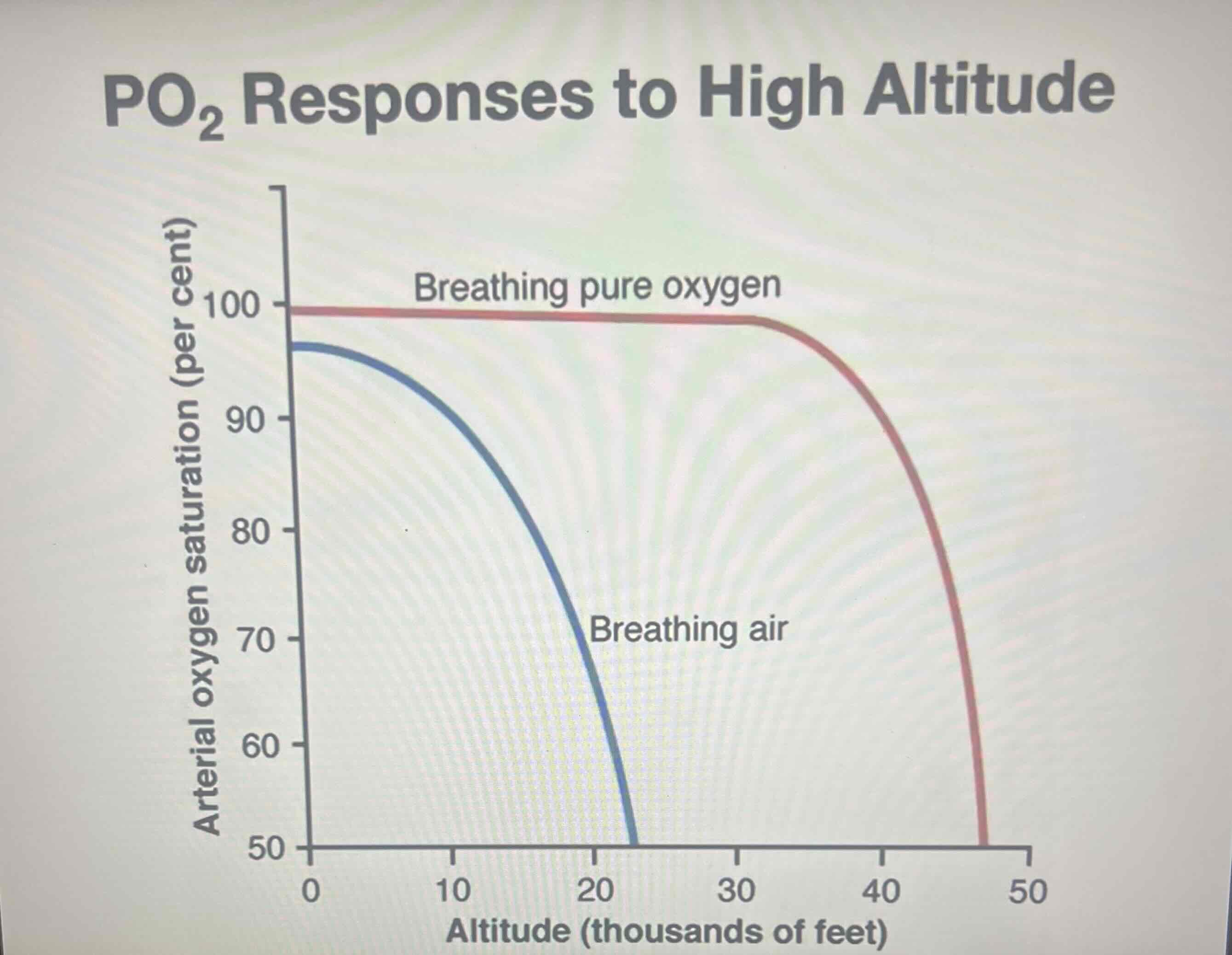
If saturation values vs altitude were graphed
We see just how much of a difference it makes @ altitudes that are typical of airline travel
Whistler Blackcomb @ 5,000 ft above seal level
Altitude related sickness in healthy individuals is very rare
Machu Picchu (Peru) @8,009 ft above seal level
Travelers may experience altitude related illness depending on the rate of ascent & how high they climb
Altitude sickness normally starts @
~8,000 ft above seal lvl
Highest peak in Africa @ over 19,000 ft
-barometric pressure is less than ½ @ sea level
Extreme altitude: Peak of Mt. Everest
Which height the barometric pressure is around 1/3 that @ sea level
How would you feel after recent altitude gain to more than 8,000 ft above sea level?
-feels like a bad hangover: vomiting, weakness, dizziness, fatigue & trouble sleeping
Acute mountain sickness
If severe: can cause acute cerebral or pulmonary edema
Chronic mountain sickness
Results from the body’s adaptation to the change in elevation
-Some changes include:
-increase in Red blood cell mass
-increase in pulmonary arterial pressure
-enlargement of the right heart
CO2 levels in the blood
Is a major stimulus for controlling breathing
@ high altitudes: the drop in O2 is due to the fact that
The barometric pressure is lower than we’re accustomed to rather than due to an increase in O2 consumption from metabolism
-Would prod. Elevated CO2 in the blood
@ high altitudes: you can have a low arterial PO2
W/out a corresponding rise in arterial PCO2
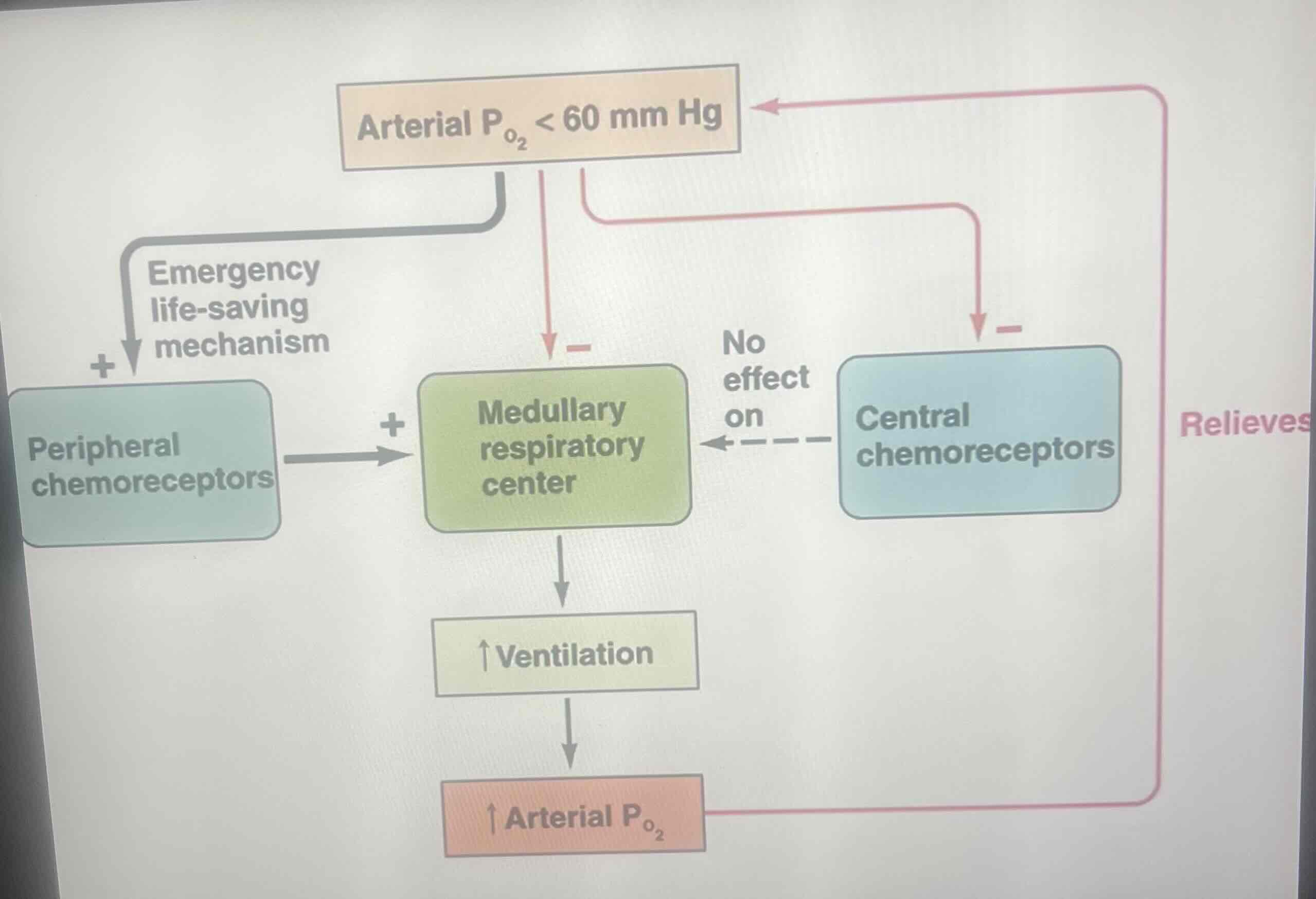
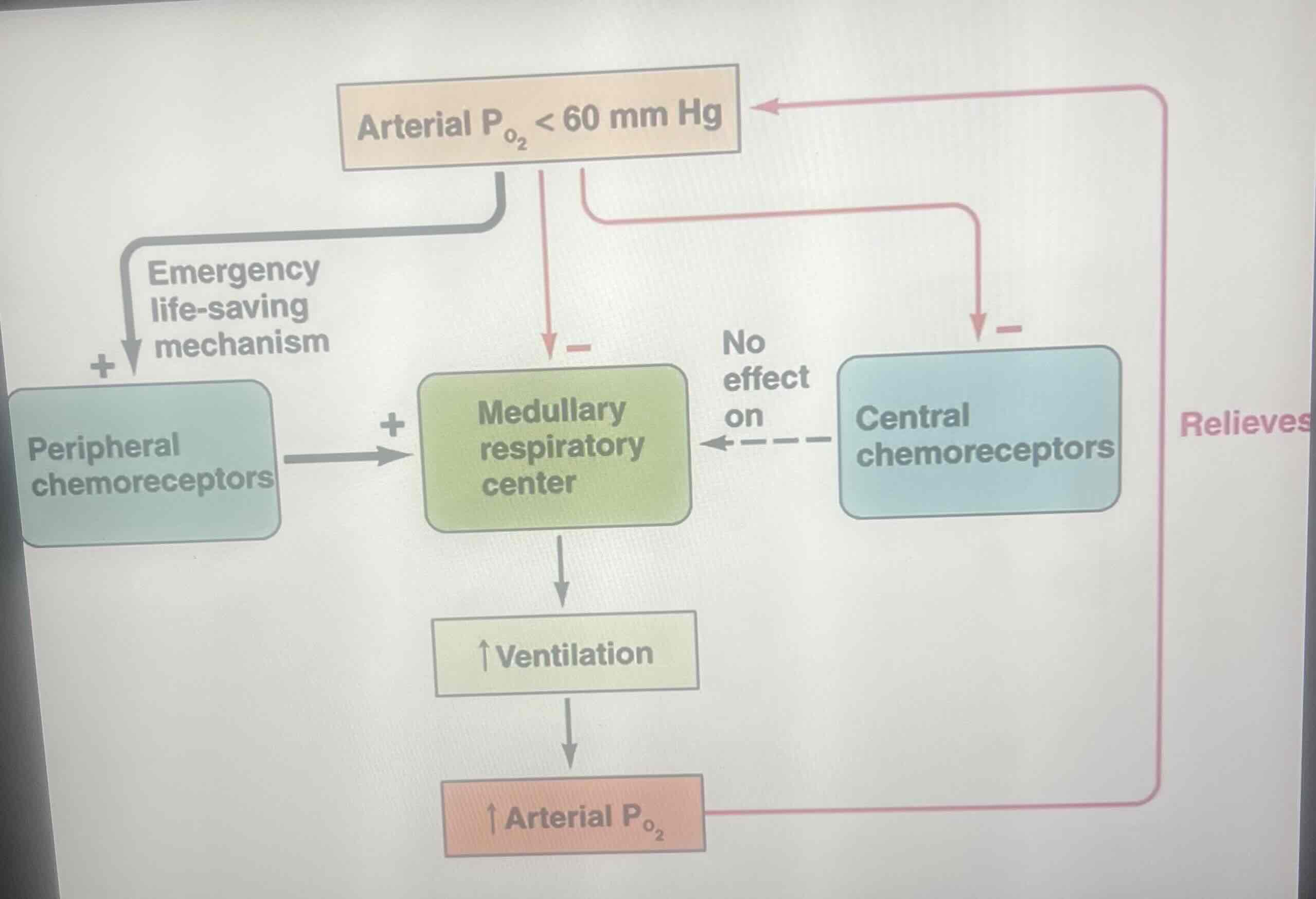
Peripheral chemoreceptors
Do respond directly to a drop in oxygen
-Activation of this mech. is very important when the oxygen supply is inadequate BUT there hasn’t been an increase in CO2 production as would occur @ high altitude in an unpressurized cabin in a aircraft
Some folks that live in high altitudes (in the Andes)
Have enlarged carotid bodies as a consequence of low oxygen tension over a long term
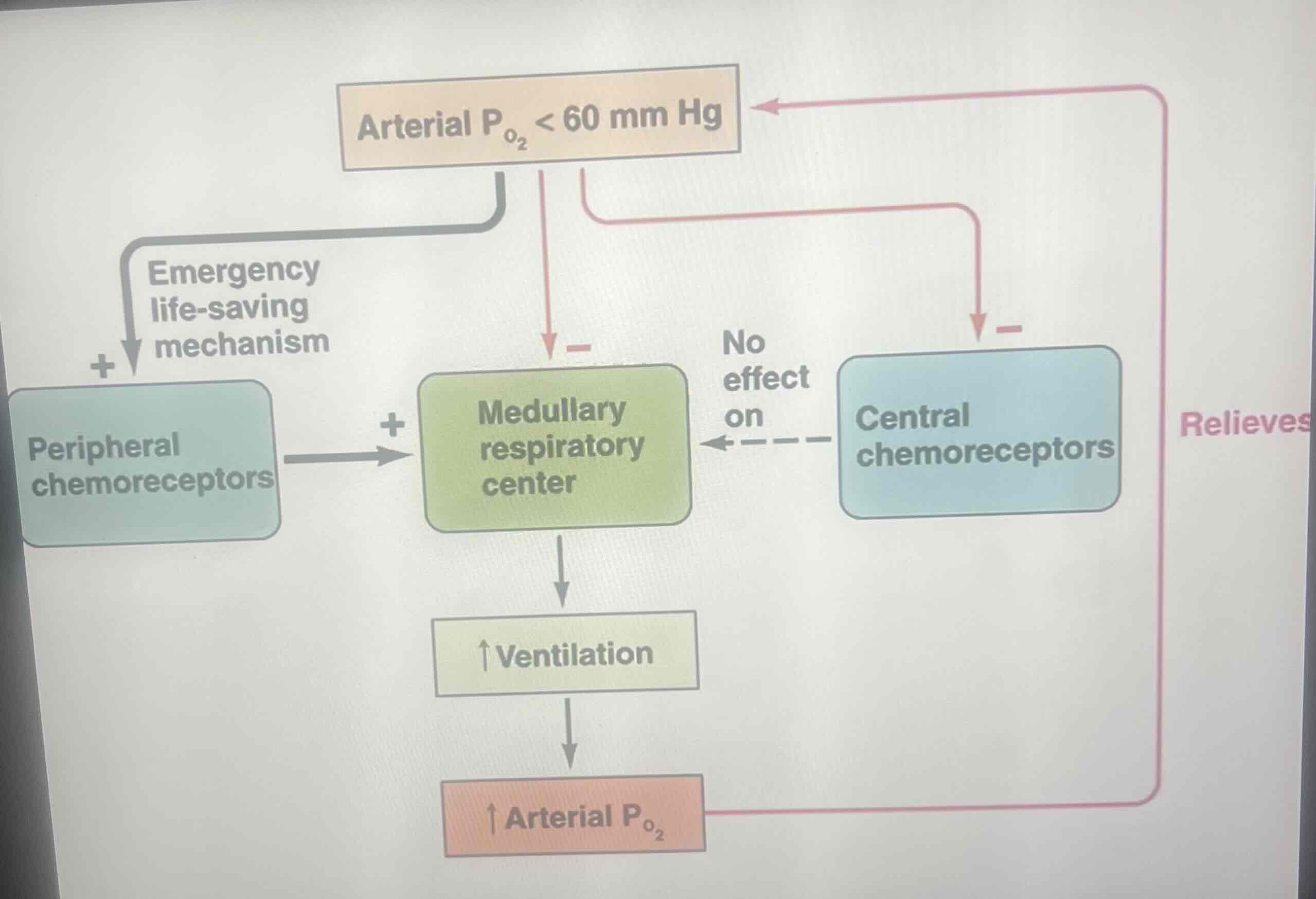
Peripheral chemoreceptors mainly sense
A decrease in arterial PO2 levels once they drop below 60 mmHg as w/ exposure to high altitude or in diseased states
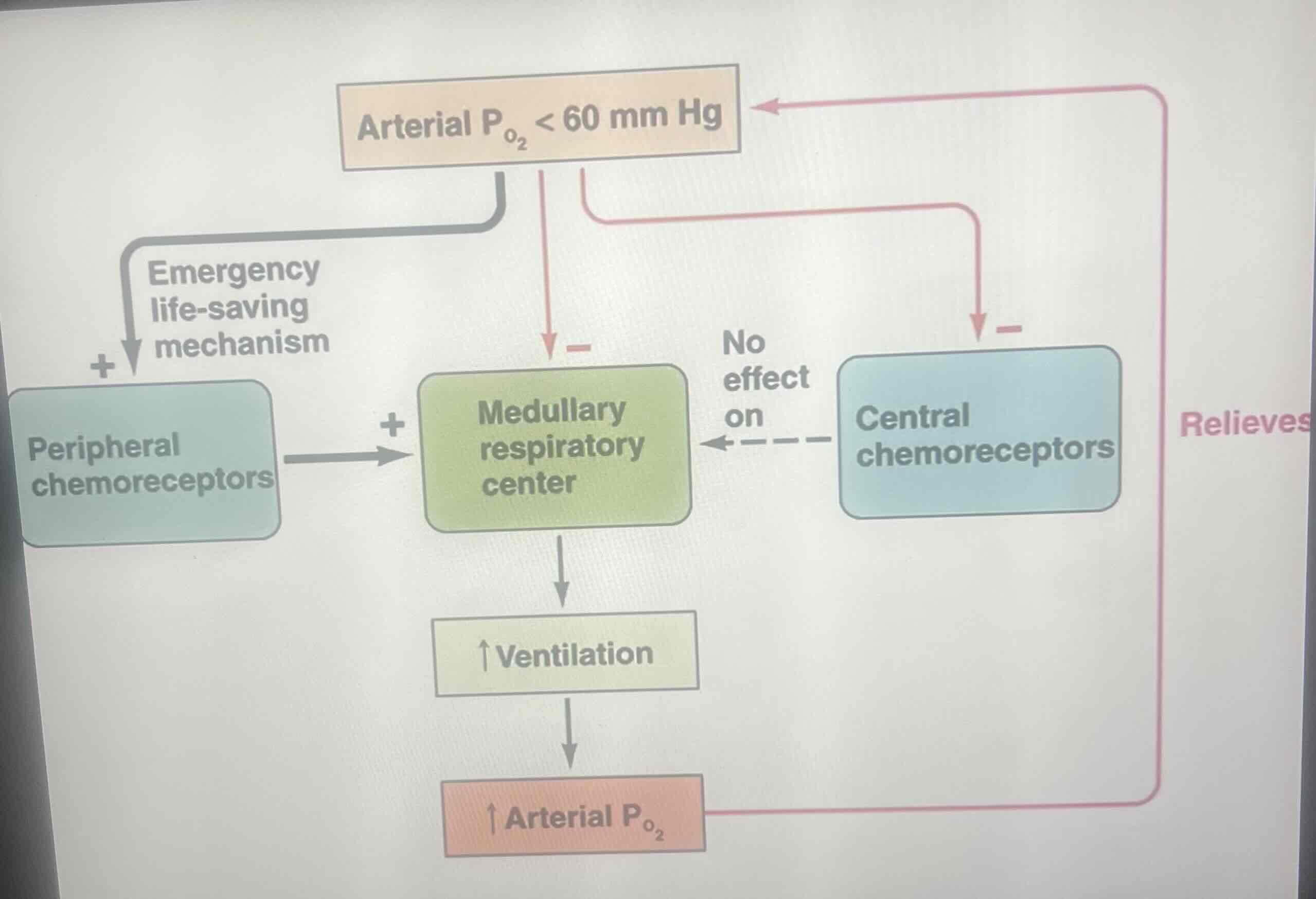
Ventilatory response to such a decrease in arterial oxygen
Is hyperventilation
-Result: In a decrease in arterial CO2 & increase in arterial O2
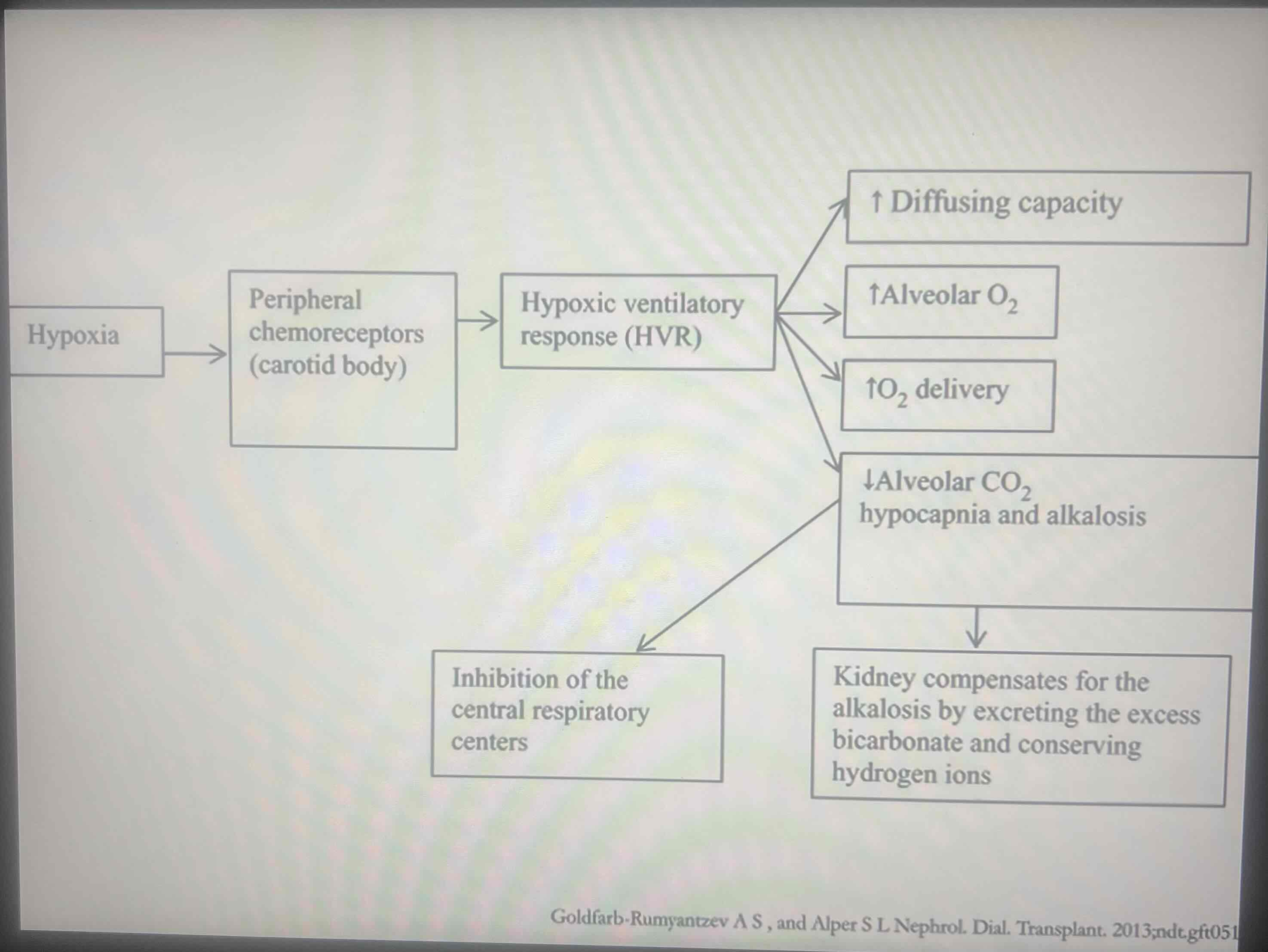
Conditions of hypoxia
Trigger the carotid bodies to initiate the hypoxic ventilatory response
Hypoxia in the body causes
A reflexive change in the breathing rate
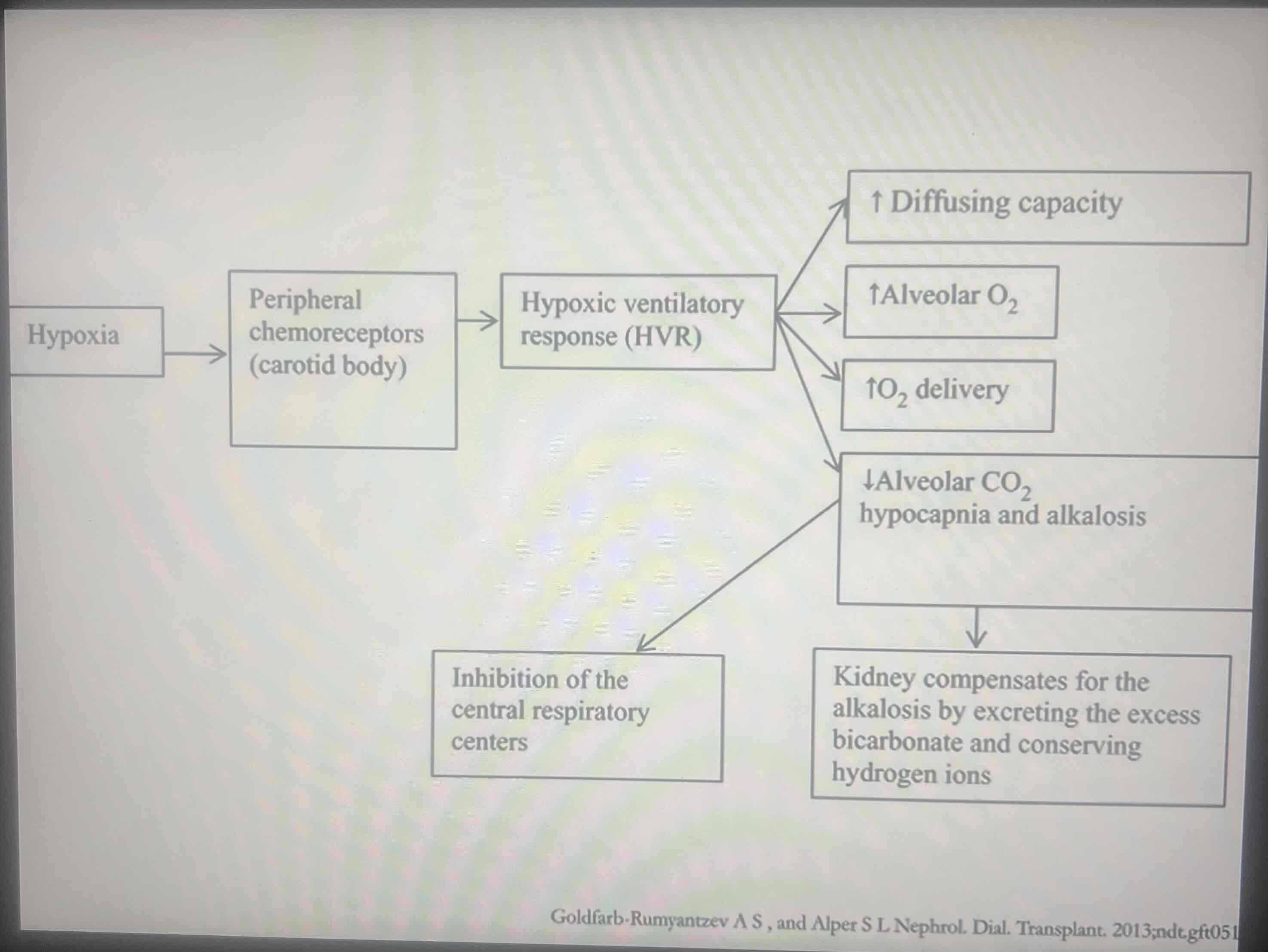
There’s 4 results in response to hypoxia causing a reflexive change in the breathing rate (Hypoxic ventilatory response)
1: A 2- to 3-fold increase in the diffusing capacity (DL) occurs due to a rise in the blood
2:
Hypoxic ventilatory response 1 results in
A 2- to 3-fold increase in the diffusing capacity (DL) occurs due to a rise in the blood volume of the pulmonary capillaries
Hypoxic ventilatory response (2- to 3-fold increase in diffusing capacity) results in an increase in the pulmonary arterial pressure CAUSES
An increase in perfusion to well ventilated apex regions in the lungs
Hypoxia also promotes
The expression of oxidative enzymes in the mitochondria
-Enhances the tissues’ ability to extract O2 from the blood
Elevated ventilation rates
increase alveolar O2 & decrease CO2 in the lungs & blood which causes blood pH to rise
To compensate for these changes that were initiated by a ventilation change
The kidney increases the excretion of bicarbonate to remove excess base from the bloodstream
Sometimes: climbers take acetazolamide
A carbonic anhydrase inhibitor in the kidney that allows the kidney to get rid of extra bicarbonate
acetazolamide
Prevents the formation of protons so that the Na+ proton exchange in the rebake tubule is prevented & Na+ is then excreted along w/ bicarbonate in the urine
By preventing proton formation
acetazolamide Prevents the formation of additional bicarbonate as well
Overall: acetazolamide functions as
A diuretic that alkalinizes the urine as it removes base from the blood to bring the pH back to balance
Hypoxic condition affect
vascular system too
Erythropoietin production
Stimulated by renal hypoxia & norepinephrine
-Increases RBC & hemoglobin production to enhance the O2 carrying capacity of the blood
Byproduct of an Increase in RBC & hemoglobin production to enhance the O2 carrying capacity of the blood is
An increase in the hematocrit & blood viscosity due to reduced plasma volume
Hypoxic conditions in the vascular system STIMULATES
Hypoxia-inducible factor-1 alpha
Hypoxia-inducible factor-1 alpha
A transcription factor that activates genes involved in erythropoiesis, angiogenesis & other processes
Tissue angiogenesis occurs
w/in days of exposure to hypoxic conditions & is triggered by growth factors that’s released by hypoxic tissues like vascular endothelial growth factor, fibroblast growth factor & angiogenin
growth factors that’s released by hypoxic tissues like vascular endothelial growth factor, fibroblast growth factor & angiogenin results in
A dramatic increase in tissue vascularity caused by hypoxia
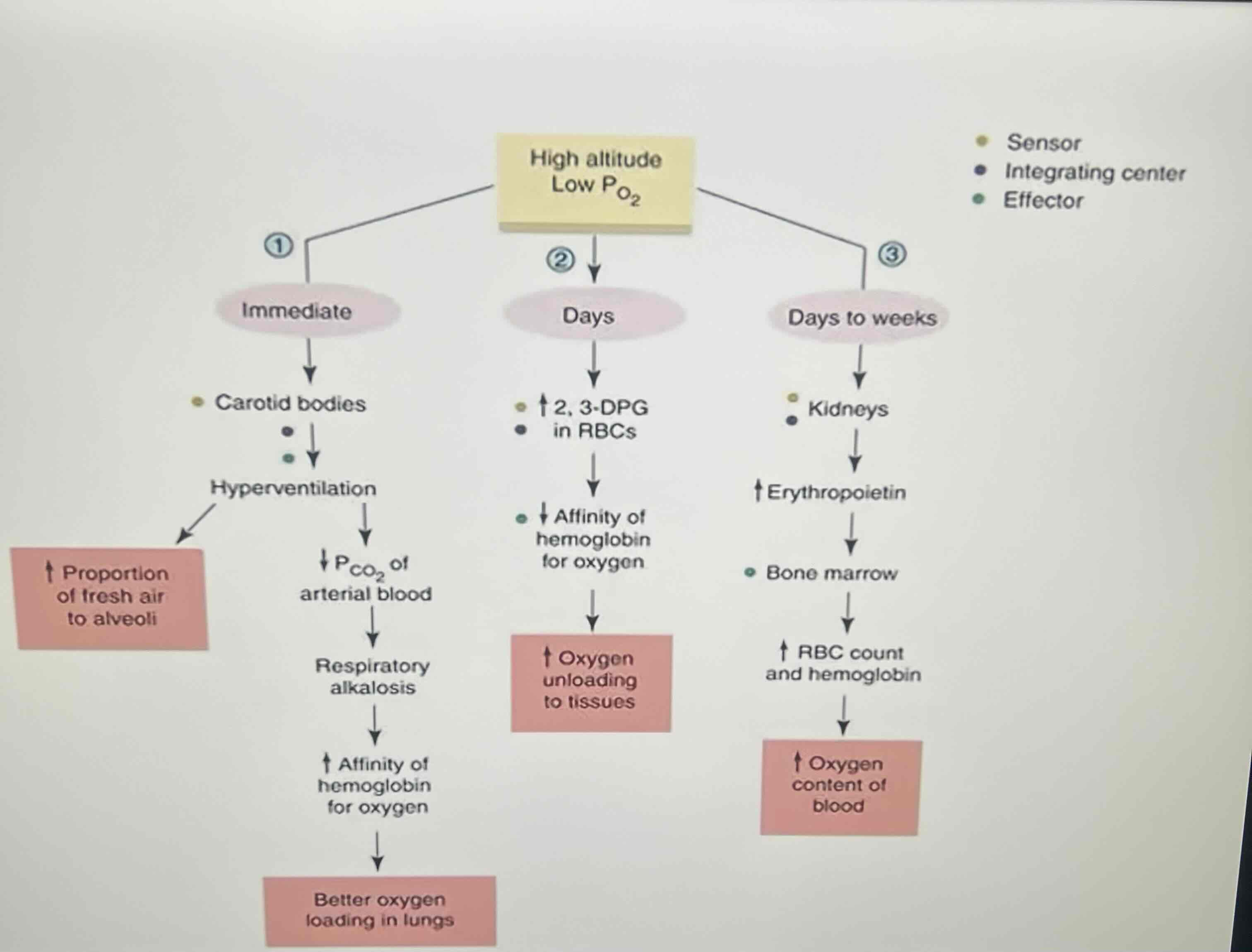
Chart shows
Various timing of the physiological changes in response to low O2 levels in the high altitude atmosphere
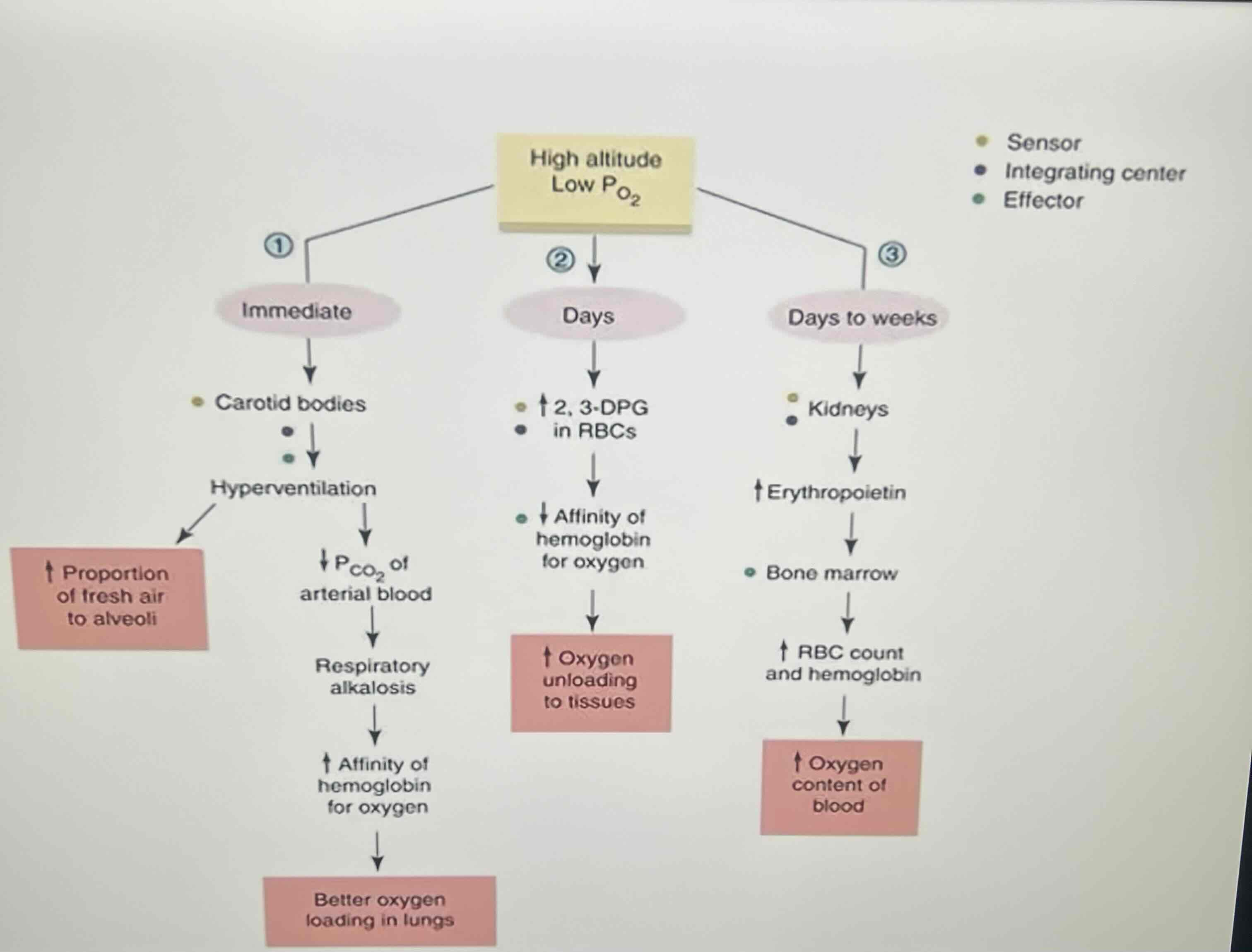
Left shows
The immediate response
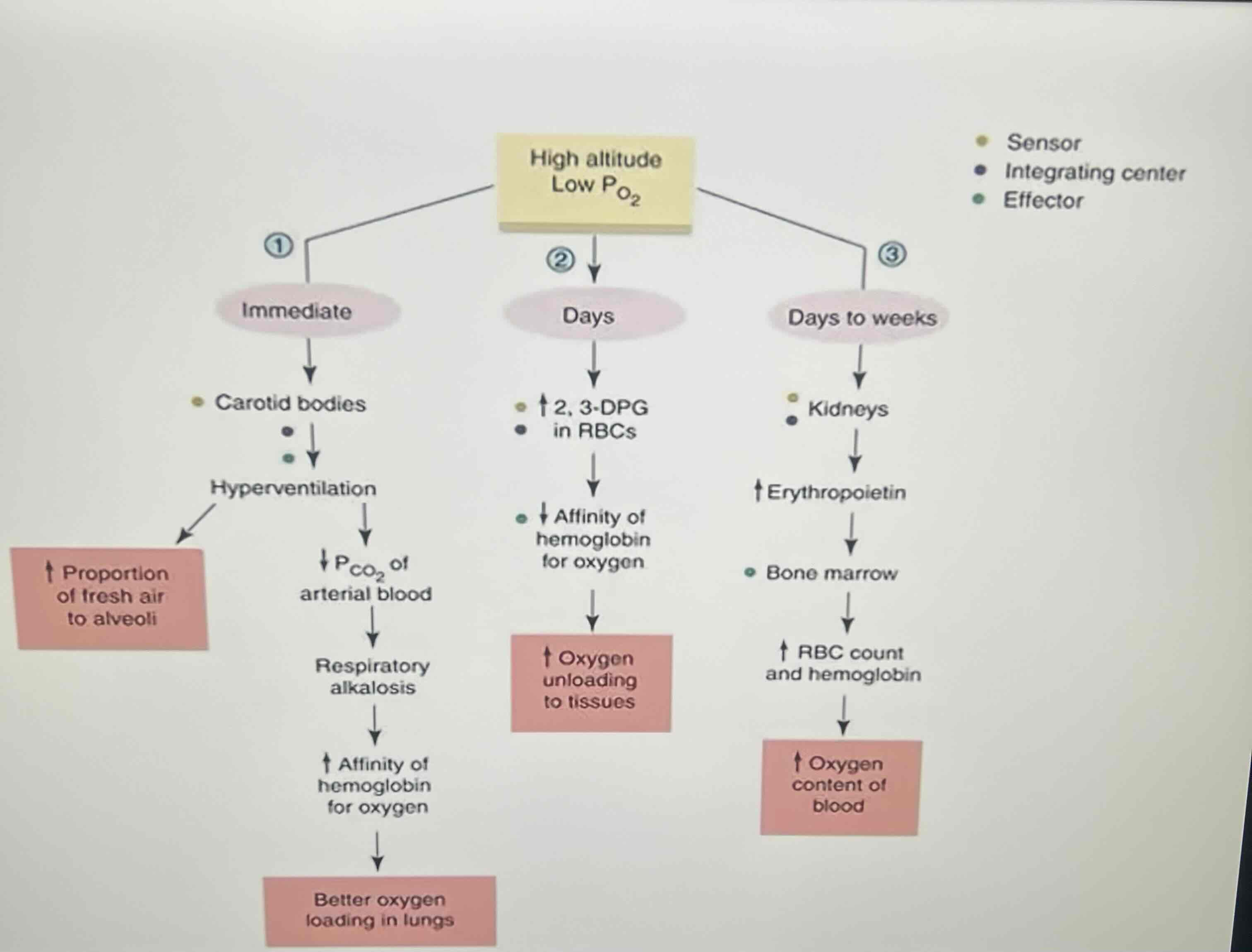
Middle shows
Changes that would occur w/in a few days
-Includes the effects of changes to gene expression upon exposure to hypoxic conditions
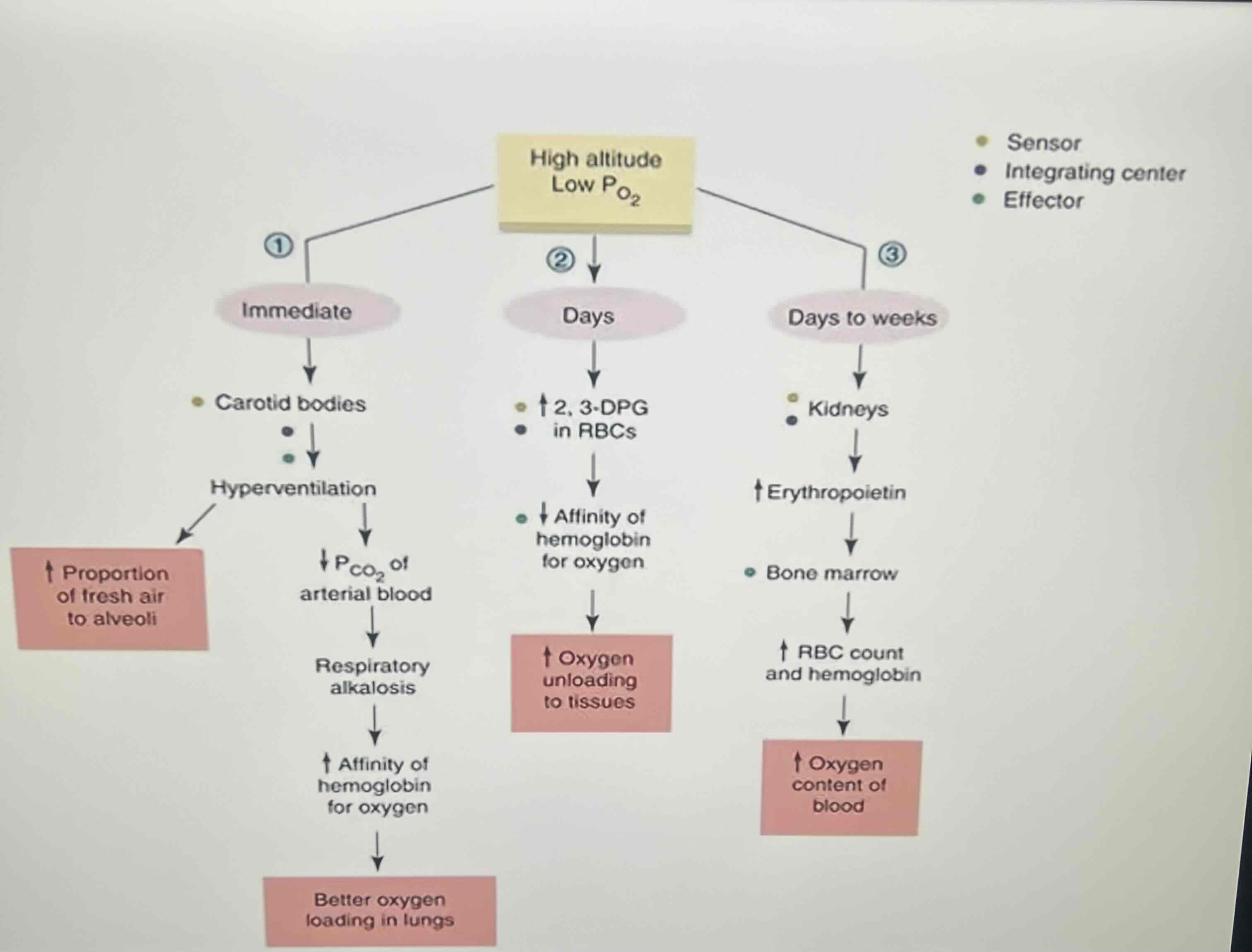
Right shows
Long term change from sea level to high altitudes results in acclimatization of the body
Moving from an initial increase in ventilation rate & lower than normal hemoglobin saturation TO THE
Increased production of erythropoietin & increased vascularization of tissues to enhance O2 delivery
Major ways that the body acclimatizes to high altitudes
-Increased ventilation
-Due to decreased PO2
-Increase slowed by decreased PCO2
-Increased hematocrit (content)
-Increased diffusing capacity
-Increases capillary
Diffusing capacity increases in Acclimatization BC
The increased ventilation & therefore lung volumes cause an increase in the surface area for O2 diffusion to occur across the alveolar membrane in accordance w/ Fick’s law
Increase in RBCs & capillary density work
To enhance O2 delivery to the tissues
Decreasing PO2
Stimulates ventilation as a means of increasing arterial PO2
Increase in ventilation rate cause
increase in expiration of CO2
-Decreases arterial PCO2
Increase in ventilation rate & decrease in PO2 causes a conflict BC
In the body’s attempt to obtain O2, blowing off CO2 causes the blood pH to increase becoming alkaline
-This is why the kidney’s excretion of bicarbonate is an important adaptation to high altitudes
A drop in PO2 is sensed only by
Peripheral chemoreceptors
Symptoms of acute mountain sickness
-Fatigue
-Nausea
-Headache
Decrease in barometric pressure @ high altitudes leads to proportional decrease in PO2 & thus smaller O2 gradient across the blood-gas barrier can lead to hypoxemia
Both statements are true
A decrease in arterial PO2 @ high altitudes stimulates peripheral chemoreceptors
True
Review: increase in EPO & RBC production
Days to weeks
Review: increase in production of 2- 3- BPG in RBCs
Days
Review: respiratory alkalosis increases Hb affinity for O2
Immediate
Review: peripheral chemoreceptors respond to drop in PO2
Immediate