Main Body: Sacrum, Pelvis, and Pelvic Viscera
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
pelvic girdle
foundation and base of the LE, consists of 2 hip bones, sacrum, and 3 joints: the pubic symphysis and the SI joints
pelvic girdle sex differences
male: denser and heavier, has a narrower outlet, more circular obturator foramen, narrower pelvic arch, larger acetabulum, more narrow greater sciatic notch (70 degrees compared to 90 degrees in female)
SI joint
joint formed between sacrum and ilium, is reinforced by irregular articular surface that adds to form closure stability, and ligaments which contribute to force closure stability, a synovial planar joint with strong articular capsule
interosseus sacroiliac ligament
blends with posterior SI ligament, large from tuberosities of sacrum to tuberosities of ilium, the primary method of force transfer at SI joint
posterior sacroiliac ligament
blends with interosseus SI ligament and inferiorly with the sacrotuberous ligament
iliolumbar ligament
communication of posterior SI ligament that attaches to the transverse process of L5
anterior SI ligament
thinner, ossifies after 50 yo, on anterior surface of SI joint
sacrotuberous ligament
attaches to the dorsal sacrum, PSIS, and coccyx to the ischial tuberosity, with some fibers of gluteus maximus attaching to it, along with the sacrospinous ligament forms the greater and lesser sciatic foramen, blends with posterior SI ligament
pubic symphysis
articulations inculde the symphyseal surfaces of pubic bones, is fibrocartilagenous, movements including sliding, nutation, counter nutation, some separation and increased movement is held to occur in gestation and participates in childbirth
SIJ movement
some sliding, gliding, rotation, also have nutation and counter nutation, translation and gliding that decreased with age as there is gradual obliteration of the synovial cavity
nutation
nodding of the sacrum- base of the sacrum move anteriorly and the ilium moves posteriorly
counter nutation
posterior rotation of the base of sacrum and the ilium moves anteriorly
pelvic girdle movement
pelvic tilt- see anterior pelvic tilt from force couple of tight hip flexors and tight lumbar extensors, see posterior pelvic tilt from tight hamstrings and gluteus max and rectus abdominis
pregnancy affects on pelvic girdle
see hormonal changes, this relaxes the pelvic joint and ligaments so that there is increased movement, the locking of the SI joint is less restrictive, also causes more movement. post partum may remain loose and more strain from weight bearing falls on the ligaments and can lead to pain
pelvic outlet
lower opening of pelvis, bounded by the sacrum, coccyx, ischial tuberosities, pubic symphysis, and inferiorly by the sacrotuberous ligament, is closed by the pelvic diaphragm
pelvic diaphragm musculature
consists of the levator ani and coccygeus, openings for the urethra, vagina, and rectum to pass through
levator ani
group of muscles making up the pelvic diaphragm including puborectalis, pubococcygeus, and iliococcygeus, is innervated by several nerves including the pudendal nerve, and sacral spinal nerves S4, S5, relaxes to allow for urination and defecation
puborectalis
forms the u-shaped sling that passes posterior to the anorectal junction, bounding the urogenital hiatus
pubococcygeus
wider but thinner intermediate part of levator ani, from the pubis to coccyx
iliococcygeus
part of levator ani (most lateral) forms the fascial opening over obturator internus to coccyx
(ischio) coccygeus
extends from the ischial spine to the coccyx, most posterior portion of the pelvic floor
function of the pelvic floor
supports the abdominal and pelvic viscera through tonic contraction, activity contracted in the valsalva maneuver, maintains fecal and urinal continence (can do KEGELS to strengthen)
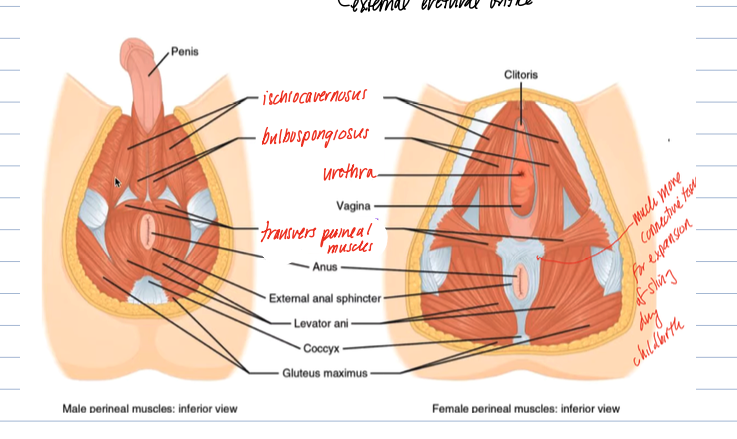
superficial muscles of the pelvic floor
attach to the perineum, include the transverse perineal, ischiocavernosus (, bulbospongiosus
pelvic viscera
organs include the male and female reproductive organs, bladder, pelvic portion of ureters, urethra, rectum, and anus
peritoneum
inner lining covering the pelvic organs, causes the formation of pouches and ligaments- such as the rectovesical pouch (in males, space between bladder and rectum), the rectouterine pouch (in females, space between uterus and bladder), and the vesicouterine pouch (in females, space between bladder and uterus), and the broad ligament
bladder
located behind the pubic symphysis, rests on the pelvic diaphragm in females and on the prostate in males, made up of interlacing smooth muscle called detrusor muscle, has 3 openings: 2 for ureters and 1 for the urethra, of which they form the trigone
internal urethral spincter
is made of smooth muscle, parasympathetic control
external urethral sphincter
made of skeletal muscle, under voluntary control
micturition process
involved the parasympathetic contraction of the detrusor muscles and relaxation of the internal urethral sphincter, as well as voluntary relaxation of the external urethral sphincter
ureters
pass anterior to the bifurcation of the common iliac artery, anterior to the SI joint, and travel to base of bladder, transports urine
male reproductive organs
include the testes, epididymus, ductus deferens, seminal glands, ejaculatory duct, bulbourethral glands, and prostrate
testes/male gonads
the primary reproductive organ, development of spermatozoa occurs here, also production of testosterone, sit inside the scrotum
layers of the scrotum
are continuations of the abdominal layers (as were pulled down with the descent of the testes)
Abdominal to scrotal layers
subcutaneous tissue → subcutaneous tissue and dartos muscle
external oblique muscle and fascia → external spermatic fascia
internal oblique muscle → cremaster muscle
fascia of IO → cremasteric fascia
transversus abdominis → internal spermatic fascia
transversalis fascia → internal spermatic fascia
peritoneum → tunica vaginalis (parietal and visceral)
epididymis
maturation of sperm occurs here, start of the reproductive tract, 23 feet long! has a head, body, tail which turns into the ductus deferensd
ductus deferens
travels from the epididymus to the ejaculatory ducts where it meets with the seminal gland duct, travels through the spermatic cord and the inguinal canal
prostate gland
found between the bladder and the urogenital diaphragm, adds to ejaculate (20% of volume) which is believed to be a chemical activator of sperm, also adds enzymes, contains smooth muscle, and prostatic tissue itself forms the prostatic urethra
seminal glands
lies against the posterior and lateral bladder, secretions add to the ejaculate (alkalytic agent with fructose), its duct joins the ductus deferens to form the ejaculatory duct which empties into the prostatic urethra
bulbourethral gland
responsible for the presemen fluid, which lubricals the urethra and cleans it of urine reside, also increases the pH as semen needs alkalytic environment
3 parts of the urethra
named based on the tissue is travels through: prostatic, membranous, and penile(spongy)
path of the sperm
testes → epididymus → vas deferens → ejaculatory duct → prostatic urethra → membranous urethra → penile urethra → external urethral orifice
spermatic cord
extends between testes and abdominal pelvic cavity, consists of layers of fascia and muscle, encloses the ductus deferens, the pampiniform plexus, blood vessels, nerves and lymphatic vessels, passes through the inguinal canal
dartos muscle
smooth muscle within the dermis, is responsible for the characteristic wrinkling of the skin of scrotum
cremaster muscle
continuation of internal oblique, involved in temperature regulation by contracting and bringing testes up closer to body, deep to dermis
contents of the ejaculate
sperm, seminal fluid, enzymes
penis
consists of the root, the body, and the glans
body of the penis
consists of three cylindrical columns of erectile tissue, 2 of corpus cavernosa, 1 of corpus spongiosum
glans of the penis
expanded distal portion of the penis, most sensitive portion
female reproductive organs
ovaries, uterine tubes, uterus, vagina, external genitalia
ovary
almond shaped, 3 cm long. suspended from the posterior lamina by mesovarium (part of the broad ligament) and attached to the lateral wall by the suspensory ligament of the ovary, medial end is attached to uterus by the ovarian ligament
uterine tube
about 10 cm long, passageway from uterus to ovary, connects the uterine cavity to the peritoneal cavity as well, is draped in mesosalpinx (part of the broad ligament) and consists of 4 parts: intrauterine part, the isthmus, ampulla, infandibulum (has fimbriae)
uterus
pear shaped, 8 cm long and 5 cm wide, sits behind the bladder, in front of the rectum, provides for the embryo and fetus, consists of the fundus (above the uterine tubes), the body, and the cervix and muscular layers consist of the endometrium, myometrium, and epimetrium
external os
the opening in the cervix that leads to the vagina
broad ligament
2 layers of peritoneum that fuse after draping around the uterus, within the broad ligament find the round ligament that attaches the uterus to the lateral wall, the proper ligament of the ovary/ovarian ligament that attaches the ovary to the uterus
vagina
contains fornix- recess around the cervix, and vaginal rugae that allow for distension and make it so elastic, is 7.5-9 cm long
vaginal muscles
bulbospongiosus along either side of the vaginal entrance, vestibular bulbs that is the same embryological orgin as the corpus spongiosum in males
pelvic blood vessel
main supply to the pelvic cavity is the internal iliac artery/internal pudendal artery, the gonadal arteries supply the gonads
gonadal arteries
branch directly from the abdominal aorta beneath the SMA, in males travels through spermatic cord to get to testes
gonadal veins
an example of unpaired venous return- the left gonadal is a branch of the left renal, however the right gonadal is directly from the aorta
internal iliac artery branches of pelvic viscera
in females see the vaginal and uterine artery, also the internal pudendal to the perineum
sacral plexus
L5-S4, S1, S2, S3 are large and sit right on top of piriformis, many branches exit through the greater sciatic foramen to supply the skin of the buttocks, posterior thigh, and the skin and muscles of the leg and foot (except the skin of the medial leg with is saphenous from femoral)
branches of the sacral plexus
nerve to piriformis, quadratus femoris, obturator internus, levator ani, large branches include the tibial nerve, the common fibular nerve, the pudendal nerve, and superior and inferior gluteal nerves