Immunology Chapter 13 - Failures of the Body's Defenses
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
27 Terms
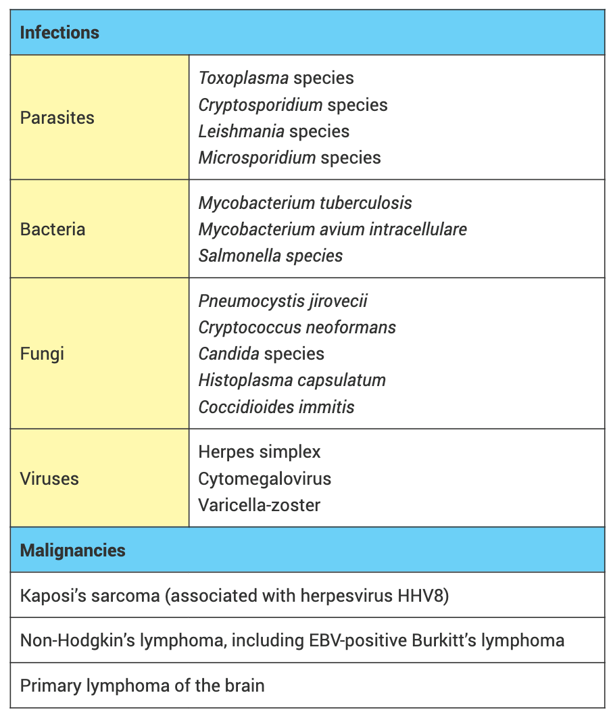
Evolution of new influenza variants by antigenic drift.
During infection with influenza strain V, person P produced antibodies against various epitopes of the viral hemagglutinin. Some antibodies are neutralizing (green); others are not (blue). Later in the flu season, when person P is again exposed to strain V, the neutralizing antibodies prevent cells from being infected (left panel). On infecting person Q, strain V mutates to give strain V*, which differs from V by an amino acid substitution (yellow) in the viral hemagglutinin (center panel). This mutation eliminates the epitope recognized by the neutralizing antibodies elicited by strain V. Consequently, strain V* influenza virus can infect cells of person P without hindrance from the V-specific antibodies (right panel). To clear this second infection, P must make a primary immune response of neutralizing antibodies specific for strain V *. Like the hemagglutinin, influenza neuraminidase (not shown) is also subject to antigenic drift.
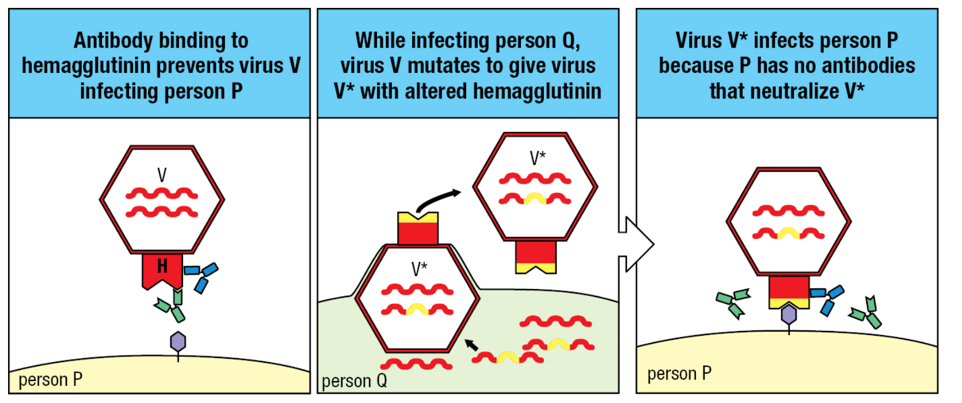
Evolution of new influenza variants by antigenic shift.
Human (red) and avian (blue) influenza viruses can also infect pigs, which serve as secondary hosts. Left panel: in a pig cell infected with human and pig viruses, the RNA genome segments are sorted to produce various recombinant viruses. Center panel: one such recombinant has a hemagglutinin of avian origin. The avian hemagglutinin is antigenically very different from the hemagglutinins of the influenza viruses currently infecting the human population, including the one that infected the pig cell. Right panel: individual humans are highly susceptible to the recombinant virus because they do not have antibodies that bind to the hemagglutinin and prevent the virus from infecting cells. Because the entire human population is vulnerable to the recombinant virus, the latter has the potential to produce a pandemic of influenza.
Outbreak
an occurrence of a particular infectious disease that is limited in extent and duration.
Epidemic
outbreak of infectious disease that affects many individuals within a population.
Pandemic
outbreak of an infectious disease that spreads worldwide. For example, the "Spanish flu" following the First World War, infection with the human immunodeficiency virus (HIV), and the spread in 2020 of COVID-19 caused by the coronavirus SARS-CoV-2.
Endemic
A disease outbreak is endemic when it is consistently present but limited to a particular region. This makes the disease spread and rates predictable. Malaria, for example, is considered ________ in certain countries and regions.
Immune Evasion
a strategy used by pathogenic organisms and tumors to evade a host's immune response to maximize their probability of being transmitted to a fresh host or to continue growing, respectively.
______________ are a group of _______________________ that have coevolved with humans and other host species throughout history. It persists in human hosts by hiding from the immune response. Compared with smallpox, measles, and polio viruses, the effects on humans are subtle. They rarely kill.
Herpesviruses; large double-stranded DNA viruses
Lytic Phase
viral replication and kills the host cell
Latency
virus is in dormant state. Its linear genome becomes circular and acquires nucleosomes and DNA methylation. Does not provoke an immune response nor cause disease.
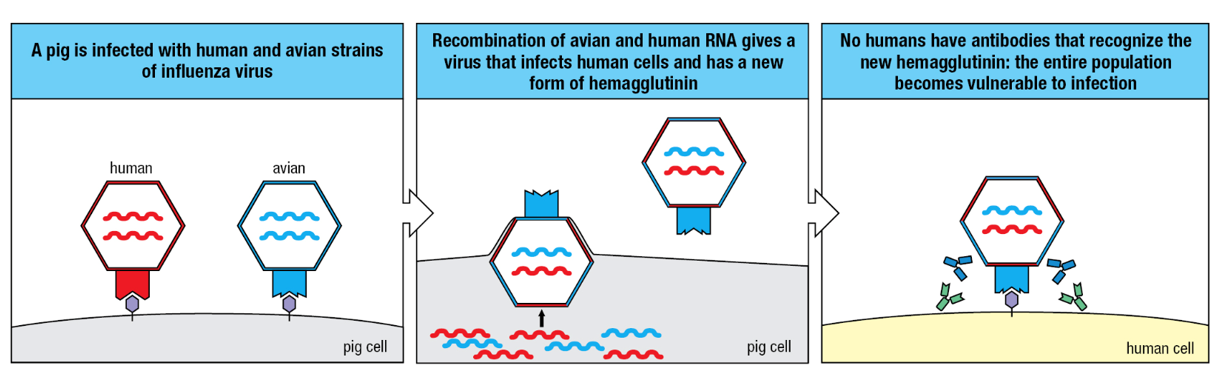
Persistence and reactivation of herpes simplex virus infection.
Initial infection around the lips is cleared by the immune response and while healing is manifested as cold sores (upper panel). Meanwhile, the virus (small red dots) enters sensory neurons, such as the trigeminal ganglion that innervates the lips, where it persists in a latent state (lower panel). At a later time, stress can cause the virus to leave the neurons and reinfect epithelial cells. This reactivates the immune response and causes cold sores. During this active phase, the virus can pass from one person to another.
Some bacteria and parasites subvert the human immune response. When Mycobacterium tuberculosis is __________________, it prevents fusion of the phagosome and the lysosome, thus protecting itself from exposure to the bactericidal contents of the lysosome. By this means, M. tuberculosis ______________ within the vesicular system of the macrophage.
phagocytosed by a macrophage; survives and flourishes
Some species of ________________, notably Staphylococcus aureus and Streptococcus pyogenes, __________________, which at minuscule concentrations induce a violent disruption of an infected _______________. Because these small bacterial protein toxins activate so many different T-cell clones, they are called ___________.
Gram-positive bacteria; secrete potent toxins; person’s immune system; superantigens
The mayhem is caused by the nonspecific activation of _____________________, involving 2–20% of the body’s CD4 T cells, and excessive production of IL-2, IFN-γ, and TNF-α.
numerous CD4 T-cell clones; IL-2, IFN-γ, and TNF-α
Toxic Shock Syndrome Toxin-1
superantigen secreted by Staphylococcus aureus that causes toxic shock, a systemic shock reaction resulting from the overproduction of cytokines by CD4 T cells activated by the superantigen.
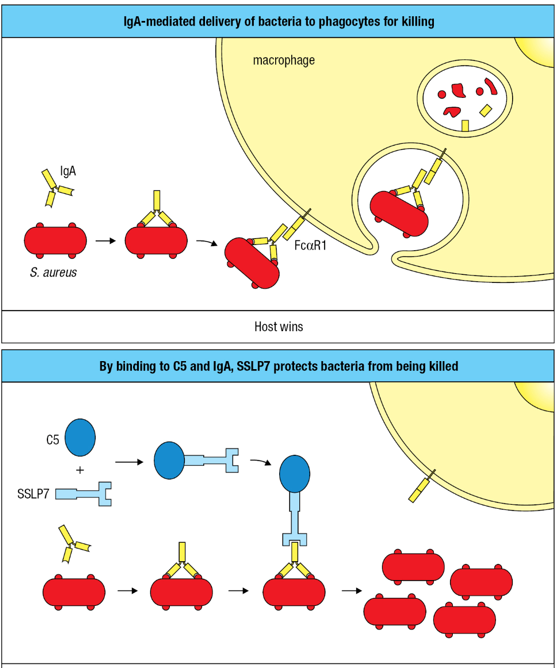
Evasion of IgA-mediated defense by a bacterial superantigen.
Upper panel: the combination of specific IgA and FcaRI on phagocytes causes the elimination of bacteria that cross a mucosal barrier and infect the underlying tissue. Lower panel: this mechanism for disposing of bacteria is thwarted by the staphylococcal superantigen-like protein 7 (SSLP7) of S. aureus. By binding to both C5 and the Fc region of IgA, SSLP7 prevents IgA from binding to FcaRI or activating complement-mediated killing of the bacteria (not shown).
Primary Immunodeficiency Disease
disease in which there is a failure of immunological function as a result of a defect in one or more genes encoding components of the immune system.
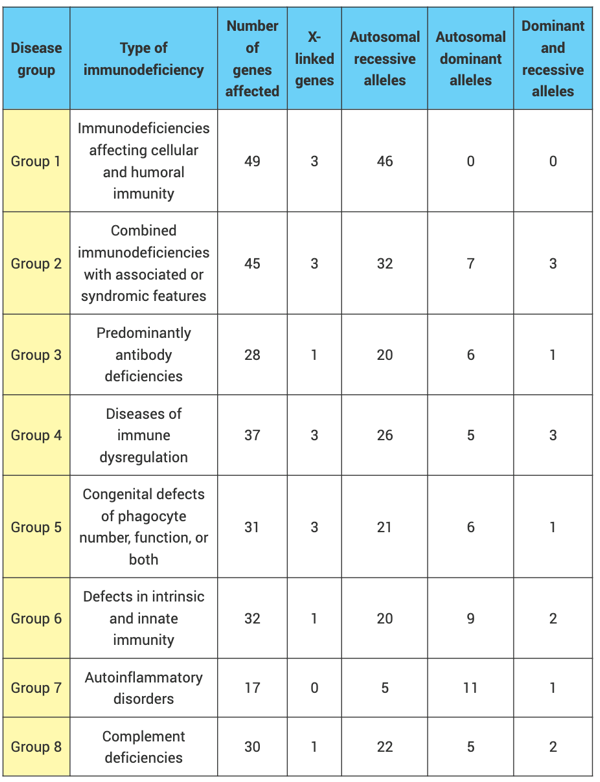
Primary immunodeficiency syndromes comprise ______ functional groups. Most of the human conditions are very rare and are caused by mutant genes. In dissecting the immune system of the laboratory mouse, immunologists routinely _________ a selected gene and examine the immunodeficiency syndrome that this causes.
eight; 'knock out'
C1 Inhibitor
regulatory protein in plasma that inhibits the enzyme activity of activated complement component 1. C1INH deficiency causes the disease hereditary angioedema, in which spontaneous complement activation causes episodes of epiglottal swelling and other symptoms.
Complement Protein
C1, C2, C4
C3
C5 C9
Factor D, properdin (factor P)
Factor I
DAF, CD59
C1INH
Effects of deficiency
Immune-complex disease
Susceptibility to encapsulated bacteria
Susceptibility to Neisseria
Susceptibility to encapsulated bacteria and Neisseria but no immune-complex disease
Similar effects to deficiency of C3
Autoimmune-like conditions including paroxysmal nocturnal hemoglobinuria
Hereditary angioedema (HAE)
Acquired Immune Deficiency Syndrome
disease caused by infection with the human immunodeficiency virus (HIV). It involves a gradual destruction of the CD4 T-cell population and increasing susceptibility to infection.
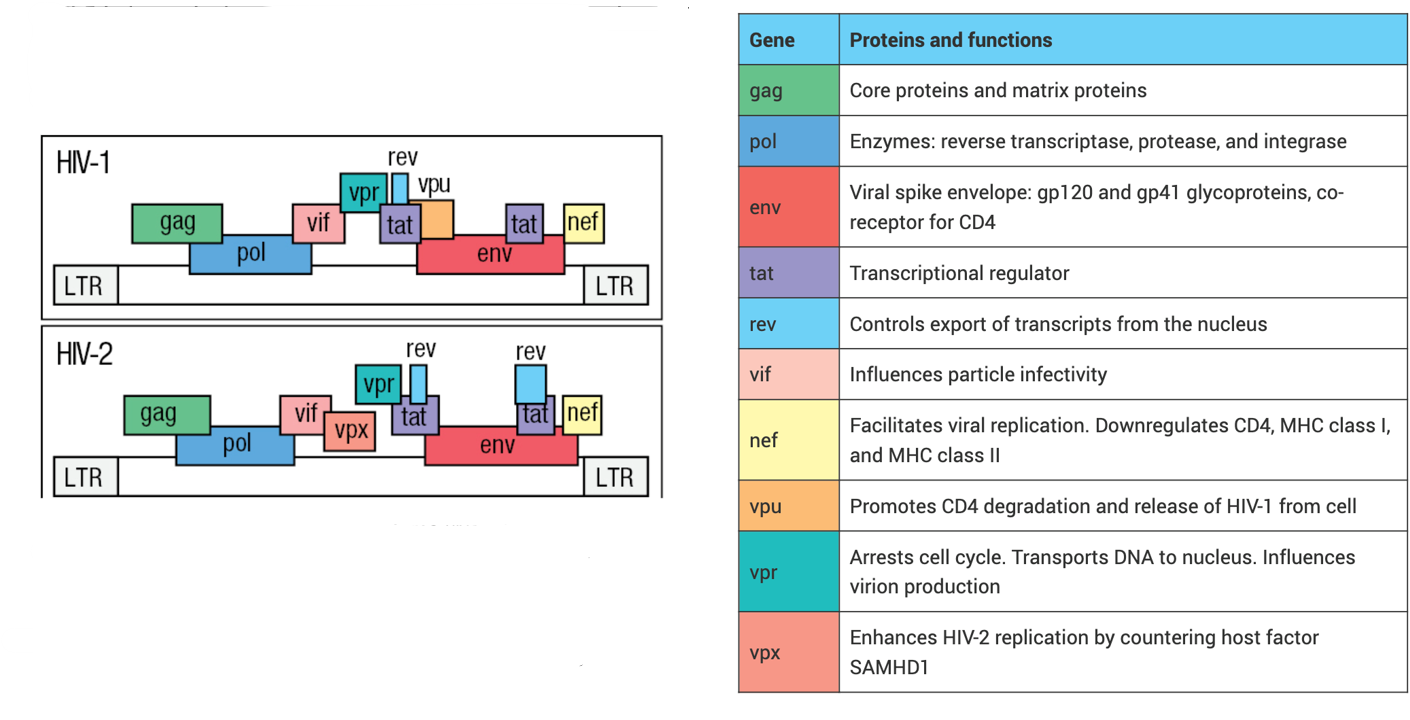
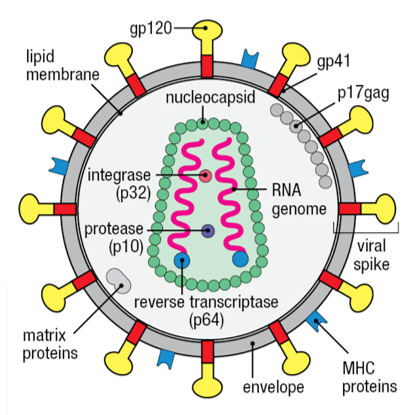
Human Immunodeficiency Virus
causative agent of the acquired immune deficiency syndrome (AIDS). HIV is a retrovirus of the lentivirus family that infects CD4 T cells, leading to their slow depletion, which eventually results in immunodeficiency and death from infection.
HIV-2 is_____________ and causes a slower ____________ to AIDS. HIV-2 is endemic to West Africa and has spread widely through Asia.
less virulent; progression
The natural course of an HIV infection and the immunity it induces.
In the early phase of HIV infection, while the adaptive immune response is being activated, the virus reaches high levels (red line). With production of HIV-specific antibodies (blue lines) and cytotoxic T cells (yellow line), the virus is controlled but is not eliminated. When the destruction of CD4 T cells outstrips their renewal, adaptive immunity declines and levels of virus increase again.
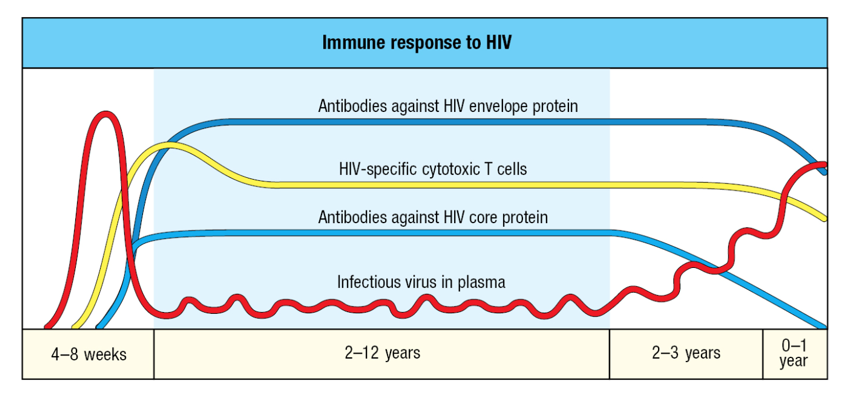
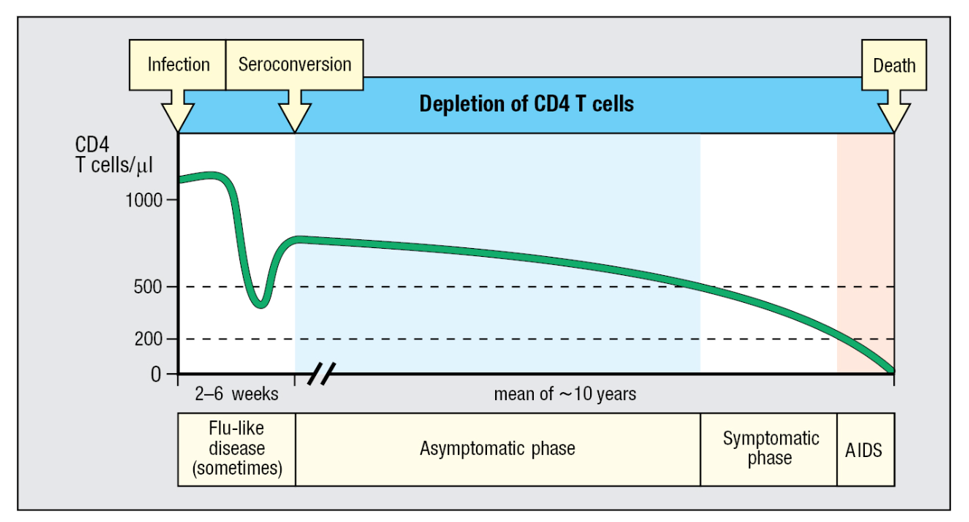
After infection with HIV there is a gradual extinction of CD4 T cells.
The number of CD4 T cells (green line) refers to those present in peripheral blood. Opportunistic infections and other symptoms become more frequent as the CD4 T-cell count falls, starting at around 500 cells/ul. The disease then enters the symptomatic phase. When CD4 T-cell counts fall below 200 cells/ul, the patient is diagnosed as having AIDS.
_________ is an enzyme that retroviruses use to ____________ into the DNA of a host cell, a vital step in the viral replication cycle:
Integrase; insert their DNA
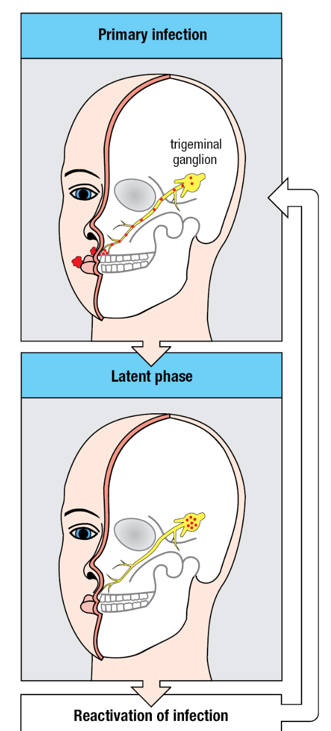
Opportunistic infections that kill AIDS patients.
Listed are the most common opportunistic infections that kill AIDS patients in developed countries. Listed separately are the malignancies, which are the consequence of inadequate immune responses to infectious agents.