8. Cardiovascular 2
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
What are the types of heart valve disorders?
Heart valve disorders include incompetent valves, which fail to close completely, and stenotic valves, which have a narrowed opening that restricts blood flow.
What can be cause of heart valve disorders?
Through developement or bacterial infections
What is mitral valve (bicuspid valve or left atrioventricular valve) prolapse, and how common is it?
Mitral valve prolapse is a condition where the mitral valve fails to close properly, affecting about 10% of the population between 14 and 30 years of age.
What is coronary artery disease (CAD), and what are its potential complications?
Coronary artery disease (CAD) occurs when the coronary arteries become blocked, reducing blood flow to the heart. It can lead to complications such as angina pectoris (chest pain) and myocardial infarction (heart attack).
What is heart failure, and what causes it?
Heart failure is the weakening of the heart muscle, which prevents it from pumping blood effectively. Causes include coronary artery disease, heart valve issues, and chronic hypertension.
What are fibrillations, and why are they dangerous?
Fibrillations are rapid, uncoordinated contractions of the heart muscles, which prevent effective blood pumping. They can lead to severe complications, including cardiac arrest if untreated.
What are some common developmental heart defects?
Common developmental heart defects include transposition of the great vessels (where major arteries are incorrectly positioned), septal defects (holes in the heart's septum), and myocarditis (inflammation of the heart muscle).
What is myocarditis, and what can cause it?
Myocarditis is inflammation of the heart muscle, which can be caused by infections, chemicals, or medications. Over time, it can lead to an accelerated heart rate and weakened heart function.
What is endocarditis, and which structures are typically affected?
Endocarditis is inflammation usually involving the heart valves and/or chordae tendinae. Bacterial endocarditis is a common form that can lead to serious damage if untreated.
What is pericarditis, and what symptoms might it cause?
Pericarditis is inflammation of the pericardium (the outer layer surrounding the heart). Symptoms may include sharp chest pain and discomfort that worsens with breathing.
What is the primary function of the vasculature system in the body?
The vasculature is a closed system responsible for carrying blood from the heart to various tissues in the body and back again.
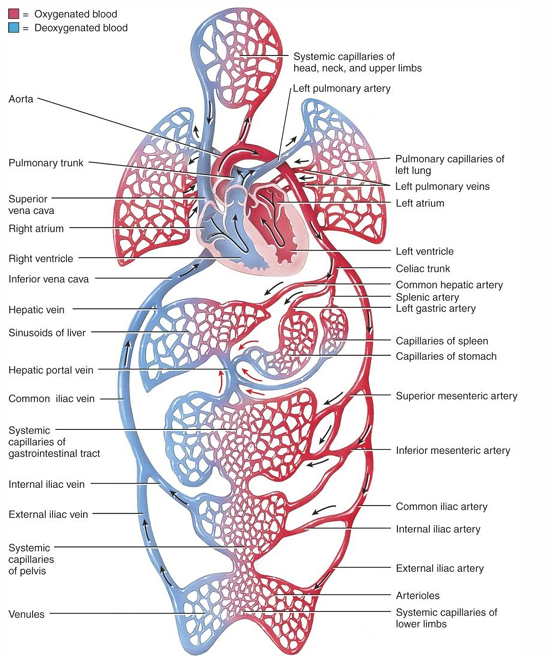
What are the three main types of blood vessels in the vasculature system?
The three main types of blood vessels in the vasculature are arteries, capillaries, and veins.
What are the three layers of an artery, and what is the primary function of each?
Tunica interna (intima): Made of flat endothelial cells to minimize blood friction and a basement membrane to anchor the endothelium.
Tunica media: Contains rings of smooth muscle, elastic, and collagen fibers, providing strength, elasticity, and the ability for vasoconstriction/vasodilation.
Tunica externa (adventitia): Elastic and collagen fibers protect, strengthen, and anchor the artery to surrounding structures.
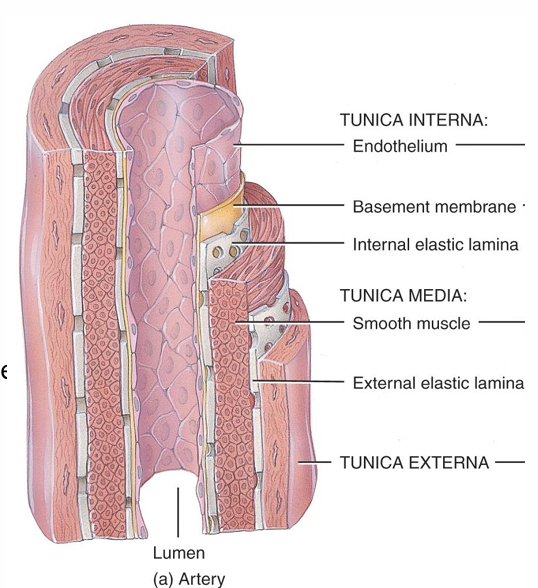
How does the tunica media differ between arteries and veins?
The tunica media is thicker in arteries to withstand higher blood pressure, whereas it is thinner in veins.
What is the internal elastic lamina and what is the primary function of the internal elastic lamina?
The internal elastic lamina is a layer within the tunica interna (intima) of an artery. The internal elastic lamina serves as a restrictive barrier, limiting the movement of large molecules (macromolecules) across the artery wall.
What are the main types of arteries?
The three main types are elastic, musclar arteries and arterioles
Where are elastic arteries located in the body, and what is their structural composition?
Includes arteries close to the heart, such as the aorta and pulmonary arteries.
Tunica Media: Rich in elastic fibers, allowing significant stretching and recoiling.
Large Lumen: Diameter typically between 1-2.5 cm.
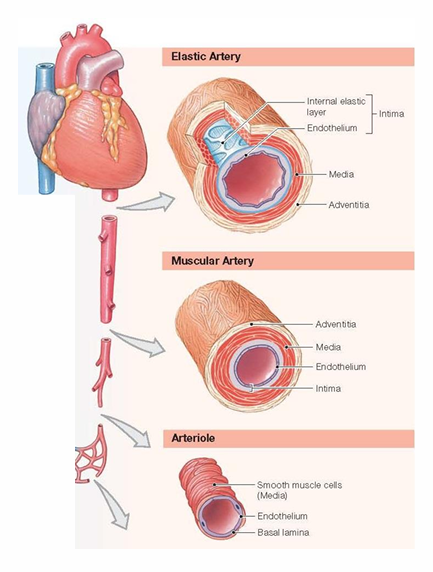
What is the function of elastic arteries?
Absorb and dampen blood pressure surges that occur with each heartbeat.
Stretch and recoil with each heartbeat, which helps propel blood forward even when the heart is in a relaxed state. They stretch when filling with blood and recoil helps propulsion of blood
What is muscular arteries’ structural composition?
Tunica Media: High concentration of smooth muscle cells relative to their lumen, enabling control of vessel diameter.
Medium-sized Lumen: Diameter ranges from approximately 0.3 mm to 1 cm.
What is the function of muscular arteries?
Distribute blood to specific organs throughout the body.
Actively control blood flow by changing their diameter (vasoconstriction and vasodilation) in response to the body’s needs, such as during exercise or rest.
What is arterioles’ structural composition?
Smallest Arteries: Diameter typically between 10 μm and 0.3 mm.
Tunica Media: Consists of 1-2 layers of smooth muscle cells. Larger arterioles have all three arterial layers (intima, media, and externa), while smaller ones may have only a single smooth muscle layer around the endothelium.
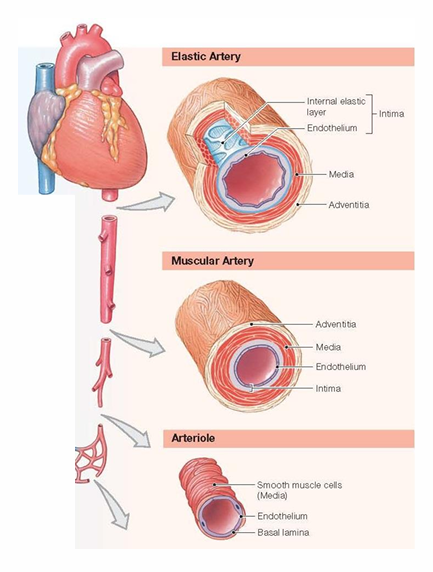
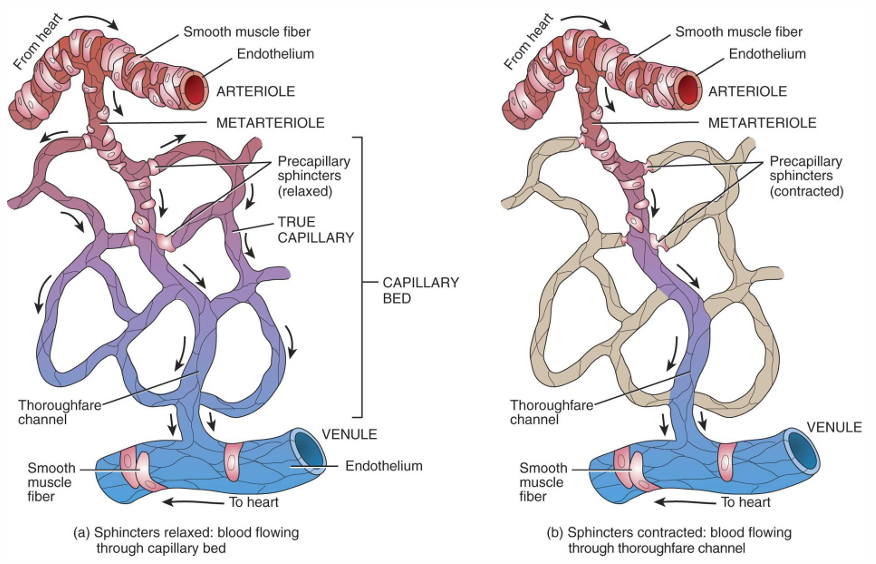
What is the function of arterioles?
Control blood flow into capillary beds through contraction and relaxation of smooth muscle in their walls.
Regulate systemic blood pressure by altering their diameter, as they provide significant resistance to blood flow.
What are capillaries, and why are they considered the smallest blood vessels in the body?
Capillaries are the smallest blood vessels in the body, typically ranging from 5-10 µm in diameter, and they facilitate the exchange of gases, nutrients, and waste products between the blood and surrounding tissues.
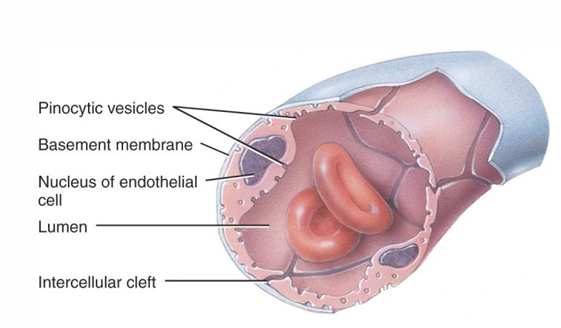
What makes capillaries permeable to fluids and solutes?
Capillaries are permeable due to their structure, consisting of a single layer of endothelial cells and a basement membrane, which allows for the passage of fluids and solutes.
What is the structure of continuous capillaries?
Continuous capillaries have endothelial cells tightly linked together with intercellular clefts, and a continuous basement membrane, allowing for the passage of fluids and solutes.
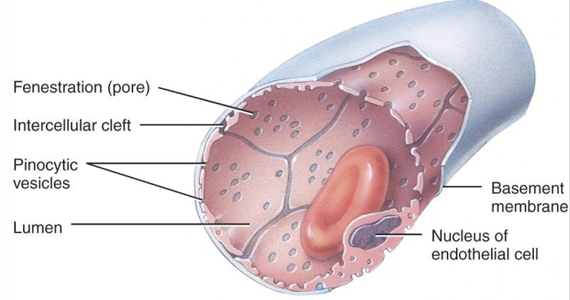
What is the structure of fenestrated capillaries?
Fenestrated capillaries have pores (fenestrations) in the endothelial cells, with a continuous basement membrane, making them more permeable than continuous capillaries, especially for larger molecules like peptides and proteins.
Where in the body are continuous capillaries typically found?
Continuous capillaries are typically found in the skin, muscles, central nervous system, and lungs, where they allow for the exchange of nutrients and waste without permitting large molecules to pass.
What is the function of fenestrated capillaries, and where are they located in the body?
Fenestrated capillaries have greater permeability than continuous capillaries due to their fenestrations (pores) in the endothelial cells. They are found in areas where rapid exchange of larger molecules occurs, such as the kidneys, intestines, and endocrine glands.
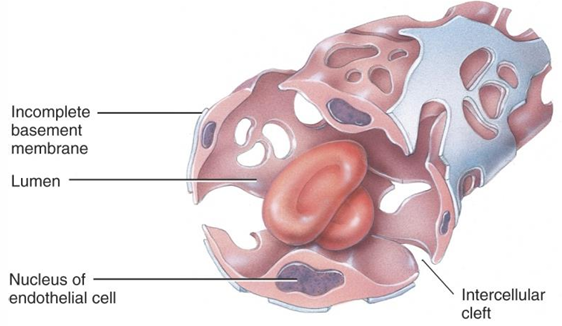
How do sinusoids differ from continuous and fenestrated capillaries?
Sinusoids have a wider lumen and more winding vessels, with large fenestrations and either an incomplete or absent basement membrane. This structure allows for the passage of large molecules and cells, facilitating slow blood flow and modifications in organs like the liver, bone marrow, spleen, and lymphoid tissue.
What is microcirculation, and which blood vessels are involved?
Microcirculation refers to the flow of blood through the smallest blood vessels in the circulatory system. It involves arterioles, capillaries, and venules.
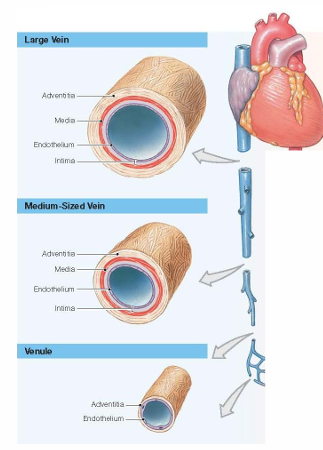
What are the main structural components of veins?
Veins consist of three main layers:
Tunica interna (intima): Endothelial cells lining the inner surface of the vein. Basement membrane underneath the endothelial cells.
Tunica media: A thin layer of smooth muscle cells and elastic fibers.
Tunica externa (adventitia): Composed of elastic and collagen fibers.
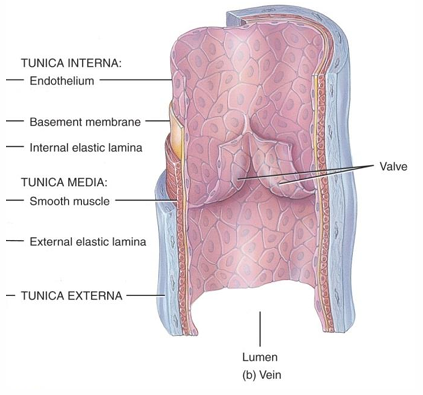
Why do veins not have an internal elastic lamina like arteries?
Veins do not have an internal elastic lamina because they do not require the same structural strength as arteries to withstand high-pressure blood flow. The absence of this layer reflects the lower pressure environment in veins.
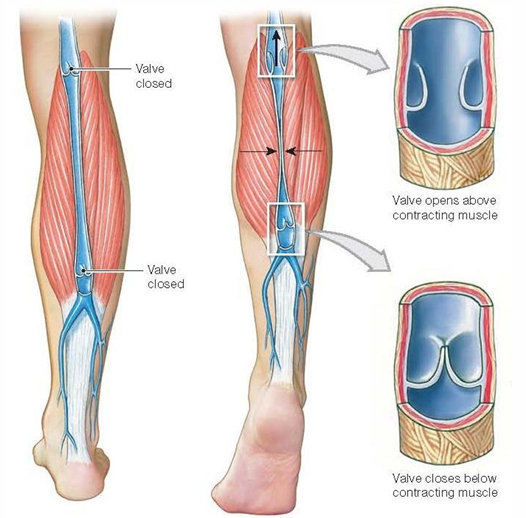
What role do valves play in the veins, and where are they found?
Valves in veins, formed by cusps of endothelial cells, help prevent backflow of blood as it is returned to the heart, particularly in the lower limbs. These valves ensure that blood flows in one direction, against gravity.
What is the main difference between venules and larger veins in terms of structure?
The walls of venules only consist of a layer of endothelial cells and tunica externa (adventitia)
Why is blood pressure in venules and medium-sized veins not sufficient to overcome gravity?
The blood pressure in venules and medium-sized veins is low, which is not enough to oppose gravity and prevent blood from flowing backward, especially in the extremities.
What role do valves play in venous circulation?
Valves in the veins prevent the backflow of blood and help prevent pooling in the extremities, ensuring that blood flows in one direction toward the heart.
How does muscle contraction assist in blood flow through veins?
Muscle contraction helps blood progression by compressing the veins and pushing blood toward the heart. Shifting body position can help with the progression of blood through veins by facilitating muscle contractions and assisting the movement of blood toward the heart.
What role does breathing play in venous circulation?
Breathing helps blood progression through veins by creating pressure changes in the thoracic cavity. These pressure changes facilitate the movement of blood toward the heart, particularly during inhalation.
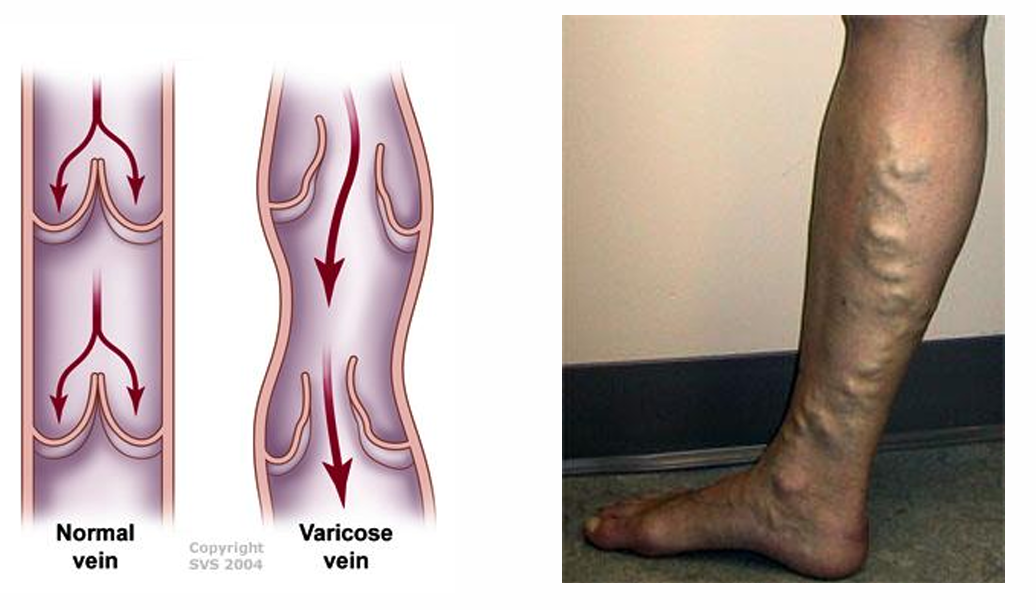
What causes varicose veins?
Varicose veins are caused by malfunctioning valves in the veins, which allow blood to flow backward and pool in the lower extremities. This leads to increased pressure in the veins, causing them to become enlarged and twisted. This condition is a form of venous insufficiency, where the veins are unable to efficiently return blood to the heart due to weakened or damaged valves.
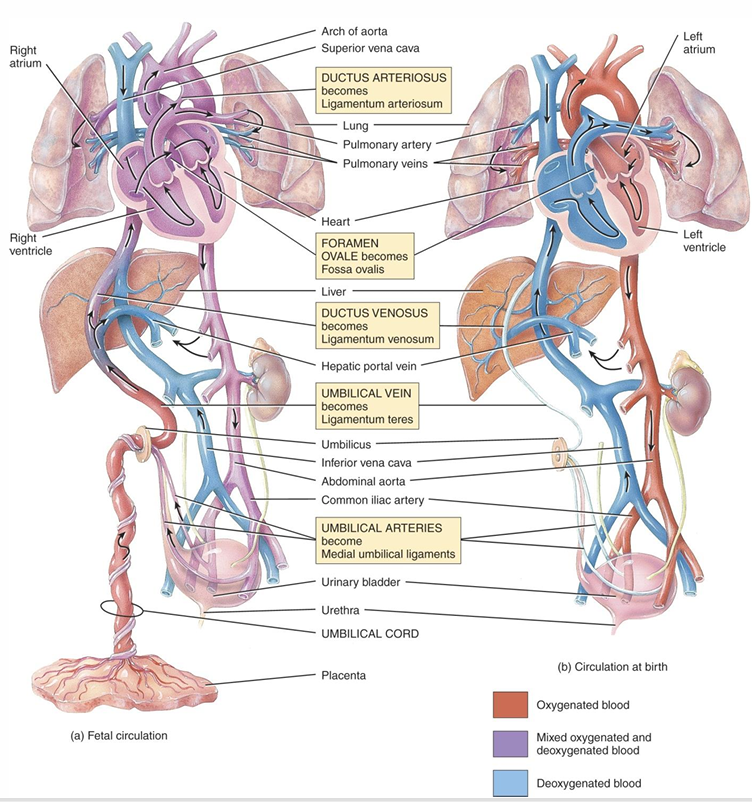
What is the difference between pulmonary, systemic and fetal circulation?
Pulmonary circulation moves blood between the heart and lungs for oxygenation.
Systemic circulation carries oxygenated blood from the heart to the body and returns deoxygenated blood back.
Fetal circulation involves blood flow between the fetus and placenta, bypassing the lungs with structures like the ductus arteriosus and foramen ovale.*
What are three subcatagories of systemic circulation?
Cerebral circulation: Supplies blood to the brain, providing it with oxygen and nutrients.
Coronary circulation: Delivers oxygen-rich blood to the heart muscle itself.
Hepatic portal circulation: Carries blood from the digestive organs and spleen to the liver for processing nutrients and detoxifying substances.
What is the main function of the hepatic portal circulation?
The main function of the hepatic portal circulation is to direct blood from the digestive organs to the liver, preventing unrefined nutrients from being immediately distributed to the rest of the body.
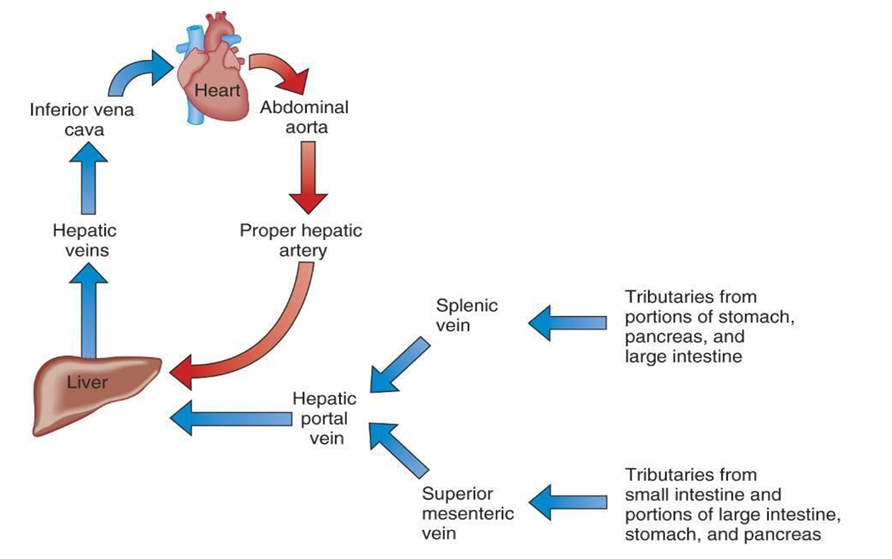
What type of blood does the hepatic portal circulation carry, and why is it significant?
The hepatic portal circulation carries oxygen-poor but nutrient-rich blood from the digestive system. This blood is significant because it allows the liver to regulate and process nutrients and detoxify harmful substances before they enter the general circulation.

What is the function of the ductus arteriosus in fetal circulation?
The ductus arteriosus diverts most of the blood leaving the right ventricle into the aorta, bypassing the lungs (pulmonary circulation bypass).
Right ventricle → Pulmonary artery → Ductus arteriosus → Aorta
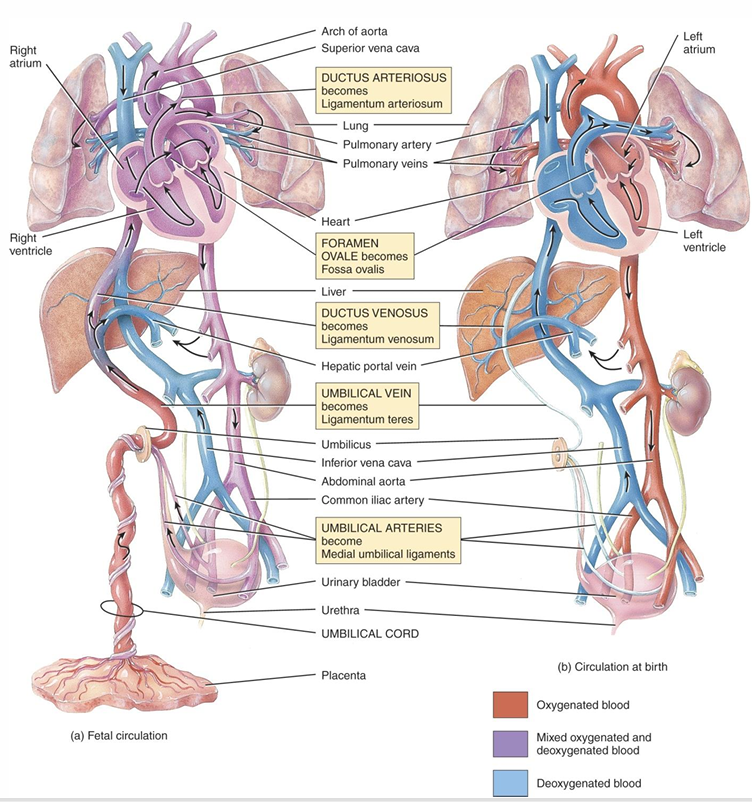
How does the foramen ovale contribute to fetal circulation?
The foramen ovale allows oxygenated blood from the right atrium to pass directly into the left atrium, bypassing the lungs and ensuring that oxygen-rich blood is directed to the body (pulmonary circulation bypass)
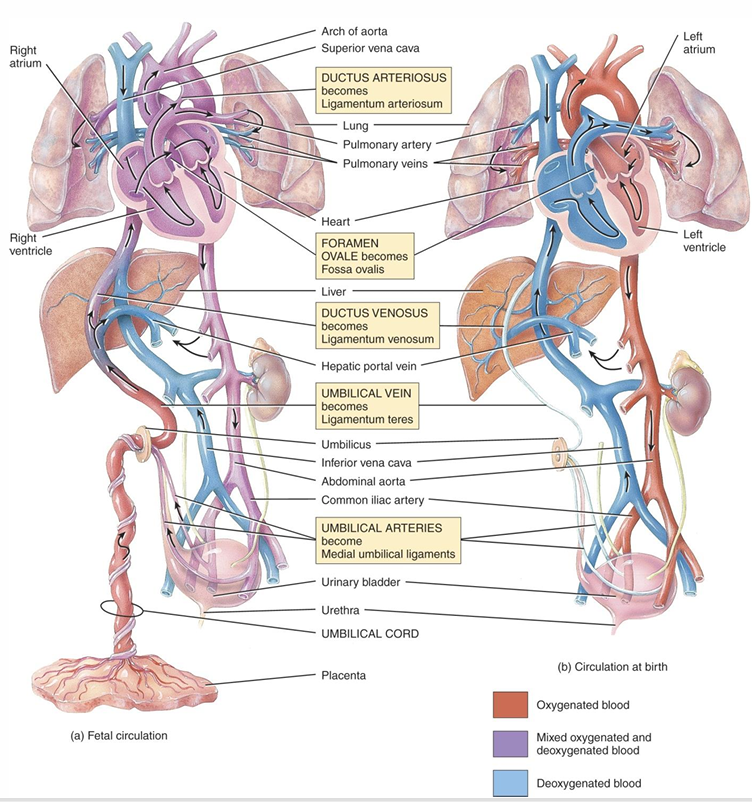
What role does the ductus venosus play in fetal circulation?
The ductus venosus allows oxygenated blood from the placenta to bypass the liver and flow directly into the inferior vena cava, delivering oxygen to the heart and body more efficiently (liver bypass)
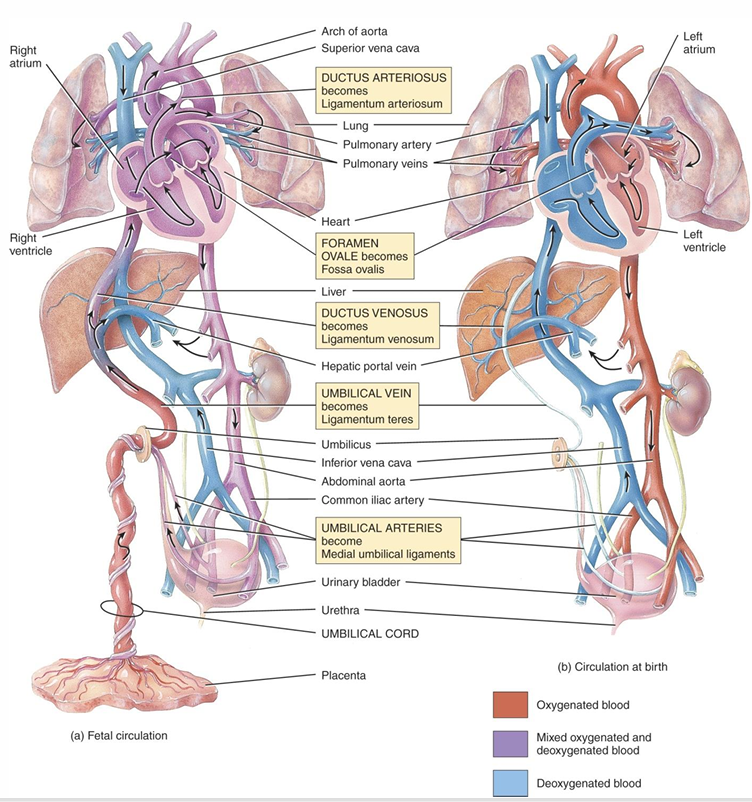
What is the function of the umbilical vein in fetal circulation?
The umbilical vein carries oxygenated blood from the placenta to the fetus, providing the fetus with the necessary oxygen and nutrients.
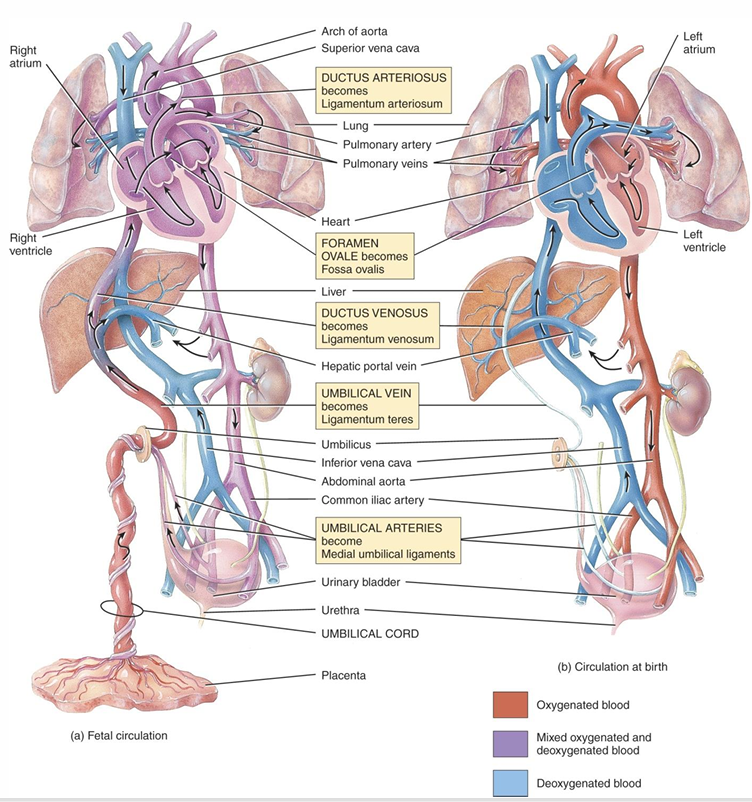
What do the umbilical arteries do in fetal circulation?
The umbilical arteries carry deoxygenated blood from the fetus to the placenta, where it can be re-oxygenated and replenished with nutrients.
What is arteriosclerosis and what causes it?
Arteriosclerosis is the hardening of the arteries due to focal calcification, loss of smooth muscle, and calcium deposition, leading to reduced elasticity and blood flow.
How does atherosclerosis differ from arteriosclerosis?
Atherosclerosis involves damage to the endothelial lining of arteries, leading to lipid deposition that causes obstruction, whereas arteriosclerosis refers to the thickening and hardening of the artery walls due to calcium buildup.
What is an aneurysm and how does it occur?
An aneurysm is a bulging or weakening of an artery wall, often due to the loss of elasticity in aging vessels. A sudden surge in blood pressure can cause the weakened area to rupture, which can cause stroke and infarction
What is a thrombus and how does it form?
A thrombus is a blood clot that forms due to changes in blood composition, often associated with atherosclerotic plaques, which can obstruct blood flow and lead to conditions like stroke or infarction.