MRAD 2218 – Module 1 (Introduction to Pathology)
1/87
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
Pathology
The study of disease processes and their effects on the body.
Etiology
The cause or origin of a disease or pathological condition.
Sign
Objective evidence of disease that can be seen or measured by a clinician (e.g., joint effusion).
Symptom
Subjective sensation reported by the patient (e.g., sharp pain).
Congenital / Hereditary Disorder
Pathology present at birth caused by genetic or environmental factors.
Inflammatory Disorder
Disease resulting from the body’s nonspecific response to injury or infection.
Degenerative Disorder
Progressive deterioration of tissue or organ function, often age-related.
Metabolic Disorder
Disease produced by abnormal physical or chemical processes in the body (e.g., osteoporosis).
Traumatic Disorder
Pathology produced by mechanical, thermal, or radiation injury to the body.
Neoplastic Disorder
Condition involving new, abnormal tissue growth (tumor formation).
Abrasion
Superficial wound caused by friction that scrapes away epidermal cells.
Laceration
Tear in tissue producing jagged wound edges.
Incision
Clean, straight-edged cut produced by a sharp instrument.
Contusion (Bruise)
Soft-tissue injury with vessel rupture and interstitial bleeding but no skin break.
Penetration (Puncture)
Narrow, deep wound created when an object pierces tissues, leaving a small surface opening.
Fracture
Break or crack in a bone.
Regeneration (First-Intention Healing)
Replacement of damaged tissue with identical cells, restoring normal function.
Fibrous Connective Tissue Repair (Second-Intention Healing)
Gap filled with collagen scar; function only partially restored.
Extent of Injury
Severity of tissue damage; greatest negative effect on healing speed and quality.
Ischemia
Reduced blood supply to tissue, hindering healing and risking necrosis.
Immobilization
Stabilizing an injured part to prevent disruption of the healing process.
Dislocation
Complete loss of articular contact between bones forming a joint.
Subluxation
Partial dislocation with widened joint space but maintained partial contact.
Alignment (Angulation)
Direction the distal fracture fragment deviates from its normal axis.
Apposition
Degree of contact between fracture fragments: good, partial, or distraction.
Hematoma
Stage 1: there is a rupture of the periosteum and endosteum, causing bleeding into the marrow and soft tissue. There is also soft tissue swelling around the injury site.
Inflammatory Process
Stage 2: granulation phase, 48 hours post injury, where fibroblasts and capillaries clear hematoma and begin repair.
Callus Formation
Stage 3: periosteal repair by formation of bony (callus) collar develops 5-10 days post-fracture.
Consolidation
Stage 4: primary callus remodeled into mature bone by osteoblasts roughly 4 weeks after injury.
Remodeling
Stage 5: final stage (8-12 weeks) where bone and periosteum return close to normal structure.
Compartment Syndrome
Dangerous rise in pressure within closed fascial space causing vascular compression and possible necrosis.
(Gas) Gangrene
Results in the loss of blood supply due to an infection process that is rapidly spreading, potentially fatal infection of tissue by Clostridium bacteria causing tissue death (1-3 days post injury/surgery)
Fat Embolism
Fat droplets from marrow enter bloodstream, lodging in lungs; manifests 24–72 h after major fracture (especially femur).
Thromboembolism (Deep Vein Thrombosis)
Blood clot formed during prolonged immobility that may travel to lungs and cause pulmonary embolism.
Osteomyelitis
Bone infection—commonly caused by Staphylococcus aureus—leading to pain and bone destruction, typically presenting in open fractures and surgical patients. Occurs within 1 month of trauma/surgery.

Hardware Failure
Breakage, bending, loosening, or migration of fixation devices, destabilizing fracture.
Complex Regional Pain Syndrome (CRPS)
Disproportionate, chronic pain with autonomic changes and possible osteopenia (decrease in bone mass) after trauma. Usually, within 30 days of injury, the patient complains of burning, stabbing, searing pain which is constant and worsening and there is decreased range of motion (ROM). Can result in osteoporosis if chronic.

Post-Traumatic Osteolysis
Bone breaks down at trauma site, often linked to inflammatory response to hardware debris.

Refracture
New break through a previously healing fracture site due to stress, disease, or non-compliance.
Synostosis
Abnormal bony fusion between adjacent bones following trauma.
Delayed Union
Fracture healing slower than normal despite evidence of progress.
Osteonecrosis (Avascular Necrosis)
Bone death from interrupted blood supply; common in femoral head, humeral head, scaphoid, talus.

Degenerative Joint Disease (Post-Traumatic Arthritis)
Premature cartilage wear after intra-articular fracture leading to osteoarthritis changes.

Non-Union
Permanent failure of fracture healing; smooth, atrophic fragment ends with sealed medullary canals.

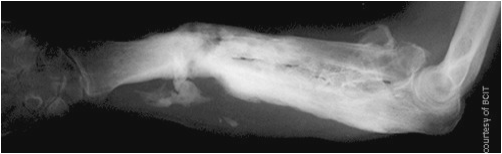
Mal-Union
Healed fracture with deformity or angulation causing functional impairment.
Reduction
Realignment of fracture fragments to restore normal anatomy; may be manual, mechanical, or closed.
Fixation
Use of devices to hold bone fragments, preventing displacement during healing.
External Fixation
Pins through skin connected to an outside frame to stabilize severe or open fractures.
Internal Fixation
Surgical placement of hardware (plates, screws, rods) inside body to maintain alignment.

Reconstruction Plate
Notched, bendable plate with oval holes designed for curved surfaces like mandible or acetabulum.
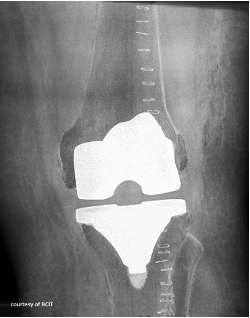
Joint Replacement
Surgical substitution of damaged joint surfaces with prosthetic components to relieve pain and restore function.
Bisphosphonate
Drug class that inhibits bone resorption; used in osteoporosis treatment.

Osteoporosis
Metabolic disease with low bone mass and structural deterioration, predisposing to fractures.
Stress View (Radiography)
Imaging projection taken while applying force to a joint to evaluate stability.
Computed Tomography (CT)
Cross-sectional imaging modality useful for complex fractures and 3-D reconstructions.
Magnetic Resonance Imaging (MRI)
Imaging technique with high soft-tissue contrast; detects sprains, occult and hairline fractures.
Nuclear Medicine Bone Scan
Functional imaging using radiotracers to reveal areas of increased metabolism such as stress fractures or infection.
Fibrous connective tissue repair: stage 1
A small cut involves the epidermis and dermis, affecting underlying connective tissue.
Fibrous connective tissue repair: stage 2
Exudate fills the wound gap; capillaries and fibroblasts begin to appear.
Fibrous connective tissue repair: stage 3
The epidermis regenerates, and the wound gap fills with granulation tissue.
Fibrous connective tissue repair: stage 4
The epidermis returns to normal, and fibroblasts produce collagen to form a permanent scar.

K-wires
These are stainless steel pins which are used to align small fracture fragments.
Immediate Complications
Arterial injuries, Compartment syndrome, Gas gangrene, Fat embolism, Thromboembolism.
Intermediate Complications
Osteomyelitis, Hardware Failure, Complex Regional Pain Syndrome, Post Traumatic Osteolysis, Refracture, Synostosis, Delayed Union, Infection.
Delayed Complications
Osteonecrosis, Degenerative joint disease, Osteoporosis, Non-union, Mal-union.
Thromboembolism
DVT is a blood clot which can impede blood flow. The inactivity imposed by the lengthy immoblization and bed rest required post injury or surgery can cause blood clots to frow. Pulmonary embolism may occur and cause death.
Arterial Injuries
Life-threatening complications where displaced bone fragments impede arterial flow, a major concern in trauma. Blood loss severity depends on fracture location and number, with pelvic fractures causing the most significant loss. Examples include compression of femoral vessels (from avulsed lesser trochanter) or damage to the popliteal artery (from dislocated knee).
Manual reduction (manipulation)
Various maneuvers are used to manually apply traction to reposition the fragments so that they are realigned.
Mechanical reduction
Sometimes gravity with or without weights is used to reduce a fracture or dislocation. For example, in the case of an arm fracture, the patient is made to lie prone with the injured arm hanging down over the edge of the bed. Gravity helps to pull the bone down so that there is good apposition of the fragments.
Closed joint reduction
a fracture is reduced or manipulated externally with the skin still intact.

Plates
Often used on long bones to hold both ends of the fracture together. They are attached to the bone with screws.
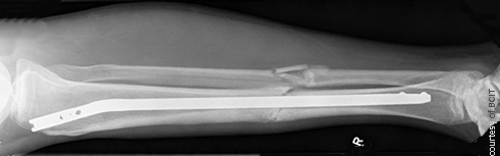
IM nails (intermedullary)
Used for fractures of weight-bearing long bones. They are stainless steel or titanium rods which are inserted into the medulla of the bone. They are usually locked at either or both ends of the rod. To lock the nail, a bolt is threaded through the bone to it to hold it in place and prevent it from twisting within the bone. Fractures treated with them tend to heal faster and the patient is able to weight-bear sooner.
Age
Younger individuals tend to have increased cell regeneration, increased metabolism and increased circulation in comparison to an older individual.
Nutrition
Vitamin C promotes the healing process. Diabetes, alcoholism and corticosteroid abuse will adversely affect the healing process.
Blood Supply
Increased ischemia will reduce the likelihood of healing.
Drainage
Normal drainage from an affected area results in decreased pus, decreased swelling and an increased rate of healing.
Immobilization
Wound edges are allowed to heal and close when the affected part is immobilized.