NURS 209: TOPIC 8 - BREAST & LYMPHATICS
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
139 Terms
Have you experienced any breast pain, lumps, or nipple discharge?
Yes/No; describe location, duration, and characteristics if yes.
Have you noticed any changes in the appearance of your breasts?
Yes/No; specify changes such as size, shape, or skin texture.
Have you had any rash, swelling, or trauma to your breasts?
Yes/No; describe details if yes.
Do you have a history of breast disease?
Yes/No; specify type and date of diagnosis.
Have you had any breast surgeries or radiation treatments?
Yes/No; provide type, date, and reason.
Are you currently taking any medications that affect your breast health?
Yes/No; list medications.
Do you perform regular breast self-examinations, and when was your last mammogram?
Yes/No for self-exam; provide date of last mammogram.
Is there a family history of breast disease, including cancer?
Yes/No; specify family member and condition.
Have you experienced any tenderness, lumps, or swelling of lymph nodes in your axilla?
Yes/No; describe location, duration, and severity.
Have you had any rash in your axilla?
Yes/No; describe appearance, location, and duration.
What is asked in the patient-centered care assessment regarding breast health?
Ask about self-breast exam (BSE) practices and provide teaching to review the basics of examination.
What guidelines should be reviewed for breast cancer screening based on age and patient history?
Review recommendations from the American Cancer Society.
At what ages can screening mammography begin according to the American Cancer Society?
Can begin at ages 40 to 44.
How often should women aged 45 to 54 receive mammography screenings?
Annually.
How often should women over age 55 receive mammography screenings?
Biennially, or they may continue annual screenings.
Until what age should breast cancer screenings continue?
Until age 74.
What is the recommended position for a woman during a breast assessment?
Woman should be sitting up facing the examiner.
What is an alternative draping method during breast inspection?
Use a short gown, open at the back, and lift it up to the woman’s shoulders during inspection.
How should a woman’s breast be covered during palpation when she is supine?
Cover one breast with the gown while examining the other.
Why is it important to use a sensitive approach during breast examination?
Many women are embarrassed to have their breasts examined; a sensitive but matter-of-fact approach helps make them comfortable.
What should the examiner be prepared to do after the breast examination?
Teach the woman breast self-examination (BSE).
What is the first step in breast examination?
Inspection, using the patient to guide you, with a sensitive but matter-of-fact approach.
What should you note about the general appearance of the breasts?
Symmetry of size and shape; slight asymmetry is common.
Is it normal for one breast to be slightly larger than the other?
Yes, often the left breast is slightly larger than the right; sudden increase in size is abnormal.
When is asymmetry considered abnormal?
Grossly different size or shape, or sudden increase in size.
What should the skin of the breast look like?
Smooth and even in color, no edema, fine blue vascular network may be visible; pale linear striae (stretch marks) may follow pregnancy or obesity.
What is normal vascularity of the breast skin?
Diffuse, not prominent, symmetrical in both breasts.
What may unilateral or localized vascular prominence indicate?
Could indicate venous engorgement feeding a tumor or cancer.
What should you do if the patient points to a lump or problem area? (2)
Use it to guide inspection and maintain a sensitive, matter-of-fact approach.
What are abnormal skin changes to look for when inspecting the breasts?
Rough, thickened skin
What abnormal findings indicate edema or inflammation of the breasts? (4)
Swelling, redness, warmth, tenderness
What types of rashes might be abnormal on breast inspection?
Any unusual rash, particularly localized or persistent rashes
What does the presence of unilateral dilated veins on the breast suggest?
Possible obstruction of venous drainage or underlying tumor
What are dimpling or retractions of the breast skin, and why are they significant?
Skin pulling inward, often due to underlying mass or malignancy
What is peau d’orange, and what does it indicate? (2)
Skin looks like orange peel, often due to edema from lymphatic obstruction, possibly indicating breast cancer
What maneuvers are used for retraction screening? (4)
Raise arms overhead, push into hips, lean forward, arms at side.
What should you look for during retraction screening? (5)
Changes in appearance, especially retractions, dimpling, fixation of the breast, or uneven nipple line.
What should you observe when inspecting the lymphatic drainage areas of the breasts?
Observe the axillary and supraclavicular regions; note any bulging, discoloration, or edema.
How should the nipples appear in terms of symmetry?
They should be symmetric on the same plane on both breasts.
What is the normal position of nipples?
They usually protrude, although some may be flat or inverted.
Is nipple inversion always abnormal?
No, normal nipple inversion may be unilateral or bilateral and usually can be pulled out.
What abnormalities should be noted when inspecting the nipples? (4)
Note any dry scaling, fissure or ulceration, and bleeding or other discharge.
What is a supernumerary nipple?
A supernumerary nipple is a normal congenital variation.
How should the areola appear? (4)
It should be round or oval, with Montgomery glands, smooth, and intact.
What are the abnormal findings to assess for in the nipple and areola? (4)
Abnormal findings include fixation, deviation in nipple pointing, scaling or rash, and discharge when not lactating.
What does nipple fixation indicate? (2)
It may indicate underlying malignancy or fibrosis that prevents normal movement of the nipple.
What does deviation in nipple pointing suggest?
It can suggest an underlying mass pulling the nipple in a different direction.
What is abnormal about scaling or rash on the nipple/areola?
It may indicate Paget’s disease of the breast, eczema, or infection.
What is concerning about nipple discharge when not lactating? (3)
Spontaneous discharge can be a sign of intraductal papilloma, infection, or breast cancer and should be evaluated.

What is an abnormal finding in the nipple that can indicate a serious condition?
Paget's disease, which is cancer of the mammary glands.
What position should the woman be in to examine the axillae?
Sitting, with her arm lifted and supported so muscles are loose and relaxed.
What should you inspect the axillae for? (3)
Rash, infection, or any skin changes.
Which hand should you use to palpate the axillae?
Use your right hand to palpate the woman’s left axilla.
How should you palpate the axilla?
Reach fingers high into the axilla and move them firmly down in four directions.
How can you increase the surface area you can reach during palpation?
Move the woman’s arm through its range of motion.
Are lymph nodes normally palpable in the axilla?
Usually not, though a small, soft, nontender node may be felt in the central group.
What could a fixed and hard lymph node indicate?
It could be cancerous.
What could a tender and warm lymph node indicate?
It could indicate an infection.
What should be noted during axillary palpation?
Any enlarged or tender lymph nodes.
What position should the patient be in to palpate the breasts?
The patient should be in a supine position with a small pillow under the side being palpated and the arm lifted over the head.
Which part of the hand should be used to palpate the breast and Tail of Spence?
Use the 3 middle fingers held together, using the flat part of the fingers, not the fingertips.
What type of movement is recommended when palpating the breast?
A rotary or circular movement.
How should pressure be applied when palpating the breast tissue?
Press firmly to feel the underlying tissue, alternating between light, medium, and deep pressure.
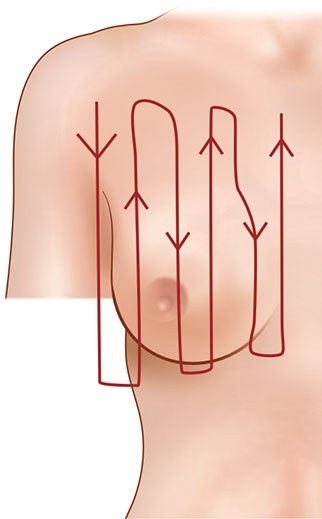
What is the vertical strip palpation pattern?
A technique in which the breast is palpated in straight vertical lines from top to bottom, side to side, ensuring the entire breast is systematically examined.
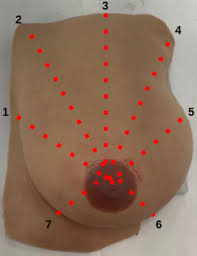
What is the wedge (spokes) palpation pattern?
A technique where the breast is palpated from the outer edges toward the nipple in a spoke-like pattern, like slices of a pie, covering all radial areas.
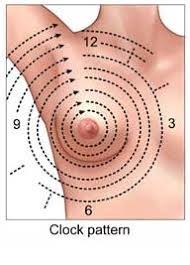
What is the circular palpation pattern?
A technique in which the breast is palpated in concentric circles starting at the outer edge and moving toward the nipple, covering the entire breast tissue.
What is the recommended method for describing the location of a breast mass?
Use the breast as a clock face and describe the distance from the nipple in centimeters.
What is the recommended position for palpating large, pendulous breasts?
Sitting position with the non-dominant hand underneath for support and the dominant hand on top to palpate.
What is the bimanual technique in breast palpation?
Using both hands, one underneath the breast for support and the other on top to palpate.
How should the nipple and areola be palpated?
Compress gently between the thumb and forefinger.
How should compression be performed during breast palpation?
Compress in all quadrants of the breast.
What should you note if breast discharge appears?
The color and consistency (thick or thin).
When is breast discharge typically considered benign?
When it occurs bilaterally.
What is galactorrhea and when does it occur?
Discharge that is present during pregnancy, lactation, and up to a year after weaning.
What should you be aware of when palpating a post-mastectomy patient?
Be aware of the patient’s concerns about the potential return of cancer.
What should you inspect on a post-mastectomy patient?
Inspect the anterior chest and the incisional site, noting the stage of healing.
Which breast should be palpated first in a post-mastectomy assessment?
Palpate the intact breast first.
After palpating the intact breast, what is the next step?
Palpate the mastectomy area.
What is the normal structure of the male breast?
The normal male breast has a flat disk of undeveloped breast tissue beneath the nipple.
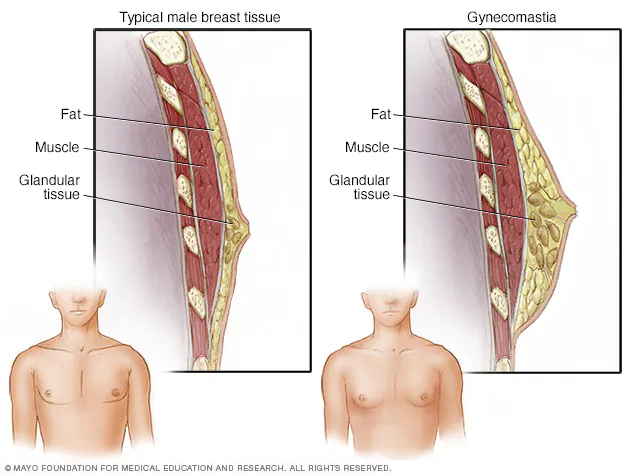
What is gynecomastia?
It is a benign growth of male breast tissue, making it distinguishable from other chest wall tissues.
How does gynecomastia feel on palpation?
It feels like a smooth, firm, movable disk beneath the nipple.
When does gynecomastia normally occur?
It occurs normally during puberty and is usually temporary.
What are other possible causes of gynecomastia besides puberty?
It can also be caused by anabolic steroid use.
What are the characteristics of male breast cancer?
It often presents as a painless mass, nipple discharge can be an early warning sign, it spreads quickly due to lack of tissue, and it is typically diagnosed about 5 years later than in women.
What does normal breast tissue feel like in nulliparous women? (3)
Normal breast tissue feels firm, smooth, and elastic.
How does breast tissue change after pregnancy?
After pregnancy, breast tissue feels softer and looser.
What is a normal cause of premenstrual breast engorgement and tenderness?
Increasing progesterone causes premenstrual breast engorgement and tenderness.
What is often the first sign of pregnancy related to the breasts?
Breast tenderness is often the first sign of pregnancy.
What is an inframammary ridge, and is it normal?
It is a firm transverse ridge in the lower quadrants, more noticeable in large breasts, and is a normal finding.
What should be noted if a lump or mass is felt during breast palpation? (5)
Note the characteristics, location, whether it is hard or soft, smooth or round, or lumpy.
What is the recommended way to assess the size of a breast mass?
Judge in three dimensions. Example: 2 cm wide, 2 cm long, 1 cm thick.
What are the possible shapes of a breast mass? (4)
Round, oval, lobulated, or indistinct.
How is the consistency of a breast mass described?
Soft, hard, or firm.
How do you determine if a breast mass is movable?
Check if it is freely mobile or fixed.
What does distinctness of a breast mass refer to? (2)
Whether it is solitary (single lump) or multiple (lumps).
What should be noted about the nipple when assessing a breast mass?
Whether it is displaced (doesn’t fall on nipple line or raised) or retracted.
What skin changes over a breast lesion should be assessed?
Redness, warmth, thickening, vascular patterns, dimpling, or retractions.
How is tenderness of a breast mass evaluated?
By checking if it is tender to palpation.
What does lymphadenopathy assessment involve?
Checking if any regional lymph nodes are palpable.
How is the depth of a breast mass described? (3)
As superficial, midlevel, or deep (against ribs).