Upper GI disorders: Mouth and Oesophagus
1/41
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
What is oral ulceration?
break in the oral epithelum exposing nerve endings in the underlying connective tissue, caused by physical or chemical injury, infections, drugs, malignacy, systematic disease - can be used as a marker of underlying diseases
What is Stomatitis?
inflammation of the lying of any of the soft-tissues of the mouth caused by poor oral hygine, poorly fitted dentures, heat burns, drugs, allergy or infection
What is leukoplakia?
painless white patches on the side of the tongue or cheeks, appears with various disoders
Dysphagia
difficulty swallowing
what motor functions does the oesophagus have?
it contracts rhythmically to propel food towards the stomach
What is the UOS and what’s its function?
upper oesophageal sphincter, prevents air entering oesphagus and oesphagopharyngeal reflux
What is the LOS, and what’s its function?
lower oesophageal sphincter, prevents gastroesophageal reflux
What holds the LOS shut?
high intraluminal pressure until food needs to enter the stomach
What does GORD stand for?
gastro-oesophageal reflux disorder
What are the causes of GORD?
obesity, medication, spicy, acidic or fatty foods, smoking
What happens in GORD?
acid from the stomach refluxes up into the oesophagus where there is no protective barrier so heartburn is felt which is due to acid irritating the surface,
What causes GORD?
genrally transient LOS relaxation in absance of swallowing, due to stimulaton od gastric vagal mechanoreceptors and oesophageal hypomotlity
What are the three types of GORD?
Non-erosive reflux disease (heartburn)
erosive oesophagitis - acute inflamatory response is triggered by multiple damages
Barrett’s oesophagus - metaplasis of mucosa
What is barrett’s oesophagus?
premalignant state caused by repeated damage to the oesophagus by acid reflux, it damages the epthelial cells of the oesophagus which regenerate as a different type of cell, continous damage can lead to malignancy
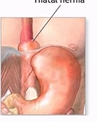
What is hiatal hernia?
part of the stomach pokes up through the diaphram, the oesophagus can move through, become trapped, can be serious as vunrable to infection and damage, sometimes fixes itself, sometimes surgery is required
What is achalasia?
inadaquate LOS relaxation
What is diffuse oesophageal spasm?
uncoordinated contraction of the oesophagus
What is hypercontraction?
the oesophagus contracts too much, this causes damage
What is ineffective oesophageal motility?
hypocontraction of the oesophagus
How do you treat motility disorders of the oesophagus?
muscular activator or blocker
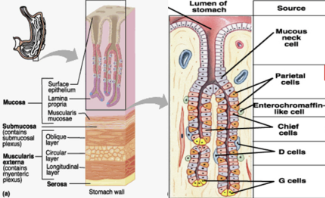
What cells are found in the acid secreating oxyntic gland area? What are there functions?
mucous cells - secreate mucous, protecting the underlying cells from damage and protection
Chief cells - secrete pepsinogen (proenzyme for pepsin)
ECL cells - EnteroChromaffin-Like cell, secrete histamine to trigger acid secreation
parietal cells - secrete HCl and intrinisic factor
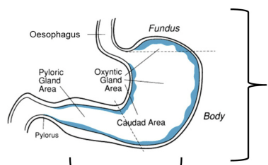
What cells are found in the pyloric gland area? What’s there functions?
mucous cells
G cells - gasterin cells - hormonal triggers when stomach is full, empty
D cells - secrete somatostatin hormone - involved in feedback mechanism in the stomach that switches off acid secretion, triggers when more alkaline as food leaves the stomach, the somatostatin then causes the parietal cells to stop producing HCl
What is the role of mucousal cells?
surface one secrete think, protective, alkaline-rich mucus creating a barrier, they are stimulated by mechanical and chemical irritation and parasympathetic inputs, barrier can be damaged by bacterial or viral infection and certain drugs (NSAIDs)
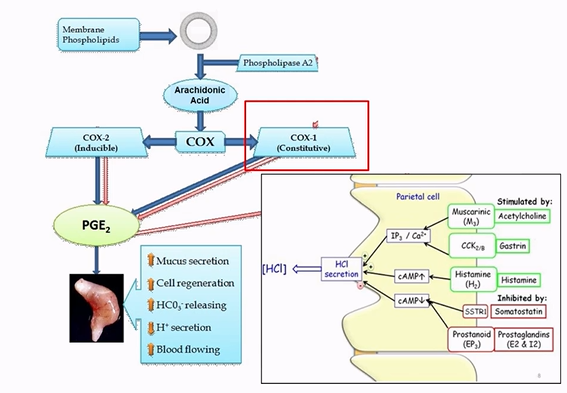
What do parietal cells do?
secrete 1-2L of 150-160mM HCl a day (pH 0.8-1)
What does stimulation of gastric acid secreation involve?
translocation of H⁺/K⁺-ATPase from cytoplasmic vesicles to the apical membrane where they fuse with the membrane to increase the surface area and membrane pumps

What are the positive regulators for gastric acid release?
acetylcholine, histamine and gastrin

How does acetylcholine stimulate gastric acid secreation?
enteric neurons directly stimilate parietal cells, acetylcholine activates muscarinic (M₃) receptors, a G-coupled receptor using the PLC pathway, uses increases in Ca²⁺ and diacylglycerol through Phospholipase-C (PLC)-inositol 1,4,5-triphosphate (IP₃) pathway
How does histamine stimulate gastric acid secreation?
from ECL cells, secreted into local environment where it has a direct effect on the parietal cells, it has paracrine activity, actvates histamine H₂ receptors, G-coupled receptor which increases cyclic AMP (cAMP), this is the most powerful stimulus, more rapid acting than the other pathways
How does gastrin stimulate gastric acid secreation?
from G cells, endocrine hormone (circulation), stimulates ECL cells to release histamine which then activates the parietal cells, directly stimulates parietal cell proliferation, acts on cholecystokinin B (CKKB/CCK2) receptors, G-coupled receptors linked to increases in Ca²⁺ and diacylglycerol through Phospholipase-C (PLC)-inositik 1,4,5-triphosphate (IP₃) pathway
What is the negative regulator for gastric acid secreation? How does it work?
Somatosatin from D cells, directly inhibits parietal cell secreation, gastrin and histamine release
What are the three phases of acid secretion stimulation?
cephalic phase, gastric phase, intestinal phase
What happens in the cephalic phase of acid secreatio stimulation?
sight/smell/thought of food

What happens in the gastric phase?
food enters stomach, causes stomach to stretch, causes mechanoreceptor neural reflex causng peptic acid release, peptides in the food stimulate G cells to release gasterin, increases pH as food nutrilises acid in the stomach preventing D cell activity
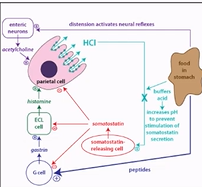
What happens in the intestinal phase?
chyme enters the duodenum, feedback mechanism that switches off acid secreation at this point by inhibiting gasterin release, the chyme entering the duodenum causes a drop in pH as the food is no longer nutralising the acid, this drop in pH then stimulates the D cells to secrete somatostatin which then stops gastric acid secreation, stomach distention decreases.

What happens when the stomach distends via the vagovagal reflex?
direct stimulation of ECL cells to release histamine and G cells to release gasterin via GRP, also increased by pyloric antrum exposure to peptides
inhibtion of somatostatin release from D cells in antrum
HCl secreation increases due to gasterin and histimine production
What is the mechanism of HCl secreation at the apical surface?
CO₂ diffuses into parietal cells from the plasma, it is hydrated to carbonic acid, by carbonic anhydrase
H₂CO₃ dissociates into H⁺ and H₂CO₃⁻
H⁺/K⁺-ATPase actively transports H⁺ out and K⁺ in, Na⁺ is also actively reabsorbed
K⁺ recycles to gastric lumen via K⁺ channel, so elevated K⁺ in gastric juice
Cl⁻ exists passively from cell via Cl⁻ channel in the basalateral membrane
The extracellular H⁺ generates osmotic gradient, causing outward H₂O diffusion
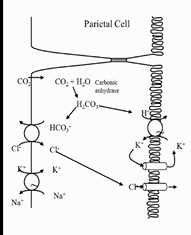
What are the concentrations of stuff in the gastric juice?
160mM HCl, 15mM KCl, small NaCl
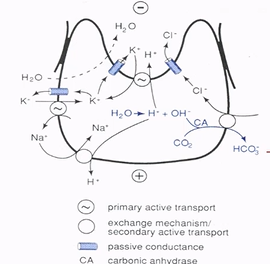
What happens at the basolateral membrane in the mechanism of HCl secreation?
Na⁺/K⁺-ATPase maintains intracellular Na⁺ and K⁺
Exchanger promotes HCO₃⁻ exit and Cl⁻ uptake, maintains cellular pH but creates an alkaline tide - the blood will go slightly alkaline during this period
negative gastric arter-venous CO₂ gradient
What is prosterglandin E₂?
triggers increase in mucus secreation, cell regeneration if there is any cell damage, and release of the bicarbonate, reduces acid secreation and increases blood flow, Cox 1 and 2 are involved
How is the mucosal protection layer formed?
vagal stimulation and irritation stimulate gastric mucous cells to secrete mucin (glycoprotein), these are cleaved by pepsin so need to be continulusly produced
gastric surface epithelial cells secrete HCO₃⁻ when stimulated by ACh, HCl and PGs, the HCO₃⁻ accumulates near the cell surface
HCO₃⁻ rich fluid is trapped near the apical border of the epithelium protecting the gastric surface epithelum, creates a ‘microenvironment’
impermeable apical cell membrane has tight junctions limiting H⁺ ion diffusion
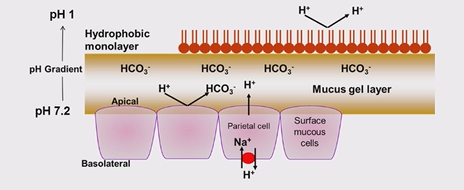
What inhibits HCO₃⁻ secretion?
adrenergic imput - this is prominant in stress
What are the two locally produced prostaglandins (Stomach) and what do they do?
PGE₂ and PGI₂, they reduce HCl secretion and increase mucus and bicarbonate secretion