Body Fluids Quiz Study Guide
1/79
Earn XP
Description and Tags
CSF, serous, synovial fluid and BAL, Amniotic, Fecal and Seminal fluid analysis lecture slides
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
Hemocytometer Formula (Low and High)
LOW: (avg. # of cells counted x dilution factor)/(# of SMALL squares counted x 0.04 x 0.1) = cells/uL
HIGH: (avg. # of cells counted x dilution factor)/(# of LARGE squares counted x 0.1) = cells/uL
(Count RBCs and TNCs separately) The 2 sides must agree within 10%
A CSF sample was diluted using 1 parts CSF and 9 parts saline. 49 nucleated cells were counted in 5 small squares on side A and 51 on side B. What is the cell count per ul?
Avg = (49+50)/2
(50 x 10)/(5 x 0.04 x 0.1) = 25 x 10^3 cells/uL
When given cells in 1 large square, which ones are counted as "in"?
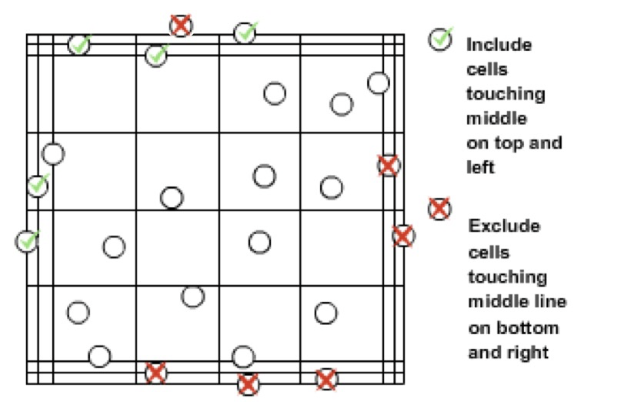
1 “small square” has 16 smaller boxes within it.
Sometimes the “small square” is bordered by 3 lines. Use the middle line as the border
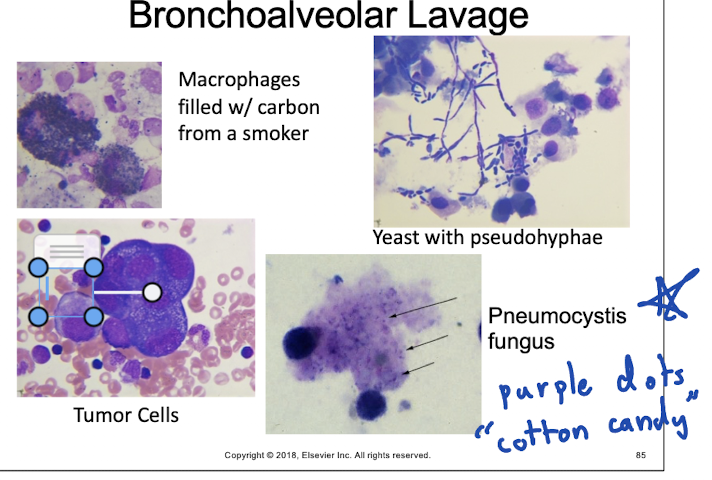
Bronchoalveolar Lavage (BAL) Fluid
Not a naturally occurring fluid
Not sterile site, common to see bacteria
Indications:
To detect microbiologic pathogens in immunocompromised patients
To detect malignancy
Synovial Fluid Collection (Arthrocentesis)
NEEDS hyaluronidase
Needle inserted into joint space.
Joint fluid dispensed into tubes based on test ordered
Chemistry: no anticoagulant
Hematology: Sodium Heparin/Liquid EDTA
Microbiology: Heparin or SPS
Patient fasting: minimum 4-6 hours for accurate glucose comparisons.
Blood sample collected at the same time.
Normal fluid volume: 0.1 to 3.5 mL, typically viscous.
Dry tap' can occur if there's no fluid buildup.
Bronchoalveolar Lavage (BAL) Fluid Collection
Done by bronchoscopy and collection in a sterile container: Aliquots of 20-50mL of sterile saline injected, then removed (1st aliquot discarded).
Common Cells Seen in BAL:
Macrophages
Lymphs
PMNs
Eosinophils
Ciliated columnar epithelial cells
Squamous cells are contaminants
Color and Appearance
Normally hazy and colorless.
May have mucus
Milky white = infection
Red = bloody
Serous Fluids Lining Cells are called?
Mesothelial Cells
CSF Lining Cells
Choroid - Lining of Choroid Plexus
Ependymal - Lining of Ventricles of neural
Spindle - Arachnoid Membrane Lining
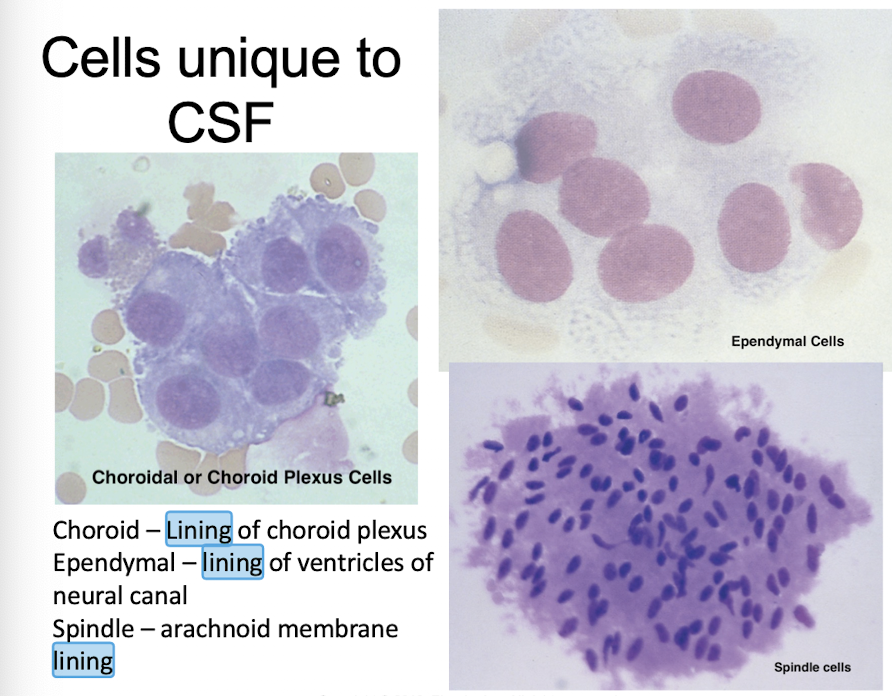
CSF Lining Cell
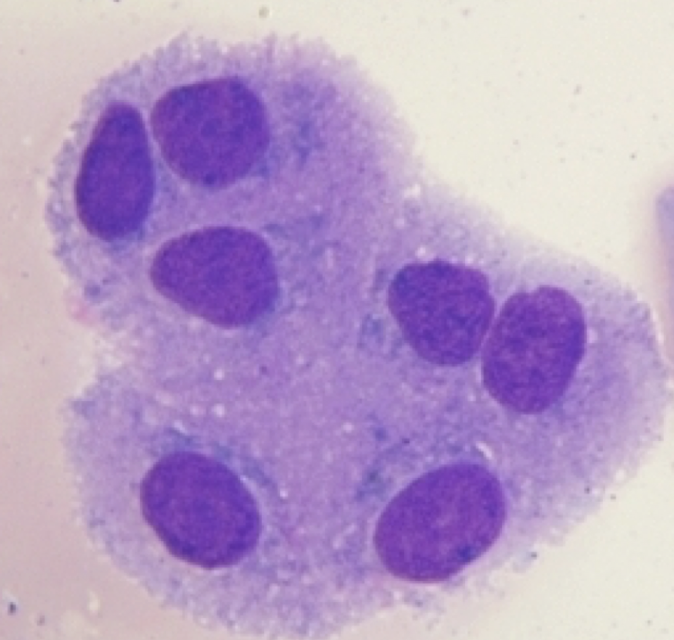
Choroid Plexus Cell
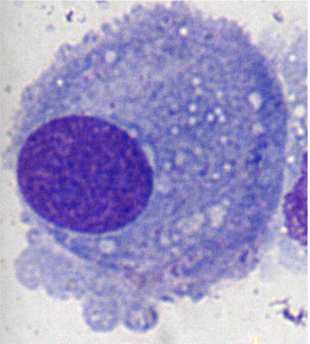
Synovial Lining Cell
Synoviocytes
Eccentric nucleus
“Fried Egg” appearance
Possible debris inside cytoplasm
Serous Fluid Lining Cell
Mesothelial Cell
Bronchoalveolar Lavage Fluid (BAL) Lining Cell
Macrophage and Ciliated Cell
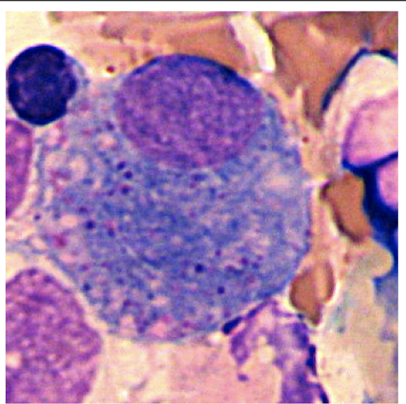
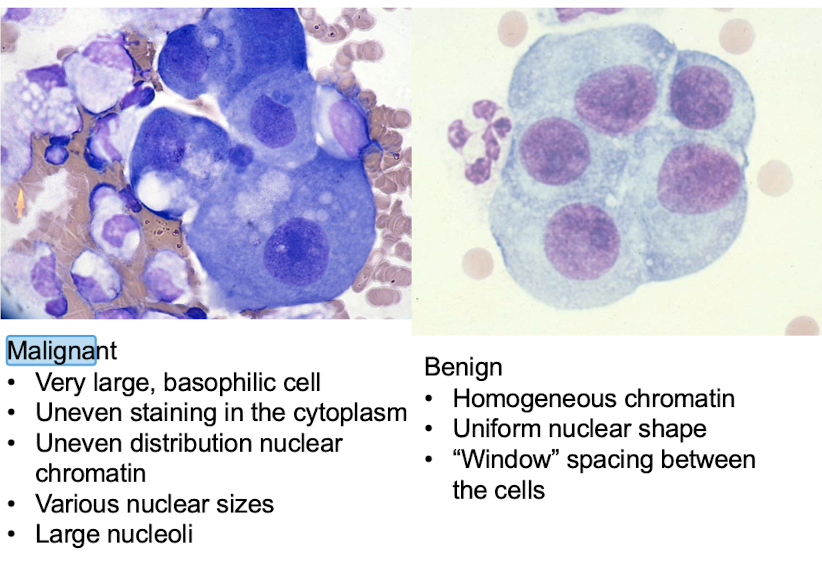
Malignant Cells
Very large, basophilic cells
Irregular shaped nuclei and nucleoli
Uneven staining in the cytoplasm
Various nuclear size and shape
Vacuoles over the nucleus
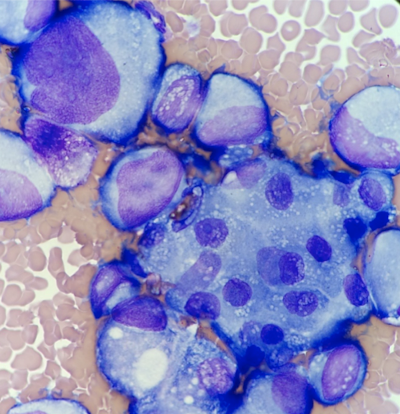
Malignant Cells vs Benign Cells
What is different about each bodily fluid?
CSF: Clear and colorless, cushions the brain and spinal cord.
Serous Fluid: Pale yellow, lubricates surfaces between organs.
Synovial Fluid: Viscous, provides lubrication in joints.
BAL (Bronchoalveolar Lavage): Obtained from lungs, reflects pulmonary pathology.
Amniotic Fluid: Surrounds fetus, cushions and facilitates movement.
Fecal Matter: Composed of waste and undigested food.
Seminal Fluid: Viscous secretion that contains sperm and nutrients.
Pleural, Pericardial, and Peritoneal Fluid Collection
Sterile tubes coated w/ anticoagulant used for fluid specimens (Containing fluid or blood) - for hematology or micro
Non-anticoagulant red-tubes (chem and immuno)
Tubes at rm temp and sent to lab IMMEDIATELY
If needed for chem: centrifuge and refrigerate supernatant
Collect a blood sample (to compare)
CSF Order of Draw
3-4 sequentially labeled tubes
#1 - Chemistry & Immunology: supernatant is refrigerated or frozen
may contain skin cells or blood from collection
#2 - Microbiology: Room temp
To avoid skin contamination
#3 - Hematology: Refrigerated
Less likely to contain blood from collection, that could interfere with CSF counts
#4- Other Testing: Refrigerated
Use Tube 4 for heme, less blood contamination
If only 1 tube for CSF, how do we proceed?
MICRO: minimize contamination/organisms might die
HEME: count cells and make slide before cells degrade
CHEM & IMMUNO: chemicals and proteins well preserved
One tube = same order as multiple tubes, but chemistry/immuno is moved back to the end of the line.
Cerebrospinal Fluid (CSF) collection
“Spinal Tap” is performed aseptically to collect CSF from the 3rd & 4th or 4th & 5th lumbar interspace, after measuring opening pressure with a manometer; normal pressure allows for 20 mL collection while abnormal pressure limits collection to 1-2 mL.
Which fluid needs hyaluronidase?
Synovial fluid →
Joint space is lined with synoviocytes:
synthesizes hyaluronate, a mucopolysaccharide that makes synovial fluid viscous
To aid pipetting for cell counts, synovial fluid is mixed with hyaluronidase or diluted with saline
Hyaluronidase breaks down hyaluronate
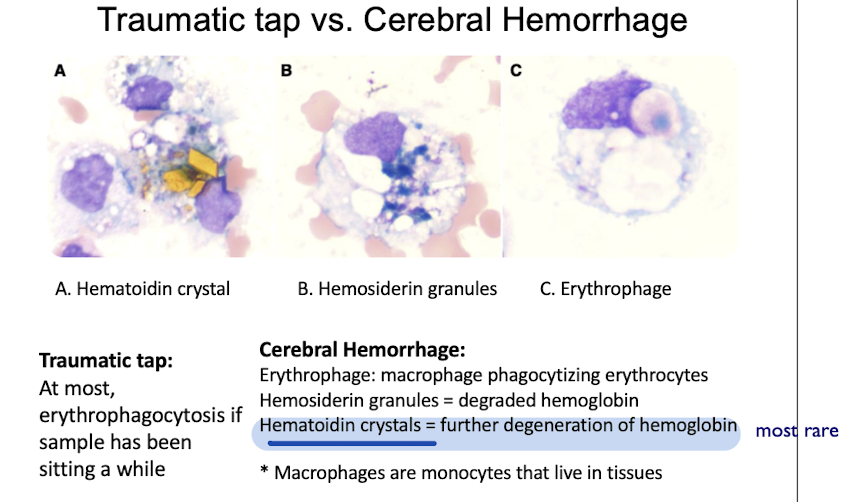
___ crystals are found in CSF?
Hematoidin crystals (rare) and/or Hemosiderin granules during Cerebral Hemorrhage
___ crystals are found in Synovial Fluid?
Monosodium Urate Crystals (MSU)
needle-shaped and can indicate gout when present in excess.
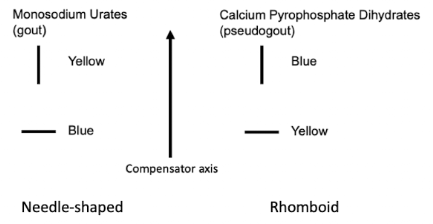
Monosodium Urate Crystals
Gout - buildup of MSU in joints
Strongly negative birefringent
Crystals are yellow (negative) when parallel to the slow axis
of the compensator
Crystals are blue (positive) when perpendicular to the axis of the compensator
Calcium Pyrophosphate Dihydrate (CPPD)
Causes pseudogout.
Associated with:
Degenerative arthritis (e.g., osteoarthritis)
Hyperparathyroidism (regulates calcium levels).
Crystals:
Weak positive birefringent.
Blue (positive) when parallel to the axis of the compensator.
Yellow (negative) when perpendicular to the axis of the compensator.
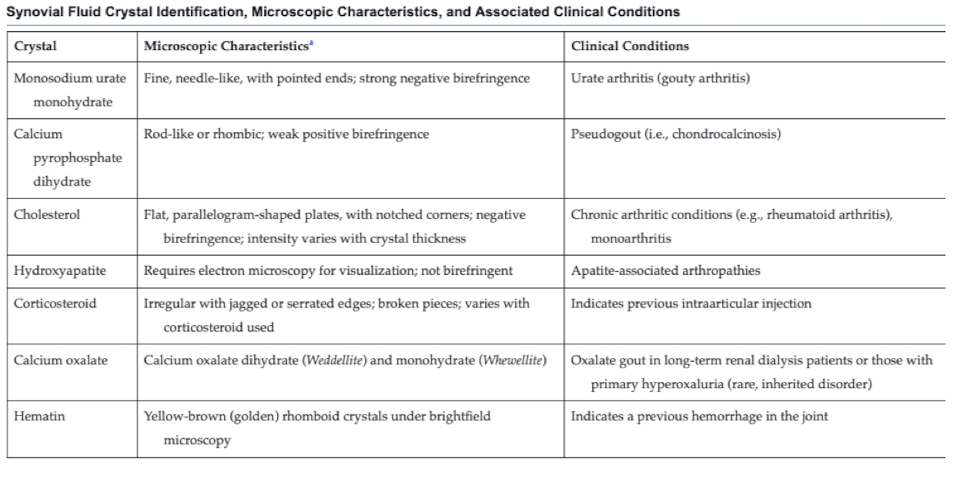
MSU vs CPPD
MSU crystals = gout, while CPPD = pseudogout. MSU crystals are needle-shaped and show strong negative birefringence, whereas CPPD crystals are rhomboid-shaped and show weak positive birefringence.
What crystal can resemble MSU or CPPD?
Corticosteroid Crystals
Crystal Identification
Which bodily fluid is sterile?
Cerebrospinal fluid (CSF), found in the central nervous system.
How is synovial fluid viscosity determined?
by the presence of hyaluronate, a mucopolysaccharide synthesized by synoviocytes, which increases the fluid's viscosity. → String Test
To aid pipetting for cell counts, synovial fluid is mixed with hyaluronidase or diluted with saline, as hyaluronidase breaks down hyaluronate, reducing viscosity.
Traumatic tap vs. Hemorrhage
Traumatic tap = blood contamination during a procedure (decreases as tubes are collected)
NO Xanthachromia
Little to no erthryophagocytosis
Hemorrhage = actual bleeding within the fluid (level of blood stays the same)
Xanthachromia present
erthryophagocytosis along with possible hemosiderin & hematoidin crystals
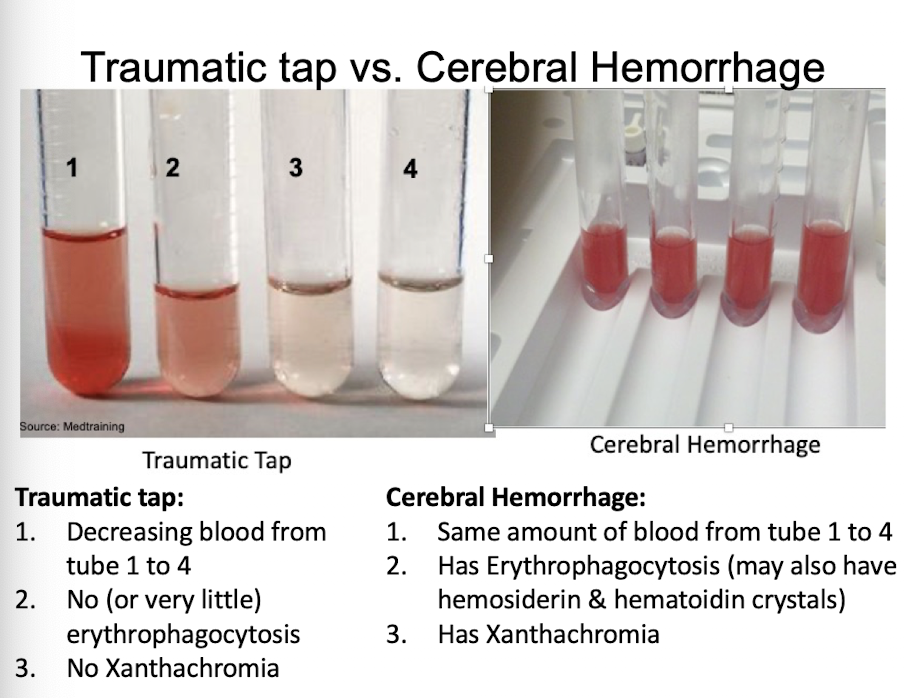
Traumatic Tap
Greatest amount of blood in tube 1, least in last tube
After centrifugation, colorless supernatant
Hemorrhage
Consistent amount of blood in all tubes
After centrifugation, xanthochromic supernatant
Macrophages with phagocytosed RBCs
Macrophages stain positive for hemosiderin and may include hematoidin crystals
(CSF)/Serum Albumin Index Purpose
CSF albumin comes from blood → used to assess permeability of blood-barrier
Formula: Albumin(CSF) mg/dL / Albumin(Serum) g/dL
<9 = normal, 9 to 14 = minimal impairment, 15 to 100 = moderate to severe; exceeding 100 complete breakdown
Quantitation: nephelometry or reflectance spectrophotometry
Cerebrospinal Fluid (CSF) Immunoglobulin G (IgG) Index Purpose
Reference interval for IgG index: 0.30 to 0.70
Values > increased intrathecal production of IgG
Ex: multiple sclerosis or inflammatory
Values < compromised blood-brain barrier
What differentiates Chylous vs. Pseudochylous Effusions?
Chylous Effusion:
Results from lymphatic obstruction.
High in triglycerides, chylomicrons, and lymphocytes.
Pseudochylous Effusion:
Associated with chronic inflammation.
Contains cholesterol and diverse cell types.
High cholesterol promotes inflammation
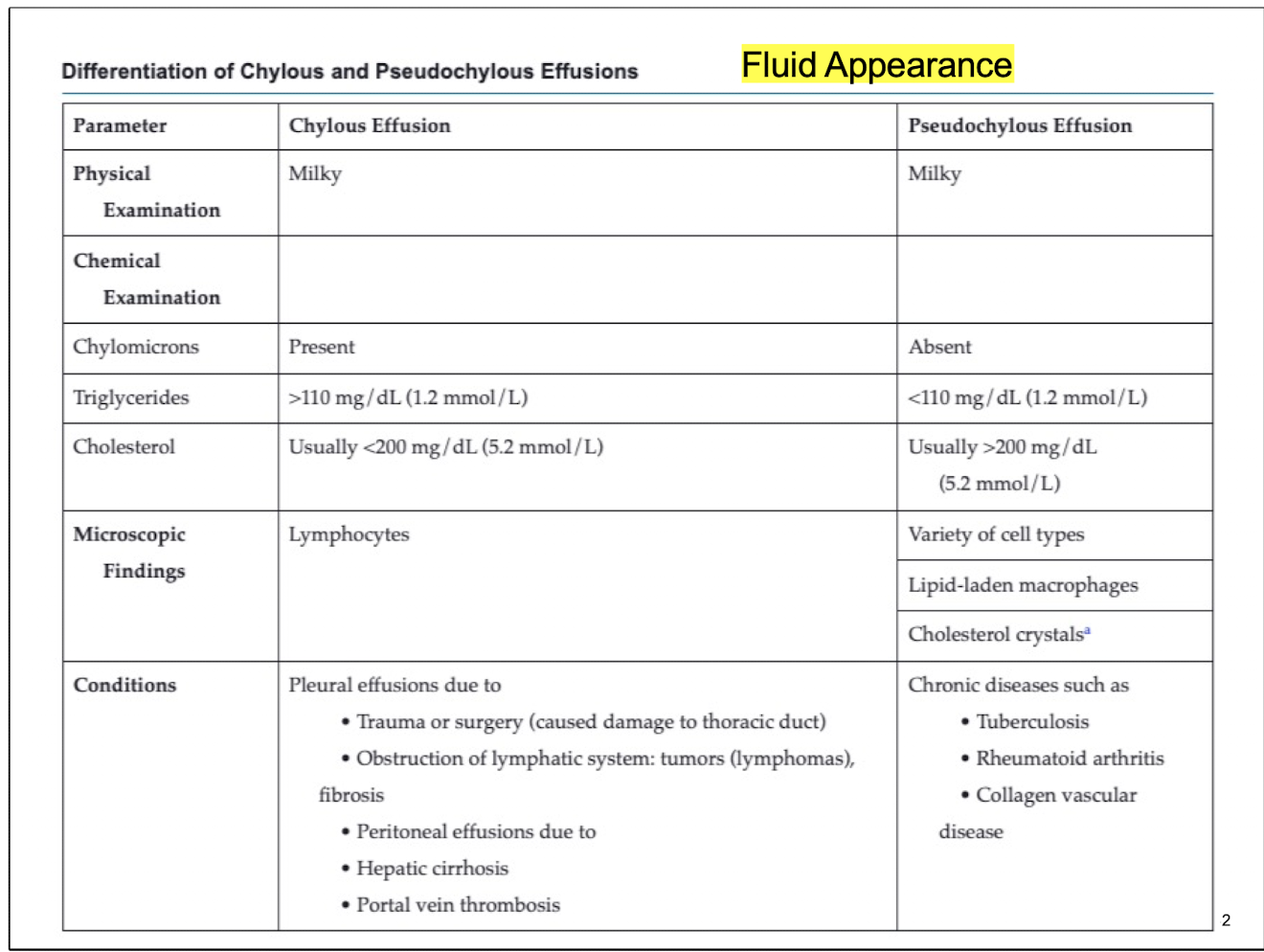
Chylous effusions
Pleural & Peritoneal effusions (b/n lungs & chest wall), High triglycerides, chylomicrons, lymphocytes
Effusions in peritoneal cavity
Result from obstructions in lymphatic drainage
Effusions = more triglycerides, chylomicrons, and lymphocytes
Chylomicrons present
Triglycerides > 110 mg/dL
Cholesterol < 200 mg/dL
Microscopic: Lymphocytes
Pleural effusions due to…
Trauma or surgery (damage to thoracic duct)
Obstruction of lymphatic system: tumors (lymphomas), fibrosis
Peritoneal effusions due to…
Hepatic cirrhosis
Portal vein thrombosis
Pseudochylous effusions
High cholesterol (= inflammation); variety of cell types
effusions w/ chronic inflammatory conditions
Contains cholesterol & variety of cell types
High cholesterol levels promote inflammation
Triglycerides <110 mg/dL
Cholesterol >200 mg/dL
Microscopic: Variety of cells, lipid-laden macrophages, cholesterol crystals
Seen in chronic diseases such as…
Tuberculosis
Rheumatoid arthritis
Collagen vascular disease
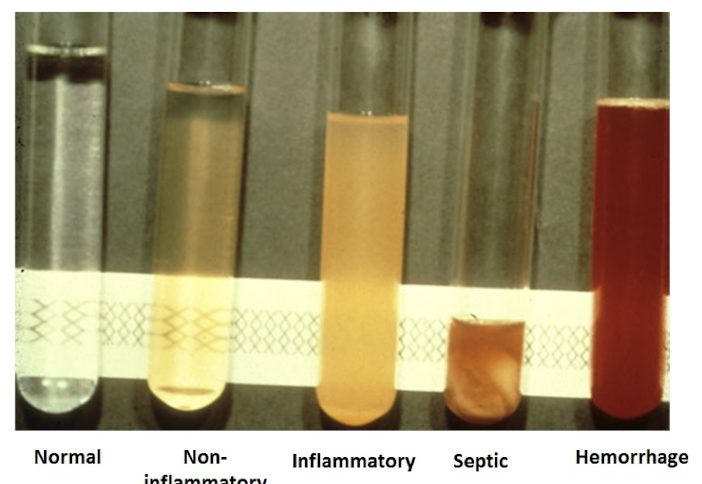
What differentiates Transudates vs. Exudates?
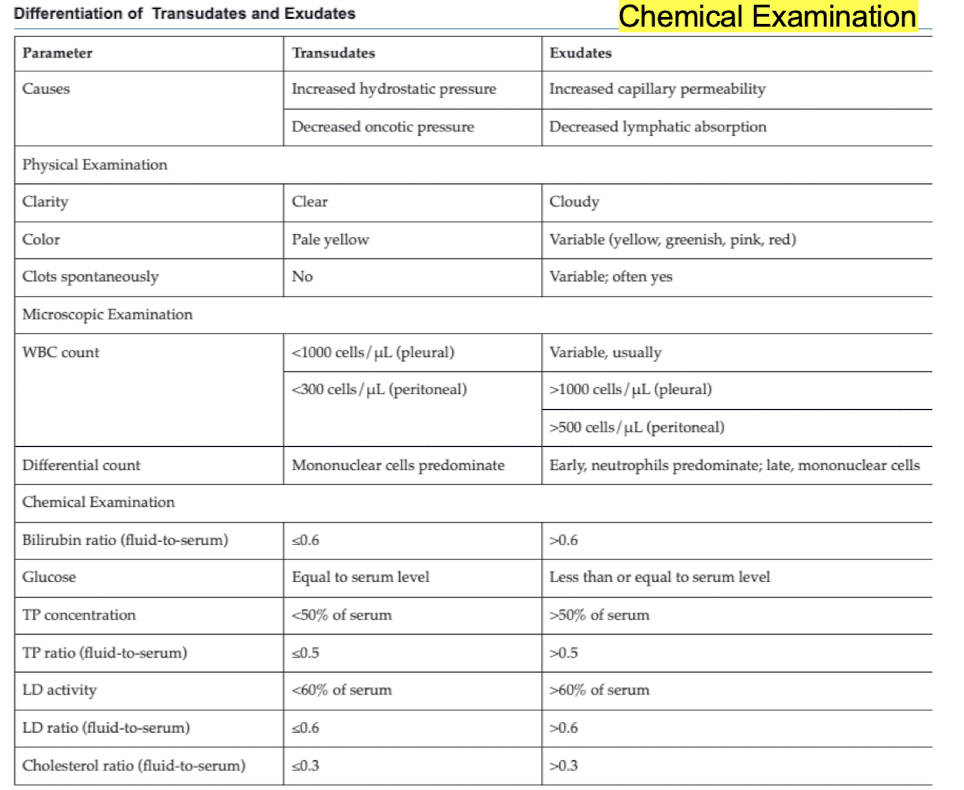
Transudates
Thin, watery fluids w/ low protein content that accumulate in body cavities due to imbalances in fluid pressure or protein levels in blood
Increased hydrostatic pressure - accumulates in body cavity
Clear, pale yellow, no clots
Lower cell count
Mononuclear cells predominate
Bilirubin, TP, LD, cholesterol LOWER
Glucose equal to serum level
Exudates
Fluids, cells, or other cellular substances that are discharged from blood vessels, usually from inflamed tissues
Increased capillary permeability
Due to malignancy, more cells/microorganisms
Cloudy, more color, could clot
Early neutrophils predominate (indicates infection), mononuclear cells
Bilirubin, TP (total protein), LD, cholesterol ALL HIGH
Glucose low, organisms consuming glucose
Charcot-Leyden crystals may be seen
Which is more severe? Transudates or Exudates
Exudates
Bilirubin, TP (total protein), LD, cholesterol ALL HIGH
Glucose low, organisms consuming glucose
(Compared to transudates:Bilirubin, TP, LD, cholesterol LOWER, Glucose equal to serum level)
Joint disorder classification - what is different about each?
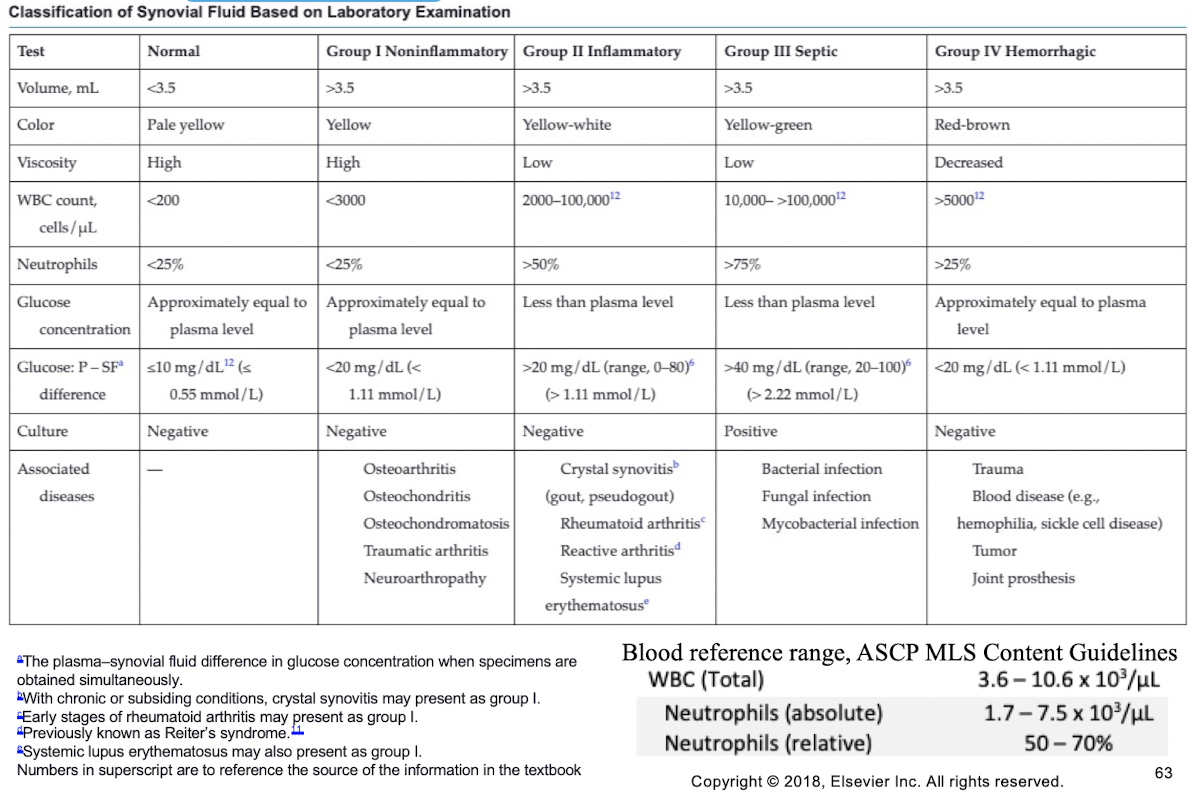
Joint Fluid Colors and Their Implications
Normal: Pale yellow or colorless, clear.
Red/Brown: Indicates trauma during collection or disorders allowing blood into the joint cavity.
Greenish/Purulent: Suggests infections.
Milky: Associated with tuberculous arthritis or systemic lupus erythematosus.
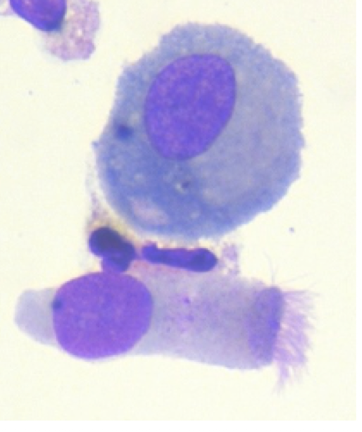
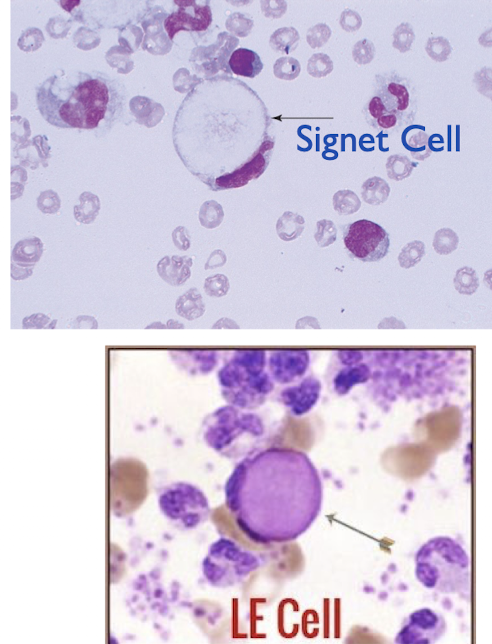
Signet ring vs. LE cell
Signet cells = Large Vacuole, nucleus flattens to one side → many: possible malignancy
LE cell (Lupus erythematosus) = ingested WBC within vacuole (pink blob) → autoimmune disease
Amniotic fluid Collection
Transabdominally or vaginally with simultaneous ultrasound examination
Using long aseptic needle into numbered tubes
10 to 20 mL of fluid collected by physician into numbered tubes
Use sterile plastic containers
Cells adhere to glass container walls
Protect from light
Bilirubin is light sensitive
Room temp or body temp: Cell culture, genetic studies, microbiology
Assay immediately or refrigerate - fetal lung maturity testing
Amniotic fluid appearance
Normal amniotic fluid is colorless or pale yellow
Yellow or amber: bilirubin
Greenish: meconium
Pale pink to red: blood or hemoglobin
* Dark red/brown: maybe fetal death
All amniotic fluid is somewhat
turbid
Early pregnancy: little particulate
matter
Late pregnancy: more turbid; increased fetal cells, hair, and vernix
Amniotic fluid RDS tests
FLM results are compared to reference
ranges based on gestational age of fetus to determine lung maturity
Fetal Lung Maturity tests:
L/S Ratio
Phosphatidylglycerol
Foam Stability Index
Lamellar Body Counts
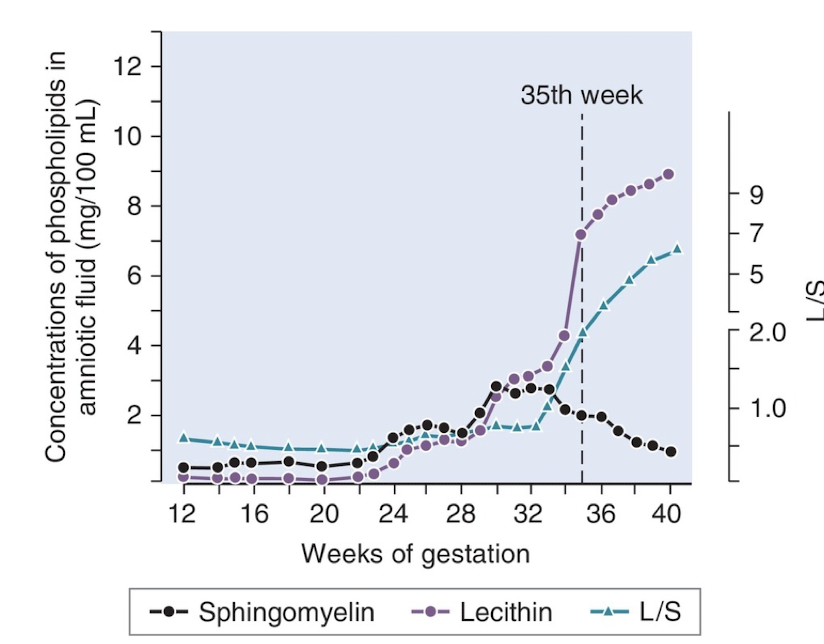
RDS tests - L/S Ratio
Surfactants keep alveoli open during respiration
Lecithin: Major pulmonary surfactant.
Sphingomyelin: Phospholipid in cell membranes; role not fully established.
Equal production of lecithin and sphingomyelin until 33 weeks.
From 34 to 36 weeks: Increased lecithin, constant/decreased sphingomyelin.
L/S ratio ≥ 2.0 indicates mature fetal lungs.
30%-40% of infants with L/S ratio 1.5 to 2.0 do not develop RDS.
Measured using thin-layer chromatography.
Blood presence in specimen decreases mature result, increases immature result.
Meconium-contaminated specimens are unreliable
Foam Stability Index (FSI) in RDS Testing
Less reliable test, not frequently used.
Stable foam produced by surfactants shaken with ethanol.
Amniotic fluid mixed with varying ethanol concentrations.
Highest ethanol concentration yielding stable foam indicates FSI.
FSI ≥ 0.47 suggests fetal maturity.
Blood and meconium contamination leads to inaccurate results.
Phosphatidylglycerol (PG) in RDS Testing
Phosphatidylglycerol is a phospholipid that enhances surfactant spread across the alveolar surface.
Not detectable until 35 weeks' gestation.
Techniques:
Thin-layer chromatography (TLC)
Slide agglutination using anti-PG antibodies.
Positive tests are very specific but may have many false negatives.
PG tests are not affected by blood or meconium contamination.
In slide agglutination, latex beads coated with anti-PG antibodies agglutinate if PG is present.
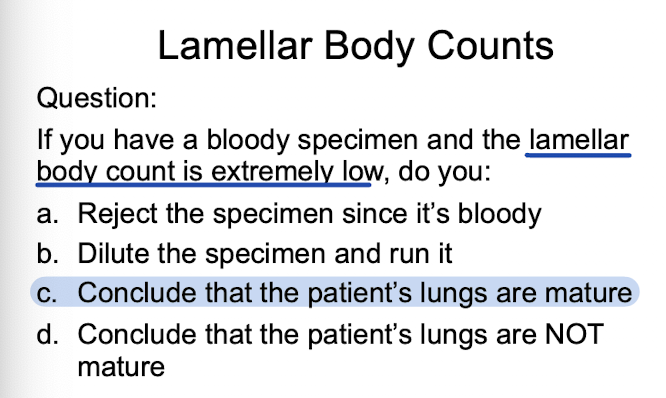
Lamellar Body Counts for RDS Testing
Measure pulmonary surfactants in lamellar bodies from amniotic fluid.
Normal levels in third trimester: 50,000 to 200,000/uL.
Level > 50,000/uL indicates fetal lung maturity.
Use automated hematology counter's platelet channel for measurement.
Avoid bloody specimens; they can falsely elevate lamellar counts.
Requires small sample size
What information can you get if a bloody specimen has a low lamellar body count?
Since blood in the sample falsely increases lamellar body count due to platelet contamination, a low LB count means that the actual result is extremely low. Therefore, the fetus’ lungs are very immature.
How to differentiate amniotic fluid from urine
Amniotic Fluid
Has glucose
Significant Protein
Creatinine is like plasma
NO UREA
Normal Urine
Essentially NO glucose or protein
High creatinine
HIGH UREA
Why do we use all 4 chemicals in Urine Differentiation from Aminotic fluid?
Late pregnancy causes an increase in amniotic fluid creatinine and urea (from fetal urine) - With renal disease, mother may have high protein and glucose in urine
Mother might have diabetes which increases urine glucose
Neural Tube Defect Testing
Neural tube defects: abnormalities in the brain, spine, or spinal cord (e.g., Spina bifida, Anencephaly).
Alpha Fetoprotein (AFP): secreted in fetal serum; found in amniotic fluid; high levels indicate neural tube defects, fetal abnormalities, or distress.
Acetylcholinesterase (AChE): enzyme in CNS, RBCs, skeletal muscle; confirms positive AFP; high levels suggest neural tube defects.
Spina bifida: incomplete closure of spinal column; leads to nerve damage and paralysis.
Anencephaly: underdeveloped brain and skull; results in stillbirth or death shortly after birth
Lung Maturity Testing
Pulmonary system is one of the last organs to mature in the fetus.
Respiratory Distress Syndrome (RDS): most common cause of death in newborns.
Lamellar bodies release surfactants that prevent lung alveoli from collapsing.
RDS occurs due to insufficient surfactant production in newborn's lungs.
FLM tests are of no value before 32 weeks; indicate immaturity at that stage.
Surfactants reduce surface tension to prevent alveolar collapse and lower pressure needed for reopening during inspiration.
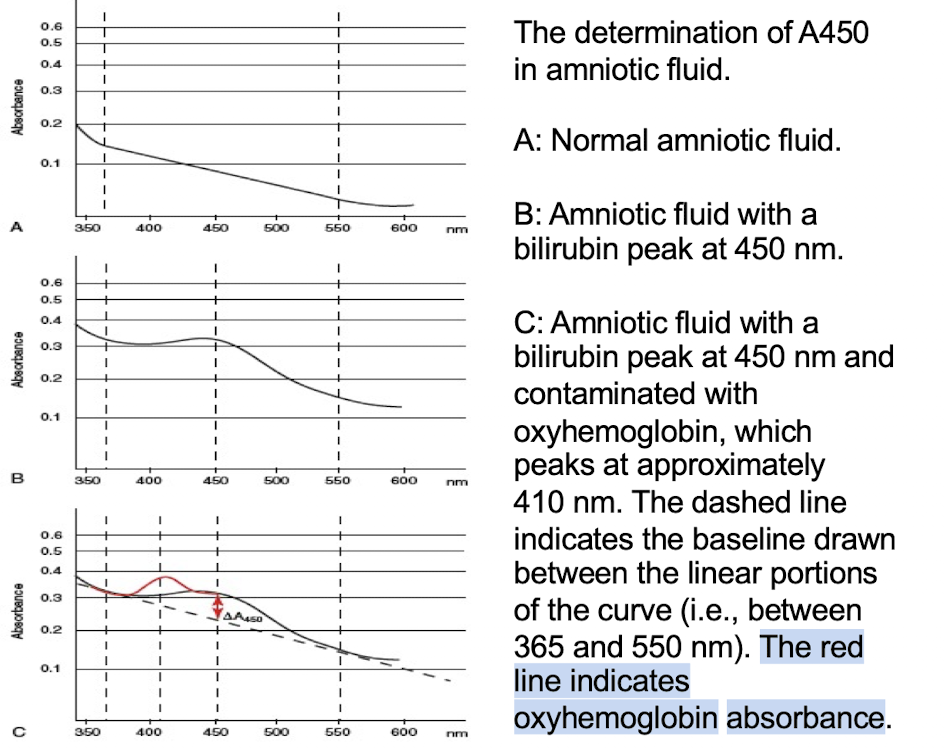
Bilirubin Testing
Blood in specimen is unacceptable (oxyhemoglobin absorbs at 410-540 nm).
Specimens are rejected if hemolyzed, but icteric color is expected.
Meconium contamination is not acceptable.
Specimens must be shielded from light after collection due to bilirubin's light sensitivity.
Icteric refers to the yellowish sample color from high bilirubin levels.
Amniotic Fluid Bilirubin: Queenan vs Liley Chart
Queenan Chart: Preferred for assessing amniotic fluid bilirubin, especially in Rh incompatibility.
Specifically designed for gestational ages <27 weeks.
Liley Chart: Less reliable <27 weeks due to insufficient data.
fetus more in danger due to hemolysis of RBCs as zones get higher in number
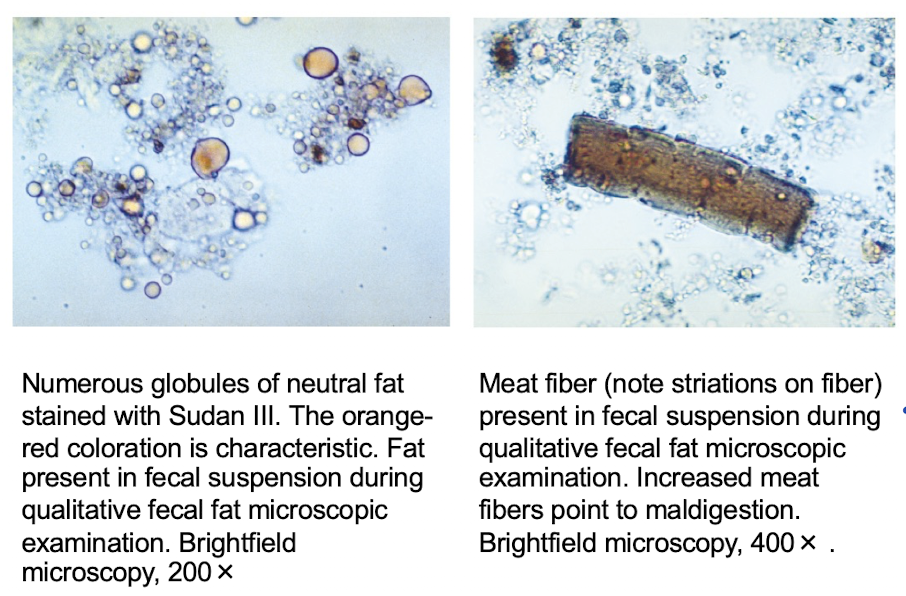
Fecal Fat Test Summary
Two-slide qualitative test for fecal fat using Sudan III, IV, or oil red O.
Slide 1: Detects neutral fats (triglycerides)
Slide 2: Acidified with acetic acid and heated to estimate total fecal fat
Fecal Fat: 2 slide test interpretation
Maldigestion: Increased neutral fats on 1st slide
Meat fibers present
Malabsorption: Normal amount of fat on 1st slide with increased total fat on the 2nd slide
characteristic, orange red color
secretory and osmotic diarrhea definition
Secretory
Enterotoxin-producing organisms
Damage to mucosa due to drugs or disease
Osmotic
Maldigestion
Malabsorption
Secretory VERSUS Osmotic Diarrhea
IF DIFFERENCE IS >20 mOsm/kg = OSMOTIC, <20 mOsm/kg = SECRETORY
Both have osmotically active solutes, but source differs
To differentiate, measure fecal osmolality, sodium (Na) and potassium (K)
Calculate fecal osmolality from Na and K, and compare w/ actual osmolality
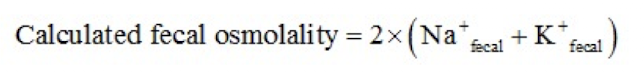
Secretory Versus Osmotic Example:
Fecal Na = 6
Fecal K = 5
Measured fecal osmolality = 10
Is this diarrhea secretory or osmotic?
Calculated Fecal Osmolality = 2 x [ Na(+) + K(+) ]
Osmotic: difference > 20 mOsm/kg
2x(6+5)=22
22-10=12 = Secretory (<20)
Fecal Carbohydrate Testing
Undigested carbohydrates (e.g., lactose) lead to bloating, flatulence, and diarrhea due to fermentation.
Stool becomes acidic: pH 5 to 6 (normal feces pH > 7).
Clinitest tablets use copper reduction to detect reducing sugars (sucrose not detected).
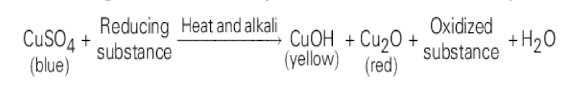
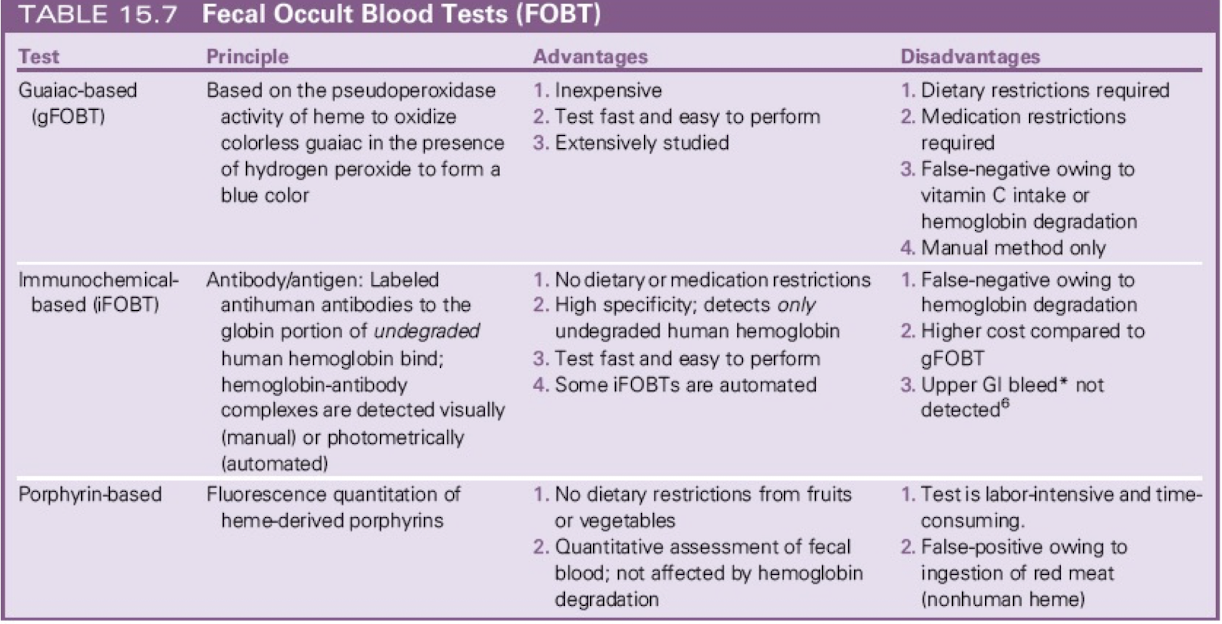
Which fecal fat test are occult blood tests?
1.Guaiac-Based (gFOBT) - more common
restrictions are required due to pseudoperoxidase or peroxidase activity of various foods and medication
Result: Oxidized indicator (colored) + H2O
2.Immunochemical based (iFOBT)
3.Porphrin-based:
Key Points about Sperm Motility
Immotile sperm cannot reach or fertilize an egg.
Evaluated either subjectively or using automated methods.
One drop of semen is analyzed under 40x with a coverslip.
At least 6 seen
At least 50% of sperm should show moderate to strong forward progression.
Temperature affects motility; testing is ideally at 37°C or room temp
Sperm Vitality
eosin-nigrosin (Blom’s) stain, brightfield, 40x
White sperm were alive (membrane intact)
pink-stained sperm were dead (membrane damaged and permeable).
Sperm Count
Semen is diluted with something that will
immobilize the sperm
Sperm is counted manually using a hemacytometer
Vasectomy = vas deferens is cut surgically
Post-vasectomy sperm counts should be at least
12 weeks after procedure; any remaining sperm
should be nonmotile
Post Vasectomy Sperm Collection
At least 2 samples needed for fertility assessment over 3-month period.
Abstinence of 2 to 7 days before each sample collection.
Entire ejaculate must be collected in a clean, sterile container.
Lab-provided container to prevent soap interference with test results.
Samples should be delivered to the lab within 1 hour, maintained between 20 °C and 40 °C.
Keep collection container warm by holding it close to the body.
Time of specimen collection is crucial for evaluating liquefaction.
Sperm Count formula
Sperm Concentration (sperm/mL) x Volume of ejaculate (mL)
Cause of Sperm Agglutination and Signficance
Causes reduced fertility & caused by IgG and IgA
associated with the presence of sperm-agglutinating antibodies.
Vaginal fluid analysis - what are the 3 chemicals for risk of premature delivery?
Fetal fibronectin (fFN)
PAMG-1
IGFBP-1
Vaginal fluid analysis Summary
Fetal fibronectin (fFN)
glycoprotein linking the placenta to the uterine wall, released during labor and detectable in cervicovaginal secretions
high levels indicate a higher risk of premature delivery.
PAMG-1 & IGFBP-1
Proteins in high concentrations in amniotic fluid
presence in cervicovaginal secretions indicates premature rupture of membranes and increased risk of premature delivery.
Sweat analysis - how Chloride sweat test works
Pilocarpine stimulates sweat glands.
Sweat collected on a gauze pad.
Sweat leached into a known volume of distilled water.
Chloridometer measures chloride concentration.
Positive test if chloride >60 mmol/L.
Confirmatory tests should be repeated on another date.
Repeat sweat test + genetic test confirm diagnosis.
Cystic Fibrosis
Autosomal recessive disease caused by mutations in the CFTR gene
Causes viscous mucous secretions, leading to pneumonia
Diagnosed with sweat chloride test
chloride stays outside = higher conc. = measured for sweat
Cerebrospinal Fluid (CSF) Reference Range + Interpretation
Greater than normal: Indicates increased intrathecal IgG production (e.g., MS, inflammatory conditions)
Less than normal: Suggests compromised blood-brain barrier
Synovial Fluid Reference Range + Interpretation
Fetal maturity (Foam Stability Index):
FSI ≥ 0.47 indicates fetal lung maturity.
Crystals
Monosodium Urate (MSU) – Gout
Parallel: Yellow
Perpendicular: Blue
Negative birefringence
Calcium Pyrophosphate Dihydrate (CPPD) – Pseudogout
Parallel: Blue
Perpendicular: Yellow
Positive birefringence
Amniotic Fluid Reference Range + Interpretation
Lamellar Body Count:
> 50,000 /µL = fetal lung maturity
Normal range during 3rd trimester: 50,000 – 200,000 /µL
L/S Ratio (Lecithin/Sphingomyelin Ratio):
≥ 2.0 suggests lung maturity
< 1.5 suggests immaturity
(standard reference knowledge)
Phosphatidylglycerol (PG):
Presence after 35 weeks gestation = lung maturity
Chylous & Pseudochylous Effusions Reference Ranges + Interpretations
Chylous:
Triglycerides > 110 mg/dL
Cholesterol < 200 mg/dL
Microscopic: Lymphocytes
Pseudochylous:
Triglycerides < 110 mg/dL
Cholesterol > 200 mg/dL
Microscopic: Lipid-laden macrophages, cholesterol crystals, cell variety
Fecal Testing Reference Ranges + Interpretations
Osmotic vs. Secretory Diarrhea:
Fecal osmolality difference > 20 mOsm/kg = Osmotic diarrhea
< 20 mOsm/kg = Secretory diarrhea
Fecal pH:
Normal: >7
Acidic: pH 5–6 → suggests carbohydrate fermentation
Quantitative Fecal Fat:
≥ 6g fat/day = Steatorrhea