PACC Skin, Hair, Nails Abnormalities
1/211
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
212 Terms
acne vulgaris
Acneiform Disorders:
Overview:
- Multifactorial cause - mostly androgens and excess sebum production (hypersensitivity of the sebaceous glands)
- Bacterium: C acnes
- Inflammation
- Higher prevalence in adolescents
Adolescent: male predominance
Postadolescent: women predominance
acne vulgaris
Acneiform Disorders:
Subjective:
- Psychological impact
- Redness of face, blackheads and white heads, raised pimples, painful cystic pimples and scar formation
- Attribute breakouts to stress, hormones, certain foods
- Go through family history!
acne vulgaris
Acneiform Disorders:
Objective:
Typical distribution of body with large, hormonally responsive sebaceous glands, including face, neck, chest, upper back, upper arms
closed comedones
Acneiform Disorders:
noninflammatory, <5 mm, dome-shaped, smooth, skin-colored, whitish, or grayish papules

open comedones
Acneiform Disorders:
noninflammatory, <5 mm papules with central, dilated, follicular orifice containing gray, brown, or black, keratotic material

papulopustular acne
Acneiform Disorders:
inflamed, relatively superficial papules and pustules, typically <5 mm in diameter

nodular acne
Acneiform Disorders:
deep-seated, inflamed, often tender, large papules or nodules, “cystic acne”

postinflammatory hyperpigmentation
Acneiform Disorders:
development of hyperpigmentation at site of active/resolving lesion (anytime there’s a break in the dermis and blood touches it)

scarring
Acneiform Disorders:
more often result of inflammatory acne than noninflammatory

rosacea
Acneiform Disorders:
Overview:
- Common with unknown etiology
- Possible genetic predisposition
- Adults between 30-50 years of age
- More females than males
- More commonly diagnosed in individuals with fair skin

rosacea
Acneiform Disorders:
Subjective:
Facial flushing precipitated by triggers
Clinical signs:
- Erythema, telangiectasia, coarseness/grittiness of skin, inflammatory papulopustular eruption resembling acne
- Intermittent symptoms at first but can lead to permanence

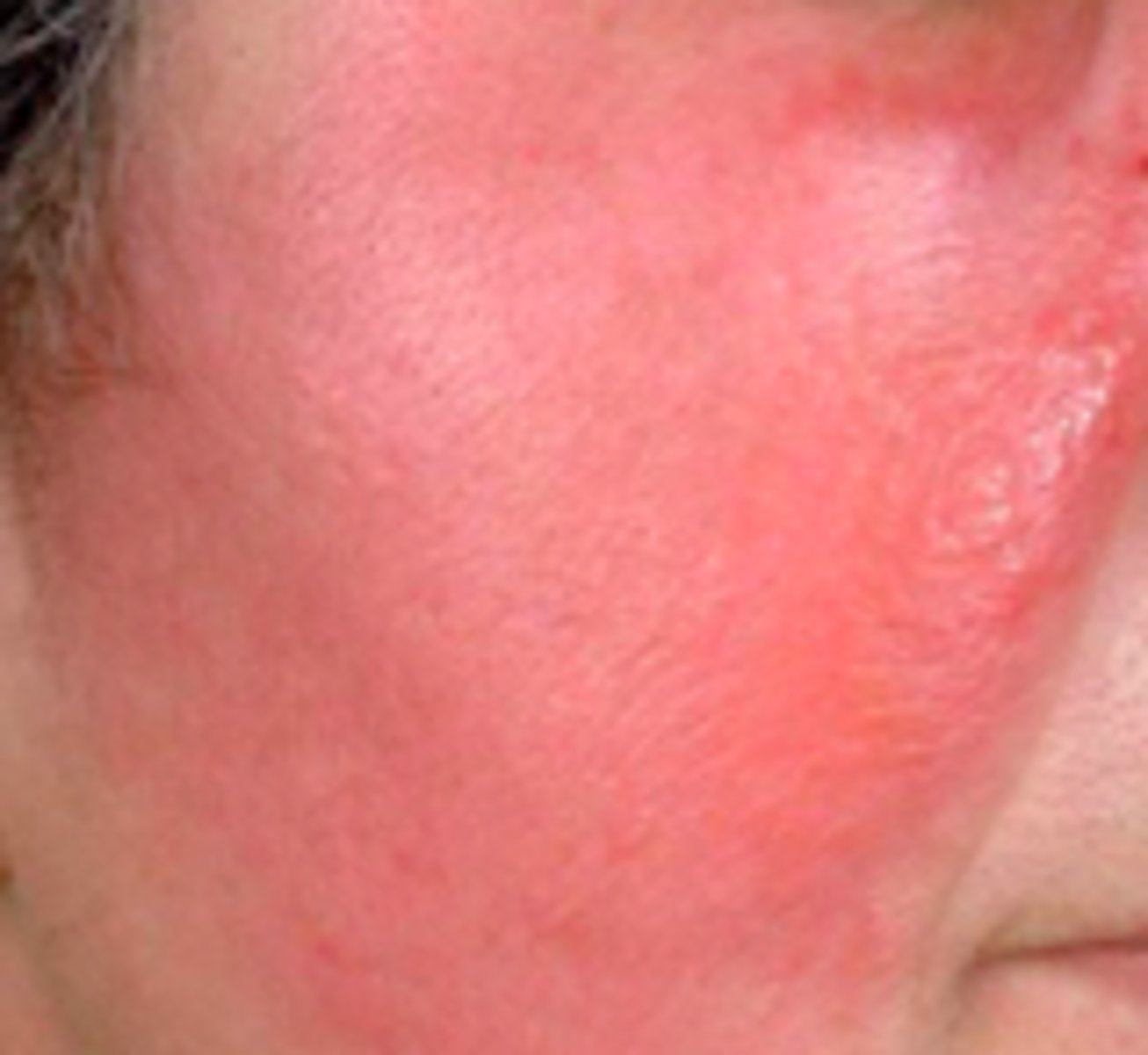
rosacea
Acneiform Disorders:
Objective:
- Variable erythema and telangiectasia
- Inflammatory papules and pustules
- Observed over the nose, forehead, and cheeks
- Prominence of sebaceous glands (thickened and disfigured noses - rhinophyma)
- Less report of greasiness; experience drying in peeling
- Absence of comedones
- Not usually scarring
sebaceous hyperplasia
Acneiform Disorders:
Overview:
- Common, benign condition of sebaceous glands
- Occurs in adults (middle-aged males)
- Can be bothersome but rarely require treatment
- Main concern: clinical dresemblance with other neoplastic lesions
- Decreasing levels of androgens lead to decrease in sebocyte turnover, which activates feedback of stimulation of sebocyte proliferation within the glands and sebaceous hyperplasia

sebaceous hyperplasia
Acneiform Disorders:
Subjective:
- Cosmetic
- pt wonder: Possible malignancy?
- Lesions are:
Asymptomatic, soft, discrete, and yellow; surface that can be smooth or slightly verrucous
1 or multiple lesions at various locations on face
Become red/irritated/bleed after scratching, shaving, other trauma
sebaceous hyperplasia
Acneiform Disorders:
Objective:
- Incidentally found
- Whitish-yellow or skin-colored papules that are soft and vary in size 2-9 mm
- Papules have central umbilication; sometimes small globule of sebum can be expressed
- Associated with characteristics similar to basal cell carcinoma, such as telangiectasis
- May be found singularly, grouped, diffuse, or extensive
- Dermoscopy by be a useful noninvasive tool to aid in diagnosis and distinguishing between basal cell carcinoma and sebaceous hyperplasia
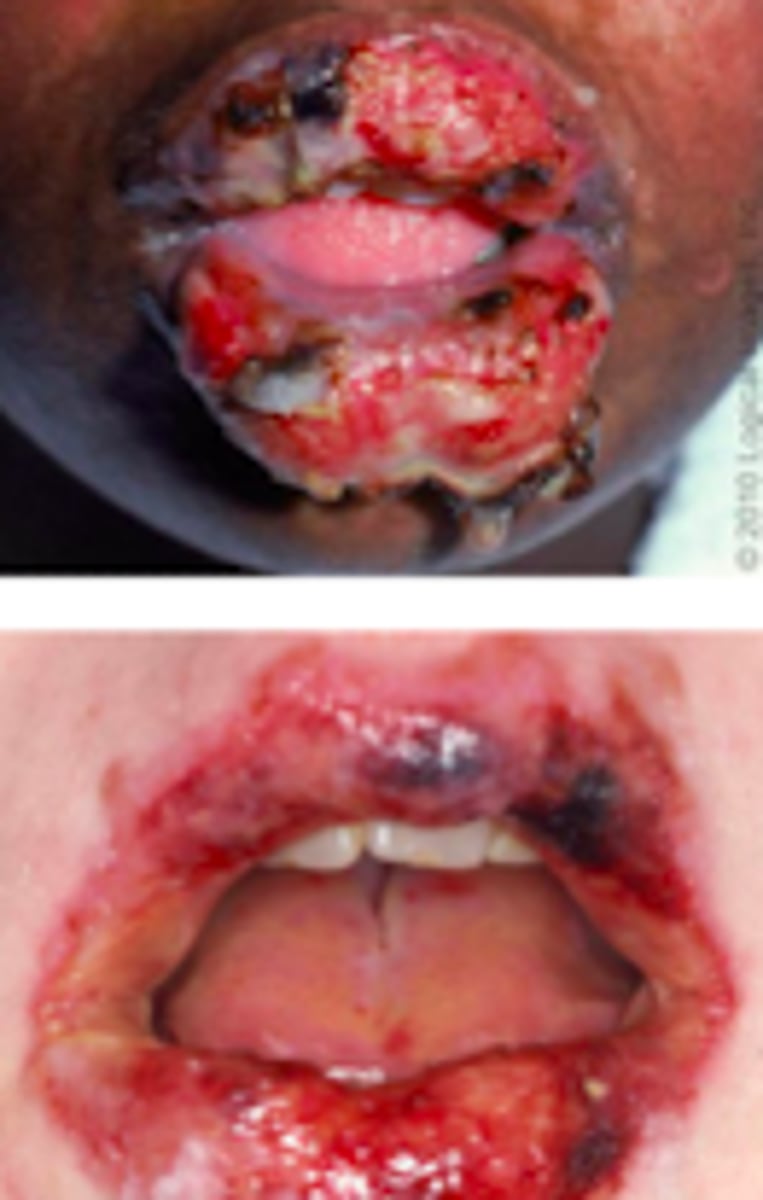
Stevens-Johnson Syndrome
Desquamation Disorders:
Overview:
- Severe, mucocutaneous reactions
- Extensive necrosis and detachment of epidermis
- Most commonly triggered by medications (usually antibiotics)
- Mucous membranes affected in over 90% of patients (usually at 2+ distinct sites)
- Skin detachment is <10% of TBSA (total body surface area)
- Initially presents with severely chapped lips and sore throat sometimes, as well as signs of conjunctivitis

Stevens-Johnson Syndrome
Desquamation Disorders:
Subjective:
- Prodrome precedes lesions by 1-3 days
- High fever
- Photophobia, conjunctival itching or burning, pain on swallowing
- Malaise, myalgia, arthralgia
- Some patients: exanthematous eruption could be heralding sign of this

Stevens-Johnson Syndrome
Desquamation Disorders:
Objective:
General:
- Fever >100.4
- Mucositis
- Skin tenderness, Skin lesions and blistering
Pt will show:
- cutaneous lesions (ill-defined, erythematous macules with purpuric centers, start on face and thorax before spreading, symmetrically distributed, scalp, palms, and sores typically spared, skin will eventually slough)
- + Nikolsky sign
- + Asboe Hansen Sign (bulla spread sign)
- mucosal and oral lesions (painful, hemorrhagic erosions covered with grayish-white membrane)
- ocular (severe conjunctivitis with purulent discharge, corneal ulceration, pain & photophobia)
- urogenital lesions (may lead to urinary retention)
- pharyngeal mucosa (trachea, bronchial, esophagus membranes)
Toxic Epidermal Necrolysis
Desquamation Disorders:
Overview:
- Severe mucocutaneous reaction
- Most commonly triggered by meds
- Extensive necrosis and detachment of epidermis
- Mucous membranes affected in >90% pt, usually at 2+ distinct sites (ocular, oral, genital)

rubella
Exanthems:
Overview:
- Vaccine-preventable viral illness
- Self-limiting illness in children, but can have devastating effects on fetus when acquired during pregnancy
- “German measles”
- Acquired via close & prolonged contact with infected individuals via inhalation of infectious large particle aerosols
14-18 day incubation period

rubella
Exanthems:
Subjective:
- Low grade fever
Acute onset of rash:
- Pruritic
- First appears on face then —> trunk and extremities
- Spares palms and soles
- Lasts ~ 3 days
Eye redness

rubella
Exanthems:
Objective:
- Fever
- Generalized maculopapular rash
- Lymphadenopathy
- Usually posterior cervical, posterior auricular, and suboccipital lymph nodes
- 5-8 days
- Mild, nonexudative conjunctivitis
- Small red spots on soft palate (Forchheimer spots)
roseola
Exanthems:
Overview:
- Caused by bB variant of human herpesvirus 6 (HHV-6)
90% in children <2 years
- Peak incidence is in spring and seasons
- No known exposure and most occurs sporadically

roseola
Exanthems:
Subjective:
- 3-5 days of fever and irritability
- Rash following fever
Most children are otherwise well-appearing, active, and alert.

roseola
Exanthems:
Objective:
Blanching macular or maculopapular rash
Starts on neck and trunk → face and extremities
Sometimes vesicular rash
Nonpruritic
Persists 1-2 days
Lymphadenopathy is common

rheumatic fever
Exanthems:
Overview:
Immune response to group A streptococcus pharyngitis
- ~2-4 weeks after initial infection
- Most commonly in 5-15 years old
- Important to ask about childhood diseases - kids get this and can lead → complications later
- Damage to cardiac valves may be chronic and progressive

rheumatic fever
Exanthems:
The following are criteria needed to Dx what:
Modified Jones Criteria:
5 major manifestations:
1. Arthritis
2. Caritis and valvulitis
3. CNS involvement
4. Subcutaneous nodules
5. Erythema marginatum (easily mistaken for regular urticaria/hives)
4 minor manifestations:
1. Arthralgia
2. Fever
3. Elevated acute phase reactants, C-reactive protein
4. Prolonged PR interval on electrocardiogram
Pt needs at least 2 major criteria to be diagnosed, or 1 major and 2 minor criteria
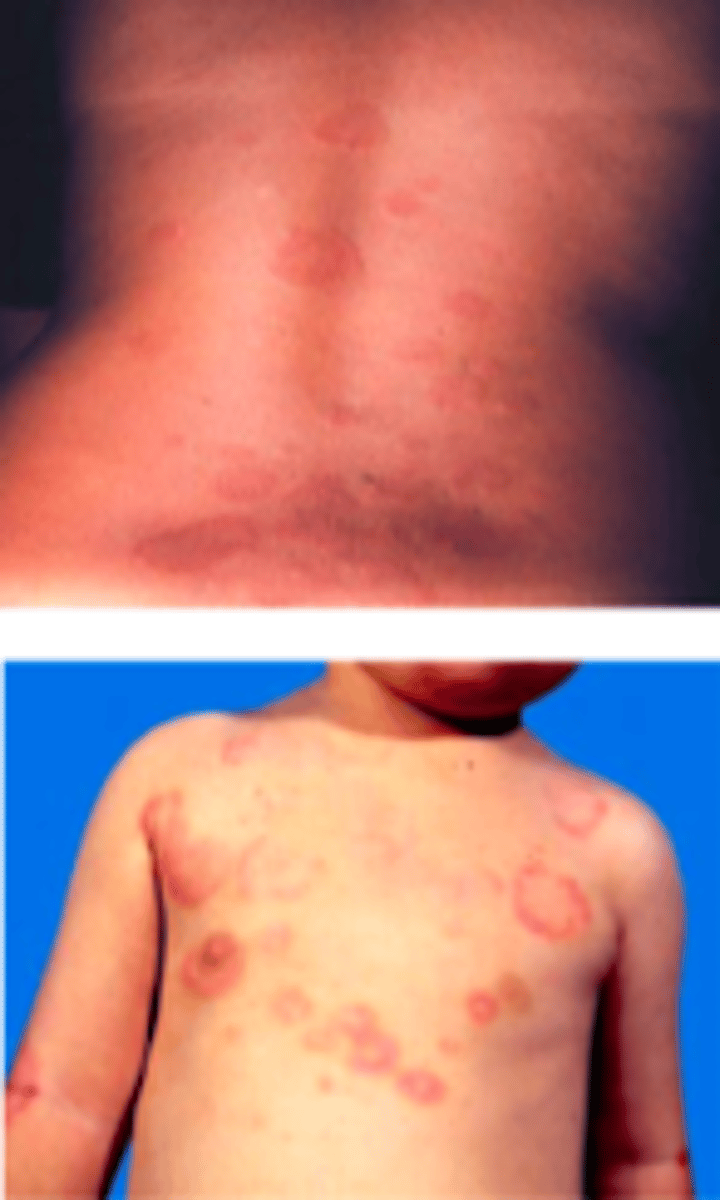
erythema infectiosum
Exanthems:
Overview:
“5th disease”
- Due to human parvovirus (PV) B19
- Classic slapped-cheek appearance and lazy exanthem
Incubation: 4-14 days
- Spread by respiratory droplets, blood products, or mother → fetus

erythema infectiosum
Exanthems:
Subjective:
Prodrome:
- Headache, fever, sore throat, pruritus, coryza (runny nose), abdominal pain, arthralgias
- Symptom free for 7-10 days, then followed by typical exanthem
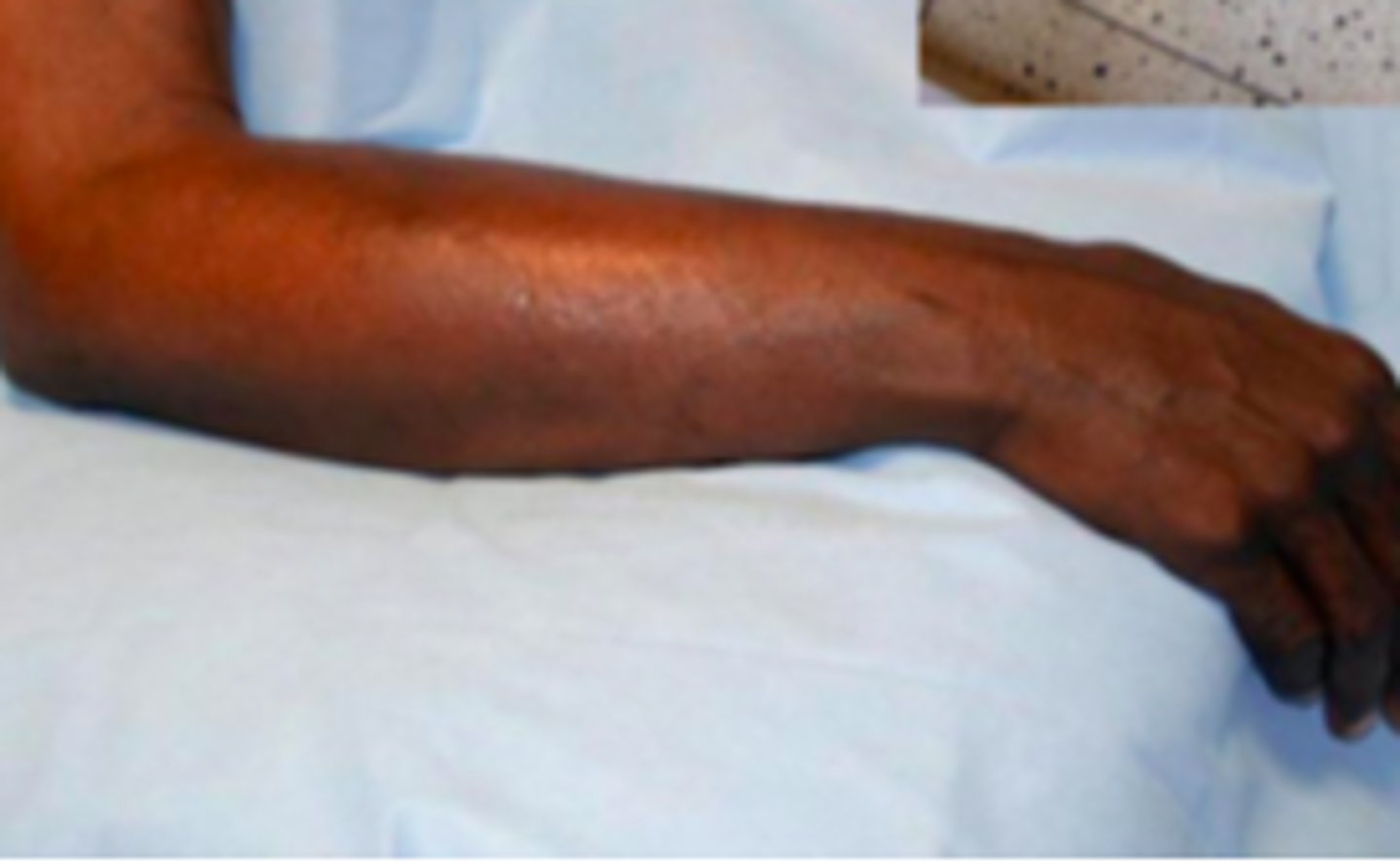
erythema infectiosum
Exanthems:
Objective:
Classic slapped-cheek appearance
- Bright red, raised erythema appears abruptly over cheeks; marked by nasal, perioral, periorbital sparing
- Appears like a sunburn, edematous sometimes; fades after 2-4 days
Next phase is 1-4 days later and is characterized by an erythematous maculopapular rash on proximal extremities (usually arms/extensor surfaces) and trunk, which fades into classic lacelike reticular pattern
Palms and soles usually spared

hand-foot-mouth disease
Exanthems:
Overview:
- Viral illness
- Presents as oral enanthem and macular, maculopapular, or vesicular rash of hands and feet (including palms & soles)
- Caused by coxsackievirus
- Transmitted person→person or fecal–oral route
- Incubation period: 3-5 days (sometimes 2 days, sometimes 7)

HFM disease
Exanthems:
Subjective:
- mouth/throat pain (verbal children)
- Refusal to eat (nonverbal children)
- Low fever
Absent prodromal symptoms! BUT
- If they are there, they have fever, fussiness, abdominal pain, emesis, diarrhea

HFM disease
Exanthems:
Objective:
- Oral lesions most commonly on tongue and buccal mucosa
- Less commonly in gingivolabial groove and on the soft and hard palates; Occasionally on uvula, lips, and tonsils
- Oral enanthem begins as erythematous macules, which process to vesicles surrounded by thin halo of erythema
- Usually small
- Vesicles quickly rupture and form superficial ulcers with grayish-yellow base and erythematous rim
- Macular, maculopapular, and/or vesicular
- Nonpruritic; May be painful
- Involves arms, hands/palms, feet/soles, legs, buttocks
- Occur more frequently in infants and young children than in older children and adults
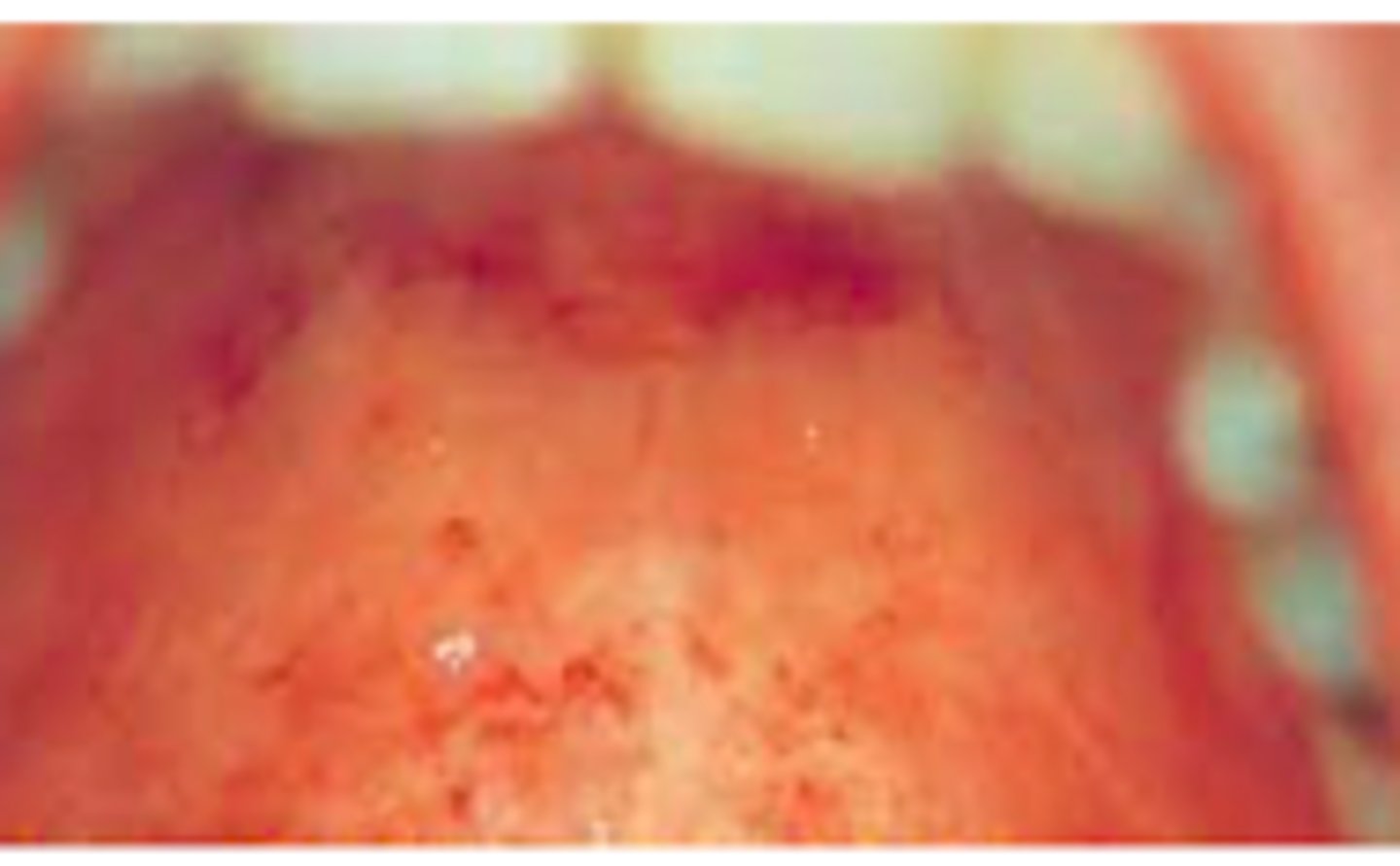
measles
Exanthems:
Overview:
- Highly contagious viral illness (up to 90% get this after exposure)
- Characterized by fever, malaise, cough, coryza, conjunctivitis, followed by exanthem
- Transmitted in public spaces, even in the absence of person-to-person contact
measles
Exanthems:
Subjective:
- Prodrome for 2-4 days
- Fever, malaise, anorexia, conjunctivitis, coryza, cough
- Varying severity of conjunctivitis; may also be accompanied by lacrimation or photophobia

measles
Exanthems:
Objective:
Koplik spots - small whitish, grayish, bluish elevations with erythematous base
- Typically seen more on buccal mucosa opposite the molar teeth
- Described as “grains of salt on a red background”
- Last 12-72 hours
- Slough when exanthem appears
Rash:
- Erythematous, maculopapular, blanching
- May include petechiae later that will not blanch
- Cranial → caudal progression
- Usually spares palms/soles
- Lymphadenopathy, high fever, pharyngitis, nonpurulent conjunctivitis

syphilis
Bacterial ID:
Overview:
- Caused by bacterium Treponema pallidum (spirochete)
- Most new cases are sexually acquired
Clinical manifestations depend upon stage of the disease: primary, secondary, tertiary
primary syphilis
Bacterial ID:
Subjective:
- Chancre (painless, heals spontaneously within 3-6 weeks)
- 21ish day incubation period prior to appearance of chancre

primary syphilis
Bacterial ID:
Objective:
- Begins as a painless papule
- Ulcerates to produce an ulcer
- Mild-moderate regional lymphadenopathy, usually bilateral
- Usually occur at genitalia but can develop at other sites (posterior pharynx, anus, vagina)

secondary syphilis
Bacterial ID:
Subjective:
- Weeks-months after chancre develops if untreated
- Not ALWAYS have history of preceding chancre due to asymptomatic/unnoticed primary infection
- Acute manifestations typically resolve spontaneously
Constitutional symptoms:
- Fever, headache, malaise, anorexia, sore throat, myalgias, weight loss
Rash:
Widespread rash that is occasionally pruritic

secondary syphilis
Bacterial ID:
Objective:
- Adenopathy
- Epitrochlear nodes (antecubital space) is particularly suggestive (minimally ender, firm, rubbery consistency)
- Diffuse, symmetric macular or papular eruption
- Entire trunk and extremities including palms and soles
- Individual lesions: copper, red, reddish-brown; scaly and nodular
- Can involve mucosa

secondary syphilis
Bacterial ID:

secondary syphilis
Bacterial ID:

pilonidal disease
Bacterial ID:
Overview:
- Common; occurs at or near upper part of natal cleft (gluteal cleft)
- Mean age: 19 y/o (women), 21 y/o (men)
- Men 2-4x more affected than women

pilonidal disease
Bacterial ID:
Subjective:
Patient presentation is highly variable! Asymptomatic, can have cavity/sinus → acute infection or chronic inflammation and drainage
Acute:
Sudden onset of mild-severe pain in intergluteal region while sitting or doing activities that stretch the skin overlying the cleft
Sometimes: Intermittent swelling sometimes, plus some mucoid, purulent, and/or blood drainage, which is associated with fever/malaise
Chronic:
recurrent/persistent drainage and pain
pilonidal disease
Bacterial ID:
Identified by retracting buttock cheeks enough to visualize pores or sinuses within natal cleft valley
- Asymptomatic: 1 or more primary pores in midline and/or painless opening cephalad and slightly lateral to cleft
Diagnosed clinical based upon findings of characteristic midline pores
- Acute Exacerbation: cellulitis in natal cleft and tender, fluctuant mass in/near top of natal cleft, slightly lateral, indicating presence of abscess
- Chronic Disease: 1+ sinus openings draining mucoid, purulent, and/or blood fluid; sometimes can see a hair protruding
Secondary tracts or pits can be identified lateral to the midline in patients with complex disease
Diagnose chronic and acute patients by being diagnosed by additional findings of a tender mass and 1+ draining sinus openings

folliculitis
Bacterial ID:
Overview:
- Bacterial infection
- Commonly: S. aureus (gram +) and gram-negative bacteria
- Can occur in infants, children, or adults
Risk factors:
- Nasal carriage of S. aureus
- Hyperhidrosis
- Occlusion of hair follicles
- Shaving

folliculitis
Bacterial ID:
Subjective:
Rash or “bumps” that can be painful, pruritic, or both
Objective:
- Follicular pustules and inflamed, follicular papules
Common sites:
- Scalp, face, upper trunk, buttocks, legs, axillae (younger pt)
Pruritus is common
Tender lesions may be present

folliculitis barbae
Bacterial ID:
- Deep portions of hair follicles in bear areas of face and neck
- Due to S. aureus
Presents with tender pustules within erythematous plaques involving multiple hair follicles

hot-tub folliculitis
Bacterial ID:
- Caused by pseudomonas aeruginosa (gram -)
- Contact with water contaminated with pseudomonas - can be result of inadequate sanitation in whirlpools, hot tubs, and swilling pools
- Bathing with contaminated sponges/nylon towels, or use of contaminated rubber gloves
Pruritic, inflamed, follicular macules, papules, or pustules
~ 8-48 hours after exposure
- Primarily on trunk and buttocks in distribution of wet bathing suit or other areas exposed to contaminated water

cellulitis
Bacterial ID:
Overview:
- Manifests as skin erythema, edema, and warmth
- Results of bacterial entry via breaches in skin barrier
- Observed in middle-aged and older adults; seasonal predilection for warmer months
Most commonly:
Group A streptococcus (strep is most common bacteria causing rashes), Streptococcus pyogenes
Risk factors:
- Skin barrier disruption due to trauma
- Skin inflammation (eczema, radiation therapy, psoriasis)
- Edema, Obesity, Immunosuppression
- Skin breaks between toes
- Preexisting skin infection (tinea pedis, impetigo, varicella)

cellulitis
Bacterial ID:
Subjective:
- Skin redness, swelling, warmth
- Pain to area
If severe: fever

cellulitis
Bacterial ID:
Objective:
- Areas of skin erythema, edema, and warmth
- Petechiae and/or hemorrhage can be seen
- Superficial bullae
- Nearly always unilateral
- Lower extremities are the most common site of involvement
- Lymphangitis - red streaking
- Regional lymphadenopathy
-Edema surrounding the hair follicles may lead to dimpling in the skin
- Fever and other systemic manifestations
erysipelas
Bacterial ID:
Overview:
- Skin infection involving the dermis layer of the skin (can extend → superficial cutaneous lymphatics)
- Group A beta-hemolytic streptococci
- More common in females but occurs in all age groups (common in extremes of age)
- Distinguishing characteristic between this and cellulitis: this is very well-demarcated (clear to tell where it starts/ends)
erysipelas
Bacterial ID:
Subjective:
- Acute onset of symptoms
- Redness of the skin, burning, tenderness, and itchiness at the site
- Systemic manifestations: fever, chills, severe malaise, and headache (can precede local inflammatory signs and symptoms by a few hours)

erysipelas
Bacterial ID:
Objective:
- Bright erythematous patch of skin with a clearly demarcated raised border
- Almost always unilateral
- Can see lymphangitis and regional lymphadenopathy
- Edema surrounding hair follicles: can lead to skin dimpling

impetigo
Bacterial ID:
Overview:
- Contagious, superficial bacterial infection
- Most common in 2-5 y/o; can affect older children and adults but uncommon
Classifications:
- Primary: direct bacterial invasion of previously normal skin
- Secondary: infection @ sites of minor skin trauma such as abrasions, minor trauma, and insect bites
Warm, humid conditions
Easily spread among individuals in close contact
Risk factors: poverty, crowding, poor hygiene, and underlying scabies
impetigo
Bacterial ID:
Symptoms:
- Begins with single erythematous macule
- Rapidly evolves into a vesicle or pustule and ruptures
- Released serous contents then dry, leaving a crusted, honey-colored exudate over the erosion (so if it says honey-colored crust - this is it!)
- Rapid spread may follow
- Face and extremities are affected most commonly (but can occur anywhere)
- May be pruritic
- Clusters in families and outbreaks in institutions are sometimes occasionally reported

candidiasis
Fungal ID:
Overview:
- Opportunistic infection due to Candida (fungi)
often present in healthy persons as part of normal flora, but can invade and cause disease, which will lead to signs/symptoms that affect skin, oral cavity, GI tract, vagina, penis, or other parts of the body
- Risk factors: host defense defects, obesity, DM, hyperhidrosis, warm climate, use of glucocorticoids

candidiasis
Fungal ID:
Subjective:
“Intertrigo”
- Invades intertriginous areas and areas of occluded skin (moist, occluded sites)
- Tenderness, extreme itching, and pain
Primary locations:
- Axilla, inframammary folds, inguinal folds, other skin folds, diaper location (diaper dermatitis)

candidiasis
Fungal ID:
Objective:
- Initial pustules on an erythematous base - becomes eroded and confluent
- Then fairly sharp demarcated, polycyclic, erythematous, eroded patches with small pustular lesions at the periphery (satellite lesions)
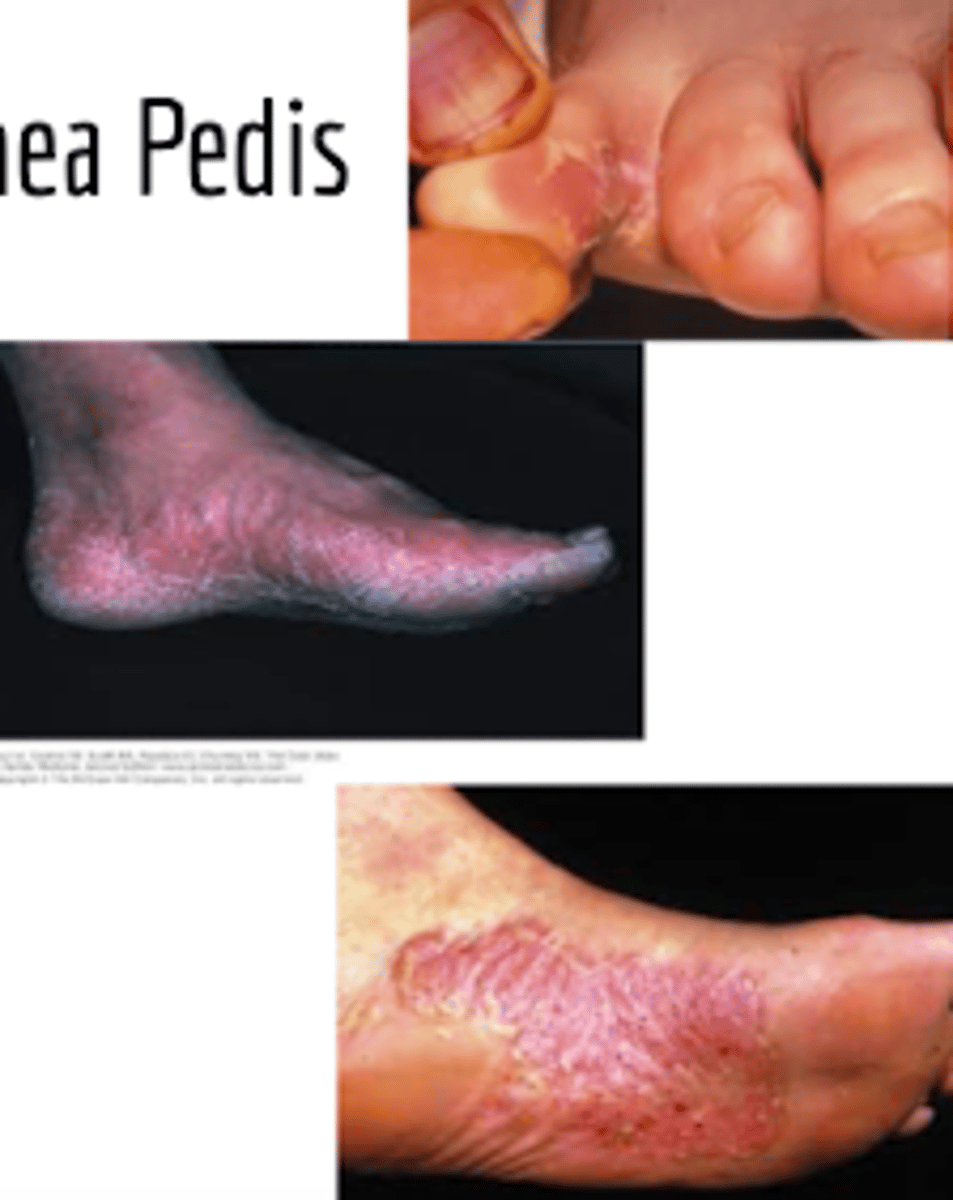
dermatophyte
Fungal ID:
Overview:
- These are the prevailing cause of fungal infections of skin, hair, and nails
Can lead to variety of clinical manifestations:
- Tinea pedis
- Tinea corporis
- Tinea cruris
- Tinea capitis or tinea barbae
- Dermatophyte onychomycosis
- Majocchi’s granuloma
Subjective:
Rash with associated scaling and itching on one of the ^^^^^ locations
- Infection usually acquired by direct contact with causative organism (can touch spot where someone infected has touched and become infected)
- Walking barefoot in locker rooms or swimming pools
- Direct skin contact with infected individual or animal
- Common among athletes sharing facilities
Objective:
Cutaneous dermatophyte infections can be strongly suspected on physical exam
Careful physical examination!!
interdigital, hyperkeratotic, vesiculobollous (inflammatory)
Fungal ID:
What are the 3 major clinical ways that tinea pedia presents?
tinea corporis
Fungal ID:
- Often begins are pruritus, circular/oval, erythematous or hyperpigmented, scaling patch or plaque that spread centrifugally
- Central clearing follows which an active, advancing, raised border remains
- “Ringworm” due to ring-shaped plaque
- Multiple plaques could coalesce and pustules occasionally appear

tinea cruris
Fungal ID:
Begins with erythematous or hyperpigmented patch on proximal medial thigh
- Infection spreads centrifugally, with partial central clearing and a slightly elevated, erythematous or hyperpigmented, sharply demarcated border
- Infection could spread → perineal areas, gluteal cleft, or onto buttocks
Scrotum often spared!

tinea capitis
Fungal ID:
Development of scaly patches with alopecia and patches of alopecia with visible black dots
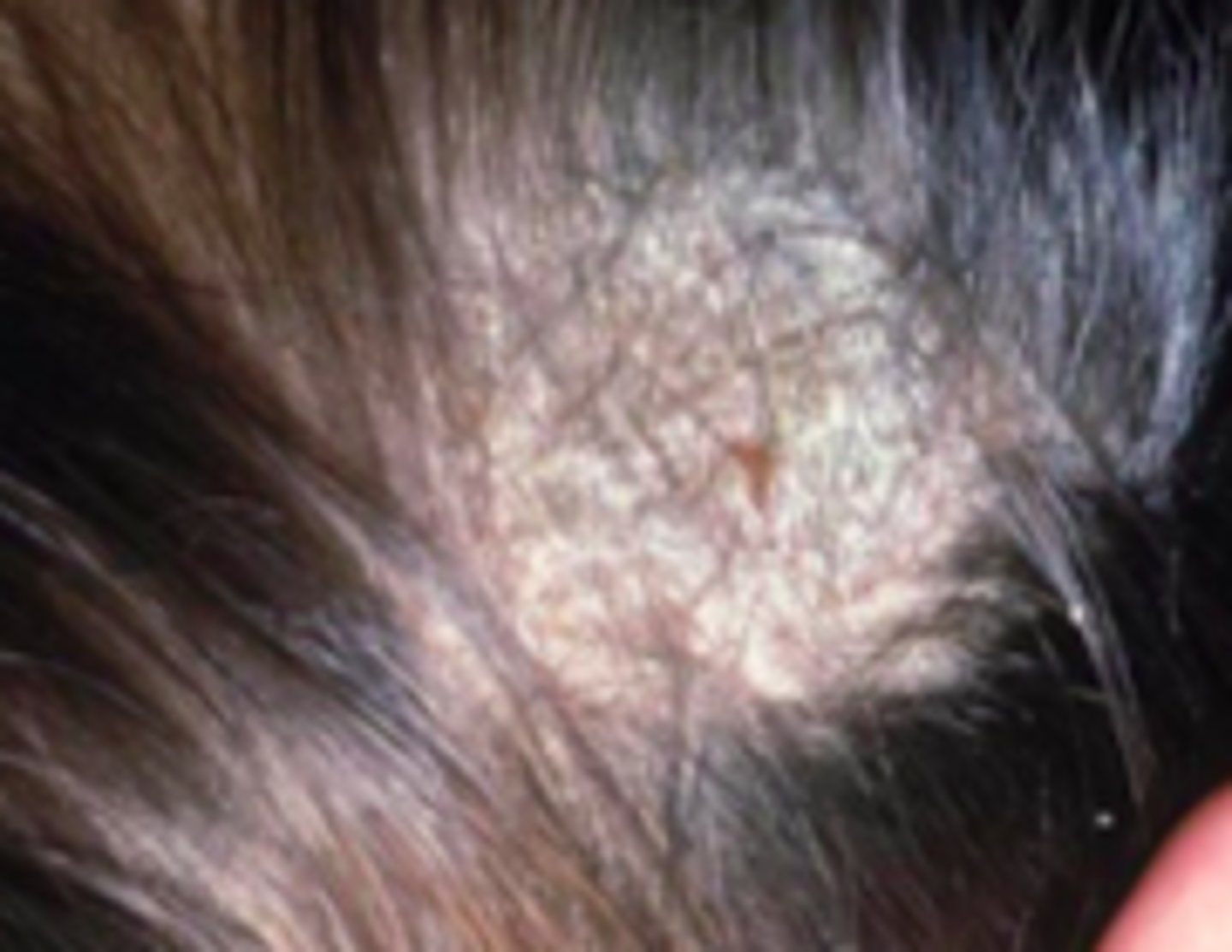
lice
Parasitic ID:
Overview:
- Pediculosis capitis
- Caused by infestation of hair and scalp by Pediculus humanus capitis (head louse)
- Children most often affected
Eggs (“nits”) = oval capsules that hatch in 8 days, releasing nymphs that require another 8 days to mature
- After hatching, egg cases become white and more visible
Adult these are equipped with mouthparts adapted to sucking blood and legs adapted to grasping hair
- Primary mode of transmission: contact with head of infested person
do not jump, fly, or use pets as vectors

lice
Parasitic ID:
Subjective:
- Pruritus of scalp and neck as an allergic reaction to live saliva injected during feeding
- Onset of itching may be delayed until sensitization occurs after 4-6 weeks
Objective:
- nits may be visible on scalp and hair shaft
- Excoriations may be visible on scalp, neck, and postauricular skin
- Secondary staph infection occurs with associated cervical and nuchal lymph node enlargement

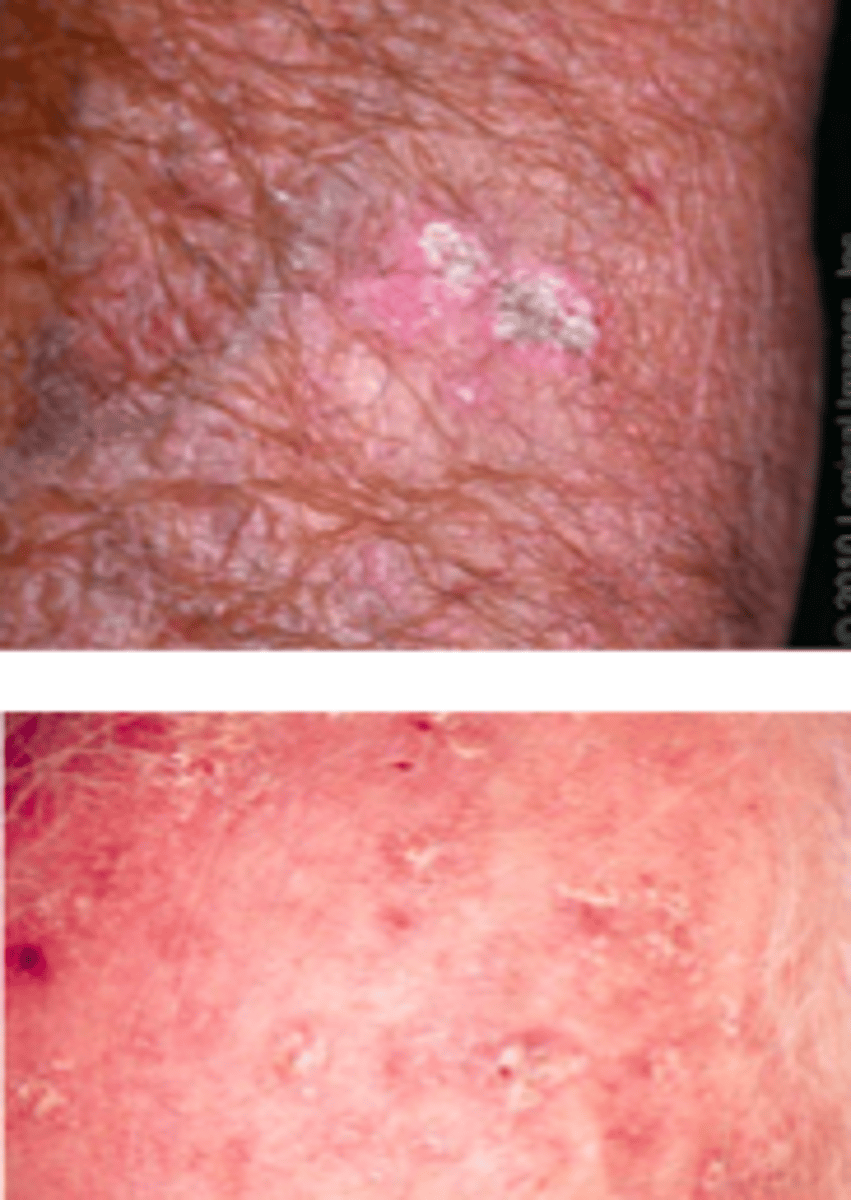
scabies
Parasitic ID:
Overview:
- Common infestation of the skin by the mite Sarcoptes scabiei
- Particularly common in resource-limited regions
- Crowded condition increase risk for scabies infestation
- Transmission usually occurs through direct and prolonged skin-to-skin contact
- May occur among family members or sexual partners; casual skin contact is unlikely to result in transmission
- Fomite (clothing , bedclothes, other objects) transmission is uncommon, but more likely to occur in the setting of crusted scabies due to a much higher parasite burden

scabies
Parasitic ID:
Subjective:
- Extreme pruritus
- Severe and worse at night
- Delayed-type hypersensitivity reaction to the mite, mite feces, and mite eggs
- Symptoms occur 3-6 weeks after primary infestation
- In previously-infested patients, symptoms usually begin within 1-3 days after infestation, presumably because of prior sensitization

scabies
Parasitic ID:
Objective:
- Small, erythematous papules, often excoriated - usually in between the fingers
- Burrows may be visible: thin, gray, red, or brown serpiginous lines
Miniature wheals, vesicles, pustules, and sometimes bullae also may be present
Distribution involves more than 1 area because it is rarely localized:

molluscum contagiosum
Viral ID:
Overview:
Poxvirus that causes a chronic, localized infection, consisting of skin-colored, dome-shaped papules on skin of infected individual
Common childhood disease
Often occurs in healthy adolescents and adults, often as sexually transmitted disease or in relation to participation in contact sports
Also associated with immunodeficiency states
Spread by direct skin-to-skin contact, and also by autoinoculation by scratching/touching lesion
Can also be spread via fomites (bath sponges, towels) or through skin contact during contact sport participation
Classified as STD when occurring in genital region in sexually active individuals
Estimates for the incubation period of the virus vary from 1 week to 6 months; typically between 2-6 weeks

molluscum contagiosum
Viral ID:
Subjective:
Skin-colored lesions (usually not red, but are usually shiny)
Pruritus can be present or absent
Generally painless unless irritated
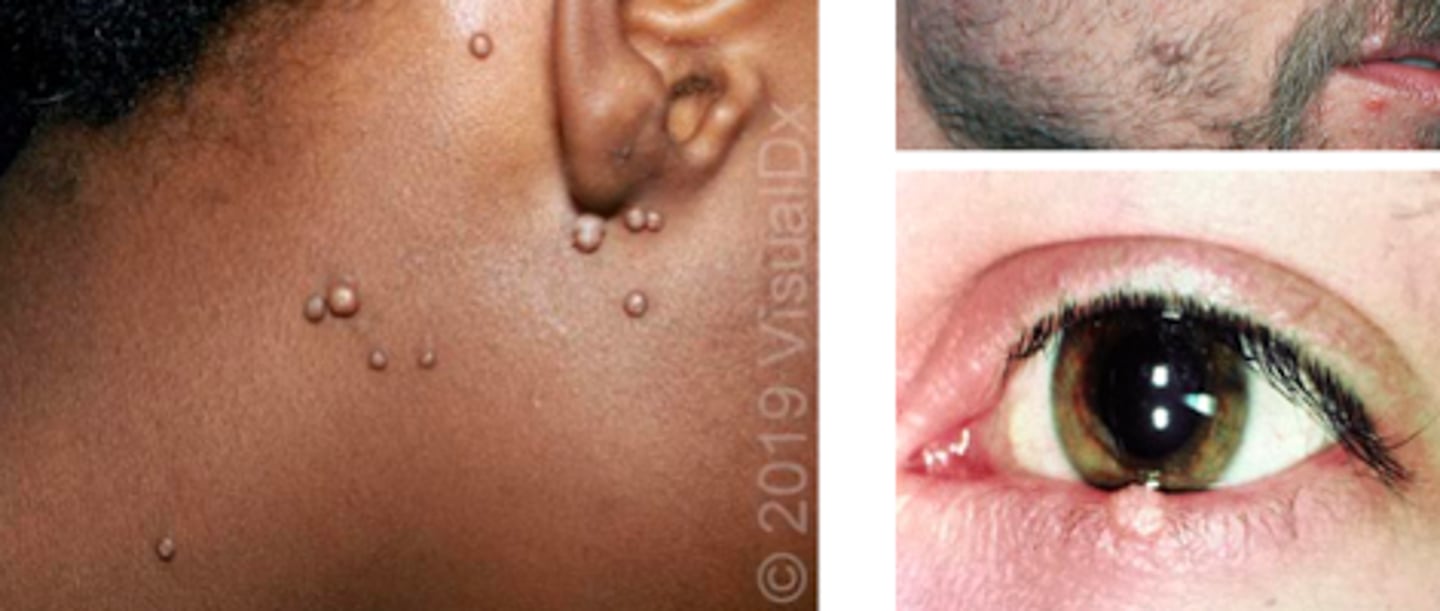
molluscum contagiosum
Viral ID:
Objective:
Lesions:
- Firm, dome-shaped papules on skin
- Shiny surface and central indentation or umbilication
- Occasionally, growths can be polypoid with stalk-like base
- Appear anywhere on body except palms and soles
- Most common areas: trunk, axillae, antecubital, popliteal fossa, crural folds
- Lesions on eyelid can cause conjunctivitis
- Oral mucosal involvement is rare
- Lesions can be large and widespread (aka giant molluscum) in immunocompromised patients

varicella zoster
Viral ID:
Overview:
1 of 8 herpes viruses known to cause human infection
- Causes 2 clinically distinct forms of disease: this (chickenpox) and herpes zoster (shingles)

varicella zoster
Viral ID:
Subjective:
- Clinical manifestations develop within 15 days after exposure
- Prodrome: fever, malaise, pharyngitis, anorexia
- Pruritic rash: develops within 24 hours of prodrome, appears in successive crops over several days

varicella zoster
Viral ID:
Objective:
Lesions:
- Begin as macules that rapidly become papules following by characteristic vesicles (“dew drops on rose petal”)
- Can then development pustular component followed by the formation of crusted papules
-Crusts tend to fall off within 1-2 weeks & leave a temporary area of hypopigmentation in the skin
- May lead to scarring
Vesicular lesions on an erythematous base!

herpes zoster
Viral ID:
Overview:
- Has latent or dormant period
If reactivation occurs:
- Can spread to ganglion to involve multiple sensory neurons
- Involved sensory ganglion exhibits intense inflammation, accompanied by hemorrhagic necrosis of nerve cells - neuropathic pain
Incidence rates progressively increase with age
herpes zoster
Viral ID:
Subjective:
- Perhaps a prodrome, but then a rash
- Acute neuritis
Objective:
- Rash starts as erythematous papules, typically in a single dermatome or several contiguous dermatomes
- Will NOT CROSS MIDLINE
- Thoracic and lumbar dermatomes are most commonly involved

herpes zoster
Viral ID:

scarring and hypo- or hyperpigmentation after herpes zoster
Viral ID:

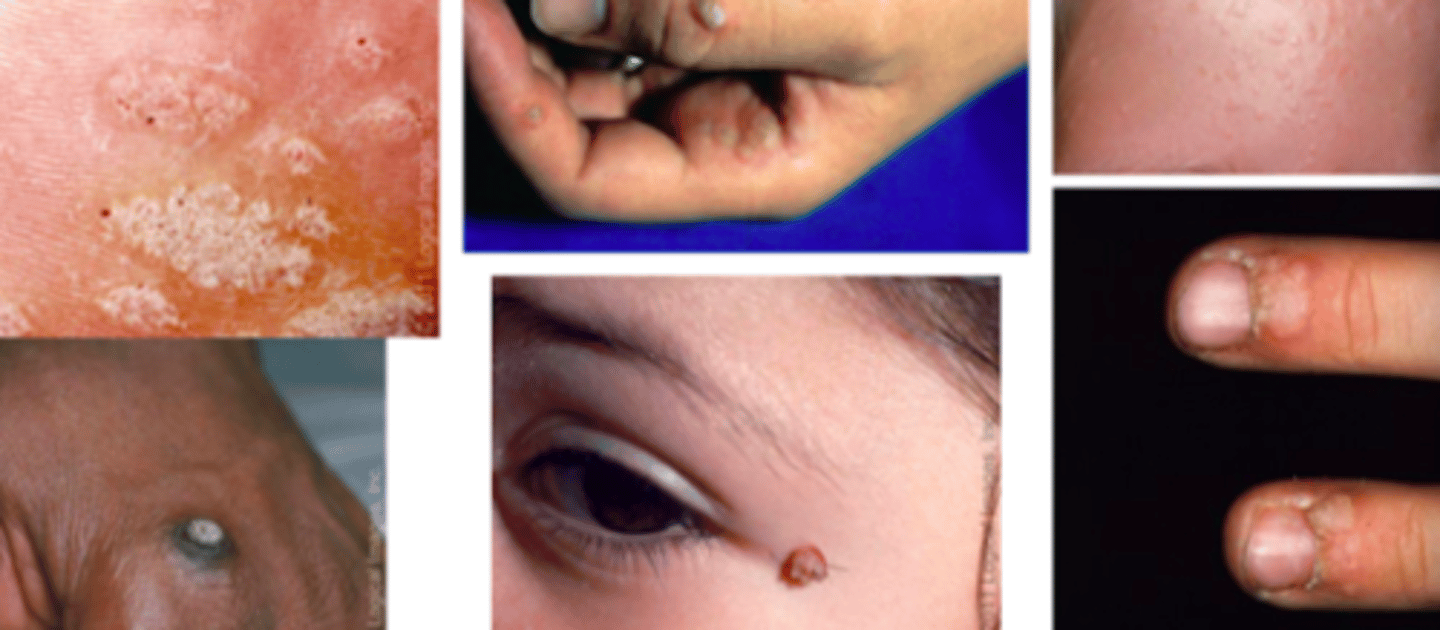
HPV (human papillomavirus)
Viral ID:
Overview:
- Infect epithelial tissues of the skin and mucous membrane
- Most common manifestation of this infection are warts (verrucae)
Type 1 - soles of feet (plantar warts)
Types 6 & 11 - anogenital area (anogenital warts)
- Infection occurs by direct skin contact
- Incubation period: 2-6 months
HPV
Viral ID:
Subjective:
- Small bump or group of bumps in various occasions
- Small or large, raised or flat
- Skin burning/itching
HPV
Viral ID:
Objective:
- Cutaneous warts may manifest as common warts (verruca vulgaris), plantar warts (verruca plantaris) and flat warts (verruca plana)
- May occur singly, in groups, or as coalescing warts forming plaques
Diagnosis based on clinical appearance:
- Flesh-colored papules may be smooth or slightly hyperkeratotic
herpes simplex
Viral ID:
Overview:
- Primarily spread by skin-to-skin contact
- Treatable but not curable
2 types: (treated similarly, just differs in location/how common they occur)
Type 1
- Mostly spreads by oral contact and causes infections in/around the mouth (cold sores)
- Can also cause genital herpes
Type 2
- Spread by sexual contact and causes genital herpes

herpes simplex
Viral ID:
Subjective:
- Many are unaware of infection, so can pass it along without knowing
- Painful, recurring vesicles or ulcers; may begin with tingling, itching, or burning near where the sores will appear
- New infections may cause fever, body aches, swollen lymph nodes
Common Type I symptoms:
- Blisters (cold sores) or open sores (ulcers) in/around mouth or lips
Common Type II symptoms:
- Papules, vesicles, or ulcers around genitals or anus
- Lesions are painful; can break open, ooze, then crust over

actinic keratosis (aka solar keratosis)
Keratotic Disorders:
Overview:
- Cutaneous lesion that results from proliferation of epidermal keratinocytes
- Present as erythematous and scaly macules/papules
Risk factors: chronic sun exposure (frequently sun-exposed areas), history of sunburn
- Most common reasons for visits to dermatologists!
This is a risk factor for the development of cutaneous squamous cell carcinoma (SCC)
actinic keratosis
Keratotic Disorders:
Subjective:
- Develop as solitary or multiple lesions on highly sun exposed areas
- more common in older/balding males that spend time in sun
- Skin adjacent to these shows signs of solar damage, such as yellow/pale color, spotty hyperpigmentation, scattered telangiectasia, xerosis
- Generally asymptomatic, but sometimes experience a local tenderness or stinging sensation
actinic keratosis
Keratotic Disorders:
Objective:
Several Clinical Variants:
Classic (Common)
- Erythematous, scaly macule, papule, plaque
- Very small
Hypertrophic
- Presence of thick, adherent scale on erythematous base
seborrheic keratosis (aka sun spots)
Keratotic Disorders:
Overview:
- Most common benign tumor in older individuals
- No specific etiological factors have been identified
Subjective:
- Usually asymptomatic, but can be an annoyance
- Can itch/rub/catch on clothing and become inflamed
- Mostly worried they could be malignant
- Sometimes a person can have many of these and not notice a dysplastic nevus or malignant melanoma that develops among the seborrheic keratoses.

seborrheic keratosis
Keratotic Disorders:
Objective:
- Initially 1 or more sharply defined, light brown, flat lesions with a velvety to finely verrucous surface
- Arise on normal skin and <1 cm
- Can become thicker with time and become deeply pigmented without light reflection
- Can be covered by greasy-appearing scale and are raised above the surface of the skin
- Round–oval, multiple lesions may be aligned in direction of skin folds (light brown, round lesion with greasy appearance)

xerosis
Keratotic Disorders:
Overview:
- medical term for dry skin that’s more severe than typical
- Common, minor, and temporary problem, but may cause discomfort
- Skin may get dry, scaly, itchy, and red

cutaneous horn
Keratotic Disorders:
Overview:
- hard, conical projection from the skin, made of compact keratin
- Arise from benign, premalignant, or malignant skin lesions
- Around ½ horns have benign base, ½ are premalignant, or malignant
cutaneous horn
Keratotic Disorders:
Subjective:
- More common in older patients, with peak incidence in those between 60-70
- More common in people with fairer skin
- Usually asymptomatic, but can be injured to cause pain/inflammation

cutaneous horn
Keratotic Disorders:
Objective:
- Diagnosed by its appearance but histological exam of the horn base is crucial to rule out malignancy
- Generally presents as straight or curved, hard, yellow-brown projection from the skin
- Usually singular but can be multiple
- Common in sun-exposed areas

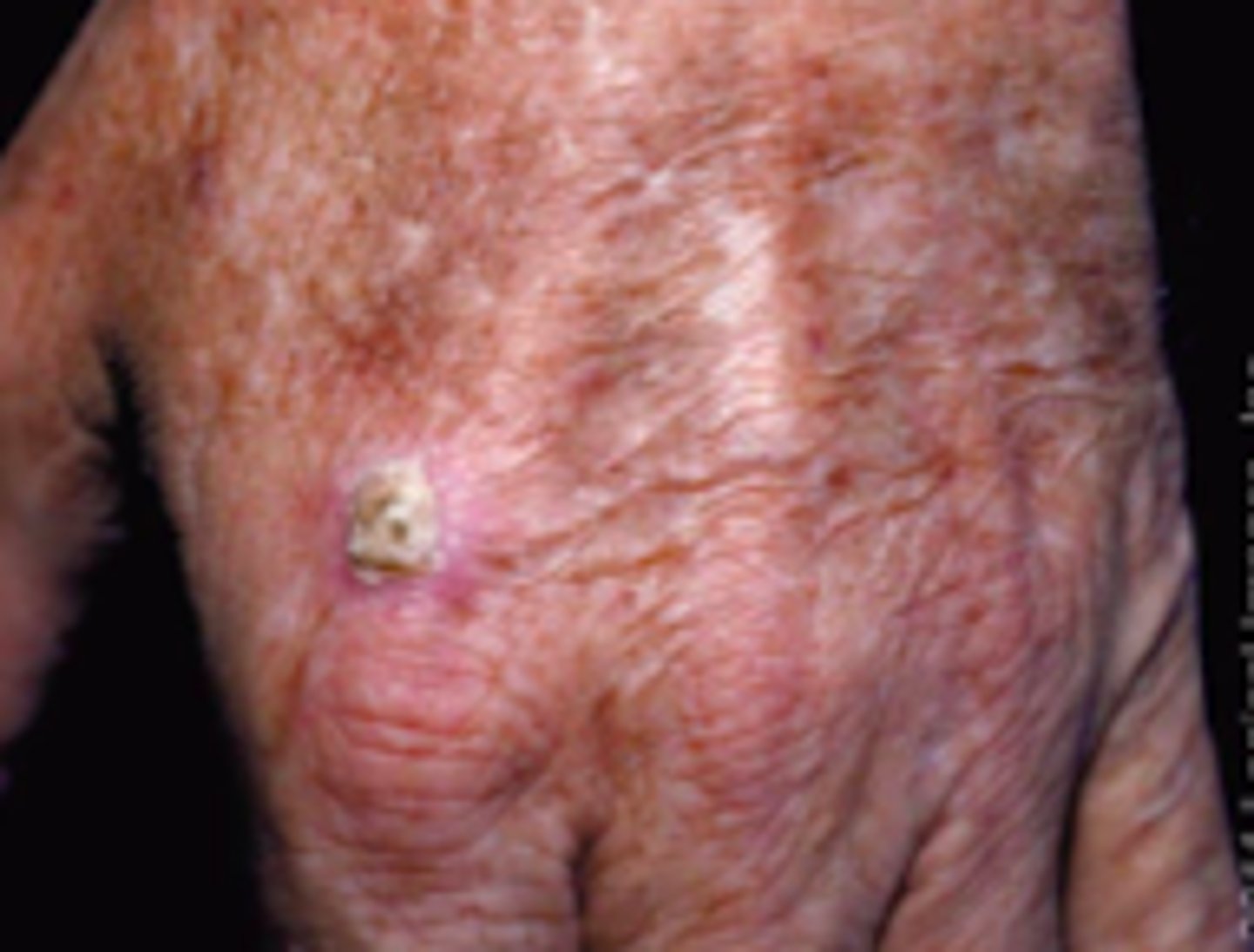
squamous cell carcinoma
Neoplasms:
Overview:
- Malignant tumor arising from epidermal keratinocytes
- In areas of photodamaged skin in lightly pigmented people
- Non-sun-exposed areas represent the most common location for this in individuals with darkly pigmented skin
- Black individuals: lower legs, anogenital region, areas of chronic inflammation or scarring
- “Bump or lump that just won’t heal”
- Can be tender to the touch or associated with open sore
- Itchy or painful
- Untreated can become invasive and metastasize
Squamous cell carcinoma
Neoplasms:
Objective:
- Presents with wide variety of cutaneous lesions:
- Papules, plaques, or nodules
- Can be smooth, hyperkeratotic, or ulcerated
2nd most common form of skin cancer
Bowen's Disease (SCC in situ)
Neoplasms:
- type of SCC
- erythematous, well-demarcated, scaly patch or plaque located in sun-exposed areas

cutaneous
Neoplasms:
type of SCC

keratoacanthoma
Neoplasms:
clinically and histologically resemble SCC; controversial whether these represent a subtype of SCC or a separate entity; lesions usually exhibit rapid growth and appear volcano-like
