Writing Rx, Making a patient record and using local formularies and national guidance to support prescribing decisions
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
11 Terms
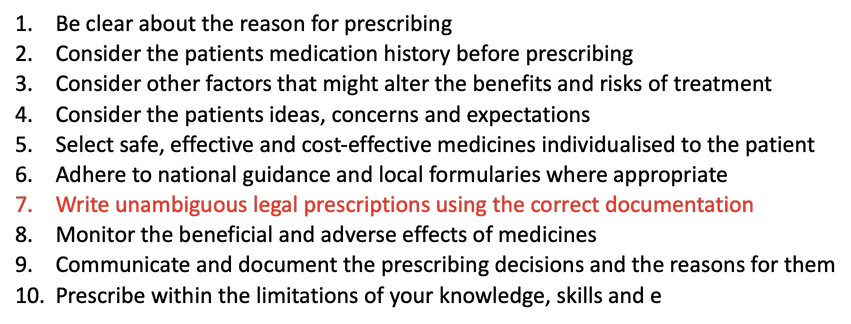
Ten Principles of good prescribing
What is Prescribing?
The professional/intellectual process of (differential) diagnosis/(shared) decision making
The technical process of making a legal/complete/accurate record of the medicine to be supplied/administered
What is needed on a Rx?
Signature of prescriber:
In INK in his/her own name
Most prescriptions now signed electronically; prescriber enters their smart card authorisation code.
Address of prescriber
Date
Valid up to 6 months (as long as not a Schedule 2,3 or 4 CD)
Particulars of prescriber – CAREFUL!!!!
Type of appropriate practitioner
Patient name
Patient address
Patient age
If under 12 years old
What is needed for a CD Rx?
Signature
In INK in his/her own name (CAN be using ‘advanced electronic signature’ for sch. 2 or 3 CDs with EPS)
Date
Valid for 28 days after the ‘appropriate date’
Address
Dose
Must be clear: NOT ‘as directed’, but ‘1 as directed’ okay…
Formulation
Must always be stated
Strength
If more than one strength
Total quantity
Words and figures…
Quantity prescribed
Should not be more than 30 days – not legal requirement
Patient name
Patient address
(Dental wording) and (Instalment wording)
What are the key points of record keeping?
Quality of record must reflect the care given
Write legibly
Include details of the patient, date and time
Avoid or be careful with abbreviations
Do not alter an entry or disguise an addition
Keep it simple and avoid abbreviations
Keep it simple and avoid unnecessary info
Remember patients can read their own notes
Write down what you said, what you did, what you were told and what you observed
Be familiar with Data Protection Act 1998
How do you ensure your notes are accurate?
It is easier to take notes throughout the consultation but might lose eye contact and rapport and non-verbal cues
Could ask permission from the patient to note down a key point
Not taking notes relies on good memory!!
Highlights the importance of summarising within the consultation and allow the patient to correct you
Key points to keep in mind when note taking
Must be able to be read and understood easily and quickly
Not too long, not too short
Have a clear plan and follow up
Don’t speculate on the future
Consider any necessary blood tests
In primary care there are section headers and templates to work from.
You have seen secondary care notes on your hospital placements.
A local formulary
the output of processes to support the managed introduction, utilisation or withdrawal of healthcare treatments within a local healthcare system, service or organisation.
Why do we need formularies?
improving patient outcomes by optimising the use of medicines
supporting the inclusion of patient factors in decision-making about medicines
improving collaboration between clinicians and commissioners
improving quality by reducing inappropriate variations in clinical care
improving quality through access to cost-effective medicines
supporting the supply arrangements of medicines across a local health economy
Who decides on formularies
Local Drug and Therapeutics Committee
Traffic Light Status of Drugs
RED: Secondary-care only. NOT to be prescribed by Primary Care
AMBER: Initiated by consultants, then prescribing can be passed onto GPs. Shared care agreements can be used.
GREEN (or blue): Can be used across primary & secondary care.