Chapter 17) Dental Soft Deposits, Stains, and Calculus
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
Dental Biofilm and Other Soft Deposit Examples:
dental biofilm (soft deposits)
acquired enamel pellicle
microbial (bacterial) biofilm
materia alba
food debris
calculus (hard mineralized deposits)
supragingival
subgingival
Pellicle Formation:
thin, acellular tenacious film/formation 30-90minutes
Types of Pellicle:
supra and subgingival pellicle
Significance of Pellicle:
protective, lubricates, acts as a nidus of attachment for bacteria and calculus
salivary proteins > high affinity for hydroxyapatite of enamel > pellicle formation
Removal of Pellicle:
patient oral self-care (tooth brushing/flossing)
polishing procedures
Oral microbiome composed of:
microorganisms
their genetic makeup
environments of oral cavity (multi-teeth, gingival sulcus, attached gingiva, tongue, oral mucosa, lips and hard and soft palates)
Good Oral Microbiome:
microorganisms perform pro and anti-inflammatory activities which maintain homeostasis
Bad Oral Microbiome:
the matrix protects the biofilm from the host’s immune system and antimicrobial agents
Formation of Biofilm: Stage 1 Formation
Initial attachment of planktonic bacterial cells to the pellicle
. Cells are “not committed” and its reversible
Formation of Biofilm: Stage 2 Bacterial Multiplication and Colonization
Microorganisms attach themselves and multiply “irreversible manner of microorganisms”
Formation of Biofilm: Stage 3 Matrix Formation
EPS secreted by cells form a Matrix (protects biofilm)
Formation of Biofilm: Stage 4 Biofilm Growth
Cell-to-cell communication (Quorum sensing)
Formation of Biofilm: Stage 5 Maturation
Bacterial colonies mature and release planktonic cells to spread and go elsewhere in the mouth
Changes in Biofilm Microorganisms: Days 1-2
gram-positive cocci present
Changes in Biofilm Microorganisms: Days 2-4
Cocci still dominate but gram-positive filamentous form and slender rods join the surface.
Within 72 hours, biofilm has matured>inflammation initiation
Changes in Biofilm Microorganisms: Days 6-10
Filaments increase, heavy leukocytes
Gram-negative bacteria
EPS secreted by bacteria> to 3-deminsional biofilm structure
Changes in Biofilm Microorganisms: Days 10-21=
clinically evident gingivitis
Supragingival Biofilm:
Made up of two layers
(basal layer) gram-positive aerobic bacteria
greater variability layer forms on top of basal layer
Subgingival Biofilm:
I. Made up of four layers
II. Predominantly spirochetes and gram- negative anaerobic and motile organisms
III. From top layer, bacteria invades connective tissue.
Composition of Dental Biofilm: Inorganic Elements
calcium and phosphorus
fluoride
Composition of Dental Biofilm: Organic Elements (found in EPS)
Carbohydrates (glucans)> tenacious adherence
Proteins & small amount of lipids
Microorganism and EPS make up __% of the biofilm, the other is _% water
80, 20
_____ transports the minerals during the mineralization and demineralization processes
Saliva
Clinical Aspects: Distribution of Biofilm (surface and location)
supragingival biofilm
gingival biofilm
subgingival biofilm
fissure biofilm
Clinical Aspects: How to Detect Biofilm
direct vision
use of explorer or probe
disclosing agent
clinical record (slight, moderate, heavy)
Dental Caries:
Cariogenic Microorganisms in Biofilm
The pH of Biofilm
Critical pH enamel=5.5
Critical pH dentin & cementum= 6.2-6.4
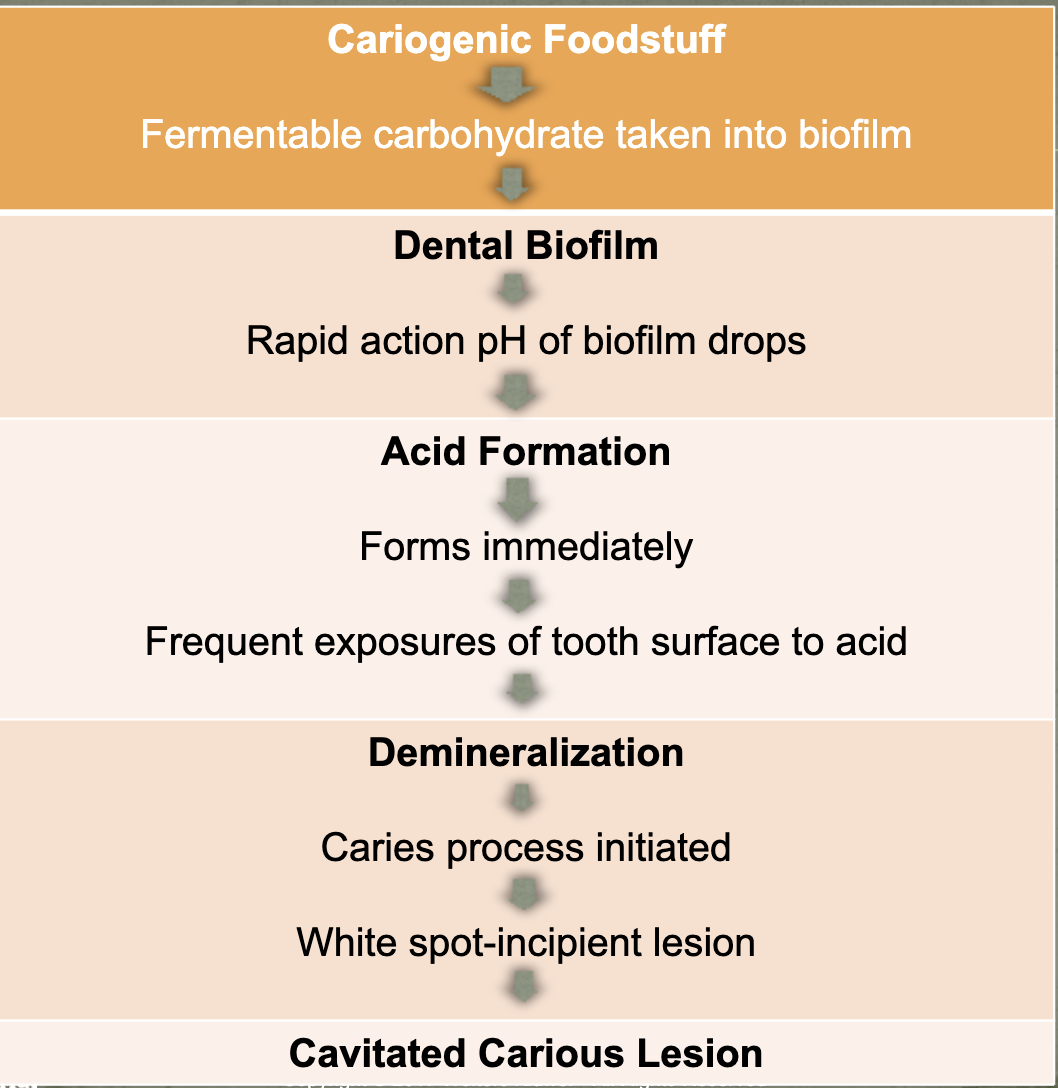
Effect of Diet on Biofilm:
high cariogenic diet, biofilm gradually increases its pH lowering ability
Materia Alba:
Clinical Appearance and Content
Soft whitish or grayish-white deposit
Clinically visible w/o disclosing agent
Unorganized accumulation of living and dead bacteria, cells, leukocytes, salivary proteins.
Prevention
Removable with water spray device or tongue action.
Food Debris:
• Collection at cervical third and proximal embrasures
• Vertical food impaction
• Contributes to general unsanitary condition and initiation of dental caries
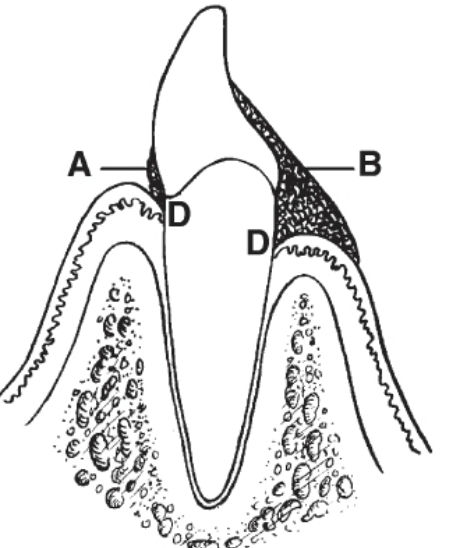
Supragingival Calculus:
Location: clinical crowns, implants, dentures, etc
Distribution: most frequent sites→ lingual of lower anterior teeth and facials of maxillary 1st and 2nd molars
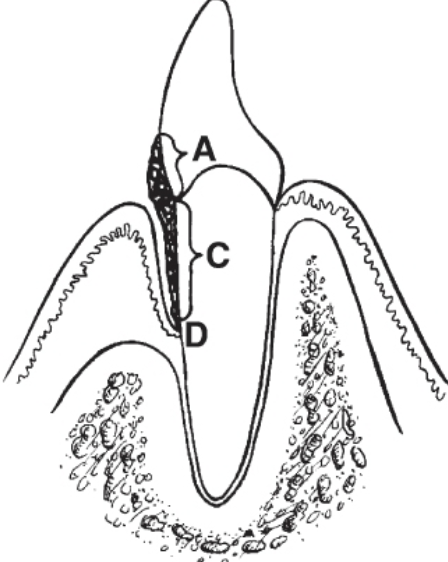
Subgingival Calculus:
Location: clinical crown apical to the gingiva margin/dental implants
Distribution: localized or generalized/heaviest deposits on hard-to-reach areas for patient
___/_____ gives subgingival calculus its dark black color
GCF/blood
Calculus Detection: Supragingival
visual
compressed air-directly on calculus causes ‘chalky’ appearance
Calculus Detection: Subgingival
visual
air
tissue color change
tactile
probe
explorer
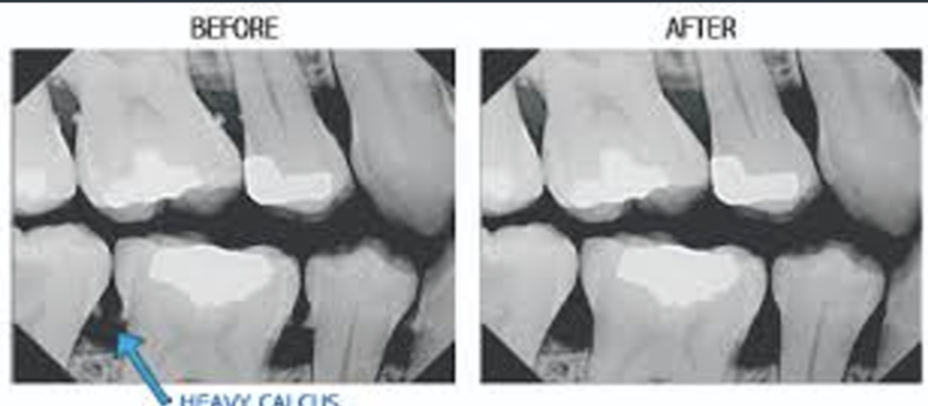
radiographic
dental endoscopy
Slight to Moderate Calculus:

Heavy Calculus/Stain:

Radiographic Calculus:
Mature calculus contains mostly ______ content
inorganic
Major Inorganic Components:
Calcium (Ca), Phosphorus (P), Carbonate (CO3), Sodium (Na), and Magnesium (Mg)
Trace Elements in Inorganic Calculus Composition:
Zinc (Zn, Strontium (Sr), Iron (Fe), Potassium (K),
Fluoride in Inorganic Calculus Composition:
binds to hydroxyapatite crystals
Inorganic Calculus Composition Crystals:
2/3 of inorganic content is crystalline (apatite)
Inorganic Calculus Compared with Teeth and Bone
dental enamel is the most mineralized tissue in the body
Steps of Calculus Formation:
pellicle forms, biofilm forms, then biofilm mineralizes
Calculus Formation: Mineralization
source elements differ between supra and subgingival calculus
saliva is source element for supra calculus
GCF and inflammatory exudate is source for subgingival
Calculus Formation: Structure of Calculus
layers parallel to the tooth surface
detectable with explorer and probe
Calculus Formation: Formation Time
Approximately 12 days and can begin as early as 24-48 hours
Types of Calculus Deposits:
crusty, spiny, nodular
ledge or ring
thin, smooth veneers
finger- and fern-like formations
individual islands/spots
supragingival or subgingival deposits
Attachment of calculus determines the difficulty of _______
removal
Attachment by means of an acquired pellicle
superficial, non-interlocking attachment, easily removed
Attachment to Minute Irregularities in the tooth surface by mechanical locking into undercuts
dentin and cementum irregularities
Attachment by direct contact between calcified intercellular matrix and the tooth surface
interlocking of inorganic apatite crystals of the enamel and cementum with the calculus
Debate over whether subgingival calculus plays a role in periodontal disease
• Rough texture of calculus acts as a reservoir for endotoxins and tissue breakdown products.
• Biofilm in contact with pocket > to inflammation
Microorganisms in biofilm layer perpetuate inflammatory state supragingivally and subgingivally
Increased flow of GCF, resulting in mineralized biofilm
Daily control of biofilm essentials:
Brushing and flossing, antimicrobial mouth rinses
Personal Dental Biofilm Control:
patient education on self oral care
Regular Professional Continuing Care:
at the dentist, maintenance appointments
Anti-calculus Dentifrice and Mouth rinses-Chemotherapeutic anti-calculus agents include:
A. pyrophosphates (anti-tartar)
B. zinc citrate (anti-tartar)
C. pyrophosphates + triclosan (antimicrobial)
Dental Stains and Discolorations Occur in 3 General Ways:
Adhere directly to surfaces
Contained within calculus and soft deposits
Incorporated within tooth structure or restorative material
Significance of stain is its ______ effect
cosmetic
Classification of Stains:
Extrinsic, Intrinsic, Exogenous, Endogenous
Recognition and Identification of Dental Stains:
medical and dental history
food dairy
oral hygiene habits
Application of Procedures of Stain Removal
Stains directly on tooth surface
Stains incorporated within tooth deposits
Stains incorporated within the tooth
Extrinsic Stains Categories:
directed extrinsic stains
indirect extrinsic stains
Most Frequently Observed Stains:
yellow
green
black line
tobacco

Yellow Stain:
Clinical Features
dull, yellowish discoloration of biofilm
Distribution on Tooth Surfaces
localized or generalized
Occurence
common in all ages
more evident with lack of personal care
Etiology
usually dietary sources

Green Stains:
Clinical Features
light yellowish-green in biofilm
Distribution on Tooth Surfaces
primarily facial, gingival 1/3 of maxillary teeth
Composition
chromogenic
Occurrence
any age, primary childhood

Black-Line Stain (Extrinsic)
Clinical Features
continuous or interrupted line, 1mm wide
Distribution on tooth surfaces
facial and lingual but rarely on max anterior facials
forms along gingival 1/3 near gingival margin
Composition and Formation
microorganisms embedded in intermicrobial substance
attachment by pellicle-like structure, mineralization is similar to the formation of calculus
Occurrence
all ages, more common in children
more common in females
frequently in clean mouths
Recurrence
quantity less with meticulous oral hygiene care

Tobacco Stain:
Clinical Features
light brown to dark leathery brown or black
Distribution on tooth Surface
cervical 1/3, primarily lingual surfaces
Composition
tar and products of combustion and brown pigments from smokeless tobacco
Predisposing factors
smoking
chewing tobacco
inadequate oral hygiene

Brown Stains:
Brown Pellicle
chemical alteration of the pellicle from staining
Stannous Fluoride
can cause staining with continuous care
Antimicrobial Agents
chlorhexidine
Betel/Acreca
betel nut chew
Swimmer Stain
chlorine or bromine in swimming pools
Orange and Red Stains:
Clinical Appearance
orange/red stains and cervical 1/3 of tooth
Distribution on Tooth Surfaces
more frequently on anterior teeth than posterior
Occurrence
rare (red more than orange)
Etiology
possibly chromogenic bacteria
Metallic Stains:
Metals or Metallic Salts from Metal-Containing Dust of Industry
copper or brass: green or blusish-green
iron: brown to greenish-brown
nickel: green
Prevention: wear a mask while working
Metallic Substances Contained in Drugs
iron: black (iron sulfide) or brown
manganese (from potassium permanganate)= black
prevention: take meds through a straw or tablet form to prevent contact with teeth

Endogenous Intrinsic Stains:
Pulpless or Traumatized Teeth
Clinical Appearance
wide range; light yellow-brown, slate gray, reddish brown, dark brown, bluish-black, black, orange, or greenish tinge
Etiology
blood-pigment from decomposed hemoglobin and pulp tissue penetrate and sicolor the dentinal tubules
Disturbances in Tooth Development: Hereditary Genetic
Amelogenesis imperfecta: enamel partially or completely missing
Dentinogenesis imperfecta (Opalescent dentin): dentin abnormality due to disturbance in odontoblastic layer during development
Disturbances in Tooth Development: Enamel Hypoplasia
damage to the tooth germ during development

Disturbances in Tooth Development: Dental Fluorosis
AKA mottled enamel
Drug-Induced Stains and Discolorations: Tetracycline
intrinsic staining via vertical transmission or absorbed while teeth are developing

Drug-Induced Stains and Discolorations: Minocycline
intrinsic staining post tooth eruption
Exogenous Intrinsic Stains: Restorative Materials
silver amalgam
endodontic therapy
tooth colored restorations stained with extrinsic staining substances
Exogenous Intrinsic Stains: Stain in Dentin
discoloration resulting from a carious lesion

Exogenous Intrinsic Stains: Other Local Causes
enamel erosion
attrition of occlusal forces
Documentation:
• Clinical description of appearance of teeth relative to biofilm, materia alba, or food debris
• Extent of supragingival and subgingival deposits
• Color, type, extent, and location of stains
• Personal patient care procedures demonstrated
Factors to Teach the Patient:
• Location and properties of biofilm and calculus
• Effects of personal oral care procedures
• Biofilm control procedures
• Sources of cariogenic foodstuff in the diet
• What calculus is and how it forms
• Etiology of individual’s dental stains
• Advantages of smoking cessation
• Effect of tetracyclines
• Select products approved by ADA or CDA
Does anterior or posterior surfaces have the least amount of biofilm?
Anterior
What is the Critical pH for enamel?
5.5
What is the critical pH for dentin and cementum?
6.2-6.4