Airways and Airflow
1/189
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
190 Terms
learning objectives (use this as a list)
Explain the anatomy and physiology of the airways, including the structures and functions of the upper and lower respiratory tract.
Describe the mechanisms of airflow, including the principles of gas exchange and the factors that influence airflow in the lungs.
Analyze the pathophysiology of common respiratory disorders that affect airway structure and function, such as asthma, chronic obstructive pulmonary disease (COPD), and bronchiectasis.
Analyze the pathophysiology of common respiratory disorders that affect airway structure and function, such as asthma, chronic obstructive pulmonary disease (COPD), and bronchiectasis.
asthma
asthma: ““gasping,” or “shortness of breath.”, because asthma is Chronic reversible airway inflammation with hyperresponsiveness.
asthma is inflammation, therefore, asthma causes bronchoCONSTRICTON.
A. AIRWAY STRUCTURAL CHANGES
Chronic inflammation → Structural remodeling
Smooth muscle hypertrophy & hyperplasia
→ Increases airway narrowing and hyperresponsiveness.Goblet cell hyperplasia + mucous gland enlargement
→ Excess thick mucus → mucus plugging.Subepithelial fibrosis (“basement membrane thickening”)
→ Makes the airway stiffer.Epithelial shedding
→ Exposes nerve endings → stimulates reflex bronchoconstriction.Infiltrates: eosinophils, Th2 lymphocytes, mast cells
B. AIRWAY FUNCTIONAL CHANGES
Bronchoconstriction (smooth muscle tightening)
Airway edema
Mucus plugging
Widespread but variable airway narrowing
When a disease process such as asthma has already caused some bronchiolar constriction, superimposed parasympathetic nervous stimulation often worsens the condition. When this occurs, administration of drugs that block the effects of acetylcholine, such as atropine, can sometimes relax the respiratory passages enough to relieve the obstruction.
atropine: specifically: competitive antagonist of M₁, M₂, M₃ muscarinic receptors.
Atropine blocks parasympathetic (ACh) activity.
COPD (chronic bronchitis, emphysema)
2. CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)
chronic: constant
obstructive: blocking
pulmonary: lungs
disease
COPD includes:
Chronic bronchitis
Emphysema
It is progressive, irreversible, and caused mainly by long-term smoking.
chronic bronchitis
A. CHRONIC BRONCHITIS
chronic: constant
bronch: “windpipe,” “airway,” “throat,” or “bronchial tube.”
“-itis”: meaning “inflammation of.”
Large airway disease with mucus overproduction
Mucus plugging → narrow airways
↓ airway diameter → ↑ resistance → obstruction
Low V/Q areas → hypoxemia (“blue bloater” phenotype)
Recurrent infections are common.
emphysema
B. EMPHYSEMA
em: “within.”
-physa: “to inflate with air.”
Emphysema = “puffing/inflation within” or “air swelling.”
destruction of alveolar walls
-air becomes trapped due (no recoil due to destruction of alveolar walls)
→ air becomes trapped
→ lungs become inflated / overdistended
→ loss of recoil → barrel chest
↑ compliance (lungs expand too easily)
Barrel chest due to hyperinflation
High V/Q areas due to destruction of capillaries (pink puffer because of lots of ventilation but low blood flow)
Mild hypoxemia (“pink puffer” phenotype)
cyanosis
cyan: lots of blood flow, poor ventilation
VA/Q is low
pink puffer
pink: lots of ventilation, poor blood flow
VA/Q is high
V/Q in COPD
cyanosis occurs in which type of COPD (chronic bronchitis or Emphysema)?
V/Q in COPD
Chronic bronchitis → LOW V/Q (poor ventilation) (cyanosis)
Emphysema → HIGH V/Q (capillary destruction → less perfusion)
bronchiectasis
ectasis: stretching
broncho: “windpipe”
“-ectasis”: “stretching,”
Bronchiectasis = “abnormal dilation or stretching of the bronchi.”
Permanent dilation of bronchi due to chronic infection + inflammation
Inflammation is neutrophil-driven: neutrophils are the primary immune cells responsible for causing and sustaining the inflammation in that disease.
neutrophils INACTIVATE bronchoconstrictors and neutrophils increase NO → bronchodilation.
Often caused by:
Recurrent pneumonia
Cystic fibrosis
Primary ciliary dyskinesia
Allergic bronchopulmonary aspergillosis (ABPA)
A. AIRWAY STRUCTURAL CHANGES
Destruction of airway smooth muscle + elastic tissue
Permanent dilation of bronchi (irreversible)
Thickened, scarred airway walls
Mucus build-up inside dilated bronchi
“Tram-track” appearance on CT
B. AIRWAY FUNCTIONAL CHANGES
Dilated but poorly functioning bronchi cannot clear mucus
→ Chronic infection → inflammation → vicious cycle.Airflow obstruction (similar PFTs to COPD)
Low V/Q due to poor ventilation
Productive cough with foul sputum
Hemoptysis from inflamed bronchial arteries
Bronchiectasis = irreversible airway dilation caused by chronic infection/inflammation → mucus retention → recurring infection → further destruction.
COPD = chronic, progressive obstruction due to:
Mucus + wall thickening (bronchitis)
Loss of recoil + alveolar destruction (emphysema)
COMPARISON TABLE
Feature | Asthma | COPD | Bronchiectasis |
|---|---|---|---|
Reversible? | Yes | No | No |
Inflammation | Eosinophils, Th2 | Neutrophils, macrophages | Neutrophilic |
Key issue | Hyperreactivity | Chronic obstruction | Airway destruction |
Major structure change | Smooth muscle hypertrophy | Emphysema + mucus glands | Bronchial dilation + fibrosis |
Mucus | Common | Very common | Very common, purulent |
V/Q mismatch | Low V/Q in attacks | Mixed high & low | Low V/Q |
PFT pattern | Obstructive, reversible | Obstructive, irreversible | Obstructive, irreversible |
airways and airflow textbook
Textbook of Medical Physiology, Guyton and Hall, 12th edition:
Chapter 37 - 39, Pg 465 - 494
Physiology, Costanzo, 6th edition:
Chapter 5, Pg 189 - 191
Textbook of Medical Physiology (Guyton and Hall) section
Textbook of Medical Physiology, Guyton and Hall, 12th edition:
Chapter 37 - 39, Pg 465 - 494.
Explain the anatomy and physiology of the airways, including the structures and functions of the upper and lower respiratory tract.
overview of respiratory tract
I. OVERVIEW OF THE RESPIRATORY TRACT
The respiratory system is divided into: upper respiratory tract and lower respiratory tract.
1. Upper Respiratory Tract
Nose
Nasal cavity
Paranasal sinuses
Pharynx (nasopharynx, oropharynx, laryngopharynx)
Larynx (borderline structure—functionally part of airway protection)
when you hit the trachea, you hit the lower respiratory tract.
2. Lower Respiratory Tract
Trachea
Bronchi (primary, secondary, tertiary)
Bronchioles (terminal, respiratory)
Alveolar ducts
Alveoli
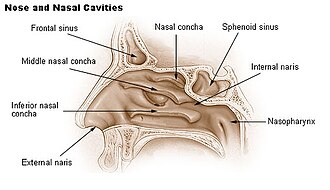
II. UPPER RESPIRATORY TRACT: ANATOMY & FUNCTIONS 1. Nose & Nasal Cavity Anatomy
External nose
Nasal septum (vomer, perpendicular plate of ethmoid, septal cartilage)
Nasal conchae (superior, middle, inferior turbinates)
Olfactory epithelium (superior region)
Physiology & Functions of upper respiratory tract
Warm air (vascular mucosa → heat exchange)
Humidify air (mucous membrane)
Filter air (vibrissae + mucociliary escalator)
Smell (olfaction)
Resonance for speech
2. Paranasal Sinuses
(frontal, ethmoid, sphenoid, maxillary)
Lighten skull
Humidify & warm air
Increase voice resonance
Produce mucus that drains into nasal cavity
3. Pharynx
Divided into:
a. Nasopharynx
Behind nasal cavity
Contains adenoids
Only conducts air
Eustachian tube openings → equalize pressure
b. Oropharynx
Behind oral cavity
Common pathway for food + air
Contains palatine tonsils
c. Laryngopharynx
Behind larynx
Directs food into esophagus and air into larynx
Functions
Conduct air
Provide immune defense (tonsils)
Swallowing coordination
larynx key structures
4. Larynx Key Structures
Cartilages: thyroid, cricoid, epiglottis, arytenoid, corniculate, cuneiform
Vocal cords
Glottis
Muscles (intrinsic and extrinsic)
Airway protection (epiglottis seals airway during swallowing)
Sound production (vocal cords)
Maintains open airway via cartilaginous support
Cough reflex initiation
lower respiratory tract anatomy and functions
III. LOWER RESPIRATORY TRACT: ANATOMY & FUNCTIONS
1. Trachea Anatomy
10–12 cm long
C-shaped hyaline cartilage rings
Posterior trachealis muscle
Lined with pseudostratified ciliated columnar epithelium (mucociliary escalator)
Conducts air to bronchi
Cartilage prevents collapse
Cilia + mucus trap particles and move them upward
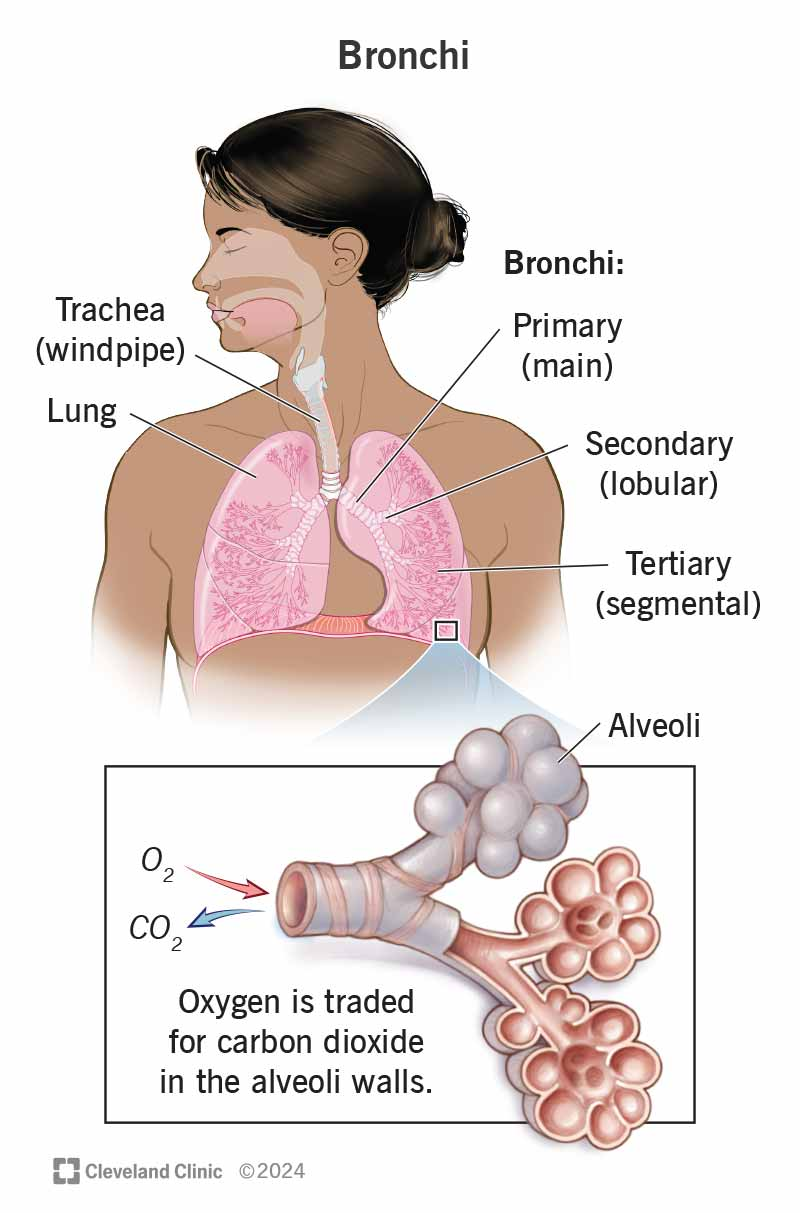
Bronchial Tree Primary (main) bronchi
primary bronchi
secondary bronchi
tertiary bronchi
2. Bronchial Tree Primary (main) bronchi
Right → wider, shorter, more vertical → aspiration risk
Left → longer, more horizontal
Secondary (lobar) bronchi
Right: 3
Left: 2
Tertiary (segmental) bronchi
Supply bronchopulmonary segments (surgical units)
Conduct air
Regulate airflow through smooth muscle tone
Filter and humidify air

bronchioles
what do the bronchioles lose and what are the bronchioles made out of?
3. Bronchioles
Bronchi → bronchioles lose cartilage and become entirely smooth muscle.
Types
Terminal bronchioles – end of conducting zone
Respiratory bronchioles – beginning of gas exchange
Control airway resistance (bronchodilation / bronchoconstriction)
Conduct air to alveoli
Participate in limited gas exchange (respiratory bronchioles)
Physiology
Sympathetic (β₂) → bronchodilation
Parasympathetic (ACh) → bronchoconstriction
Asthma → hyperresponsive constriction
Alveolar Ducts & Alveoli Anatomy
what are the alveoli lined by?
4. Alveolar Ducts & Alveoli Anatomy
Alveoli: tiny air sacs (300 million)
the alveoli are lined by pneumocytes and macrophages:
Type I pneumocytes – gas exchange (95%)
Type II pneumocytes – secrete surfactant
Alveolar macrophages
Primary gas exchange site
Surfactant ↓ surface tension → prevents alveolar collapse (especially during expiration)
Thin respiratory membrane (~0.5 µm) → rapid diffusion
Partial Pressure Gradients
O₂: alveoli → blood
CO₂: blood → alveoli
functional divisions of respiratory system
-conducting zone
-respiratory zone
IV. FUNCTIONAL DIVISIONS OF RESPIRATORY SYSTEM Conducting Zone
Includes:
Nose → terminal bronchioles
Warm, humidify, filter air
Conduct air (no gas exchange)
Mucociliary clearance
Respiratory Zone
Includes:
Respiratory bronchioles
Alveolar ducts
Alveoli
Gas exchange
Diffusion of O₂ and CO₂
Surfactant secretion
Describe the mechanisms of airflow, including the principles of gas exchange and the factors that influence airflow in the lungs.
pressure gradients
airway resistance
I. MECHANISMS OF AIRFLOW
Airflow in the lungs is governed by pressure gradients and airway resistance.
air flows from a region of higher pressure to lower pressure
Airflow (𝑄) is described by:
airflow (Q)= ((ΔP) / Resistance)
Where:
ΔP = alveolar pressure – atmospheric pressure
Resistance = airway radius, smooth muscle tone, mucus, inflammation
II. HOW AIR MOVES DURING BREATHING
A. Inspiration (Airflow Into the Lungs)
1. Pressure changes
Diaphragm contracts → thoracic volume increases
Intrapleural pressure becomes more negative (intrapleural pressure drives alveolar pressure changes)
Alveolar pressure drops below atmospheric pressure
Air flows into lungs
2. Muscles involved
Primary: Diaphragm
Secondary: External intercostals
Accessory (deep breaths): SCM, scalenes, pec minor
3. Result
↑ Volume → ↓ Pressure → Air enters
B. Expiration (Airflow Out of the Lungs)
1. Quiet expiration
Passive
Diaphragm relaxes
Elastic recoil of lungs increases alveolar pressure above atmospheric
Air flows out
2. Forced expiration
Active (internal intercostals + abdominal muscles)
Strongly ↑ intrathoracic pressure
Rapid expulsion of air
3. Result
↓ Volume → ↑ Pressure → Air exits
III. PRINCIPLES OF GAS EXCHANGE
Gas exchange occurs across the respiratory membrane (alveoli + capillaries) by simple diffusion.
Driving force = Partial pressure gradients Oxygen (O₂)
Alveoli: ~104 mmHg
Pulmonary capillary: ~40 mmHg
→ O₂ diffuses into blood (because the blood has a lower partial pressure, and the gas goes from a higher partial pressure to a lower pressure.)
Carbon dioxide (CO₂)
Pulmonary capillary: ~45 mmHg
Alveoli: ~40 mmHg
→ CO₂ diffuses into alveoli
Diffusion follows Fick's Law
Rate of diffusion ∝ Surface Area × Pressure Gradient × Solubility
/ Membrane Thickness
Thus diffusion is impaired by:
thicker membrane (fibrosis, edema)
decreased surface area (emphysema)
decreased perfusion (PE)
fluid/pus-filled alveoli (pneumonia)
CO₂ diffuses 20× faster than O₂ due to higher solubility.
IV. FACTORS THAT INFLUENCE AIRFLOW
Airflow is determined by airway resistance, lung compliance, and elastic recoil.
1. Airway Resistance
Resistance ∝ 1 / (radius⁴)
Increased resistance (reduces airflow)
Bronchoconstriction (asthma, ACh, allergens)
Mucus plugging (COPD, chronic bronchitis)
Airway edema (inflammation)
Low lung volumes (airways less stretched open)
Dynamic airway collapse in emphysema (loss of support)
Decreased resistance (increases airflow)
Bronchodilation (β₂ agonists, sympathetic stimulation)
High lung volumes (airways pulled open)
2. Lung Compliance
Compliance = ΔV/ΔP (how easily lungs expand)
High compliance
Emphysema (floppy lungs)
Easy to inflate → but poor recoil → air trapping
Low compliance
Fibrosis, ARDS, pneumonia
Hard to inflate → reduced ventilation
Compliance affects:
Work of breathing
Inflation/deflation curves
Ability to generate adequate alveolar ventilation
3. Elastic Recoil
Provided by elastin fibers + surface tension
Necessary for expiration
Decreased in emphysema → air trapping
Increased in fibrosis → stiff lungs
4. Pulmonary Blood Flow (Perfusion)
Good ventilation requires matching V (airflow) with Q (blood flow).
V/Q mismatch
Dead space (ventilation without perfusion) → pulmonary embolism
Shunt (perfusion without ventilation) → pneumonia, atelectasis
Gas exchange efficiency depends on matching ventilation to perfusion.
V. SUMMARY (Exam-Ready) Airflow depends on:
Pressure gradients (ΔP)
Airway resistance (radius, smooth muscle, mucus)
Lung compliance
Elastic recoil
Adequate pulmonary blood flow (V/Q matching)
Gas exchange depends on:
Partial pressure gradients (O₂ & CO₂)
Thin respiratory membrane
Large surface area
Adequate perfusion
Gas solubility (CO₂ > O₂)
CHAPTER 37
Pulmonary Ventilation
Pulmonary Ventilation
Respiration provides oxygen to the tissues and removes carbon dioxide.
The four major functions of respiration are:
(1) pulmonary ventilation, which means the inflow and outflow of air between the atmosphere and the lung alveoli;
(2) diffusion of oxygen and carbon dioxide between the alveoli and the blood;
(3) transport of oxygen and carbon dioxide in the blood and body fluids to and from the body’s tissue cells; and
(4) regulation of ventilation and other facets of respiration.
This chapter is a discussion of pulmonary ventilation, and the subsequent five chapters cover other respiratory functions plus the physiology of special respiratory abnormalities.
Mechanics of Pulmonary Ventilation
Muscles That Cause Lung Expansion and Contraction
Pressures That Cause the Movement of Air In and Out of the Lungs
Compliance of the Lungs
Surfactant, Surface Tension, and Collapse of the Alveoli
Surfactant and Its Effect on Surface Tension.
Pressure in Occluded Alveoli Caused by Surface Tension
Effect of Alveolar Radius on the Pressure Caused by Surface Tension
Effect of the Thoracic Cage on Lung Expansibility
Muscles That Cause Lung Expansion and Contraction (Mechanics of Pulmonary Ventilation)
Muscles That Cause Lung Expansion and Contraction
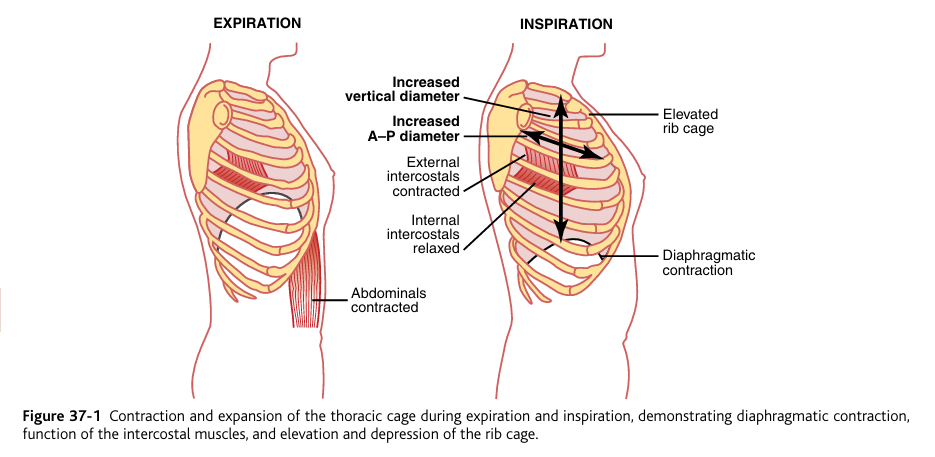
The lungs can be expanded and contracted in two ways:
(1) by downward and upward movement of the diaphragm to lengthen or shorten the chest cavity
(2) by elevation and depression of the ribs to increase and decrease the anteroposterior diameter of the chest cavity. Figure 37-1 shows these two methods.
Normal quiet breathing is accomplished by movement of the diaphragm. During inspiration, contraction of the diaphragm pulls the lower surfaces of the lungs downward. Then, during expiration, the diaphragm simply relaxes, and the elastic recoil of the lungs, chest wall, and abdominal structures compresses the lungs and expels the air. During heavy breathing, however, the elastic forces are not powerful enough to cause the necessary rapid expiration, so extra force is achieved mainly by contraction of the abdominal muscles, which pushes the abdominal contents upward against the bottom of the diaphragm, thereby compressing the lungs.
The second method for expanding the lungs is to raise the rib cage. This expands the lungs because, in the natural resting position, the ribs slant downward, as shown on the left side of Figure 37-1, thus allowing the sternum to fall backward toward the vertebral column. When the rib cage is elevated, however, the ribs project almost directly forward, so the sternum also moves forward, away from the spine, making the anteroposterior thickness of the chest about 20 percent greater during maximum inspiration than during expiration. Therefore, all the muscles that elevate the chest cage are classified as muscles of inspiration, and those muscles that depress the chest cage are classified as muscles of expiration. The most important muscles that raise the rib (during inhalation) cage are the external intercostals, but others that help are the (1) sternocleidomastoid muscles, which lift upward on the sternum; (2) anterior serrati, which lift many of the ribs; and (3) scaleni, which lift the first two ribs.
The muscles that pull the rib cage downward during expiration are mainly the (1) abdominal recti, which have the powerful effect of pulling downward on the lower ribs at the same time that they and other abdominal muscles also compress the abdominal contents upward against the diaphragm, and (2) internal intercostals.
Figure 37-1 also shows the mechanism by which the external and internal intercostals act to cause inspiration and expiration. To the left, the ribs during expiration are angled downward, and the external intercostals are elongated forward and downward. As they contract, they pull the upper ribs forward in relation to the lower ribs, and this causes leverage on the ribs to raise them upward, thereby causing inspiration. The internal intercostals function exactly in the opposite manner, functioning as expiratory muscles because they angle between the ribs in the opposite direction and cause opposite leverage.
Pressures That Cause the Movement of Air In and Out of the Lungs (Mechanics of Pulmonary Ventilation)
thoracic cavity
pleural fluid
continual suction of excess fluid into lymphatic channels
The lung is an elastic structure that collapses like a balloon and expels all its air through the trachea whenever there is no force to keep it inflated. Also, there are no attachments between the lung and the walls of the chest cage, except where it is suspended at its hilum from the mediastinum, the middle section of the chest cavity.
Instead, the lung “floats” in the thoracic cavity, surrounded by a thin layer of pleural fluid that lubricates movement of the lungs within the cavity.
Further, continual suction of excess pleural fluid into lymphatic channels maintains a slight suction between the visceral surface of the lung pleura and the parietal pleural surface of the thoracic cavity.
Therefore, the lungs are held to the thoracic wall as if glued there, except that they are well lubricated and can slide freely as the chest expands and contracts.
thoracic cavity
the thoracic cavity is is the “hollow space inside the thorax” thorax means chest, the lungs are located in the thoracic cavity.
pleural cavity
pleural: side, rib, flank
cavity: space
“The hollow space at the sides (around the ribs) of the chest.”
the pleural fluid is located inside the pleural cavity
The pleural cavity is the thin potential space between:
Visceral pleura (on the lung)
Parietal pleura (lining the chest wall)
Inside this space is a very thin layer of pleural fluid (just a few milliliters).
the pleural cavity literally just houses the pleural fluid.
the LUNGS ARE NOT LOCATED in the pleural cavity, the lungs are located in the thoracic cavity.
The lungs are located in the thoracic cavity.
The lungs are NOT located inside the pleural cavity.
Instead, each lung is surrounded by a pleural cavity.
Pleural Pressure and Its Changes During Respiration (Mechanics of Pulmonary Ventilation)
pleural pressure
slightly negative
lung expansion
really negative
expiration
more positive
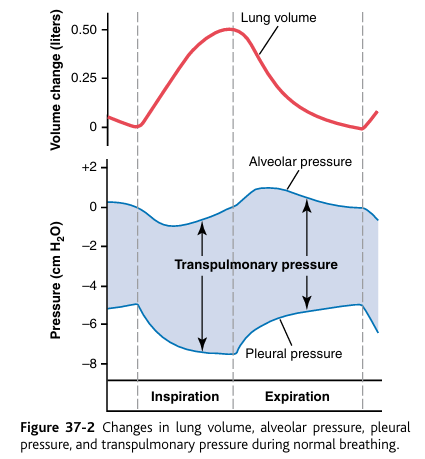
Pleural pressure is the pressure of the fluid in the thin space between the lung pleura and the chest wall pleura. As noted earlier, this is normally a slight suction, which means a slightly negative pressure.
The normal pleural pressure at the beginning of inspiration is about −5 centimeters of water, which is the amount of suction required to hold the lungs open to their resting level. Then, during normal inspiration, expansion of the chest cage pulls outward on the lungs with greater force and creates more negative pressure, to an average of about −7.5 centimeters of water.
These relationships between pleural pressure and changing lung volume are demonstrated in Figure 37-2, showing in the lower panel the increasing negativity of the pleural pressure from −5 to −7.5 during inspiration and in the upper panel an increase in lung volume of 0.5 liter. Then, during expiration, the events are essentially reversed.
Boyle’s Law (inverse relationship between volume and pressure)
More volume → lower pressure (Boyle’s law)
Because the pleural cavity gets slightly larger:
more volume
air pressure becomes more negative
air flows in
Alveolar Pressure
Alveolar pressure is the pressure of the air inside the lung alveoli (it’s in the name).
When the glottis is open and no air is flowing into or out of the lungs, the pressures in all parts of the respiratory tree, all the way to the alveoli, are equal to atmospheric pressure, which is considered to be zero reference pressure in the airways—that is, 0 cm water pressure.
To cause inward flow of air into the alveoli during inspiration, the pressure in the alveoli must fall to a value slightly below atmospheric pressure (below 0).
The second curve (labeled “alveolar pressure”) of Figure 37-2 demonstrates that during normal inspiration, alveolar pressure decreases to about −1 centimeters of water. This slight negative pressure is enough to pull 0.5 liter of air into the lungs in the 2 seconds required for normal quiet inspiration.
During expiration, opposite pressures occur: The alveolar pressure rises to about +1 centimeter of water, and this forces the 0.5 liter of inspired air out of the lungs during the 2 to 3 seconds of expiration.
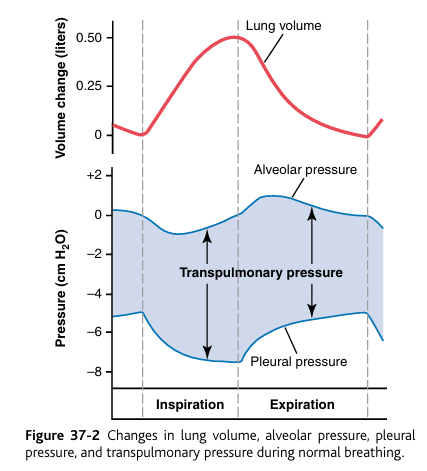

Transpulmonary Pressure
Transpulmonary pressure is the pressure that keeps your lungs open.
Finally, note in Figure 37-2 the transpulmonary pressure is the difference between the alveolar pressure and the pleural pressure.
Recoil pressure refers to the force with which the lungs naturally try to collapse inward due to their elastic properties.
Recoil pressure = Transpulmonary pressure
(at static conditions)
Alveolar pressure (Pₐ): the pressure inside the air sacs (alveoli).
Intrapleural pressure (Pᵢₚ): the pressure in the pleural cavity (the thin space between lung and chest wall), which is normally negative.
If transpulmonary pressure is:
High (positive) → lungs are more expanded.
Low → lungs are less expanded.
Zero → lung would collapse (like in pneumothorax).
Compliance of the Lungs
The extent to which the lungs will expand for each unit increase in transpulmonary pressure (if enough time is allowed to reach equilibrium) is called the lung compliance.
The total compliance of both lungs together in the normal adult human being averages about 200 milliliters of air per centimeter of water transpulmonary pressure. That is, every time the transpulmonary pressure increases 1 centimeter of water, the lung volume, after 10 to 20 seconds, will expand 200 milliliters.
Compliance Diagram of the Lungs (relationship between volume and transpulmonary pressure)
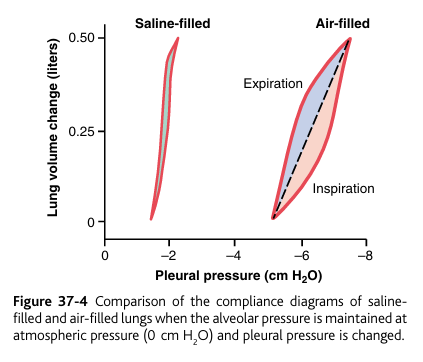
Figure 37-3 is a diagram relating lung volume changes to changes in transpulmonary pressure. Note that the relation is different for inspiration and expiration. Each curve is recorded by changing the transpulmonary pressure in small steps and allowing the lung volume to come to a steady level between successive steps. The two curves are called, respectively, the inspiratory compliance curve and the expiratory compliance curve, and the entire diagram is called the compliance diagram of the lungs.
Figure 37-3: as lung volume increases (inspiration), pleural pressure (not transpulmonary) becomes more negative, and compliance decreases (because you are running out of compliance)
The characteristics of the compliance diagram are determined by the elastic forces of the lungs (that’s why it’s called Compliance Diagram). These can be divided into two parts: (1) elastic forces of the lung tissue and (2) elastic forces caused by surface tension of the fluid that lines the inside walls of the alveoli and other lung air spaces.
The elastic forces of the lung tissue are determined mainly by elastin and collagen fibers interwoven among the lung parenchyma. In deflated lungs, these fibers are in an elastically contracted and kinked state; then, when the lungs expand, the fibers become stretched and unkinked, thereby elongating and exerting even more elastic force.
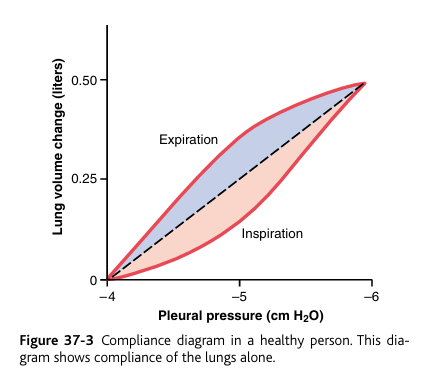
The elastic forces caused by surface tension are much more complex. The significance of surface tension is shown in Figure 37-4, which compares the compliance diagram of the lungs when filled with saline solution and when filled with air. When the lungs are filled with air, there is an interface between the alveolar fluid and the air in the alveoli. In the case of the saline solution–filled lungs, there is no air-fluid interface; therefore, the surface tension effect is not present—only tissue elastic forces are operative in the saline solution–filled lung.
Note that transpleural pressures required to expand air-filled lungs are about three times as great as those required to expand saline solution–filled lungs. Thus, one can conclude that the tissue elastic forces tending to cause collapse of the air-filled lung represent only about one third of the total lung elasticity, whereas the fluid-air surface tension forces in the alveoli represent about two thirds.
The fluid-air surface tension elastic forces of the lungs also increase tremendously when the substance called surfactant is not present in the alveolar fluid. Let us now discuss surfactant and its relation to the surface tension forces.
why is does water + air mean surface tension, and what does this mean for lungs?
water + water= equal pull
water + air= water molecules at the top become “tight” creating surface tension.
when lungs are filled with saline:
-there is no air
-All sides of the water molecules are surrounded by fluid.
-surface tension disappears completely.
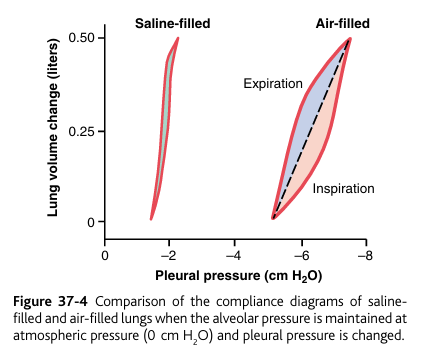
air vs saline solution effect on lung compliance
1. When lungs are filled with air
The alveoli have an air–fluid interface.
the water molecules on the surface have an especially strong interaction with each other
This creates surface tension (contraction)
Surface tension adds a big collapsing force, making the lung less compliant (stiffer).
So more pressure is needed to expand the lungs.
(This is the normal situation in real life.)
2. When lungs are filled with saline solution
There is no air–fluid interface (air is replaced by fluid).
That means no surface tension, because surface tension only exists when fluid meets air.
Only the tissue elastic forces remain.
*this experiment shows that saline is crucial because it lowers surface tension, making lungs much more compliant.
So the lung becomes very compliant (easy to inflate).
You need much less pressure to inflate saline-filled lungs.
Surfactant, Surface Tension, and Collapse of the Alveoli
Principle of Surface Tension.
surface tension elastic force
Principle of Surface Tension. When water forms a surface with air, the water molecules on the surface of the water have an especially strong attraction for one another. As a result, the water surface is always attempting to contract. This is what holds raindrops together—a tight con tractile membrane of water molecules around the entire surface of the raindrop.
Inside the alveoli, the water surface is also attempting to contract. This results in an attempt to force the air out of the alveoli through the bronchi and, in doing so, causes the alveoli to try to collapse. The net effect is to cause an elastic contractile force of the entire lungs, which is called the surface tension elastic force.
surface tension elastic force: the collapsing force created by the surface tension of water in the lungs.
water contraction (surface tension) → attempt to force air out of alveoli → lung collapse
Surfactant and Its Effect on Surface Tension
type II alveolar epithelial cells
Surfactant: greatly reduces the surface tension of water.
surfactant is secreted by special surfactant-secreting epithelial cells called type II alveolar epithelial cells,
type II alveolar epithelial cells which constitute about 10 percent of the surface area of the alveoli. These cells are granular, containing lipid inclusions that are secreted in the surfactant into the alveoli.
the name “type II alveolar epithelial cells” doesnt tell you the function, you just have to know the function.
Surfactant
Surfactant is a complex mixture of several phospholipids, proteins, and ions. The most important components are the phospholipid dipalmitoylphosphatidylcholine, surfactant apoproteins, and calcium ions.
The dipalmitoylphosphatidylcholine and several less important phospholipids are responsible for reducing the surface tension.
They do this by not dissolving uniformly in the fluid lining the alveolar surface. Instead, part of the molecule dissolves while the remainder spreads over the surface of the water in the alveoli.
This surface has from one-twelfth to one-half the surface tension of a pure water surface.
Pressure in Occluded Alveoli Caused by Surface Tension.
occlude: “block, obstruct”
If the air passages leading from the alveoli of the lungs are blocked, the surface tension in the alveoli tends to collapse the alveoli. This creates positive pressure in the alveoli, attempting to push the air out. The amount of pressure generated in this way in an alveolus can be calculated from the following formula:
Pressure = 2 x surface tension/ radius of alveolus
more surface tension = more positive pressure pushing air out.
For the average-sized alveolus with a radius of about 100 micrometers and lined with normal surfactant, this calculates to be about 4 centimeters of water pressure (3 mm Hg). If the alveoli were lined with pure water without any surfactant, the pressure would calculate to be about 18 centimeters of water pressure, 4.5 times as great. Thus, one sees how important surfactant is in reducing alveolar surface tension and therefore also reducing the effort required by the respiratory muscles to expand the lungs.
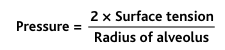
Effect of Alveolar Radius on the Pressure Caused by Surface Tension
Note from the preceding formula that the pressure generated as a result of surface tension in the alveoli is inversely affected by the radius of the alveolus, which means that the smaller the alveolus, the greater the alveolar pressure caused by the surface tension.
Thus, when the alveoli have half the normal radius (50 instead of 100 micrometers), the pressures noted earlier are doubled. This is especially significant in small premature babies, many of whom have alveoli with radii less than one quarter that of an adult person. Further, surfactant does not normally begin to be secreted into the alveoli until between the sixth and seventh months of gestation, and in some cases, even later than that. Therefore, many premature babies have little or no surfactant in the alveoli when they are born, and their lungs have an extreme tendency to collapse, sometimes as great as six to eight times that in a normal adult person. This causes the condition called respiratory distress syndrome of the newborn. It is fatal if not treated with strong measures, especially properly applied continuous positive pressure breathing.
respiratory distress syndrome
small babies have small alveolar radii + no surfactant production
Respiratory Distress Syndrome literally means:
“A set of symptoms that occur together due to severe difficulty in breathing.”
Clinically, in infants (NRDS), it refers to:
lack of surfactant
high surface tension
alveolar collapse
poor gas exchange
Compliance of the Thorax and the Lungs Together
The compliance of the entire pulmonary system (the lungs and thoracic cage together) is measured while expanding the lungs of a totally relaxed or paralyzed person.
To do this, air is forced into the lungs a little at a time while recording lung pressures and volumes. To inflate this total pulmonary system, almost twice as much pressure as to inflate the same lungs after removal from the chest cage is necessary. Therefore, the compliance of the combined lung-thorax system is almost exactly one half that of the lungs alone—110 milliliters of volume per centimeter of water pressure for the combined system, compared with 200 ml/cm for the lungs alone. Furthermore, when the lungs are expanded to high volumes or compressed to low volumes, the limitations of the chest become extreme; when near these limits, the compliance of the combined lung-thorax system can be less than one fifth that of the lungs alone.
therefore, the thoracic cage decreases lung compliance.
“Work” of Breathing
during normal quiet breathing, what process using respiratory muscle contraction?
We have already pointed out that during normal quiet breathing, all respiratory muscle contraction occurs during inspiration; expiration is almost entirely a passive process caused by elastic recoil of the lungs and chest cage. Thus, under resting conditions, the respiratory muscles normally perform “work” to cause inspiration but not to cause expiration.
work of inspiration divided into three fractions
compliance work
tissue resistance work
airway resistance work
The work of inspiration (the energy your respiratory muscles must use to pull air into the lungs) can be divided into three fractions:
(1) that work required to expand the lungs against the lung and chest elastic forces, called compliance work or elastic work;
(2) that work required to overcome the viscosity of the lung and chest wall structures, called tissue resistance work
(3) that work required to overcome airway resistance to movement of air into the lungs, called airway resistance work.
(energy required for normal respiration)
energy required during normal respiration
energy required during heavy exercise
Energy Required for Respiration. During normal quiet respiration, only 3 to 5 percent of the total energy expended by the body is required for pulmonary ventilation.
But during heavy exercise, the amount of energy required can increase as much as 50-fold
especially if the person has any degree of increased airway resistance or decreased pulmonary compliance.
Therefore, one of the major limitations on the intensity of exercise that can be performed is the person’s ability to provide enough muscle energy for the respiratory process alone.
Pulmonary Volumes and Capacities
Pulmonary Volumes and Capacities
Recording Changes in Pulmonary Volume—Spirometry
spiro: “breathe”
metry: measure
can be studied by recording the volume movement of air into and out of the lungs, a method called spirometry.

Pulmonary Volumes (not pulmonary capacities)
tidal volume
inspiratory reserve volume
expiratory reserve volume
residual volume
the names tells you what the pumonary volumes are
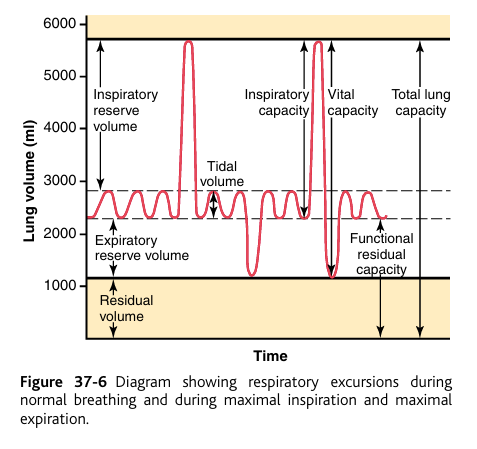
Pulmonary Volumes To the left in Figure 37-6 are listed four pulmonary lung volumes that, when added together, equal the maximum volume to which the lungs can be expanded. The significance of each of these volumes is the following:
1. The tidal volume (“The amount that rises and falls like a tide.”) is the volume of air inspired or expired with each normal breath; it amounts to about 500 milliliters in the adult male.
2. The inspiratory reserve volume is the extra volume of air that can be inspired over and above the normal tidal volume when the person inspires with full force; it is usually equal to about 3000 milliliters.
3. The expiratory reserve volume is the maximum extra volume of air that can be expired by forceful expiration after the end of a normal tidal expiration; this normally amounts to about 1100 milliliters.
4. The residual volume (residual= residing) is the volume of air remaining in the lungs after the most forceful expiration; this volume averages about 1200 milliliters

Pulmonary Capacities (not pulmonary volumes)
inspiratory capacity
functional residual capacity
vital capacity
total lung capacity
pulmonary capacities: two or more volumes together To the right in Figure 37-6 are listed the important pulmonary capacities, which can be described as follows:
1. The inspiratory capacity (“The amount the lungs can take in by breathing in”) equals the tidal volume plus the inspiratory reserve volume. This is the amount of air (about 3500 milliliters) a person can breathe in, beginning at the normal expiratory level and distending the lungs to the maximum amount.
2. The functional residual capacity (The amount remaining for normal function) equals the expiratory reserve volume plus the residual volume. This is the amount of air that remains in the lungs at the end of normal expiration (about 2300 milliliters).
3. The vital capacity (“The capacity essential for life”) equals the inspiratory reserve volume plus the tidal volume plus expiratory reserve volume. This is the maximum amount of air a person can expel from the lungs after first filling the lungs to their maximum extent and then expiring to the maximum extent (about 4600 milliliters).
vital capacity is another way to say the max amount of air a person can inhale and exhale after 1 breathe.
4. The total lung capacity (everything) is the maximum volume to which the lungs can be expanded with the greatest possible effort (about 5800 milliliters); it is equal to the vital capacity plus the residual volume. All pulmonary volumes and capacities are about 20 to 25 percent less in women than in men, and they are greater in large and athletic people than in small and asthenic people.
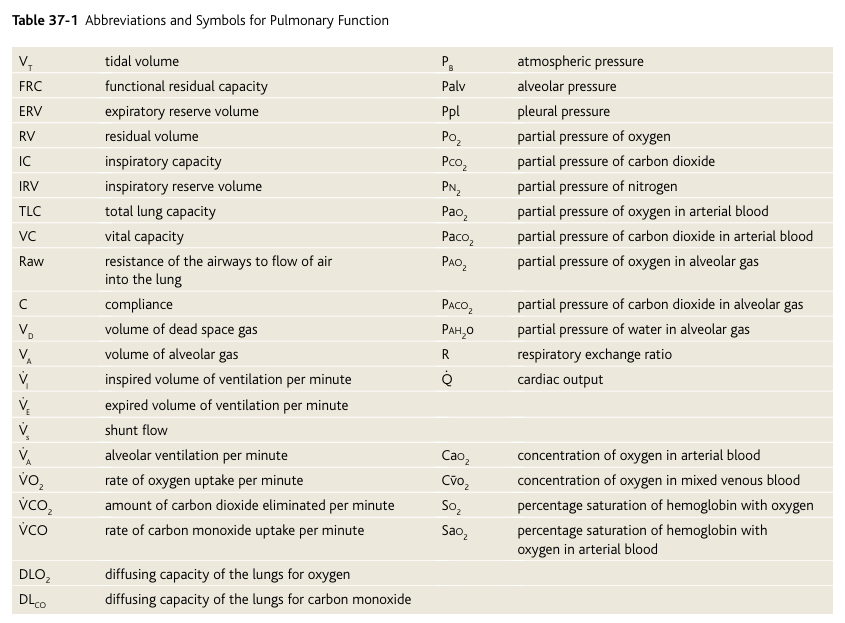
Abbreviations and Symbols Used in Pulmonary Function Studies
Spirometry is only one of many measurement procedures that the pulmonary physician uses daily. Many of these measurement procedures depend heavily on mathematical. computations. To simplify these calculations, as well as the presentation of pulmonary function data, several abbreviations and symbols have become standardized. The more important of these are given in Table 37-1. Using these symbols, we present here a few simple algebraic exercises showing some of the interrelations among the pulmonary volumes and capacities; the student should think through and verify these interrelations.
VC = IRV + VT + ERV
VC = IC + ERV
TLC = VC + RV
TLC = IC + FRC
FRC = ERV + RV
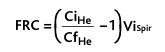
Helium dilution method and FRC
the helium dilution method is a way to determine the FRC.
The functional residual capacity (FRC), which is the volume of air that remains in the lungs at the end of each normal expiration, is important to lung function.
Because the FRC value changes markedly in some types of pulmonary disease, it is often desirable to measure this capacity.
The spirometer cannot be used in a direct way to measure the functional residual capacity because the air in the residual volume of the lungs cannot be expired into the spirometer, and this volume constitutes about one half of the functional residual capacity.
To measure functional residual capacity, the spirometer must be used in an indirect manner, usually by means of a helium dilution method, as follows. A spirometer of known volume is filled with air mixed with helium at a known concentration. Before breathing from the spirometer, the person expires normally. At the end of this expiration, the remaining volume in the lungs is equal to the functional residual capacity. At this point, the subject immediately begins to breathe from the spirometer, and the gases of the spirometer mix with the gases of the lungs. As a result, the helium becomes diluted by the functional residual capacity gases, and the volume of the functional residual capacity can be calculated from the degree of dilution of the helium, using the following formula: (look at the picture)
FRC= (CiHe/CfHe)ViSpi
Cᵢₕₑ = initial helium concentration in the spirometer
C𝒻ₕₑ = final helium concentration after mixing
Vᵢₛₚᵢ = volume of gas in the spirometer
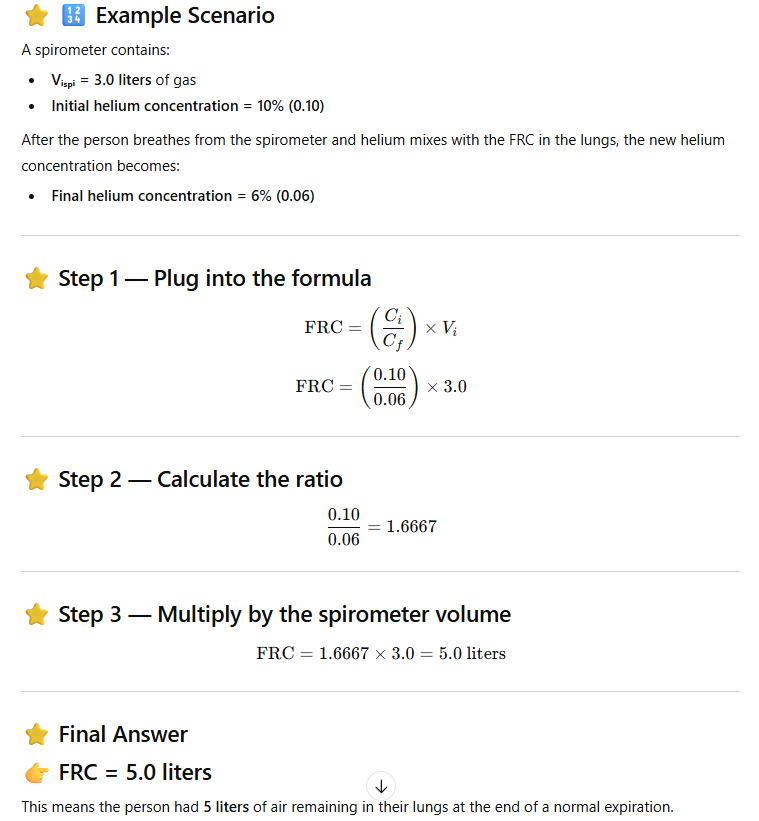
Once the FRC has been determined (by the helium dilution method) , the residual volume (RV) can be determined by subtracting expiratory reserve volume (ERV), as measured by normal spirometry, from the FRC. Also, the total lung capacity (TLC) can be determined by adding the inspiratory capacity (IC) to the FRC. That is RV = FRC - ERV and TLC = FRC + IC
RV= FRC-ERV
rv: the volume of air in lungs after MAX epiration
FRC: the volume of air in lungs after NORMAL expiration.
Minute Respiratory Volume Equals Respiratory Rate x Tidal Volume
The minute respiratory volume is the total amount of new air moved into the respiratory passages each minute; this is equal to the tidal volume x respiratory rate per minute. The normal tidal volume is about 500 mL, and the normal respiratory rate is about 12 breaths per minute.
500mL x 12 breathes per minute: 6L/min
Therefore, the minute respiratory volume averages about 6 L/min. A person can live for a short period with a minute respiratory volume as low as 1.5 L/min and a respiratory rate of only 2 to 4 breaths per minute. The respiratory rate occasionally rises to 40 to 50 per minute, and the tidal volume can become as great as the vital capacity, about 4600 milliliters in a young adult man. This can give a minute respiratory volume greater than 200 L/min, or more than 30 times normal. Most people cannot sustain more than one half to two thirds of these values for longer than 1 minute
Alveolar Ventilation
The rate at which new air reaches the alveoli, alveolar sacs, alveolar ducts, and respiratory bronchioles.
“Dead Space” and Its Effect on Alveolar Ventilation
dead space air: air that a person breathes but never reaches gas exchange, instead fills respiratory passages where gas exchange does not occur (nose, pharynx trachea). called “dead space air” because it’s not useful for gas exchange.
effect on alveolar ventilation: On expiration, the air in the dead space is expired first, before any of the air from the alveoli reaches the atmosphere. Therefore, the dead space is very disadvantageous for removing the expiratory gases from the lungs.
measurement of dead space volume (nitrogen)
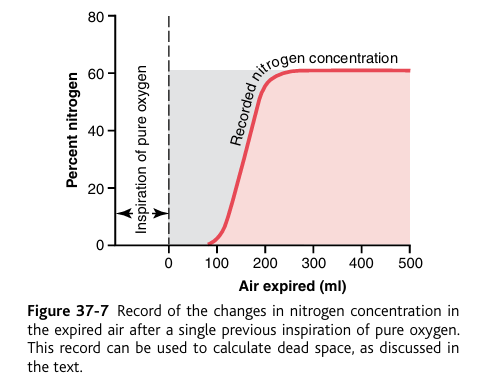
Measurement of the Dead Space Volume. A simple method for measuring dead space volume is demonstrated by the graph in Figure 37-7. In making this measurement, 1. the subject suddenly takes a deep breath of oxygen.
Goal of the test: measure the dead space
Measurement of the Dead Space Volume. A simple method for measuring dead space volume is demonstrated by the graph in Figure 37-7. In making this measurement, the sub ject suddenly takes a deep breath of oxygen. This fills the entire dead space with pure oxygen. Some oxygen also mixes with the alveolar air but does not completely replace this air. Then the person expires through a rapidly recording nitrogen meter, which makes the record shown in the figure. The first portion of the expired air comes from the dead space regions of the respiratory passageways, where the air has been com pletely replaced by oxygen. Therefore, in the early part of the record, only oxygen appears, and the nitrogen concentration is zero. Then, when alveolar air begins to reach the nitrogen meter, the nitrogen concentration rises rapidly, because alve olar air containing large amounts of nitrogen begins to mix with the dead space air. After still more air has been expired, all the dead space air has been washed from the passages and only alveolar air remains. Therefore, the recorded nitrogen concentration reaches a plateau level equal to its concentra tion in the alveoli, as shown to the right in the figure. With a little thought, the student can see that the gray area repre sents the air that has no nitrogen in it; this area is a measure of the volume of dead space air. For exact quantification, the following equation is used:
Anatomic Versus Physiologic Dead Space.
anatomic dead space
alveolar dead space
physiological dead space
1. Anatomic Dead Space (Normal, Structural)
This is the air that never reaches the alveoli.
It is simply the volume of the conducting airways:
nose
pharynx
larynx
trachea
bronchi
terminal bronchioles
These passages do not participate in gas exchange.
📌 Typical value:
~150 mL
This is what the nitrogen washout test measures.
⭐ 2. Alveolar Dead Space (Abnormal, Functional Problem)
Usually ALL alveoli participate in gas exchange.
But sometimes:
Some alveoli get air but not blood
This means they are ventilated but not perfused
So no gas exchange happens there
Examples:
Pulmonary embolism
Low pulmonary blood flow
Disease destroying capillaries
Shock
These alveoli behave like dead space even though they are alveoli, not airways.
3. Physiologic Dead Space = Anatomic + Alveolar
This is the total volume of wasted ventilation, meaning:
Air that enters the lungs
But does NOT participate in gas exchange
Physiologic Dead Space = Anatomic Dead Space + Alveolar Dead Space\textbf{Physiologic Dead Space = Anatomic Dead Space + Alveolar Dead Space}Physiologic Dead Space = Anatomic Dead Space + Alveolar Dead Space
4. What the passage is saying ✔ The helium dilution/nitrogen washout test measures anatomic dead space.
It measures only the conducting airways, because alveoli get mixed nitrogen and do not show the same zero-nitrogen signal.
✔ But if some alveoli are nonfunctional (no blood flow), these alveoli act like dead space.
So they must be included in the physiologic dead space.
✔ In a healthy person:
Anatomic dead space ≈ physiologic dead space
Because all alveoli are working.
✔ In lung disease:
Physiologic dead space can increase dramatically
Up to 10 times normal
Even 1–2 liters of wasted space
Rate of Alveolar Ventilation
what is the difference between alveolar ventilation and minute ventilation?
1. What is alveolar ventilation?
Alveolar ventilation = the amount of fresh air that actually reaches the alveoli (gas exchange areas) per minute.
This is the air that can actually exchange O₂ and CO₂ — not the air stuck in the dead space.
2. Why alveolar ventilation is NOT the same as minute ventilation
Minute ventilation = VT × respiratory rate
= total air moved in/out per minute
But some of that air is wasted in dead space.
Dead space air never reaches alveoli → no gas exchange.
So the lungs care about alveolar ventilation, not total ventilation.
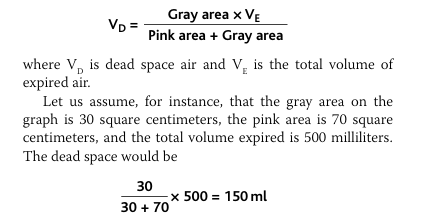
3. Formula for Alveolar Ventilation
VA=Respiratory Rate x (Vt-Vd)
Where:
Va = alveolar ventilation per minute
VT = tidal volume
VD = physiologic dead space
Respiratory rate (Freq) = breaths/min
Meaning:
You only count the portion of each breath that actually reaches the alveoli.
what is the alveolar ventilation?
tidal volume (Vd): 500mL
normal dead space: 150mL
respiratory rate: 12 breathes per minute
Thus, with a normal tidal volume of 500 milliliters, a normal dead space of 150 milliliters, and a respiratory rate of 12 breaths per minute, alveolar ventilation equals 12 × (500ml − 150ml), or 4200 ml/min
alveolar ventilation is useful for finding the concentrations of what gases in the alveoli?
Alveolar ventilation is one of the major factors deter mining the concentrations of oxygen and carbon dioxide in the alveoli.
Functions of the Respiratory Passageways
Trachea, Bronchi, and Bronchioles
what keeps the trachea from collapsing?
what keeps the walls of the bronchi from collapsing?
what keeps the bronchioles from collapsing?
Figure 37-8 shows the respiratory system, demonstrating especially the respiratory passageways.
The air is distributed to the lungs by way of the trachea, bronchi, and bronchioles.
One of the most important challenges in the respiratory passageways is to keep them open and allow easy passage of air to and from the alveoli.
To keep the trachea from collapsing, multiple cartilage rings extend about five sixths of the way around the trachea.
In the walls of the bronchi, less extensive curved cartilage plates also maintain a reasonable amount of rigidity yet allow sufficient motion for the lungs to expand and contract.
These plates become progressively less extensive in the later generations of bronchi and are gone in the bronchioles, which usually have diameters less than 1.5 millimeters. The bronchioles don’t have walls BUT are kept expanded by the same transpulmonary pressures that expand the alveoli. That is, as the alveoli enlarge, the bronchioles also enlarge, but not as much.

the bronchioles and alveoli don’t collapse and stay expanded due to ______
transpulmonary pressure
Muscular Wall of the trachea, Bronchi and Bronchioles and Its Control
what areas is the muscular wall located?
what areas is the muscular wall NOT located?
what is the most terminal bronchiole made of instead?
where do obstructive diseases from?
In all areas of the trachea and bronchi not occupied by cartilage plates, the walls are composed mainly of smooth muscle.
Also, the walls of the bronchioles are almost entirely smooth muscle, with the exception of the most terminal bronchiole (end of bronchiole), called the respiratory bronchiole, which is mainly pulmonary epithelium and underlying fibrous tissue plus a few smooth muscle fibers.
Many obstructive diseases (blockage) of the lung result from narrowing of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself.
Resistance to Airflow in the Bronchial Tree.
what is the condition of air flow in normal respiratory conditions?
in which area is the greatest amount of resistance to air flow?
why is the greatest amount of resistance to air flow in the larger bronchioles and bronchi?
in disease conditions, why do the smaller bronchioles play a greater role in determining air flow resistance?
Under normal respiratory conditions, air flows through the respiratory passageways so easily that less than 1 centimeter of water pressure gradient from the alveoli to the atmosphere is sufficient to cause enough airflow for quiet breathing. The greatest amount of resistance to airflow occurs not in the minute air passages of the terminal bronchioles but in some of the larger bronchioles and bronchi near the trachea. The reason for this high resistance is that there are relatively few of these larger bronchi in comparison with the approximately 65,000 parallel terminal bronchioles, through each of which only a minute amount of air must pass. Yet in disease conditions, the smaller bronchioles often play a far greater role in determining airflow resistance because of their small size and because they are easily occluded by (1) muscle contraction in their walls,
(2) edema occurring in the walls, or
(3) mucus collecting in the lumens of the bronchioles.
Nervous and Local Control of the Bronchiolar Musculature— “Sympathetic” Dilation of the Bronchioles.
which area of the lung is very much exposed to norepinephrine and epinephrine?
what receptor does norepinephrine and epinephrine bind to on the bronchial tree?
Direct control of the bronchioles by sympathetic nerve fibers is relatively weak because few of these fibers penetrate to the central portions of the lung.
However, the bronchial tree is very much exposed to norepinephrine and epinephrine released into the blood by sympathetic stimulation of the adrenal gland medullae. Both these hormones, especially epinephrine because of its greater stimulation of beta2-adrenergic receptors (B2), cause dilation of the bronchial tree.
sympathetic is “fight or flight”, which means the body needs oxygen, and if the body needs oxygen, the binding of norepinephrine and epinephrine upon the beta-adrenergic receptors will cause the bronchial tree to dilate (because oxygen is needed).
T1–T5 → sympathetic chain → pulmonary plexus
Parasympathetic Constriction of the Bronchioles.
vagus nerve
lung parenchyma
acetylcholine
Parasympathetic Constriction of the Bronchioles.
A few parasympathetic nerve fibers derived from the vagus nerves (CN X) penetrate the lung parenchyma.
the lung parenchyma is NOT the same as the bronchial tree.
lung parenchyma:
para- =beside, alongside
enchein= to pour in / that which is poured in
So parenchyma means: “the substance that fills the organ.”
These nerves secrete acetylcholine and, when activated, cause mild to moderate constriction of the bronchioles.
acetylcholine binds to M3 receptors to cause bronchoconstriction.
When a disease process such as asthma has already caused some bronchiolar constriction, superimposed parasympathetic nervous stimulation often worsens the condition. When this occurs, administration of drugs that block the effects of acetylcholine, such as atropine, can sometimes relax the respiratory passages enough to relieve the obstruction.
Sometimes the parasympathetic nerves are also activated by reflexes that originate in the lungs. Most of these begin with irritation of the epithelial membrane of the respiratory passageways themselves, initiated by noxious gases, dust, cigarette smoke, or bronchial infection. Also, a bronchiolar constrictor reflex often occurs when microemboli occlude small pulmonary arteries.
atropine
m3 blocker (blocks binding of acetylcholine= blocks bronchoconstriction)
atropine causes bronchodilation.
used as treatment for obstructive lung diseases.
Local Secretory Factors Often Cause Bronchiolar Constriction.
histamine
anaphylaxis
mast cells
Several substances formed in the lungs are often quite active in causing bronchiolar constriction.
Two of the most important of these are histamine and slow reactive substance of anaphylaxis.
Both of these are released in the lung tissues by mast cells during allergic reactions, especially those caused by pollen in the air.
Therefore, they play key roles in causing the airway obstruction that occurs in allergic asthma; this is especially true of the slow reactive substance of anaphylaxis.
The same irritants that cause parasympathetic constrictor reflexes of the airways—smoke, dust, sulfur dioxide, and some of the acidic elements in smog—often act directly on the lung tissues to initiate local, non-nervous reactions that cause obstructive constriction of the airways.
Term | Root Meaning | Literal Translation | Why Named This |
|---|---|---|---|
Histamine | histos + amine | “tissue amine” | Found in tissues as an amine compound, causes BRONCHOCONSTRCTION |
Anaphylaxis | ana + phylaxis | “against protection” | Reaction opposite of protective immunity, causes extreme BRONCHOCONSTRICTION. |
Mast cell | Mastzelle (German) | “fattened cell” | Cells look stuffed with granules, release histamine and anaphylaxes |
Mucus Lining the Respiratory Passageways, and Action of Cilia to Clear the Passageways
what does mucous do?
by what cells secret mucous?
All the respiratory passages, from the nose to the terminal bronchioles, are kept moist by a layer of mucus that coats the entire surface.
The mucus is secreted partly by individual mucous goblet cells in the epithelial lining of the passages and partly by small submucosal glands.
In addition to keeping the surfaces moist, the mucus traps small particles out of the inspired air and keeps most of these from ever reaching the alveoli.
The mucus itself is removed from the passages in the following manner. The entire surface of the respiratory passages, both in the nose and in the lower passages down as far as the terminal bronchioles, is lined with ciliated epithelium, with about 200 cilia on each epithelial cell. These cilia beat continually at a rate of 10 to 20 times per second by the mechanism explained in Chapter 2, and the direction of their “power stroke” is always toward the pharynx. That is, the cilia in the lungs beat upward, whereas those in the nose beat downward. This continual beating causes the coat of mucus to flow slowly, at a velocity of a few millimeters per minute, toward the pharynx. Then the mucus and its entrapped particles are either swallowed or coughed to the exterior.
Cough Reflex
The bronchi and trachea are so sensitive to light touch that slight amounts of foreign matter or other causes of irritation initiate the cough reflex.
The larynx and carina (the point where the trachea divides into the bronchi) are especially sensitive, and the terminal bronchioles and even the alveoli are sensitive to corrosive chemical stimuli such as sulfur dioxide gas or chlorine gas.
Afferent nerve impulses pass from the respiratory passages mainly through the vagus nerves to the medulla of the brain. There, an automatic sequence of events is triggered by the neuronal circuits of the medulla, causing the following effect.
First, up to 2.5 liters of air are rapidly inspired.
Second, the epiglottis closes, and the vocal cords shut tightly to entrap the air within the lungs.
Third, the abdominal muscles contract forcefully, pushing against the diaphragm while other expiratory muscles, such as the internal intercostals, also contract forcefully. Consequently, the pressure in the lungs rises rapidly to as much as 100 mm Hg or more. (very strong expiration)
Fourth, the vocal cords and the epiglottis suddenly open widely, so that air under this high pressure in the lungs explodes outward.
Indeed, sometimes this air is expelled at velocities ranging from 75 to 100 miles per hour. Importantly, the strong compression of the lungs collapses the bronchi and trachea by causing their noncartilaginous parts to invaginate inward, so the exploding air actually passes through bronchial and tracheal slits. The rapidly moving air usually carries with it any foreign matter that is present in the bronchi or trachea.
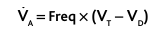
Sneeze Reflex
The sneeze reflex is very much like the cough reflex, except that the sneeze reflex applies to the nasal passageways instead of the lower respiratory passages.
The initiating stimulus of the sneeze reflex is irritation in the nasal passageways;
the afferent impulses pass in the fifth cranial nerve to the medulla, where the reflex is triggered.
A series of reactions similar to those for the cough reflex takes place; however, the uvula is depressed, so large amounts of air pass rapidly through the nose, thus helping to clear the nasal passages of foreign matter.
Uvula = “little grape”
what is the difference between the cough reflex and the sneeze reflex?
cough reflex are irritants in the respiratory passage
sneeze reflex are irritants in the nasal passage.
you sneeze to get the irritants out of the NOSE.
Normal Respiratory Functions of the Nose (air conditioning function)
warming
humidified
partially filtered
As air passes through the nose, three distinct normal respiratory functions are performed by the nasal cavities: (1) the air is warmed by the extensive surfaces of the conchae and septum, a total area of about 160 square centimeters (see Figure 37-8);
(2) the air is almost completely humidified even before it passes beyond the nose.
(3) the air is partially filtered.
These functions together are called the air conditioning function of the upper respiratory passageways. Ordinarily, the temperature of the inspired air rises to within 1°F of body temperature and to within 2 to 3 percent of full saturation with water vapor before it reaches the trachea. When a person breathes air through a tube directly into the trachea (as through a tracheostomy), the cooling and especially the drying effect in the lower lung can lead to serious lung crusting and infection.
Filtration Function of the Nose.
large hairs in the nose
turbulent precipitation
The hairs at the entrance to the nostrils are important for filtering out large particles.
Much more important, though, is the removal of particles by turbulent precipitation.
That is, the air passing through the nasal passageways hits many obstructing vanes: the conchae (also called turbinates, because they cause turbulence of the air); the septum; and the pharyngeal wall.
Each time air hits one of these obstructions, it must change its direction of movement.
The particles suspended in the air, having far more mass and momentum than air, cannot change their direction of travel as rapidly as the air can.
Therefore, they continue forward, striking the surfaces of the obstructions, and are entrapped in the mucous coating and transported by the cilia to the pharynx to be swallowed.
Size of Particles Entrapped in the Respiratory Passages
nasal turbulence
gravitational precipitation
terminal bronchiolar disease, coal miners, settled dust particles
The nasal turbulence mechanism for removing particles from air is so effective that almost no particles larger than 6 micrometers in diameter enter the lungs through the nose. This size is smaller than the size of red blood cells.
Of the remaining particles, many that are between 1 and 5 micrometers settle in the smaller bronchioles as a result of gravitational precipitation. For instance, terminal bronchiolar disease is common in coal miners because of settled dust particles. Some of the still smaller particles (smaller than 1 micrometer in diameter) diffuse against the walls of the alveoli and adhere to the alveolar fluid. But many particles smaller than 0.5 micrometer in diameter remain suspended in the alveolar air and are expelled by expiration. For instance, the particles of cigarette smoke are about 0.3 micrometer. Almost none of these particles are precipitated in the respiratory passageways before they reach the alveoli. Unfortunately, up to one third of them do precipitate in the alveoli by the diffusion process, with the balance remaining suspended and expelled in the expired air.
Many of the particles that become entrapped in the alveoli are removed by alveolar macrophages, as explained in Chapter 33, and others are carried away by the lung lymphatics. An excess of particles can cause growth of fibrous tissue in the alveolar septa, leading to permanent debility.
Vocalization
cerebral cortex
respiratory control centers of the brain
articulation and resonance structures of mouth and nasal cavities
phonation, larynx
articulation, mouth
Speech involves not only the respiratory system but also
(1) specific speech nervous control centers in the cerebral cortex
(2) respiratory control centers of the brain
(3) the articulation and resonance structures of the mouth and nasal cavities.
Speech is composed of two mechanical functions: (1) phonation, which is achieved by the larynx, and (2) articulation, which is achieved by the structures of the mouth.
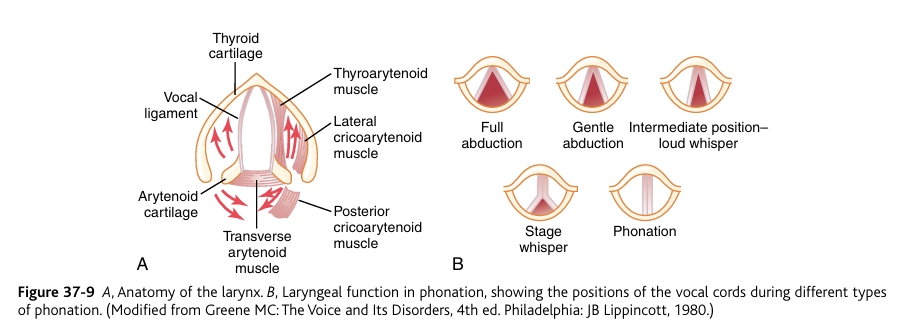
Phonation.
Phonation is the process of producing sound through the vibration of the vocal cords in the larynx, driven by air pressure from the lungs
The larynx, shown in Figure 37-9A, is especially adapted to act as a vibrator. The vocal cords are the vibrating element. The vocal cords protrude from the lateral walls of the larynx toward the center of the glottis; they are stretched and positioned by several specific muscles of the larynx itself.
Figure 37-9B shows the vocal cords as they are seen when looking into the glottis with a laryngoscope. During normal breathing, the cords are wide open to allow easy passage of air.
During phonation, the cords move together so that passage of air between them will cause vibration.
The pitch of the vibration is determined mainly by the degree of stretch of the cords, but also by how tightly the cords are approximated to one another and by the mass of their edges.
Figure 37-9A shows a dissected view of the vocal folds after removal of the mucous epithelial lining. Immediately inside each cord is a strong elastic ligament called the vocal ligament. This is attached anteriorly to the large thyroid cartilage, which is the cartilage that projects forward from the anterior sur face of the neck and is called the “Adam’s apple.” Posteriorly, the vocal ligament is attached to the vocal processes of two arytenoid cartilages. The thyroid cartilage and the arytenoid cartilages articulate from below with another cartilage not shown in Figure 37-9, the cricoid cartilage.
The vocal cords can be stretched by either forward rotation of the thyroid cartilage or posterior rotation of the arytenoid cartilages, activated by muscles stretching from the thyroid cartilage and arytenoid cartilages to the cricoid cartilage. Muscles located within the vocal cords lateral to the vocal ligaments, the thyroarytenoid muscles, can pull the arytenoid cartilages toward the thyroid cartilage and, therefore, loosen the vocal cords. Also, slips of these muscles within the vocal cords can change the shapes and masses of the vocal cord edges, sharpening them to emit high-pitched sounds and blunting them for the more bass sounds.
Several other sets of small laryngeal muscles lie between the arytenoid cartilages and the cricoid cartilage and can rotate these cartilages inward or outward or pull their bases together or apart to give the various configurations of the vocal cords shown in Figure 37-9B.
organs of articulation
lips
tongue
soft palate
The three major organs of articulation are the lips, tongue, and soft palate.
CHAPTER 38
Pulmonary Circulation, Pulmonary Edema, Pleural Fluid
the lung has two circulations:
A high-pressure, low-flow circulation (bronchial artery, the lung blood flow itself)
A low-pressure, high-flow circulation (pulmonary artery and pulmonary veins TO ALVEOLI)
The lung has two circulations:
(1) A high-pressure, low-flow circulation (bronchial artery, the lung blood flow itself)
-(bronchial arteries) supplies systemic arterial blood to the trachea, the bronchial tree including the terminal bronchioles, the supporting tissues of the lung, and the outer coats (adventia) of the pulmonary arteries and veins. (NOT ALVEOLI)
high pressure in bronchial arteries because Systemic arteries = high-pressure system (~120/80 mmHg), so bronchial arteries inherit the high pressure system
low flow because the lung tissues themselves need very little blood supply because most of the oxygen for lungs comes from alveolar gas exchange, not blood flow
(2) A low-pressure, high-flow circulation (pulmonary artery and pulmonary veins TO ALVEOLI)
-carried out by the pulmonary artery and its branches
-the pulmonary artery receives blood from the right ventricle.
-pulmonary artery supplies venous blood (deoxygenated blood) from all parts of the body to the alveolar capillaries where oxygen is added and carbon dioxide is removed.
-pulmonary veins then return the blood to the left atrium to be pumped by the left ventricle through the systemic circulation.
Low pressure
Pulmonary artery pressure ≈ 15/8 mmHg (much lower than systemic arteries ~120/80)
Needed to protect delicate alveolar capillaries from rupture
Prevents pulmonary edem
High flow
Pulmonary artery carries the entire cardiac output (5 L/min at rest, more during exercise)
Every drop of venous blood must pass through the lungs to be oxygenated.

Physiologic Anatomy of the Pulmonary Circulatory System
Physiologic Anatomy of the Pulmonary Circulatory System
(Pulmonary Vessels)
pulmonary artery
why do pulmonary arteries have a large compliance?
what is the similarity between pulmonary arteries and pulmonary veins?
The pulmonary artery divides into right and left main branches that supply blood to the two respective lungs.
The pulmonary artery is thin, with a wall thickness one third that of the aorta. The pulmonary arterial branches are very short, and all the pulmonary arteries, even the smaller arteries and arterioles, have larger diameters than their counterpart systemic arteries.
This, combined with the fact that the vessels are thin and distensible, gives the pulmonary arterial tree a large compliance, averaging almost 7 ml/mm Hg, which is similar to that of the entire systemic arterial tree. This large compliance allows the pulmonary arteries to accommodate the stroke volume output of the right ventricle.
The pulmonary veins immediately empty their effluent blood into the left atrium.
pulmonary veins are also short like the pulmonary arteries.
Bronchial Vessels.
Blood also flows to the lungs through small bronchial arteries that originate from the systemic circulation, amounting to about 1 to 2 percent of the total cardiac output.
This bronchial arterial blood is oxygenated blood, in contrast to the partially deoxygenated blood in the pulmonary arteries.
bronchial arteries supplies the supporting tissues of the lungs, including the connective tissue, septa, and large and small bronchi.
bronchial arterial blood, after passing through the lungs, empties into the pulmonary veins and enters the left atrium, instead of passing back to the right atrium.
Therefore, the flow into the left atrium and the left ventricular output are about 1 to 2 percent greater than that of the right ventricular output
Lymph vessels in lungs
the lymph vessels begin____, course to the _____, and mainly into the _____.
what kind of matter (2) is partly removed by lymph channels?
Lymph vessels are present in all the supportive tissues of the lung, beginning in the connective tissue spaces that surround the terminal bronchioles, coursing to the hilum of the lung, and then mainly into the right thoracic lymph duct.
Particulate matter entering the alveoli is partly removed by way of these channels, and plasma protein leaking from the lung capillaries is also removed from the lung tissues, thereby helping to prevent pulmonary edema.
particulate matter and plasma protein is emptied from the lungs by lymph ducts.
Pressures in the Pulmonary System
Pressures in the Pulmonary System
Pressure Pulse Curve in the Right Ventricle.
The pressure pulse curves of the right ventricle and pulmonary artery are shown in the lower portion of Figure 38-1.
the right ventricle sends blood through the pulmonary artery.
y-axis: pressure
x-axis: seconds
These curves are contrasted with the much higher aortic pressure curve shown in the upper portion of the figure. The systolic pressure in the right ventricle of the normal human being averages about 25 mm Hg, and the diastolic pressure averages about 0 to 1 mm Hg, values that are only one-fifth those for the left ventricle.
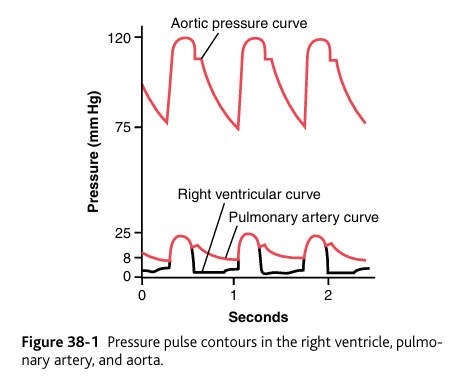
Pressures in the Pulmonary Artery.
during what phase (systole or diastole) is the pressure in the pulmonary artery equal to the pressure in the right ventricle?
during what phase is (systole or diastole) does the ventricular pressure fall precipitously and the pulmonary arterial pressure falls more slowly?
During systole, the pressure in the pulmonary artery is essentially equal to the pressure in the right ventricle, as also shown in Figure 38-1.
during diastole, the ventricular pressure falls precipitously, whereas the pulmonary arterial pressure falls more slowly as blood flows through the capillaries of the lungs. As shown
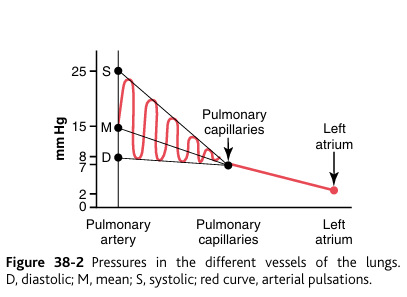
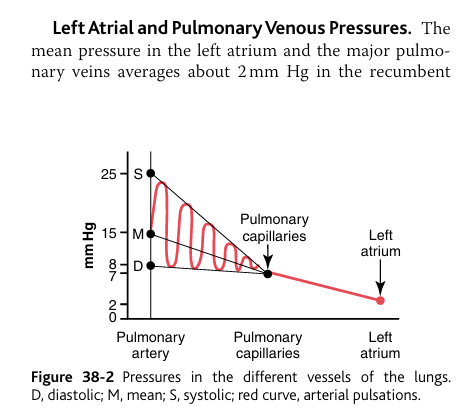
in Figure 38-2, the systolic pulmonary arterial pressure averages about 25 mm Hg in the normal human being, the diastolic pulmonary arterial pressure is about 8 mm Hg, and the mean pulmonary arterial pressure is 15 mm Hg.
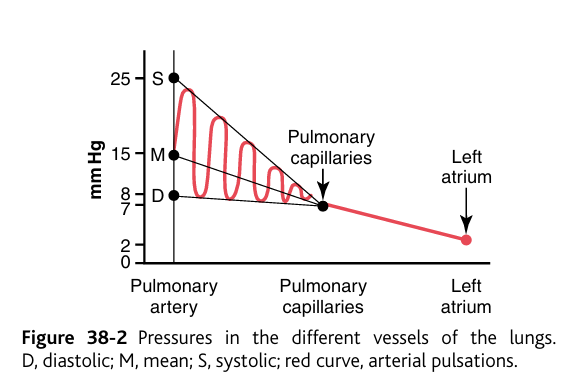
Pulmonary Capillary Pressure.
The mean pulmonary capillary pressure, as diagrammed in Figure 38-2, is about 7 mm Hg. The importance of this low capillary pressure is discussed in detail later in the chapter in relation to fluid exchange functions of the pulmonary capillaries.
(Left Atrial and Pulmonary Venous Pressures.)
pulmonary wedge pressure
what is the relationship between left atrial pressure and pulmonary venous pressure (direct).
It usually is not feasible to measure a human being’s left atrial pressure using a direct measuring device because it is difficult to pass a catheter through the heart chambers into the left atrium.
the pulmonary wedge pressure can be used to estimate the left atrial pressure with moderate accuracy.
pulmonary: lung
wedge: “to force into a tight space”
pulmonary wedge pressure is achieved by:
inserting a catheter through a peripheral vein to the right atrium,
through the right side of the heart
through the pulmonary artery into one of the small branches of the pulmonary artery, finally pushing the catheter until it wedges tightly in the small branch of the pulmonary artery.
The pressure measured through the catheter, called the “wedge pressure,” is about 5 mm Hg.
Because all blood flow has been stopped in the small wedged artery, and because the blood vessels extending beyond this artery make a direct connection with the pulmonary capillaries, this wedge pressure is usually only 2 to 3 mm Hg greater than the left atrial pressure, so in reality, the left atrial pressure is 3mmHG or 2mmHG.
When the left atrial pressure rises to high values, the pulmonary wedge pressure also rises (direct relationship)
Therefore, wedge pressure measurements can be used to clinically study changes in pulmonary capillary pressure and left atrial pressure in patients with congestive heart failure.
Blood Volume of the Lung
Blood Volume of the Lung
The Lungs Serve as a Blood Reservoir.
Under various physiological and pathological conditions, the quantity of blood in the lungs can vary from as little as one-half normal up to twice normal. For instance, when a person blows out air so hard that high pressure is built up in the lungs—such as when blowing a trumpet—as much as 250 milliliters of blood can be expelled from the pulmonary circulatory system into the systemic circulation. Also, loss of blood from the systemic circulation by hemorrhage can be partly compensated for by the automatic shift of blood from the lungs into the systemic vessels.
Cardiac Pathology May Shift Blood from the Systemic Circulation to the Pulmonary Circulation.
Failure of the left side of the heart or increased resistance to blood flow through the mitral valve as a result of mitral stenosis or mitral regurgitation causes blood to dam up in the pulmonary circulation, sometimes increasing the pulmonary blood volume as much as 100 percent and causing large increases in the pulmonary vascular pressures.
Because the volume of the systemic circulation is about nine times that of the pulmonary system, a shift of blood from one system to the other affects the pulmonary system greatly but usually has only mild systemic circulatory effects.
Blood Flow Through the Lungs and Its Distribution
what is the relationship between blood flow in the lungs and cardiac output?
The blood flow through the lungs is essentially equal to the cardiac output.
Therefore, the factors that control cardiac output—mainly peripheral factors, as discussed in Chapter 20—also control pulmonary blood flow.
Under most conditions, the pulmonary vessels act as passive, distensible tubes that enlarge with increasing pressure and narrow with decreasing pressure.
For adequate aeration of the blood to occur, it is important for the blood to be distributed to those segments of the lungs where the alveoli are best oxygenated. This is achieved by the fol lowing mechanism.