15-Embryology of Reproductive Tract
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
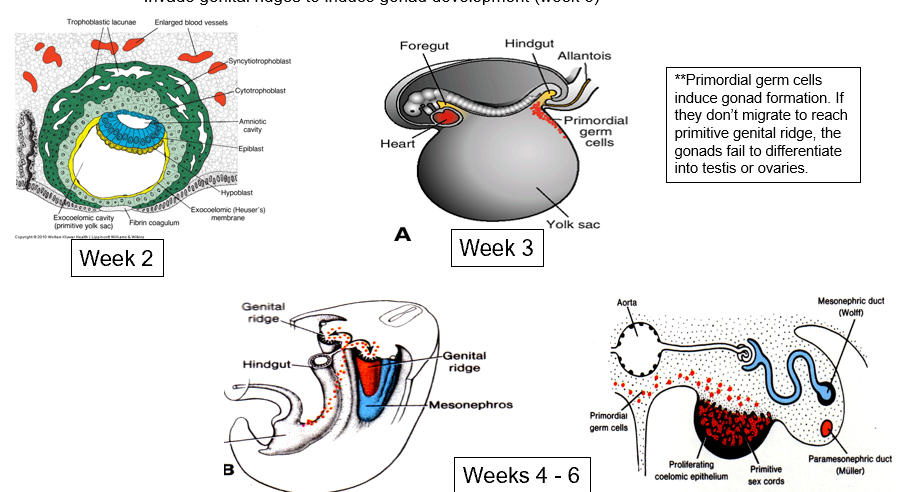
Primordial Germ Cells
Arise from the epiblast and migrate into primitive streak ( 2nd week)
Migrate into the endoderm of yolk sac near allantois (week 3)
Migrate along dorsal mesentery of hindgut (week 4)
Arrive at genital ridge beginning (week 5)
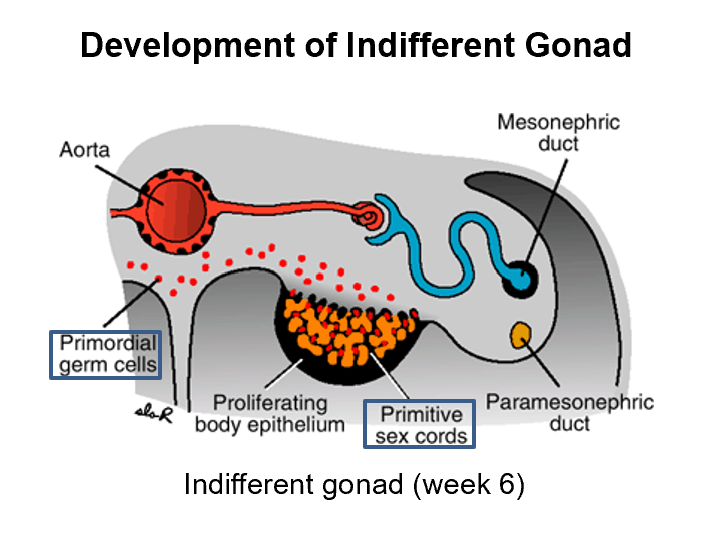
Invade genital ridges to induce gonad development (week 6)
They induce gonad formation!
Intermediate mesoderm
Internal Genitalia origin
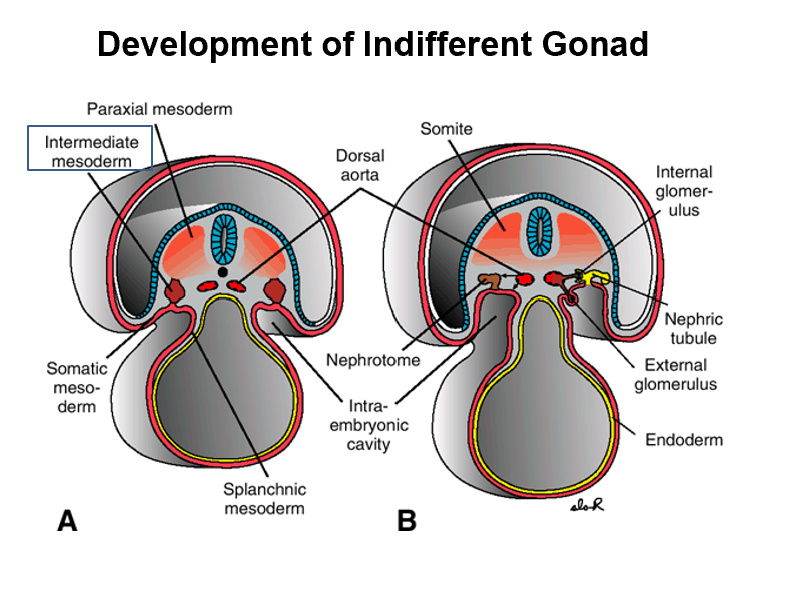
Somatopleure
External genitalia origin
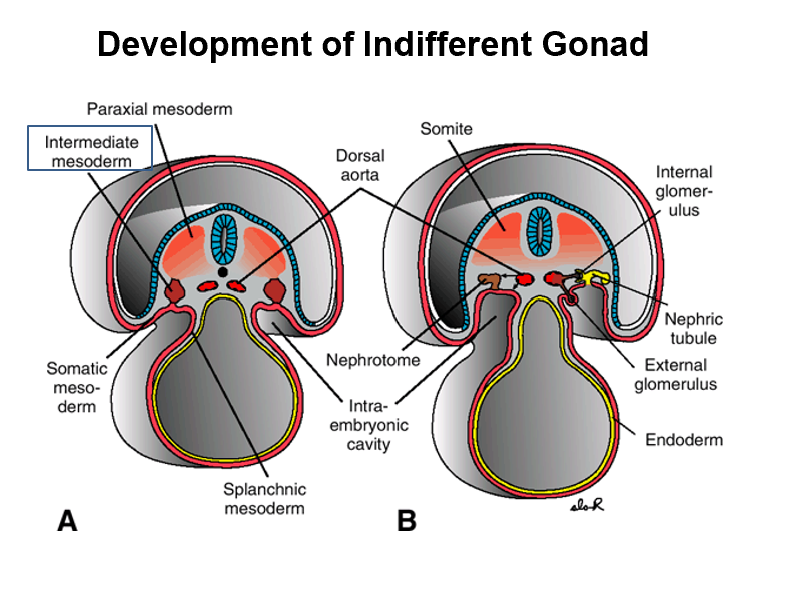
Genital Ridge
Forms the gonads
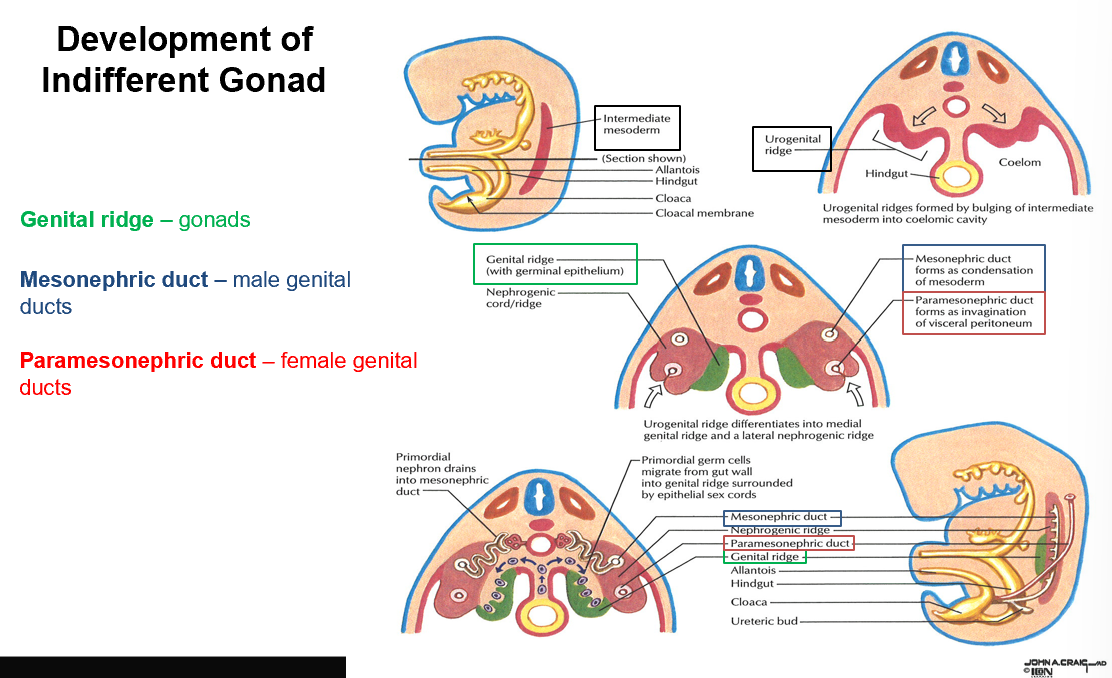
Mesonephric Duct
Forms the male genital ducts
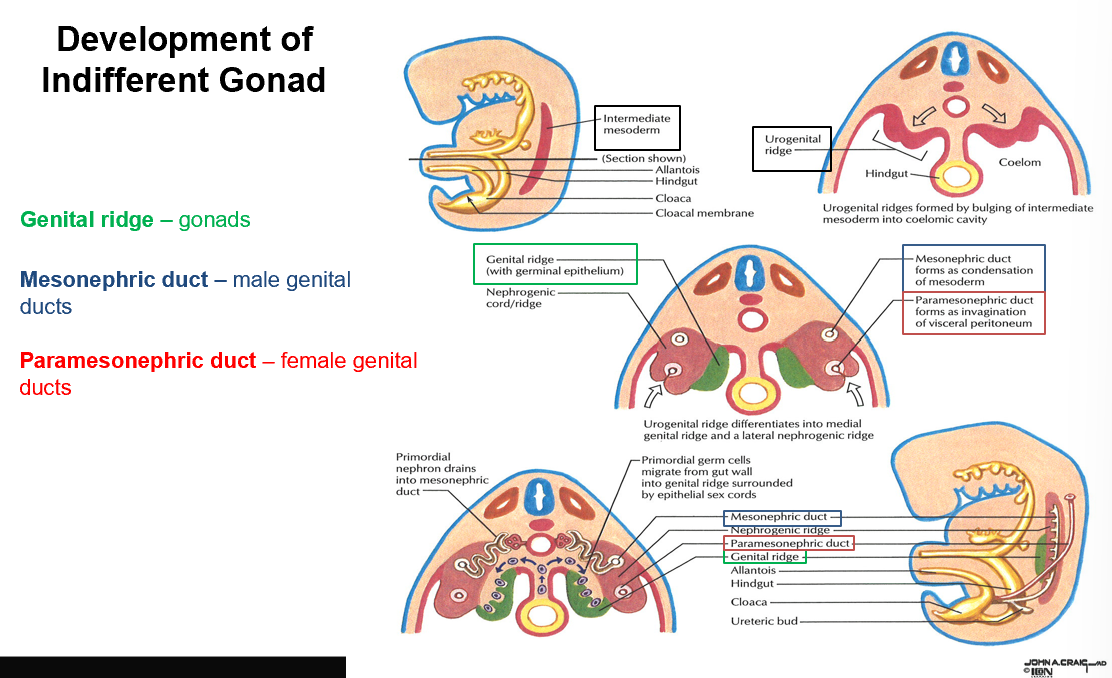
Paramesonephric Duct
Forms the female genital ducts
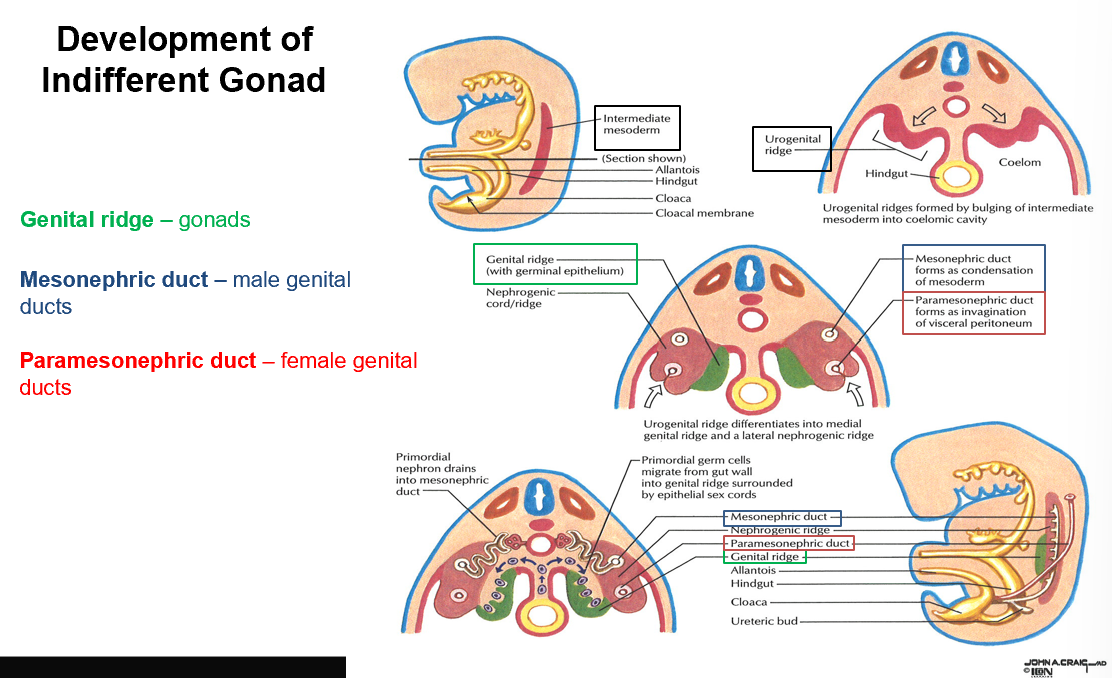
Indifferent Gonad
Primordial germs cells move up and invade THIS.
These germ cells also form primitive sex cords.
Both male and female karyotypes form THIS!
Indifferent Gonad Differentiation
In order to differentiate the indifferent gonad, you need a Y chromosome present. Otherwise, you form female genitalia like “normal”.
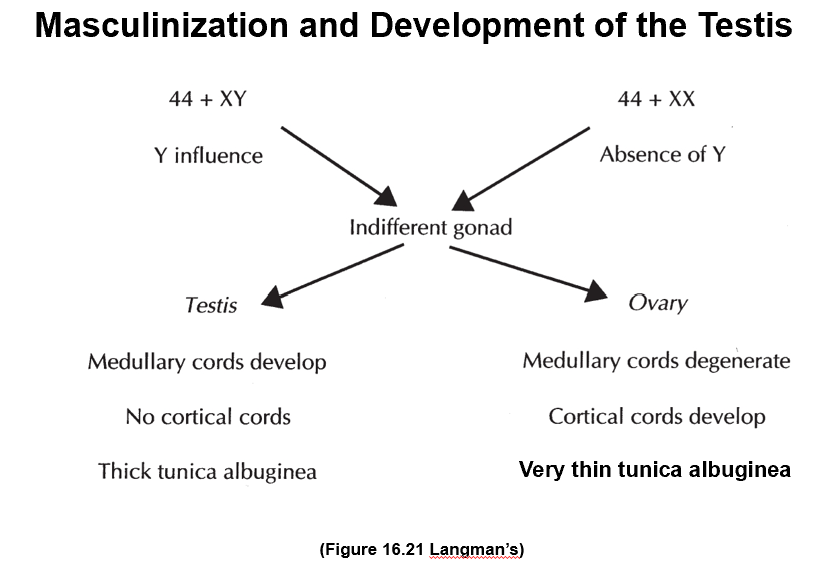
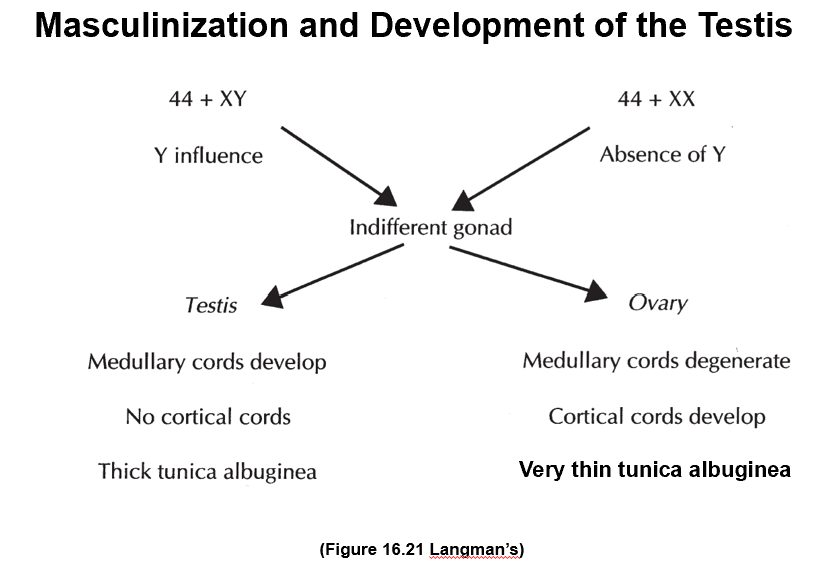
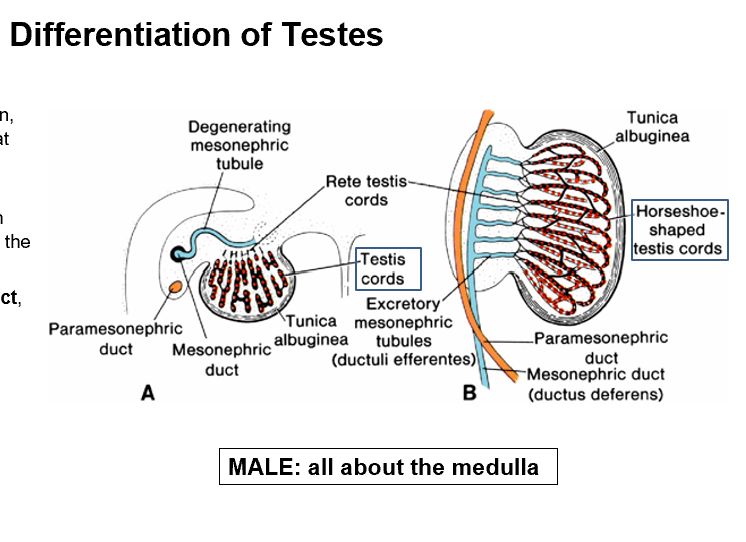
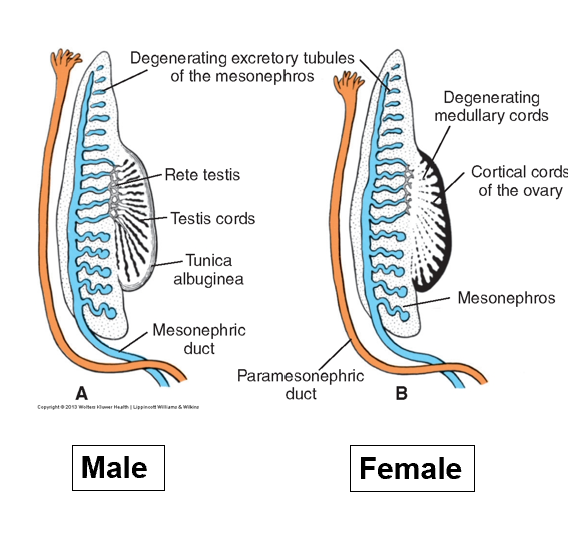
Testis Development
Presence of Y chromosome → Forms Testis
Medullary cords develop
No cortical cords
Thick tunica albuginea
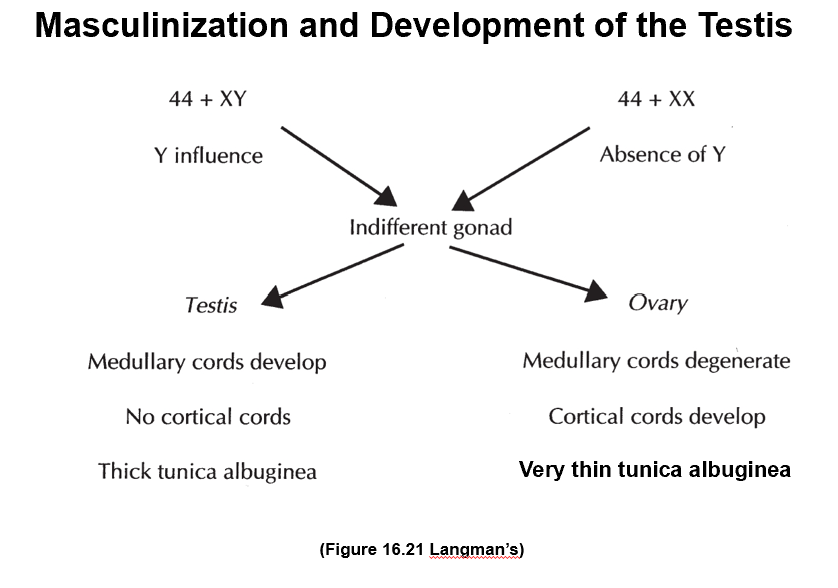
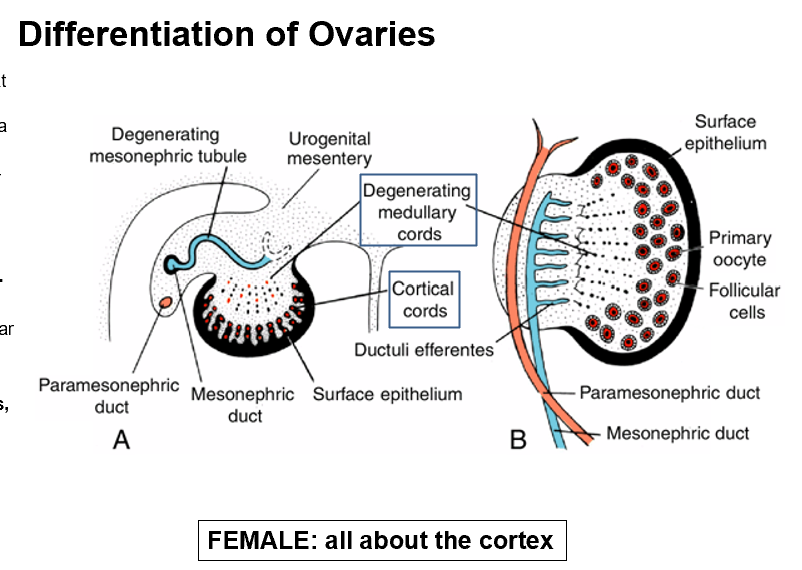
Ovary Development
No Y chromosome present → Forms ovary
Medullary cords degenerate
Cortical cords develop
Very thin tunica albuginea
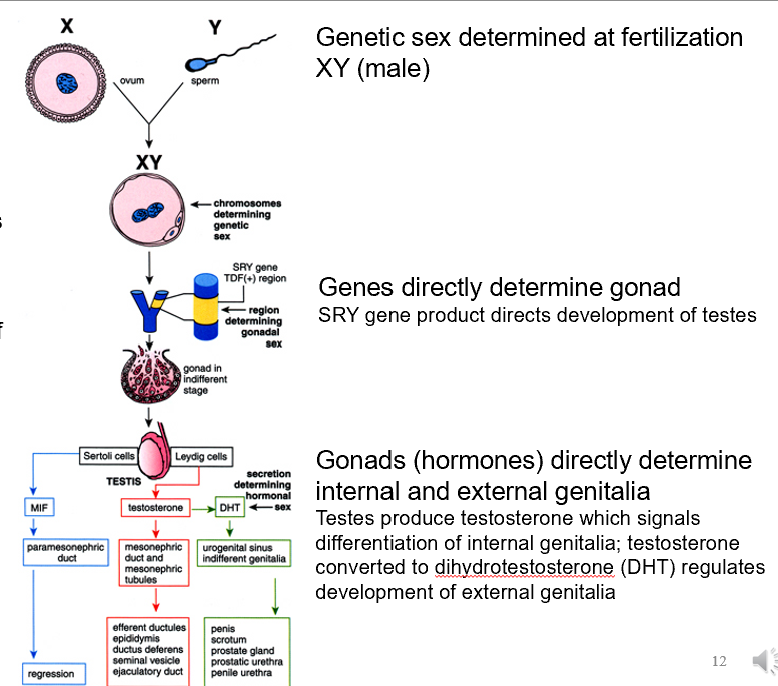
Masculinization of the testis
Sperm and Ovum (Y and X) come together and form XY embryo
Y chromosome contains SRY gene that produces TDF (testis-determining factor)
TDF induces further development of the testes
After inducing, Sertoli cells produce MIF (malarian inhibiting factor)
Causes degeneration of paramesonephric duct
Creates the Male Reproductive Tract
After inducing, Leydig Cells produce testosterone
Creates mesonephric duct and tubules
Testosterone makes the internal structures but also produces DHT (dihydrotestosterone) which creates the external genitalia
Differentiation of Testes
Primordial germ cells invade genital ridge
After testosterone is made, primordial germ cells further differentiate deep into the medulla → forming testis (medullary) cords
These cords become Rete Testis Cords around month 4 (connecting old mesonephric tubules to testis cords)
Surface epithelium on the testis gives rise to sustentacular cells of Sertoli, which produce antimüllerian hormone (AMH/MIH).
Paramesonephric ducts degenerate
Gonadal ridge mesenchyme forms interstitial cells of Leydig that reside between testis cords and begin to produce testosterone at week 8
Allowing testis to influence sexual differentiation of genital ducts.
Dense fibrous connective tissue, tunica albuginea, will form and separate testis cords from the surface epithelium after the cortex regresses.
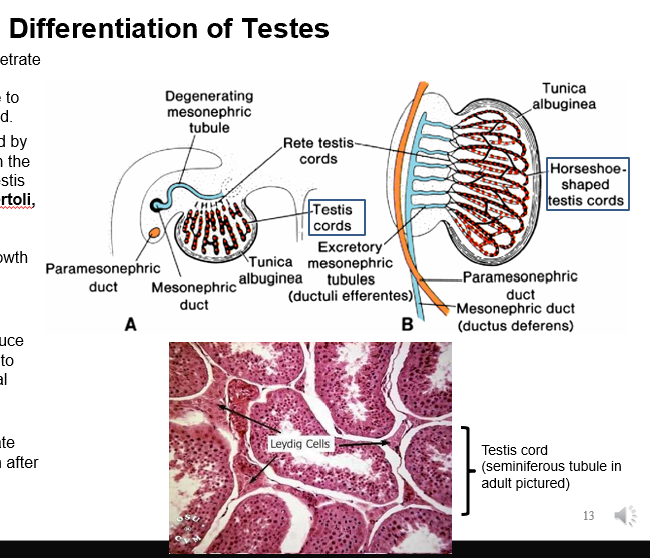
Puberty
THIS is when testis cords acquire a lumen
Forming the seminiferous tubules that join the rete testis tubules.
Rete testis tubules drain to ductuli efferentes, or efferent ductules, which are the remaining excretory tubules of the mesonephric kidney.
Efferent ductules drain to Wolffian duct, which becomes the ductus deferens.
Differentiation of Ovaries
XX chromosomes at fertilization
Determine gonad (development of ovaries)
Ovaries form in the absence of TDF, AMH, and Testosterone
Further becoming Mullerian duct → Female Internal Genitalia
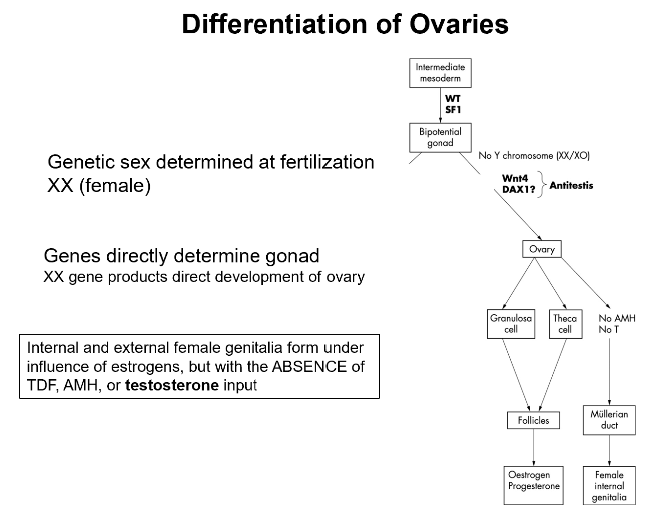
Ovary Differentiation Steps
Week 7, primordial germ cells arrive at the genital ridge, they differentiate into oogonia.
Primitive sex cords dissociate into irregular clusters in the medullary part of the gonad that contain groups of oogonia.
Some medullary oogonia divide mitotically and grow in size forming primary oocytes.
Medullary clusters (with oogonia/oocytes) later disappear and are replaced by vascular stroma forming the ovarian medulla.
Surface epithelium proliferates to form a second generation of cords, cortical cords, that penetrate underlying mesenchyme in Week 7.
Cortical cords split into isolated clusters in Weeks 9 & 10.
Cells proliferate within clusters to surround remaining primary oocytes with layer of epithelial cells, follicular cells.
Primary oocyte + follicular cells = primordial follicle.
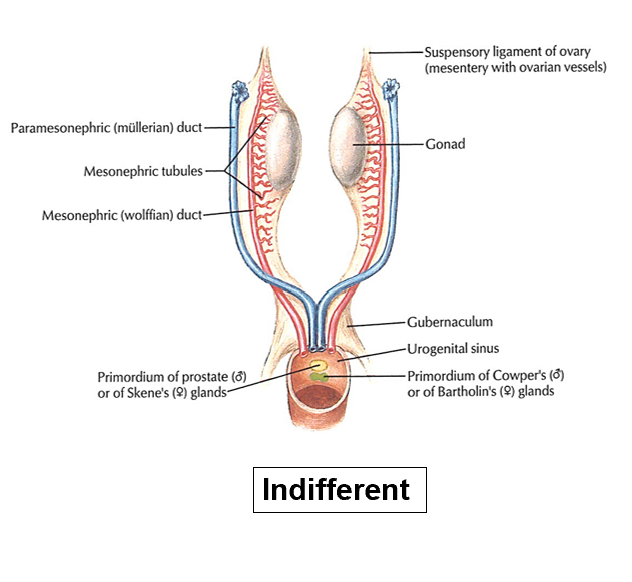
Genital Ducts: Indifferent (what it becomes)
Paramesonephric ducts come together caudally to enter urogenital sinus.
Note: gonad in both M and F is tethered to the posterior abdominal wall by mesenchyme!
In M: Cranial Gonadal Ligament will disappear later to allow the testes to descend.
In F: Cranial Gonadal Ligament will remain and become Suspensory Ligament of Ovary.
In M: Caudal Gonadal Ligament forms Gubernaculum (pulls testes down into scrotum).
In F: Caudal Gonadal Ligament forms Gubernaculum which becomes Ovarian Ligament Proper & Round Ligament of Uterus
Medulla of the gonad
In the female, the THIS has degenerated and turned into the vascular stroma. In males it stays.
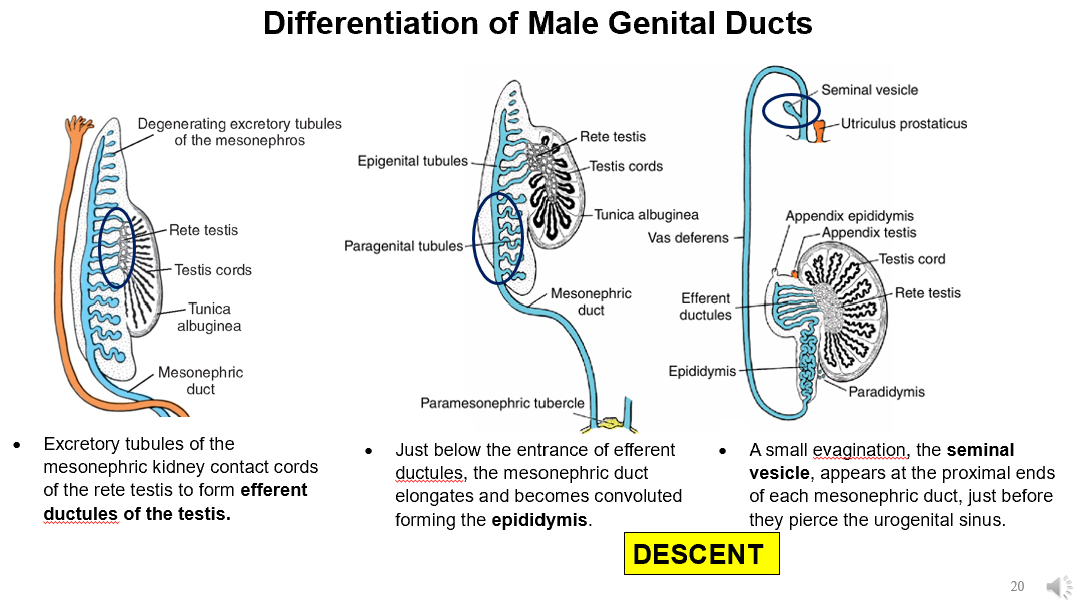
Male Genital Duct Formation Steps
Excretory tubules of the mesonephric kidney contact cords of the rete testis to form efferent ductules of the testis.
Mesonephric duct elongates and becomes convoluted forming the epididymis.
Seminal vesicle appears at the proximal ends of each mesonephric duct, just before they pierce the urogenital sinus.
Mesonephric tubules at caudal end of kidney and testis don’t join cords of rete testis, they stay as Paradidymis.
Cranial mesonephric tubules don’t combine with rete testis cords, they stay as Appendix Epididymis.
Part of mesonephric duct between urogenital sinus & seminal vesicle becomes Ejaculatory Duct.
Mesonephric duct between seminal vesicle & epididymis grows a thick muscular coat forming the ductus (vas) deferens.
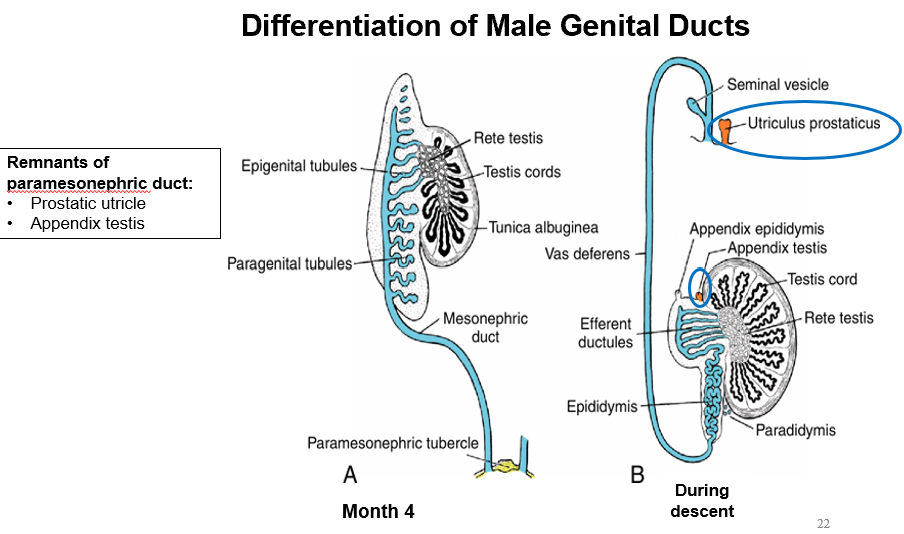
Sertoli cells produce antimüllerian hormone or Müllerian inhibiting hormone (MIH), which causes Müllerian ducts to degenerate.
A small remnant of the cranial end of the Müllerian ducts fuses to the tunica albuginea of each testis forming the appendix testis.

Prostatic Utricle
What the paramesonephric tubule regresses into
Remnants of paramesonephric duct:
Prostatic utricle
Appendix testis
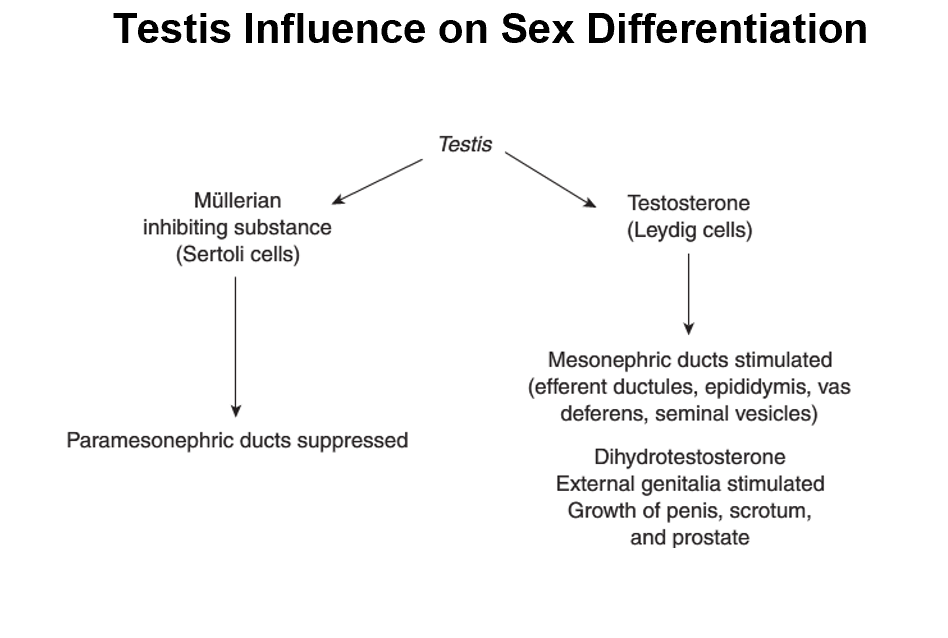
Mullerian Inhibiting Substance & Testosterone
Testis produces both of these things from:
Sertoli Cells
Leydig Cells
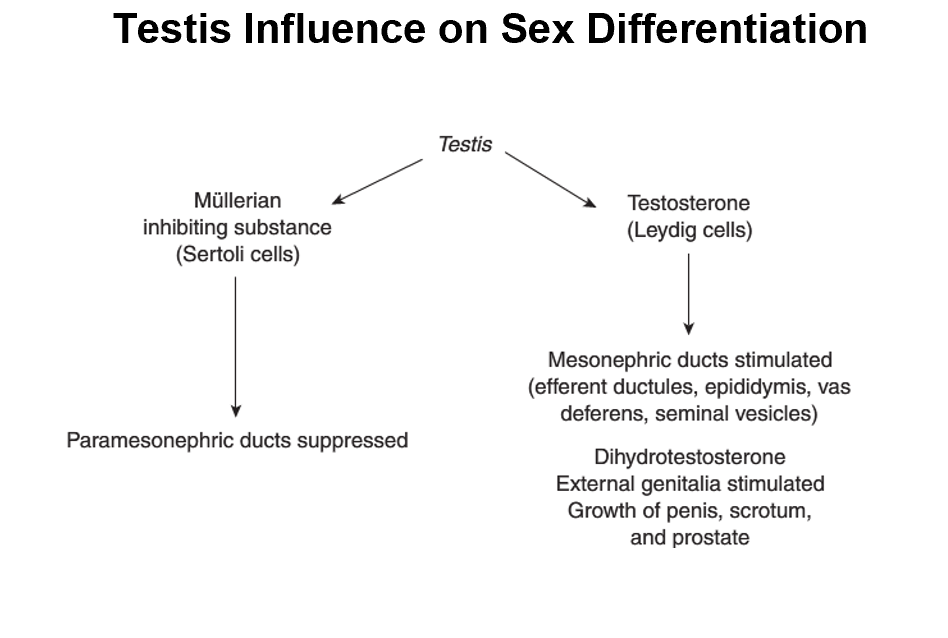
Mullerian Inhibiting Substance
Suppresses paramesonephric ducts
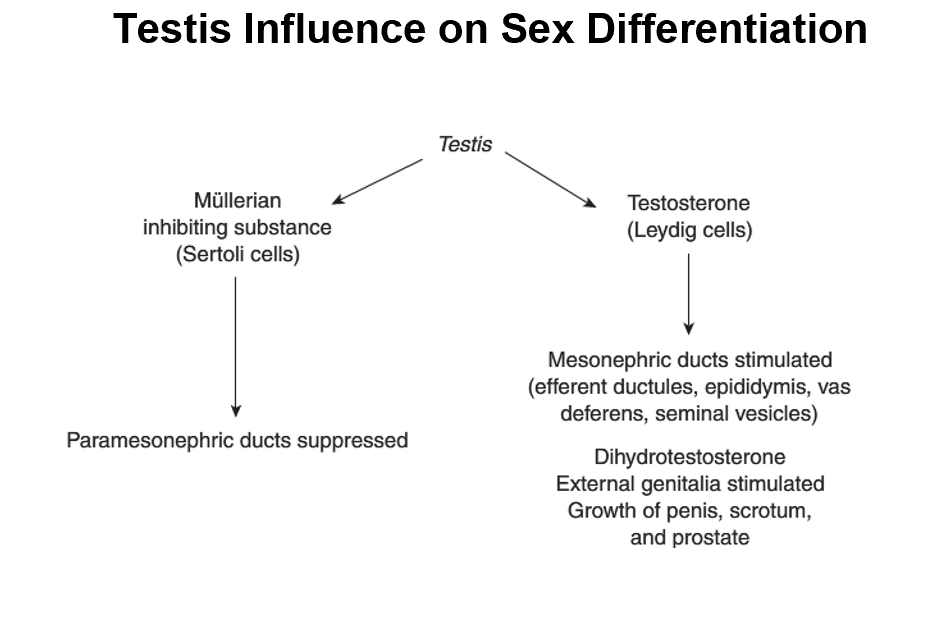
Testosterone
Mesonephric ducts are stimulated
Dihydrotestosterone for external genitalia
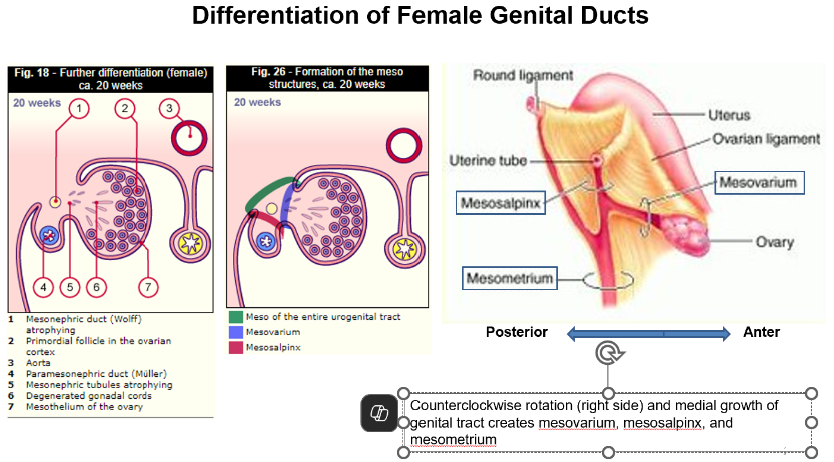
Female Genital Ducts Formation Steps
Absence of testosterone and presence of estrogen causes the Müllerian ducts to develop as the genital ducts of the female, while the mesonephric ducts degenerate
Ovary descends and the funnel-like end and distal 2/3rds of each duct become the uterine tubes, while the fused proximal ends become the corpus and cervix of the uterus and the cranial portion of the vagina.
Urogenital ridges grow and rotate medially until Müllerian ducts fuse in the midline, forming a transverse pelvic fold that extends from right and left pelvic walls, called the broad ligament of the uterus.
Here the uterine tubes are within its superior border, while the ovaries are on its posterior surface
Gubernaculum connects the gonad to the diaphragm and anterior body wall
During ovarian descent, the cranial gubernaculum disappears and becomes the suspensory ligament of the ovary
The intermediate part attaches to the developing uterus to become the ovarian ligament
The caudal-most gubernaculum exits the anterior body wall, crosses over the pubis and terminates in the labia majora as the round ligament of the uterus
Uterus and broad ligament divide the pelvic cavity into the Uterorectal and Uterovesical pouches.
If cranial and/or caudal excretory tubules (Wolffian) persist after genital duct formation, they form epoophoron and paroophoron, respectively that are found in the mesovarium.
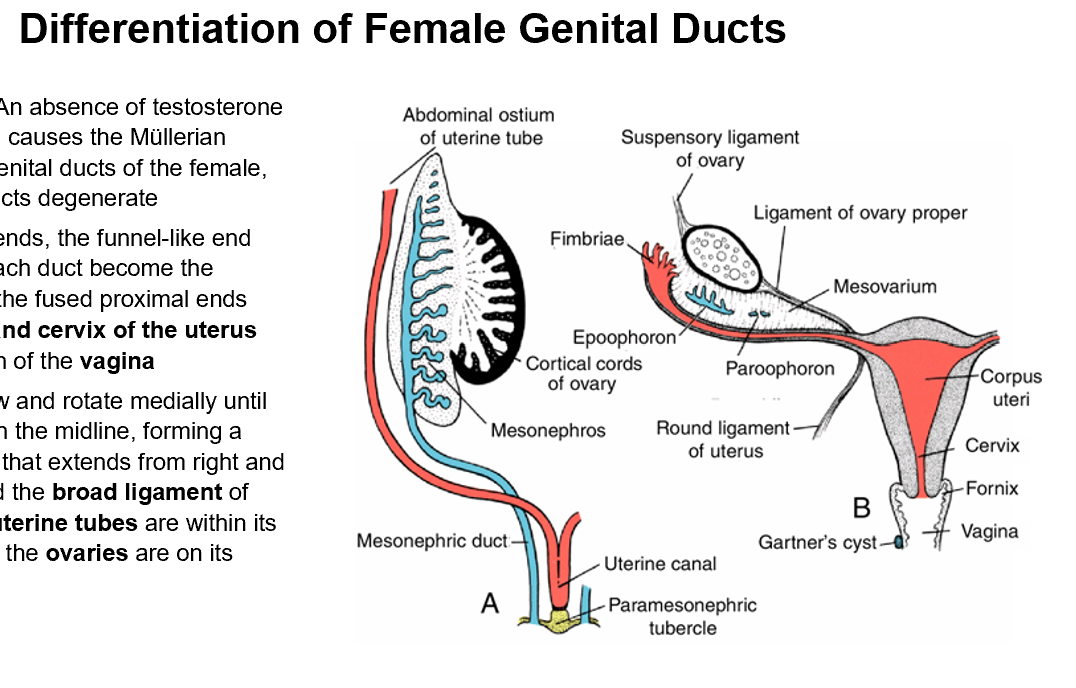
Mesovarium, mesosalpinx, and mesometrium
In females, counterclockwise rotation (right side) and medial growth of genital tract creates:
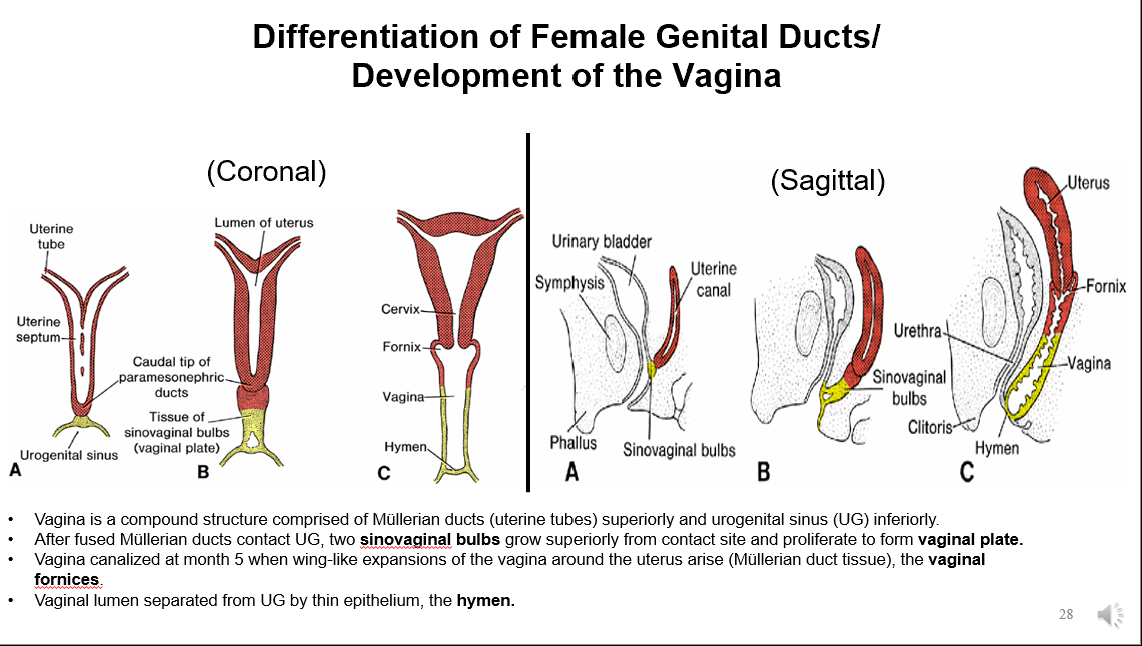
Development of the Vagina
Vagina is comprised of Müllerian ducts (uterine tubes) superiorly and urogenital sinus (UG) inferiorly.
After fused Müllerian ducts contact UG, two sinovaginal bulbs grow superiorly from contact site and proliferate to form vaginal plate.
Vagina canalized at month 5 when wing-like expansions of the vagina around the uterus arise (Müllerian duct tissue), the vaginal fornices.
Vaginal lumen separated from UG by thin epithelium, the hymen.
Congenital Anomalies of Female Reproductive System
Due to different degrees of lack of fusion of paramesonephric ducts
Uterus Arcuatus
Uterus Bicronis Bicollis
Uterus Didelphys
Uterus Bicronis Unicollis
Uterus Unicornis
Incomplete Canalization of Sinovaginal Bulb
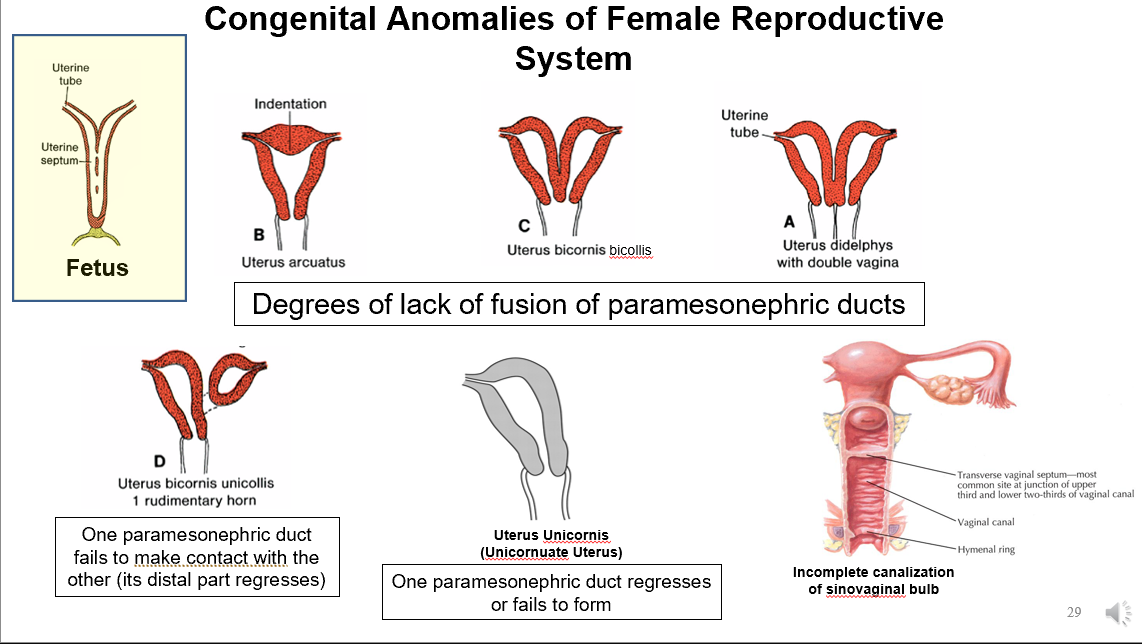
Uterus Arcuatus
Indentation of the fundus of the uterus into the lumen
Uterus Bicronis Bicollis
Uterine septum never formed, they fused at caudal end (makes 2 uteruses that empty into common vagina)
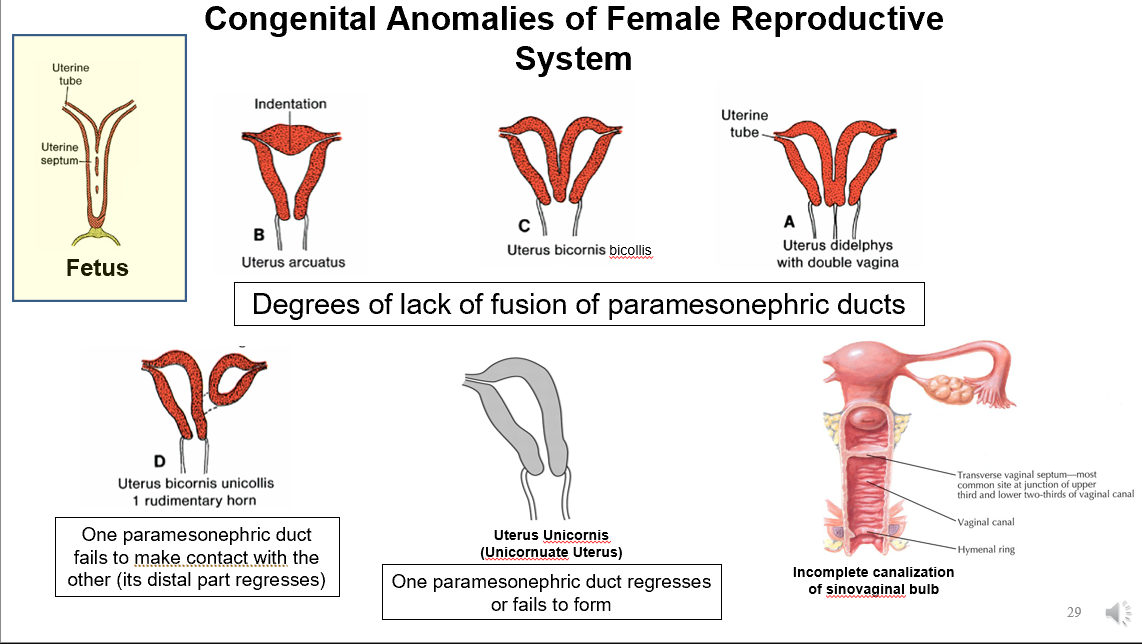
Uterine Didelphys
2 uteruses that each have their own vaginas
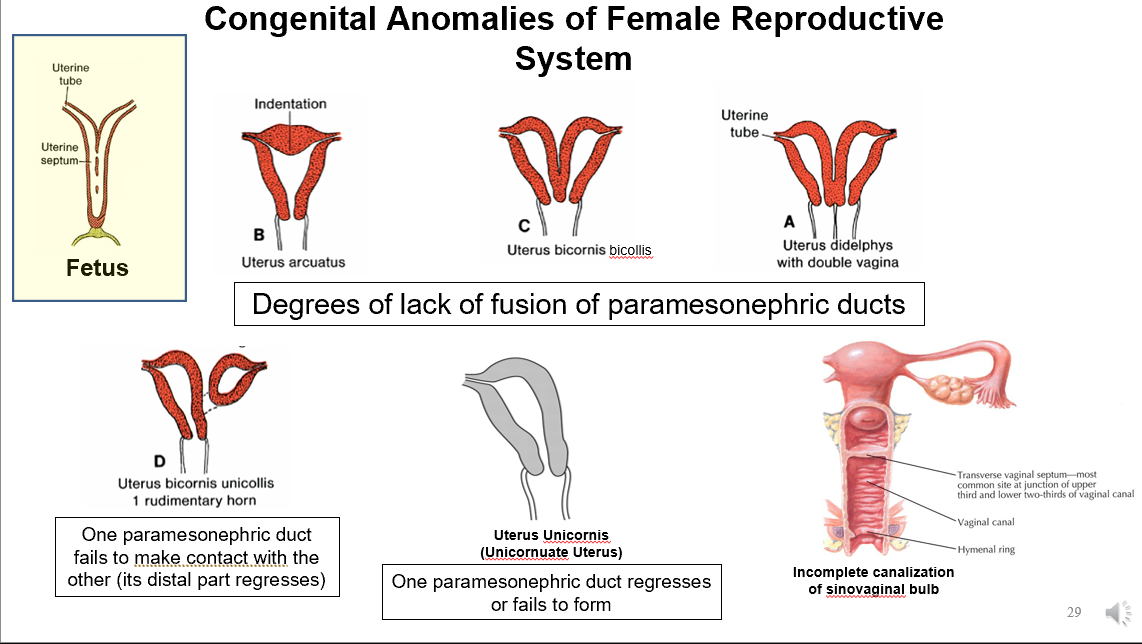
Uterus Bicronis Unicollis
One ovary/uterine tube going to vagina
One uterine horn that persists
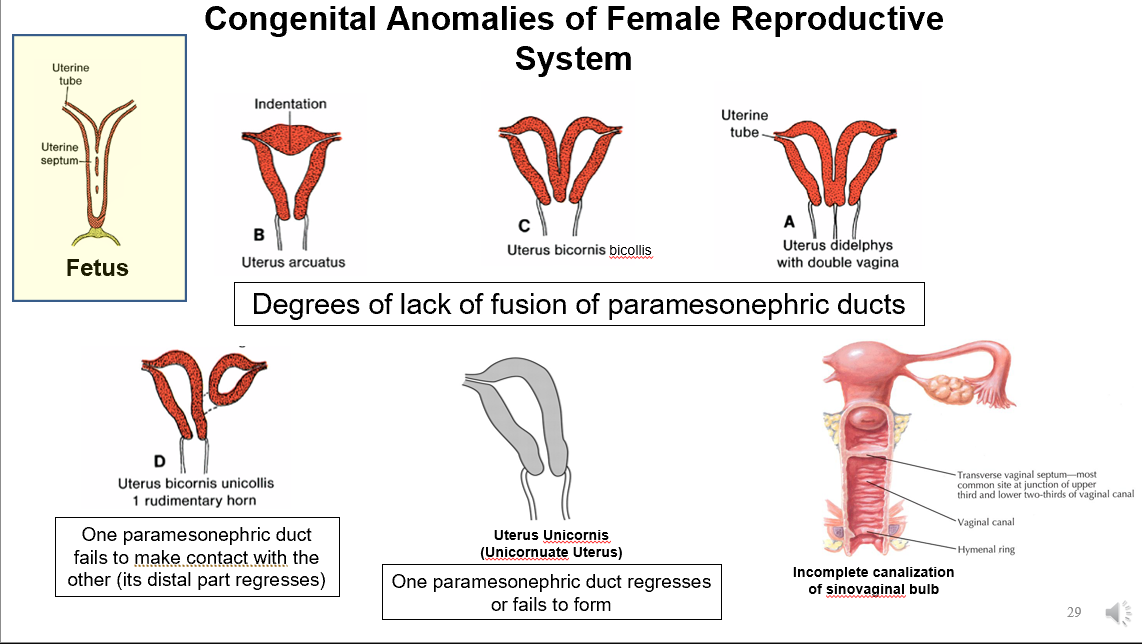
Uterus Unicornis
Only one Mullerian duct contributes to formation of the uterus (result is unilateral ovary)
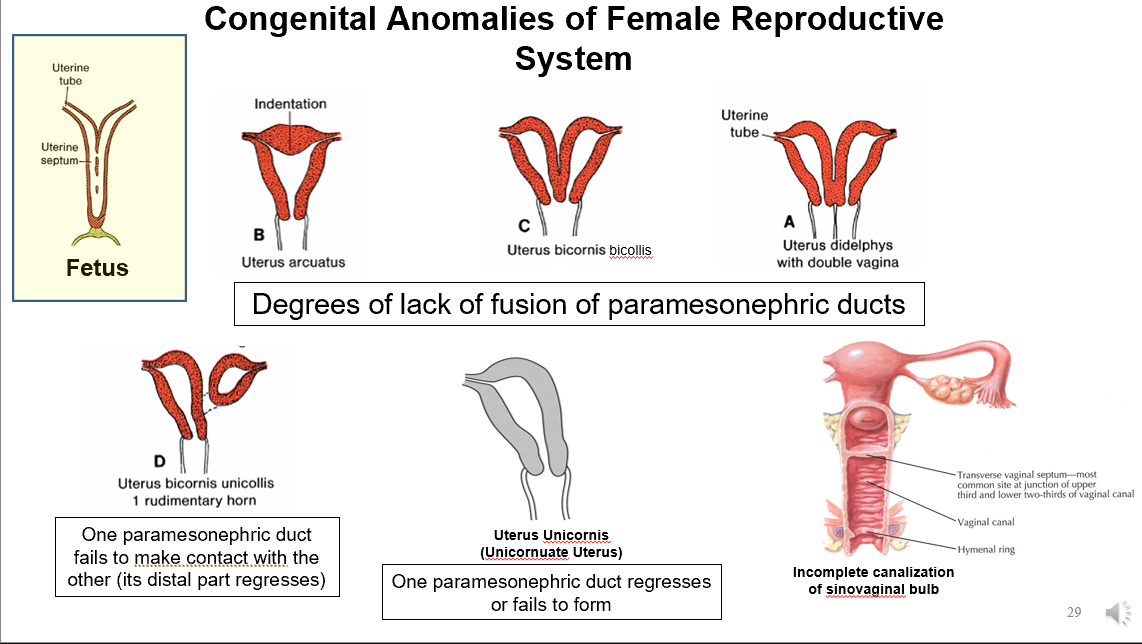
Incomplete Canalization of Sinovaginal Bulb
Typically creates lower 2/3 of distal vagina
In this case, forming 2 different cavities

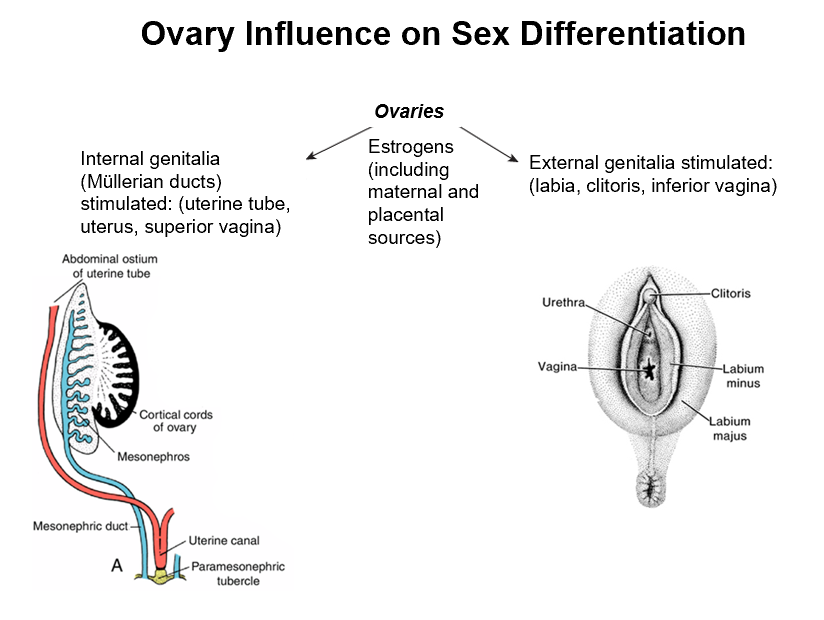
Ovaries and Sex Differentiation
Has to do with estrogens (from maternal and placental sources)
Forms:
Internal genitalia (Mullerian ducts, uterine tube, uterus, superior vagina)
External genitalia (labia, clitoris, inferior vagina)
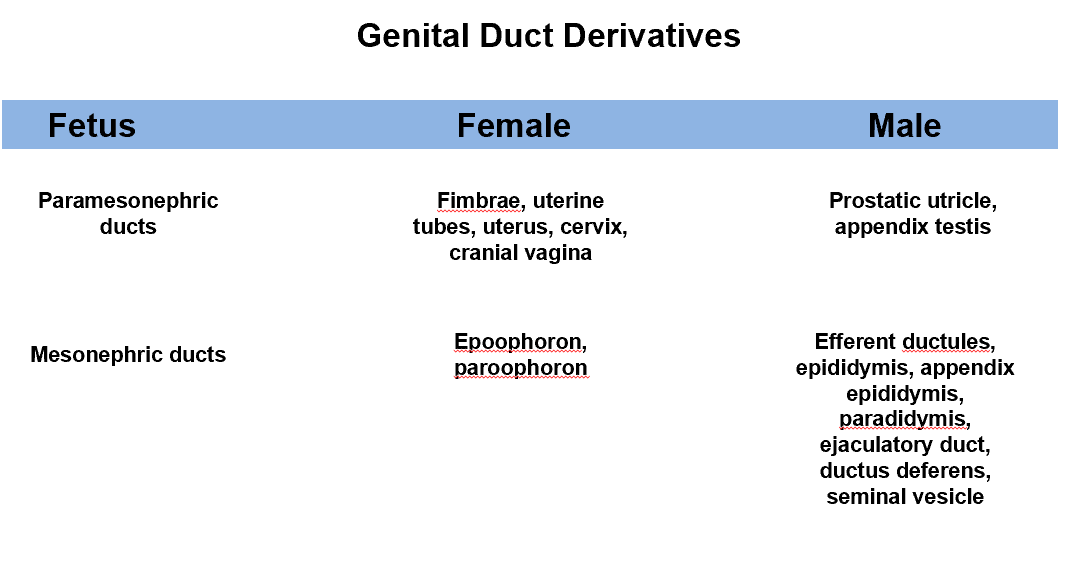
Female Development
Paramesonephric ducts: Fimbriae, uterine tubes, uterus, cervix, and cranial vagina.
Mesonephric ducts: Epoophoron and paroophoron.
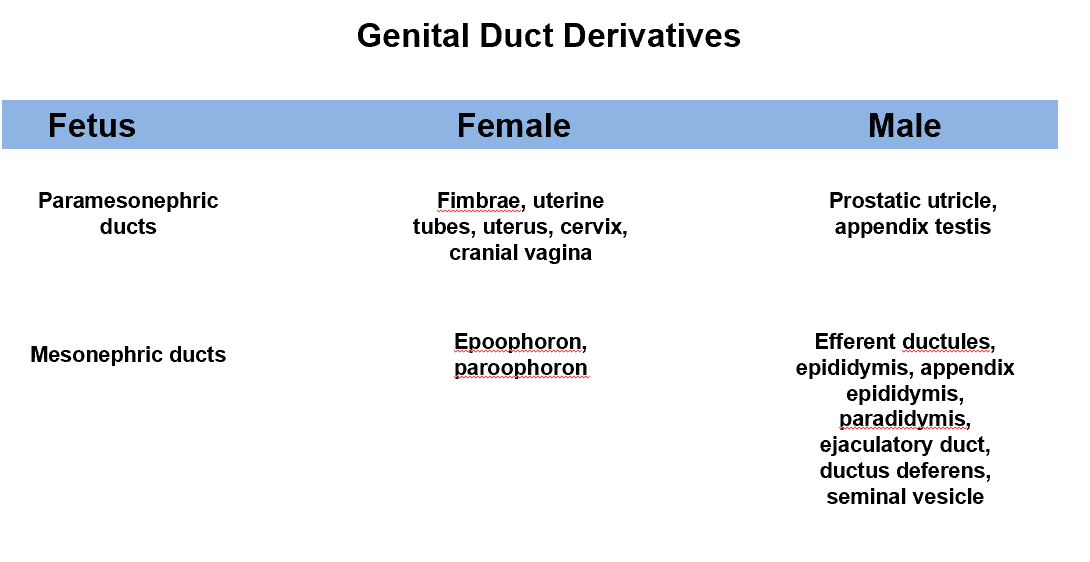
Male Development
Paramesonephric ducts: Prostatic utricle and appendix testis.
Mesonephric ducts: Efferent ductules, epididymis, appendix epididymis, paradidymis, ejaculatory duct, ductus deferens, and seminal vesicle.
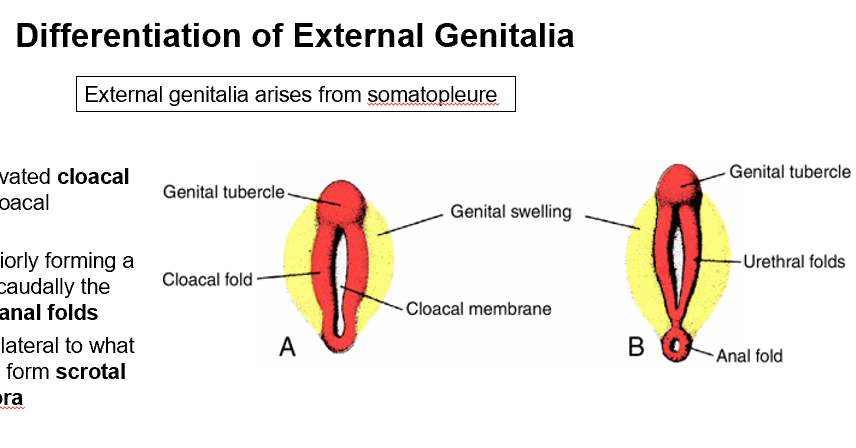
External Genitalia Differentiation
Arises from somatopleure
Somatopleure forms elevated cloacal folds surrounding the cloacal membrane in week 3
Cloacal folds fuse superiorly forming a genital tubercle, while caudally the folds form urethral and anal folds
Genital swellings form lateral to urethral folds to form scrotal swellings or labia majora
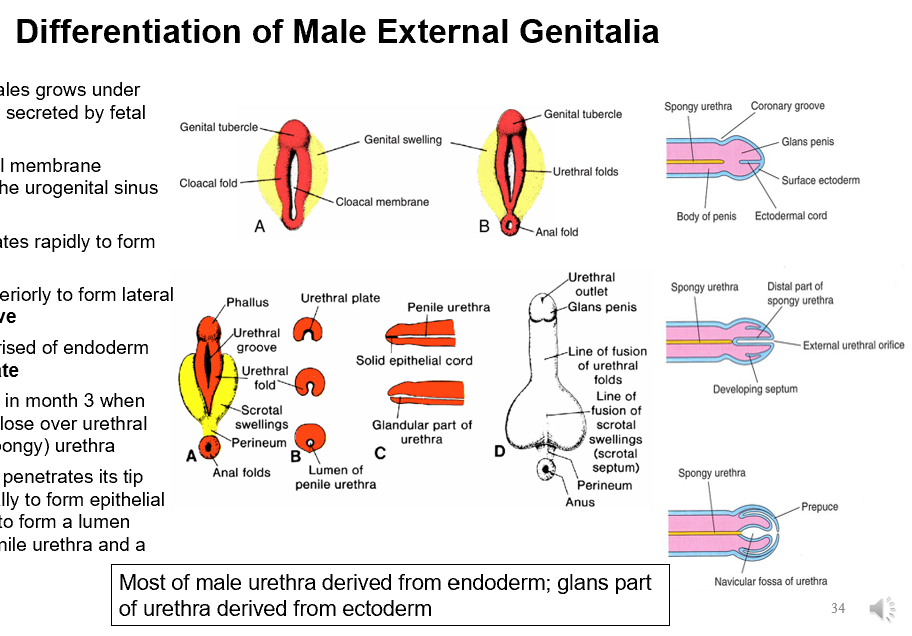
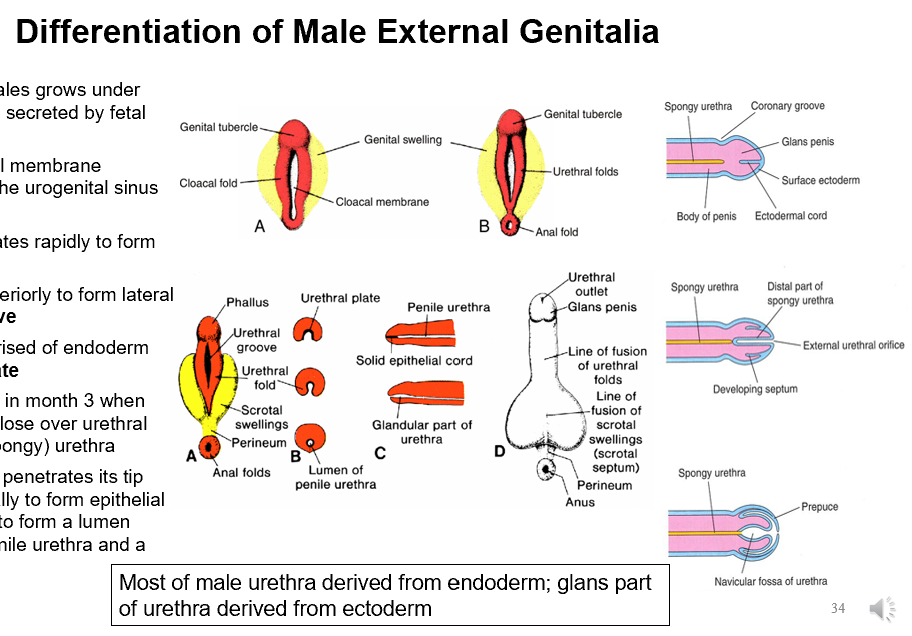
Differentiation of Male External Genitalia
External genitalia in males grows under influence of androgens secreted by fetal testes
The ectodermal cloacal membrane disappears, exposing the urogenital sinus and anorectal canal
Genital tubercle elongates rapidly to form the phallus
Urethral folds grow anteriorly to form lateral walls of urethral groove
Lining of groove comprised of endoderm and forms urethral plate
Penile urethra formed in month 3 when the two urethral folds close over urethral plate to form penile (spongy) urethra
Ectoderm of the glans penetrates its tip centrally and peripherally to form epithelial cords, later canalizing to form a lumen continuous with the penile urethra and a prepuce
Endoderm
Most of male urethra derived from _; glans part of urethra derived from ectoderm
Congenital Anomalies in forming male genitalia
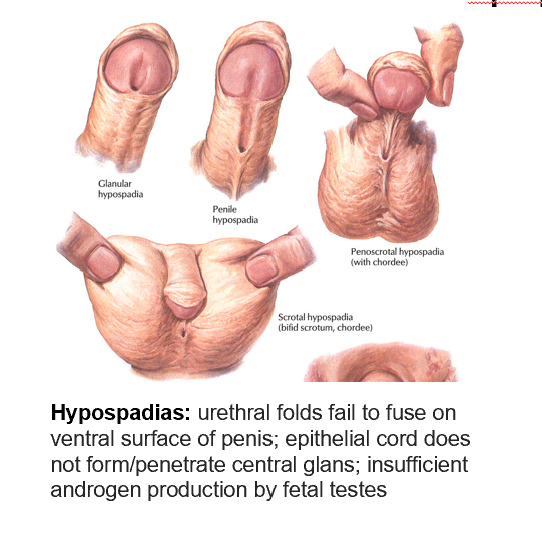
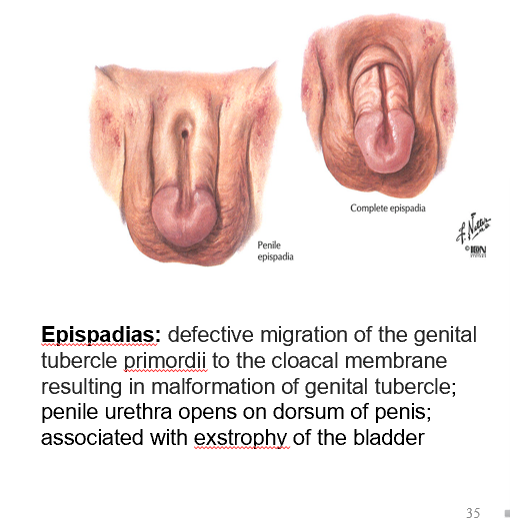
Hypospadias and Epispadias
Hypospadias
Urethral folds fail to fuse on ventral surface of penis; epithelial cord does not form/penetrate central glans; insufficient androgen production by fetal testes
Epispadias
Defective migration of the genital tubercle primordii to the cloacal membrane resulting in malformation of genital tubercle; penile urethra opens on dorsum of penis; associated with exstrophy of the bladder
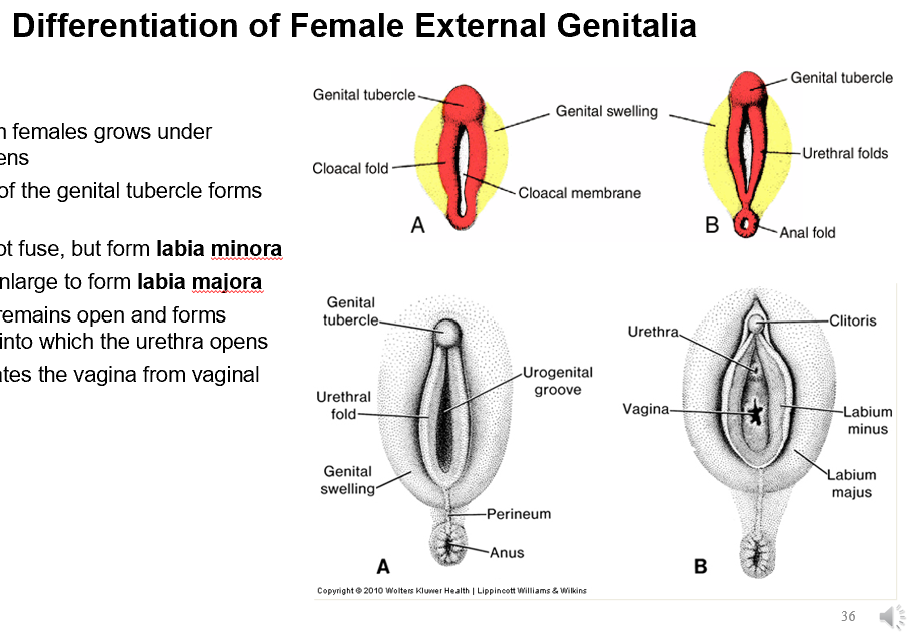
Differentiation of Female External Genitalia
External genitalia in females grows under influence of estrogens
A short elongation of the genital tubercle forms the clitoris
Urethral folds do not fuse, but form labia minora
Genital swellings enlarge to form labia majora
Urogenital groove remains open and forms vaginal vestibule into which the urethra opens
The hymen separates the vagina from vaginal vestibule
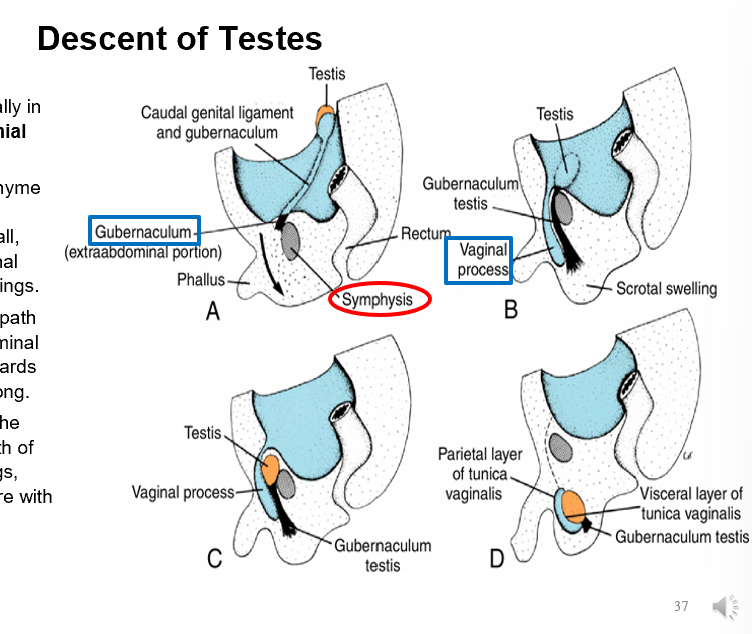
Descent of Testes
Testes and ovaries develop retroperitoneally in the lumbar area of the abdomen with cranial and caudal mesenchymal attachments.
The gubernaculum is a mesenchymal band extending from the caudal end of the testes/ovaries to the anterior abdominal wall, between the external and internal oblique muscles, and into the scrotal swellings.
As the testes begin to descend, they follow the path of the gubernaculum to the anterior abdominal wall.
The gubernaculum grows distally towards the scrotal swellings, pulling the testes along.
An evagination of the peritoneum forms, called the processus vaginalis, which follows the gubernaculum into the scrotal swellings.
The processus vaginalis pulls the anterior abdominal wall musculature with it, forming the inguinal canal.
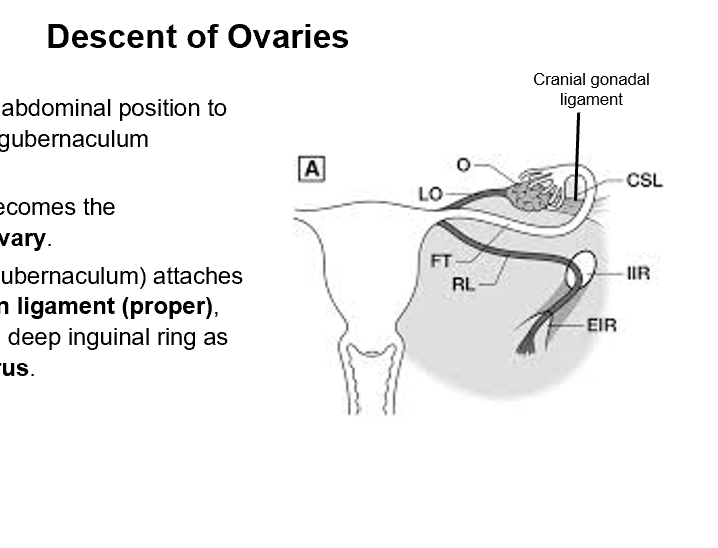
Descent of Ovaries
The ovaries descend from their abdominal position to just below the pelvic rim as the gubernaculum shortens.
The cranial gonadal ligament becomes the suspensory ligament of the ovary.
The caudal gonadal ligament (gubernaculum) attaches to the uterus to form the ovarian ligament (proper), then extends laterally to exit the deep inguinal ring as the round ligament of the uterus.
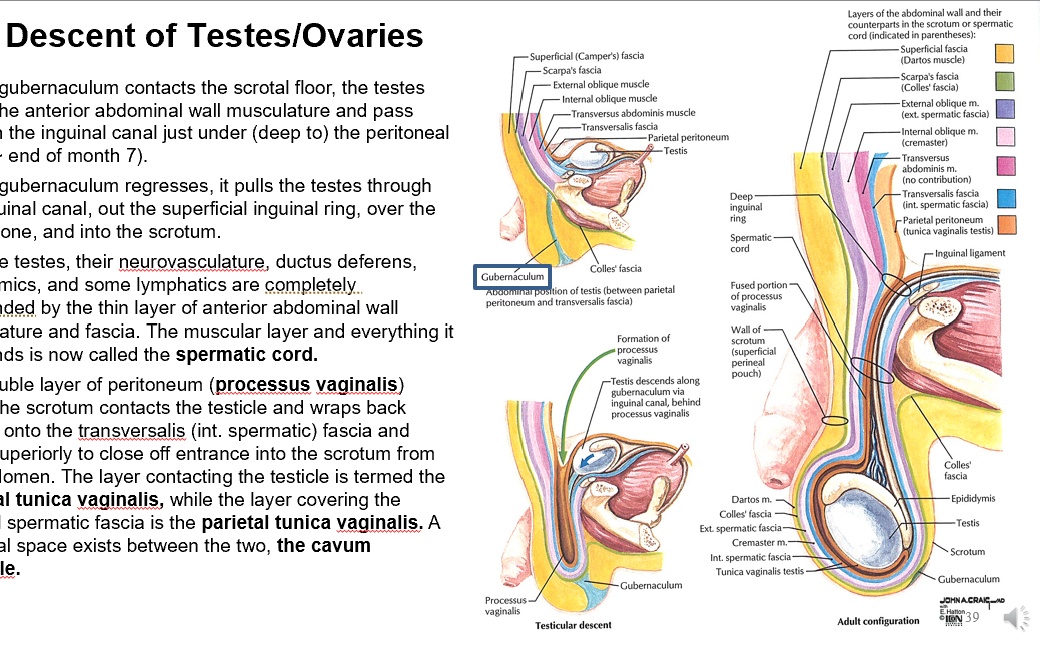
After Gubernaculum Descent
After end of month 7
Now the testes, their neurovasculature, ductus deferens, autonomics, and some lymphatics are completely surrounded by the thin layer of anterior abdominal wall musculature and fascia. The muscular layer and everything it surrounds is now called the spermatic cord.
The double layer of peritoneum (processus vaginalis) inside the scrotum contacts the testicle and wraps back around onto the transversalis (int. spermatic) fascia and fuses superiorly to close off entrance into the scrotum from the abdomen.
The layer contacting the testicle is termed the visceral tunica vaginalis, while the layer covering the internal spermatic fascia is the parietal tunica vaginalis.
A potential space exists between the two, the cavum vaginale.
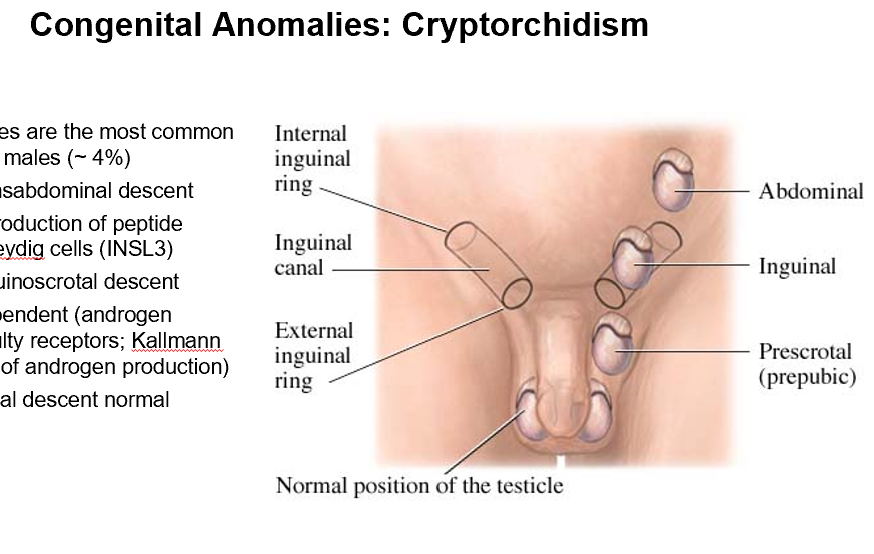
Cryptorchidism
Undescended testes are the most common genital anomaly in males (~ 4%)
Problems with transabdominal descent
inadequate production of peptide produced by Leydig cells (INSL3)
Problems with inguinoscrotal descent
androgen dependent (androgen insensitivity/faulty receptors; Kallmann syndrome/lack of androgen production)
transabdominal descent normal
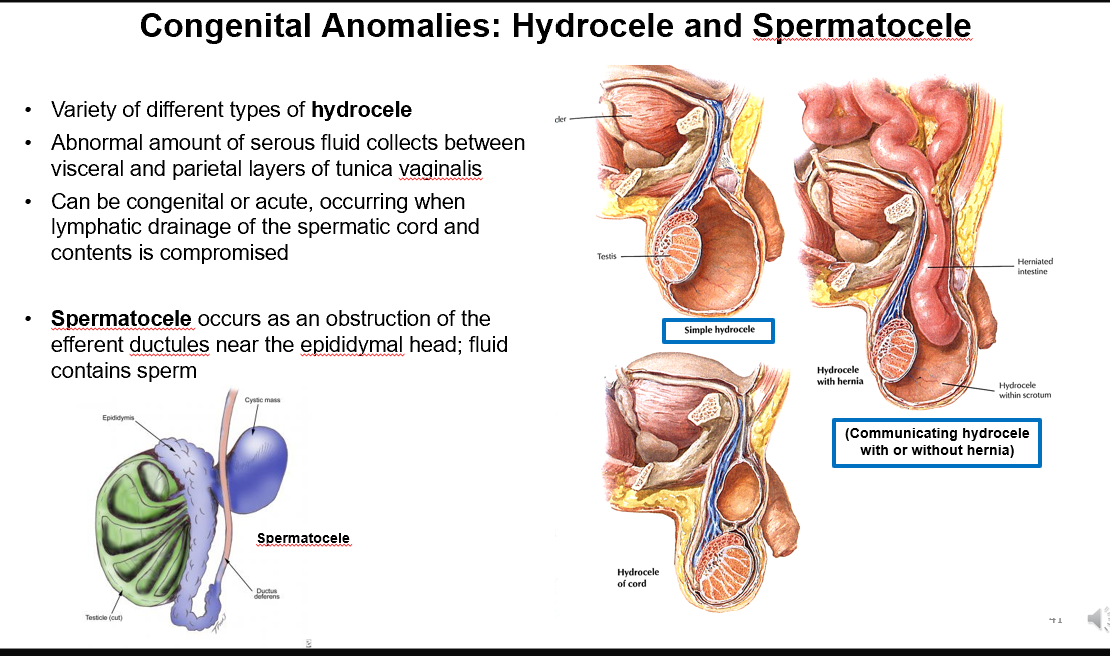
Hydrocele
Variety of types
Abnormal amount of serous fluid collects between visceral and parietal layers of tunica vaginalis
Can be congenital or acute, occurring when lymphatic drainage of the spermatic cord and contents is compromised
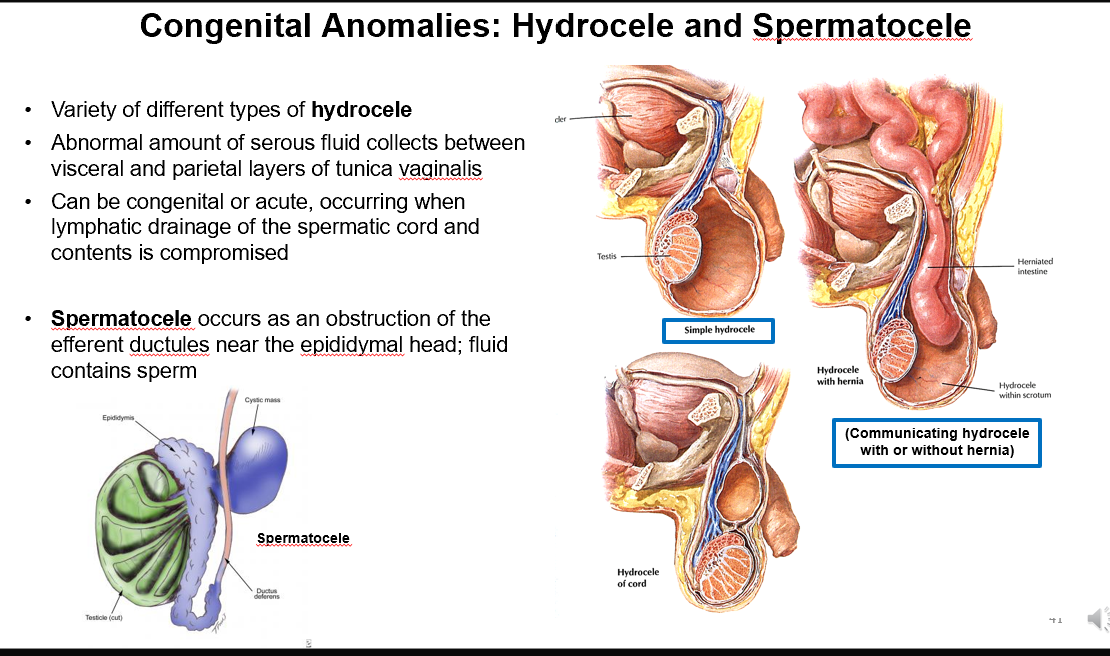
Spermatocele
Occurs as an obstruction of the efferent ductules near the epididymal head; fluid contains sperm
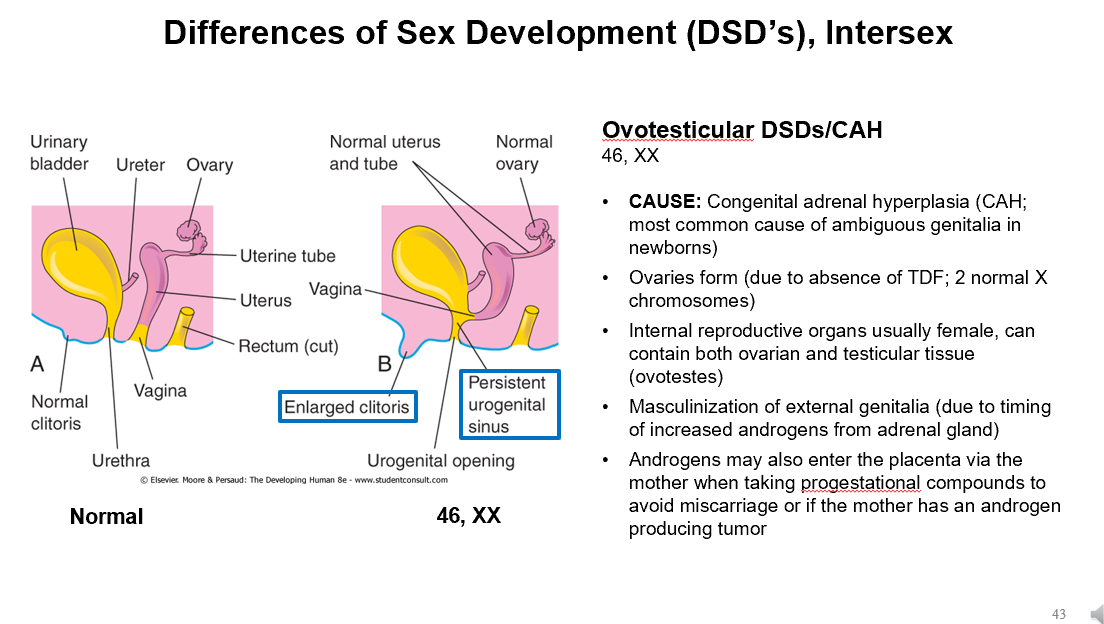
Ovotesticular DSDs/CAH
46 XX
CAUSE: Congenital adrenal hyperplasia (CAH; most common cause of ambiguous genitalia in newborns)
Ovaries form (due to absence of TDF; 2 normal X chromosomes)
Internal reproductive organs usually female, can contain both ovarian and testicular tissue (ovotestes)
Masculinization of external genitalia (due to timing of increased androgens from adrenal gland)
Androgens may also enter the placenta via the mother when taking progestational compounds to avoid miscarriage or if the mother has an androgen producing tumor
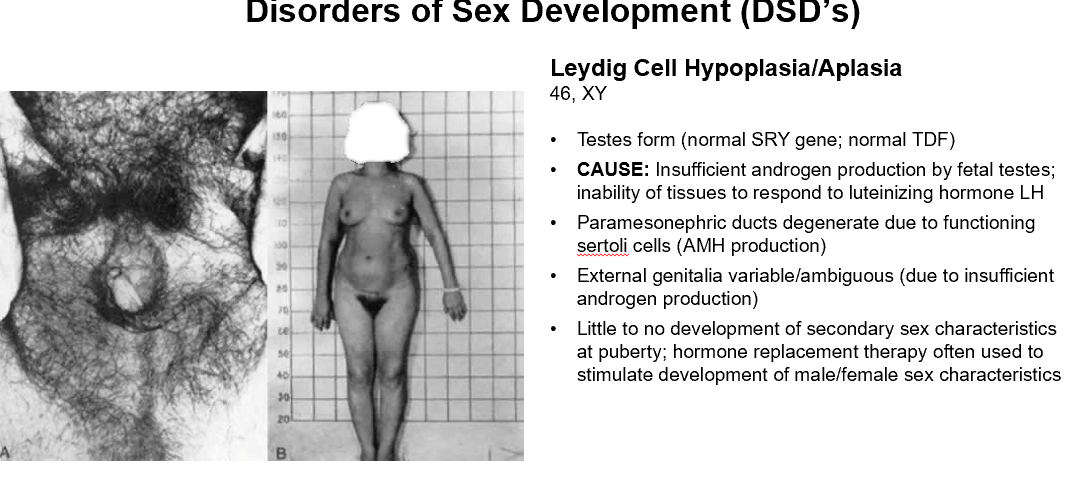
Leydig Cell Hypoplasia/Aplasia
46 XY
Testes form (normal SRY gene; normal TDF)
CAUSE: Insufficient androgen production by fetal testes; inability of tissues to respond to luteinizing hormone LH
Paramesonephric ducts degenerate due to functioning sertoli cells (AMH production)
External genitalia variable/ambiguous (due to insufficient androgen production)
Little to no development of secondary sex characteristics at puberty; hormone replacement therapy often used to stimulate development of male/female sex characteristics
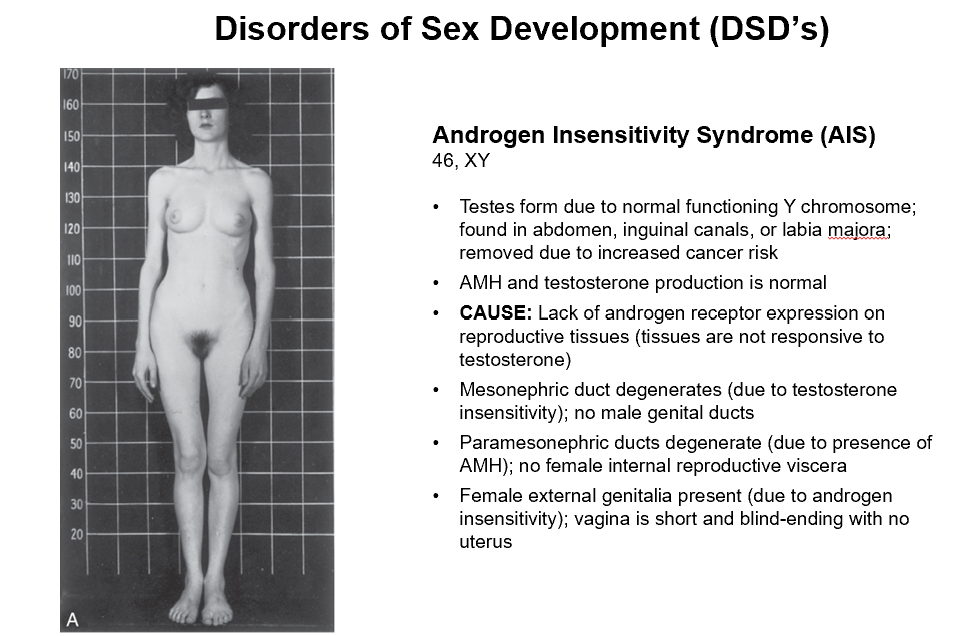
Androgen Insensitivity Syndrome (AIS)
46 XY
Testes form due to normal functioning Y chromosome; found in abdomen, inguinal canals, or labia majora; removed due to increased cancer risk
AMH and testosterone production is normal
CAUSE: Lack of androgen receptor expression on reproductive tissues (tissues are not responsive to testosterone)
Mesonephric duct degenerates (due to testosterone insensitivity); no male genital ducts
Paramesonephric ducts degenerate (due to presence of AMH); no female internal reproductive viscera
Female external genitalia present (due to androgen insensitivity); vagina is short and blind-ending with no uterus