Silverstein and Hopper Ch 32, 33, 35, 36
1/244
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
245 Terms
Mechanical Ventilators vs Spontaneous Breathing
Mechanical ventilators use an increase in airway pressure to move gas into the lungs in contrast to spontaneous breathing when airway pressure decreases below atmospheric pressure in order to generate the inspiratory phase of a breath
Oxygenation
Movement of oxygen from the alveoli into the pulmonary capillaries
Primarily dependent on the surface area available for gas exchange and preservation of the gas-exchange barrier
Ventilation
Removal of carbon dioxide
Primarily dependent on fresh gas movement into the alveoli
Intrathoracic Pressure
During spontaneous breathing, the intrathoracic or pleural pressure falls (becomes subatmospheric) during inspiration as a result of the expansion of the chest wall and movement of the diaphragm
This pressure change results in the inspiratory flow of air into the lungs
In contrast, PPV utilizes positive airway pressures to generate inspiratory gas flow
Equation of Motion
Pvent + P muscles = Elastance x Volume + Resistance x Flow
Pvent - pressure generated by the ventilator
Pmuscles - pressure generated by inspiratory muscles
Elastance is the inverse of compliance
Total pressure needed to generate a ventilator breath
Resistance
Reflects the pressure required to generate a given flow
Ohm’s Law Equation for Resistance
Resistance = driving pressure/flow
Airway Resistance During Mechanical Ventilation
Any narrowing of the airways will increase resistance including airway collapse or narrowing or diffuse bronchoconstriction
The endotracheal tube is often the source of greatest resistance present during mechanical ventilation
Compliance
A measure of the distensibility of the lung, defined as the change in lung volume for a given change in pressure
In ventilated patients, this translates to delivered VT/pressure required to generate the VT
Elastance - inverse of compliance
A lung with high compliance will accept a large increase in volume for a small pressure change
Low compliance would require a large pressure change to create a small increase in volume
Compliance Equation
Compliance = delta volume/delta pressure
Dead Space
Portion of the tidal volume that does not participate in gas exchange
Can be categorized as apparatus, anatomic, and alveolar in origin
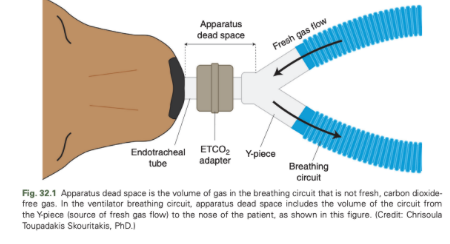
Apparatus Dead Space
The volume of the circuit from the Y-piece to the nose of the patient
Anatomic Dead Space
The volume of the conducting airways from the nose to the level of the alveoli
Alveolar Dead Space
Alveoli that are ventilated but not perfused
What are the two major types of ventilator breath?
Mandatory
Spontaneous
Mandatory Breath
When the machine controls initiation and/or termination of inspiration
Assisted Breath
When a mandatory breath is initiated by the patient
Spontaneous
Patient is responsible for both initiation and termination of inspiration
Supported Breath
A spontaneous breath in which the inspiratory flow is augmented by the machine
Mandatory Breath Initiation (Trigger)
Ventilator
Mandatory Breath Inspiratory Flow
Ventilator
Mandatory Breath Termination (Cycle)
Ventilator
Assisted Breath Initiation (Trigger)
Patient
Assisted Breath Inspiratory Flow
Ventilator
Assisted Breath Termination (Cycle)
Ventilator
Spontaneous Breath Initiation (Trigger)
Patient
Spontaneous Breath Inspiratory Flow
Patient
Spontaneous Breath Termination (Cycle)
Patient
Supported Breath Initiation (Trigger)
Patient
Supported Breath Inspiratory Flow
Ventilator
Supported Breath Termination (Cycle)
Patient
What are the three possible breath patterns?
Continuous mandatory ventilation (CMV)
Intermittent mandatory ventilation (IMV)
Continuous spontaneous ventilation (CSV)
Continuous Mandatory Ventilation (CMV)
All mandatory breaths are delivered
Intermittent Mandatory Ventilation (IMV)
Both mandatory and spontaneous breaths
Continuous Spontaneous Ventilation (CSV)
All spontaneous breaths
Assist/Control
When all breaths delivered are mandatory while allowing the patient to trigger a mandatory breath to allow ventilation to be synchronized with the patient’s efforst
What are the four phases of breath that can be controlled by the ventilator?
The start of inspiration
Inspiration
The end of inspiration
Exhalation
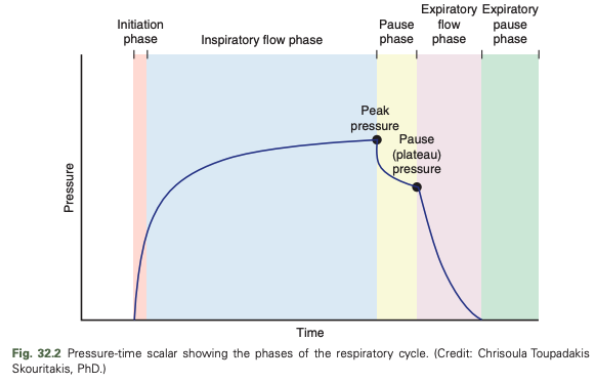
Pressure-Time Scalar of the Respiratory Cycle Diagram
What variables are not under ventilator control?
Compliance and resistance of the system are inherent to the patient and not under ventilator control
What are the three interdependent variables that can be manipulated by the ventilator machine?
In any one breath, the ventilator can only directly control one of these variables at a time, and the other two variables become dependent variables
What are the three types of control that ventilator breath can be considered?
Pressure-controlled
Volume-controlled
Flow-Controlled
Control Variable
The magnitude of the remaining two dependent variables will be determined by the set value of the control variable and the compliance and resistance of the system
Pressure-Controlled Breath
In a pressure-controlled breath, the machine will maintain airway pressure as determined by the operator, and inspiration ends when a preset inspiratory time is reached
The tidal volume and gas flow rate generated during the breath are dependent on the magnitude of the preset airway pressure as well as the resistance and compliance inherent to that animal
Volume-Controlled and Flow-Controlled Breaths
Volume-controlled and flow-controlled breaths are essentially the same, the machine will deliver the preset tidal volume over the preset inspiratory time
Airway pressure reached during these breaths is dependent on the magnitude of the preset tidal volume and subsequent flow rate, as well as the resistance and compliance of the patient's respiratory system
Cycle Variable
Parameter by which inspiration is terminated
Time is the most common cycle variable
Determined by the preset respiratory rate and the I:E
Inspiratory time of ~1 second commonly recommended
Trigger Variable
Parameter that initiates inspiration
In animals that are not making respiratory efforts of their own, the trigger variable will be time and is determined from the set respiratory rate
If the animal is making respiratory efforts, the trigger variable may be a change in airway pressure or gas flow in the circuit resulting from the patient's attempt to initiate inspiration
On most machines, the trigger sensitivity can be set by the operator
An airway pressure decrease of 2 cm H2O or gas flow change of 2 L/min are usually effective trigger sensitivities, but lower settings may be necessary in smaller patients
Appropriate trigger sensitivity ensures that ventilator breaths are synchronized with genuine respiratory efforts made by the patient
If trigger variable is too sensitive, it can lead to initiation of breaths after nonrespiratory movements such as patient handling - avoid
Limit Variable
Parameter that the breath cannot exceed during inspiration, but is different from the cycle variable because it does not terminate the breath
May be found on modern intensive care ventilators
Baseline Variable
Controlled during exhalation
Airway pressure is the most common baseline variable manipulated
If airway pressure during exhalation is maintained above atmospheric pressure, it is referred to as positive end expiratory pressure (PEEP)
Continuous Mandatory Ventilation
A minimum respiratory rate is set by the operator
If the trigger sensitivity is set appropriately, the patient can increase the respiratory rate, but all breaths delivered will be of a mandatory breath type
Controlled Ventilation
Patient is unable to trigger breaths
A/C (Assist/Control)
Patients are allowed to trigger their own respiratory rate
Intermittent Mandatory Ventilation
A set number of mandatory breaths are delivered
Between these breaths, patients can breathe spontaneously
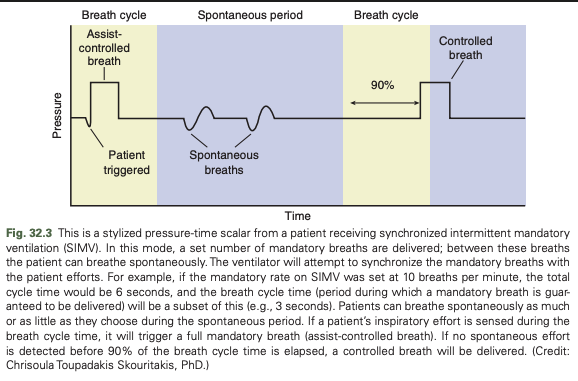
Synchronized Intermittent Mandatory Ventilation (SIMV)
The machine tries to synchronize the mandatory breaths with the patient's inspiratory efforts (assisted breaths)
The ventilator has a window of time in which it will deliver a mandatory breath
If the patient triggers a breath during this period, it will be assisted appropriately
If no breath is triggered by the end of this time period, a mandatory breath will be given
Between these mandatory breaths, the patient can breathe spontaneously as often or as few times as desired
Operator can control only the minimum respiratory rate and minimum minute ventilation
No control over the maximum rate or maximum minute ventilation
Continuous Spontaneous Ventilation
Every breath is triggered and cycled by the patient
Respiratory rate, inspiratory time and tidal volume are also determined by the patient
What are the two most common forms of continuous spontaneous ventilation?
Continuous positive airway pressure (CPAP)
Pressure support ventilation (PSV)
Continuous Positive Airway Pressure (CPAP)
Provides a constant level of positive pressure throughout the respiratory cycle
Increases the functional residual capacity and compliance, enhancing gas exchange and oxygenation
Pressure Support Ventilation (PSV)
Inspiratory flow is augmented to a preset level of inspiratory pressure
Reduces the effort required to maintain spontaneous breathing in patients with adequate respiratory drive but inadequate ventilatory (inspiratory) strength
Can help overcome the resistance of breathing through the endotracheal tube and ventilator breathing circuit
Can be used alone or to augment the spontaneous breaths during SIMV or CPAP
Cycle variable is a set reduction in inspiratory flow rate, a patient dependent variable
I:E Ratio and Respiratory Rate
Normal respiratory rate of 15-20 breaths is usually selected when assisted ventilation is initiated
Then can be changed as appropriate for the patient
I:E ratio may be preset by the operator or in some older ventilators is a default setting within the machine
An I:E ratio of 1:2 is commonly used to ensure that the patient has exhaled fully before the onset of the next breath
As respiratory rates are increased, the expiratory time will be sacrificed to "squeeze" in the necessary number of inspirations
Reverse or Inverse I:E Ratio Ventilation
When inspiratory time exceeds the expiratory time
Can occur as a result of the patient's respiratory pattern, such as fast respiratory rates
Can result in breath stacking or intrinsic PEEP because the animal is not able to exhale fully before the start of the next inspiration
Have been used as a ventilation strategy to improve oxygenation
Positive End-Expiratory Pressure (PEEP)
PEEP maintains positive pressure in the airway during exhalation that prevents the lung from emptying completely so the lung is "held" at a higher volume and pressure during exhalation
PEEP can increase the oxygenating efficiency of diseased lungs by recruiting previously collapsed alveoli, preventing further alveolar collapse, and reducing ventilator-induced lung injury
Appropriate magnitude of PEEP depends on the severity of the lung disease, the clinical response of the patient, and the presence of comorbidities in the patient (e.g. hypotension and intracranial hypertension)
Low levels of PEEP are commonly provided in animals with normal lung function to help prevent atelectasis
PEEP can have detrimental effects
PEEP maintains elevated intrathoracic pressures during exhalation and as a result may compromise venous return
Parameters that the Operator Can Preset on the Ventilator
With volume-controlled ventilation the tidal volume (or minute ventilation) is preset by the operator and peak airway pressure is a dependent variable
A peak airway pressure alarm limit is set to alert the operator of excessive airway pressures
With pressure-controlled ventilation, the airway pressure generated during inspiration is preset and tidal volume is a dependent variable
I:E ratio can be preset directly on some ventilators, but with some machines it is the consequence of the inspiratory time and respiratory rate that is chosen by the operator
Rise Time
Time in which the airway pressure increases from baseline to peak pressure
Faster rise times are indicated in patients with rapid respiratory rates
Caution in animals with small endotracheal tubes because of increased resistance to flow
What is normal tidal volume for a healthy dog and cat?
~10-15 ml/kg
Peak Airway Pressure Setting
Peak airway pressure is generally kept below 20 cm H2O, often closer to 10 cm H2O in patients with normal lungs
Animals with pulmonary disease have reduced pulmonary compliance and therefore require higher pressures in order to deliver an adequate tidal volume
Airway pressures up to 30 cm H2O may be necessary in animals with severe, diffuse lung disease
What are common causes for the low pressure alarm?
Patient disconnect
Leak
What are common causes for the high pressure alarm?
Patient-ventilator dyssynchrony
ET tube kink or obstruction
Small size ET tube with high inspiratory flow rate
VC mode: pneumothorax
Common Causes for Low PEEP/CPAP Alarm
Leak
Common Causes for Low Tidal Volume Alarm
Leak
PC mode: patient-ventilator dyssynchrony, decreased compliance, pneumothorax, ET tube obstruction
VC mode: patient-ventilator dyssynchrony, ET tube obstruction
Common Causes for the Apnea Alarm
In spontaneous breathing modes, will need appropriate settings for mandatory rescue breaths
Common Causes for Low Minute Ventilation Alarm
Causes of low tidal volume
Spontaneous breathing modes: low respiratory rate
What are the three main indications for mechanical ventilation?
Severe hypoxemia despite oxygen supplementation
Severe hypoventilation despite therapy
Excessive respiratory effort with impending respiratory fatigue or failure
What indicates severe hypoxemia?
Indicated by cyanosis, PaO2 of less than 60 mmHg or a SpO2 of less than 90%
Cannot use venous values to diagnose hypoxemia
Indications for Mechanical Ventilation - Severe Hypoxemia Despite Oxygen Supplementation
Most of these animals have primary lung disease
Inspired oxygen concentrations of greater than 60% for a prolonged period (24-48 hours) can lead to oxygen toxicity and subsequent pulmonary damage
Animals that require high concentrations of inspired oxygen for longer than 24 hours in order to achieve adequate oxygenation may also benefit from mechanical ventilation
Hypoventilation
An elevation in the partial pressure of carbon dioxide (PCO2)
In patients that are hemodynamically stable, venous CO2 is an accurate reflection of arterial PCO2 and can be used to evaluate hypoventilation
Severe hypoventilation is defined as a PaCO2 higher than 60 mmHg and may be an indication for mechanical ventilation if the patient is unresponsive to therapy for the primary disease
Indications for Mechanical Ventilation - Severe Hypoventilation Despite Therapy
Hypercapnia is a consequence of reduced effective alveolar ventilation
May be due to increased dead space in a breathing circuit, upper airway obstruction, sedative overdose, or neurologic or neuromuscular diseases that impair respiratory rate or chest wall movement
Most patients with increased apparatus dead space, upper airway obstruction, or sedative overdoses respond to appropriate therapy and do not require mechanical ventilation
Patients requiring ventilation in this category have neurologic, muscular, or neuromuscular disease processes such as brain disease, high cervical spinal cord disease, peripheral neuropathies, neuromuscular junction abnormalities, or primary myopathies (collectively neuromuscular diseases)
Animals with brain disease may not tolerate small elevations in PCO2 and mechanical ventilation may be beneficial in these patients if the PaCO2 is higher than 45 mmHg
Another group of patients that may require PPV to prevent hypoventilation are those animals that require general anesthesia for reasons such as maintenance of an endotracheal tube or provision of effective analgesia
The anesthetic drugs invariably cause hypoventilation and PPV during the anesthetized period is ideal
Many post-cardiopulmoanary arrest patients will require PPV for a time after return of spontaneous circulation
For short durations, manual ventilation may be sufficient, but animals with apnea, inadequate or unreliable ventilatory efforts, hypercapnia, or concerns for intracranial hypertension will benefit from mechanical ventilation
Indications for Mechanical Ventilation - Excessive Respiratory Effort with Impending Respiratory Fatigue or Failure
Animals with pulmonary disease may be able to maintain adequate oxygenation and ventilation by increasing their respiratory effort
If respiratory effort is marked, patients can become exhausted and respiratory arrest may occur despite acceptable blood gas values
Intervention before the arrest and initiation of mechanical ventilation may successfully stabilize these patients
What is a fourth indication for PPV?
Severe hemodynamic compromise that is refractory to therapy
Anesthesia is often feasible in these patients with opioid and benzodiazepine drugs alone
Mechanical ventilation can decrease oxygen consumption and support left heart function and may allow ongoing support of the patient while definitive measures to improve the hemodynamic state can be made
Initiation of Mechanical Ventilation
If the patient is in a life-threatening state, it maybe necessary to anesthetize, intubate, and provide manual PPV while ventilator setup is performed
The operator should anticipate that animals with primary lung disease may require more PEEP and higher inspired oxygen concentrations that patients with neuromuscular disease
Turn on machine and test to ensure its functioning properly with an artificial lung or rebreathing bag
Always start mechanical ventilation with 100% oxygen until appropriate machine function and patient stability can be confirmed
After initial stabilization, the FiO2 can be tailored appropriately
A separate source of 100% oxygen with a means to provide manual ventilation should be available at all times in case of machine failure
Immediately after the patient is connected to the ventilator, the chest should be observed for appropriate movements
Ventilator settings should be adjusted if the chest wall movements appear excessive or inadequate
Auscultation performed to confirm the presence or absence of breath sounds bilaterally
If breath sounds are not audible bilaterally, endobronchial intubation may have occurred and the endotracheal tube should be repositioned appropriately
Patients require general anesthesia in order to start mechanical ventilation unless they have severe neurologic deficits
Anesthesia is required to enable intubation, keep the patient immobile, and allow the patient to tolerate positive pressure ventilation
Animals that are immobile and unable to fight the ventilator, such as patients with respiratory paralysis, may benefit from placement of a temporary tracheostomy tube
Allows for reduction (or even removal) of anesthetic agents and makes neurologic evaluation and patient treatment simpler to interpret
Patients with normal neurologic function cannot be ventilated without general anesthesia, even with a temporary tracheostomy tube
Brachycephalic animals may benefit from the placement of a temporary tracheostomy tube for the weaning process
Monitoring tools should be evaluated and significant abnormalities addressed immediately
Once the patient is considered stable, an arterial blood gas is evaluated and the ventilator settings modified accordingly
In the absence of arterial blood gases, ventilator management is based on physical examination findings, venous PCO2 levels, and pulse oximetry
What is the goal of mechanical ventilation?
To maintain adequate arterial blood gas levels (PaCO2 35-50 mmHg, PaO2 80-120 mmHg) with the least aggressive ventilator settings possible
Carbon Dioxide in Mechanical Ventilation
Arterial PCO2 is directly proportional to CO2 production and is inversely proportional to alveolar minute ventilation
In most disease state, CO2 production is relatively stable, and minute-to-minute changes of PaCO2 are the result of change in alveolar minute ventilation
Endotracheal tube obstruction caused by kinks or the accumulation of airway secretions may also reduce the volume of effective alveolar ventilation
In the absence of these equipment issues, hypercapnia is considered to be a result of inadequate VA
Because minute ventilation is equal to the product of the respiratory rate and tidal volume, one or both of these ventilator settings can be increased and the PCO2 concentration reevaluated to determine if the new ventilator protocol is adequate
If PCO2 is low, VA should be decreased
If end-tidal CO2 correlates reliably with PCO2, it can be an excellent real time monitor
Total Minute Ventilation (VT)
Equal to the product of the respiratory rate and the tidal volume, but a portion of this inspired gas volume does not participate in gas exchange (dead space) and so does not contribute to the elimination of CO2
Alveolar Minute Ventilation Equation
Respiratory rate x (VT - dead space volume)
What can cause significant increases in dead space in small animals?
In small patients, excess tubing length between the breathing circuit Y-piece and the animal's mouth can cause significant increases in dead space
Can be a consequence of excessive endotracheal tube length, extension pieces, or monitoring devices connected to the endotracheal tube
What is the first priority with oxygen in mechanical ventilation?
First priority is to reduce the FiO2 to less than or equal to 60% as soon as possible to reduce the risk of oxygen toxicity
Magnitude of reduction in FiO2 dictated by the measured PaO2
PaO2 should be reevaluated after any reduction in oxygen concentration
If SpO2 correlates well with the PaO2 (or arterial blood samples are unavailable), pulse oximetry can be used to help guide changes in ventilator settings as well
What is the oxygen goal with mechanical ventilation once FiO2 is reduced to less than 60%?
Once FiO2 is reduced to less than 60%, the focus becomes reducing the magnitude of the ventilator settings, namely PEEP and the peak inspired airway pressure, can be considered if the PaO2 is significantly higher than the targeted range
Hypoxemia Despite Ventilation with 100% Oxygen
In severe cases, hypoxemia will persist despite ventilation with 100% oxygen
Changes in the ventilator settings are required
Increases in PEEP, peak inspired airway pressure/tidal volume, and/or respiratory rate may help improve the oxygenating efficiency of the lung
Prone positioning will maximize lung function in most patients
Animals with hypoxemia should be maintained in sternal recumbency until stabilized
Mechanical Ventilation Complications - Cardiovascular Compromise
Cardiovascular compromise as a result of impairment of intrathoracic blood flow is often an issue for patients with cardiovascular instability or when aggressive ventilator settings are necessary
Mechanical Ventilation Complications - Ventilator-Induced Lung Injury
Volutrauma and repetitive alveolar opening and collapse are believed to be the major causes of ventilator-induced lung injury and may be reduced with protective ventilation strategies
Mechanical Ventilation Complications - Ventilator-Associated Pneumonia
Aseptic airway procedures, intensive oral care, and reducing the incidence of gastric regurgitation are all important in preventing the incidence of ventilator-associated pneumonia
Patients should be monitored continuously for evidence of a nosocomial infection and changes in pulmonary function
Routine sampling of airway fluid for cytology and culture and sensitivity testing may help to detect early ventilator-associated pneumonia
Mechanical Ventilation Complications - Pneumothorax
Has been shown to occur more often when very high airway pressures are used in human patients (plateau airway pressure >35 cm H2O)
When more conventional ventilator settings are used, there is no correlation among airway pressure, PEEP, or other settings, and the occurrence of pneumothorax
Development of pneumothorax is more likely the result of underlying lung disease rather than the ventilator setting used
Pneumothorax should be a primary consideration when a patient has an acute decline in oxygenating ability, elevation in PCO2, decreased chest wall movement and compliance, and patient-ventilator asynchrony
Tension pneumothorax can be rapidly fatal if not diagnosed and treated in animals receiving PPV
Unilateral or bilateral thoracostomy tubes with continuous drainage are indicated when managing these ventilated animals
If an acute, life-threatening pneumothorax develops in the ventilator patient, an emergency thoracotomy to create an open pneumothorax may be required to prevent cardiopulmonary arrest
Thoracostomy tubes placed after stabilization of cardiovascular parameters
Mechanical Ventilation Troubleshooting - Patient-Ventilator Asynchrony (Bucking the Ventilator)
Occurs when the patient is breathing against the machine
Can prevent effective ventilation and may lead to hypoxemia, hypercapnia, and hyperthermia
Increases the work of breathing and can increase patient morbidity
Mechanical Ventilation Troubleshooting - Sudden Decrease in Oxygenation
Oxygen supply to the machine should be checked and confirm the breathing circuit is intact and the ventilator is delivering breaths as prescribed
If the patient has become hypoxemic, the FiO2 should be increased immediately to 100% and the animal placed in sternal recumbency until the condition is improved
Mechanical Ventilation Troubleshooting - Sudden Elevations in PCO2
Can occur as a consequence of equipment faults, patient problems (e.g. pneumothorax, airway obstruction), or inappropriate ventilator settings
If no mechanical abnormalities are evident and patient disease such as pneumothorax is ruled out, the ventilator settings should be changed to increase minute ventilation
Hypercapnia may be an acceptable consequence of some protective ventilation strategies (permissive hypercapnia)
Causes of Hypoxemia in the Ventilator Patient
Loss of oxygen supply
Machine or circuit malfunction
Deterioration of the underlying pulmonary disease
Development of new pulmonary disease
Pneumothorax
Pneumonia
VILI
ARDS
Potential Responses to Hypoxemia in the Ventilator Patient
Increase FiO2
Sternal positioning
Thoracic auscultation
Verify machine function
Evaluate for leaks
Increases in PEEP
Increases in PIP/tidal volume
Causes of Hypercapnia in the Ventilator Patient
Pneumothorax
Bronchoconstriction
Endotracheal tube or airway obstruction
Circuit leak
Increased apparatus dead space
Increased alveolar dead space
Alveolar overdistension
Pulmonary embolism
Inadequate ventilator settings
Low VT and/or RR
Potential Responses to Hypercapnia in the Ventilator Patient
Evaluate patient data
Thoracic auscultation
Assess endotracheal tube
Verify machine function
Ensure adequate expiratory time
Increase VT and/or RR
Note: hypercapnia may be an acceptable consequence of some ventilation strategies
Causes of Hyperthermia in the Ventilator Patient
Impaired natural cooling mechanisms
Potential Responses to Hyperthermia in the Ventilator Patient
Rule out fever
Active cooling
Inappropriate Ventilator Settings in the Ventilator Patient
Patient efforts/requirements are not being met with ventilation strategy