Additional Procedures
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
102 Terms
What are some of the additional procedures that you might be doing?
arthrography
hysterosalpingogram
myelography
sialography
orthorentgenoraphy
bone densitometry
conventional tomography
What is arthrography?
Contrast media study of synovial joints and related soft tissue structures
What are the two most common arthrography procedures done?
shoulders and knees
TMJs used to be done frequently too
What has greatly reduced the need for arthrography?
MRI (however, still a useful way to see the soft tissue structures located near joints)
What must you have from the patient with any study involving the injection of a contrast medium?
Signed consent form
What are the pathological indication for arthrography?
due to some type of trauma (tears of menisci or ligaments)
non-trauma would be a baker’s cyst in the knee
What is the only contraindication for arthrography?
If the patient is allergic to the iodine-based contrast or to the local anethetics
What is the technologists responsibilities for arthrography?
explaining the procedure to the patient
getting the consent form signed
room prep (fluoro is working, tray set up)
have contrast ready for radiologist (single or double)
assist radiologist
after films- sometimes
What are the common joints studies for arthrography?
hip
knee
ankle
shoulder
elbow
wrist
TMJ
Knee arthrography
assesses knee joint and associated soft-tissue structures
joint capsule, menisci, and ligaments
What are the indications for knee arthrography?
tears in joint capsule
tears or degeneration of menisci
ligament injury
What are the contraindications for knee arthrography?
Hypersensitivity to iodine or local anesthetics
What is included in the arthrogram tray?
prep sponge
fenestrated drape
syringes
flexible connector
needles
What are the steps of needle placement and injection for arthrography?
site prepared
skin anesthetized (numbbed)
fluid aspirated (not always needed)
contrast media instilled
needle removed and knee bandaged
knee exercised (helps disperse contrast)
How many ccs of positive and negative contrast are needed for arthrography?
5 cc of positive, 80-100 cc of negative
What does shoulder arthrography demonstrate?
Soft-tissue structures
How much positive and negative contrast is used for shoulder arthrography?
10-12 cc positive, 10-12 cc negative
What is needed for the needle placement for shoulder arthrography?
Fluoroscopic guidance
What is the positioning sequence for the shoulder arthrogram?
scout AP projection
internal and external rotation
glenoid cavity (AP oblique)
inferosuperior axiolateral or
interubercular groove
What is a hysterosalpingography (HSG)?
Radiographic demonstration of the female reproductive tract with a contrast medium
What does the hysterosalpingography (HSG) demonstrate?
The uterus and the fallopian tubes (degree of openness) of the female reproductive system
What are the pathological indications for hysterosalpingography?
infertility
demonstrates any intrauterine pathology (lesions)
to evaluate the fallopian tubes after a tubal ligation or reconstructive surgery has been done
What are the contraindications for hysterosalpingography?
Pregnancy, acute pelvic inflammatory disease and active uterine bleeding
Approximately how much contrast is injected for a hysterosalpingography?
10 ccs of a positive contrast
What are the technologists responsibilities for a hysterosalpingography?
explaining the procedure to the patient
consent form
room prep (fluoro and tray set up)
have contrast ready for the OB/rad
assist the OB/rad with running the equipment and moving the pt
How would you know that a hysterosalpingography (HSG) is abnormal?
Contrast doesn’t spill out to ends of fallopian tubes
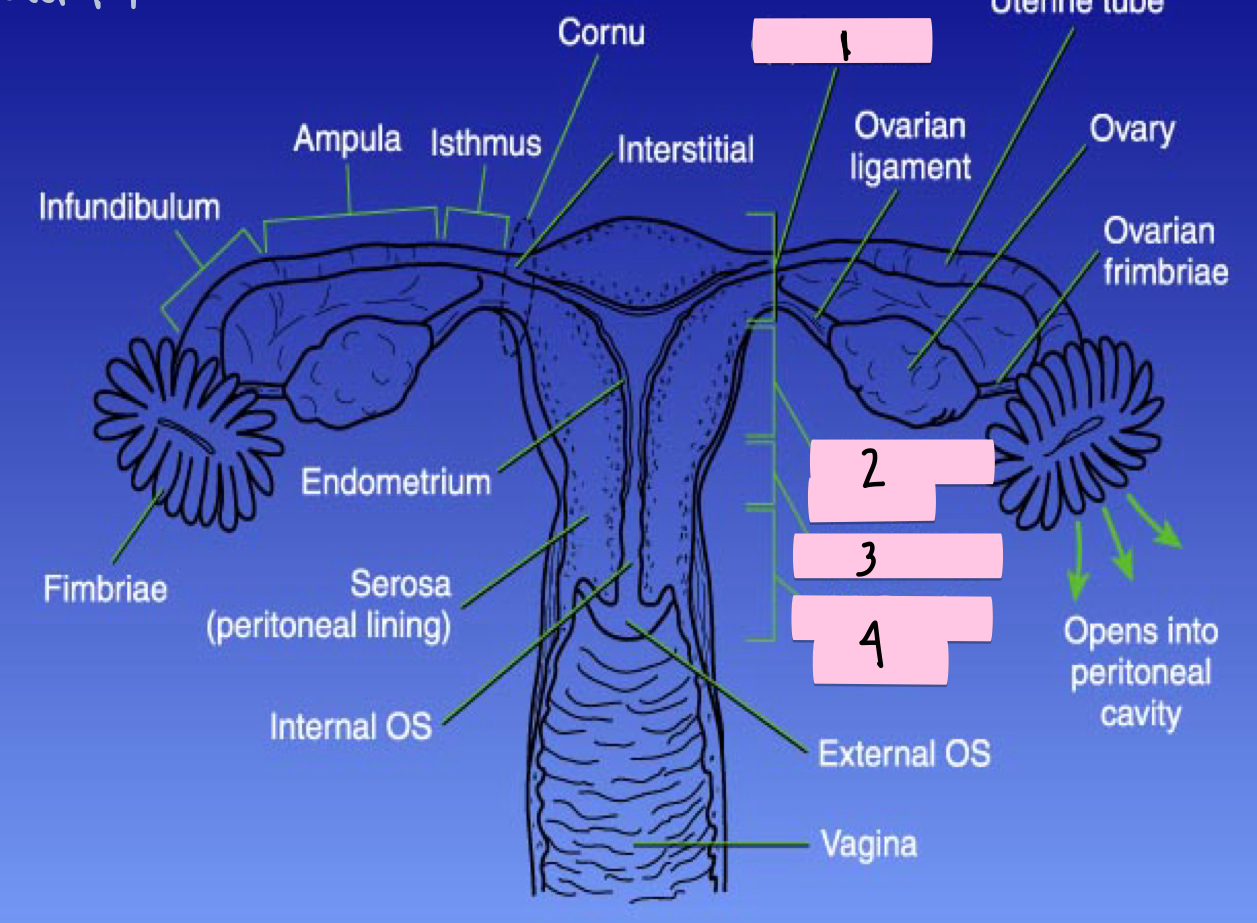
What is 1 pointing to?
Fundus
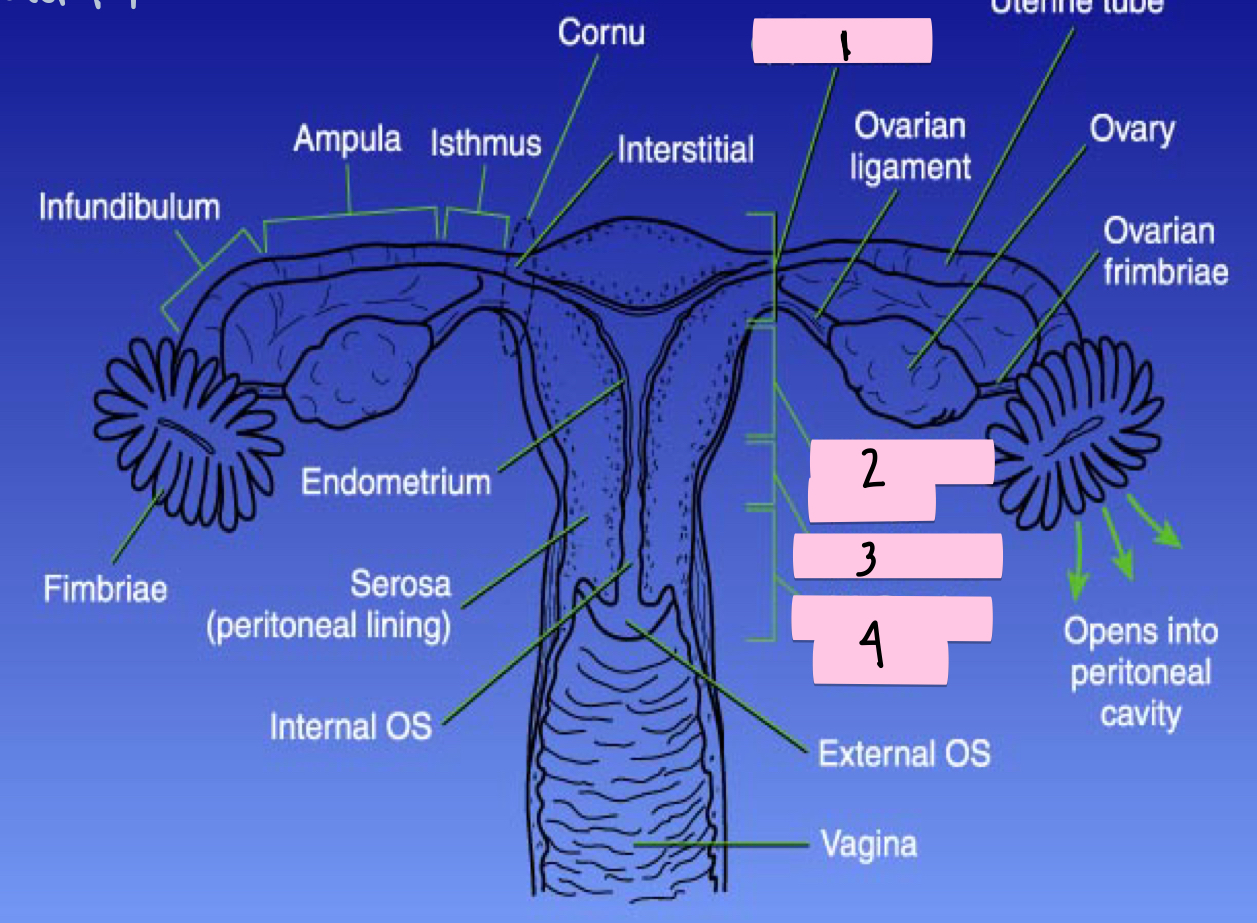
What is 2 pointing to?
Corpus (body)
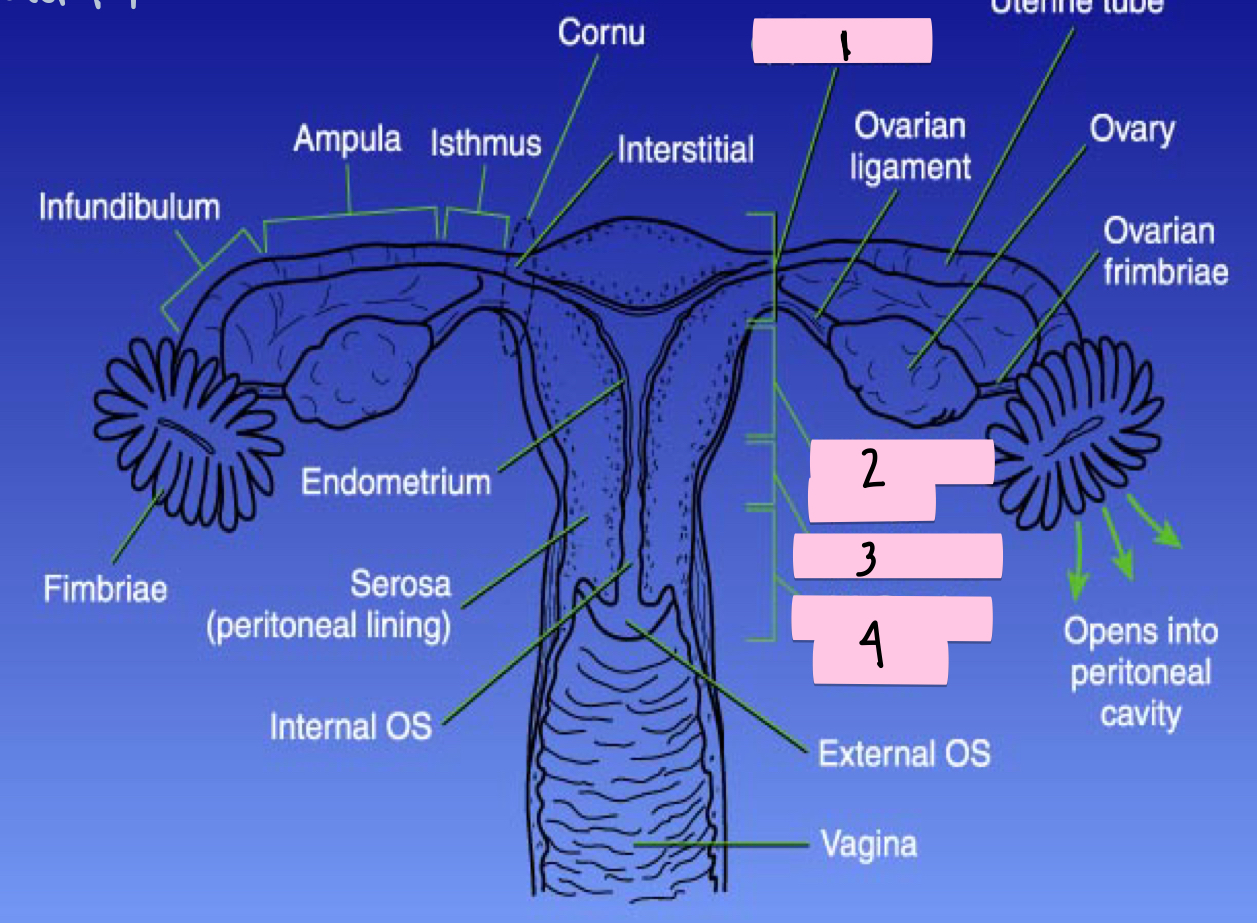
What is 3 pointing to?
Isthmus
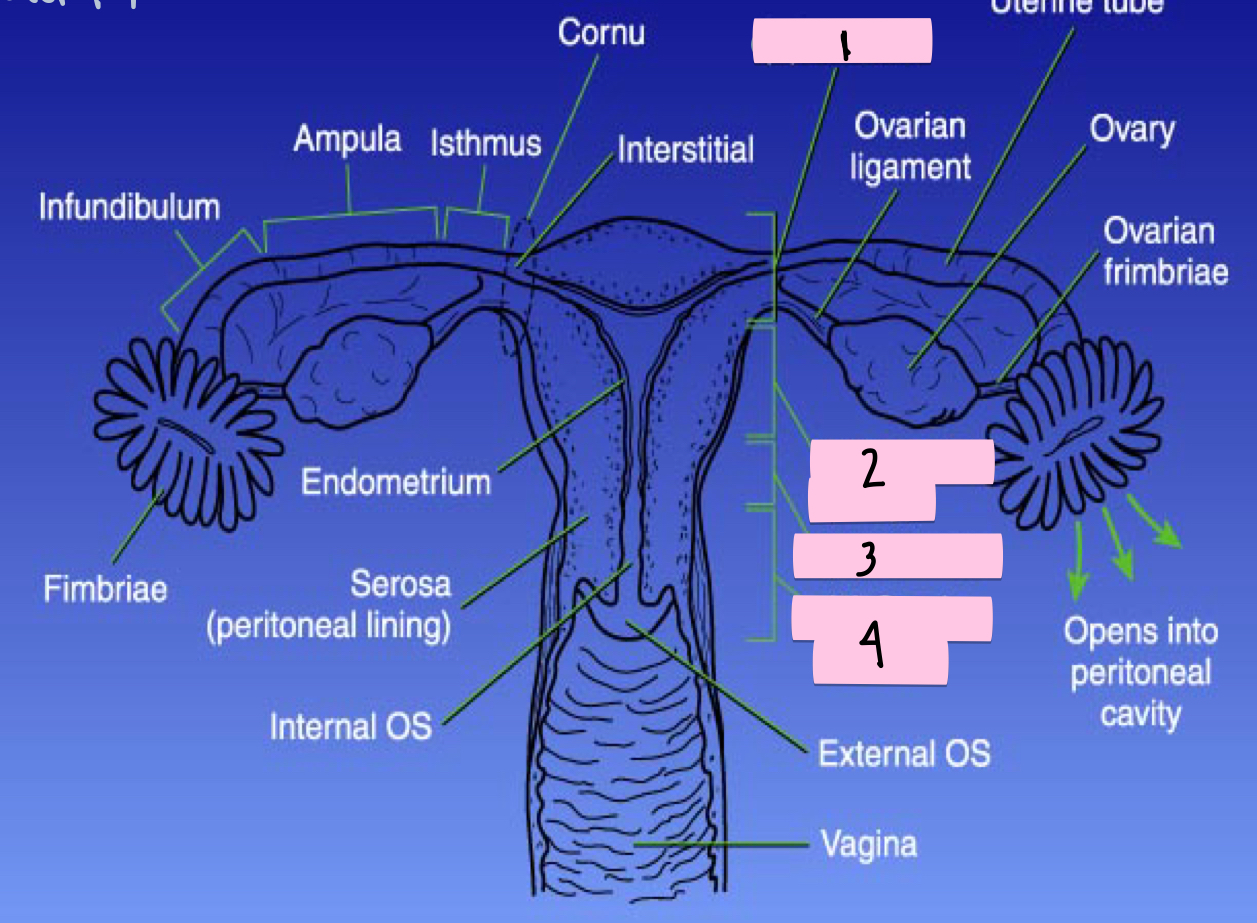
What is 4 pointing to?
Cervix (neck)
What else should you grab for the HSG kit that it usually doesn’t come with?
Separate cervical catheter/HSG catheter and a pad/feminine hygiene product for after exam
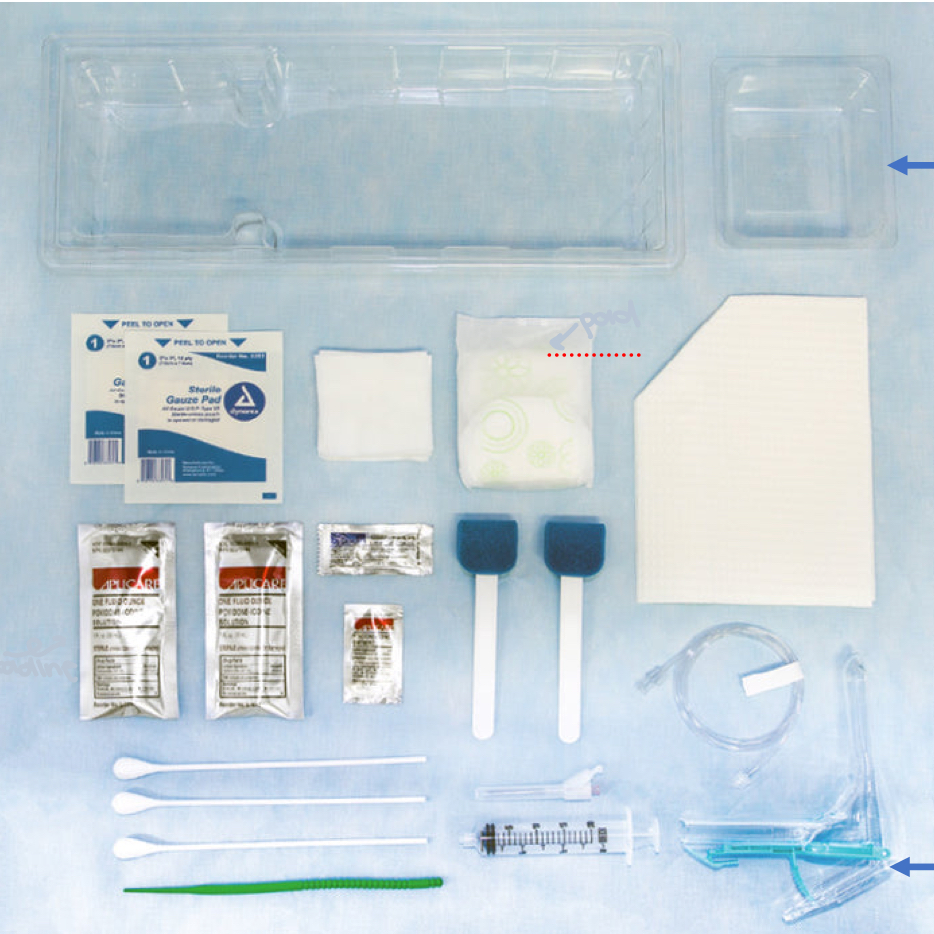
What type of procedure is this tray used for?
Hysterosalpingography
What should you see in your image for the HSG?
pelvic ring centered
cannula/catheter visible within cervix
opacified uterine cavity and tubes visible
contrast medium seen in peritoneum
What is myelography?
A radiographic stick of the spinal cord and its nerve root branches with a contrast medium
What has greatly reduced the number of myelograms done?
MRI and CT
True or false: for myelography sometimes the patient is admitted for the study and may leave later that same day
True
What are the pathological indications for myelography?
When a pt’s symptoms indicate the presence of a lesion, a herniated nucleus pulpous (most common reason), tumors, cysts, and bone fragments (trauma)
What are the contraindications for myelography?
blood in the cerebrospinal fluid
arachnoiditis
increased intracranial pressure
recent lumbar puncture (within 2 weeks)
What are the technologists responsibilities for myelography?
explain the procedure to the patient, and consent signed
room prep- trays, IRs, shoulder and foot harness, large pillow or sponge
get contrast ready for doctor (make sure it’s the right one)
assist doctor during procedure (moving pt, getting supplies, changing spot films, collecting CSF- mark vials as they come out)
after films- shoot throughs and erect
transport to CT
Why is knowing the needle placement for myelograms important?
The doctor may want the patient on their side, prone, or even sitting up
If your patient is prone for a myelogram what else do you need?
Sponge under their belly
How are the exams done for the myelogram?
explain procedure to pt
tell pt table will be moving during exam, including being angled to help move contrast through spine
scout of lateral lumbar
radiologist will perform exam
some post films done by radiographer
What should you make sure to do with your pt after the myelogram is done?
Keep patients head elevated slightly (30-40 degrees) to avoid contrast media passing into cerebral ventricles
What will happen if contrast media moves upward after a myelogram?
Patient will get a spinal headache/migraine
What are the most common injection sites for myelograms?
L3-L4 and C1-C2
How many ccs are injected for the myelogram and where are they injected into?
9-15 ccs into the subarachnoid space
Why is L3-L4 a common in section site for the lumbar myelograms?
The conus medullaris is here, where the spinal cord tapers off (not a solid cord)

What procedure is this tray used for?
Myelogram
What is the needle placement and injection process for the myelogram?
skin prep
lumbar puncture (prone or left lateral position)
CSF sample collected
contrast medium instilled
needle removed
How do you get CSF out of the spinal cord?
Do not suck it out, it must drip out on its own
What color is CSF?
Clear
What type of contrast is used for a myelogram?
Ionic or nonionic, water soluble iodine based
What views do you do for the cervical myelogram?
transcervical lateral- CR to C5
swimmers lateral- CR to C7
What views do you do for the lumbar myelogram?
semi-erect trans abdominal lateral- CR to L3
possible additional views- anterior obliques, PA/AP
What is sialography?
Radiographic examination of the salivary glands and associated ducts with a contrast medium
What has widely replaced sialography?
MRI and CT
What are the accessory organs of digestion located within and adjacent to the oral cavity?
Teeth and salivary glands
What do the salivary glands do?
Secrete the majority of the saliva found within the oral cavity that helps to dissolve food and facilitate digestion
How do the salivary glands communicate with the mouth?
Via the ducts
What are the three major salivary glands?
parotid
submandibular
sublingual
Parotid salivary gland
Largest
Submandibular salivary gland
Second largest
Sublingual salivary gland
Smallest
What are the other associated ducts?
parotid duct- AKA Stenson’s duct
submandibular duct- AKA submaxillary or Wharton’s duct
ducts of rivinus- 12 small ducts, one or two are larger and are referred to as Bartholin’s ducts
When is an sialography exam done?
pt’s symptoms indicate a potential pathologic process of the salivary duct or gland
can include obstruction of the duct by a stone; stricture or tumors located within the duct
also can be done to look for a possible fistula
What is a fistula?
Abnormal connection or opening between two different parts (not supposed to be connected but is)
What are the contraindications for sialography?
When the patients shows severe inflammation or allergy to the contrast
What are the technologists responsibilities for sialography?
explain the procedure
consent form
pt prep- remove dentures, jewelry
room prep- tray, fluoro working
get contrast ready for doctor- only need 1-2 mL
scout film
assist the doctor and pt through put the procedure
after films if needed
What is the purpose of sialogarphy?
To opacify salivary duct and glands to demonstrate potential pathology
What are the indications for a sialogram?
obstruction of the ducts by calculi, strictures, or tumors
sialectasia (dilation of a duct)
possible fistula
What is orthorentgenography- long bone study?
An exam to determine if there are any limb length discrepancies
Who do you usually do orthorentgenography studies on?
Adults or children, but more commonly children
True or false: orthorentgenography can be done for either upper or lower limbs, but more commonly done for lower
True
How do you do orthorentgenography?
You take three images on one film centered on three joints and coned into the particular joint
What are the three joints done for lower limb orthorentgenography?
Hip, knee, and ankle
What are the three joints done for upper limb orthorentgenography?
Shoulder, elbow, and wrist
What is the name of the ruler used for orthorentgenography?
Bell-Thompson, metallic markings
Where do you put the ruler for a long bone study?
Under the patients limb and tape it to the table
What is a more modern way to do a long bone study?
Using image stitching
What are the indication for orthorentgenography?
back pain due to difference in the length of legs
developmental anomalies
epiphysiodesis- surgical procedure to shorten a limb
bone-lengthening surgery
Epiphysiodesis
Surgical procedure to shorten a limb
What is bone densitometry?
Specialty that uses various method in assessing bone mineral density for diagnosis of osteoporosis
What are the three most commonly used bone denstometery tests?
dual energy x-ray absorption- DXA
quantitative computer tomography- QCT
quantitative ultrasound- QUS
Dual energy x-ray absorptiometry (DXA)
most common method
uses both high and low energy range for maximum attenuation differences
scout image for correct positioning and artifacts
What is a Z-score in bone densitometry?
Compares patient to an average individual same age and sex
What is a T-score in bone densitometry?
Compares person to someone young and healthy
Quantitative computer tomography (QCT)
provides analysis of attenuation data as individual slices or provides a 3D analysis
costs more and the patient dose is higher than for other methods
Quantitative ultrasound (QUS)
non ionizing technique using ultrasound
peripheral site selections such as the os calcis
provides quick and simple measurements for screening purposes
What is conventional tomography?
Special type of imaging used to obtain a diagnostic image of a specific layer of tissue or object that is superimposed by other tissues or objects
What are the five types of tube trajectories (way the tube moves over the body) in conventional tomography?
linear
elliptical
circular
spiral
hypocyclodial
Fulcrum
Pivot point through which the x-ray tube and IR move
What are the two types of fulcrum levels?
fixed
variable
Fixed fulcrum level
Adjust the table height not the fulcrum
Variable fulcrum level
Fulcrum level is moved not the table height
How can you determine you starting fulcrum level?
First take two scout films (AP and lateral) to locate the area of interest, then according to what your scout films show, set your fulcrum level
What are the four influencing and controlling factors which determine the amount of blurring in conventional tomography?
distance the object is from the objective plane
exposure angle
distance the object is from the IR
tube trajectory
Objects within the body that are (closer or farther) from the focal plane have greater blurring
Farther
True or false: if the arc of the tube movement increases the blurring increases
True
True or false: the straighter the line of the tubes trajectory the less blurring that occurs
True
What are the other conventional tomography methods?
breathing technique
pantomography- panorex unit
digital tomosynthesis