cvrs
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
How is the skin adapted to protect against environmental insults?
Skin:
Physical barrier of the skin
Stratified squamous keratinised epithelium:
Multiple layers of keratinocytes, where the keratin they release makes stronger barriers.
Keratinocytes have TLR receptors that detect viruses and bacteria and stimulate the release of cytokines (increase body temp) and chemokines (attract immune cells).
They also produce AMPs that can cause microbe death.
Melanocytes: cells in the epidermis that protect the skin from UV rays.
Langerhans cells: ‘scavenger cells’ that help induce the immune response.
Sebaceous glands: produce sebum that has waterproof and anti-microbial properties.
Commensal flora: ‘good bacteria’ that form a barrier against pathogens reaching the skin.
How is the respiratory tract adapted to protect against environmental insults?
Respiratory system:
Mucus:
Contains water, electrolytes, glycoproteins and lipids
Also contains antimicrobial compounds like lysozymes, transferrin and lactoferrin.
Antibodies and antioxidants
Secreted by the goblet cells, lines both the respiratory and alimentary tracts.
Mucociliary escalator:
Where mucus gets trapped and moved by the cilia on epithelial cells. This therefore also traps microbes and pathogens and moves them out of the lungs.
Alveolar macrophages: white blood cells that phagocytose pathogens.
How is the alimentary tract adapted to protect against environmental insults?
Alimentary tract:
Stratified squamous epithelium
Lysozymes in saliva
Acidic pH in stomach
Mucus lining of stomach
Cryptdins in small intestine: are toxic to bacteria
Lymphoid tissue in the GIT:
Induce immune response
e.g. Peyer’s patches: made of lots of T and B cells and so produce lots of antibodies that are secreted into the tract and form a mucosal antibody barrier.
What are the functions of the cardiovascular system?
Transport of oxygen and substrates to tissues.
Transport of carbon dioxide and metabolites away from cells.
Distribute hormones
Transport defence molecules
Haemostasis
Thermoregulation
What are the components of the cardiovascular system?
Heart:
Muscle, beats roughly 70x per minute.
2 atria and 2 ventricles
Intrinsic pacemaker and autonomic nervous stimulation
Vessels:
Arteries (away from heart)
Veins (to heart)
Microcirculation (exchange with tissues - capillaries)
What are some differences between mammalian cardiovascular systems and the systems in other species?
Mammals, birds and crocodilians have a fully developed septum with a dual circulatory system - the right side of the heart has a lower pressure and the left has higher pressure.
Fish have a single circulatory system, with one atria and one ventricle.
Amphibians have a double circulatory system with two atria and one ventricle.
What is systolic and diastolic pressures?
Systolic pressure: highest pressure during contraction
Diastolic pressure: lowest pressure, during relaxation
Label this diagram of the heart, including chambers, vessels, membranes and valves.
Where do you listen for the sound of heartbeats?
REMEMBER PAM
Between ribs 3 and 4: pulmonary valve
Between ribs 4 and 5: aortic valve
Between ribs 5 and 6: left atrioventricular valve (mitral)
What is the cardiac skeleton?
A fibrous connective tissue that supports the muscle. It insulates and therefore directs the electrical impulses.
What are the differences between arteries and veins?
Arteries are round, veins are flattened
Arteries are thick walled, veins have thinner walls
Tunica adventitia:
arteries - collagen and elastic fibres, nerve endings, vasa vasorum (vessels that supply the vessels)
veins - collagen and elastic fibres, smooth muscle, nerve terminals
Tunica media:
arteries - thick, smooth muscle and elastic fibres, external elastic membrane
veins - thin, smooth muscle and collagen
Tunica intima: Arteries - rippled, internal elastic membrane; veins - smooth
Describe the relationship between blood flow and resistance.
Blood flow is inversely proportional to resistance.
Use the equation blood flow = pressure gradient/resistance
Describe what occurs in terms of fluid movement in the capillaries.
There are two forces:
Hydrostatic pressure: exerted by the blood
Oncotic pressure: pressure exerted by proteins
These cause 4 opposing forces - 2 forces in the capillaries, 2 forces outside
This causes a net movement of fluid out of the capillaries from the arteriole to venule end. This fluid becomes lymph.
This travels through the lymphatic system and collects in the thoracic duct and empties back into the blood by the vena cava.
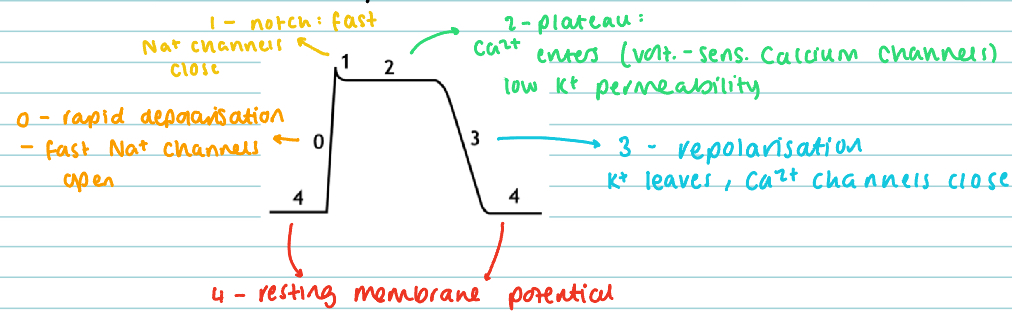
Describe the origin and propagation of the heartbeat.
The SA node in the right atrium depolarises spontaneously:
This starts with a slow depolarisation, where leaky sodium channels allow the slow movement of Na+ ions in. There’s some Ca2+ channels open too.
When the threshold voltage is reached, there is faster depolarisation via voltage sensitive Ca2+ channels.
The spontaneous depolarisation is resting heart rate.
The signal travels along the Purkinje fibres (specialised cardiac myocytes).
The conduction travels from the SA node to the atrial muscle, to the AV node, to the bundle of His, along the Purkinje fibres and to the ventricular muscle.
The muscle is then repolarised. The other channels close, K+ channels open. K+ moves in and this allows depolarisation.
What are the features of cardiac muscle?
The muscle is a functional syncytium - all behave the same
High mitochondria count for continuous supply of ATP for contraction
Intercalated discs: junctional proteins that allow connections
What makes cardiac muscle contract, and what pathway does the action potential take?
The cause of contraction is the entering of Ca2+ ions into the cell (in phase 2). This causes calcium-induced calcium release: calcium stored in the sarcoplasmic reticulum is released into the cytosol. Calcium combines to form troponin C, which causes tropomyosin to move away from the myosin binding site and muscle contraction can occur.
How does cardiac muscle relax?
By removing the Ca2+ ions.
This is done through a few ways:
Calcium pump out of cells
Ca2/Na+ exchanger
Ca2+ pump back to the sarcoplasmic reticulum.
Describe the steps of the cardiac cycle.
Atrial contraction: blood enters the ventricles
Isovolumetric contraction: systole starts but all valves are closed so there is no volume change.
Rapid ejection: where blood leaves the ventricles and enters arteries.
Reduced ejection: where the blood leaving wanes slightly.
Isovolumetric relaxation: again, valves are closed
Rapid filling: ventricles filling
Reduced filling
What are the heart sounds?
S1-S4
You always hear the ‘lub-dub’ of S1 and S2
S1 is the closure of the AV valves (systole)
S2 is the closure of the SL valves (diastole)
You can sometimes hear S3-S4, depending on age and species or pathology. And you can always hear it in horses.
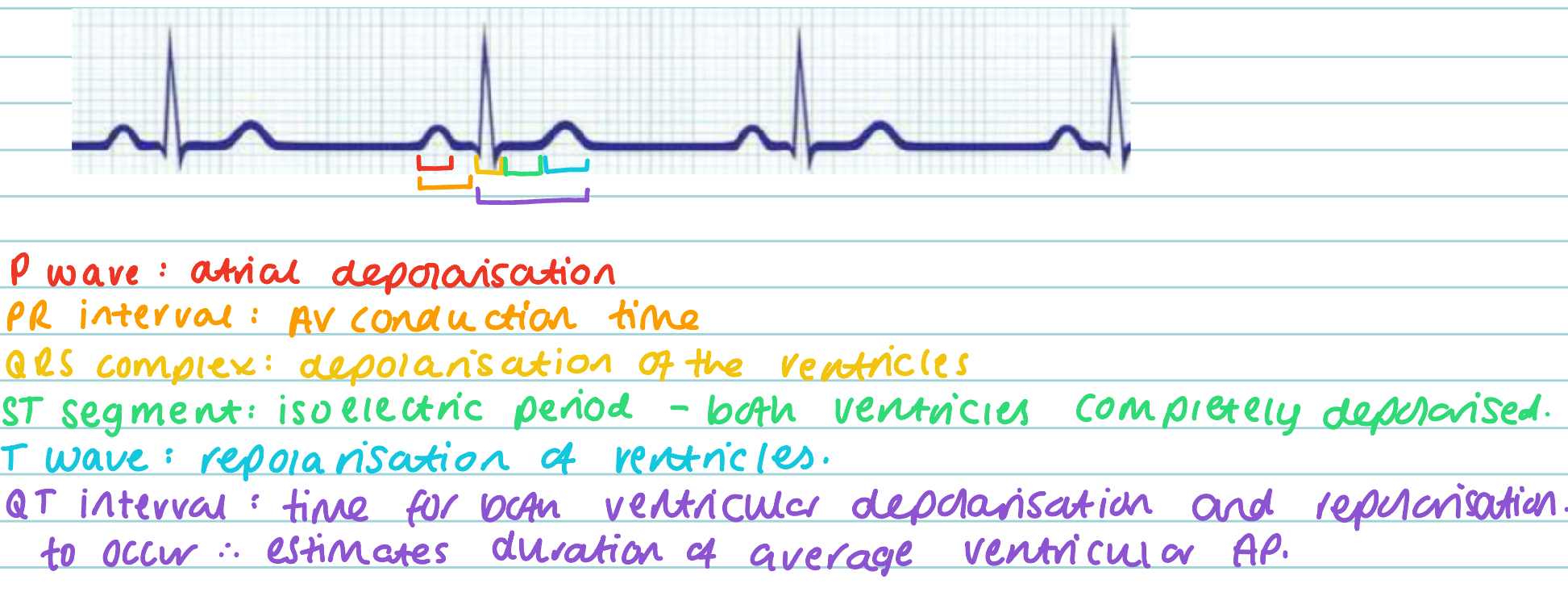
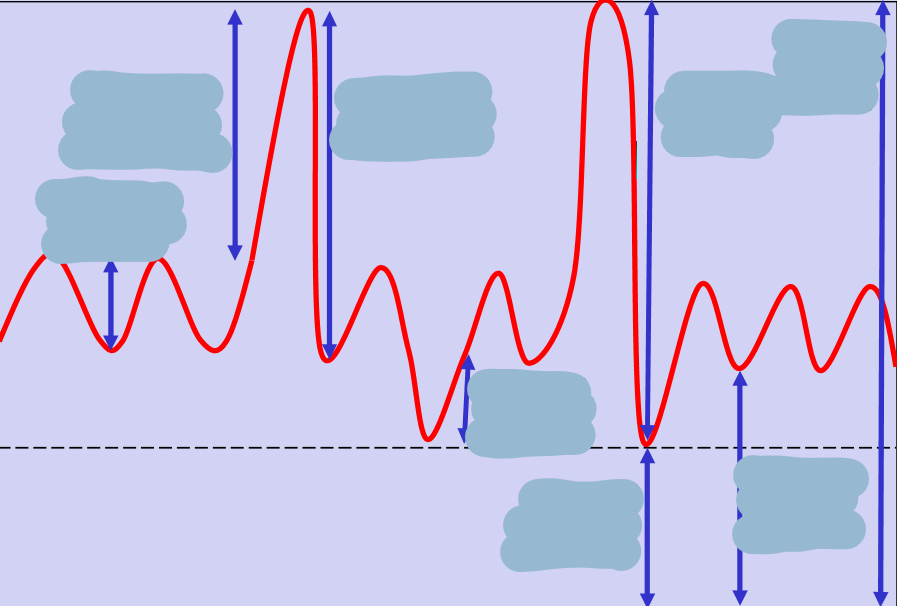
Describe the parts of an ECG wave.
Define cardiac output, preload, afterload and stroke volume.
Cardiac output: the amount of blood being pumped into the aorta per unit time. (This should be equal to venous return). L/Min
Preload: the filling pressure of the heart
Afterload: the pressure against which the heart ejects.
Stroke volume: volume put out with each stroke of the heart. mL
Describe the relationship between cardiac output, stroke volume and rate.
The relationship can be defined by the equation:
cardiac output (L/min) = stroke volume (ml) x heart rate (bpm)
Therefore the factors of cardiac output are:
Heart rate
Stroke volume:
Contractility
Preload
Afterload
What influences heart rate? Talk about the systems and their nerves/fibres.
Both the parasympathetic and sympathetic nervous systems play a role:
Parasympathetic: the vagus nerve (cranial nerve 10) innervates all regions and a little bit the atria, but nothing to the ventricles. They release acetylcholine that binds to muscarinic receptors and slows HR
Sympathetic: adrenergic fibres innervate all parts of the heart. They release noradrenaline which binds to β-adrenoreceptors and increases HR.
At rest, parasympathetic effects dominate, so to increase heart rate, you decrease the vagal tone and increase sympathetic tone.
Describe the effects of the different nervous systems on pacemaker potentials and the AV node.
Pacemaker potentials:
Sympathetic: increases slope of depolarisation so it reaches the threshold more quickly.
Parasympathetic: slower depolarisation so less heart beats.
AV node:
Parasympathetic: increases the AV refractory period and decreases the AV conduction, leading to a slower heart rate.
Sympathetic: decreases AV refractory period and increases AV conduction, so a faster heart rate.
How is stroke volume regulated?
The factors are contractility, preload and afterload:
Contractility: Is a measure of the force generated by cardiac myocytes.
Preload: The greater pressure filling the ventricles means more blood, so myocytes stretch more and therefore have greater contraction.
Venous return is also a factor of preload. This can be affected by vasoconstriction, the skeletal muscle pump and the thoracic pump (where central venous pressure will fall during inspiration, so the pressure gradient encourages blood back to the heart).
Afterload: Determined by peripheral resistance, which is proportional to arterial pressure. Increased afterload means more contractility is needed to maintain the cardiac output, therefore the sympathetic nervous system is increased.
So overall:
Intrinsic regulation: the mechanical properties of the myocytes
Extrinsic regulation: Sympathetic stimulation
What are the determinants of blood pressure?
Systemic arterial pressure is the major determinant of tissue perfusion pressure.
This is controlled by a negative feedback system, with both short term and long term mechanisms.
Short term:
Autonomic nervous system - baroreceptors
Long term:
Control of fluid volume by kidneys, involving vasopressin and the renin-angiotensin-aldosterone system
Diastolic pressure is directly proportional to total peripheral resistance, which is determined by arteriolar tone.
So, this forms the equation cardiac output = arterial pressure/TPR, which can be rearranged to MAP = CO x TPR
And the equation for cardiac output can therefore be substituted into this: MAP = (HR*SV) x TPR
Define systolic and diastolic arterial pressures.
Systolic arterial pressure: peak pressure in arteries when left ventricle is ejecting blood during systole.
Diastolic arterial pressure: residual pressure in the arteries when the left ventricle is filling during diastole.
Blood pressure measurements are systolic over diastolic.
Describe the reflex control of blood pressure.
This is short term control, requiring sensors, an integrating system (the brain) and effectors (heart and blood vessels).
Sensors: baroreceptors - nerve endings in the adventitial layer of blood vessels, mainly found in the aortic arch and carotid sinus. They monitor pressure changes.
The axons terminate in the medulla oblongata.
The receptors are mechanoreceptors, so respond to mechanical distortion.
Acute rise in BP:
Increase in blood pressure means more vessel stretch, so increased discharge of baroreceptors.
The signals travel to the medulla oblongata.
Blood pressure needs to fall, so the equation MAP = (HR*SV) x TPR needs to be affected.
Vagal output increased - slows heart rate
Sympathetic output decreased - reducing heart rate, hence reducing contractility (stroke volume), and also arteriolar tone will decrease (reducing TPR).
This all reduces blood pressure.
Acute fall in BP:
Opposite of above - push sympathetic stimulation and stop parasympathetic system
Constrict arterioles and veins, increasing TPR
Increase heart rate and contractility, increasing cardiac output.
Decrease parasympathetic outflow, increasing heart rate.
Increasing all factors increases MAP.
Describe the long term control of blood pressure.
There is a link between changing circulating volume and changing blood pressure.
Increase circulating volume, and you increase preload, which causes higher contractility and therefore, a higher stroke volume. This means a higher cardiac output, which increases mean arterial pressure.
The renin-angiotensin-aldosterone system plays a role in the long-term control of blood pressure.
In the case of low blood pressure, there will be less renal perfusion, which causes the release of the hormone renin from the macula densa cells in the kidney. This can also be caused by sympathetic stimulation.
Renin causes the conversion of the peptide angiotensinogen into the shorter peptide angiotensin I. The enzyme ACE then catalyses the conversion of this into angiotensin II, which then plays multiple roles:
1. It travels in the circulation to the adrenal gland, where the adrenal cortex is stimulated to produce the hormone aldosterone, which causes retention of Na+ and therefore of water in the kidney. This increases plasma volume, increasing preload and hence increasing cardiac output and therefore increasing blood pressure.
2. It also travels to the posterior gland, stimulating the release of vasopressin, which increases water retention and therefore plasma volume, causing the same effect as above.
3. Finally, it binds to receptors in the smooth muscle of the arterioles, causing vasoconstriction, increasing TPR and therefore increasing blood pressure.
There are also volume receptors in the atrial walls. They are low pressure stretch receptors.
In the case of blood volume increase, signals are sent to the brain and mechanisms are deployed to decrease blood volume.
They inhibit sympathetic vasoconstrictor pathways to the kidney, leading to diuresis (more urine) so fluid is expelled from body.
They also inhibit the secretion of ADH, so less water is retained and more is expelled in urine.
These things reduce blood volume, reducing central venous pressure (a determinant of preload, therefore) reducing stroke volume and therefore reducing cardiac output and arterial pressure.
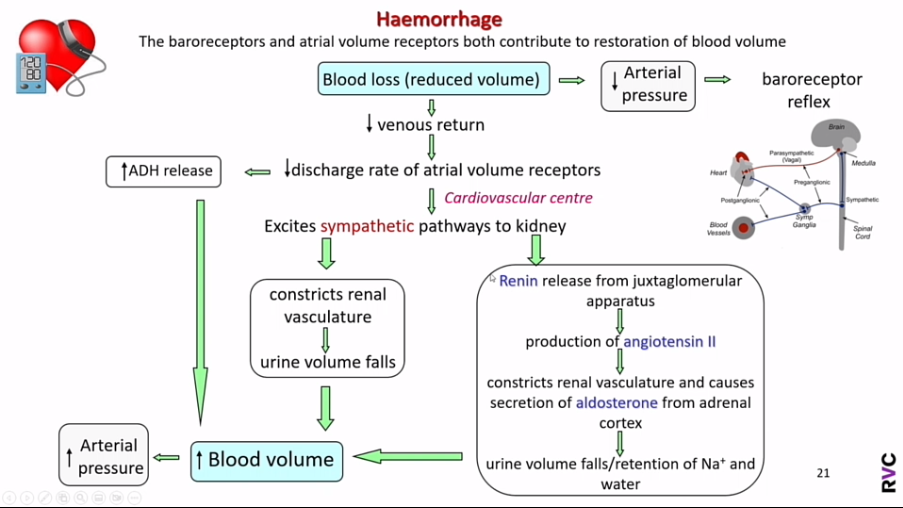
Describe how the cardiovascular system will respond to blood loss.
Haemorrhage is blood loss, so will reduce blood volume. The system will try to restore blood volume.
Firstly, the blood loss will cause a lower arterial pressure, which will stimulate the baroreceptor reflex to:
Switch off the parasympathetic system and switch on the sympathetic system, therefore increasing heart rate and stroke volume - so higher cardiac output.
Increase total peripheral resistance.
Secondly, the blood loss will cause a lower venous return. This decreases the volume in the atria, so the atrial volume receptors will have a reduced discharge rate. This leads to two things:
It excites sympathetic pathways to the kidney.
Firstly, this constricts renal vasculature, causing urine volume to fall and blood volume to increase.
The sympathetic drive also stimulates the release of renin and hence the production of angiotensin II, which constricts renal vasculature and also causes aldosterone to be secreted. These things also cause blood volume to increase.
It stimulates the release of ADH, increasing blood volume and therefore arterial pressure.
Fill in the diagram with the correct terms and define them.
What are the functions of the respiratory tract?
To maintain correct concentrations of oxygen, carbon dioxide and hydrogen ions in the tissues.
Non-respiratory functions:
Blood pressure regulation by ACE
Thermoregulation
Speech
Immune defence
Acid-base balance
Filter out particulates
Describe the general structures of the lungs and the variations between species.
Left lung:
All domestic species have two lobes (cranial and caudal).
The cranial lobe is typically divided into two parts (cranial and caudal).
The horse does not appear to have two lobes, because it has no fissure, however it does have two lobes determined by the branching of the principal bronchi.
Right lung:
Four lobes: cranial, middle, caudal and accessory.
The accessory lobe sits tucked under the heart, and aims to use up all space not taken by the heart, ensuring all thorax volume is taken up.
Ruminants appear to have five lobes, but it is simply the cranial lobe being split as in the left lung.
Ruminants and pigs have a tracheal bronchus - splits off from trachea before principal split of the bronchi - supplies the cranial lobe.
Define the costal pleura.
The pleural membrane lining the inner side of the thoracic walls formed by the ribs.
Define the diaphragmatic pleura.
The pleural membrane covering the cranial surface of the diaphragm.
Define the visceral pleura.
The pleural membrane covering the lungs. It contains plenty of elastic fibres to allow the movement of the lungs.
Define the mediastinal pleura.
The pleural membrane forming the mediastinum.
Define the parietal pleura.
The pleural membrane lining the pleural cavity, that can be divided into the costal pleura, the mediastinal pleura and the diaphragmatic pleura.
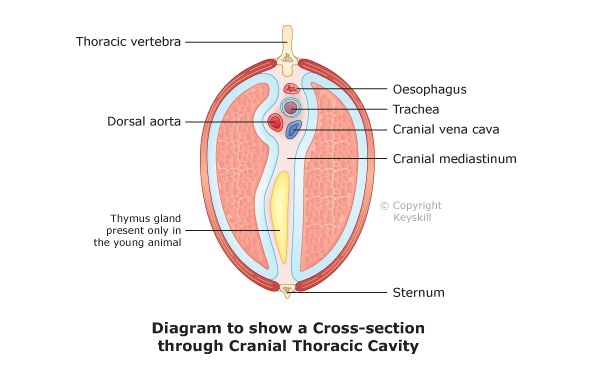
What is the mediastinum?
The division between the two pleural cavities. It is formed from two layers of mediastinal pleura with a potential space between them. The heart, trachea, oesophagus and the major blood vessels lie in the space between the two layers of the mediastinal pleura.
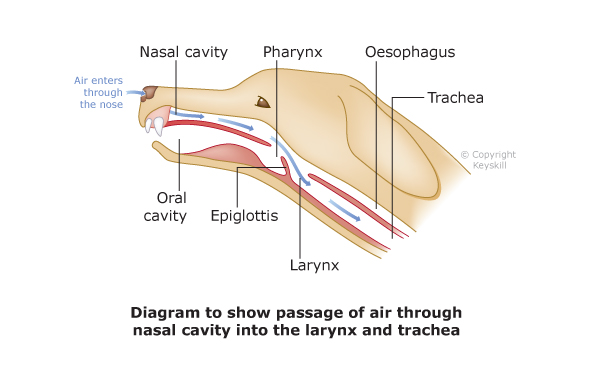
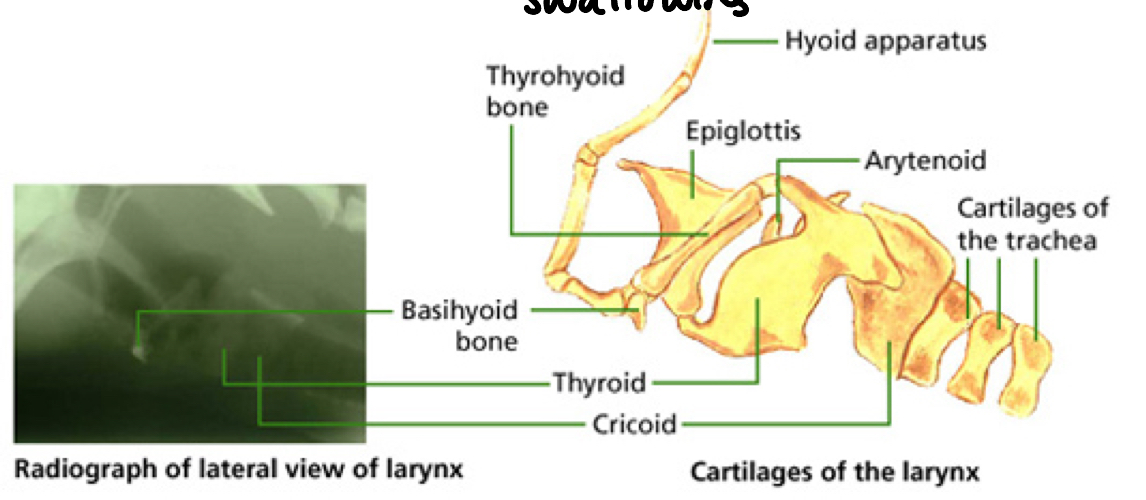
Describe the structure of the upper respiratory tract, using the diagram to help.
Pharynx: a muscular tube formed by the nasopharynx and the oropharynx. It lies at the back of the oral and nasal cavities and a number of structures open into it.
Larynx: air passes from the pharynx to the larynx. It is made of interconnecting cartilages (epiglottis, thyroid, cricoid and the arytenoids) linked by ligaments. It is attached to the skull by the hyoid apparatus.
Epiglottis: a cartilage of the larynx that closes over the trachea when food is swallowed.
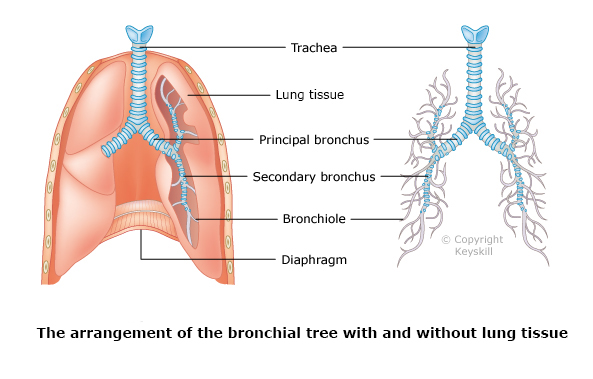
Describe the structure of the lower respiratory tract.
Trachea: tubular structure that passes down the neck and into the chest. Air flows through the trachea to the lungs. It lies ventral to the oesophagus and slightly to the left. It bifurcates just cranial to the base of the heart, into two principal bronchi. It is lined with ciliated columnar mucous membrane.
Bronchi: air travels from the trachea into the bronchi. Similar structure to the trachea, but with no cartilage and a smaller diameter. The principal bronchi enter its own lung and divides again into secondary bronchi, which supply the lobes of the lung. These then divide into bronchioles.
Bronchioles: These are kept open by cartilage rings lined with ciliated epithelium. They continue to divide and terminate in pulmonary bronchioles and alveoli (also lined with ciliated mucous membrane).
Alveoli: lined with type I and II epithelial cells. Type I is a thin epithelium while type II secretes surfactant. The alveoli and the capillaries next to them share a basement membrane, to allow for short diffusion distances. Alveoli are also interconnected by sharing septum with other alveoli, to protect against alveolar collapse. Pores of Kohn between alveoli allow efficient movement of inspired air between alveoli.
What is compliance, and what structure in the body have high compliance?
Defined by the equation compliance = change in volume/change in pressure.
Both the lungs and veins have high compliance - a small change in pressure leads to a large change in volume.
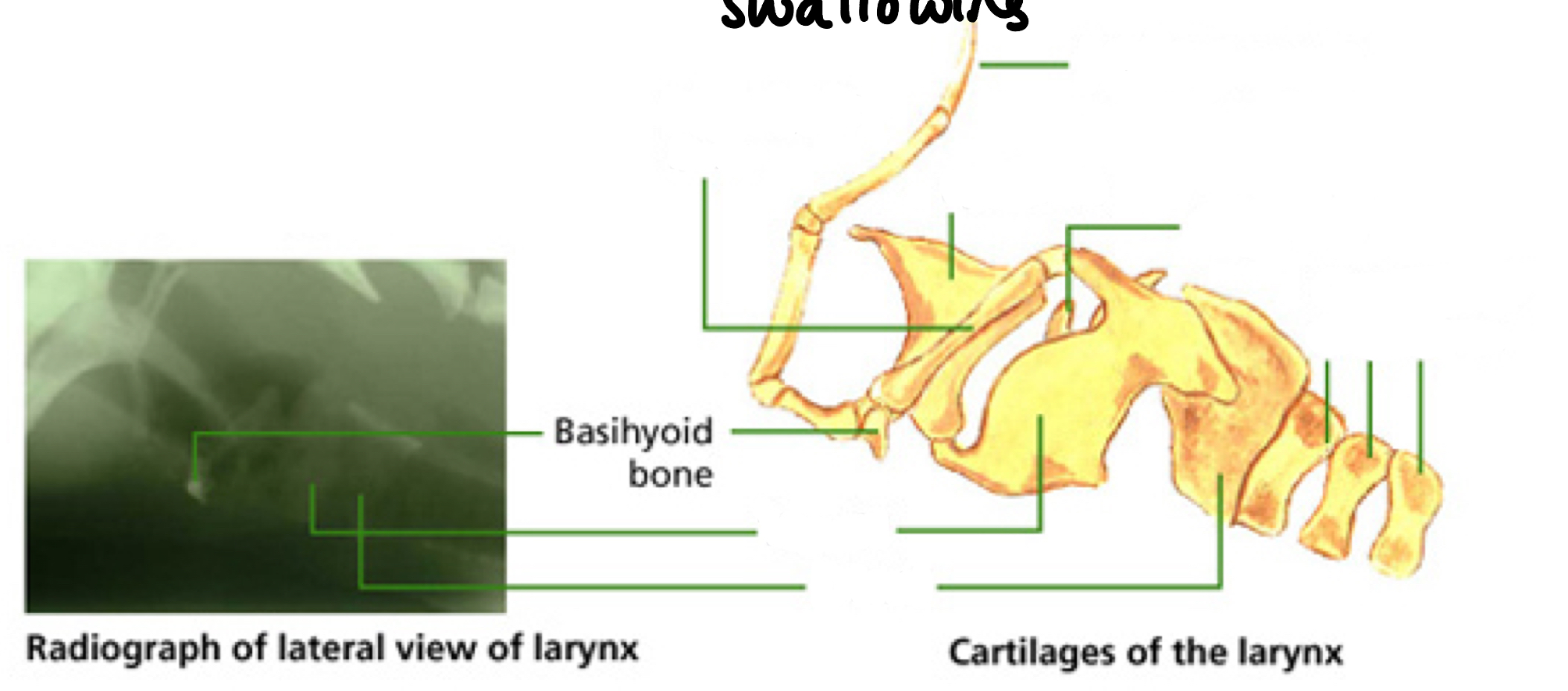
Use this diagram to name the parts of the larynx.
What is the role of surfactant in ventilation?
It increases lung compliance, making it easier to expand, meaning less energy is needed to inflate the lung. It also stops the collapse of alveoli by working against surface tension.
Describe the process of inspiration.
The phrenic nerve (C3-C5) stimulates the diaphragm to contract and flatten, enlarging the thoracic cavity. The ribs move up and out by way of the external intercostal muscles contracting. The thoracic pressure is now less than atmospheric pressure and air moves into the lungs.
Describe the process of expiration.
This is a passive action where the diaphragm and external ICMs relax and all returns to its original position. This reduces the volume of the thoracic cavity, increasing pressure and forcing air out.
What is different about expiration in horses?
It is biphasic, first passive, then active, even at rest.
Describe the blood circulations in the lungs.
Pulmonary circulation: brings low pressure venous blood to the lungs for gas exchange. A large volume system.
Bronchial circulation: A low volume but higher pressure system from the aorta that brings oxygen and nutrients to the lung cells. This blood is returned to the right side of the heart as normal (via vena cava) but also to the left side via the right to left shunt, which happens through anastomoses between the two circulations.
What happens during hypoxic vasoconstriction?
Capillaries near to hypoxic alveoli are constricted to direct blood flow to areas with better oxygenated alveoli.
How are pulmonary embolisms overcome?
Enlarging the bronchial arteries to increase flow rate.
Angiogenesis - producing new bronchopulmonary arterial anastomoses.
How does oxygen diffuse into tissues from capillaries?
There is a large oxygen pressure difference between the capillary and the interstitial fluid, so there is a rapid diffusion of oxygen into the tissues.
What factors affect gas exchange?
Fick’s law:
Area of the respiratory surface
Thickness of the respiratory surface (e.g. scar tissue or damage can thicken it)
PO2 differences between the alveolus and the capillary
Pulmonary oedema (gas travels less efficiently through fluid than air).
Adequate ventilation:
Atelectasis (alveolar collapse) means no gas exchange can occur.
Tracheal/bronchial collapse can be due to trauma or old age
Bronchoconstriction of the bronchioles
Perfusion of the lung:
Pulmonary embolism
Hypoxia
What is the structure of haemoglobin?
2 alpha and 2 beta units forming one protein with a quaternary structure. Each sub unit has its own haem group.
What effect does pH have on the oxygen-haemoglobin dissociation curve?
Lower pH: can be due to exercise. Shifts the curve to the right, due to higher H+ levels that cause Hb to have a lower affinity for oxygen, so it offloads more easily (Bohr effect)
Higher pH: will shift the curve to the left.