EXAM 2 PATHOPHYSIOLOGY
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
116 Terms
Atrial septal defect
A congenital heart defect, a hole in the septum separating the left and right atria. This allows oxygenated blood from the higher-pressure left atrium to shunt to the lower-pressure right atrium, leading to increased blood flow to the lungs. Small defects may be asymptomatic, while larger ones can lead to pulmonary hypertension over time. bigger the hole, bigger the damage, increased volume means increased force to longs so it damages the vasclature of the lungs.
Ventricular septal defect
A congenital heart defect characterized by a hole between the left and right ventricles. This is the most common congenital heart defect, allowing blood to move from the higher-pressure left ventricle to the right ventricle, increasing blood flow to the lungs and the workload on the right side of the heart. Can cause heart murmurs, failure to thrive, and pulmonary hypertension if severe.
Patent ductus arteriosus
Before birth: every fetus has a vessel called the ductus arteriosus, which connects the pulmonary artery to the aorta. This connection is completely normal and necessary because the fetus does not breathe air or use its lungs for oxygen. Since the fetal lungs are filled with fluid and have very high resistance, blood takes a shortcut through the ductus arteriosus to bypass the lungs and flow directly into the aorta and out to the body.
After birth, when the baby takes its first breath, the lungs expand and fill with air. This causes lung pressure to drop and oxygen levels to rise, which signals the ductus arteriosus to close naturally within the first few days of life.
If it fails to close, the condition is called Patent Ductus Arteriosus (PDA). This means the connection between the aorta (a high-pressure vessel) and the pulmonary artery (a low-pressure vessel) remains open. As a result, blood flows from the aorta into the pulmonary artery, sending too much blood to the lungs. This can lead to pulmonary congestion, increased workload on the left side of the heart, and blood pooling in areas it shouldn’t, such as the lungs instead of the body’s tissues. Over time, this can cause pulmonary hypertension and even heart failure if untreated.
Tetralogy of Fallot
a congenital heart defect: causes low oxygen levels and bluish skin because oxygen-poor blood circulates through the body. It consists of four heart defects that occur together:
Ventricular septal defect (VSD): A hole between the right and left ventricles allows blood to move between them.
Pulmonary stenosis: Narrowing of the pulmonary valve or artery makes it hard for blood to flow from the right ventricle to the lungs. This increases pressure on the right side of the heart.
Overriding aorta: The aorta sits directly over the VSD, receiving blood from both ventricles. Because it’s handling blood from both sides, the aortic valve becomes enlarged from the stress.
Right ventricular hypertrophy: The right ventricle becomes thickened because it must work harder to push blood through the narrowed pulmonary valve.
Because of the high pressure caused by pulmonary stenosis, blood that normally flows left → right through the VSD is forced to go right → left instead. This means deoxygenated blood goes from the right ventricle into the aorta and out to the body instead of going to the lungs
cyanotic: oxygen levels in the blood drop, and the skin, lips, and nails can turn bluish.
Cardiogenic shock
when the heart can’t pump effectively, so the body’s tissues don’t get enough oxygen.
often occurs as a result of a heart attack (MI)
An MI is when part of the heart muscle dies due to a blocked coronary artery (physical damage to heart)
Cardiogenic shock is the severe complication that follows, when the damaged heart muscle can’t pump blood forward (the whole body failing because heart cannot maintain circulation)
Blood backs up → pulmonary congestion → crackles, low oxygen, shortness of breath.
↓ Stroke volume: ↓ Cardiac output, ↓ BP (less fluid)
↑ HR and contractility to compensate, but this only increases oxygen demand and worsens damage.
Key signs:
Low BP, high HR, weak pulses, cool skin, crackles in lungs, chest pain.
Treatment: improve heart function (e.g., meds to increase contractility, oxygen, possible mechanical support).
Hypovolemic shock
(Shock means the body’s tissues and organs aren’t getting enough oxygen-rich blood to function)
A type of shock that occurs due to a significant loss of circulating blood / fluid.
can be caused by: severe hemorrhage, profuse burns, severe dehydration, or excessive vomiting/diarrhea.
inadequate preload, reduced cardiac output, and insufficient tissue perfusion
↓ Intravascular fluid: ↓ Blood volume, ↓ Stroke volume, ↑ Heart rate, ↑ Contractility → to comepensate for cardiac output
Obstructive shock
Caused by a physical blockage preventing blood flow from flowing normally through the circulation. (e.g., pulmonary embolism, cardiac tamponade, pneumothorax).
The heart itself might be fine, but something outside or around it keeps blood from moving forward.
Blood can’t move forward: ↓ stroke volume, ↓ cardiac output, ↑ HR, ↑ contractility, ↑ vasoconstriction to raise BP, but oxygen delivery still fails.
Key sign: muffled heart sounds, tracheal deviation (depending on cause).
Distributive shock
massive vasodilation throughout body → blood vessels widen, ↓ vascular resistance, ↓ BP.
Blood pools in vessels instead of returning to the heart, ↓ preload and ↓ stroke volume.
Subtypes:
Septic: infection → inflammation → vasodilation + capillary leak.
Anaphylactic: allergic reaction → histamine release → vasodilation + airway swelling.
Neurogenic: loss of sympathetic tone (spinal injury) → vasodilation + bradycardia.
Signs: warm skin early, hypotension, tachycardia (except neurogenic).
Dyslipidemia
An abnormal level of lipids (fats) in the blood that significantly increases the risk of cardiovascular disease
high levels of low-density lipoprotein (LDL) cholesterol, high total cholesterol, low levels of high-density lipoprotein (HDL) cholesterol, or high triglycerides
risk factors: genetics, dietary, obesity, type 2 dieabetes
cause for atherosclerosis, coronary artery disease, and stroke.
Thrombus
A blood clot that forms and remains attached to the wall of a blood vessel or within the heart. It obstructs blood flow at its point of origin and can lead to conditions such as deep vein thrombosis (DVT), myocardial infarction, or stroke if it forms in a critical artery.
Embolus
Freely moving blood clot (thrombus) that travels in larger vessels and lodges in a smaller vessel, occluding blood flow, most often from atrial fibrillation or prosthetic heart valves (since not organtic tissue and body clots around the structure, then dislodge)
most concerned about pulmonary embolism (embolism travels to lungs)
Blood Flow Through the Heart
deoxygenated blood comes in from superior or inferior vena cava, goes to right atrium then right ventricle, then pulmonary artery, then to lungs
after blood goes to lungs, gas exchange happens
oxygenated blood comes back
oxygenated blood comes through pulmonary vein into left atrium, then left ventricle, then aorta
oxygenated blood from aorta goes back to body to give O2 to organs
- left side of heart: pumps blood to body (aorta) and oxygen delivered to organs (left sided failure means lungs fill with fluid, pulmonary congestion)
- the right side of the heart pumps blood to the lungs for oxygenation (right sided heart failure, fluid backs up into the body, systemic congestion)
- left sided failure can lead to right sided failure: if the left side cant pump effectively blood backs up into the lungs and increases pressure in pulmonary circulation which strains the right side to give right heart failure
The 7 P's
A mnemonic used to recall the signs and symptoms of ischemia caused by emboli and thrombi: (tissue below occlusion will have these signs):
presents acutely
pallor
polar (cold)
pulselessness
pain
parasthsia
paralysis
neoplasms
an abnormal mass of tissue where growth is excessive and uncoordinated compared to normal cells.
- does not follow normal cell growth rules and keeps dividing even without a stimulus.
- It grows at the expense of the host, causing damage.
- It serves no useful purpose and is classified as benign (non-cancerous) or malignant (cancerous).
Benign vs. Malignant Neoplasms
Benign: Well-differentiated (mature), slow-growing, may stop growing, expands without invading tissue, often encapsulated, and doesn’t metastasize. Ends with -oma.
Malignant: Poorly differentiated (anaplastic), fast-growing, carcinoma in situ: preinvasive (good to catch here), invades nearby tissue, spreads through blood or lymph, and can metastasize to other organs. Ends with -coma.
more undifferentiated (most immature) = faster growth
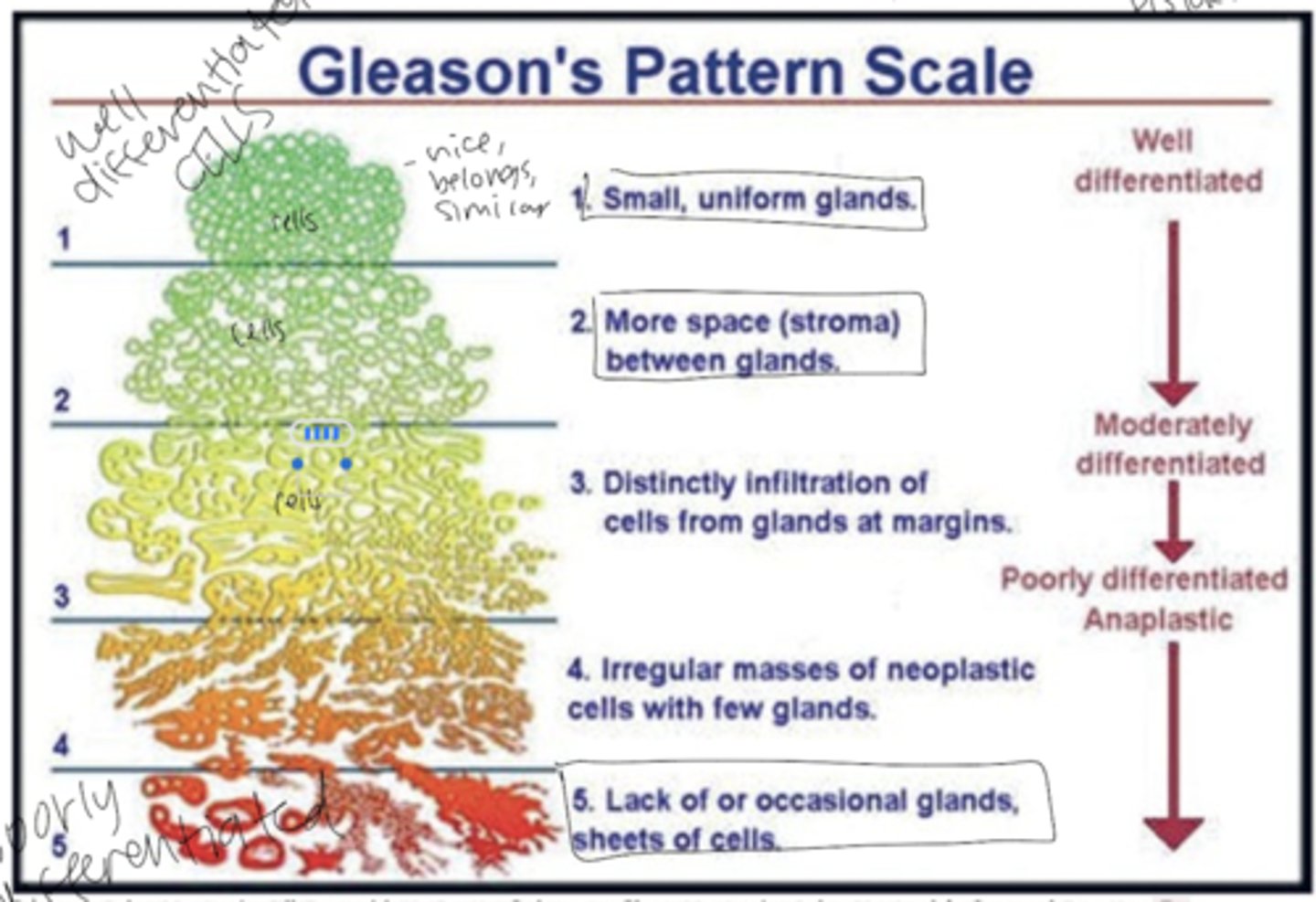
Gleason's Pattern Scale
measures how differentiated cancer cells are (how much tumor cells resemble normal cells)
- Well-differentiated (1-2): Cells look similar to normal tissue, grow slower, and are less aggressive.
- Moderately differentiated (3): Cells show some abnormality and faster growth.
- Poorly differentiated / Anaplastic (4-5): Cells lose structure and function, appear distorted, and grow uncontrollably — indicating high malignancy
More undifferentiated = more aggressive, invasive, and dangerous cancer.
cancer cells vs normal cells
- genetic instability
- frequent mutations
- can keep dividing without being told to (grow without growth factors)
- ignore contact inhibition (stopping growth upon contact) allowing uncontrolled growth
- unlimited lifespan dividing endlessly
- produce enzymes, hormones, and substances that support invasion and metastasis.
stages of carcinogenesis (cancer development)
1. Initiation: Exposure to a carcinogen that causes genetic mutation.
2. Promotion: Cell growth triggered by promoters like hormones or chemicals; reversible if the promoter (substance that accelerates tumor) is removed.
3. Progression: During progression, tumor cells undergo genetic and behavioral changes that make them more invasive, able to spread (metastasize), grow uncontrollably, and genetically unstable.
host and environmental factors increasing cancer risk
- Heredity (e.g., breast cancer genes)
- Hormones (e.g., estrogen)
- Immune dysfunction
- Chemicals (direct agents act immediately; indirect agents need metabolic activation, (DELAYED, smoking will not show as cancer for 30+ years)
- Radiation
- Oncogenic viruses:
- HPV → cervical cancer
- EBV → lymphoma, nasopharyngeal cancer
- HBV → liver cancer
main clinical manifestations of cancer
- Local effects: Impaired tissue integrity → ulceration, necrosis, bleeding, poor healing.
- Effusions: Fluid in pleural, pericardial, or peritoneal spaces.
- Systemic effects: pure exhaustion, weight loss (cachexia - muscle loss, loses reserve for healing and alters metabolism), anorexia, anemia, frequent infections, pain.
cancer detection and diagnosis
- Screening: secondary prevention: finding cancer early before symptoms appear.
- Observation: Skin, mouth, external genitalia
- Palpation: Breast, thyroid, rectum/anus, prostate, lymph nodes
- Lab tests/procedures: Pap smear, colonoscopy, mammogram
Diagnosis confirms cancer through:
- Tissue biopsy, Pap test, immunohistochemistry, microarray
- Tumor markers: Substances like antigens, hormones, or enzymes from tumor cells present in blood used to monitor treatment but can also rise in benign conditions.
How are cancers graded and staged?
Grading (I–IV): Based on differentiation and anaplasia (higher grade = more abnormal).
Staging (TNM):
- T: Tumor size/invasion (TX: nothing measured, T0: cannot be found, T1–T4, tumor has been MEASURED, higher number = larger expanse).
- N: Node involvement (NX: no information about nodes, N0: nearby lymph nodes not affected, N1–N3 higher number = more nodes with cancer).
- M: Metastasis (MX: spread cant be measured, M0 = none, M1 = cancer has spread to other parts of the body).
How do cancer types differ between adults and children
Adults: Cancers usually from epithelial cells (lung, breast, colorectal).
Children: Involve hematopoietic, nervous, or connective tissues (bone, kidney). divides more and more rapidly
Embryonal tumors (e.g., nephroblastoma, neuroblastoma) are most common in infancy and early childhood.
normal cell progression to metastasis
DNA damage (from carcinogens or inherited mutation) → activation of oncogenes, loss of tumor suppressor genes, decreased apoptosis → uncontrolled growth → tumor progression → malignant tumor → metastasis.
where is fluid located in the body
- Intracellular fluid (ICF): Fluid inside the cells that make up most of the body's total water
- Extracellular fluid (ECF): Fluid outside the cells found in blood vessels (plasma) and between tissues (interstitial fluid)
- Labs measure extracellular fluid values, not what's inside the cells.
fluid movement
- Fluid moves from high → low pressure.
- Fluid moves from low solute → high solute concentration (osmosis).
- high volume = higher pressure
- low volume = lower pressure
What is osmosis and how does tonicity affect fluid movement
Osmosis: Water moves through a semipermeable membrane from areas with low solute to high solute concentration to balance things out.
Tonicity: the relative concentration of solutes in a solution compared to the inside of a cell, determining the direction water will move across the cell membrane.
Isotonic: Same solute concentration as cell → no water movement → cell stays normal.
Hypotonic: Fewer solutes in solution→ water moves into cell → swells.
Hypertonic: More solutes outside → water moves out of cell → shrinks.
Capillary interstitial fluid exchange
A capillary is the tiny blood vessel that connects arteries (which carry blood away from the heart) to veins (which carry blood back toward the heart).
At the arterial end of a capillary, blood coming from the heart under high pressure (closer to the left ventricle) creates a high hydrostatic pressure that pushes plasma (the fluid part of blood) out of the capillaries into the surrounding tissues. This process is called filtration and delivers oxygen and nutrients to the tissues.
At the venous end, where blood pressure is lower, the hydrostatic pressure drops while osmotic pressure—the force caused by proteins like albumin inside the capillaries—increases. This osmotic pressure pulls fluid back into the capillaries in a process called reabsorption.
(Most of the plasma that left at the arterial end is reabsorbed at the venous end, while the blood cells remain inside the capillaries. Any excess fluid that is not reabsorbed stays in the tissues and is eventually removed by the lymphatic system.)
This balance between hydrostatic pressure pushing fluid out and osmotic pressure pulling fluid back in helps maintain proper fluid levels and equilibrium in the body’s tissues.
What is edema and what are its types and signs
Definition: Palpable swelling from excess interstitial fluid.
Localized (one area) or generalized - edema seen throughout the body (anasarca). (more volume in capillaries = greater hydrostatic pressure on vessels increases amount fluid will leak out)
Clinical effects: Limits motion, oxygen/nutrient delivery, causes pain.
Pitting edema: Rated +1 (mild) to +4 (severe).
What causes edema formation
↑ Capillary (hydrostatic) pressure: more pressure means more pushing out the fluid, Heart failure, kidney disease, venous obstruction.
↓ Colloidal osmotic pressure: Loss or low plasma proteins means proteins are not drawing fluid back in (burns, malnutrition, liver disease).
↑ Capillary permeability: more easy accessibility for fluid to leak out since less resistance, Inflammation, tissue injury, burns.
Lymphatic obstruction: system to decrease fluid isnt working, fluid builds up, Tumor or surgical removal of lymph nodes.
What controls fluid balance in the body?
Thirst brings fluid in: Tells you to drink when fluid levels drop.
ADH (antidiuretic hormone): Keeps water in the body by telling kidneys to stop making so much urine, disorders like DIABETES INSIPIDUS cant do this and loses fluid in urination
RASS System: triggering the kidneys to retain sodium and water
increased osmolality indicates needing more fluids
RASS (Renin-Angiotensin-Aldosterone System):
The RAAS system controls fluid balance by triggering the kidneys to retain sodium and water, which increases blood volume and raises blood pressure when it's too low.
1. Blood pressure drops → kidneys release renin
2. Renin changes angiotensin I → angiotensin II
3. Angiotensin II causes blood vessels to tighten (↑BP)
4. Also releases aldosterone, which makes kidneys keep sodium and water → increases blood volume & pressure.
What is hypervolemia and what causes it:
Hypervolemia = too much fluid in the body.
Causes:
- Heart failure: Heart isn't pumping well → fluid backs up.
- Renal (kidney) failure: Kidneys can't get rid of excess fluid.
- Too much IV fluid.
What is hypovolemia and what causes it:
Hypovolemia = loss of body fluids.
Causes:
- Not drinking enough.
- Vomiting or diarrhea (GI losses).
- Excess urine loss (renal).
- Sweating
- Third spacing: Fluid trapped in tissues (like edema or ascites).
How do nurses assess fluid balance:
Daily weights (same time every day - indicates fluid retention).
Visual checks (swelling,edema, dryness).
Press skin for pitting edema.
Check skin turgor (elasticity).
Vital signs (BP, pulse).
Intake and Output (I&O).
What are electrolytes and why are they important:
Substances in blood that carry an electric charge.
Cations (+): sodium (Na⁺), potassium (K⁺).
Anions (−): chloride (Cl⁻), bicarbonate (HCO₃⁻).
Fluids have equal amounts of both.
Na⁺ → most important for brain & nerves (neuro).
K⁺ → most important for heart (cardiac).
What does sodium do and what happens when it's off balance:
Found mostly outside cells (extracellular).
Maintains fluid balance.
Low sodium (hyponatremia): GI losses, SIADH (body puts out too much anti dieuretic hormone, fluid builds up that dilutes sodium), sweating, drinking too much water flushes out sodium.
High sodium (hypernatremia): Dehydration, not enough water.
Both cause brain and nerve symptoms → confusion, muscle twitching, seizures.
What does potassium do and what happens when it's off balance:
Found mostly inside cells
Very small window of normal values, small changes can have major consequences
Kidneys control levels of elevation.
Both low (hypokalemia) and high (hyperkalemia) cause heart rhythm problems (arrhythmias).
Low K⁺: weakness, paralysis.
High K⁺: weakness, tingling, heart issues.
What causes low potassium (hypokalemia):
Not enough intake (diet).
Too much loss:
Diuretics (makes kidneys lose K⁺).
Vomiting, diarrhea, GI suction.
(potassium is more sensitive to loss because small changes = big difference)
Insulin lowers blood potassium by shifting it into cells, so large doses can cause hypokalemia and require careful monitoring.
What causes high potassium (hyperkalemia):
Too much intake (usually by TPN).
Kidneys not eliminating enough:
Kidney failure.
Potassium-sparing diuretics (potassium stays in the body and isn’t excreted with urine).
Addison's disease (not enough aldosterone means potassium builds up).
Movement out of cells: injury or trauma (cells break open and release K⁺).
calcium, phosphorus, magnesium and disorders
these 3 minerals are tightly linked, when one changes, the others often change too
vitamin D helps absorb calcium and phosphorus from the gut to put into bloodstream, without vitamin D, low calcium and low phosphorus
parathyroid hormone: PTH raises calcium and lowers phosphorus in blood, needs magnesium to work properly, if magnesium is low, PTH cant be released and calcium drops
low magnesium, low PTH, low calcium
low vitamin D, low calcium and low phosphorus
DISORDERS:
hypoparathyroidism: low PTH, low calcium, high phosphorus
hyperthyroidism: high PTH, lower phosphorus, high calcium
What causes hypercalcemia and what are its effects:
Causes: Too much vitamin D, high calcium intake, hyperparathyroidism, cancer, or immobility.
Hypocalcemia = muscle twitching, spasms, arrhythmias.
Hypercalcemia = confusion, weakness, arrhythmias.
Ionized calcium is the "active" form (not calcium bound to protein) that affects body function.
What causes hypo- and hyperphosphatemia
Hypophosphatemia (low phosphorus): Caused by antacids, diarrhea, low vitamin D, hyperparathyroidism, diabetic ketoacidosis, alcohol use.
Hyperphosphatemia (high phosphorus): Caused by laxatives/enemas with phosphorus or kidney failure.
Inverse relationship with calcium: ↑ Phosphorus = ↓ Calcium.
What causes hypo- and hypermagnesemia:
Hypomagnesemia: Chronic alcohol use, malnutrition, diuretics, hyperaldosteronism, diabetic ketoacidosis (lots of uresis).
Hypermagnesemia: Too much Mg medication, kidney failure.
Low Mg → causes muscle twitching, tremors, weakness, arrhythmias.
High Mg → slows reflexes, can cause dangerous cardiac arrhythmias.
Regulation of pH (ratio + balance)
- pH = ratio of H₂CO₃ (acid) to - HCO₃⁻ (base)
- Normal ratio 20:1
when ratio is less than 20:1 (pH decreases, more acidic)
when ratio is more than 20:1 (pH increases, more basic)
- H₂CO₃ = carbonic acid, CO₂ dissolved in water
- pH stays normal if both change equally
- pH shows balance of acidic or alkali, not where the problems originate
Regulation of pH (mechanisms)
- The body keeps blood pH balanced using 3 systems:
- Buffers: chemically work instantly to keep pH from changing too much.
- Lungs: control CO₂ (acid).
Breathing faster (↑ ventilation) gets rid of CO₂ → less acid → higher pH.
Breathing slower (↓ ventilation) keeps CO₂ in → more acid → lower pH.
- Kidneys: control bicarbonate (base).
They get rid of hydrogen (acid) and make bicarbonate (base) to restore balance.
Anion Gap
- helps find the cause of metabolic acidosis (why someones blood is too acidic), difference between measured cations (Na+) and anions (chloride, bicarbonate) that represent unmeasured acids in the blood
-metabolic acidosis: bicarbonate is low, it is lost or not made because of extra acids
- chloride will go up to compensate for lost bicarbonate so anion gap stays normal
- A large anion gap means there are extra acids in the blood (like ketones or lactic acid).
- more unmeasured anions (like ketones) means more acids in plasma, bicarbonate decreasing means unmeasured anions get higher means lots of ketones
- consumption of bicarbonate by unmeasured ketones increases anion gap by lowering serum bicarbonate level
- A normal anion gap means acid levels are normal, but bicarbonate was lost (like from diarrhea).
Metabolic Acidosis
- decreased base (HCO3-)
- Causes: diabetic ketoacidosis (produces too much acid), lactic acidosis (sepsis), kidney failure (decreases acid excretion).
- Signs: fast breathing, nausea, irregular heartbeat, confusion.
- Compensation: lungs breathe faster to get rid of CO₂ (acid) so respiratory rate goes up.
Metabolic Alkalosis
- Excess base (HCO3-)
- Causes: vomiting (loss of acid), too many antacids or bicarbonate.
- Signs: confusion, sluggishness, decreased alertness.
- Compensation: breathing slows down to keep CO₂ (acid) in the body.
Respiratory Acidosis
- Increased acid (CO₂) from not breathing enough (hypoventilation).
- Causes: lung disease, drug overdose - affects CNS, chest injury - hard to breathe out, decreased ventilation.
- Signs MORE INTENSE: behavior changes, tremors, hallucinations
- Compensation: kidneys keep bicarbonate (base) to raise pH.
Respiratory Alkalosis
- Decreased acid (CO₂) from breathing too fast (hyperventilation).
- Causes: anxiety, fear, fever, pain.
- Signs: lightheadedness, tingling, faintness.
- Compensation: kidneys get rid of bicarbonate (base) to lower pH.
ABG (Arterial Blood Gas)
- Measures acid-base balance and oxygen levels in the blood by analyzing the gases in a sample of arterial blood.
- Tells if the imbalance is metabolic or respiratory to treat better since such different conditions.
- Arterial blood is used because it's rich in oxygen, high pressure (since closest to LV) and shows lung function.
- values differ between arterial and venous blood
What are the first three steps to interpret ABG results?
- Look at pH first – determines acidosis or alkalosis
- Look at PaCO₂ next – respiratory component
- Look at HCO₃⁻ next – metabolic component(Ignore PaO₂ and SaO₂ for acid-base balance)
How do you interpret pH values in an ABG?
- pH 7.35–7.45 = Normal or compensated
- pH <7.35 = Acidosis
- pH >7.45 = Alkalosis
How do you determine the type of acidosis or alkalosis from ABGs?
- If pH <7.35 (acidosis):
High CO₂ → Respiratory acidosis
Low HCO₃⁻ → Metabolic acidosis
- If pH >7.45 (alkalosis):
Low CO₂ → Respiratory alkalosis
High HCO₃⁻ → Metabolic alkalosis(CO₂ = acid, HCO₃⁻ = base)
R.O.M.E (respiratory: opposite, metabolic: equal)
Respiratory: ↑CO₂ = ↓pH; ↓CO₂ = ↑pH
Metabolic: ↑HCO₃⁻ = ↑pH; ↓HCO₃⁻ = ↓pH
What ABG findings indicate respiratory acidosis?
- pH: Low (<7.35)
- PaCO₂: High (>45)
- HCO₃⁻: Normal or slightly ↑ (if compensating)
= Example: pH 7.30, CO₂ 60, HCO₃⁻ 26 → Respiratory Acidosis
What ABG findings indicate metabolic acidosis?
- pH: Low (<7.35)
- PaCO₂: Normal or ↓ (if compensating)
- HCO₃⁻: Low (<22)
- Example: pH 7.23, CO₂ 43, HCO₃⁻ 16 → Metabolic Acidosis
What ABG findings indicate respiratory alkalosis?
- pH: High (>7.45)
- PaCO₂: Low (<35)
- HCO₃⁻: Normal or ↓ (if compensating)
Example: pH 7.47, CO₂ 33, HCO₃⁻ 24 → Respiratory Alkalosis
What is "compensation" in the context of pH balance?
The body's attempt to correct large changes in pH through renal and respiratory mechanisms, which can be partial or full.
What defines partial compensation in pH imbalance?
Partial compensation happens when the body starts to correct an acid-base imbalance, but the blood pH is still abnormal. The other system (lungs or kidneys) adjusts CO₂ or bicarbonate levels to help, but the pH hasn’t returned to the normal range yet.
What defines full compensation in pH imbalance?
Full compensation happens when the body’s other system (lungs or kidneys) has adjusted enough to bring the blood pH back into the normal range, despite the original acid-base problem still being present.
What are the main types of diagnostic tests for heart conditions?
12-lead EKG (snapshots electrical activity with more leads, views electrical activity, more detailed)
telemetry, use first, then EKG (continuous electrical activity with fewer leads - fewer views of the heart, views electrical activity of heart)
echocardiogram (ultrasound of heart)
stress testing (treadmill or pharmacological agent),
cardiac catheterization and arteriography (catheter and dye to visualize heart structures).
infective endocarditis
Infection of inner heart surface, usually valves; bacteria attach to valves leading to bulky bumps that break down valve issue so valves stop working
risk factors include IV drug use, dental/surgical procedures, artificial valves
clinical manifestations include systemic inflammation, petechial and splinter hemorrhages under nails of fingers and toes, congestive heart failure
diagnosis by blood cultures (3 diff sites in 24 hours), echo, clinical signs.
stenosis vs regurgitation in valve disorders
Stenosis: narrowed or incomplete valve opening, increasing work of chamber trying to empty through the narrowed valve (pushes extremely hard to get through the small opening), can be aortic or mitral valves
Regurgitation: incomplete valve closure causing backflow of blood, can be aortic or mitral valves
both diagnosed w echo.
What are the types of cardiomyopathies and their clinical manifestations?
Hypertrophic cardiomyopathy: can be primary or secondary thickened septum obstructing LV outflow and diastolic filling, causes exercise intolerance and arrhythmias, chest pain during exertion (snow shoveling) - echo
Dilated: enlarged ventricles, weak heart impairing systolic function, EF <40, causes dyspnea and heart failure, arrhythmias - echo
Myocarditis: inflammation of myocardium from virus, asmptomatic, causes systemic inflammation and heart failure - echo, cardiac cath
mitral stenosis, mitral valve regurgitation, mitral valve prolapse, aortic stenosis, aortic valve regurgitation
Mitral stenosis: narrowing of mitral valve, incomplete opening of mitral valve during diastole (filling), will not fill properly, pulmonary congestion, a-fib, murmur
Mitral regurgitation: mitral valve not closing completely, causes blood to move back to LA during systole, pulmonary congestion, asymptomatic, murmur
Mitral valve prolapse: degeneration of mitral valve leaflets, becomes floppy, slip out of normal position
Aortic stenosis: calcification of leaflets, hard to move, increased resistance to ejection of blood from LV into aorta, congenital, wear and tear expected for older adults
Aortic valve regurgitation: backflow during diastole, causes scarring, pulmonary edema (fluid buildup in lungs, deadly
causes and complications of pericardial effusion
Accumulation of fluid around pericardium due to inflammation, infection, or trauma; can be asymptomatic (slowly fills over time, gives ample time for pericardium to stretch) or lead to cardiac tamponade.
acute pericarditis
Inflammation of pericardium
- causes include viruses/bacteria
- symptoms include chest pain relieved by tripod position, pericardial friction rub, ST elevation/PR depression on EKG, elevated WBC and CRP, pericardial effusion.
process of cardiac tamponade
fluid builds up in the pericardial sac, putting pressure on the heart and preventing it from filling and pumping blood effectively, decreased cardiac output
cardiac output = stroke volume x heart rate
Fluid compresses heart → decreased diastolic filling → decreased stroke volume → decreased cardiac output → increased heart rate (to compensate) → blood backs up into superior vena cava causing jugular venous distension and narrow pulse pressure.
Coronary Artery Disease
a condition where the coronary arteries (the blood vessels that supply your heart muscle with oxygen-rich blood) become narrowed or blocked usually due to atherosclerosis, cigarette smoking, hypertension, diabetes, age, obesity, physical inactivity, abnormal cholesterol levels.
This narrows the arteries, reducing blood flow to the heart muscle.
This narrows the arteries, reducing blood flow to the heart muscle
Can cause acute coronary syndrome: unstable angina, myocardial infarctioin, nstemi, stemi and can cause chronic coronary syndrome: heart disease and stable angina
What are the potential complications following a myocardial infarction
Sudden death, cardiogenic shock, arrhythmias, pericarditis, mechanical defects, heart failure.
What distinguishes stable angina from acute coronary syndrome (ACS) pathophysiologically
stable angina: chest pain or pressure that happens predictably with activity or stress when narrowed coronary arteries (from atherosclerosis) can’t supply enough oxygen to the heart, and it goes away with rest or nitroglycerin.
Stable angina is due to build-up of plaque causing partial coronary narrowing without rupture, ACS results from plaque rupture leading to thrombus formation causing partial or complete coronary occlusion, and myocardial infarction.
What occurs during the postinfarction recovery period in the heart tissue
After an infarction, the heart tissue is affected in three zones: the central zone of necrosis (irreversibly dead tissue), the surrounding zone of injury (potentially salvageable), and the outer ischemic zone (still viable but at risk). Cardiac muscle cannot regenerate, so necrotic tissue is permanently replaced by fibrous (scar) tissue. Injured cells may recover or undergo apoptosis, depending on how quickly blood flow is restored.
Preload
Volume of blood in the ventricles at the end of diastole (filling), higher volume = higher preload
Ejection Fraction
The percentage of blood that is pumped out of the ventricle with each contraction. (normal: 50-70%)
Contractility
The force of the heart muscle when it contracts and pumps blood, not static, can change force, lower contractility = not doing good job pumping volume out of ventricle which causes EF to be low
Afterload
the resistance the heart's ventricle must overcome to eject blood into the body's arteries during contraction, how hard it is to pump blood out based on what is outside of heart (like vessels constriction or dilation)
Heart Failure
Heart failure results from any functional or structural disorder of the heart that impairs its pumping ability. impaired pumping means decreased contractility since no force, can be right, left or both sided heart failure
Left Heart Failure (lungs affected)
- Blood Flow: Oxygen-rich blood from Lungs -> Left Atrium -> Left Ventricle -> Body.
-Problem: Weak Left Ventricle
- Causes: Damage (heart attack), High BP (hypertension), valve issues. This makes it hard to pump blood out to the body.
- Backup: Blood backs up into Pulmonary Veins -> Pulmonary Congestion (fluid in lungs).
- Consequences: LUNG issues: Shortness of Breath (Dyspnea, Orthopnea, PND), Cough (frothy sputum), Fatigue (less O2 to body), Crackles (fluid sound in lungs).
Right Heart Failure
- Blood Flow: Deoxygenated blood from Body -> Right Atrium -> Right Ventricle -> Lungs.
- Problem: Weak Right Ventricle
- Causes: Left HF (most common), Lung disease (COPD, pulmonary hypertension), valve issues. This makes it hard to pump blood to the lungs.
- Backup: Blood backs up into Systemic Veins -> Systemic Congestion (fluid in body).
- Consequences: BODY issues: Edema (legs, ascites), Weight Gain (fluid), Liver Enlargement, GI Issues (nausea, loss of appetite), JVD (swollen neck veins).
B-Type Natriuretic Peptide (BNP)
BNP is a peptide secreted by the ventricles in response to increased ventricular pressure (fluid overload). It inhibits sodium and water reabsorption.
It's elevated in heart failure and its level correlates with the extent of ventricular dysfunction.
Heart Failure Diagnosis
- History & Physical: Evaluate clinical manifestations.
- Class I - IV
- BNP: Elevated levels indicate heart failure.
- Echo: Echocardiogram to assess heart function.
Classes of Heart Failure
- Class I: Heart disease, no symptoms with ordinary activity
- Class II: Slight limitations, symptoms with ordinary activity
- Class III: Comfortable at rest, symptoms with ordinary activity
- Class IV: Symptoms at rest.
stable vs unstable angina
angina: chest pain caused by reduced blood flow to heart muscle
stable angina: muscle is not getting enough oxygen because coronary arteries are blocked, caused by a fixed plaque narrowing the coronary artery, plaque has a thick fibrous cap that keeps it from rupturing, triggered by exertion or stress, relieved by rest or nitroglycerin, no permanent heart damage, blood flow returns to normal at rest
unstable angina: plaque becomes thin and unstable, prone to rupture, when it ruptures, platelets stick, clot forms and blood flow drops, can cause ischemia which progresses to NSTEMI (partial blockage, incomplete occlusion) and STEMI (full blockage (complete occlusion, heart tissue death)
Stable Angina Vs. Types of ACS
Unstable Angina (UA):
Pain: Constricting, squeezing, suffocating; often triggered by exertion, stress, or cold
Relief: Usually relieved by rest or nitroglycerin within 10 minutes
ECG: May be normal or show ST depression or T wave changes
Biomarkers: Normal (no heart muscle damage)
NSTEMI (Non-ST-Elevation Myocardial Infarction):
Pain: Similar to UA but more severe or frequent; can occur at rest and lasts >20 minutes
Relief: Not always relieved by rest or nitroglycerin
ECG: ST depression and/or T wave inversion
Biomarkers: Elevated troponin I or T (indicates heart muscle damage); CK-MB may be elevated
STEMI (ST-Elevation Myocardial Infarction):
Pain: Severe, prolonged chest pain; abrupt onset or progression from UA/NSTEMI
Relief: Not relieved by rest or nitroglycerin
ECG: ST elevation and T wave changes
Biomarkers: Elevated troponin I and T; CK-MB often elevated
main signs, symptoms, and diagnostic findings of congenital heart defects
signs and symptoms: babies may have respiratory difficulty, fatigue, poor feeding, murmur, and recurrent respiratory infections.
- In cyanotic defects (like Tetralogy of Fallot), skin looks bluish because oxygen-poor blood is pumped to the body instead of the lungs (the problem isn’t oxygen supply, but blood going to the wrong place (right-to-left shunt).
Diagnosis: ECHOt. If the baby is given 100% O₂ for 10 min and PO₂ fails to rise, it suggests a cyanotic heart defect, meaning the issue is with heart structure, not the lungs.
artherosclerosis
when plaque builds up inside the arteries, narrowing them and reducing blood flow. It develops slowly and often has no symptoms until the artery becomes severely blocked or the plaque ruptures.
Risk factors: High LDL cholesterol, high blood pressure, smoking, diabetes, obesity, physical inactivity, older age, and family history.
Development process:
Endothelial injury to the vessel wall (from high BP, smoking, or high LDL).
Inflammation attracts macrophages that engulf LDL, forming foam cells (macrophage WITH LDL).
Plaque forms — a lipid core with a fibrous cap develops inside the artery wall. Over time, the plaque hardens or ruptures, increasing the risk for heart attack or stroke.
chronic arterial inflammation and plaque buildup → decreased oxygen supply to tissues.
Peripheral Artery Disease
gradual narrowing of arteries that leads to reduced blood flow (ischemia), especially in lower extremities.
- PAD basically clinical manifestation of atherosclerosis
- Caused by progression of atherosclerosis (when arterial blockage becomes symptomatic (≈90% occluded).
Atherosclerosis = plaque buildup in arteries (can happen anywhere).
PAD = when that plaque buildup in the peripheral arteries (like in the legs) becomes severe enough to reduce blood flow and cause symptoms such as pain, weak pulses, or cool feet.
clinical signs:
Calf pain when walking (intermittent claudication)
Cool feet or lower extremities
Weak pedal pulses (partial, not total occlusion)
Skin changes, slow healing → can lead to gangrene if untreated
risk factors: smoking, diabetes, hypertension, high cholesterol, obesity, sedentary lifestyle
venous thrombosis
formation of a thrombus (clot) in a vein with inflammation of the vein wall (most common as DVT (deep vein thrombosis) in the lower extremities).
Causes (Virchow’s Triad):
Stasis of blood: bed rest, immobility, long flights
Hypercoagulability: increased clotting tendency (hormone therapy, contraceptives, cancers, low blood volume)
Vessel wall injury: trauma, surgery, infection, inflammation
Symptoms:
Can be asymptomatic or show pain, swelling, redness, fever, malaise, and elevated WBCs from inflammation.
Diagnosis:
Ultrasound (to visualize clot)
D-dimer test (detects protein fragments from blood clot breakdown)
Chronic Venous Insufficiency
occurs when leg veins don’t properly return blood to the heart, causing blood to pool in the lower legs.
This happens due to damaged or weak vein valves that fail to keep blood moving upward.
Risk Factors:
Prolonged standing (increases venous pressure)
History of DVT (deep vein thrombosis)
Symptoms:
Edema (swelling) in legs
Pain or heaviness with walking or standing
Varicose veins from chronic blood pooling
varicose veins
dilated, twisted veins of the lower extremities caused by increased venous pressure and valve failure.
They can lead to chronic venous insufficiency.
Risk factors: DVT, congenital vein defects, pregnancy, tumors, obesity, prolonged standing or lifting.
Clinical manifestations: aching, heaviness, and edema in the lower legs with visible distended veins.
Orthostatic Hypotension
an abnormal drop in blood pressure when standing up, defined as a decrease of ≥20 mmHg systolic or ≥10 mmHg diastolic.
occurs when blood pools in the lower body instead of returning to the heart.
Clinical manifestations: dizziness, lightheadedness, syncope (fainting).
Risk factors: older adults, reduced blood volume, bed rest, impaired mobility, and medications such as antihypertensives.
Hypertension
a sustained elevation of blood pressure within the arterial system. Caused by increased vascular resistance from vessel narrowing or stiffness.
Risk factors: age, family history, high sodium or fat diet, obesity, physical inactivity, tobacco, alcohol, dyslipidemia, obstructive sleep apnea.
Clinical manifestations: often asymptomatic (silent killer).
Complications:
Organ & vessel damage from chronic pressure.
Atherosclerosis: endothelial injury → plaque buildup.
Heart: LV hypertrophy, heart failure.
Kidney: nephrosclerosis, renal failure.
Brain: stroke, aneurysm.
Eyes: retinopathy, blindness.
Hypertensive Emergency & Preeclampsia
Hypertensive emergency:
Sudden BP rise >180/120 mmHg
Causes organ damage (especially brain, heart, kidneys).
Can lead to stroke, pulmonary edema, headache.
Requires immediate intervention.
Preeclampsia:
Occurs during pregnancy; causes high BP and protein in urine (proteinuria).
Leads to organ damage and reduced blood supply to fetus.
Protein leaks occur because the kidneys’ filtration barrier is damaged, allowing large proteins (like albumin) to pass into urine.
aneurysm
an abnormal, localized dilation (ballooning) of a blood vessel wall, most commonly in the aorta, occurs when arterial walls weaken due to pressure or structural damage.
Types:
Aortic aneurysm (most common)
Thoracic: presses on nearby organs (can cause cough, hoarseness, swallowing difficulty).
Abdominal: often asymptomatic until it ruptures.
Risk factors:
Atherosclerosis (damages vessel walls)
Hypertension (adds constant high pressure)
Smoking (weakens connective tissue in vessels)
Clinical notes:
Usually asymptomatic until rupture or dissection.
Diagnosis: Imaging (CT, ultrasound).
Rupture = life-threatening hemorrhage.
Aortic Dissection
occurs when the inner layer of the aorta tears, allowing blood to flow between the layers of the aortic wall — causing them to separate (dissect). life threatening because blood flow to other areas can slow or stop, and it may rupture, causing massive bleeding.
Risk factors:
Hypertension (constant high pressure damages aortic wall)
Cardiac surgery (post-op weakness)
Congenital aortic defects (e.g., Marfan syndrome).
Clinical manifestations:
Severe, tearing (“ripping”) pain in the chest or back.
Elevated BP, with difference in BP between arms (shows disrupted flow).
CT scan used for diagnosis.
Key difference:
Aneurysm = bulging of all vessel wall layers.
Dissection = tearing within the wall layers.
Rupture = blood breaks through all layers (fatal hemorrhage).
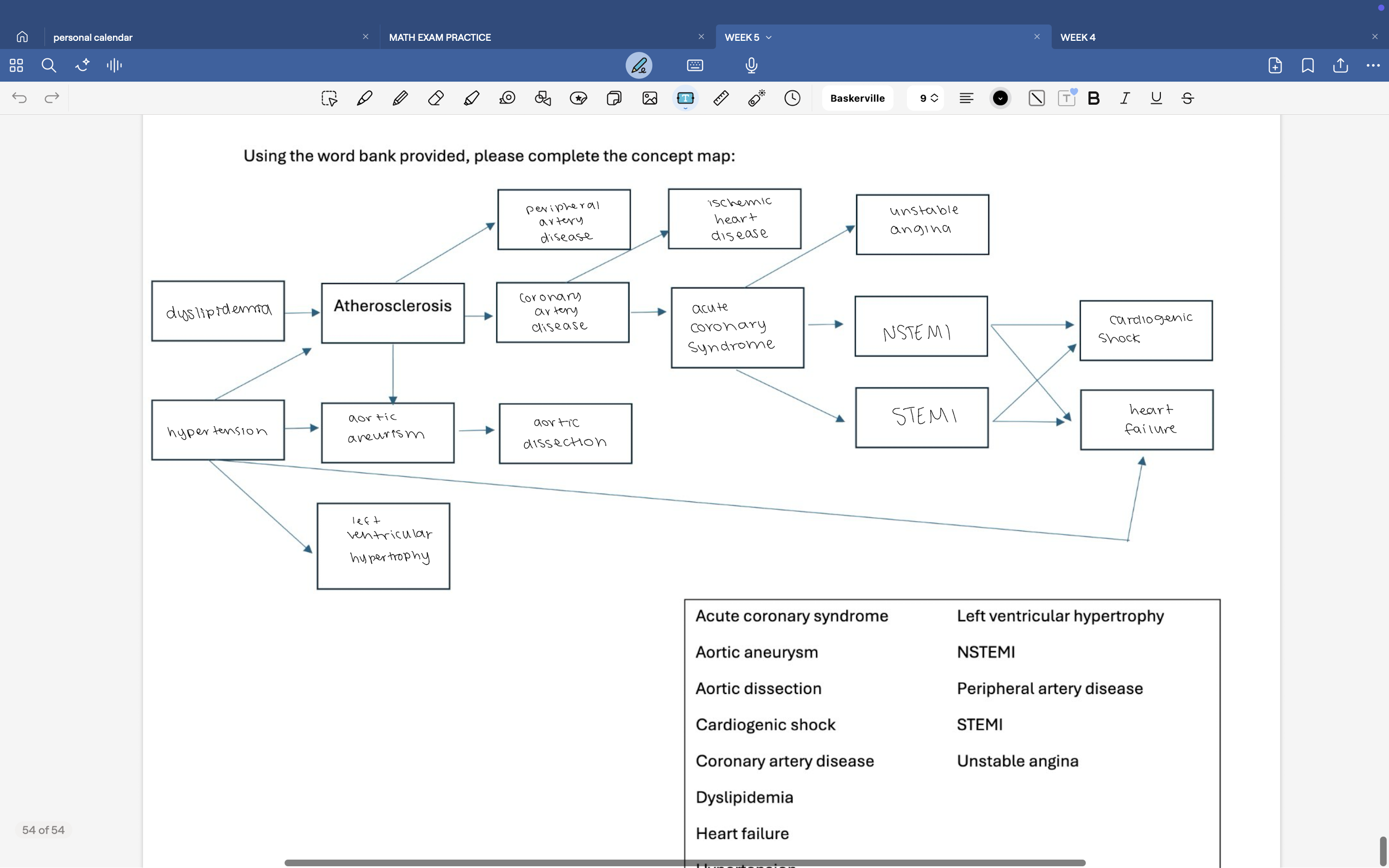
relationships between all heart diseases
Dyslipidemia causes an imbalance in blood lipids, particularly high LDL cholesterol, which leads to the buildup of fatty deposits in the arterial walls. Over time, these deposits form plaques, resulting in atherosclerosis.
As atherosclerosis develops, arteries become narrowed and stiff, which increases resistance to blood flow. This added resistance causes the heart to work harder to pump blood, eventually leading to hypertension. At the same time, hypertension damages the inner lining of arteries, making them more susceptible to plaque buildup, so hypertension and atherosclerosis worsen each other in a continuous cycle.
When atherosclerosis affects the coronary arteries that supply the heart, it causes coronary artery disease. The restricted blood flow to the heart muscle results in ischemic heart disease, meaning the heart tissue is not receiving enough oxygen. If a plaque in one of these arteries ruptures, a blood clot forms, suddenly reducing or blocking blood flow, which leads to acute coronary syndrome.
Acute coronary syndrome can present in different forms depending on how complete the blockage is. A partial blockage causes unstable angina, which is chest pain even at rest but without permanent heart damage. If the blockage becomes more severe and part of the heart muscle begins to die, this results in a non-ST elevation myocardial infarction (NSTEMI). When the blockage is complete and a large portion of the heart muscle dies, it becomes a ST elevation myocardial infarction (STEMI).
Both NSTEMI and STEMI weaken the heart muscle. If the damage is severe enough, the heart cannot pump blood effectively, causing cardiogenic shock, an acute and life-threatening failure of circulation. Over time, continued strain or damage to the heart muscle can progress to heart failure, a chronic condition where the heart can no longer meet the body’s demands.
When atherosclerosis occurs in arteries outside the heart, such as those supplying the legs, it leads to peripheral artery disease (PAD). This reduced blood flow to the limbs causes pain, numbness, and poor wound healing.
Atherosclerosis can also weaken the walls of large arteries like the aorta, leading to an aortic aneurysm, where the vessel wall bulges outward. If that weakened wall tears, it becomes an aortic dissection, which can cause severe internal bleeding and is often fatal.
Finally, long-term hypertension places constant strain on the heart. To overcome the increased pressure, the left ventricle thickens its muscle wall, leading to left ventricular hypertrophy. Over time, this thickening reduces the heart’s efficiency, eventually contributing to heart failure.
3 stages of the General Adaptation System (GAS)
Alarm Stage: acute stress, initial “fight or flight” response; activation of the sympathetic nervous system and release of epinephrine and cortisol.
Resistance Stage: Body attempts to recover while continuing to respond to stress by secreting hormones; energy remains high but coping resources begin to wear down, where signs of stress begin to occur, If recovery doesn’t occur → chronic stress.
Exhaustion Stage: Resources depleted → fatigue, burnout, illness.
If recovery doesn’t occur → chronic stress.
Recovery Stage: after alarm stage, your body returns to homeostasis after stressor has passed
What does a normal diurnal cortisol curve look like?
Peak: Morning (around 30 min after waking).
Decline: Gradually decreases throughout the day.
Lowest: Nighttime (during sleep).
Helps regulate metabolism, alertness, and energy throughout the day.
What happens during the acute stress response?
Sympathetic-Adreno-Medullary System:
“Fight or flight” response. Releases epinephrine/norepinephrine from adrenal medulla.
gives an immediate burst of energy and alertness
Vasoconstriction to concentrate blood flow to brain: ↑BP, HR, CO, glucose, O₂ consumption, skeletal muscle blood flow; ↓GI motility.
Results: Increased alertness, cognition, burst of physical power.
Hypothalamic-Pituitary-Adrenal (HPA) Axis, supports longer term energy and adaptation to stress:
Triggers release of cortisol from adrenal cortex.
Increases glucose, enhances epinephrine activity, suppresses immune system, increases cognition with improvement in blood flow