Delirium, Mild/Major Neurocognitive Disorder, Syncope, Narcolepsy, Coma
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
38 Terms
Delirium
_______ is reversible, while dementia is not.
Etiology
• Fluid and electrolyte disturbances (dehydration, hyponatremia, and hypernatremia)
• Infections (urinary tract, respiratory tract, skin, and soft tissue)
• Drug or alcohol toxicity
• Withdrawal (alcohol, barbiturates, benzodiazepines, and selective serotonin reuptake inhibitors)
• Metabolic disorders (hypoglycemia, hypercalcemia, uremia, liver failure, thyrotoxicosis)
• Low perfusion states (shock, heart failure)
• Postoperative states (especially in older adults; multifactorial - pain medications, anesthesia)
Delirium
an acute process of neurocognitive change from baseline caused by an underlying medical condition that can be treated
Changes in:
-Attention- ability to direct, focus, sustain and shift attention
-Awareness- orientation to the environment
→One domain of cognition: • Learning & memory • Language
• Executive function • Complex attention • Perceptual-motor • Social
Delirium
Epidemiology
-common, can be found wherever there are sick patients
Risk Factors: older, sicker patient increases risk
•any medical condition
•Baseline cognitive dysfunction
• Multiple underlying medical conditions (especially vascular, endocrine and hepatic)
• Multiple medications
• Surgery
• Hospitalization
Clinical Presentation
-family or caregivers who report that patient “isn’t acting quite right” should be taken seriously (especially elderly)
→NO neurologic findings on physical exam
confusion assessment method (CAM)
What is a screening tool used to identify delirium that follows the DSM-5 criteria?
→Delirium is a clinical diagnosis
Sundowning
Phenomenon when confusion becomes worse in evening with an established pattern of behavior
→first episode should be considered delirium until proven otherwise, or consistent pattern is established
Delirium Tremens (DT)
A rapid-onset, fluctuating disturbance of attention and cognition in the presence of alcohol withdrawal
- Seizures usually occur within 12 to 48 hours (1-2 days) after the last alcoholic drink
- Delirium with alcohol withdrawal (in 1/3 of patients with untreated withdrawal seizures)
Tx: IV Benzodiazepines
Mild Neurocognitive Disorder (MCI)
mild cognitive impairment in one or more domains, often memory, with relative preservation of functioning and the absence of dementia
→cognitive changes are of concern to individual/family, does NOT impair activities of daily living
Dx: Clinical Diagnosis; Screening Tools: MMSE, MoCA, PHQ-9, neuropsychiatric testing
Tx: adjust modifiable factors/good support systems
Mild Neurocognitive Disorder (MCI)
What disorder may be a precursor to dementia?
S/Sx: impaired memory (primarily)
→behavioral symptoms more common with MCI (depression, irritability, anxiety, aggression, apathy
→one or more cognitive domains are impaired significantly
•Learning & memory • Language • Executive function • Complex attention • Perceptual-motor • Social
MMSE (Mini-Mental State Examination)
Screening test for cognitive impairment assessing verbal, memory, constructional abilities (visuospatial); does NOT assess executive function directly
- Age, education, and race/ethnicity each appear to have significant
effects on overall scores
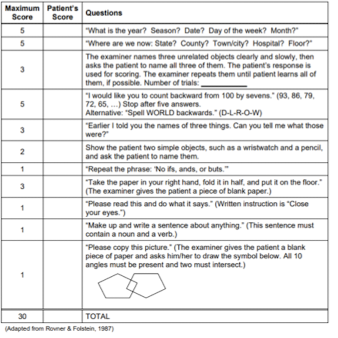
MoCA (Montreal Cognitive Assessment)
Screening test for cognitive impairment that assesses executive function
→more sensitive than the MMSE for detecting mild cognitive impairment

Major Neurocognitive Disorder (MND)
Neurocognitive disorder where the decline in cognitive functioning is substantial and interferes with the ability to be independent
S/S: Memory Difficulty (most common)
- Decline in cognition causing significant impairment
- Changes from baseline
Dx: Clinical Diagnosis (MMSE, MoCA; PHQ-2; neuropsychiatric testing, MRI imaging when indicated)
formerly classed as ‘dementia’
Alzheimer Disease (AD)
Disease characterized by early dementia, confusion, loss of recognition of persons or familiar surroundings, restlessness, and impaired memory
→the most common cause of dementia (MND)
- Risk Factors: Age (>65yo), family history, genetics, Down syndrome
Pathophysiology
→overproduction and/or decreased clearance of amyloid beta protein →deposits of amyloid beta peptides (plaques) and intracellular accumulation of tau proteins (neurofibrillary tangles)
→ neuron degenerates; atrophy starts in hippocampus (memory center) → temporal lobe → parietal lobe
Alzheimer Disease (AD)
Clinical presentation
-memory impairment about recent events (most common initial symptom in patient older than 65yo)
→behavioral and psychologic symptoms: apraxia, sleep disturbance more common as disease progresses
→loss of executive function: less organized or less motivated, multitasking often particularly compromised →Perceptual Motor deficits: easily disordered, get lost in unfamiliar environments →reduced insight into deficits (anosognosia), loss of insight declines over time clinical and pathological condition in which amyloid (proteins) accumulates
deposition of amyloid proteins in vessels of the brain, higher risk for hemorrhagic stroke
Dx: Clinical Diagnosis; definitive diagnosis requires histopathologic examination (post-mortem)
→MoCA has better sensitivity for executive and language dysfunction
Alzheimer Disease (AD)
Management
→primary focus on long-term amelioration of associated behavioral and neurologic problems, provide caregiver support
→memory aids early in disease (notebooks, reminders)
-keep familiar routine and setting
→medical therapy for management of symptoms
AVOID anticholinergic medications
Caregiver Education
-patient isn’t going to get better, goal to make their life better and keep them safe
-don’t force activities they don’t like
-don’t remind patient they are wrong/forget things
-plan for when patient will need help
-patient will eventually need to stop driving
-plan for self-care of caregivers
Dementia with Lewy Body (DLB)
Umbrella term that includes the neurocognitive diseases where Lewy bodies are found
- one of the most common causes of dementia after Alzheimer disease (AD) and vascular dementia
Pathophysiology
round eosinophilic, cytoplasmic inclusions in neurons → cortical atrophy following similar pattern of AD, involving frontal, temporal, parietal lobes, limbic structures; dopaminergic neurons more susceptible to alpha-synuclein dysfunction
Dementia with Lewy Body (DLB)
S/S: Dementia + Delirium
- Fluctuating cognition, spontaneous and episode episodes
- Recurrent visual hallucinations
- REM sleep behavior disorder (dream enactment after loss of atonia)
-Parkinsonism (bradykinesia, resting tremor, rigidity)
Dx: Clinical diagnosis, difficult to define
Tx: no cure; symptomatic treatment (trade-off between Parkinsonism and psychosis; medication management by neurologist)
Frontotemporal Dementia (FTD)
Clinically and neuropathologically heterogeneous disorder characterized by disturbances in behavior, personality, and language accompanied by focal degeneration of the frontal/temporal lobes and loss of cortical serotonergic innervation
- Risk Factors: genetic; 58yo mean age onset
→Behavioral variant (bvFTD): frontal variant, most common
→Primary Progressive Aphasia (PPA)
• Semantic variant primary progressive aphasia (svPPA)- historically known as temporal variant
• Nonfluent variant primary progressive aphasia (nfvPPA)- aka agrammatic
Frontotemporal Dementia Behavioral Variant (bvFTD)
most common variant of FTD involving progressive changes in personality and behavior
S/S:
• Disinhibition: kissing strangers, public flatulence, offense remarks, invading others’ personal space
• Apathy: losing interest and/or motivation for activities and social relationships
• Loss of empathy: “cold or unfeeling”
• Hyperorality: change in food preferences, binge eating/drinking/tobacco use, consuming inedible objects
• Compulsive behaviors: compulsive ritualistic behaviors; rigid personality, rigid food preferences, and inflexibility to changes in routine
• Anognosia: lack of insight about disease process
Primary Progressive Aphasia (PPA)
hallmark is early and progressive language disturbance/changes
→ relative preservation of episodic memory and other cognitive domains
→primary language dysfunction causing difficulty word finding and communicating with others
Variants:
Nonfluent Variant (nfvPPA) - causing effortful, halting speech with inconsistent speech-sound errors and distortions and agrammatism in language production; temporal variant analogous to Broca’s aphasia
Semantic Variant (svPPA): causing impaired single-word comprehension and object naming in setting of preserved fluency, repetition, and grammar; variant analogous to Wernicke’s aphasia
Progressive Supranuclear Palsy (PSP)
A neurodegenerative syndrome consisting of supranuclear gaze palsy, axial dystonia with a hypererect posture, bradykinesia, rigidity, and falls
→primarily affects basal ganglia (substantia nigra) and cerebellum
S/S:
• Oculomotor Dysfunction: eyes move slowly and cannot voluntarily look fully upwards or downwards
• Faces: eyes rarely blink, eyelid retraction which gives the appearance of “perpetual surprise”
• Cognitive Dysfunction: executive function deficits, changes in speech (some overlap with bvFTD)
• Neuropsych: apathy, insomnia
• Pyramidal signs: hyperreflexia, Babinski, dysarthria, dysphagia
• Postural instability and unexplained ‘spectacular’ fаlls backward out of proportion to other parkinsonian signs and symptoms
• Rigidity in axial muscles, especially the neck and upper trunk
“Gait stiff and broad based with knees and trunk extended and arms slightly abducted,” has been called the “drunken sailor gait”
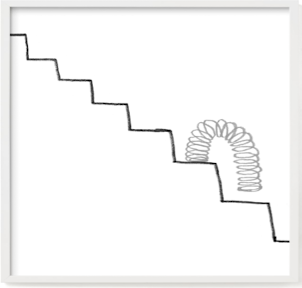
Vascular Dementia
Form of dementia caused by a stroke or other restriction of the flow of blood to the brain
- Risk factors: age, hypertension, diabetes mellitus, hyperlipidemia, low physical activity
Variants
A. Clinically patient is diagnosed with a stroke then develops dementia
B. No clinical history of stroke but changes in cognition, brain imaging identifies vascular brain injury in a patient with dementia
Vascular Dementia
Which form of dementia shows a "step-wise" decline of executive function?
→typically post stroke/blood restriction to brain
Normal Pressure Hydrocephalus (NPH)
pathologically enlarged ventricular size with normal opening pressures on lumbar puncture
→rare condition
S/Sx: TRIAD
1. Dementia: evolves over months/years after onset of gait disturbance
2. Gait disturbance: move slowly and take small steps, often with a wide base; difficulty turning, vulnerable to falls when turning
3. Urinary incontinence: urgency at early stages, urinary incontinence at later stages
Dx: Lumbar puncture (normal opening pressure); Imaging (enlarged ventricles)
Tx: implanted ventricular shunt in the brain (gold standard)
Syncope
transient loss of consciousness (TLOC) caused by period of inadequate cerebral blood flow
→peak in late adolescence to early adulthood (largely vasovagal); second peak later in older age with sharp rise after 70yo (more likely disease-related)
Subtypes:
1. Vasovagal (reflex-mediated; most common cause)
2. Orthostatic hypotension
3. Cardiac causes (arrhythmias, structural cardiopulmonary disease)
S/S: Brief loss of postural tone (8-10 seconds), total unresponsiveness to external stimulation (briefly no attention, awareness, cognition)
Tx: Self-limiting in 1-2 minutes
*EKG recommended after any episode

Reflex-Mediated Syncope
TLOC due to a reflex response that encompasses vasodilatation and/or bradycardia, leading to systemic hypotension and cerebral hypoperfusion
Three variants:
1. Vasovagal (most common; fear, prolonged standing, emotional)
2. Situational (urination, dedication, swallowing, coughing/sneezing)
3. Carotid sinus syndrome
*EKG recommended after any episode
Vasovagal
Most common cause of reflex-mediated syncope
→Often young and otherwise healthy patients
Triggers: fear, prolonged standing, emotional, warm environment
Prodrome
-lightheadedness -feeling of being warm/cold -sweating -palpitations -nausea -pallor reported by onlooking -tunnel vision, whooshing noise
Tx: self-limiting (1-2 minutes with fatigue afterward)
*EKG recommended after any episode
Orthostatic Hypotension Syncope
Reflex-mediated syncope due to a decrease in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg upon standing
Triggers:
1. Medication-related (diuretics, vasodilators, antidepressants)
2. Volume depletion (hemorrhage, GI issues, diminished thirst drive)
3. Autonomic failure:
Primary: Parkinson’s disease, pure autonomic failure, Lewy body dementia
Secondary: diabetes mellitus, amyloidosis, spinal cord injury, Guillain Barre
Tx: hydration, lower medication dose
*EKG recommended after any episode
Cardiac Causes Syncope
Reflex-mediated syncope involving heart rate that is too slow or too fast to permit maintenance of an adequate cardiac output and systemic arterial pressure
Etiology:
1. Tachyarrhythmias
2. Bradyarrhythmias (with inadequate ventricular response)
3. Structural heart disease (severe aortic stenosis, hypertrophic cardiomyopathy, cardiac tamponade, prosthetic valve dysfunction)
4. Cardiopulmonary/vascular (pulmonary embolus, severe pulmonary hypertension, aortic dissection)
*EKG recommended after any episode
Narcolepsy
A clinical syndrome of chronic daytime sleepiness with cataplexy, hypnagogic hallucinations, and sleep paralysis
→ begins in teens and early twenties; genetics; triggering event results in autoimmune destruction of orexin-producing neurons (strep pharyngitis, influenza)
Narcolepsy
S/Sx:
• Chronic daytime ѕlееpinеѕѕ (defining factor)
• Cataplexy: sudden loss of muscle tone (resulting in partial weakness), normally related to REM sleep; emotionally-triggered transient muscle weakness from positive emotions such as laughter, joking, or excitement, consciousness remains intact, and the weakness usually resolves in less than two minutes
• Hypnagogic hallucinations: dream-like hallucinations at sleep onset, can be visual, tactile or auditory, normally related to REM sleep
• Hypnopompic hallucinations: dream-like hallucinations at waking
• Sleep paralysis: complete inability to move for one or two minutes when awakening or when falling asleep
Ddx: Sleep Study (polysomnography)
Tx:
-Sleep hygiene (avoid sleep deprivation)- sleep deprivation often worsens symptoms
-Daytime naps (mainstay of therapy, 1-2 20 min naps)
-Avoid substances that increase sleepiness and/or that prevent nighttime sleep
-Pharmacotherapy to improve wakefulness
Coma
Unarousable unresponsiveness; the most profound degree to which the two components of consciousness, arousal and awareness, can be diminished
Etiology: brain injury (trauma); cerebrovascular disease, intoxications, infections, seizures (including nonconvulsive status epilepticus [NCSE]), metabolic derangements
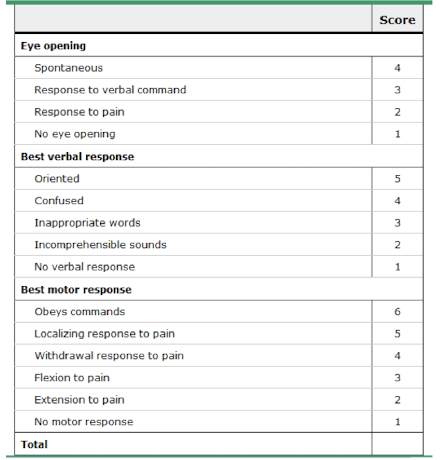
PE: neurologic examination and Glasgow Coma Scale (GCS)
- Level of "consciousness" (GCS)
- Motor response (muscle tone - spastic/flaccid; posturing)
- Brainstem reflexes (pupillary, corneal, vestibuloocular reflex ‘doll’s eyes)
Tx: acute, life-threatening emergency, requiring prompt intervention for preservation of life and brain function
→ABCs, intubation with GCS <8, stabilize cervical spine, supplement oxygen, IV access, blood pressure support
GCS (Glasgow Coma Scale)
What is the index of depth of impaired consciousness and for prognosis of coma?
→higher score = better prognosis
→technically used as serial assessments of comatose patients
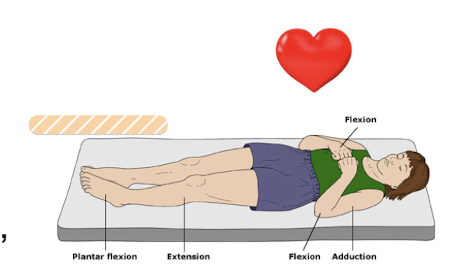
decorticate posturing
What type of motor response during coma assessment involves upper extremity adduction, flexing “hands toward the heart”?
→better prognosis
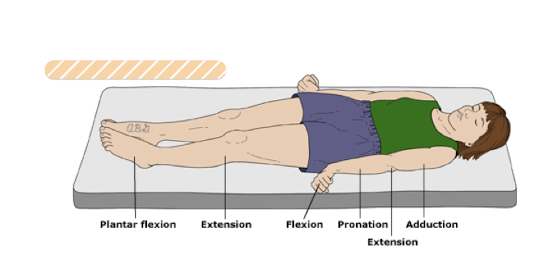
decerebrate posturing
What type of motor response during coma assessment involves upper extremity abduction, extension and pronation, lower extremity extension?
→worse prognosis
brainstem reflexes
A. Pupillary: direct/consensual response to light; mediated at level of midbrain
B. Corneal: eyes blink when cornea is touched; mediated at level of the pons
C. Vestibuloocular reflex (VOR): response to maintain line of sight stable with head movement; mediated from midbrain to pons and medulla
Essential during coma evaluation to localize brainstem involvement (mediates heart rate/respiratory) and severity
Pupillary Reflex
Which brainstem reflex tested during coma evaluation is mediated at level of midbrain?
→Positive reflex: assesses direct/consensual response to light

Corneal Reflex
Which brainstem reflex tested during coma evaluation is mediated at level of pons?
→Positive reflex: eyes blink when cornea is touched
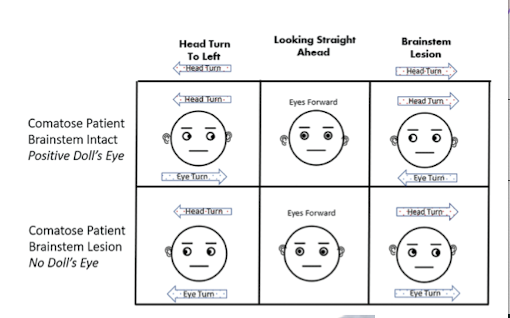
Vestibuloocular Reflex (VOR)
Which brainstem reflex tested during coma evaluation is mediated from midbrain to pons and medulla?
→response to maintain line of sight stable with head movement
→”Doll’s Eyes”: assuming NO C-spine injury; move head from one side to the other
Positive Doll’s eyes: reflex is present, normal finding
Negative Doll’s eye: eyes fall in same direction as movement of head ABNORMAL, poor prognosis; brainstem is not intact
Special Testing: Caloric Testing: only done if Doll’s eye is negative, providing stronger stimulus for reflex eye