The digestive system - chapter 21
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
92 Terms
What is the routs food in the oral cavity take when swallowed?
esophagus
stomach
small intestine
duodenum
jejunum
ileum
large intestine
rectum
Of what 4 layers does the GI tract wall consist?
an inner mucosa facing the lumen:
mucosal epithelium → The cells of the mucosa include transporting epithelial cells, endocrine and exocrine secretory cells, and stem cells.
lamina propria → subepithelial connective tissue that contains nerve fibers and small blood and lymph vessels. This layer also contains wandering immune cells.
muscularis mucosae → a thin layer of smooth muscle, separates the lamina propria from the submucosa. Contraction of muscles in this layer alters the effective surface area for absorption by moving the villi back and forth
submucosa —> composed of connective tissue with larger blood and lymph vessels. it also contains the submucosal plexus, which innervates cells in the epitheliul layer and smooth muscle of the muscularis mucosae
muscularis externa → contains the myenteric plexus, which lies between the inner and outer muscle layer, and coordinates motor activity of the muscles
an inner circular layer
an outer longitudinal layer
The stomach has an incomplete third layer of oblique muscle between the circular muscles and the submucosa.
serosa -? connective tissue membrane that is the continuation of the peritoneal membrane.
What types of cells are found in the GI mucosal epithelium?
transporting epithelial cells
endocrine and exocrine secretory cells
stem cells
What do epithelial cells secrete at the luminal surface?
Ions, enzymes, mucus, and paracrine molecules.
How do tight junctions differ between parts of the GI tract?
stomach and colon — the junctions form a tigh barrier so that little can pass between the cells
the small intestine — junctions are not so tight. the intestinal epithelium is considered “leaky”
What makes the GI tract particularly susceptible to cancer?
The rapid turnover and division rate of stem cells in the epithelium.
What are Peyer’s patches?
Lymphoid aggregations that are part of the gut-associated lymphoid tissue(GALT). these structures are found in the lamina propria of the mucosal layer of the GI tract.
What structures increase surface area in the GI tract?
the gut wall is crumpled into folds:
Rugae in the stomach
Plicae in the small intestine
additional surface is aided by:
Villi in the intestinal mucosa
Gastric glands and crypts (tubular invaginations)
What is the primary function of the digestive system?
to move nutrients, water and electrolytes from the external environment into the body’s internal environment.
What are the chalenges of autodigestion that the GI tract faces?
the food we eat is mostly in the form of macromolecules. so our digestive system must secrete powerful enzymen to digest food into molecules that are small enough to be absorbed into the body.
at the same time, these enzymes must not digest the cells of GI tract itself — autodigestion
What is the challange of mass balance that the GI tract faces?
matching fluid input with output
What is the challenge of defence that the digestive system faces?
protecting the pody from foreign invaders.
the GI tract is assisted by an array of physiological defence mechanisms, including mucus, digestive enzymes, acid and the largest collection of lymphoid tissue in the body—GALT
What are the 4 processes the digestive system to perform their primary function?
digestion
absorption
secretion
motility
What is digestion?
the chemical and mechnical breakdown of food into smaller units that can be taken across the intestinal epithelium
What is absorption?
the movemnt of substances from the lumen to the GI tract to the extracellular fluid
What is secretion?
can mean 2 things:
the movement of water and ions from the ECF to the digestive tract lumen
the release of substances synthesized by the GI epithelial cells into either the lumen or the ECF
What is motility when it comes to the GI tract?
the movement of materials in the GI tract as a result of muscle contraction
What are the 2 purposes of motility in the GI tract?
moving food from the mouth to the anus
mechanically mixing food to break it into uniformly small particles. This mixing maximizes exposure of the particles to digestive enzymes by increasing particle surface area.
What are tonic contractions?
contractions that are sustained for minutes or hours.
They occur in some smooth muscle sphincters and in the anterior portion of the stomach.
What are phasic contractions?
consist of contraction-relaxation cycles lasting only a few seconds.
these occur in tthe posterior region of the stomac and in the small intestine.
What are slow wave potentials/slow waves?
cycles of depolarization and repolarization.
When a slow wave potential does reach threshold, voltage-gated Ca2+ channels in the muscle fiber open, Ca2+ enters, and the cell fires one or more action potentials. The depolarization phase of the slow wave action potential, like that in myocardial autorhythmic cells, is the result of Ca2+ entry into the cell. In addition, Ca2+ entry initiates muscle contraction.
these cycles are associated with teh cycles of smooth muscle contraction and relaxation.
What is a single-unit smoorth muscle?
a type of smooth muscle tissue where individual muscle cells contract together as a single unit
What is the migrating motor complex?
a pattern → between meals, when the tract is largely empty, a series of contractions begins in the stomach and passes slowly from section to section, each series taking about 90 minutes to reach the large intestine.
it is a “houskeeping” function taht sweeps food remnant and bacteria out of the upper GI tract and into the large intestine
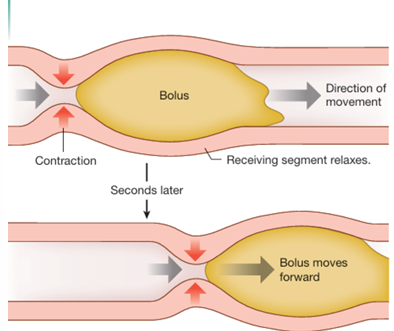
What is peristalsis?
progressive waves of contraction that move from one sectrion of the GI tract tp the nex.
the circular muscles contract just behind a mass, which pushes the bolus forward into the receiving segment.
Peristalsis contributes to food mixing in the stomach but in normal digestion, intestinal peristaltic waves are limited to short distances.
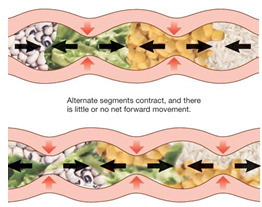
What are segmental contraction?
short segments of the intestine alternately contract and relax.
in the contracting segments → circular muscles contract while longitudinal muscles rela
alternating segmental contractions churn the intestinal contents, mixing them and keeping them in contact with the absorptive epithelium.
What is the function of the enteric nervous system?
controls the motility, secretion and growth of the digestive tract
What are the features the ENS has in common with the CNS?
intrinsic neurons of the 2 nerve plexus of the digestive tract are those neurons that lie completely within the wall of the gut, just like the interneurons are completly contained within the CNS
ENS neurons release more than 30 neurotransmitters and neuromodulators, most of which are identical to the brain
glial support cells within the ENS are more similar to astroglia of the brain than to Schwann cells of the peripheral nervous system
diffusion barrier. the capiillaries that surround the ganglia in the ENS are not very permeable and create a dissufion barrier that is similar to the blood-brain barrier of the cerebral blood vessels
integrating centers. Reflexes that originate in the GI tract can be integrated and acted on without neural signals leaving the ENS. For this reason, the neuron network of the ENS is its own integrating center, much like the brain and spinal cord.
What are short reflexes?
reflexes that originate in the ENS and are integrated there without outside input
What does the submucosal plexus do?
it receives sensory signals from the gut lumen →Integrates sensory information → initiates responses.
Controls secretion by GI epithelial cells
What is the role of the myenteric plexus?
influences motility in the muscularis externa
What are long reflexes?
digestive reflexes that are integrated into the CNS
What local stimuli can initiate digestive (short) reflexes via the ENS?
Distension,
presence of food,
osmolarity,
acid
in the gut lumen
What activates a feedforward reflex?
a feed forward reflex is long reflec, that usually begins with the isght, smell of food, and preare the digestive system for food that the brain is anticipating
How do GI peptide control the digestive system?
they excite or inhibit motility and secretion.
GI hormones are secreted into the blood and transported throughout the body. They act on the GI tract, on accessory organs, and on distant targets.
What are the 3 families of GI hormones?
gastrin
gastrin and cholecystokinin (CCK)
secretin
secretin, VIP, GIP, GLP-1
those that do not fit into the other 2 families
motilin
What is the function of gastrin?
stimulates gastric acid secretion and mucosal growth
What is the function of CCK?
stimulates galbladder contraction and pancreatic enzyme secretion
inhibits gastric emptying and acid secretion
What is the function of secretin?
stimulates HCO3- sercetion
inhibits gastric emptying and acid secretion
What is the function of motilin?
stimulates migrating motor complex
What is the function of gastric inhibitory peptide(GIP)?
stimulates insulin release(feedforward mechanism)
inhibits gastric emptying and acid secretion
What is the function of glucagon-like peptide-1(GLP-1)?
stimulates insulin release
inhibits glucogon release and gastric function
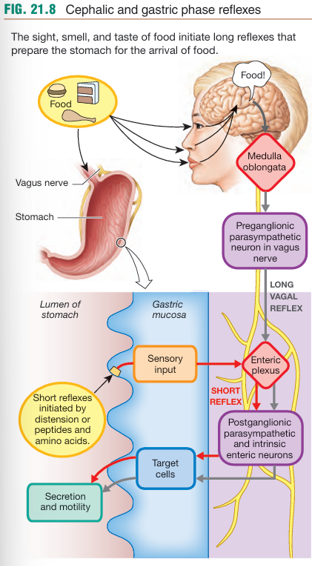
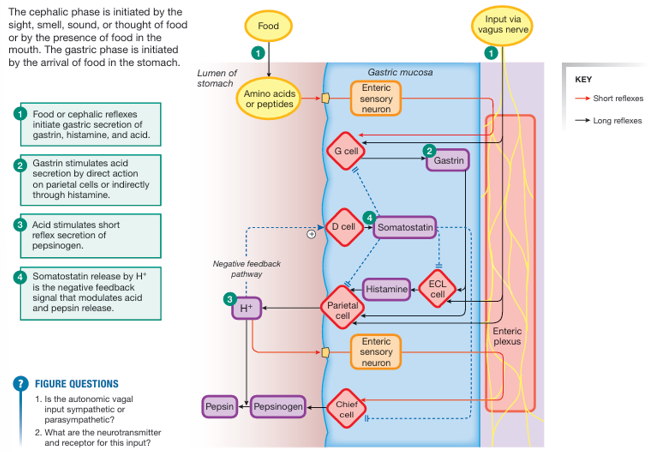
How does the cephalic phase work?
it is a feedforward response, created by long reflexes that began in the brain.
anticipatory stimuli and stimulus of food in the oral cavity activate neurons in the medulla oblongata
the medulla in turn sends an efferent signal through autonomic neurons to the salivary glands and through the vagus nerve to the ENS
in response to the signals, the stomach intestine and accessory glandular organs begin secretion and increase motility in anticipation of the food to come
What are the 4 important functions of saliva?
soften and moisten food
digestion of startch → Chemical digestion begins with the secretion of salivary amylase. Amylase breaks starch into maltose after the enzyme is activated by Cl- in saliva.
taste → saliva dissolves food so that we can taste it
defene →lysozyme is an antibacterial salivary enzyme, which diables bacteria and virusses. 1. In addition, saliva helps wash the teeth and keep the tongue free of food particles.
What does saliva contain?
water
ions
mucus
proteins
immunoglobulins
What causes the secretion of saliva?
Salivation is under autonomic control and can be triggered by multiple stimuli, including the sight, smell, touch, and even thought of food. Parasympathetic innervation is the primary stimulus for secretion of saliva, but there is also some sympathetic innervation to the glands.
Which 3 salivary glands produce saliva?
parotid glands → produce a watery solution of enzymes
sublingual glands → produce mucus-rich saliva
submandibular glands → secretions are mixed, with both mucus and enzymes
How is saliva produced?
the initial fluid secreted by acinar cells resembles extracellular fluid in its ionic composition: an isotonic NaCl solution
as the fluid passes through the duct, epithelial cells along the duct reabsorb NaCl and secrete K+ and HCO3- until the ion ratio in the duct fluid is more like that of intracellular fluid
The apical membranes of the duct cells have very low water permeability, and the net removal of solute from the secreted fluid results in saliva that is hyposmotic to plasma.
what are the steps of deglutition(swallowing) reflex?
swallowing is intergrated in the medulla oblongata. sensory afferent in cranial nerve IX and somatic motor and automatic neurons mediate the reflex.
the tongue pushes the bolus against soft palate and back of the mouth, triggering the swallow reflex
breathing is inhibited as the bolus passes the closed airway
food moves downward into the esophagus, propelled by peristaltic waves and aided by gravity
What are the three functions of the stomach?
storage — the stomach stores food and regulated its passage into the small intestine, where most of the digestion and absorption takes place
digestion — the stomach chemically and mechanically digests food into chyme
defence — teh stomach protects the body by destroying many bacteria and other pathogens that are swallowed with the food and trapped away in the mucus
How is the gastric phase controlled?
before food arrives:
digestive activty in the stomach begins with the long vagal reflex of the cephalic phase
when food enters the stomach:
stimuli in the gastric lumen initiate a series of short reflexes — the gastric phase
digestion of the stomach and the presence of amino peptides or amino acids in the lumen activate endocrine cells and enteric neurons
What is receptive relaxation in the stomach?
A neurally mediated reflex that allows the stomach to relax and expand to accommodate food from the esophagus.
What happens in the upper stomach after food arrives?
it holds the food until it is ready to be digested
Why must the stomach regulate the rate at which food enters the small intestine?
To prevent overwhelming the small intestine's digestive and absorptive capacity.
What is the role of the distal stomach during digestion?
It performs peristaltic waves that mix food with acid and enzymes, and slowly push chyme into the duodenum.
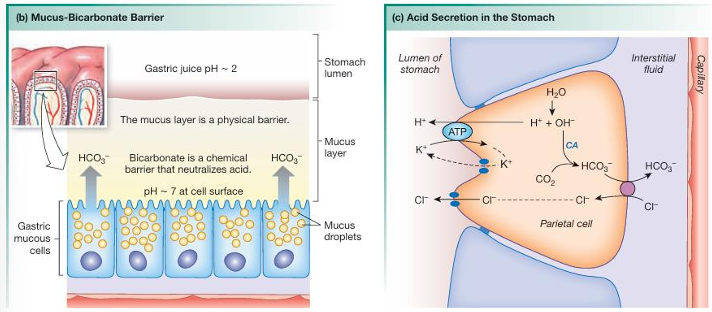
How does acid secretion take place in the stomach?
H+ from water inside the parietal cell is pumped into the stomach lumen by a H+-K+-ATPase, in exchange for K+ entering the cell
Cl- then flows the electrical gradient created by H+, by moving though the open Cl- channels
this gives a net result of HCl secretion
while the acid is being secreted into the lumen, HCO3- made from CO2 and OH-(from water) is absorbed in the blood
HCO3- makes the blood leaving the stomach less acidic, creating a alkaline tide.
How are the cephalic phase and gastric phase secretion integrated?
the cephalic reflex initiates gastic secretion of gastrin, histamine, and acid
gastrin stimulates acid secretion by direct action on arietal cells or indirectly through histamine
acis stimulates a short reflex of pepsinogen secretion
somatostatin release by H+ is the negative feedback signal that modulates acid and pepsin release
What is the intrinsic factor?
a protein secreted by the same gastric parietal cells that secrete acid.
in the lumen of the stomch the intrinsic factor complexes with vitamine B12, a step that is needed for the vitamin absorption in the intestine
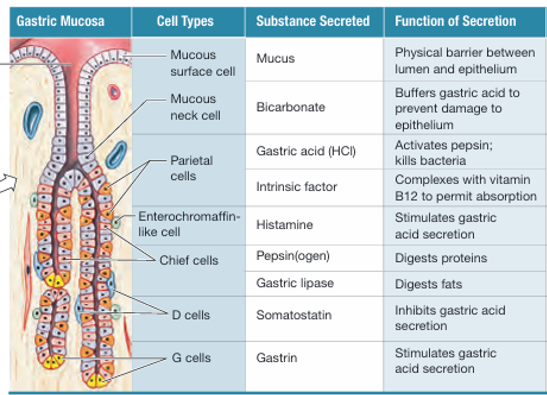
name the cells and their function
see figure
What is the function of the controlled motility in the small intestine?
the intestinal contents are slowly propelled forward by a combination of segmental and peristaltic contractions.
these actions mix chyme with enzymes and they expose digested nurtients to the mucosal epithelium for absorption
What promotes intestinal motility?
parasympathetic innervation
gastrin
CCK
the forward movemnt of chyme through the intestine must be slow enough to allow degestion and absorption to go to completion.
What is the difference in the motility of the large and small intestine?
small intestine → the intestinal contents are slowly propelled forward by a combination of segmental and peristaltic contractions. these actions mix chyme with enzymes and they expose digested nurtients to the mucosal epithelium for absorption
large intestine → Haustral contractions (slow segmenting), peristalsis, and mass movements.
What is the difference in the digestion and absorbption of the large and small intestine?
small intestine → Major site for chemical digestion and nutrient absorption. — different enzymes aid the digestion and it absorbs most nutrients
large intestine → no significant digestion of organic molecules, however numerous bacteria inhibiting the colon break down significant amount of undigested complex carbohydrates and proteins through fermentation.
— Absorbs water, electrolytes, and some vitamins produced by gut
Where does the most absorbtion take place?
in the small intestine specifically:
duodenum
jejunum
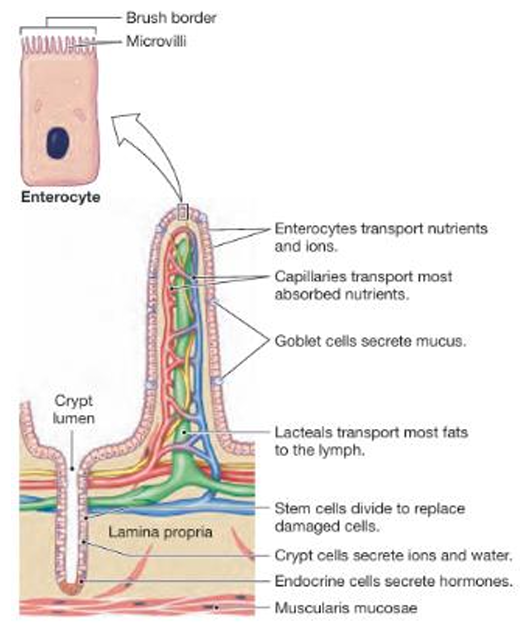
How does the small intestine facillitate secretion, digestion and absorption?
by maximizing the surface area.
absorption takes place along the villi
fluid an hormone secretion and cell renuwal from stem cells ocuurs in the crypts
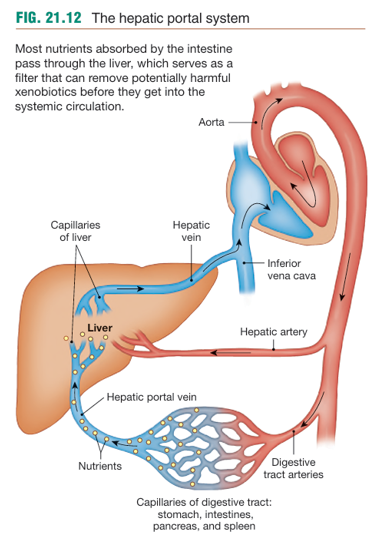
Venous blood from the digestive tract first passes into the hepatic portal system. This specialized region of the circulation has two sets of capillary beds.
What are these 2 capillary beds?
one that pick u absorbed nutrients at the intestine
another that delivers the nutrients directly to the liver
What are the 2 secretory epithelia of the pancrease and what do they secrete?
endocrine — islets of Langerhans, and secrete insulin and glucagon
exocrine — include digestive enzymes(tripsinogen) and a watery solution of sodiumbicarbonate(NaHCO3)
What is secreted by hepatocytes, liver cells, and what does it consist of?
Bile
bile salts → facilitate enzymatic fat digestion
bile pigments → waste products of hemoglobin degradation
cholesterol → is excreted in the feces
What is the function of bile salts?
they act as detergens to make fats soluble durning digestion
What is the function of mucus produces from the intestinal goblet cells?
protects the epithelium and lubricates the gut’s contents
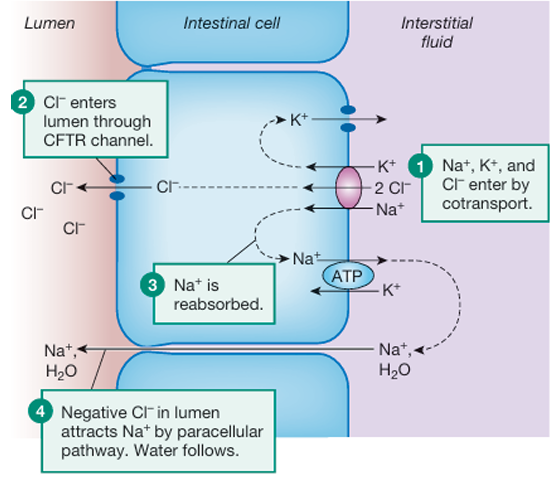
How do crypt cells in the small intestine and colon secrete isotonic NaCl solution?
Na+, K+ and Cl- enter the cell by co-transport
Na+ is reabsorbed (K+ is also reabsorbed)
Cl- enters the lumen through CFTR channel
negative Cl- in the lumen attracts Na+ by paracellular pathway, and water follows
Of what does the exocrien protion of the pancrease consist?
The exocrine portion of the pancreas consists of acini. Ducts from the acini empty into the duodenum. The acinar cells secrete digestive enzymes, and the duct cells secrete the NaHCO3 solution.
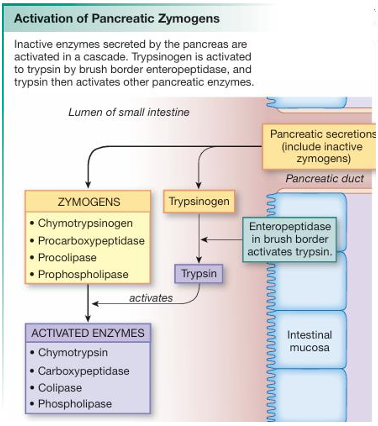
How are pancreatic zymogen activated?
the brush border enteropeptidase converts inactive trypsinogen to active trypsin.
trypsin then is able to convert the orther pancreatic zymogens to their active forms.
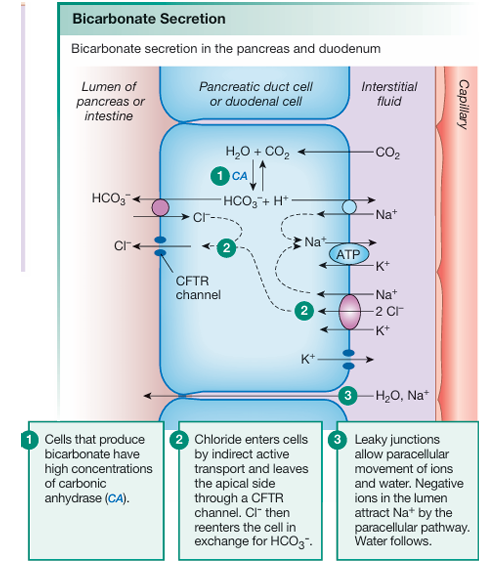
How is bicarbonate secreted in the pancrease and duodenum?
cell that produce bicarbonate have high concentrations of carbonic anhydrase(CA)
Cl- enters cells by indirect active transport and leaves the apical side through the CFTR channel. Cl- ten reenters the cell in exchange for HCO3-
leaky junctions allow paracellular movement of ions and water. negative ions in the lumen attract Na+ by the paracellular pathway. water follows
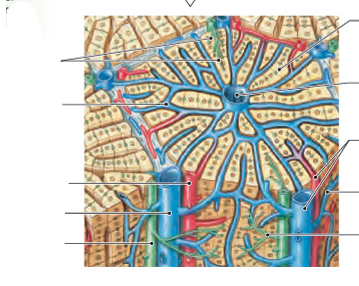
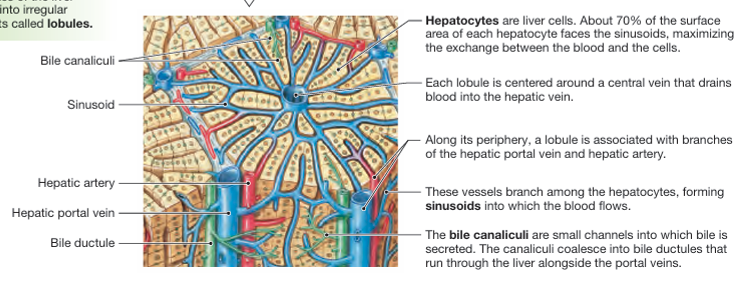
name the structures
see figure
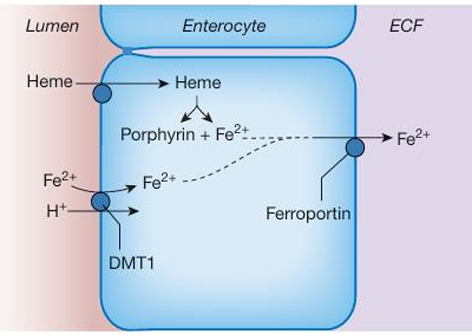
How is ion(Fe2+) absorbed?
ionized iron Fe2+ is actively absorbed by apical co-transport with H+ on the divalent metal transporter 1(DMT1)
inside the cell, enzymes converts heme iron into Fe2+
both pools of ion leave the cell in the transporter ferroportin
Iron uptake by the body is regulated by hepcidin.
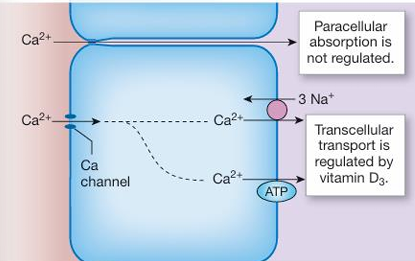
How is calcium absorbed?
passive, unregulated movement through paracellular pathways
hromonally regulated transepithelial Ca2+ transport takes place in the duodenum.
Ca2+ enters the enterocyte through apical Ca2+ channels
then is actively transported across the basolateral membrane by either Ca2+-ATPase or Na+-Ca2+ antoporter
Ca2+ absorption is regulated by vitamin D3
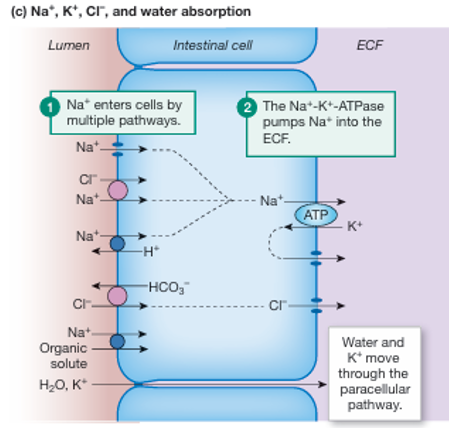
How does Na+, K+, Cl-, and water absorption work?
Na+ absorbtion
Na+ enters the cells by multiple pathways
apical Na+ channels such as ENaC
Na+-Cl- symporter,
Na+-H+ exchanger (NHE).
The Na+-K+-ATPase pumps Na+ into the ECF
Chloride uptake uses an apical Cl--HCO3 - exchanger and a basolateral Cl- channel to move across the cells.
Potassium and water absorption in the intestine occur primarily by the paracellular pathway.
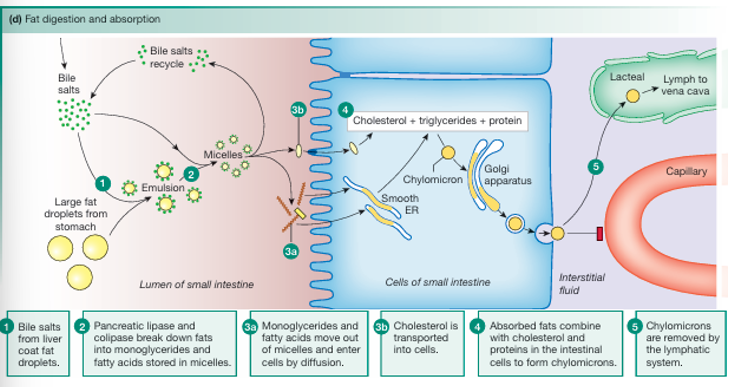
How are fats digested and absorped?
bile salts from liver coat fat droplets
pancreatic lipase and colipase break down fats into monoglycerades and fatty acids stored in micelles
a and b
monoglycerades and fatty acids move out of micelles and enter the cell by diffusion
cholesterol is transported into the cells
the absorbed fats combine with cholesterol and proteins in the intestinal cell to form chylomicrons
Once monoglycerides and fatty acids are inside the enterocytes, they move to the smooth endoplasmic reticulum, where they recombine into triglycerides. The triglycerides then join cholesterol and proteins to form large droplets— chylomicrons.
Because of their size, chylomicrons must be packaged into secretory vesicles by the Golgi. The chylomicrons then leave the cell by exocytosis.
chylomicrons are absorbed into lacteals, the lymph vessels of the villi.
Chylomicrons pass through the lymphatic system and finally enter the venous blood just before it flows into the right side of the heart.
How is glucose digested?
digestion
The enzyme amylase breaks long glucose polymers into smaller glucose chains and into the disaccharide maltose.
Pancreatic amylase then resumes digestion of starch into maltose.
Maltose and other disaccharides are broken down by intestinal brush border disaccharidases to glucose
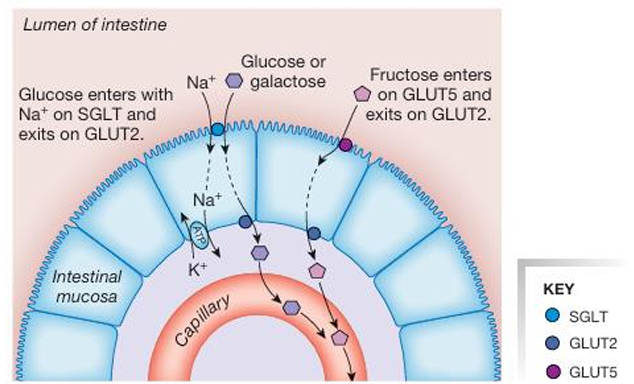
How is glucose absorped?
glucose and galactose is transported over the apical membrane via Na+ - glucose SGLT sympoters
and transported over the basolateral membrane via GLUT2 transpoters
fructose moves across the apical membrane by facilitated difussion on the GLUT5 transporter and across the basolateral membrane by a GLUT2 transpoter
What are the 2 groups of enzymes for protein digestion?
endopeptidase → proteases attack peptide bonds in the interior of the amino acid chain and break a long peptide chain into smaller fragments
exopeptidase → release single amino acids from peptidases by chopping them off the ends one at a time
What are the primary products of protein digestion?
free amino acids
dipeptides
tripeptides
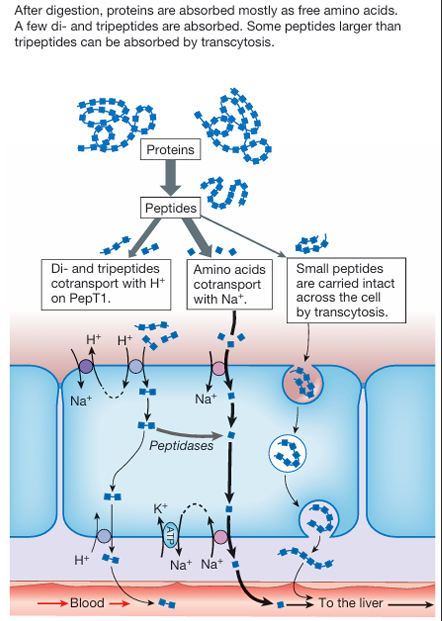
How are the digested proteins absorbed?
most free amino acids are carried by Na+-dependent co-transport
a few amino acids transporters are H+ dependent
dipeptided and tripeptides are carried into enterocytes on the oligopeptide transporter PepT1 that uses H+-dependent co-transport
once ingested oligopeptides have two possible fates:
Most are digested by cytoplasmic peptidases into individual amino acids, which are then transported across the basolateral membrane and into the circulation.
Oligopeptides that are not digested are transported intact across the basolateral membrane on an H+-dependent exchanger.
Some peptides larger than three amino acids are absorbed by transcytosis after binding to membrane receptors on the luminal surface of the intestine.
How is vitamin B12 absorbed?
The intestinal transporter for B12 is found only in the ileum and recognizes B12 only when the vitamin is complexed with an intrinsic factor
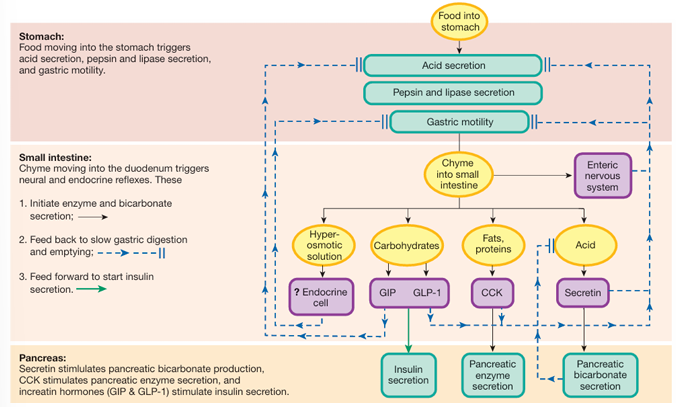
How is the intestibal phase of digestion controled(neural and hormonal control)?
chyme entering the intestine activates the ENS, which then decreases gastric motility and secretion and slows gastric emptying
secretin is released by the presence of acidic chyme in the duodenum, and inhibits acid production and decreases gastric motility. production of pancreatic HCO3- is stimulated, and neutralizes the chyme
CCK is secrted due to fat. it slows the gastric motility and acid secretion
GIP and GLP1 is released if the meal contains carbohydates, they feedforward to promote insulin release, allowing cell to prepare for glucose that is about to be absorbed. they also decrease gastric motility and acid secretion
the mixture of acid, enzymes and digested food in chyme forms a hyperosmotic solution. sensors in the intestine wall are sensitive to this and inhibit gastric emptying in a reflex.
What is the purpose of the bacteria in the gut?
numerous bacteria inhibiting the colon break down significant amounts of undigested complex carbohydates and proteins, through fermentation. colonic bacteria also produce significant amounts of absorbable vitamins, like vitamin K
What are the 7 regions of the large intestine?
The cecum is a dead end pouch with the appendix, a small fingerlike projection, at its ventral end.
Material moves from the cecum upward through the ascending colon,
horizontally across the body through the transverse colon,
then down through the descending colon and sigmoid colon.
The rectum is the short terminal section of the large intestine.
It is separated from the external environment by the anus, an opening closed by two sphincters, an internal smooth muscle sphincter and an external skeletal muscle sphincter.
What is the function of the defecation reflex?
it removed undigested feces from the body.
it is a spinal reflex triggered by distension of the organ wall. the movement of the fecak material into the normally empty rectum usually triggers the reflex
What is diarrhea and what causes it?
a pathological state in which intestinal secretion of fluid is not balanced by absorption, resulting in watery stools.
Diarrhea occurs if normal intestinal water absorption mechanisms are disrupted or if there are unabsorbed osmotically active solutes that “hold” water in the lumen.
What is the function of GALT?
Gut-associated lymphoid tissue prevents pathogens from entering the body through delicate absorptive tissues
The first lines of defense are the enzymes and immunoglobulins in saliva and the highly acidic environment of the stomach. if this fails:
sensory receptors and the immune cells of teh GALT respond.
The immune system of the intestinal mucosa consists of immune cells scattered throughout the mucosa, clusters of immune cells in Peyer’s patches and specialized epithelial cells called M cells (microfold cells) that overlie the Peyer’s patches.
The M cells provide information about the contents of the lumen to the immune cells of the GALT.
What is vomiting?
the forcefull expulsion of gastric and duodenal contents from the mouth.
it is a reflex that removes toxic material from the GI tract before they can be absorbed.
What causes diarrheas to occur?
when bacterial toxins enhance colonic Cl- and fluid secretion. when exessive fluid secretion is coupled with increased motility, diarrhea results.
Secretory diarrhea in response to intestinal infection can be viewed as adaptive because it helps flush pathogens out of the lumen.