Lecture 15 - Radiation Protection in Diagnostic Imaging & Fluoroscopy + Phantoms
1/96
Earn XP
Description and Tags
ONCOL 243 - Radiation Safety. University of Alberta
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
measures must be taken to ensure that radiographic equipment operates safely to protect ….
patients and staff
what are two things that every diagnostic imaging system must have
protective tube housing
correctly functioning control panel
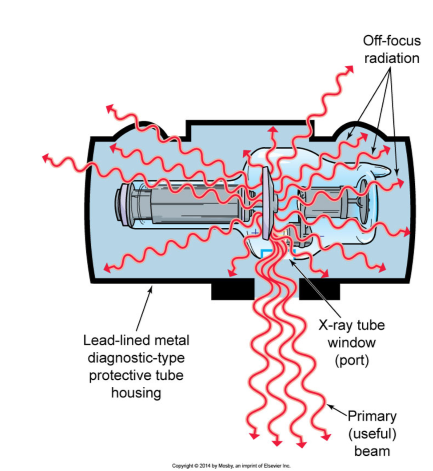
why do x-ray tubes need to be surrounded by a lead protective housing tube?
to reduce off focus radiation
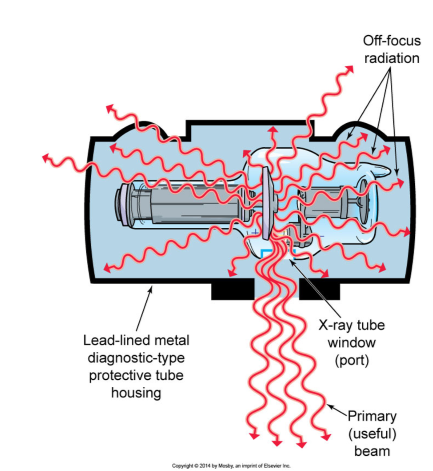
what dose rate value must the lead housing be constructed to minimize dose from 1 m away from the sorurce?
1 mGy/hr or less
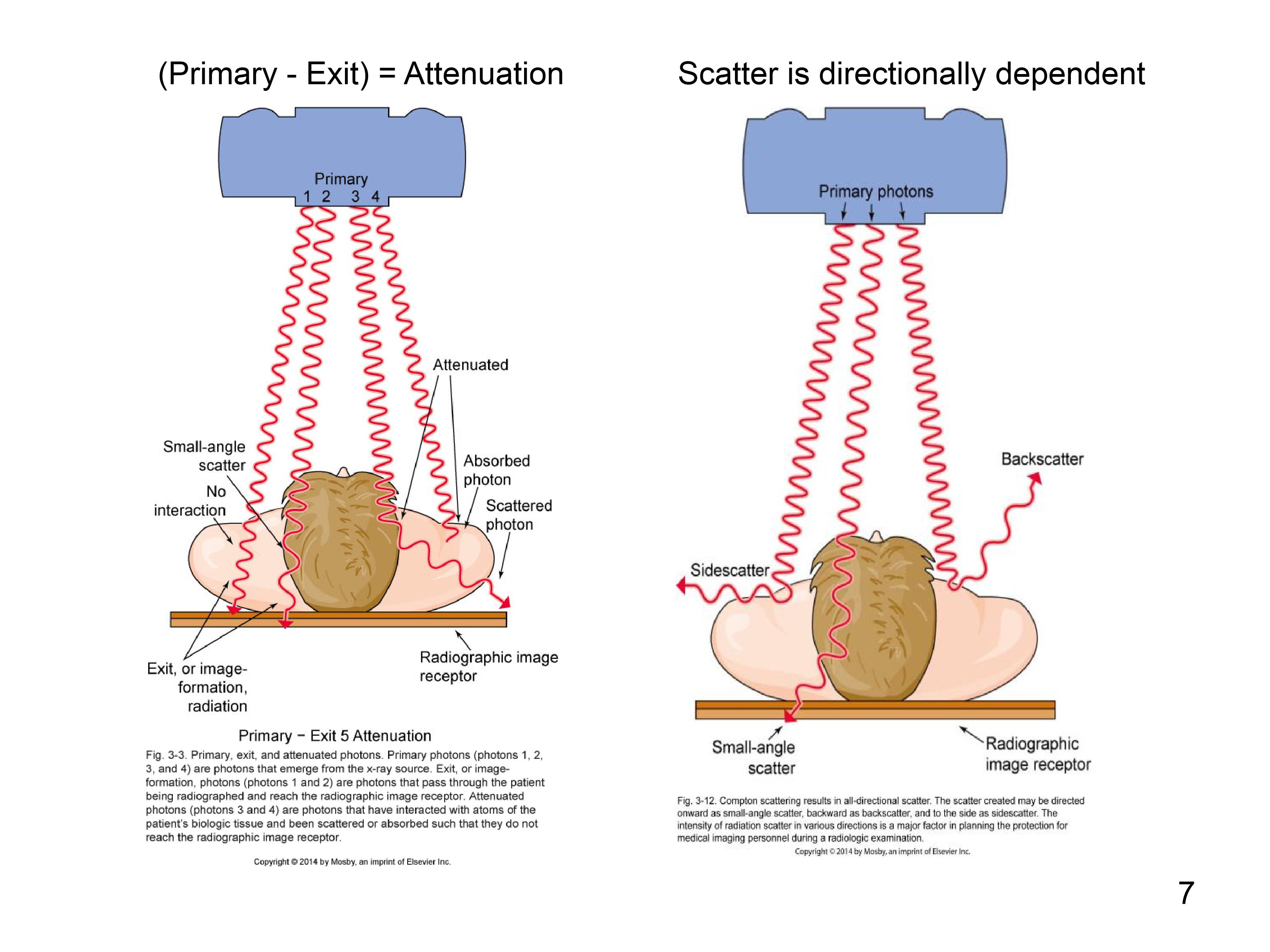
what three types of photons need to be considered when creating radiation protection
absorbed, scattered, and attenuated photons

where must the x-ray control panel be located, and what must it have
must be located behind a protective barrier that still allows observation of the patient
must have mA and kVp readouts and a beeper to tell you when radiation is on

What 4 requirements are there of the radiographic examination table
table must be able to adequatly support patient
must be able to move around to maneuver patient
must have uniform thickness
must be as radiolucent as possible
why must the exam table be radiolucent (transparent to x-rays)
to absorb minimal amount of radiation to reduce patient dose
why must the exam table be uniform thickness?
to ensure consistent imaging quality and reduce distortion during radiographic procedures.
What is Source to Image Receptor (SID) distance?
The distance between the radiation source and the image receptor, which affects image quality and patient dose.
what device is used to measure the SID
can be something as simple as a tape measure or as complex as lasers
What are x-ray beam limitation devices?
decices that are placed on on the end of the x-ray tube to adjust the size and shape of the x-ray beam to minimize exposure
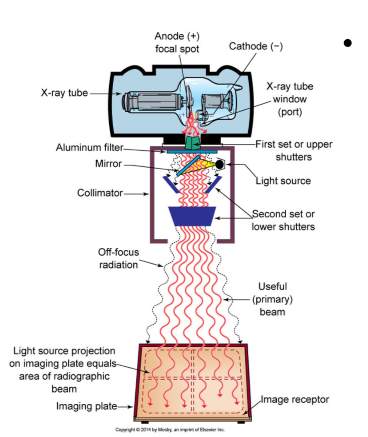
what is the most common type of beam limitation device for x-rays machines (don’t need to know off top of head)
light-localizing variable-aperature rectangular collimator (LLVARs)
What do LLVARs (light-localizing variable-aperature rectangular collimator) do?
redice the off-focus radiation to minimize skin exposure to photons or electrons (produce by photon interactions with collimator)
also help with alignment of beam
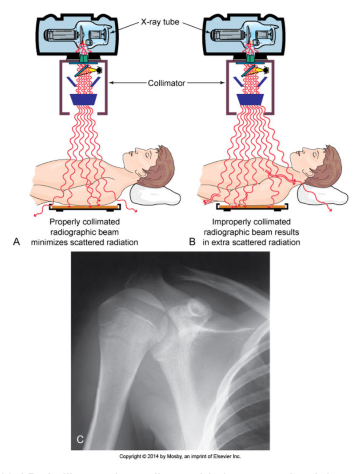
What does Positive Beam Limitation (PBL) imply?
Positive Beam Limitation (PBL) implies that the x-ray beam is automatically collimated to the size of the image receptor, ensuring that the area exposed is no larger than necessary, thereby reducing patient radiation exposure.
radiographic beam must not be larger than image detector
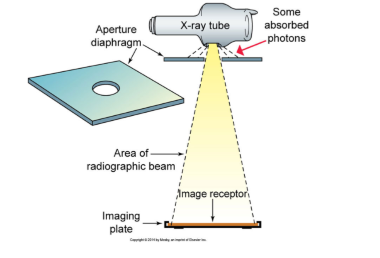
what are the simplest types of beam limitation devices?
aperature diaphragms and cones
what are cones?
a non-electronic way to collimate the beam involving metal tubes
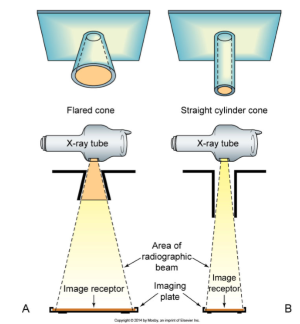
when are cones used for radiography?
when examining specific areas, like the head or teeth
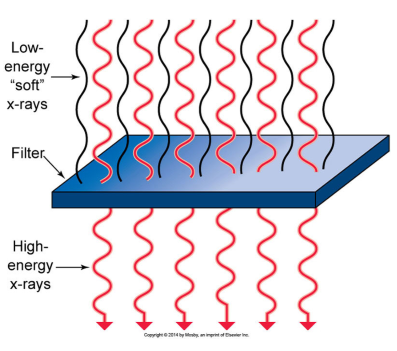
what is the purpose of radiographic beam filtration
to remove low-energy photons from the beam, improving image quality and reducing patient dose.
two types of filtration
inherent and added
Inherent filtration + added filtration = ?
total filtration
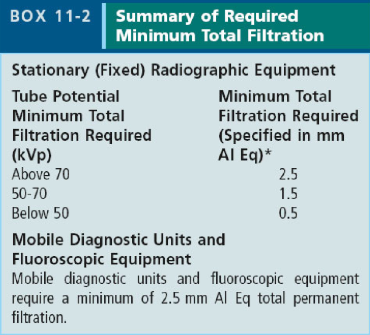
how is the minimum amount of filtration required for a radiography machine determined?
by the kVp/energy of the machine
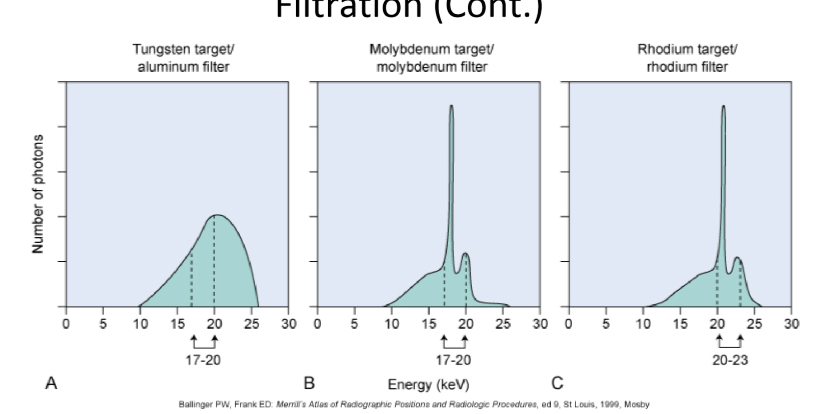
what is the most common type of filtration material for radiography
aluminum
why is aluminum the most widely selected filter material?
removes soft x-rays from polyenergetic x-ray beam without decreasing beam intensity
what filtration material is used for mammography?
molybedenum and rhodium
why does mammo use molybedenum and rhodium instead of aluminum
to get the proper contrast needed for visualing structures in dense breast tissue
uses higher energies
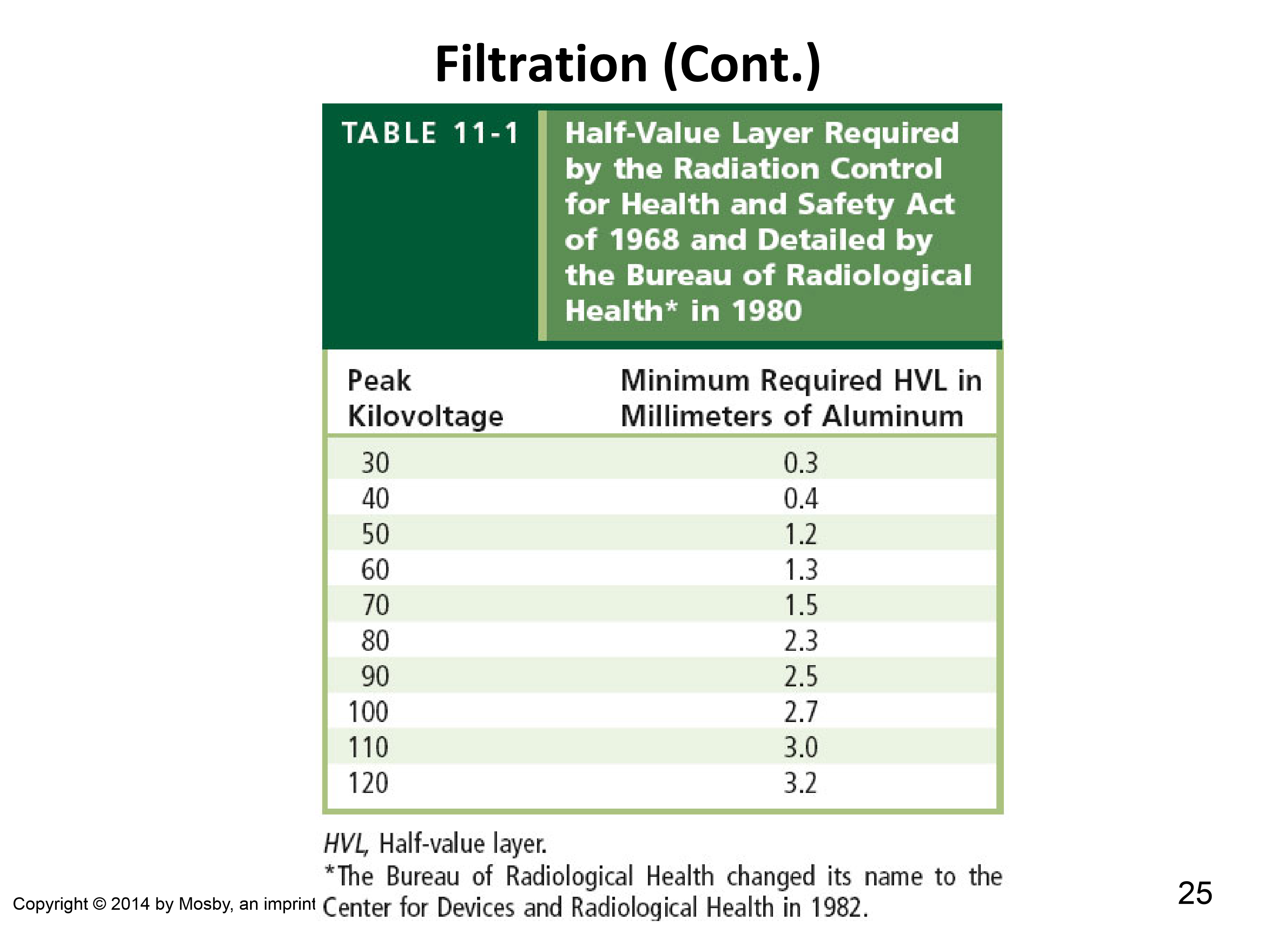
define HVL
the thickness of the designated absorbed (like aluminum) to decrease the intensity of the beam by 50% of its initial value
how is the minimum HVL layer of radiographic machines determined
based of the machines kVp
What are compensating filters?
filters that are used to reduce dose and create a more uniform image of body parts that may have variability in their thickness
allows more radiation to strike thicker areas
what are compensating filters typically made of
aluminum or lead-acrylic
two types of compensating filters
wedge filters
bilateral filters (troughs)
what is exposure reproducibility?
the consistency in output of radiaiton intensity for identical settings from one exposure to the next
what is the acceptable variance of reproducibility in radiography (in %)
5%
what is exposure linearity?
the ratio of the difference in mR/mAs values between successive generatre settings
Essentially saying if we double the mA, the dose should double
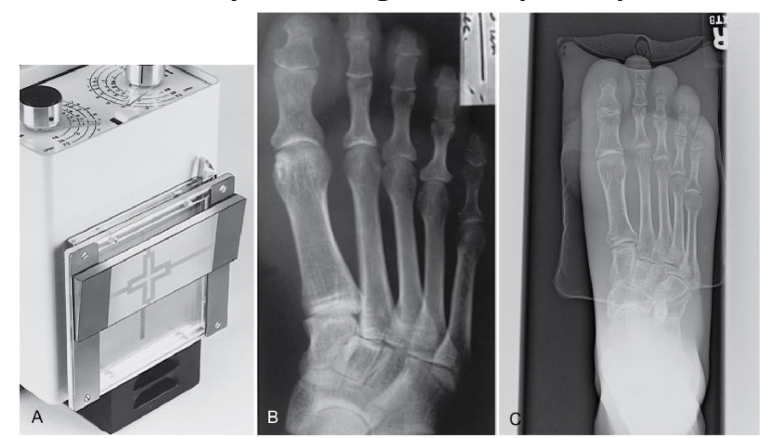
What are screen film combinations
the use of radiographic film and intensifying screens to reduce radiographic exposure time
what are screen film combinations made of?
rare-earth metals: gadolinium, lanthanum, yttrium
what effect does increased kV of machine have on screen speed and patient dose
screen speed increases to reduce patient dose
when the speed of the screen film doubles, radiation exposure is reduced by _____
50% (half)
although higher speed screen films reduce patient dose, what are two cons for using them?
lower resolution
grain/image noise
when may carbon be used as a fron material for screen-film combinations
to prolong the life of the x-ray tube
using carbon forces machine to use lower energy, which also helps reduce patient dose

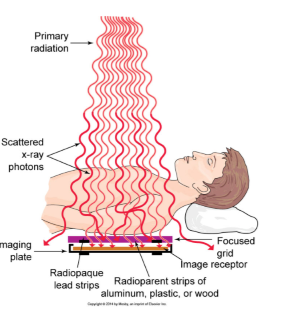
what are anti-scatter grids?
grids of lead/aluminum that placed between the source and the detector restrict the photons from scattering and improve image quality
con of anti-scatter grids
increases patient dose (but improves patient quality)
how can further reduce scatter between grids and detector?
use air gaps
scattered photons will miss detector completly, so they wont contribute to blur
what is the minimum SSD for radiography
30 cm
but 100 cm is typically used
what happens if the SSD is too close
there is more dose that enters the body then what hits the image detector
unnescessary dose
what type of image is conventional radiography
analog image
what is digital imaging?
using computers to process and resolve the image
types of digital imaging
CT, MRI, US, Mammo, Digital radiography
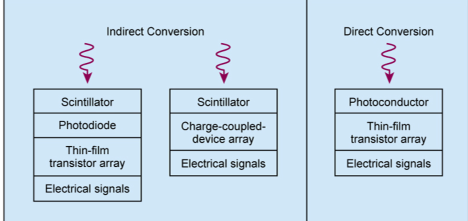
difference between indirect and direct conversion of image
indirect conversion uses scintillators to convert radiation to visble light before creating image
direct conversion detects radiation directly
what effect does digital radiography have on repeat (redo) images?
nearly eliminates the need for retakes since contrast can be manipulated after image acquisition
however mispositioning repeats can still occur
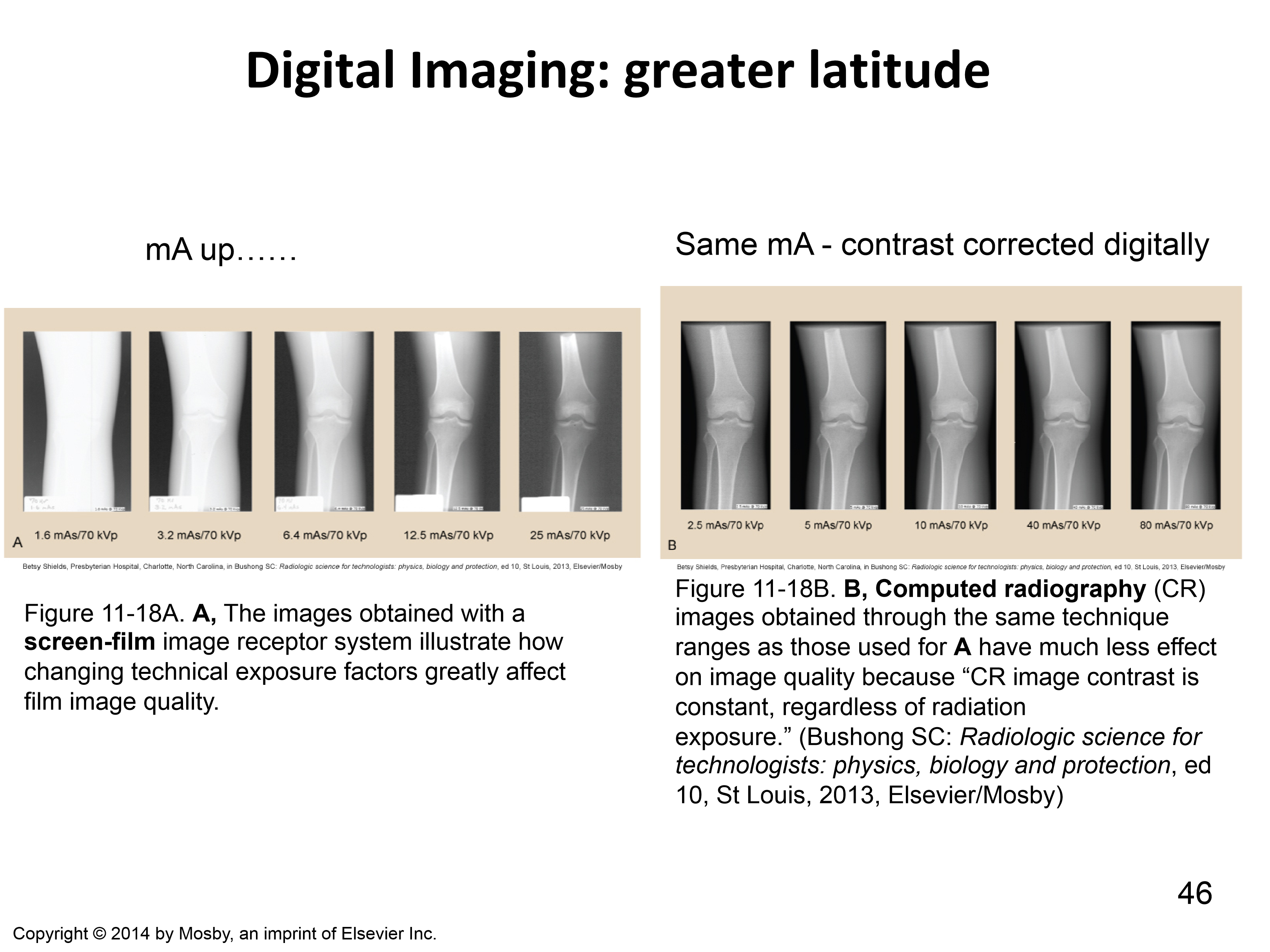
how does digital imaging differ from analong imaging in terms of exposure and contrast
can adjust contrast after photo is taken in digital imaging
what must radiographers still be careful of with digital imaging
Don't overexpose patient even though you can fix image after the fact
Don't want to give maximimal dose
what is dose creep
the gradual increase in patient radiation dose over time due to reliance on digital imaging systems. Since digital detectors can compensate for overexposure without visibly degrading image quality, technologists may unintentionally use higher doses than necessary, leading to unnecessary radiation exposure.
why are anti-scatter grids used more commonly for digital imaging (computer radiography)?
CR is more sensitive to scatter radiation
Which imaging modality has the greatest patient radiation exposure rate in diagnostic radiology?
Fluoroscopy
Why does fluoroscopy result in high radiation exposure?
The X-ray tube stays on for real-time imaging, leading to prolonged exposure.
What are the two risks associated with fluoroscopy, known as the "Fluoro Double Whammy"?
1. Patients receive a high radiation dose.
2. Healthcare workers are exposed due to proximity.
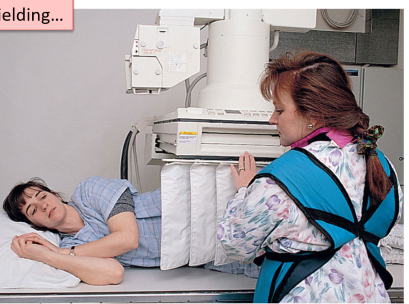
what do fluoroscopic image technologists often wear
shielding
what is the primary function of the image intensifier in fluoroscopy?
increase brightness of image by 10 000 times
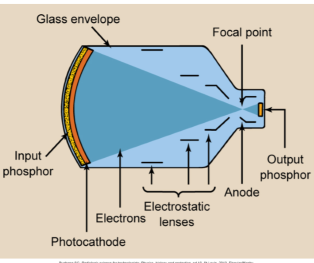
how does an image intensifier work?
X-rays come in and create light on input phosphor causing photoelectric effect, photoelectrons get focused to the anode which then create an image
how does an image intensifer contribute to dose reduction
Allows the use of lower mA, reducing patient radiation exposure.
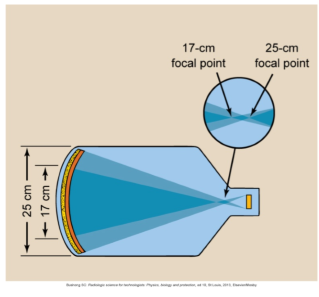
What is the purpose of a multifield (magnification) image intensifier tube?
magnification of image
how does the magnification image intensifer tube affect dose?
requires higher mA, increasing pt dose
what happens to image quality in magnification mode
image quality decreases
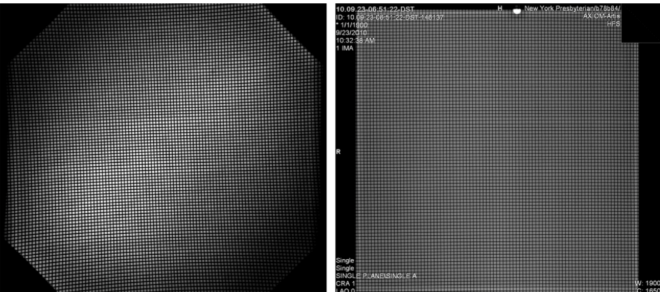
difference between image intensifier and flat panel detectors
Image intensifier has darkened corners,
Flat panel detector is consistent
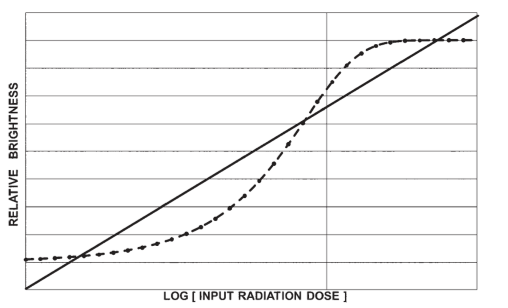
image intensifer vs. flat panel brightness comparison
Can make brightness linear with exposure with FPD
I.I will oversaturate if over or under exposed
Need proper range for decent image
How does intermittent or pulsed fluoroscopy reduce patient dose?
It uses a manual stop-start technique, significantly decreasing exposure, especially in long procedures.
What is the purpose of the last-image-hold feature in fluoroscopy?
It allows viewing of the last captured image without additional radiation exposure.
Why is it important to limit the fluoroscopic field size?
It reduces radiation exposure by focusing only on the organs of interest.
How should the fluoroscopic beam be limited in size?
The beam length and width should not exceed the image receptor, and borders should be visible.
kVp range for fluorscopic procedures
75-110 kVp for adults
decrease by 25% for kids
SSD for fluoroscopic procedures
no less than 38 cm
detector position for fluoroscopic procedures
needs to be as close as is practical to reduce patient’s entrance exposure rate
HVL filtration value for fluoroscopic procedures
3-4.5 mm aluminum
what is cumalative timing device
a beeper that tells you when the beam has been on for more than 5 mins
exposure rate limit for fluoroscopic procedures (in mGy per min)
100 mGy/min
what type of control switch is needed on fluoroscopic equipment
dead man switch (press foot pedal to operate)
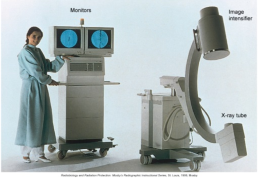
What is a mobile C-arm fluoroscopy unit?
portable X-ray unit with a C-shaped arm, an X-ray tube on one end, and an image intensifier on the other.
what type of procedures are C-arms used for
orthopedic and cardiac procedures
Why does C-arm fluoroscopy pose a radiation risk to patients?
It has the potential to deliver a relatively large radiation dose.
What is the minimum required source-to-end collimator distance for mobile C-arm fluoroscopy?
30 cm
How can patient dose be minimized during C-arm fluoroscopy?
Keep the patient-image intensifier distance as short as possible to reduce entrance dose.
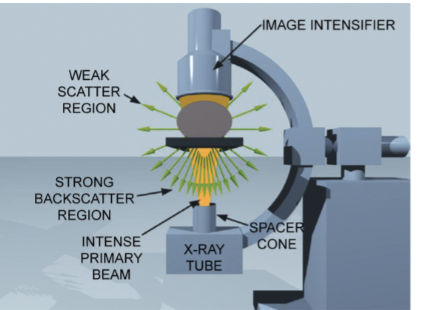
why is the C-arm’s x-ray tube positioned under the patient ?
back scatter radiation is very strong, so kept under the table to shield
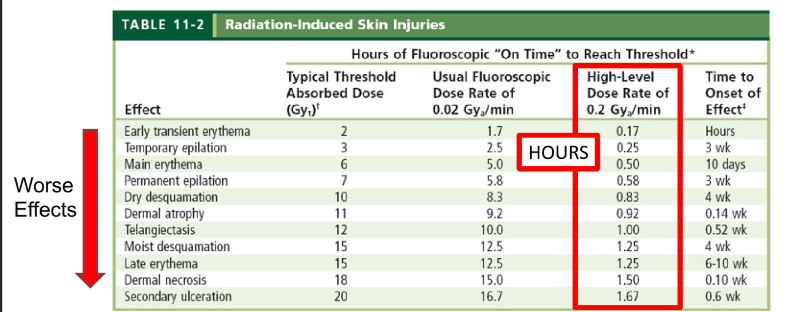
examples of side effects from fluroscopic image procedures
erythema and epilation up to necrosis and ulceration
Why is ongoing education and training important in high-level interventional fluroscopic procedures?
To ensure proper use of fluoroscopic equipment and minimize radiation exposure.
What are the reasons for high radiation exposure during interventional procedures?
Prolonged fluoroscopy times and frequent use during complex procedures.
what is the aim of phantom dosimetery?
to measure or predict the absorbed dose of various tissues of patient undergoing radiotherapy
how is dose predicted using phantoms
deposited dose is assessed by detector in phantom, and then data is used to calulate the dose at a point in a patient
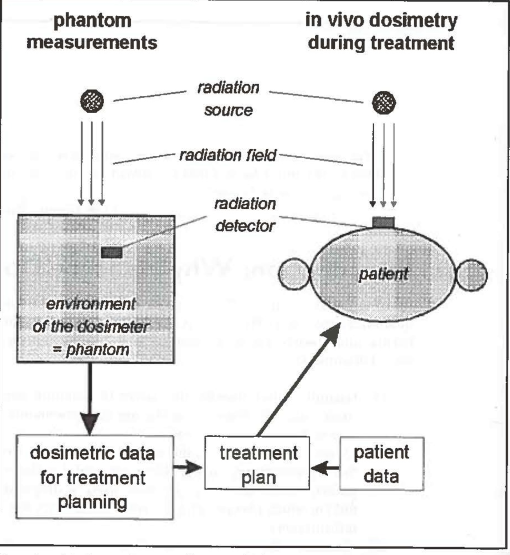
why is dose measured in a phantom
to help with treatment planning
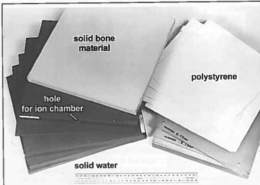
what is a dosimetry phantom?
material and structure that models the absorption and scattering of human tissue
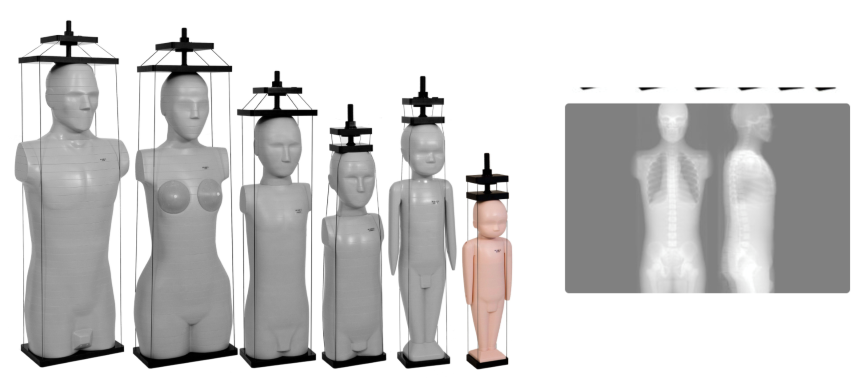
two types of phantoms
geometric (water tanks)
antropomorphic (human shaped)
what are phantoms made of
often water or PMMA plastic which mimics muscles, kidney, liver, brain, and intestines well
what parts of the body are phantoms now great at mimicing
lung and bone
what types of phantoms are used for lung and bone (and for daily QAs)
solid phantoms
what are the two types of ion chamber probes than can be used in geometric phantoms?
chamber arrays (many little chambers)
scanning probes (movable chambers)
what are anthropomorphic phantoms
phantoms that mimic properties of human tissues and contour the patient body similarly