West Chapter 7: Mechanics of Breathing
1/92
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
93 Terms
What is the most important muscle of inspiration?
Diaphragm
What nerves supply the diaphragm?
Supplied by the phrenic nerves from cervical segments 3, 4, and 5
Action of the Diaphragm
When it contracts, the abdominal contents are forced downward and forward and the vertical dimension of the chest cavity is increased
Rib margins are lifted and moved out, causing an increase in the transverse diameter of the thorax
During normal tidal breathing, the level of the diaphragm moves about 1 cm, but on forced inspiration and expiration, a total excursion of up to 10 cm may occur
Paradoxical Movement of the Diaphragm
When one side of the diaphragm is paralyzed and it moves up rather than down with inspiration because the intrathoracic pressure falls
Action of the External Intercostal Muscles
Connect adjacent ribs and slope downward and forward
When they contract, ribs are pulled upward and forward, causing an increase in the lateral and anteroposterior diameters of the thorax
Paralysis of the intercostal muscles alone does not seriously affect breathing at rest because the diaphragm is so effective
What nerves supply the external intercostal muscles?
The intercostal nerves that come off the spinal cord at the same level
What are the muscles of inspiration?
Diaphragm
External intercostal muscles
Scalene muscles
Sternocleidomastoids
Action of the Scalene Muscles
Elevate the first two ribs
Action of the Sternocleidomastoids
Raise the sternum
Is expiration active or passive?
Passive during quiet breathing
Due to elasticity of lung and chest wall, they return to equilibrium positions after being actively expanded during inspiration
Becomes active during exercise and voluntary hyperventilation
What is the most important muscle of expiration?
Those of the abdominal wall
Rectus abdominis, internal and external oblique muscles, and transversus abdominis
Action of the Muscles of the Abdominal Wall
When these contract, intra-abdominal pressure is ra ised and the diaphragm is pushed upward
Also contract forcefully during coughing, vomiting, and defecation
Action of the Internal Intercostal Muscles
Assist active expiration by pulling the ribs downward and inward (opposite action to external intercostal muscles)
Decrease thoracic volume
Stiffen the intercostal spaces to prevent them from bulging outward during straining
Pressure-Volume Curve of the Lung
When the pressure within the jar is reduced below atmospheric pressure, the lung expands
Change in volume can be measured with a spirometer
Pressure held at each level for a few seconds allowing the lung to come to rest
Allows the pressure-volume curve of the lung to be plotted
Expanding pressure around the lung is developed by an increase in volume of the chest cage
Lung volume at any given pressure during deflation is larger than is that during inflation
The lung without any expanding pressure has some air inside of it
Even if the pressure around the lung is raised above atmospheric pressure, little further air is lost because small airways close, trapping gas in the alveoli
Airway closure occurs at higher lung volumes with increasing age and also in some types of lung disease (emphysema)
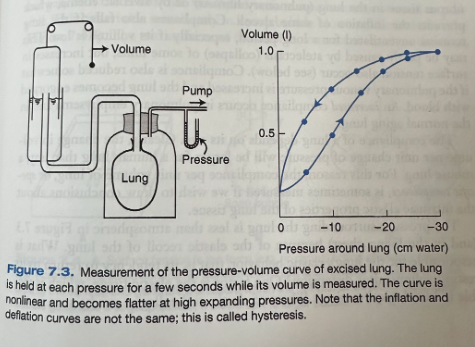
Hysteresis
The curves that the lung follows during inflation and deflation are different
Transpulmonary Pressure
Difference in pressure between the inside and the outside of the lung
Numerically equal to the pressure around the lung when the alveolar pressure is atmospheric
Compliance Equation
Compliance = delta V/delta P
Compliance of the Lung
Slope of the pressure-volume curve, or the volume change per unit pressure change
In the normal range (expanding pressure of about -5 to -10 cm water) the lung is very compliant
At high expanding pressure the lung is stiffer so compliance is smaller
Shown by the flatter slope of the curve
Causes of Reduced Compliance in the Lungs
Increase of fibrous tissue in the lung (pulmonary fibrosis)
Alveolar edema
Prevents the inflation of some alveoli
Falls if the lung remains unventilated for a long period, especially if its volume is low
May be partly caused by atelectasis of some units, but increases in surface tension also occur
Increased pulmonary venous pressure that causes the lung to become engorged with blood
Causes of Increased Compliance in the Lungs
Pulmonary emphysema
Normal aging lung
Change in the Compliance of the Lung Based on Size
Compliance is larger in larger lungs
Specific Complicance
Compliance per unit volume of lung
Elastic Recoil of the Lung
The pressure surrounding the lung is less than atmospheric because of the elastic recoil of the lung
Elasticity of the lung due to elastic tissues
Elastin and collagen present in alveolar walls and around vessels and bronchi
Elastic behavior likely has less to do with simple elongation of these fibers than it does with their geometrical arrangement
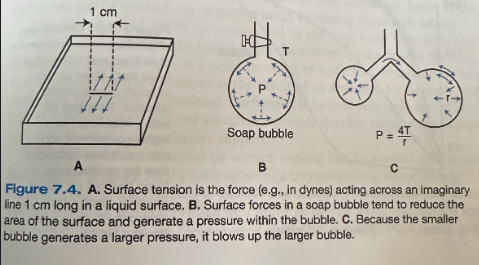
Surface Tension
Force (in dynes) acting across an imaginary line 1 cm long in the surface of the liquid
Arises because the attractive forces between adjacent molecules of the liquid are much stronger than are those between the liquid and gas, with the result that the liquid surface area becomes as small as possible
Pressure of a Soap Bubble
Pressure of a soap bubble can be predicted from Laplace's law: P = 4T/r
P - pressure
T - surface tension
R - radius
When only one surface is involved in a liquid-lined spherical alveolus, the numerator is 2 rather than 4
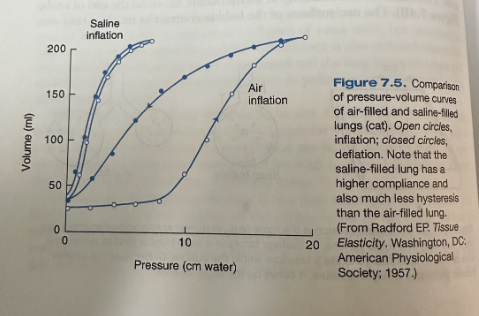
Lungs Inflated with Saline vs Lungs Inflated with Air
Lungs inflated with saline have a much larger compliance than air-filled lungs because the saline abolished the surface tension forces but did not affect the tissue forces of the lung
Surfactant
Some of the cells lining the alveoli secrete surfactant which profoundly lowers the surface tension of the alveolar lining fluid
Phospholipid whose important constituent is dipalmitoyl phosphatidylcholine (DPPC)
DPPC is synthesized in the lung from fatty acids that are either extracted from the blood or synthesized in the lung
Synthesis is fast and there is rapid turnover of surfactant
Formed relatively late in fetal life
What are the two types of alveolar epithelial cells?
Type I
Type II
Type I Alveolar Epithelial Cells
Have the shape of a fried egg with long cytoplasmic extensions spreading out thinly over the alveolar walls
Type II Alveolar Epithelial Cells
More compact with lamellated bodies within them that are extruded into the alveoli and transform into surfactant
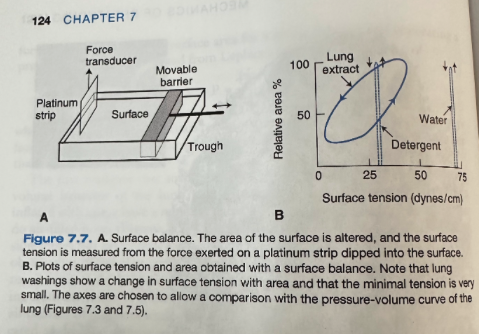
Effects of Surfactant on Surface Tension via a Surface Balance
Consists of a tray containing saline on which a small amount of test material is placed and the area of the surface is then alternately expanded and compressed while the surface tension is measured
Adding detergent reduces the surface tension, but this is independent of area
Adding lung washings yields the curve in 7.7B
Surface tension changes greatly with the surface area and there is hysteresis
Surface tension falls to extremely low values when the area is small
How does surfactant reduce the surface tension so much?
The molecules of DPPC are hydrophobic at one end and hydrophilic at the other and they align themselves in the surface
Their intermolecular repulsive forces oppose the normal attracting forces between the liquid surface molecules that are responsible for surface tension
Reduction in surface tension is greater when the film is compressed because the molecules of DPPC are crowded closer together and repel each other more
What are the physiological advantages of surfactnat?
Low surface tension in alveoli increases the compliance of the lung and reduces the work of expanding it
Stability of the alveoli is promoted
Areas of atelectasis often form in the presence of disease
The pressure generated by a given surface force in a bubble is inversely proportional to its radius so if surface tensions are the same, the pressure inside a small bubble exceeds that in a large bubble
When lung washings are present, a small surface area is associated with a small surface tension so the tendency for small alveoli to empty into large alveoli is reduced
Surfactant also helps keep alveoli dry
Surface tension forces tend to collapse alveoli and also tend to suck fluid out of the capillaries
By reducing surface forces, surfactant prevents the transudation of fluid
Consequences of Loss of Surfactant
Stiff lungs (low compliance)
Areas of atelectasis
Alveoli filled with transudate
These are the pathophysiologic features of neonatal respiratory distress syndrome, occurring in premature infants born without adequate quantities of surfactant
Interdependence
Support offered to lung units by those surrounding them
All the alveoli are surrounded by other alveoli and therefore support each other
With a structure like this, any tendency for one group of units to reduce or increase its volume releative to the rest of the structure is opposed
Why do the lower regions of the lung ventilate more than the upper zones?
Intrapleural pressure is less negative at the bottom than the top of the lung
This is due to the weight of the lung
Pressure near the base is higher than at the apex
The volume of a portion of the lung expands as the pressure around it is decreased
Pressure inside the lung is the same as atmospheric pressure
The lung is easier to inflate at low volumes than high volumes where it becomes stiffer
Because the expanding pressure at the base of the lung is small, this region has a small resting volume, however because it is located on a steep part of the pressure-volume curve, it expands easily on inspiration
The apex of the lung has a big resting volume, is situated on a flatter portion of the pressure-volume curve, has large expanding pressure, and undergoes small changes in volume in inspiration
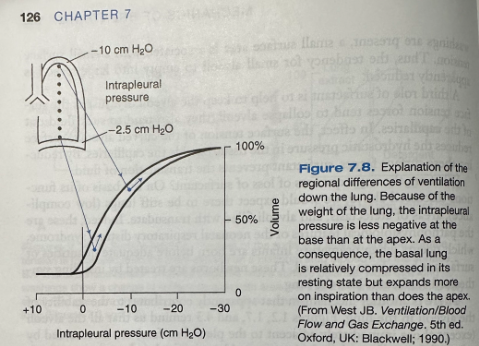
What do regional differences in ventilation refer to?
The change in volume per unit resting volume
The base of the lung has both a larger change in volume and smaller resting volume than the apex so its ventilation is greater
Although the base of the lung is relatively poorly expanded compared to the apex, it is better ventilated
Distribution of Ventilation at Low Lung Volumes
Represents the situation at residual volume (RV), after full expiration
The intrapleural pressures are less negative because the lung is not so well expanded and the elastic recoil forces are smaller
The differences between apex and base are still present because of the weight of the lung
The intrapleural pressure at the base now exceeds airway (atmospheric) pressure so the lung at the base is not being expanded, but rather compressed, and ventilation is impossible until the local intrapleural pressure falls below atmospheric pressure
The apex of the lung is on a favorable part of the pressure-volume curve and ventilates well
At low lung volumes the normal distribution of ventilation is inverted, the upper regions ventilating better than the lower zones
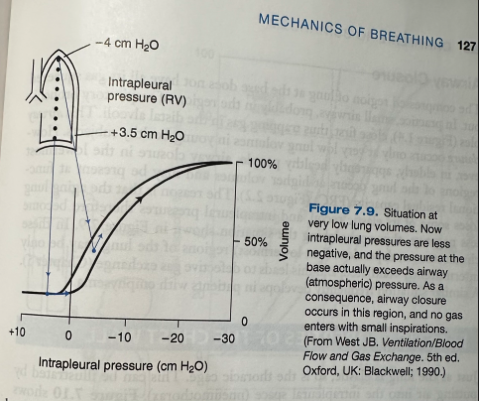
Airway Closure
The compressed region of lung at the base does not have all its gas squeezed out
Small airways, probably in the region of the respiratory bronchioles close first, trapping gas in the distal alveoli
This only occurs at very low lung volumes in young healthy individuals
In elderly, apparently healthy people, airway closure in the lowermost regions of the lung occurs at higher volumes and may be present at functional residual capacity (FRC)
This is because the aging lung loses some of its elastic recoil, and intrapleural pressures therefore become less negative
Dependent regions of the lung may be only intermittently ventilated leading to defective gas exchange
Similar situation occurs with emphysema
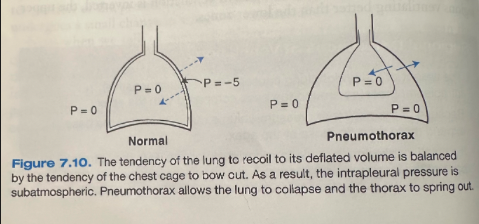
Elastic Properties of the Chest Wall as Illustrated by Pneumothorax
Normally pressure outside the lung is subatmospheric
When air is introduced into the intrapleural space, raising the pressure to atmospheric, the lung collapses inward and the chest wall springs outward
Under equilibrium conditions, the chest wall is pulled inward while the lung is pulled outward
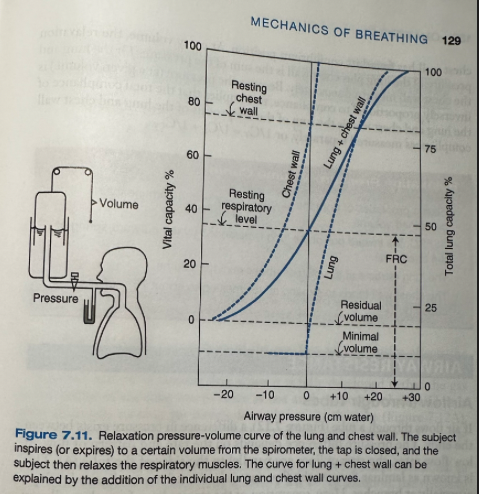
Pressure-Volume Curve for the Lung and Chest Wall
Subject inspires or expires from a spirometer and then relaxes the respiratory muscle while the airway pressure is measured ("relaxation pressure")
At FRC, the relaxation pressure of the lung plus chest wall is atmospheric
FRC is the equilibrium volume when the elastic recoil of the lung is balanced by the normal tendency for the chest wall to spring out
At volumes above this pressure is positive
At volumes below this, pressure is subatmospheric
At zero pressure, the lung is at its minimal volume, which is below RV
Chest wall alone
At FRC, the relaxation pressure is negative so at this volume the chest cage is tending to spring out
It is not until the volume is increased to about 75% of the vital capacity that the relaxation pressure is atmospheric, the chest wall has found its equilibrium position
At every volume, the relaxation pressure of the lung plus chest wall is the sum of the pressures for the lung and the chest wall measured separately
The pressure (at a given volume) is inversely proportional to compliance, this implies that the total compliance of the lung and chest wall is the sum of the reciprocals of the lung and chest wall compliances measured separately
1/CT = 1/CL + 1/CCW
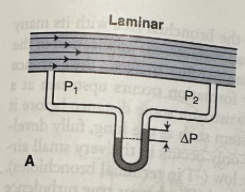
Laminar Flow
At low flow rates, the stream lines are parallel to the sides of the tube
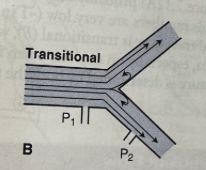
Transitional Flow
As the flow rate is increased, unsteadiness develops, especially at branches and separation of the stream lines from the wall may occur, with the formation of local eddies
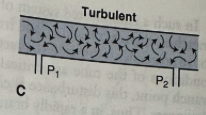
Turbulence
At high flow rates, complete disorganization of the stream lines is seen
Driving Pressure Equation with Laminar Flow
P = KV
Resistance Equation for Laminar FLow
R = 8nl/pi x r4
Radius is important, if the radius is halved, the resistance increases 16 fold
Doubling the length only doubles resistancfe
What characteristics of the gas affect the pressure-flow relationship under laminar flow conditions
The viscosity of the gas, but not its density, affects the pressure-flow relationship under laminar flow conditions
Velocity of the Gas with Laminar Flow
With laminar flow, the gas in the center of the tube moves twice as fast as the average velocity
Pressure Equation for Turbulent Flow
P = KV2
Pressure is not proportional to flow rate but approximately to its square
What characteristics of a gas are important with turbulent flow?
The viscosity of the gas becomes relatively unimportant, but an increase in gas density increases the pressure drop for a given flow
What determines if flow will be laminar or turbulent?
Depends to a large extent on the Reynolds number, Re
Reynolds Number Equation
Re = 2rvd/n
D- density
V - average velocity
R- radius
N - viscosity
Gives the ratio of internal to viscous forces
When is turbulence probable?
In straight, smooth tubes, when the Reynolds number exceeds 2,000
Turbulence is most likely to occur when the velocity of flow is high and the tube diameter is large
Low-density gas such as helium tends to produce less turbulence
What conditions affect the ability for laminar flow to occur?
The entrance conditions of the tube are critical
If eddy formation occurs upstream at a branch point, the disturbance is carried downstream some distance before it disappears
Air Flow Profiles in Throughout the Lung
In a rapidly branching system such as the lung, laminar flow probably only occurs in the very small airways
In most of the bronchial tree, flow is transitional
True turbulence may occur in the trachea, especially on exercise when flow velocities are high
Airway Resistance
The pressure difference between the alveoli and the mouth divided by a flow rate
Airway Pressures During Inspiration
Before inspiration begins, the intrapleural pressure is -5 cmH2O because of the elastic recoil of the lung and alveolar pressure is 0 because with no airflow, there is no pressure along the airways
For inspiratory flow to occur, the alveolar pressure falls, establishing the driving pressure
Extent of the fall depends on the flow rate and resistance of the airways
Intrapleural pressure falls during inspiration for two reasons
As the lung expands, its elastic recoil increases
The reduction in alveolar pressure causes a further fall in intrapleural pressure
Hatched area represents this additional fall in pressure
The vertical distance between lines ABC and AB'C reflects the alveolar pressure at any instant
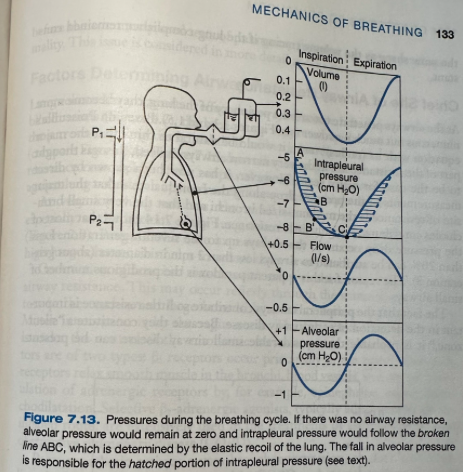
Equation of Airway Pressure
(Mouth-intrapleural) = (mouth-alveolar) + (alveolar-intrapleural)
Airway Pressures During Expiration
Equation of pressure (mouth-intrapleural) = (mouth-alveolar) + (alveolar-intrapleural)
Similar changes occur on expiration
Intrapleural pressure is less negative than it would be in the absence of airways resistance because alveolar pressure is positive
With forced expiration, intrapleural pressure goes above zero
The alveolar pressure tracing will be identical to flow if airway resistances remains constant during the cycle
The intrapleural pressure curve ABC will be the same shape as the volume tracing if the lung compliance remains constant
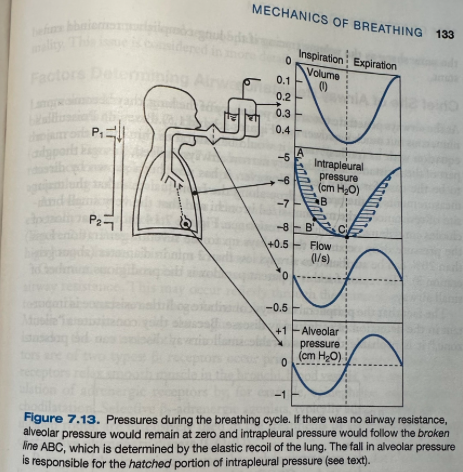
What is the major site of resistance in the airways?
The medium-sized bronchi
The very small bronchioles contribute relatively little resistance
This is due to the large number of small airways
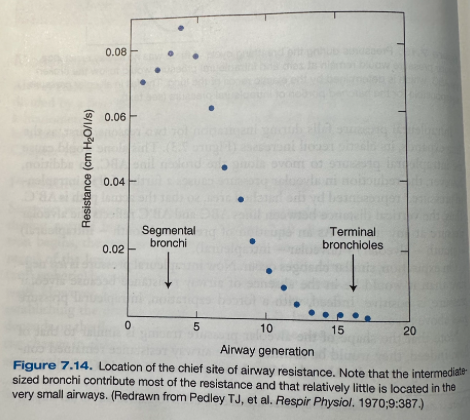
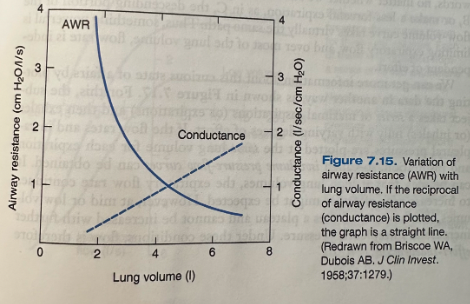
Effect of Lung Volume on Airway Resistance
Like the extra-alveolar blood vessels, the bronchi are supported by the radial traction of the surrounding lung tissue and their caliber is increased as the lung expands
As lung volume is reduced, airway resistance rises rapidly
At veery low lung volumes, the small airways may close completely, particularly at the bottom of the lung where the lung is less well expanded
Patients with increased airway resistance often breathe at high lung volumes, helping to reduce airway resistance
Conductance
The reciprocal of resistance
Linear relationship when plotted against lung volume
What narrows the airways and increases airway resistance?
Contraction of bronchial smooth muscle
May occur reflexively through the stimulation of receptors in the trachea and large bronchi by irritants
What is the motor innervation for bronchial smooth muscle?
Vagus nerve
What controls the tone of the bronchial smooth muscle?
Autonomic nervous system
B-adrenergic receptors
B1 Receptors
Primarily in the heart
B2 Receptors
Relax smooth muscle in the bronchi, blood vessels, and uterus
Stimulation of adrenergic receptors by, for example, epinephrine, causes bronchiodilation
Selective B2 agonists used for the treatment of asthma and COPD
What causes bronchoconstriction?
Parasympathetic activity and acetylcholine
Antimuscarinic agents are used in COPD and occasionally asthma
A fall of PCO2 in alveolar gas causes an increase in airway resistance as the result of direct action on bronchiolar smooth muscle
Injection of histamine into the pulmonary artery causes constriction of smooth muscle in the alveolar ducts
How do density and viscosity of the inspired gas affect the resistance to flow?
Resistance is increased during a deep dive because increased pressure raises gas density
Fact that changes in density rather than viscosity have such an influence on resistance is evidence that flow is not purely laminar in the medium-sized airways which is the main site of resistance
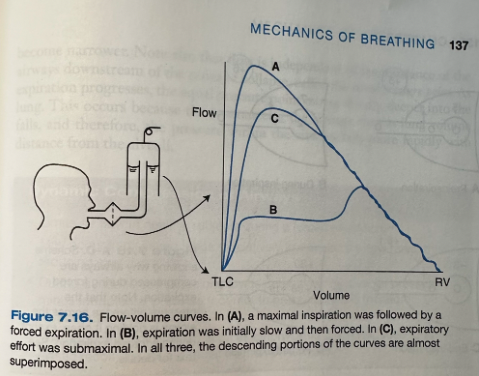
Flow-Volume Curve
Flow rises very rapidly to a high value (peak expiratory flow) but then declines over most of expiration
Whether we start exhaling slowly and then accelerate (B) or make a less forceful expiration ( C ), the descending portion of the flow-volume curve takes virtually the same path
Indicates that something powerful is limiting expiratory flow and over most of the lung volume, flow rate is independent of effort
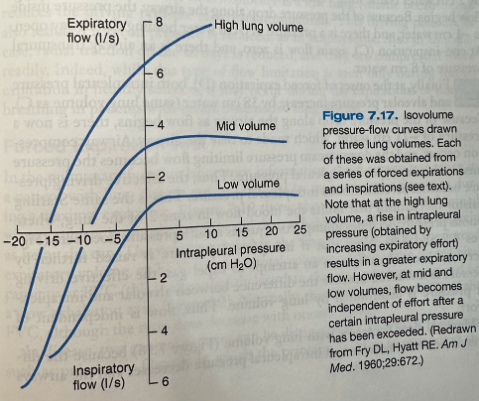
Isovolume Pressure-Flow Curves
At high lung volumes, the expiratory flow rate continues to increase with effort
At mid or low volumes, the flow rate reaches a plateau and cannot be increased with further increase in the intrapleural pressure
Under these conditions, flow is effort-independent
The reason for this behavior is dynamic airway compression (compression of the airways by intrathoracic pressure)
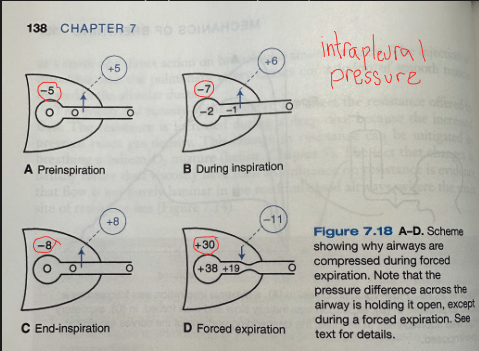
Why are airways compressed during forced expiration?
A - preinspiration
Airway pressure everywhere is zero (no flow)
Because intrapleural pressure is -5 cmH2o, there is a pressure of 5 cmH2O (transmural pressure) holding the airway open
B - during inspiration
As inspiration starts, both intrapleural and alveolar pressure fall by 2 cmH2O and flow begins
Because of the pressure drop along the airway, the pressure inside is -1 cmH2O and there is a pressure of 6 cmH2O holding the airway open
C - end inspiration
Flow is again zero and there is an airway transmural pressure of 8 cm water
D - forced expiration
At the onset of forced expiration, both intrapleural pressure and alveolar pressure increase by 38 cmH2O
Because the pressure drop along the airway as flow begins, there is now a pressure of -11 cm of water which tends to close the airway
Airway compression occurs and the downstream pressure limiting flow becomes the intrapleural pressure so the effective driving pressure becomes alveolar minus intrapleural pressure
If intrapleural pressure is raised further by increased muscular effort in an attempt to expel gas, the effective driving pressure is unaltered because the difference between alveolar and intrapleural pressure is determined by lung volume
Flow is independent of effort
Flow is independent of the resistance of the airways downstream of the point of collapse
Equal pressure point - point of collapse
As expiration progresses, the equal pressure point moves distally, deeper into the lung because the resistance of the airways rises as lung volume falls and therefore the pressure within the airways falls more rapidly with distance from the alveoli
Why does maximal flow decrease with lung volume?
The difference between alveolar and intrapleural pressure decreases and airways become narrower
Factors Exaggerating Flow-Limiting Mechanism
Factors exaggerating flow-limiting mechanism
Any increase in resistance of the peripheral airways
Magnifies the pressure drop along them and thus decreases the intrabronchial pressure during expiration
Low lung volume
Reduces the driving pressure (alveolar-intrapleural)
Reduced recoil pressure (e.g. emphysema)
Reduces driving pressure
This type of flow limitation is seen only during forced expiration in healthy patients, it may occur during the expirations of normal breathing in patients with severe obstructive lung disease
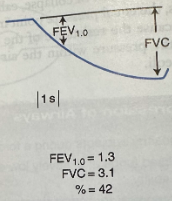
Forced Expiratory Volume (FEV1.0)
Volume exhaled in the first second
Normally about 80% of the FVC
Forced Vital Capacity (FVC)
Total volume exhaled
What are the two general patterns able to be distinguished in respiratory disease?
Restrictive
Obstructive
Restrictive Respiratory Pattern
E.g. pulmonary fibrosis
The primary problem is expanding the respiratory system on inhalation
Both FEV1.0 and FVC are reduced
Characteristically the FEV1.0/FVC% is normal or increased
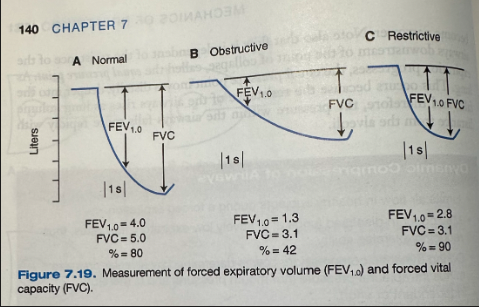
Obstructive Respiratory Pattern
E.g. COPD or bronchial asthma
Primary problem is obstruction to airflow on expiration
The FEV1.0 is reduced much more than is the FVC
FEV1.0/FVC% is low
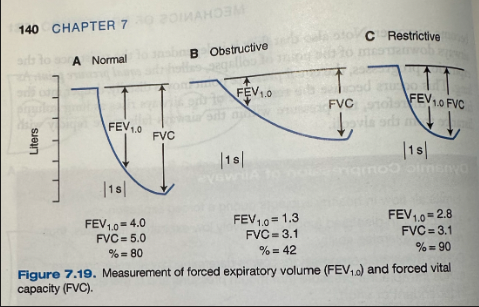
What type of respiratory pattern is this?
Obstructive
What type of respiratory pattern is this?
Restrictive
Forced Expiratory Flow Rate (FEF25-75%)
Average flow rate measured over the middle half of expiration
Generally closely related to the FEV1.0 but is occasionally reduced when FEV1.0 is normal
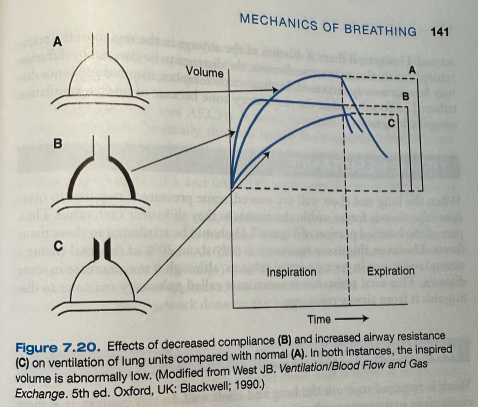
Effect of Alterations in Compliance or Resistance on Ventilation of Lung Units
A - normal distensibility and airway resistance
Volume change on inspiration is large and rapid so that it is complete before expiration for the whole lung begins
B- low compliance
Change in volume is rapid but small
C- large airway resistance
Inspiration is slow and not complete before the lung has begun to exhale
Time Constant
Time constant = compliance x resistance
The shorter the time available for inspiration, the smaller the inspired volume
Said to have a long time constant
Effect of Dilation of the Airways on Diffusion
Dominant mechanism of ventilation of the lung beyond the terminal bronchioles is diffusion
Normally occurs so rapidly that differences in gas concentration in the acinus are abolished within a fraction of a second
If there is dilation of the airways in the region of the respiratory bronchioles, the distance to be covered by diffusion may be greatly increased
The inspired gas is not distributed uniformly within the respiratory zone because of uneven ventilation along the lung units
Tissue Resistance of the Lungs
When the lung and the chest wall are moved, some pressure is required to overcome the viscous forces within the tissues as they slide over each other
This tissue resistance is only ~20% of the total (tissue + airway) resistance in young subjects, may increase in some diseases
Total resistance sometimes called pulmonary resistance to distinguish from airway resistance
Total Resistance in the Lungs
Total resistance = tissue resistance + airway resistance
Work Equation
Work = pressure x volume
Work Done on the Lung
Intrapleural pressure follows curve ABC during inspiration
Work done on the lung is given by the area 0ABC0
The trapezoid 0ABC0 represents the work required to overcome the elastic forces
The hatched area ABCEA represents the work overcoming viscous (airway and tissue) resistance
The higher the airway resistance or the inspiratory flow rate, the more negative (rightward) would be the intrapleural pressure excursion between A and C and the larger the area
The area AECFA is the work required to overcome airway (+tissue) resistance on expiration
Normally falls within the trapezoid 0AECD0
So this work can be accomplished by energy stored in the expanded elastic structures and released during passive expiration
The difference between the areas AECFA and 0AECD0 represents the work dissipated as heat
The higher the breathing rate, the faster the flow rates and the larger the viscous work area ABCEA
The larger the tidal volume, the larger the elastic work area 0AECD0
Patients who have reduced compliance tend to take small rapid breaths, whereas patients with severe airway obstruction sometimes breathe slowly
These patterns tend to reduce the work done on the lungs
Efficiency % Equation
Efficiency % = (Work required to ventilate the lung/Total energy expended (or O2 cost)) x 100
What is % efficiency of breathing?
~5-10%
Cost of Breathing
Cost of quiet breathing is very small, less than 5% of total resting O2 consumption
Possible to increase to 30% with voluntary hyperventilation
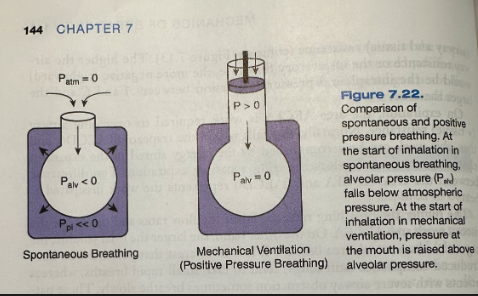
Mechanics of Positive Pressure Ventilation
Spontaneously breathing patients generate a driving pressure by increasing the size of the thorax, thereby lowering airway pressure below atmospheric pressure
With modern mechanical ventilators, driving pressure is primarily established by raising the pressure at the mouth (positive pressure ventilation)