Case 2: Matthew Clarke
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
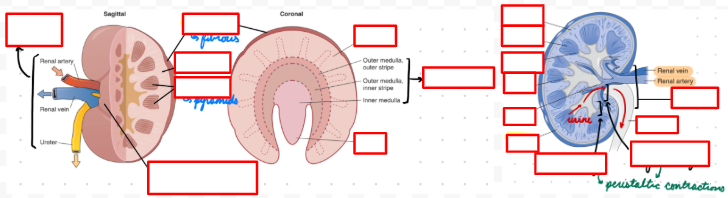
Kidney Anatomy: Cortex
Outer layer
Surround renal medulla
Contain nephrons (corpuscle) and renal tubules (proximal and distal convoluted tubules)
Kidney Anatomy: Medulla
Kidney inner
Contain renal tubules (loop of Henle) and collecting ducts
Connect to minor calyces
Kidney Anatomy: Columns
Renal cortex extensions into medulla
Contain interlobular arteries and veins
Kidney Anatomy: Pyramids
Medullary sections
Formed from renal columns (cortex) projecting into medulla
Kidney Anatomy: Papillae
Renal pyramid apex
Connect to minor calyx
Kidney Anatomy: Nephron
Filtration unit in kidney
Renal corpuscle → Tubules → Collecting ducts → Ureter
Contains renal corpuscle and filtration barrier
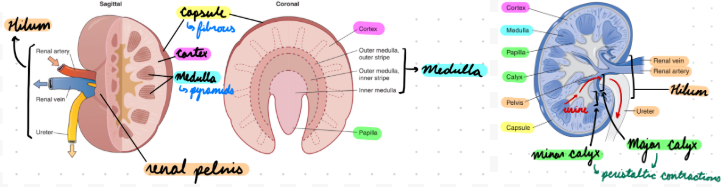
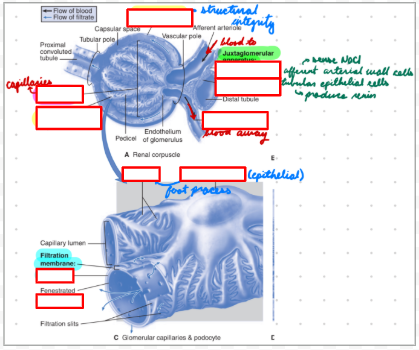
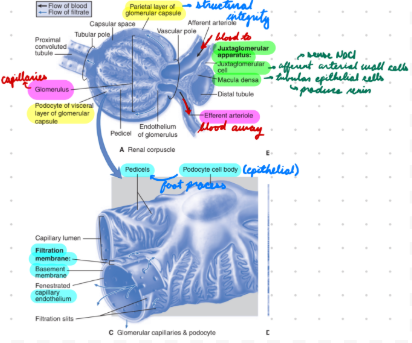
Nephron: Renal Corpuscle
Hollow double-layered epithelial cell sphere (Bowman’s capsule)
Layers:
Parietal: Structural integrity
Visceral: Podocytes
Contain capillaries and arterioles
Capillaries: Glomerulus
Arterioles: Blood transport to and from glomerulus
Afferent: Blood to
Efferent: Blood away
Renal Corpuscle: Bowman’s Space
Empty space between layers in capsule
Renal Corpuscle: Juxtaglomerular (JG) Apparatus
Between distal tubule and arterioles
Cells:
Macula Densa: Tubular epithelial cells
JG: Afferent arterial wall cells
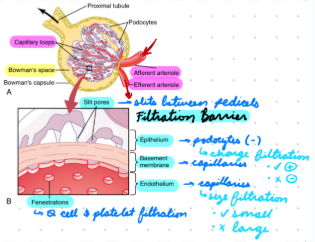
Nephron: Filtration Barrier
Separate plasma (glomerular capillaries) from fluid (Bowman’s space)
3 layers:
Endothelial Cells: Inner layer
Basement Membrane: Middle layer
Podocytes (Epithelial cells): Outer layer
Filtration Barrier: Endothelial Cells
From capillaries
Fenestrae (holes)
Permeable to blood content
Impermeable to cells and platelets
Filtration Barrier: Basement Membrane
From capillaries
Glycoprotein and proteoglycan mesh
Filtration Barrier: Podocytes
Pedicels (foot processes) embed in basement membrane
Slit Diaphragms: Covered in ECM = Bridge slits between pedicels

Kidney Physiology: Cortex
Corpuscle: Filtration
Tubules: Solute and water reabsorption
Kidney Physiology: Medulla
Urine concentration
Tubules + Ducts: Maintain concentration gradients for water/ion reabsorption
Kidney Physiology: Columns
Structural support and blood supply to cortex and medulla
Kidney Physiology: Pyramids
Same as medulla
Kidney Physiology: Papillae
Urine concentration
Conduct urine to calyces
Modify urine osmolality
Kidney Physiology: Nephron
Renal Corpuscle
Filtration Barrier
Nephron: Renal Corpuscle
Filtration through glomerular filtration barrier
Arterioles: Vessel tone maintains glomerular filtration rate (GFR)
Afferent: Vasodilation = Increase filtration
Myogenic response
Efferent: Vasoconstriction = Increase filtration
Tubuloglomerular feedback from macula densa
JG Apparatus: Regulate BP, ECF, and electrolyte balance
Macula Densa Cells: Sense NaCl concentration
JG Cells: Produce renin
Nephron: Filtration Barrier
Selective filtration
By size
Small Particles: Freely cross (ions, glucose, urea, amino acids)
Large Particles: Blocked (albumin, macromolecules)
By charge
Negative: Less filtration
Negative coating on filtration barrier repels negative molecules
Positive: More filtration
Depend on Starling forces
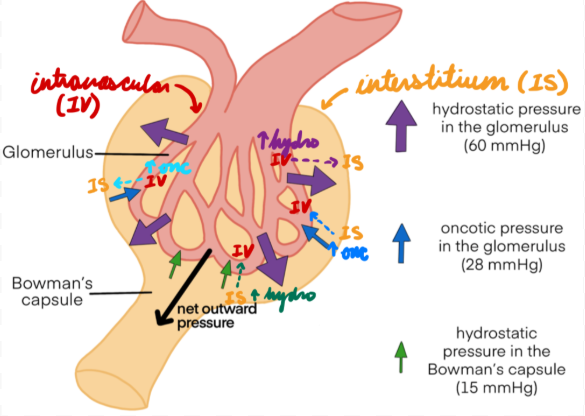
Filtration Barrier: Starling Forces
Regulate fluid movement between intravascular and interstitial (Bowman’s capsule) spaces
Hydrostatic Pressure: Pressure pushing fluid out
High intravascular fluid volume (pressure) = Fluid from vessels → Bowman’s capsule
High Bowman’s capsule volume (pressure) = Fluid from Bowman’s capsule → Vessels
Oncotic Pressure: Pressure drawing fluid in
High intravascular solutes (low fluid volume/pressure) = Fluid from Bowman’s capsule → Vessels
High Bowman’s capsule solutes (low fluid volume/pressure) = Fluid from vessels → Bowman’s capsule
Nephrotic Syndrome
Signs and symptoms indicating damage to the glomerular filtration barrier
Usually…
Proteinuria > 3.5 g/day
Hypoalbunimeia
Edema
Nephritic Syndrome
Signs and symptoms indicating glomerular inflammation
Glomerular hematuria
Proteinuria < 3.5 g/day
Hypertension
Nephrotic Syndrome: Epidemiology
Glomerular disorders
Systemic diseases
Toxic exposure
Nephrotic Syndrome: Etiology
Primary/Idiopathic: Common
Minimal change disease: Flat podocytes
After viral infection
In children
Focal segmental glomerulosclerosis: Lost foot processes on podocytes
Glomerular lesions
Membranous nephropathy: Retracted podocytes
Thick glomerular capillaries
Secondary:
Diabetes
Amyloidosis
Lupus
Infection (Hep B and C, malaria)
Medications (NSAIDs)
Malignancies
Nephrotic Syndrome: Pathogenesis
Damaged glomerular filtration barrier causing proteinuria/hypoalbuminemia and edema
Nephrotic Syndrome: Proteinuria/Hypoalbuminemia
≥1 filtration barrier layers damaged = Albumin/proteins pass into from blood vessels into urine (filtrate)
Barrier Damage:
Podocytes: Loss of - charge = Increased albumin filtration (- charge)
Basement Membrane: Macromolecule filtration = Increased protein filtration (non-selective)
Results:
High protein in urine
Low protein in blood
Albumin, antithrombin III, vit D binding protein
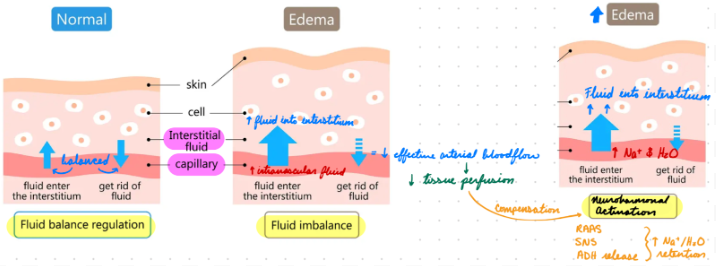
Nephrotic Syndrome: Edema
Net fluid filtration from plasma into interstitium
Underfill Hypothesis: Intravascular volume depletion
Decreased plasma albumin concentration = Low oncotic pressure
Fluid from intravascular space → Interstitial space = Hypervolemia
*Overfill Hypothesis: Intravascular volume expansion
Renal Na+ retention from epithelial Na+ channel activation = Increase intravascular water reabsorption = High hydrostatic pressure
Fluid from intravascular space → Interstitial space = Hypervolemia
Nephrotic Syndrome: Clinical Presentation
Edema + weight gain → Position/Gravity-dependent
Peripheral (lower limbs, presacral area)
Periorbital
Pleural effusion
Pericardial effusion
Acites
Fatigue
SOB
Hypoalbuminemia
Proteinuria
Frothy urine
Hyperlipidemia
Nephrotic Syndrome: Investigations
Urine dipstick
Urinalysis
Urine sediment microscopy
Blood test
BP
Biopsy
Nephrotic Syndrome: Urine Dipstick
≥ 3+ proteins
Hematuria
Not always in nephrotic
Usually in nephritic (inflammation)
Nephrotic Syndrome: Urinalysis
Protein excretion > 3.5 g/day
Urine protein:creatinine ratio > 3.5 g/g
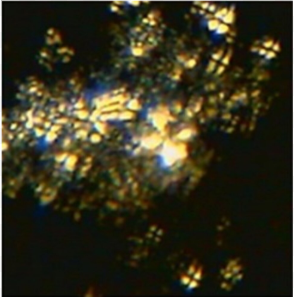
Nephrotic Syndrome: Urine Sediment Microscopy
Nephrotic sediments
Lipiduria: Fatty casts + Maltese cross under polarized light
Hematuria
Nephrotic Syndrome: Blood Test
Low serum protein
Low coagulation factors
Hyperlipidemia
Nephrotic Syndrome: BP
If high
Usually nephritic
Prescribe diuretics
Nephrotic Syndrome: Biopsy
Determine cause for adults
NOT usually for children
Nephrotic Syndrome: Treatment/Management
Steroids
Diet changes**
Diuretics
RAAS inhibitors
Statins
Nephrotic Syndrome Treatment: Steroids
Idiopathic: Inhibit autoimmune reaction attacking podocytes
Nephrotic Syndrome Treatment: Diet Changes
Decrease Na+, fluids, and protein
Benefits:
Control edema, BP, and proteinuria
Prevent metabolic complications (hyperlipidemia)
Risks:
Malnutrition (low protein, hyponatremia)
Nephrotic Syndrome Treatment: Diuretics
First-Line: Oral loop diuretic
Second-Line: + oral thiazide diuretic, IV loop diuretic
Consider: + IV albumin
Loop Diuretics MOA
Inhibit Na+/K+/2Cl- cotransporter in thick ascending loop of Henle = Decrease Na+ and Cl- reabsorption = Increase water excretion
Ex: Furosemide
Thiazide Diuretics MOA
Inhibit Na+/Cl- cotransporters in distal convoluted tubule = Increase Na+ and Cl- excretion = Increase water excretion
Diuretics: Benefits and Risks
Benefits: Decrease edema (pulmonary, skin breakdown from peripheral)
Risks: Hypovolemia, AKI, electrolyte disturbances (hypokalemia, hypernatremia)
Nephrotic Syndrome Treatment: RAAS Inhibitors
Ex: ACE inhibitor (ramipril), ARB (losartan)
Decrease proteinuria and hypertension
Slow renal disease
NOT for patients with AKI, hyperkalemia, or sudden nephrotic syndrome
Nephrotic Syndrome Treatment: Statins
Decrease lipids
Nephrotic Syndrome: Complications
Thrombotic events (antithrombin loss)
Thromboembolism
Renal vein thrombosis
Chronic kidney disease
Atherosclerotic complications
Vit D deficiency
From vit D binding protein loss in urine
Anemia
Urinary loss of iron, erythropoietin, and transferrin
Nephrotic Syndrome: Prognosis
90-95% remission
Children and adults
Fluid Retention: Physical Findings
Weight gain
Ascites
Pulmonary edema (SOB, orthopnea)
Congestive HF
Fluid Retention with Contracted Circulation
Increased intravascular fluid → Interstitial space (misdistribution) = Decreased effective arterial blood volume = Low tissue perfusion
From:
Low CO (CHF)
Arterial vasodilation
Low oncotic pressure
Protein loss (kidney disease)
Low protein synthesis (liver disease)
Compensatory neurohormonal activation = Increase Na+ and water retention = Worsen edema
RAAS
SNS (epinephrine/norepinephrine)
ADH release (vasopressin)

Prerenal Conditions
Conditions leading to decreased renal perfusion (hypoperfusion) without intrinsic damage
Hypovolemia
Hypotension
Decreased effective arterial volume
Renal artery stenosis
Drugs affecting glomerular perfusion
Prerenal Conditions: Kidney Response
Reabsorb Na+ and water = Increase intravascular fluid = Increase perfusion
Prerenal Conditions: Blood Abnormalities
Increased blood urea nitrogen (BUN)/creatinine ratio
Hypoperfusion → Increased proximal tubular urea reabsorption
Increased serum creatinine
From impaired filtration → Low GFR
Normal: 62-106 umol/L
Hemoconcentration: High RBC concentration
Blood volume loss = Increase solute (RBC) concentration
Prerenal Conditions: Urine Abnormalities
Low Na+
Hypoperfusion → Increased tubular Na+ reabsorption
High osmolality and specific gravity
Density of solutes in fluid (compared to water)
Osmolality: more precise
Specific Gravity:
< 1.010: Dilute
> 1.020: Concentrated
Increased water reabsorption = High urine concentration