1 - OTHER BODY FLUIDS
1/237
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
238 Terms
CSF
is routinely collected by lumbar puncture between the third, fourth, or fifth lumbar vertebrae
three
CSF
Specimens are collected in _ sterile tubes, which are labeled 1, 2, and 3 in the order in which they are withdrawn
Tube 1
CSF
used for chemical and serologic tests
Tube 2
CSF
usually designated for the microbiology laboratory
Tube 3
CSF
used for the cell count
fourth tube
CSF
A _ _ may be drawn for the microbiology laboratory to provide better exclusion of skin contamination or for additional serologic tests
Supernatant fluid
CSF
_ _ that is left over after each section has performed its tests may also be used for additional chemical or serologic tests
Excess fluid
CSF
_ _ should not be discarded and should be frozen until there is no further use for it
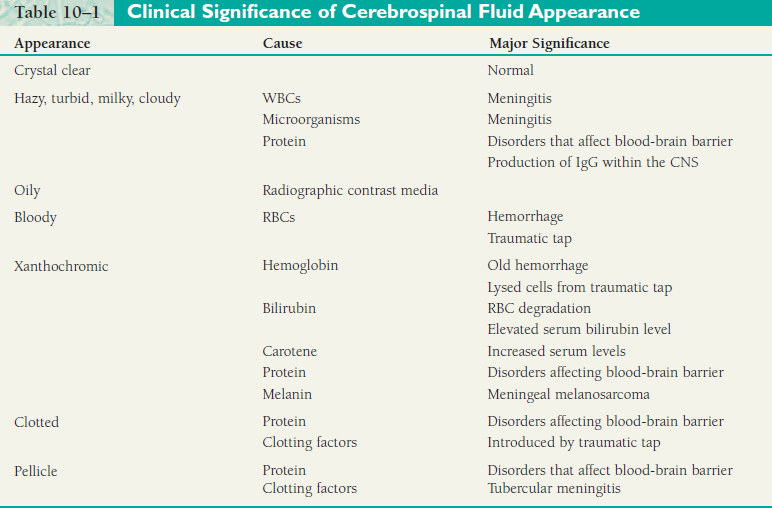
crystal clear, cloudy or turbid, milky, xanthochromic, and hemolyzed/bloody
CSF
appearance includes (5)
Xanthochromia
CSF
_ is a term used to describe CSF supernatant that is pink, orange, or yellow
oxyhemoglobin
hemolysis
unconjugated bilirubin
CSF
Due to the presence of RBC degradation products, the color will vary from pink (very slight amount of _) to orange (heavy _) to yellow (conversion of oxyhemoglobin to _ _).
CSF
leukocyte (WBC) count
CSF
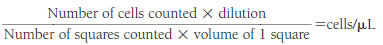
Cell Count
The cell count that is routinely performed on CSF specimens is the _ _
RBC counts
CSF
Cell Count
_ _ are usually determined only when a traumatic tap has occurred and a correction for leukocytes or protein is desired
total cell count
WBC count
CSF
Cell Count
The RBC count can be calculated by performing a _ _ _ and a _ _ and subtracting the WBC count from the total count, if necessary
0 to 5
30
CSF
Cell Count
Normal adult CSF contains _-_ WBCs/L. The number is higher in children, and as many as _ mononuclear cells/L can be considered normal in newborns
200
400
CSF
Cell Count
Specimens that contain up to _ WBCs or _ RBCs/l may appear clear, so it is necessary to examine all specimens microscopically
Clear
CSF
Total Cell Count
_ specimens may be counted undiluted, provided no overlapping of cells is seen during the microscopic examination
normal saline
CSF
Total Cell Count
Dilutions for total cell counts are made with _ _, mixed by inversion, and loaded into the hemocytometer with a Pasteur pipette
four corner
center
CSF
Total Cell Count
Cells are counted in the _ _ squares and the _ square on both sides of the hemocytometer
CSF
Total Cell Count
Formula
Undiluted
CSF
CSF Dilution
Clear
1:10
CSF
CSF Dilution
Slightly hazy
1:20
CSF
CSF Dilution
Hazy
1:100
CSF
CSF Dilution
Slightly cloudy
1:200
CSF
CSF Dilution
Cloudy/Slightly bloody
1:10,000
CSF
CSF Dilution
Bloody/Turbid
Lysis
CSF
WBC Count
_ of RBCs must be obtained prior to performing the WBC count on either diluted or undiluted specimens
methylene blue
CSF
WBC Count
Addition of _ _ to the diluting fluid stains the WBCs, providing better differentiation between neutrophils and mononuclear cells
four
3% glacial acetic acid
1
CSF
WBC Count
To prepare a clear specimen that does not require dilution for counting, place _ drops of mixed specimen in a clean tube. Rinse a Pasteur pipette with _% _ _ _, draining thoroughly, and draw the four drops of CSF into the rinsed pipette. Allow the pipette to sit for _ minute, mix the solution in the pipette, discard the first drop, and load the hemocytometer
dilution factor
CSF
WBC Count
As in the total cell count, WBCs are counted in the four corner squares, and the center square on both sides of the hemocytometer and the number is multiplied by the _ _ to obtain the number of WBCs per microliter
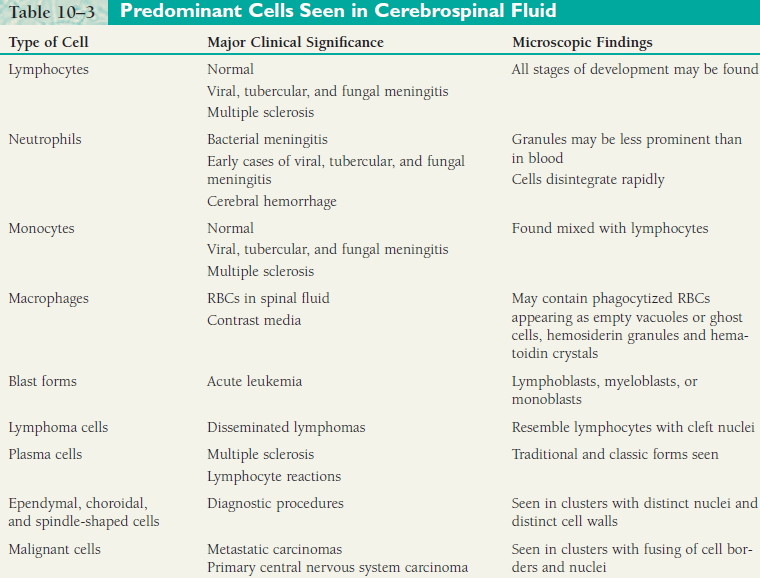
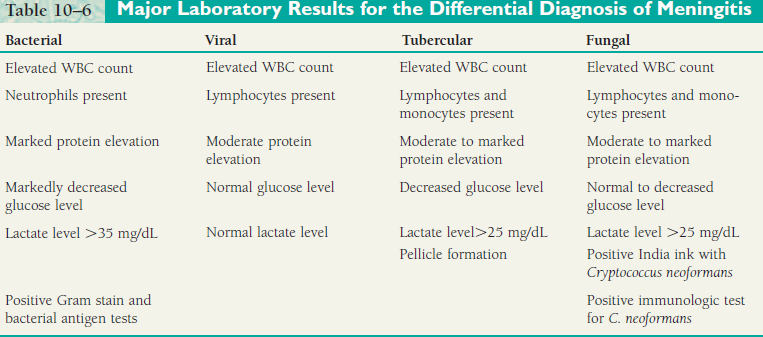
Lymphocytes
CSF
Predominant Cells Seen in Cerebrospinal Fluid
Major Clinical Significance: Normal, viral, tubercular, and fungal meningitis, multiple sclerosis
Microscopic Findings: All stages of development may be found
Neutrophils
CSF
Predominant Cells Seen in Cerebrospinal Fluid
Major Clinical Significance: Bacterial meningitis, early cases of viral, tubercular, and fungal meningitis, cerebral hemorrhage
Microscopic Findings: Granules may be less prominent than in blood, cells disintegrate rapidly
15 to 45
CSF
Cerebrospinal Protein
Normal CSF contains a very small amount of protein. Normal values for total CSF protein are usually listed as _-_ mg/dL, but are somewhat method dependent
elevated
CSF
Cerebrospinal Protein
The causes of _ CSF protein include damage to the blood-brain barrier, production of immunoglobulins within the CNS, decreased clearance of normal protein from the fluid, and degeneration of neural tissue
Meningitis
hemorrhage
CSF
Cerebrospinal Protein
_ and _ conditions that damage the blood-brain barrier are the most common causes of elevated CSF protein
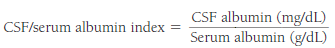
CSF
Cerebrospinal Protein
CSF serum albumin index formula
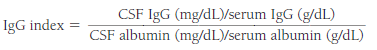
CSF
Cerebrospinal Protein
IgG index formula
60, 70
65
CSF
Cerebrospinal Fluid Glucose
Glucose enters the CSF by selective transport across the bloodbrain barrier, which results in a normal value that is approximately _% to _% that of the plasma glucose. If the plasma glucose is 100 mg/dL, then a normal CSF glucose would be approximately _ mg/dL
2
CSF
Cerebrospinal Fluid Glucose
The blood glucose should be drawn about _ hours prior to the spinal tap to allow time for equilibration between the blood and fluid. CSF glucose is analyzed using the same procedures employed for blood glucose
plasma
CSF
Cerebrospinal Fluid Glucose
Elevated CSF glucose values are always a result of _ elevations
bacterial meningitis
CSF
Cerebrospinal Fluid Glucose
The finding of a markedly decreased CSF glucose accompanied by an increased WBC count and a large percentage of neutrophils is indicative of _ _
tubercular meningitis
CSF
Cerebrospinal Fluid Glucose
If the WBCs are lymphocytes instead of neutrophils, _ _ is suspected
viral meningitis
CSF
Cerebrospinal Fluid Glucose
Likewise, if a normal CSF glucose value is found with an increased number of lymphocytes, the diagnosis would favor _ _
meningitis
CSF
Cerebrospinal Fluid Lactate
The determination of CSF lactate levels can be a valuable aid in the diagnosis and management of _ cases
25
CSF
Cerebrospinal Fluid Lactate
In bacterial, tubercular, and fungal meningitis, the elevation of CSF lactate to levels greater than _ mg/dL occurs much more consistently than does the depression of glucose and provides more reliable information when the initial diagnosis is difficult
bacterial meningitis
viral meningitis
CSF
Cerebrospinal Fluid Lactate
Levels greater than 35 mg/dL are frequently seen with _ _, whereas in _ _, lactate levels remain lower than 25 mg/dL
hypoxia
CSF
Cerebrospinal Fluid Lactate
Destruction of tissue within the CNS owing to oxygen deprivation (_) causes the production of increased CSF lactic acid levels
8 to 18
CSF
Cerebrospinal Fluid Glutamine
The normal concentration of glutamine in the CSF is _-_ mg/dL.
liver disorders
CSF
Cerebrospinal Fluid Glutamine
Elevated levels are found in association with _ _ that result in increased blood and CSF ammonia
Gram Stain
AFB
India Ink
Culture
CSF
Microbiology Tests
(4)
VDRL
FTA-ABS
Latex agglutination and enzyme-linked immunosorbent assay (ELISA) methods
Test kits are available to detect Streptococcus group B, H. influenzae type b, S. pneumoniae, N. meningitidis A, B, C, Y, W135, and E. coli K1 antigens.
BACTIGEN Test
CSF
Serologic Testing
(5)
Synovium
Synovial Fluid
refers to the tissue lining synovial tendon sheaths, bursae, and diarthrodial joints except for the articular surface
1-3
Synovial Fluid
Synovium
Compose of _-_ cell layers that form a discontinuous surface overlying fatty, fibrous, or periosteal joint tissue
Synovial Fluid
Synovial Fluid
Synovium
an imperfect ultrafiltrate of plasma combined with hyaluronic acid produced by the synovial cells
plasma
Synovial Fluid
Synovium
Small ions and molecules like glucose and urea cross easily into the joint space and are therefore similar in concentration to _, but large molecules are absent or present only in trace amounts
Synovial fluid
Synovial Fluid
Synovium
_ _ acts as a lubricant and adhesive and provides nutrients for the avascular articular cartilage
Arthrocentesis
Synovial Fluid
Specimen Collection
indicated in a patient with an undiagnosed effusion or a clinical change related to a known effusion
Effusion
Synovial Fluid
Specimen Collection
escape of fluid into a part; exudation, transudation
bacteremia
Synovial Fluid
Specimen Collection
caution is necessary to avoid aspirating a sterile joint in someone with _ or aspirating through a cutaneous or peroarticular soft tissue infection into a sterile joint
4
Synovial Fluid
Specimen Collection
Even large joints like the knee normally contain no more than _ mL of synovia, so a small sample size is common unless an effusion is present
plastic syringes
Synovial Fluid
Specimen Collection
Sterile, disposable needles are used; _ _ are used to avoid contamination by birefringent particulates
25
Synovial Fluid
Specimen Collection
Syringe may be heparinized by _ units of sodium heparin per millilitre of SF in routine arthrocentesis
Oxalate, powdered EDTA, and lithium heparin
Synovial Fluid
Specimen Collection
(3) should be avoided because they form crystal artifacts that may be misleading during examination
5-10
Synovial Fluid
Specimen Collection
_-_ ML placed in a sterile heparinized tube or syringe for microbiologic studies
2-5
Synovial Fluid
Specimen Collection
_-_ ML is placed in an anticoagulant tube (sodium heparin of liquid EDTA) for microscopic examination
5
Synovial Fluid
Specimen Collection
_ ML is put into a plain, “red top” tube and allowed to clot (normal SF does not clot)
125
1 or 2
Synovial Fluid
Specimen Collection
Concentrations of heparin greater than _ U/mL have an inhibitory effect on some pathogenic bacteria; specimens for culture should therefore be at least _ or _ mL in volume if they are submitted in “green top” heparin tubes
infectious arthritis
synovial fluid crystals
Synovial Fluid
Recommended Tests
Diagnosis of _ _ and _ _ _ is the most compelling reason for SF analysis
Diagnosis
Synovial Fluid
Recommended Tests
It is vital that they be performed well because they can provide highly specific diagnostic information
bedside
Synovial Fluid
Recommended Tests
Total volume should be recorded at the _, especially if the sample is to be divided for submission to different laboratory sections
Color
Synovial Fluid
Recommended Tests
_ is evaluated in a clear glass tube against a white background
colorless
pale yellow
Synovial Fluid
Recommended Tests
Normal SF is _ to _ _ owing to diapedesis of a few RBCs associated with even mild trauma
Diapedesis
Synovial Fluid
Recommended Tests
_ - the passage of blood cells through capillary walls into the tissues—called also emigration
xanthochromia
Synovial Fluid
Gross Examination
Non-inflammatory and inflammatory disorders are usually straw to yellow in color (_)
Septic fluid
Synovial Fluid
Gross Examination
_ _ may be yellow, brown, or green depending on the chromogen produced by the offending organism and the host response, including the WBCs and RBCs
Traumatic Tap
Synovial Fluid
Gross Examination
produces an uneven distribution of blood during arthrocentesis or streaking in the syringe
Red-Brown
Synovial Fluid
Gross Examination
color following centrifugation is good evidence of pathologic hemarthrosis
Clarity
Synovial Fluid
Gross Examination
relates to the number and type of particles within the synovia
transparent
Synovial Fluid
Gross Examination
Normal SF is _; newsprint is easily read through tube
leukocytes
Synovial Fluid
Gross Examination
_ are most commonly responsible for changes in clarity, but massive numbers of crystals may produce an opaque, milky-opalescent fluid without white cells
cholesterol crystals
Synovial Fluid
Gross Examination
A shimmering, oily-appearing specimen suggests an abundance of _ _ which may look like pus
fibrin
Synovial Fluid
Gross Examination
Increased turbidity is less often due to concentrations of _, free-floating “rice bodies” (fragments of degenerating proliferative synovial cells)
ground pepper
Synovial Fluid
Gross Examination
A “_ _” appearance resulting from pigmented cartilage is a sign of ochronosis; hardening of tendons & ligaments can predispose them to rupture. Colour changes in the joints can be observed clinically
Total Cell Count
Synovial Fluid
Microscopic Examination
should be promptly performed to avoid degenerative cell loss, which begins as soon as one hour following arthrocentesis
inverted
haemocytometer
Synovial Fluid
Microscopic Examination
Total Cell Count
Tubes must be _ before sampling to ensure uniform mixing; Counts are performed in standard _
0-2
1300
Synovial Fluid
Microscopic Examination
Total Cell Count
A wet-prep slide count of _-_ leukocytes/hpf (average 10 fields/hpf) predicts less than _ WBCs by cell count
50,000
Synovial Fluid
Microscopic Examination
Total Cell Count
Leukocytes counts over _/uL require dilution which should be done with saline not acetic acid, to avoid mucin clot formation and cell clumping
hyaluronidase
Synovial Fluid
Microscopic Examination
Total Cell Count
Highly viscous should be incubated with _ before it is counted
hyaluronan
Synovial Fluid
Microscopic Examination
Total Cell Count
hyaluronidase lowers the viscosity of _, thereby increasing tissue permeability
0.3 N saline
0.1 N HCl
1% saponin in saline
Synovial Fluid
Microscopic Examination
Total Cell Count
RBCs should be counted unless it is obvious traumatic tap; if in large number, lyse first with the use of _ _, _ _, or _ _ in _
150-200/uL
Synovial Fluid
Microscopic Examination
Total Cell Count
upper limit of normal SF for leukocytes in clinical specimens
Cytospin preparations
Synovial Fluid
Microscopic Examination
Differential Count
_ _ are preferred over smears of centrifuged SF because they have better cell morphology; treatment with hyaluronidase may be necessary to produce thin smears in viscous specimens
Neutrophils
Synovial Fluid
Microscopic Examination
Differential Count
normally account for about 20% of SF leukocytes. SF from patients with urate gout or RA may also have high percentages
pyknosis
karyorrhexis
Synovial Fluid
Microscopic Examination
Differential Count
Neutrophils frequently exhibits _ and _ and may contain bacteria, crystals, lipid droplets, vacuoles or dark blue inclusions (ragocytes, RA cells)
Lymphocytes
Synovial Fluid
Microscopic Examination
Differential Count
15% of the differential, prominent in early RA, chronic infections and collagen disorders. Reactive forms, including immunoblasts may be seen
Monocytes and macrophages
Synovial Fluid
Microscopic Examination
Differential Count
accounts for approximately 65% of the normal cell count. Monocytosis may be self-limited in patients with viral arthritis or serum sickness or more chronic in those with SLE
Eosinophilia
Synovial Fluid
Microscopic Examination
Differential Count
defined over 2% of the leukocyte count; reported in RA, RF, metastatic carcinoma. Lyme disease, parasitic infections, chronic urticarial, angioedema, and following arthrography and irradiation