CSDI 4100 Final Exam
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
How many different types of waves are there? What are they?
3; Longitudinal, Sine, and Transverse.
What is a longitudinal wave?
Waves move the medium parallel to the direction in which the waves travel. For example, wheat blowing in the wind, SOUND WAVE.
What is a sine wave?
Graphic representation of sound waves, which are not visible. One cycle of vibration or oscillation begins at any point on a wave and ends at the same point on the next wave. If a sine wave occurred without any other vibrations or tones imposed upon it, it is called a pure tone.
What is a transverse wave?
The direction of particle displacement is perpendicular to wave propagation. For example, the surface of water is disturbed by a pebble, basilar membrane motion, and a stadium spectator "wave."
What is Visual Reinforcement Audiometry (VRA)? Furthermore, what are VRA responses & what might you expect?
This assessment is great for children 10 months to about 3 years of age. It may be used for children older or difficult-to-test populations.
- It is possible to watch a child's responses to sound by monitoring the head turn response to sounds coming from sound field speakers (narrowband noise and/or speech stimuli) or earphones (pure tone and/or speech stimuli) (can be completed with and without hearing aids (if the patient has them)).
- VRA relies on a child's ability to localize sound by turning toward the source of sound.
Procedure:
- Stimulus presented, child looks for a light picture.
- Children are reinforced for appropriate responses to sound (through video images; animated toy; light; etc.)
How many types of Visual Reinforcement Audiometry (VRA) are there?
There are two types of VRA:
- Traditional VRA
- Video VRA
What is an FM system? What is its purpose?
An FM system is a device that works with external speakers or connects to a hearing aid or cochlear implant.
An FM system is used to help improve the signal-to-noise ratio in a listening environment.
A microphone is worn by the teacher or communication partner. This microphone sends a signal to the receiver unit.
What are the different types of FM systems?
Wireless FM Ear Level Examples:
- This type of FM connects directly to the personal hearing aid or cochlear implant worn by the individual.
Soundfield FM Systems:
- Speakers are used to augment the signal (located on the desktop or in the room).
- Advantageous for all children in the classroom.
Where do AuD's refer patients? Why?
Typical referral sources include SLP, otolaryngologist, genetic counselor, and psychologist.
What is hyperacusis?
Hyperacusis is an abnormal intolerance to loud sounds.
- While some believe that it is just having abnormally sensitive hearing abilities, it is actually an abnormal loudness sensitivity due to damage in the auditory system (cochlear or central issue).
- Ear plugs may exacerbate, or make worse, the condition; audiological rehabilitation has been successful for some patients.
What are the different types of vestibular abnormalities tests?
-Caloric Testing
*ENG
*VNG
-Head Impulse Test (vHIT)
-Rotary Chair Testing
-Computerized Dynamic Posturography (CDP)
-Vestibular-Evoked Myogenic Potential (VEMP)
What is nonorganic hearing loss?
Nonorganic hearing loss refers to an apparent loss of hearing without any organic disorder or with insufficient pathological evidence to explain the extent of the loss.
Physiological Tests for Nonorganic Hearing Loss
-Useful in cases of possible erroneous hearing loss- requires no voluntary response.
- Immittance measures (tymps; ARTs)
- OAEs
- AEPs (ABRs)
Management of Patients with Nonorganic Hearing Loss
- Confronting patients may result in improved test validity.
- Clinicians usually advise the patient that test inconsistencies exist and then shift "blame" onto their shoulders (not explaining directions correctly; something wrong with equipment). Many times, the patient will have an honorable way out.
- For children, determining the underlying cause of the behavior is helpful (school, home life, etc.)
- May write "suspected nonorganic hearing loss" on the audiogram.
The Goals of Audiological Treatment
1. Enhance the activities and participation of a person with hearing loss.
2. Achieve adequate receptive and expressive communication.
3. Use of devices to minimize hearing loss.
4. Teach strategies and problem-solving to assist patients in overcoming interpersonal, psychosocial, educational, and vocational difficulties from hearing loss.
5. Limit negative effects on significant others.
6. Help patient and families to accept hearing loss and advocate for appropriate treatment and accommodations.
Hearing Aid Batteries/Battery Options
- Some hearing aids are rechargeable- if not, they need batteries to work.
- These are disposable batteries that come in various sizes.

How does a cochlear implant work?
- Used by individuals with moderately severe to profound hearing loss who cannot benefit from traditional hearing aid amplification.
- Must be able to discriminate speech information well enough to be able to access the majority of spoken phonemes.
- By-passes the cochlear and directly stimulates the auditory nerve via an electrical impulse carried along an internal electrode array.
What is the modiolus?
The core of the cochlea.
What is the auditory nerve?
- Nerve fibers from the cochlea spiral together to form a bundle or "cable" with basal fibers (high frequencies) to the outside of the cable- this is the auditory nerve.
- Low-frequency fibers (from apical areas) in the center.
- High-frequency fibers (from the basal turn) along the perimeter.
- Auditory nerve extends 17 to 19 mm beyond the IAC, attaching to the brainstem where the cerebellum, medulla oblongata, and pons form the cerebellopontine angle (CPA).
- At this point, the auditory nerve separates with one part going to the dorsal cochlear nucleus and the other to the ventral cochlear nucleus. The auditory nerve fibers terminate at the cochlear nuclei.
What are the roles of educational audiology?
- Wide range of responsibilities to help children with hearing loss access classroom curriculum- identification, referral, rehabilitation, selection, and evaluation of individual and group amplification.
- May provide ______ and counseling programs.
- May work closely with SLPs and teachers of the deaf and hard of hearing.
- Share information with other classroom professionals regarding hearing loss.
- Maintain and provide appropriate classroom technologies ranging from hearing aids to FM technology.
- Plan for changing technology and accessibility needs.
Describe 1-3-6 for infant identification.
- Test by 1 month.
- Diagnosed by 3 months.
- Intervention (device) by 6 months.
What are Spontaneous OAEs (SOAEs)?
- Can be detected without external stimulation.
- Occur in about half the general population of persons having normal hearing abilities.
- Generally is inaudible to the person in whose ear it is occurring.
- Can occur in one or both ears.
What are Evoked OAEs (EOAEs)?
- Given that we know that spontaneous OAEs can occur, we have found that we can cause them to occur.
- Can be transient (recorded in response to a click or tone pip signal) or distortion product (recorded as a different tone created by introducing two different frequencies).
- Can test a number of frequencies (similar to those tested on an audiogram) and indicate the presence of hearing loss.
- Recorded through the use of a probe inserted in the external auditory canal, attached to a signal-averaging computer (that filters out internal and external noise).
- Environment and patient must be very quiet during testing as any extraneous noise can affect results.
Describe Ipsilateral and Contralateral.
(Same side) Ipsilateral- Sound presented to one ear can evoke acoustic reflex in the same ear.
(Opposite side) Contralateral- Sound presented to one ear evokes an acoustic reflex in the opposite ear.
- Clinically, we test these pathways separately.
- 4 Sets of Reflex Thresholds:
*Ipsilateral Right
* Contralateral Right
*. Ipsilateral Left
* Contralateral Left
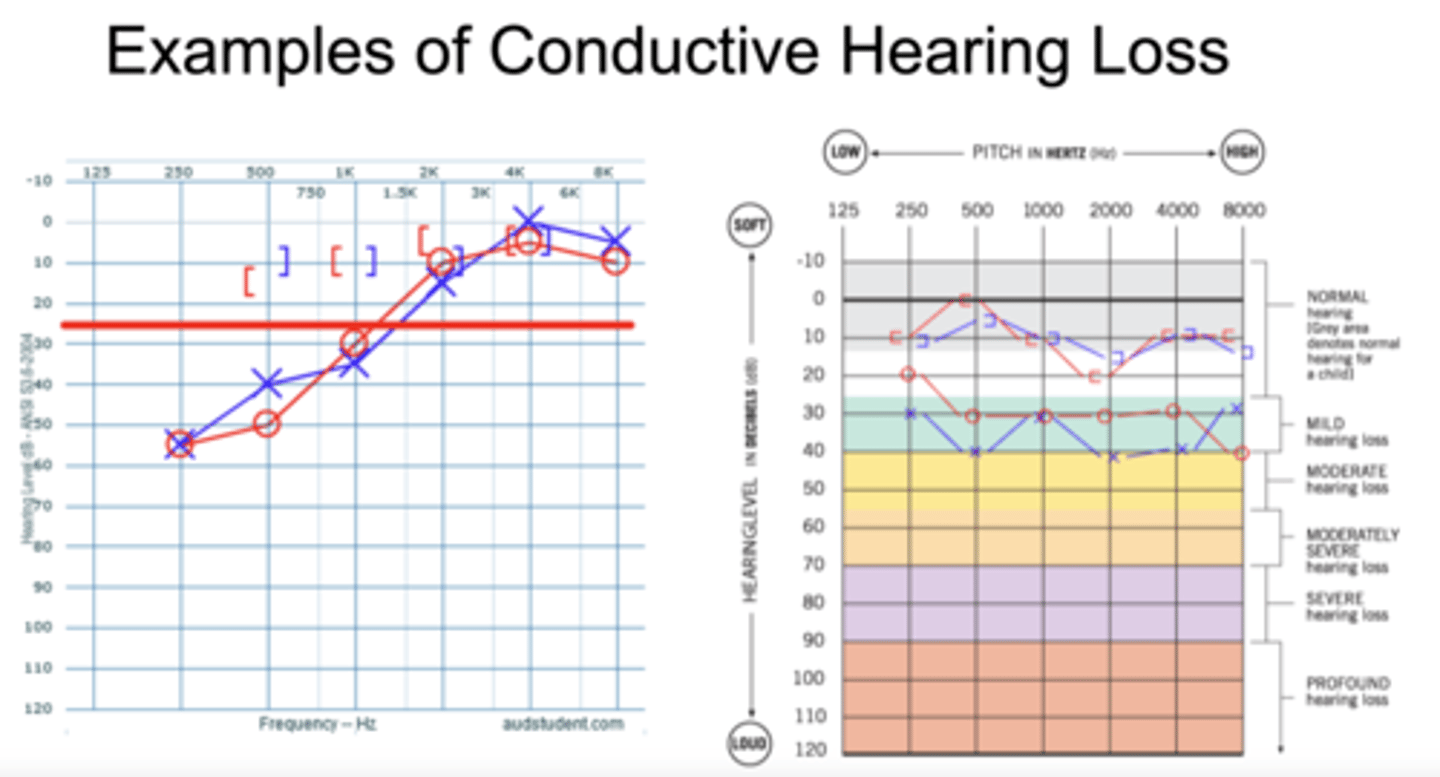
Air-Bone Gap
Air conduction thresholds -> degree of hearing loss.
Describe assistive devices.
- Hearing aids can be connected to other devices to aid in communication.
- These can include: Bluetooth Streamer, Remote Control Communication Microphone, Television Streamer, Phone Streamer
What is tinnitus?
Can presented as a ringing, roaring, hissing, whistling, chirping, rustling, clicking, buzzing, or other terms.
Tinnitus can be divided into two categories:
- Subjective: Much more common, experienced by the individual.
- Objective: Less frequent, caused by sounds generated by blood vessels or muscles near the ear, can frequently be heard by the examiner with a stethoscope.
What is the cause of tinnitus?
There is no one cause of tinnitus.
Describe a tinnitus evaluation.
Often completed through a multidisciplinary approach, tinnitus patients should be evaluated medically beforehand.
Describe the management of tinnitus.
If there does not appear to be a medical cause for the tinnitus, strategies such as retraining therapy, biofeedback exercises, or use of a tinnitus masker device can help.
CLSIM (What is it?) Primary Waystations
Central Auditory Pathway (CSLIMA)
- Cochlear Nucleus
- Superior Olivary Complex
- Lateral Leminscus
- Inferior Colliculus
- Medial Geniculate Body
- Auditory Cortex
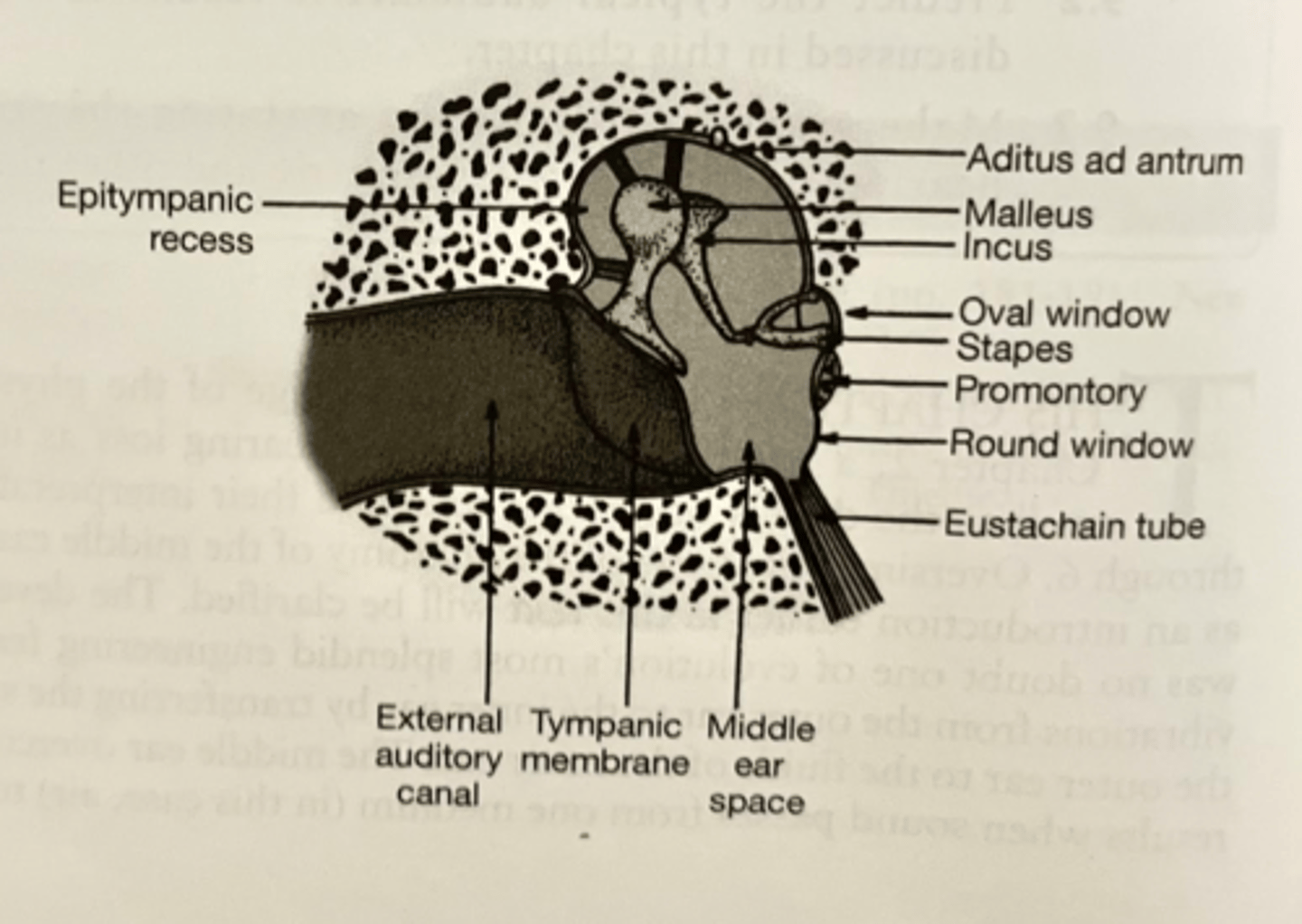
What are the parts of the tympanic membrane?
- Pars Tensa: Greatest surface area of the TM
- Pars Flaccida: Upper portion of TM where fibers are looser
- Movement of the TM causes movement of the three bones of the middle ear system (ossicles)
Describe the characteristics of the tympanic membrane.
Pearly-grey in color, translucent, shiny, and mobile on insufflation.
What is a SOAP note?
A popular way to report on a patient's appointment (sometimes used in-house only).
- S: Subjective- Relevant complaints/reason for the visit. Subjective observations and family, medical, and otologic history.
- O: Objective- Test or procedures completed; findings and test results.
- A: Assessment- A summary of the "S" and "O" to provide a diagnostic statement and the implications of the findings.
- P: Plan- Appropriate recommendations, follow-up.
Describe prelingual hearing loss.
Prelingual hearing loss occurs before a child develops speech and language, and is usually associated with severe or profound hearing loss.
Describe postlingual hearing loss.
Postlingual hearing loss appears at any point after a child has acquired speech and expression skills. In this case, their communicative ability is not necessarily affected when they experience hearing loss.
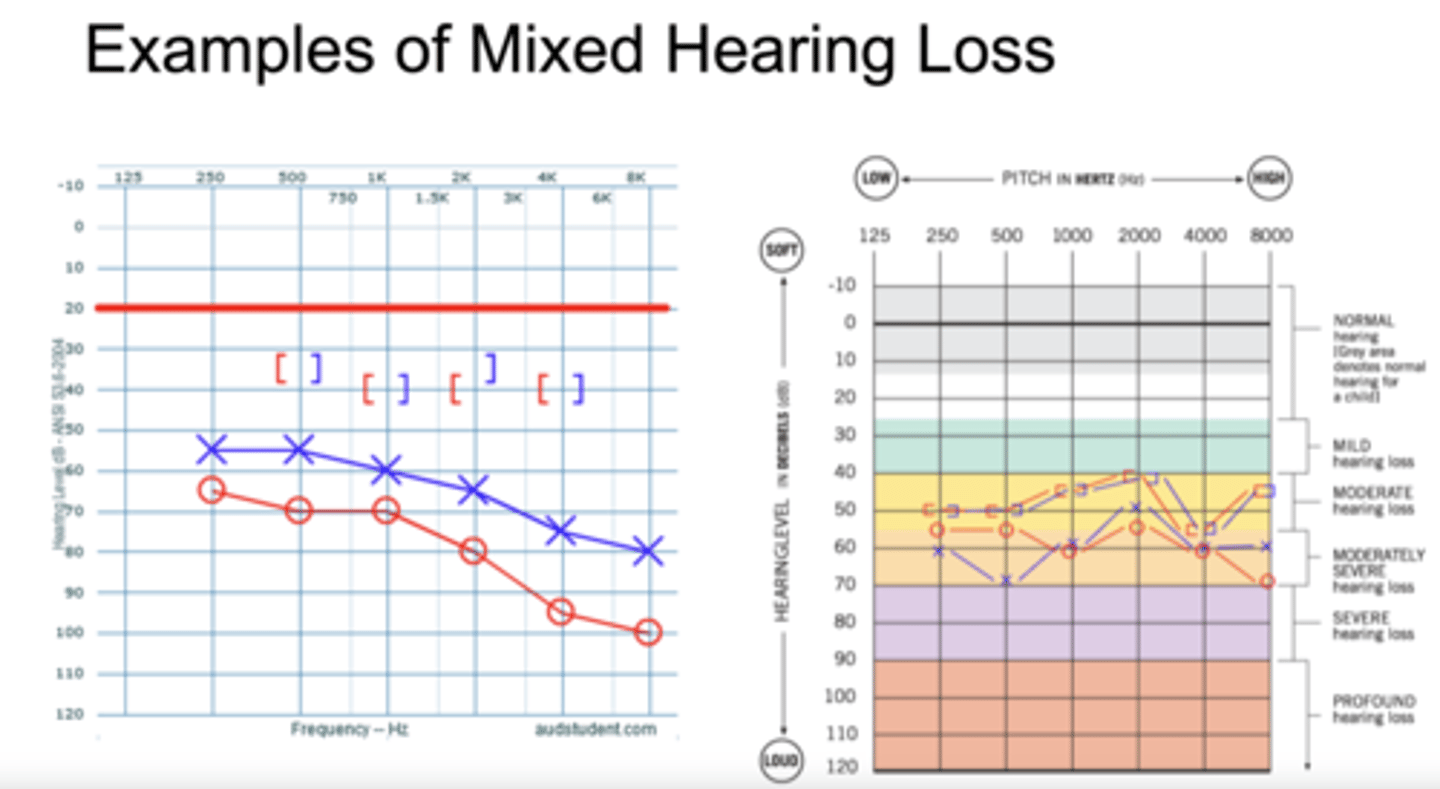
What are the degrees of hearing loss?
-Normal: 0-20 dB HL
- Mild: 25-40 dB HL
- Moderate: 40-55 dB HL
- Moderately-Severe: 55-70 dB HL
- Severe: 70-90 dB HL
- Profound: > 90 dB HL
How many types of hearing loss are there? What are they?
3; Conductive, Sensorineural, and Mixed
What is a conductive hearing loss?
Hearing loss originates from the outer or middle ear.
Audiogram: No bone conduction loss, air conduction loss, and air-bone gap greater than 10 dB.
What is a sensorineural hearing loss?
Hearing loss originates in the inner ear or auditory nerve.
Audiogram: Air conduction AND bone conduction loss, and air-bone gap is 10 dB or less.

What is a mixed hearing loss?
Hearing loss originates from the outer or middle ear AND the inner ear or auditory nerve.
Audiogram: Air conduction loss, bone conduction loss, and air-bone gap greater than 10 dB.
Where does ear wax occur?
In the cartilaginous portion of the external auditory canal (closest to the outside).
How do we screen infants' hearing?
Methods of infant hearing screenings:
- ABR Screening
- OAE Screening
What are Jerger types?
Jeger developed a category system for tympanograms in the 1970s.
What are the five Jerger tympanogram types?
1. Type A = "normal"
- Suggest ______ middle ear function.
- All values are WNL.
- No conductive component suspected.
2. Type As = "stiff"
- SAA: Low
- TPP: WNL
- ECV: WNL
- Underlying disorder will determine the degree of hearing loss.
3. Type AD = "hypermobile"
- SAA: High
- TPP: WNL
- ECV: WNL
- Underlying disorder will determine the degree of hearing loss.
4. Type B = "flat"; co compliance; ECV could be normal or abnormal
- No peak is seen (flat line).
- Suggests middle ear dysfunction, a blockage in the external auditory canal, or TM perforation.
- Could also be seen with abnormally low or high ECV.
- SAA: None
- TPP: None
- ECV: Could be low; WNL: Or high dependent on underlying condition.
Component most likely to present.
5. Type C = negative pressure
- SAA: Normal
- TPP: Abnormal (>-149 daPa)
- ECV: WNL
- Usually consistent with negative middle ear pressure; Eustachian tube dysfunction.
Describe eustachian tube orientation in adults versus children.
More horizontal in children, vertical in adults.
What is the acoustic reflex threshold (ART)?
The contraction of the stapedius muscle in response to intense sounds (automatic response).
Acoustic reflex threshold -> Lowest intensity level at which an acoustic reflex can be obtained (see change of compliance).
This reflex also causes the middle ear system to stiffen and decrease the static acoustic admittance.
Requires good function of outer ear, middle ear, cochlea, and neural function.
What are the test frequencies for acoustic reflex threshold (ART)?
Test frequencies: 500, 1000, 2000, and 4000 Hz (4000 Hz can have limited clinical variability).
Tones are presented in a similar fashion to pure tone testing (down 10; up 5) until a threshold can be determined.
Acoustic reflex threshold (ART), what are we measuring?
The intensity required to see a change in compliance that indicates the muscle is contracting.
The patient has to be still and silent for testing.
Permanent Hearing Loss
Permanent is a sensorineural hearing loss.
Transient Hearing Loss
Transient isn't life long.
What is the SLP's scope of practice in hearing screenings?
SLP- ASHS Scope of Practice includes hearing screening therapeutic aspects of audiological rehabilitation, and basic checks of hearing aid performance.
Children in Mainstream Classroom that have Hearing Loss
Mainstreaming features:
- Inclusion in all aspects of a regular classroom. Classroom adapts to children with hearing loss. Use of verbal or cued speech, total communication, FM system, etc.
Be familiar with Figure 9.1 in your textbook.
How does a low frequency hearing loss affect your ability to discriminate speech?
Difficulty understanding vowel sounds.
How does a high frequency hearing loss affect your ability to discriminate speech?
Difficulty understanding consonant sounds.
What is the Stenger test?
Used for hearing losses that there is at least a 25 dB admitted difference between ears (i.e., unilateral; asymmetrical).
Based on the Stenger Principle, when two tones of the same frequency are introduced simultaneously in both ears, only the louder tone will be perceived.
Can also be used with spondaic words.
Describe the Stenger test procedure.
Determine the thresholds for each ear.
Introduce a tone at 10 dB above the threshold of the "better" ear.
A response should be obtained
Introduce a tone at 10 dB below the threshold of the "worse" ear.
A response should not be obtained (either patient is unwilling to respond, or they cannot hear it)
Then introduce both tones simultaneously (10 dB above the threshold of the "better" ear and 10 dB below the threshold of the "worse" ear).
This can be completed at all frequencies where there is a difference of at least 25 dB between ears.
Describe a Positive Stenger and a Negative Stenger.
Positive Stenger (malingers):
- If a patient fails to respond, it is because they hear the tone in the poorer ear, which they do not wish to admit. This suggests that the threshold results obtained in the poorer ear are inaccurate, but do not reveal the true organic thresholds. They are unaware that there is a tone in the better ear, owing to the Stenger effect, and so will not respond at all.
Negative Stenger (not malingers):
- Patient responds when both ears are stimulated. This suggests the absence of erroneous behavior, at least at the frequencies tested.
Mass vs. Frequency
Think more about the relationship between mass and frequency (think vibration).
Properties of Sound: Frequency: Mass
Mass increases - frequency decreases.
Example: Thicker guitar strings produce lower-frequency vibrations while thinner guitar strings produce higher-frequency vibrations.
Describe the ear canal.
2 sections:
- Cartilaginous (outer 1/3)
* Thicker skin
- Bony (inner 2/3)
* Thinner skin
Length of approximately 2.5 cm for adults. 15 mm at birth.
What are the main functions of the outer ear?
Sound transmission:
- Pinna helps with sound localization
- Funnels sound to TM via the ear canal
- EAC had resonant frequency (around 3000 Hz) which amplifies
Protection:
- Protection of the middle and inner ear structures
- Keeps out dirt, water, external infection
Describe sound attenuation.
Definition: A decrease in the strength of the sound.
Sound can be attenuated (or decreased in intensity) when there is something blocking the sound from being transferred.
- Ex: ear plugs reduce the amount of sound waves that enter into the ear canal, therefore reducing the strength of the sound that is reaching the TM/auditory system
Sound is also attenuated by the head.
- If someone is speaking to you on your right side then the sound will be attenuated as it passes over to your left ear.
- The right ear will hear the sound unattenuated.
What is the speech recognition threshold (SRT)?
Lowest level at which a patient can recognize or identify words at least 50% of the time.
How can SRT be detected?
Can be assessed monaural, binaural, and in soundfield.
What is the SRT-PTA agreement?
Within +/- 10 dB
What is interaural attenuation?
Loss of energy of a sound presented by either AC or BC as it travels from test ear to non-test ear; dB lost in cross hearing.
What is the interaural attenuation for air conduction supra-aural earphones?
40 dB
What is the interaural attenuation for air conduction insert earphones?
60 dB
What is the interaural attenuation for bone conduction?
0 dB
Main Types of Hearing Aids
-BTE (Behind the ear)
- RIC (Receiver in the canal)
- ITE (In the ear)
- ITC (In the canal)
- CIC (Completely in the canal)
BTE (Behind the ear) Hearing Aids
The hearing aid rests on top of the auricle.
A tube goes around the top of the ear and connects to an earmold which fits the patient's ear.
There are controls available on the hearing aid (volume, programs, FM).
RIC (Receiver in the canal) Hearing Aid
Very popular style today.
Instead of the receiver (loudspeaker) in the case of the hearing aid, it is in the part that goes into the ear.
Uses a thinner tube than a BTE.
May use an earmold or a disposable dome piece.
ITE (In the ear) Hearing Aids
Fill the concha of the ear and extend into the external auditory canal.
All the hearing aid components are built into the hearing aid itself.
ITC (In the canal) Hearing Aids
Smaller than ITE.
Fills opening to external auditory canal.
CIC (Completely in the canal) Hearing Aids
One of the smallest hearing aids.
Fits deeper inside the external auditory canal.
Bone-Conduction Hearing Aids
Looks similar to a bone conduction testing device.
This example would be worn as a headband over the head, with the vibrator being placed on the mastoid process.
Not very common today; uncomfortable.
Bone-Anchored Hearing Aid (BAHA)
Also known as an "osseotympanic implantable amplifier."
A titanium implant is surgically placed in the mastoid area.
Once firmly in place (about 3 months post-op), an external processor is attached to the external abutment.
The amplifier drives the sound via mechanical vibration that travels down the pin into the skull.
Specific applications for atresia, microtia, and chronic outer/middle ear disease, unilateral profound SNHL.
What are the external components of a cochlear implant?
Called the processor, this contains a microphone and internal, digital circuitry that processes the sound according to an algorithm (called a MAP).
What are the internal components of a cochlear implant?
Includes a magnet, power pack, electrode array, and guide.
If all heals well, external components can be put on and cochlear implant will be activated at a later date (weeks to months).
Why do patients fake hearing loss?
Expected financial gain:
- Lawsuit
- Worker's Compensation
- Other benefits
Expected psychological gain:
- Attention
- Peer acceptance
- Parental affection
- Decreased academic pressures
The person may essentially be incapable of more reliable behavior or has a psychological disorder.
What are the behavioral tests used for nonorganic hearing loss?
- Stenger test
- Speech Stenger Test
- Yes-No Test (usually for pediatrics)
- Doerfler-Stewart Test
- Delayed Speech Feedback Test
- Pure Tone Delayed Auditory Feedback Test
- Variations on Bekesy Audiometry
- Varying Intensity Story Test
What are the goals of vestibular rehabilitation?
To decrease the frequency, intensity, and duration of dizziness episodes.
To improve an individual's functional balance.
To decrease the severity of the related symptoms of nausea, headache, and lightheadedness.
To improve the individual's performance of daily activities.
To develop compensation strategies for comping with disequilibrium, dizziness, and accompanying anxiety.
Where can AuD work?
- Private Practice
- Hospitals
- Physician offices
- Community clinics
- Schools
- Industry
- Military/Government (VA)
- Universities- clinics and academia
What is a false negative response?
When the patient does not react when they hear a sound.
What is a false positive response?
When the patient responds when no sound is emitted.
What does the air-bone gap need to be for conductive hearing loss?
Greater than 10 dB; bone conduction is normal.
What is the air-bone gap for a mixed hearing loss?
Greater than 10 dB and BC is better than AC.
Masking. Why do we mask?
To prevent participation from the non-test ear.
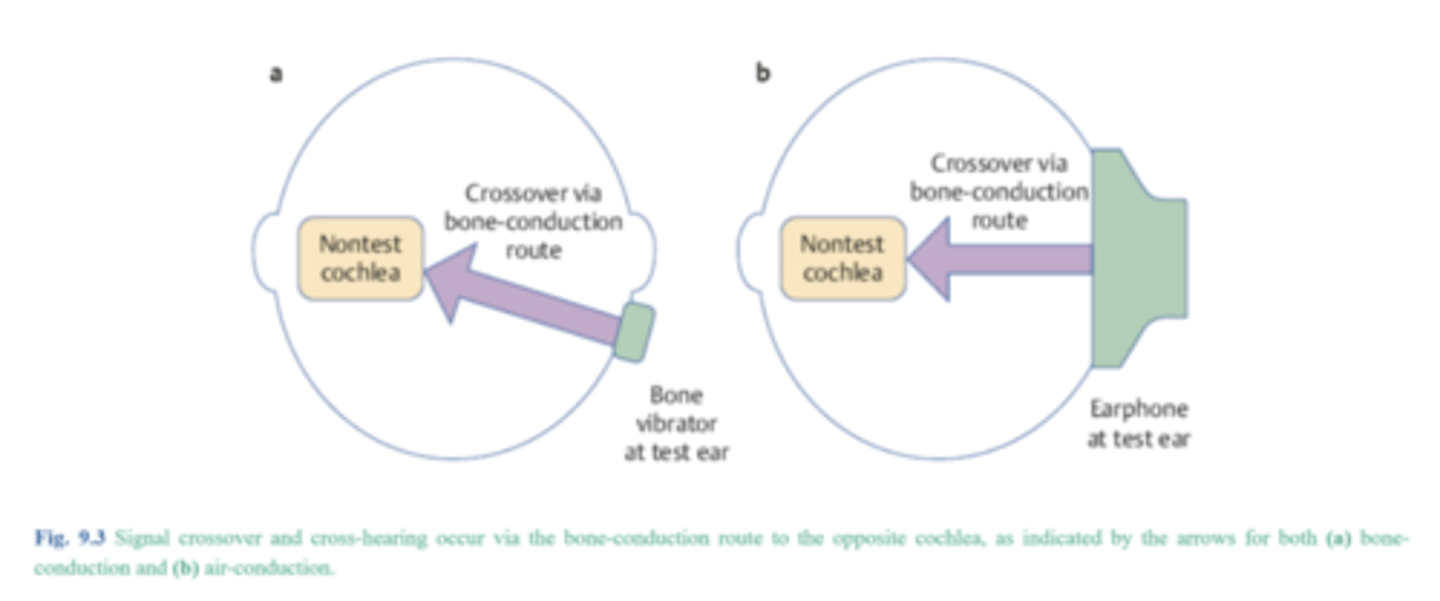
What is air conduction masking?
What are we comparing? Air threshold of test ear to opposite bone threshold of the non-test ear.
Rule: AOBG > IA
AOBG = air opposite bone gap
IA = either 40 or 60
If the rule is true, you have to mask.
What is bone conduction masking?
What are we comparing? Air threshold of the test ear to the bone conduction threshold of the test ear.
Rule: ABG > 10
If the rule is true, then you have to mask.
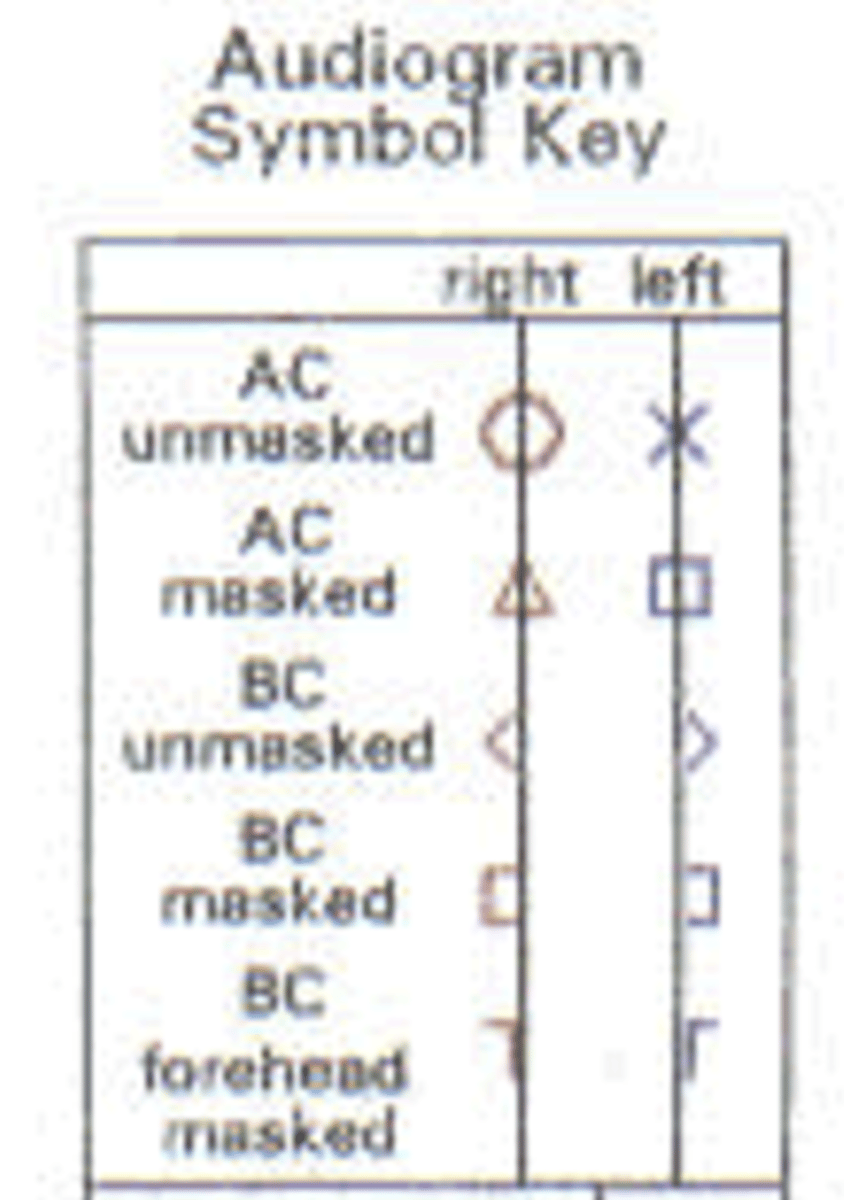
Symbols
What is dynamic range?
Dynamic range is the difference between the threshold of sensitivity and the patient's UCL
- Threshold of sensitivity-lowest level that the patient can hear
A patients dynamic range is the range of sounds that they have access to in the environment.
re: SRT
If a patient's SRT is 40 dB HL and you plan to present a word list at 30 dB SL re: SRT, what level would this be?
- Re: = above
- 40 + 30 = 70
- 70 dB would be the presentation level
Configuration of Audiogram
Sloping - better in low frequencies
Flat- all thresholds are within 15-20 dB of each other
Precipitous- steep slope
High-frequency loss (above 2000 Hz)
Sensation Level
dB SL - sensation level
- Level of presentation above client's threshold- Present at 30 dB SL
■ Patient A threshold 25 dB HL 55
■ Patient B threshold 40 dB HL 70
■ Patient C threshold 80 dB HL 110
dB HL - hearing level
- This is how dB is reported on the audiogram
- HL is a decibel unit that was developed in order to straighten out the human hearing curve and it is related by correction factors to dB SPL
- 1920s research
dB SPL - sound pressure level
- Research-based levels- SPL is logarithmically related to the physical units of sound pressure, such as: pascals