Ch. 2 Microscopic Anatomy of the Periodontium
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
Tissue is a group of…
interconnected cells that perform a similar function within an organism
Tissues and organs of the body are composed of several different types of ____ and ________ elements outside of the cells
cells, extracellular
Cells:
Smallest structural unit capable of functioning independently
as a group, they form tissue
Four basic types of tissue:
Epithelial
Connective
Nerve
Muscle
Extracellular Matrix:
Gel-like substance (mesh-like) containing interwoven protein fibers surrounding most cells
serves as scaffolding for cells as it creates a framework where cells can interact with one another
Fibers of the matrix are collage (majority), elastin and reticular fibers
Extracellular Matrix in Epithelial Tissue:
sparse
thin mat called basal lamina underlies epithelium
Extracellular Matrix in Connective Tissue:
more plentiful
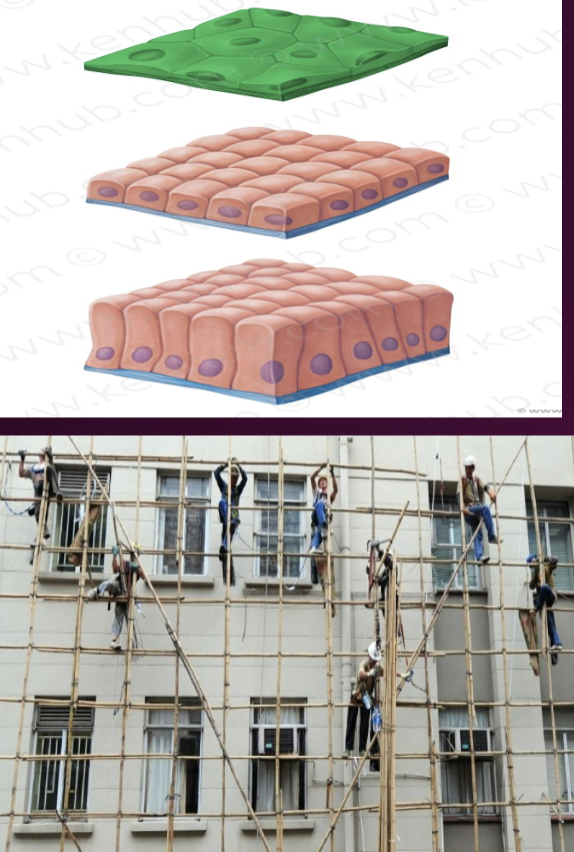
Microscopic Anatomy of Epithelial Tissue:
epithelial tissue is the body’s skin or epidermis and lines body cavities (mouth, stomach) mucosa
closely packed epithelial cells are bound into sheets
the only part of extracellular tissue that is part of epithelial tissue is the thin mat called basal lamina (supports like a scaffolding)
Keratinized Epithelial Cells:
process by which epithelial cells on a surface become stronger and waterproof
keratinized epithelial cells have no nuclei
mostly heavily keratinized body parts-hands, feet
Non Keratinized Epithelial Cells:
have nuclei
softer and more flexible
found in mucosa: lining of cheeks
allows. flexibility to speak and chew
Blood Supply of Epithelial Cells:
epithelial cells are avascular
they contain no blood vessels
receive O2 and nourishment from vessels in underlying connective tissue
called diffusion
Connective tissue fills _____ between tissues and organs in the body and ______ or binds other tissue
space, supports
Connective tissue cells are ______ ______ in extracellular matrix
sparsely distributed
Is extracellular matrix a major component of connective tissue?
Yes
Connective tissue is composed of:
Fibroblasts that form extracellular matrix
Macrophages that devour invading microorganisms
Neutrophils that devour invading microorganisms
Lymphocytes as part of the immune system
Examples of Dental Connective Tissue:
cementum
dentin
alveolar bone
pulp
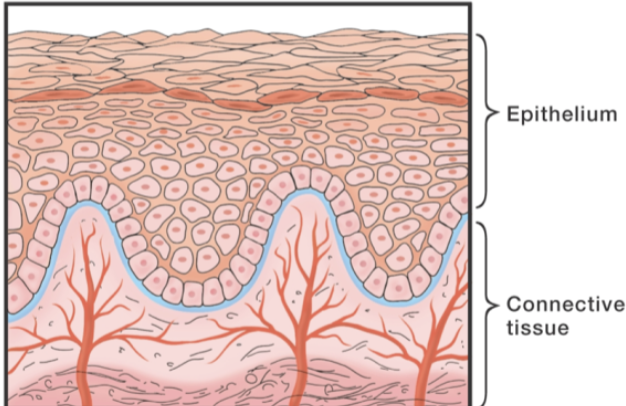
The interface is where epithelial tissue and connective tissue meet and can be…
wavy or smooth
if it is a wavy boundary, it will have deep extensions of epithelial ridges of epithelium that reach down into connective tissue
epithelial ridges are also called rete pegs
Summary of Epithelial Tissues:
many, many cells; composed primarily of cells
very little extracellular matrix
no blood supply
Summary of Connective Tissue:
few cells
comprised mostly of extracellular matrix
rich blood supply
Wavy Boundaries:
enhances adhesion of epithelium to connective tissue by increasing surface area
allows skin to resist mechanical forces
provides larger area to receive nourishment from underlying connective tissue
Epithelial Cell Junctions:
cellular structures that mechanically attach a cell’s cytoskeleton to its neighbor or the basal lamina
binding is needed to form a structurally strong unit
the more the mechanical stresses, the more the abundant cell junctions
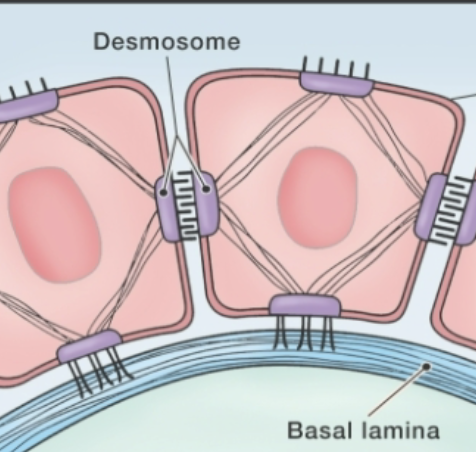
Cell Junction: Desmosome
connects two neighboring epithelial cell cytoskeletons
cell-to-cell connection
found in gingival epithelium
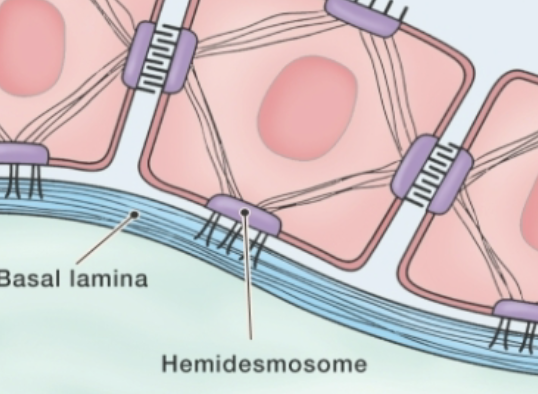
Cell Junctions: Hemidesmosome
connects epithelial cells to the basal lamina
cell-to-basal lamina connection
also found in gingival epithelium
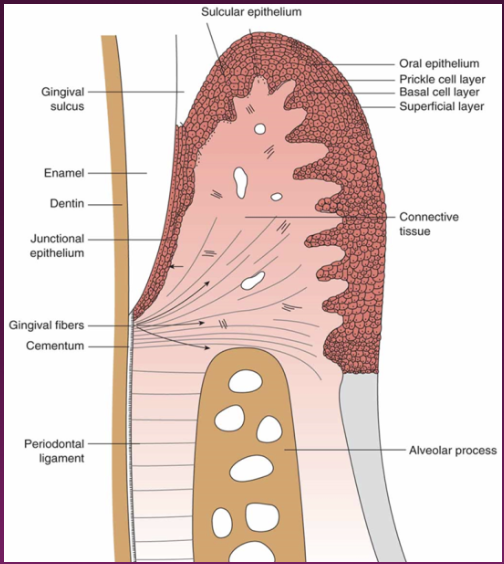
Microscopic Anatomy of Gingival Epithelium:
stratified squamous epithelium in the oral cavity functions well in a wet environemnt
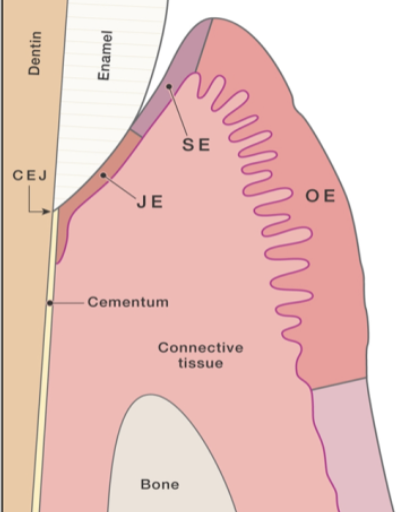
Three Anatomical Areas of Gingival Epithelium:
Oral Epithelium (OE)
Sulcular Epithelium (SE)
Junctional Epithelium (JE)
Oral Epithelium:
covers outer surface of free gingiva and attached gingiva from the crest of the gingival margin to the mucogingival junction
may be keratinized or parakeratinized (partially keratinized)
joins connective tissue in a wavy interface with epithelial ridges
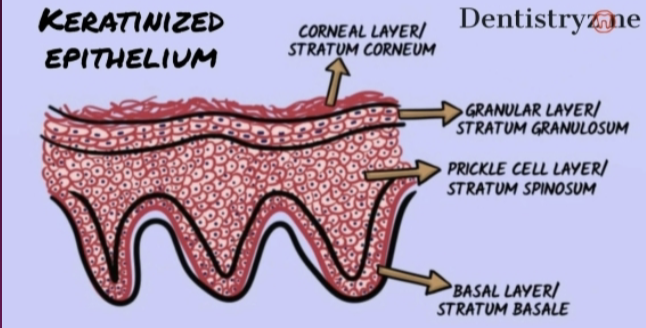
Four Layers of Stratified Squamous Epithelium:
Cube-shaped cells in the basal layer
Spine-like cells in the prickle cell layer
Flattened cells in the granular cell layer
Flattened cells with extensive intracellular keratin in the keratinized cell layer (Stratum Corneum)
Microscopic Anatomy of Sulcular Epithelium:
the epithelial lining of the gingival sulcus is thin and nonkeratinized
continuous with oral epithelium extending from crest of gingival margin to coronal edge of junctional epithelium
permeable, allowing fluid to flow from gingival connective tissue into sulcus-gingival crevicular fluid
The Cellular Layers of the Sulcular Epithelium:
Basal cell layer
Prickle cell layer
Superficial cell layer
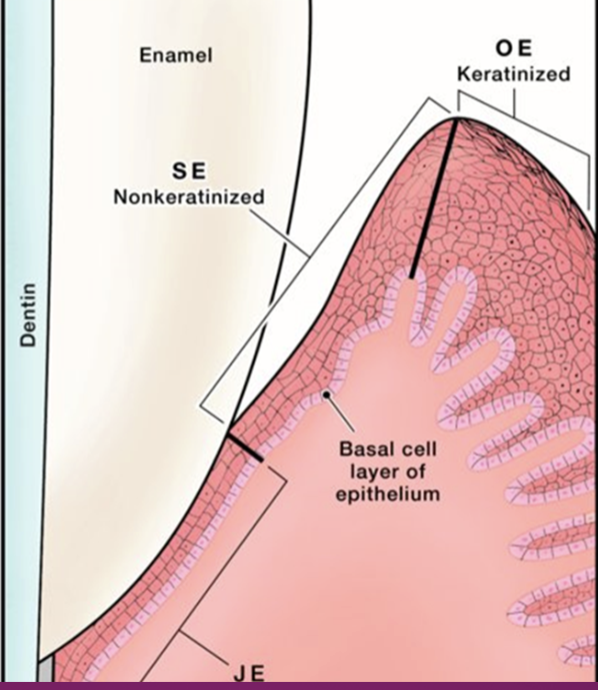
Microscopic Anatomy of Junctional Epithelium:
forms the base of the sulcus and joins gingiva to the tooth
in health, JE attaches to the tooth slightly coronal to the cementoenamel junction
thin and nonkeratinized, easily penetrable
easiest entry point for bacteria to invade into connective tissue
comprised of closely packed epithelial cells
has a sparse extracellular matrix with a thin basal lamina between JE and the tooth surface and JE and gingival connective tissue
Two Cell Layers of Junctional Epithelium:
basal cell layer
prickle cell layer
15 to 30 cells thick at coronal zone and tapers to 4 to 5 cells thick at the apical zone
Cells next the tooth form __________that attach the internal basal lamina with the tooth surface
hemidesmosomes
Cells next to gingiva that form ____________ that attach the external basal lamina with gingival connective tissue
hemidesmosomes
The interface tissue of the junctional epithelium is ____ with connective tissue
smooth
Junctional Epithelium’s Importance to Teeth:
when teeth erupt through epithelium (protective coating covering body), they create an opening where bacteria can enter the body
the body’s attempt to “seal” the opening created during eruption results in junctional epithelium
JE provides an attachment between gingiva and tooth sealing the base of the periodontal pocket
Microscopic Anatomy of Gingival Connective Tissue:
also known as lamina propria, gingival connective tissue provides solidity and attaches gingiva to root cementum and alveolar bone
is the opposite of gingival epithelium in that it has an abundance of extracellular matrix and few cells
extracellular matrix is produced by fibroblasts
protein fibers, including collagen fibers, account for 55% to 65% of gingival connective tissue: gel-like material 30-35%
collagen forms the rigid “cuff” around the tooth
transportation of water, nutrients, oxygen, and metabolites to the gingiva occurs within the matrix
Three Types of Cells in Gingival Connective Tissues:
fibroblasts
mast cells
immune cells-macrophages, neutrophils, and lymphocytes
Supragingival Fiber Bundles:
a network of rope-like collagen fiber bundles located coronal to the crest of alveolar bone
strengthen attachment of JE to tooth by bracing the gingival margin against the tooth
JE and gingival fibers are known collectively as dentogingival unit
Supragingival Fibers Function to:
reinforce attachment of JE to tooth
provide rigidity to free gingiva so it can withstand chewing forces
connect free gingiva with root cementum and alveolar bone
connect adjacent teeth to one another
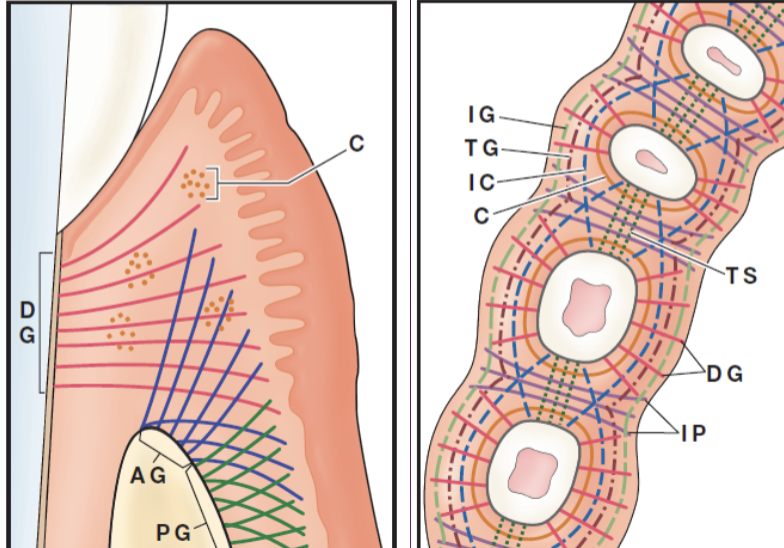
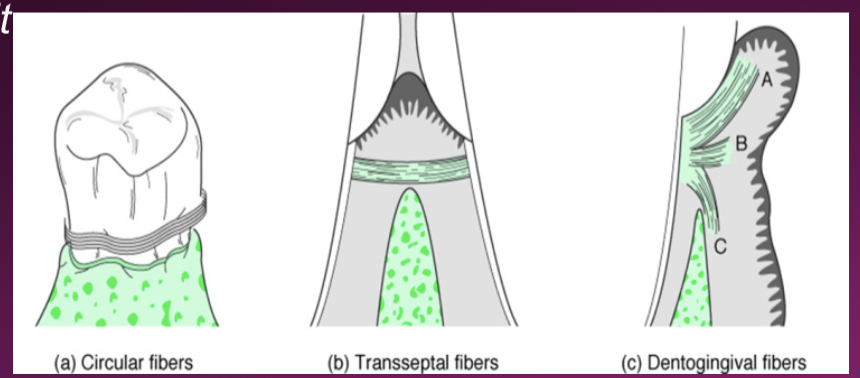
9 different fibers bundles named after orientation and insertion:
alveologingival
circular
dentogingival
periosteo gingival
intergingival
intercurricular
interpapillary
transgingival
transseptal
Periodontal Ligament Fibers:
rope-like collagen fibers that stretch across space between cementum and alveolar bone of tooth socket
have a rich supply of nerves and blood vessels
main function is to provide support and sensing of pain and tactile pressure
embedded ends are known as Sharpey fibers
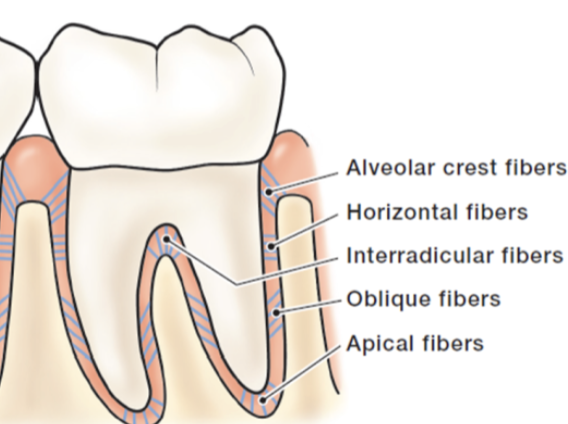
5 Principal Periodontal Ligament Fibers:
alveolar crest
horizontal
oblique
apical
interradicular
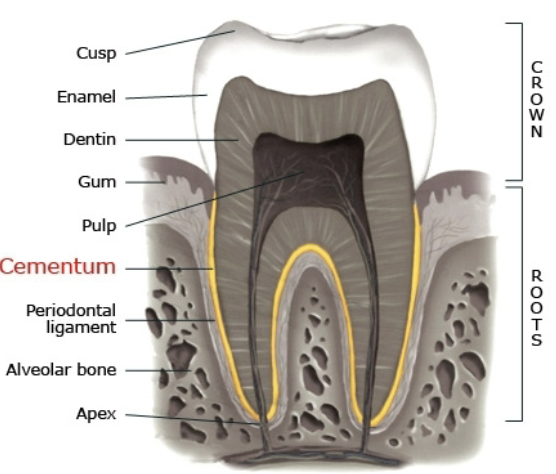
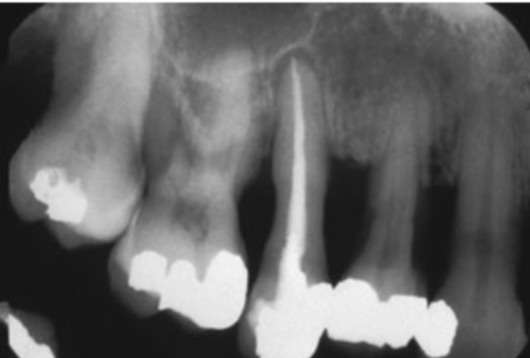
Microscopic Anatomy of Cementum:
mineralized tissue covering tooth roots
periodontal ligament fibers embed in cementum to attach tooth to bone
involved in tooth repair and generation
seals open dentinal tubules
continues to grow in thickness as we age, to compensate for occlusal/incisal attrition
Three Components of Mature Cementum:
Organic: densely packed collagen fibers oriented parallel to long axis of tooth
groups of proteins form cementum proteins that may regulate formative mineralization
Mineralized: hydroxyapatite crystals
Biologic: growth factor molecules are produced during formation then stored in matrix to assist with periodontal ligament regeneration
Cementum Conservation when Instrumenting:
instrumentation can lead to exposure of dentin, causing hypersensitivity
cementum removal is not necessary to eliminate bacteria
preservation of cementum is important because of its source for growth factors
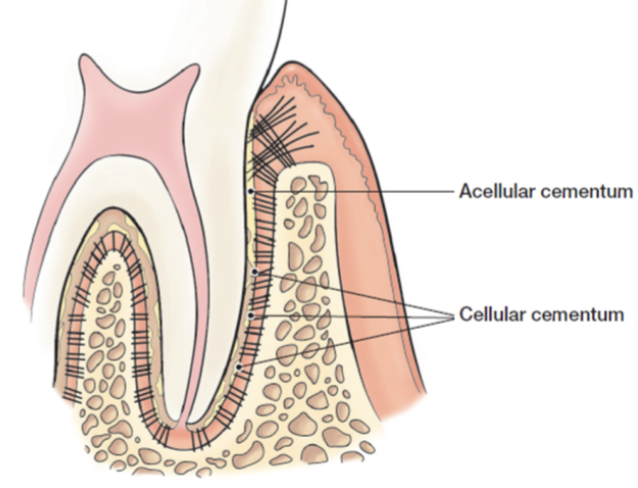
Three Types of Cementum:
Intermediate-located at CEJ
Acellular-composed mainly of Sharpey Fibers, contains no living cells
Cellular-contains cementocytes and fibroblasts
present at apical and interradicular parts of root
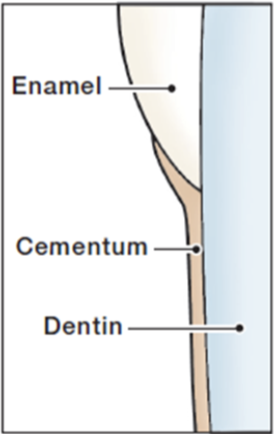
Three Arrangements of Cementum to Enamel (OMG):
cementum overlaps enamel for a short distance
cementum meets enamel
cementum leaves a gap between itself and enamel

Functions of Alveolar Bone:
alveolar bone protects roots of teeth by forming bony sockets that provide support
constantly undergoes periods of bone remodeling when teeth are subject to mechanical forces
comprised of mineralized connective tissue formed by osteoblasts
least stable part of periodontium because of constant osteoclastic/osteoblastic action
Two Major Cell Types:
osteoblastss which produce the bone matrix of collagen fibers and other protein fibers
osteoclasts which are cells that remove mineral material and organic matrix of bone
Characteristics of the Alveolar Bone:
extracellular matrix contains-collagen fibers and gel-like substances-major component
bone matrix is rigid because of mineral deposition of calcium and phosphate-subsequently transformed into hydroxyapatite
alveolar bone contains-blood vessels and nerve innervation