510 Midterm 3 - GI System
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Define Bolus
Food in mouth/esophagus + saliva
Define Chyme
Bolus + HCl + enzymes (in stomach)
List the main components of the GI tract
Oral cavity
Esophagus
Stomach
Small intestine - Duodenum, Jejunum, Ilium
Large intestine - (Vit production) Cecum, Colon, Rectum, Anus
How does the stomach differ in Ruminants?
4 chambered:
Rumen
Reticulum
Omasum
Abomasum
How do the following accessory organs contribute to digestion?
Pancreas
Liver
Gal bladder
Pancreas: releases enzymes into Duodenum/Jejunum
Gal bladder: storage of bile; released into Duodenum/Jejunum
Liver: releases enzymes into Jejunum; production of bile
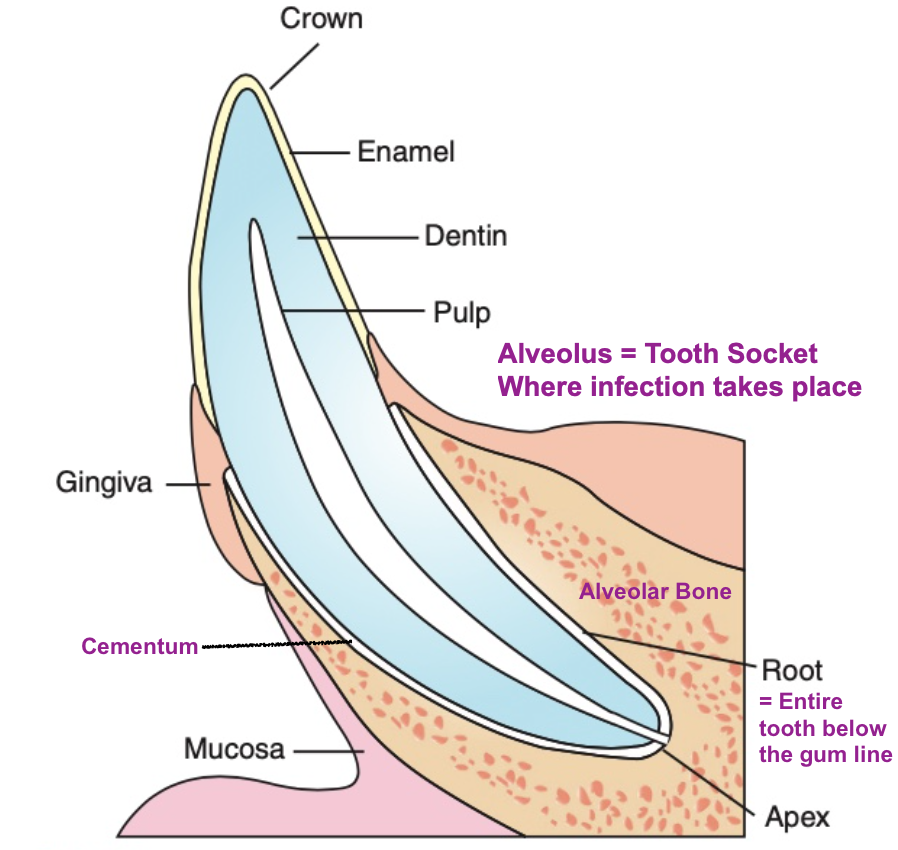
What part of the tooth does Gingivitis infect?
The gingiva at the Gingiva Sulcus
Compare Plaque to Tartar/Dental Calculus
Plaque = bacterial coating on the teeth - but usually friendly
Dental calculus = Tartar = mineralized plaque = very irritating to Gingiva
What is Gingivitis?
How does it progress to Pariodontitis?
Gingiva = infectious, reversible inflammation of the gum margins
-Changes in pH of mouth —> multiplication/invasion of pathogenic bacteria —> further inflammation —> weakened tooth attachment (periodontitis)
Pariodontitis = “around” the “tooth” “inflammation”
Irreversible loss of gingival attachment + bone dissolving/reabsorption - Once the ligaments and alveolus become inflamed —> gum recedes to expose tooth roots + bone no longer protected, begins to dissolve/get reabsorbed —> tooth falls out b/c nothing to hold on to (wiggly is painful too)
What are the 4 stages of tooth decay?
Stage 1: Gingivitis - sulcus depths still normal (gums red)
Stage 2: Gingival hyperplasia - plaque becomes mineralized
Stage 3: Periodontitis w/vertical bone destruction
Stage 4: Periodontitis w/horizontal bone destruction
Clinical Sings for Gingivitis/Pariodontitis
Halitosis (bad breath)
Reluctance to eat/chew hard food, oral pain, loose teeth
Pawing at mouth
Head shyness (pain)
Increased saliva, possible bloody
Sneezing/nasal discharge - hard palate (roof of mouth) = floor of nasal cavity; infection can spread to nasal passage in a top tooth is involved
Facial Swelling
Tooth loss
Diagnostics for Gingivitis/Pariodontitis
Oral exam (req sedation)
Assess Tartar/inflammation
Probe (to assess sulcus depth)
Radiography - should not see any exposed root or bacteria in the alveolus
Treatment for Gingivitis/Pariodontitis
Dental scaling - using medical grade equipment to scrape calculus off
Must clean BELOW the gumline to be effective
Clean debris around tooth
Extract loose teeth
Antibiotics
Prevention for Gingivitis/Pariodontitis
Practice oral hygiene once adult teeth come in (~2yrs old)
Brushing - can even be an enriching experience for the animal
Wipes not as effective b/c don’t get under the gum line
** Pathology lives in the Sulcus; removing only the external calculus = purely cosmetic
Gels, water additives
Routine “dentals” by vet/tech
Feed hard, crunchy food or greenies/other chew toys
Tx gingivitis early (as soon as gums are red)
Vaccination (still controversial)
Esophageal Disease - CHOKE
Define the condition
How does it differ for horses and cows
Partial/total esophageal obstruction
Super dangerous in Cows b/c they fore-gut ferment and need to belch the gas out. Horses can fart it out. W/o eructation, cows bloat and can die
Causes of Choke
Food - incomplete chewing/lubrication (maybe eating too quickly b/c competing for food), or tries to eat whole fruits—> get stuck/expands in esophagus
Foreign body (FB) such as wood etc hidden in food
Drugs that decrease smooth muscle motility
Trauma/inflammation
Scar tissue
Neoplasia (tumor/mass growth) in the neck
Clinical signs of Choke, Horse
What similar condition should you rule out?
Anxious, sweating salivating (salivating most indicative of GI issue vs. other)
Stretching the neck - stuck food is painful
Swelling of throat
Nasal discharge w/NON DIGESTED food
When head is lowered, food comes back up since can’t go into stomach
Coughing - when food is suck, epiglottis can’t close —> food/liquid in trachea —> coughing —> pneumonia (dangerous!!)
***CAUTION - Can look like RABIES***
Also includes sad/depressed, head hanging, foamy saliva (can’t swallow)
Clinical signs of Choke, Cow
Bloat = Accumulation of free gas (type2) or froth (type 1) in the rumen
(bloat can be result of other things too tho, more later)
Can’t eructate = very dangerous
Microbes in rumen produce >10gal gas/hr; Rumen itself is only ~50gal
Horses ferment later in digestive process so gas can come out back end
Frequency in goats < sheep << cows
Expansion of rumen compresses other organs and blood vessels
i.e. Caudal Vena Cava which drains blood from the back of body to return to heart, gets pushed up against spine
Diaphragm/chest cavity compressed —> smash lungs —> can’t take deep breath
Abdominal distention (especially the left side)
“Downer cow” - cow literally can’t stand and collapses; respiration + circulation both impacted
Abdominal pain, Anxiety, Resp. distress
Diagnostics, Choke
Palpation of neck - esophagus lays along left side of trachea/neck
The distention itself is a huge clue
“Ping” in left side
Endoscopy - if NG tube won’t go all the way to stomach, you know theres a blockage
Radiography
Treatment of Choke, Horses
NPO (Nothing Per Os)
Hydrate w/IV fluids - sometime dehydration is actually the cause (less lube)
Gently massage (careful if object is sharp!)
Irrigate with stomach tube
Muscle relaxants/anti-inflammatories
Sedation/anesthesia (to limit anxiety)
Antibiotics - especially tin aspirating/inhaling food
Surgery not commonly necessary
Warm water lavage through NG tube
Antibiotics and NSAIDS
Treatment of Choke, Cows
EMERGENCY
Trocar - insert through rumen —> gas/froth release
“Pop the balloon”
For froth: DSS/mineral oil/veg oil
Once air is released, can deal with any esophageal obstruction
Rumenotomy
Complications of Choke
Pressure necrosis - While the grass sits in the esophagus, it rubs and wares at the ET
Constant pressure can cause the skin to die
More likely to get another blockage in that same place later
Asporation pneumonia
Rupture - increased risk if any pressure necrosis from a previous blockage
Stricture (narrow spot in the esophagus)
Prevention, Choke
Dental health - painful teeth = less chewing = swallowing bigger pieces of food
Avoid: cubes, pellets, feeding after exercise, without water, or < 4hrs post surgery
Slow their eating —> smaller bits + more saliva to lubricate
Ex: Rock/salt block in feeder, hay nets
Keep away from orchards (no whole fruit)
Stomach Disease - Bloat (cows)
Differentiate between Primary and Secondary
Primary = Frothy bloat, due to diet - traps normal fermentation gases in a foam
Secondary = free gas bloat = caused by physical prevention of belching/eructation
Diagnostics, Bloat
Must asses if version 1 or 2
Trocar —> Foamy material = primary ; Gas = secondary
Treatment, Bloat
Primary bloat = always an emergency —> try to decompress with trocar
Administer antifoaming agent
If not enough —> emergency rumenotomy
2ndary: if non emergency —> stomach tube + antifoaming agent
Prevention, Bloat
Avoid young legumes (prebloom = less fiber, more moisture) - alfalfa, clover
Avoid grains (lead to slime/foam)
Feed antifoam
Gastric Dilatation/Volvulus (GVD)
Define the condition/signalment
Whos most affected?
= Stomach distended with gas/food/fluid (G) —> twists (V)
Most common in large/giant breeds with deep, narrow chest cavities
Risk increases with age (starting at 2yrs)
1/3 fatality rate; treat ASAP
Etiology/causes, GDV
Chest conformation
Diet - large/single meals; better to split food into two meals per day
Also avoid feeding near exercise (before or after)
Avoid dry food —> thirsty —> chug water —> extra full stomach = unstable
Avoid elevated food bowls
Volvulus (now pathological, w/o was just bloat)
Stomach twists clockwise
Both inlet and outlet get kinked - can’t swallow OR vomit
Nerve/artery damage —> necrosis
Compression of lungs and veins
Clinical Sings, GDV
Anxious, uncomfortable
Nonproductive retching
Hypersalivating
Abdominal distention/pain
Weakness, collapse (circulatory system and lungs not working properly)
No blood flow —> no ATP production —> no muscle contraction —> “Shock” (collapse)
Pushed up against diaphragm
HR and RR increase to try to compensate for lack of efficient circulation
Diagnostics, GDV
Attempt but failure to vomit
Prolonged capillary refill time (CRT)
Abnormal mucous membranes
Radiographs - gas appears dark on an X-ray; Flesh = gray ; Bone = white
Treatment, GDV
Decompress stomach
Stomach tube if not too twisted; can damage if is tho so be careful
Trocar
Treat circulatory deficiency
IV catheter (thoracic limb preferred due to circulation block) fluids
Surgery - expensive tho so focus on prevention
Can do a gastropexy @ time of neuter; sow stomach to side of abdominal wall
Pain management
Prevention, GDV
Feeding: small amounts, w/o large volumes of water, not near exercise, not in elevated bowl
Try for high quality, non fermentable food
Intestinal Diseases = Canine Parvovirus
Define the condition
Where did it originate?
Who’s most affected?
= Infectious enteritis = inflammation of the Enteron AKA intestines
Originated/mutated from Feline Panleukopenia in 1978
Super contagious!!
Spread via Fecal-Oral Route
Primarily occurs in puppies 6-20 weeks old (window of vulnerability)
Recall: Small intestine = simple columnar ET covering Villi (folds) for increased SA
Virus completely destroys these cells —> Primary Barrier GONE, no more villi visible
Blood and other tissue fluids from body leak out to intestinal tract
Microbes + toxins from food leak into body
Clinical Signs, Canine Parvovirus
Note: Incubation is 3-7 days for the virus; can spread to others unknowingly during this time
Acute onset - quick once it actually starts
Fever, depression, anorexia, vomiting, bloody diarrhea, malodorous stool (stinky!)
Dehydration
Diagnostics, Canine Parvovirus
Specific: ELISA test (fecal) - specifically tests for CVP Ag
Recent vaccination can lead to false positive
Nonspecific: CBC - tests WBC counts, virus attacks bone marrow —> dec counts
Treatment, Canine Parvovirus
Supportive care = help body fight better but on its own
IV fluids - must avoid over-hydration
Antibiotics
Antiemetics (Emesis = vomiting) - V takes energy the animal doesn’t have right now
NPO, then slowly introduce bland diet
Prevention, Canine Parvovirus
Sanitation - Bleach, Parvo specific cleaners, Foot baths
Deworming - decreases susceptibility/harm if infected
Vaccination (special regimen)
How does the puppy vax schedule for Parvovirus differ from others? Why?
Typically vax at 6-8 weeks
For Parvo tho: Start @ 4 weeks —> every 3-4 weeks until 16-20 weeks old (maternal Ab gone)
How? Have developed Modified Live Virus that’s “High virus titer, less attenuated”
Overriedes maternal Ab
Potentially more harmful tho if bad reaction to vacc