MOD 2 - Pediatric Fractures
1/54
Earn XP
Description and Tags
Flashcards about Pediatric Fractures
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
In children, where do most distal forearm fractures occur?
In the distal one-sixth of the forearm.

Why are torus or buckle fractures more common in children?
Due to the elasticity of pediatric bones.

What types of fractures can result from more severe trauma in children?
Greenstick or complete fractures.


What is a common result of pediatric injury mechanisms like FOOSH?
Dorsal displacement of the distal fragment or epiphyseal separation.

What is a torus or buckle fracture?
An incomplete fracture resulting in buckling or folding of the bone cortex.
What age group is most affected by torus fractures?
Children aged 6 to 10 years.

What is the typical cause of a buckle fracture?
FOOSH or direct trauma to the forearm.
How is a torus fracture treated?
Immobilization with a short arm cast.
Are there complications associated with buckle fractures?
No.

What characterizes a greenstick fracture?
Incomplete break with bending and disruption of only one cortex.

What is the mechanism of injury for greenstick fractures?
FOOSH or direct blow to the arm.
What is the treatment for a greenstick fracture?
Manual realignment and immobilization with a cast.
Are greenstick fractures common in any specific age group?
Yes, primarily in children under 10 years old.

What is a bow or plastic deformity in children?
A bowing or bending of the long bone without a visible fracture.

What causes a bow deformity?
Forceful bending of the long bone.
How is bow deformity treated?
Immobilization with a cast.
Are there any complications with bow deformities?
No.

What type of Salter-Harris fracture is most common in the radius and ulna?
Salter-Harris Type II.

What age group most commonly experiences epiphyseal fractures?
Children over 10 years old.
What is the typical mechanism for an epiphyseal fracture?
FOOSH (Fall On OutStretched Hand).
What are possible complications of epiphyseal fractures?
Bone deformity, malunion, and nerve damage.
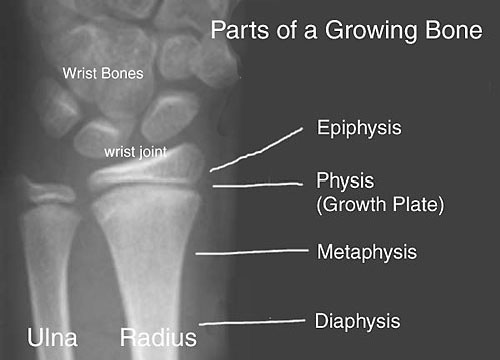
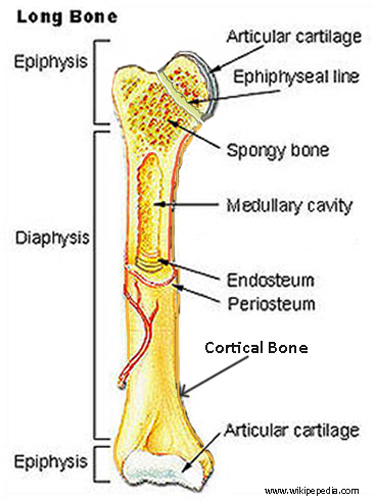
What is the physis in pediatric bones?
The cartilaginous growth plate between the diaphysis and epiphysis.
When do Salter-Harris fractures occur?
Before complete ossification, at the growth plates.
Why are growth plates more prone to injury in children?
They are weaker due to immature ossification.
What is a Salter-Harris Type I fracture?
A transverse fracture through the growth plate with complete separation of the epiphysis.

What are common sites for Type I injuries?
Wrist, ankle, and phalanges.
How is a Type I injury treated?
Reduction and immobilization.
What is the incidence and prognosis of Type I injuries?
6% of Salter-Harris cases; complications are rare.
What defines a Salter-Harris Type II fracture?
Fracture through the growth plate and metaphysis, creating a triangular metaphyseal fragment.

What is the most common site for Type II fractures?
Distal radius.
How common is Type II among Salter-Harris fractures?
75% – it is the most common type.
How is a Type II injury typically treated?
Closed reduction and immobilization.
What is a Salter-Harris Type III fracture?
Fracture through the epiphysis and across the growth plate, often involving a joint surface.

Where do Type III fractures commonly occur?
Distal tibia, distal femur, and distal phalanx.

What is the major concern with Type III fractures?
They involve the joint space and may affect growth and joint function.
How are Salter-Harris Type III fractures typically managed?
Closed reduction with immobilization.
What defines a Salter-Harris Type IV fracture?
A vertical fracture through the metaphysis, growth plate, and epiphysis.

What complication is associated with Type IV injuries?
Premature physeal fusion and joint deformity.

Where are Type IV fractures commonly found?
Distal femur, distal tibia, and distal humerus.
What treatment might be necessary for Salter-Harris Type IV fractures?
Reduction and possibly surgical repair.
What is a Salter-Harris Type V injury?
A compression injury to the growth plate and its blood supply.

How common is Type V?
It is the rarest type – only 1% of Salter-Harris fractures.
What is the primary complication of Type V fractures?
Premature growth plate fusion and limb shortening.
How is Type V treated?
Depends on injury severity; may require realignment and monitoring for growth issues.
Why are pediatric bones more resistant to complete fractures compared to adults?
They are more elastic and pliable, allowing for deformation rather than complete breakage.
What common pediatric fracture shows dorsal displacement of the distal fragment?
Epiphyseal fractures, often from a FOOSH injury.
What are the four major pediatric fracture types based on bone flexibility?
Torus/Buckle, Greenstick, Bow/Plastic deformity, and Epiphyseal fractures.
What does FOOSH stand for, and why is it significant in pediatric trauma?
Fall On OutStretched Hand; it's a common cause of forearm and wrist fractures in children.
What type of fracture usually affects only one cortex of the bone, leaving the opposite side bent?
Greenstick fracture.

Which pediatric fracture type often requires manipulation for proper alignment?
Greenstick fracture.

What does the "corner sign" on imaging indicate?
A small metaphyseal fragment typical of a Salter-Harris Type II fracture.

Why is joint involvement in Salter-Harris Type III and IV fractures clinically significant?
Because it may impair joint function and disrupt the growth plate, leading to long-term complications.
Which Salter-Harris fracture type is most likely to require surgical intervention?
Type IV, due to joint deformity and blood supply damage.

What Salter-Harris type is caused by a crushing or compression force to the growth plate?
Type V.

Why are Salter-Harris fractures concerning in pediatric patients?
They can impair future bone growth and lead to deformity or limb length discrepancies.