CLINICAL CLASSIFICATION & PRESENTATION OF PULP & PERIAPICAL DISEASE
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
what does the apical constriction allow for
the apical constriction allows in apical vessels which maintain pulp vitality
what type of tissue is the pulp
an adaptive tissue - shrinks away from caries/ trauma by laying down dentine
what gives rise to pulpal inflammation
bacteria and their by-products

what does this image show
dentinal tubule with bacteria that has entered it
what is the first irritant that will affect the pulp
the byproducts of bacteria
define sign VS symptom
sign: what you can observe as a clinician
symptom: what the patient complains about
can presenting symptoms be used to make the final diagnosis
presenting symptoms, whilst suggestive cannot be used alone to make the final diagnosis
what information is used to diagnose pulp and periapical disease
patient complaint
history of complaint
clinical examination
special investigations
pulp tests
periapical tests - palpating/ putting pressure on tooth to see patient response
additional tests
radiography
what are anatomical features unique to the dental pulp
unyielding walls
constricted blood source
tooth surrounded by bone
what is the unfavourable result of unyielding walls
unyielding walls
limited volume to accommodate pulpal swelling
no room for expansion
what is the unfavourable result of constricted blood source
constricted blood source
intra-pulpal pressure increases
interferes with blood and lymph flow
there is no other blood supply into the pulp tissue so if blood supply is interrupted, the pulp will lose vitality
what is the unfavourable result of tooth surrounded by bone
tooth surrounded by bone
bone infection invariably results
what are the classifications/ types of pulpal diagnoses
normal pulp
reversible pulpitis
symptomatic irreversible pulpitis
asymptomatic irreversible pulpitis
pulp necrosis
outline normal pulp
pulp is symptom free
‘normal’ response to pulp testing e.g. cold testing results in mild or transient response of no more than 1 or 2 seconds
what is focal pulpitis and how does it arise
focal pulpitis: the initial stage of tooth pulp inflammation where only a portion of the pulp is affected
inflammatory response in the pulp leads to focal pulpitis
what are causes of pulpitis
caries
primary caries
secondary caries
restorative interventions
restorations, crowns etc.
thermal damage
trauma
tooth surface loss
note about the causes of pulpitis
all apart of caries will cause a transient pulpal inflammation
however, without the involvement of bacteria, unlikely that it will be significant and lead to pulpal necrosis
how does pulpal inflammation lead to response to non-painful stimuli
pulpal inflammation will result in a lower threshold to nerve pathway firing, resulting in pain to otherwise non-painful stimuli
outline reversible pulpitis
reversibly inflamed pulp tissue - will heal provided the initial cause of inflammation is removed
discomfort to stimuli such as cold or sweet lasting a few seconds after the removal of the stimulus
subjective diagnosis based on clinical findings and not related to histological status
NO SPONTANEOUS PAIN
what may be found in conjunction with reversible pulpitis
early caries clinically or radiographically
outline symptomatic irreversible pulpitis
irreversibly inflamed pulp tissue with associated symptoms
subjective diagnosis that the pulp is incapable of healing and endodontic treatment is required
no possibility of healing - pulp will inevitably die
tooth either needs to be extracted or RCT
what are pain characteristics of symptomatic irreversible pulpitis
lingering pain
spontaneous
keeps patient awake at night
referred pain
pain may be difficult to localise as the inflammation has not reached the periapical tissues yet
pain will generally never cross the _______
midline
outline asymptomatic irreversible pulpitis
irreversibly inflamed pulp tissue without associated symptoms
subjective diagnosis that the pulp is incapable of healing and endodontic treatment or extraction is required
not a particularly frequent diagnosis
what is an example where a diagnosis of asymptomatic irreversible pulpitis may be made
vital, responsive pulp
extent of caries is too much for the pulp to recover
» asymptomatic irreversible pulpitis
explain what happens if pulpal inflammation is left untreated
untreated inflammation leads to pulp necrosis
invasion of microbes into the resulting pulp space will lead to periapical pathology
initially, just the microbial toxins causes inflammation in the pulp but as infection progresses, the microbes themselves will penetrate the pulpal space
can pulps die/ become necrotic without any symptoms
yes!
many pulps die with no symptoms
a tooth may be asymptomatic but have gone through the necrosis process already
what is the pathway to pulp death
does not necessarily have to follow this
outline pulp necrosis
dental pulp is necrotic and endodontic treatment is indicated
tooth is non-responsive to pulp testing and is asymptomatic
a tooth might not respond to pulp testing for other reasons such as calcification - pulp can calcify as a response to a threat
can pulp necrosis cause periodontitis by itself
pulp necrosis by itself does not cause periapical periodontitis without the presence of bacteria
for what other reason can the pulp become necrotic
the pulp can also become necrotic due to trauma
why do teeth that become necrotic due to trauma get infected quickly
the pulp tissue has died so the tooth no longer has defensive mechanisms that are usually able to respond to any bacteria that attack it
so as soon as that tooth has a crack or gum recession i.e. the dentinal tubules are exposed, the bacteria will have a portal of entry
how does pulp necrosis lead to infection
pulp dies
invasion of the pulp chamber space by microbes
development of an ecosystem and formation of biofilm within the root canal system » infection
toxins from the infection will eventually leak through the apical foramen » periapical pathology
why do bacteria generally stay within the pulpal space
bacteria have something to feed on within the pulp space (the necrotic tissue)
the bacteria are also kept away from the body’s host defences within the pulpal space
however bacteria can progress through the apical foramen » extraradicular infection
what happens at the periapex if it is infected
tissue fluid buildup
inflammatory exudate
immune cells
bony tissue around the tooth apex starts to resorb
terminology to remember
apical periodontitis = periapical periodontitis = peri-radicular periodontitis
peri-radicular: around the root, not necessarily at the apex of the tooth
chronic = asymptomatic
acute = symptomatic
the great majority of periapical periodontitis lesions are ____________
the great majority of periapical periodontitis lesions are asymptomatic
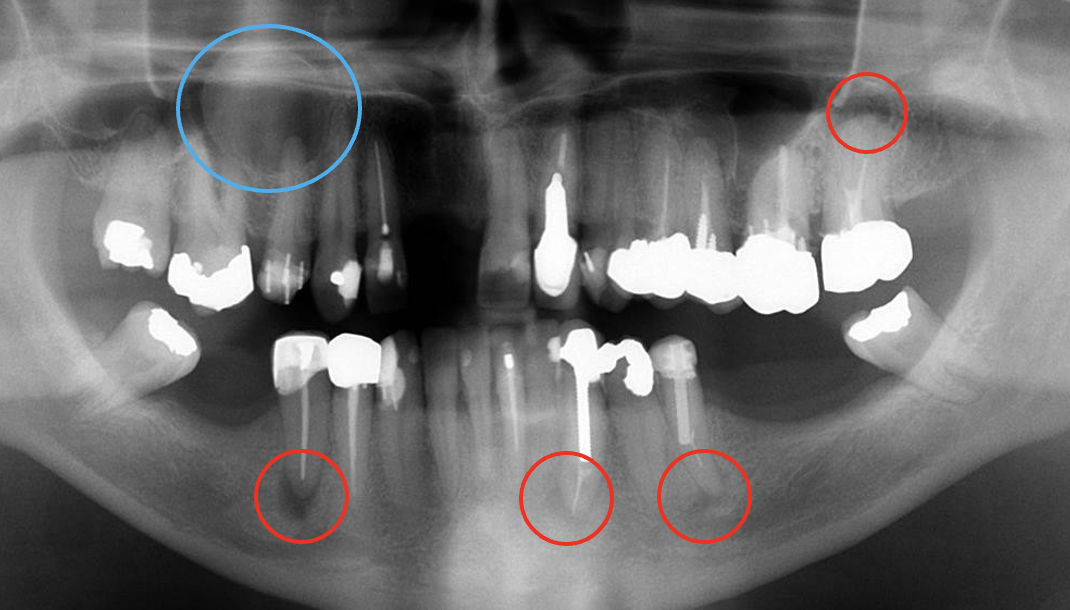
what do the red and blue circles indicate
red circles = periapical pathology
blue circle = cyst
what are the classifications/ types of periapical diagnoses
normal apical tissues
symptomatic (acute) periapical periodontitis
asymptomatic (chronic) periapical periodontitis
acute periapical abscess
chronic periapical abscess
condensing osteitis
outline normal apical tissues
normal apical tissues
tissues are not sensitive to clinical testing
radiographs show normal periapical tissues
outline symptomatic (acute) periapical periodontitis
symptomatic (acute) periapical periodontitis
inflammation has spread to the periapical tissues resulting in tenderness to pressure
patient is able to localise the source of the pain to a specific tooth - infection has now reached PDL which has mechanoreceptors that tell patient the source of pain
radiographic changes may or may not be visible
outline asymptomatic (chronic) periapical periodontitis
asymptomatic (chronic) periapical periodontitis
inflammation has spread to the periapical tissues
the inflammation is low grade and presents with no symptoms
radiographic changes appear as a periapical radiolucency
outline acute periapical abscess
acute periapical abscess
inflammation of the periapical tissues with pus formation and swelling
rapid onset
spontaneous pain
extreme tenderness of tooth to pressure
patient may experience malaise, fever and lymphadenopathy
radiographic changes may or may not be visible
outline chronic periapical abscess
chronic periapical abscess
inflammation of periapical tissues with intermittent discharge of pus through an associated sinus tract
usually associated with little or no discomfort because the pus is able to escape (no pressure buildup)
radiographic changes usually appear as a periapical radiolucency
usually presents as a little red lump just above the tooth

outline condensing osteitis
condensing osteitis
diffuse radiopaque lesion representing a localised bony reaction to a low grade inflammatory stimulus usually seen at the apex of the tooth
increased mineralisation around apices of teeth
stimulus will often have been present for a long time
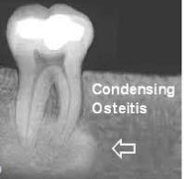
is the tooth vital or non-vital in condensing osteitis
tooth may still be vital but chronically inflamed
tooth can also be non vital and unresponsive to special testing
radiographic examples of periapical pathologies
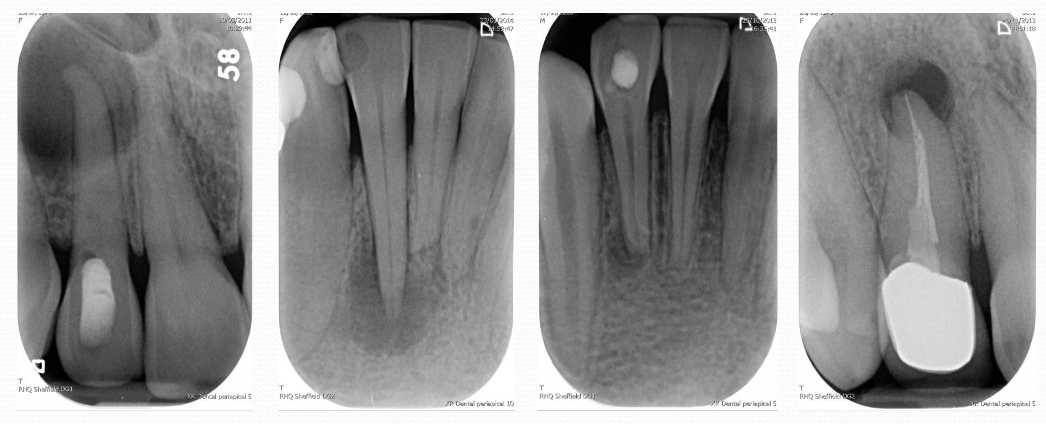
note!
important to come up with both a pulpal and a periapical diagnosis!