Eating Disorders
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
Eating disorders
- widely accepted as a serious mental illness
- wide spectrum
- arise from complex interaction between environmental, societal, developmental, psychosocial, genetic, & biologic factors
- median age of onset 18-21 years, 12-13 years
3 most prevalent forms of eating disorders
- anorexia nervosa (AN)
- bulimia nervosa (BN)
- binge-eating disorder (BED)
- treatment remains difficult (pharmacologic intervention & psychotherapy)
According to DSM-5, there are categories of...
- Specified and Unspecified Feeding & Eating Disorders
- apply to cases where sx result in distress, but DO NOT meet full diagnostic critera for any feeding or eating disorders
Etiology of eating disorders
- likely combo of genetic, biologic, developmental and environmental factors
Anorexia nervosa
Restriction of energy intake that leads to low bodyweight and self-evaluation that is influenced by perceptions of weight and body shape
Sx of anorexia nervosa
- Obsessions/fears about eating & gaining weight
- “Feeling full” even though have eaten very little
- Denial of symptoms, low self-esteem
- Lack of self-control
Signs of anorexia nervosa
- Weakness, lethargy
- Amenorrhea
- Vomiting
- Restricted food intake
- Constipation, abdominal pain
- Bradycardia, hypotension
- Delayed sexual development
Laboratory abnormalities of anorexia nervosa
- Hypo many things
- QT interval prolongation
- bradycardia
DSM-5 further classifies AN as either __________________ or ___________________
- restricting type
- binge eating/purging type
Severity of AN is based on __________ in adults and ___________________ in children/adolescents
- BMI
- BMI percentiles
DSM-5 Diagnostic Criteria for AN
- evaluated for behavior the past 3 months of restriction binge eating/purging
- BMI determines severity of AN
BMI and AN severity
Mild:
Moderate:
Severe:
Extreme:
Mild: ≥17 kg/m2
Moderate: 16-16.99 kg/m2
Severe: 15-15.99 kg/m2
Extreme: <15 kg/m2
Bulimia nervosa
- Binge eat and stop when they have abdominal pain or self-induced vomiting
- Pattern of severe dieting followed by binge eating episodes
- Concerned about body image but do not have the drive to thinness
Symptoms of bulimia nervosa
- Do not eat regular meals
- Do not feel satiety at end of meal
- May use purging methods such as laxatives for weight control
- Have guilt & depression after binges
- Social isolation can result from frequent binging
Signs of bulimia nervosa
- Binging, vomiting, erosion of dental enamel, abdominal pain, upper end of normal body weight or slightly overweight, frequent weight fluctuations
Laboratory abnormalities in bulimia nervosa
- hypokalemia
- hypochloremic metabolic acidosis
- elevated serum amylase
Clinical presentation of bulimia nervosa
- core feature is recurrent episodes of binge-eating
- # of binging episodes/week determines severity
to meet DSM-5 criteria, binging/compensatory behaviors must occur on average at least ......
once weekly for 3 months
DSM-5 further differentiates BN by...
PURGING TYPE or NON-PURGING TYPE
DSM-5 Diagnostic Criteria: # of binging episodes/week
Mild:
Moderate:
Severe:
Extreme:
Mild: avg. 1-3 episodes/week
Moderate: 4-7 episodes/week
Severe: 8-13 episodes/week
Extreme: 14 or more episodes/week
Binge eating disorder
- Repeated episodes of binge-eating that include lack of self-control and eating an amount of food beyond normal
- Episodes of binge-eating may include rapid eating, sense of fullness to point of being uncomfortable, eating when not hungry, and sense of self-disgust ,depression and guilt
Symptoms of binge eating disorder
- Episodes of binge-eating
- Lack of self-control
- Rapid consumption of food
- Feeling full and eating when not hungry
- Isolation and guilt/depression
Signs of binge eating disorder
- Obesity
- Hx of weight loss followed by weight gain
- Binge-eating w/o compensatory purging
- Psychiatric and medical conditions (GERD, HTN) are not uncommon
Laboratory abnormalities in binge eating disorder
- elevated lipids, glucose, and hemoglobin A1c
- abnormal electrolytes
- increased weight
Clinical presentation of binge eating disorder
recurrent episodes of bingeing w/o compensatory behaviors associated w/ AN or BN
DSM-5 diagnostic criteria requires recurrent episodes of binge eating and must be associated with at least three of the following:
1. Eating more rapidly than normal
2. Eating until feeling uncomfortably full
3. Eating large amounts of food when not physically hungry
4. Eating alone because of embarrassment of how much is being eaten
5. Feeling disgusted with oneself, depressed or guilty after the episode
Severity of BED is determined by the...
number of binge-eating episodes per week
Severity levels of BED
1. Mild = 1-3 episodes per week
2. Moderate = 4-7 episodes per week
3. Severe = 8-13 episodes per week
4. Extreme = 14 or more episodes per week
Eating problems can also be a sign of other mental disorders (depression, OCD, schizophrenia). What are major differences?
- Overriding drive for thinness
- Disturbed body image
- Increased energy directed at losing weight
- Binge eating episodes that are relatively specific for eating disorders
Most patients with eating disorders experience relief of psychiatric symptoms on _______________
refeeding
Cardiac complications of eating disorders
- Fatal CV collapse due to refeeding syndrome
Metabolic complications of eating disorders
- Electrolyte disturbances
- Dehydration
- Acute and chronic renal failure
GI/Hormonal complications of eating disorders
- GI, oropharyngeal, and dental complications
- Lethargy and fatigue are frequent
- Hormonal changes such as irregular menses, osteoporosis and osteopenia (complication of suppressed estrogen)
Other complications of eating disorders
- Brain atrophy
- Presence of Russell’s sign
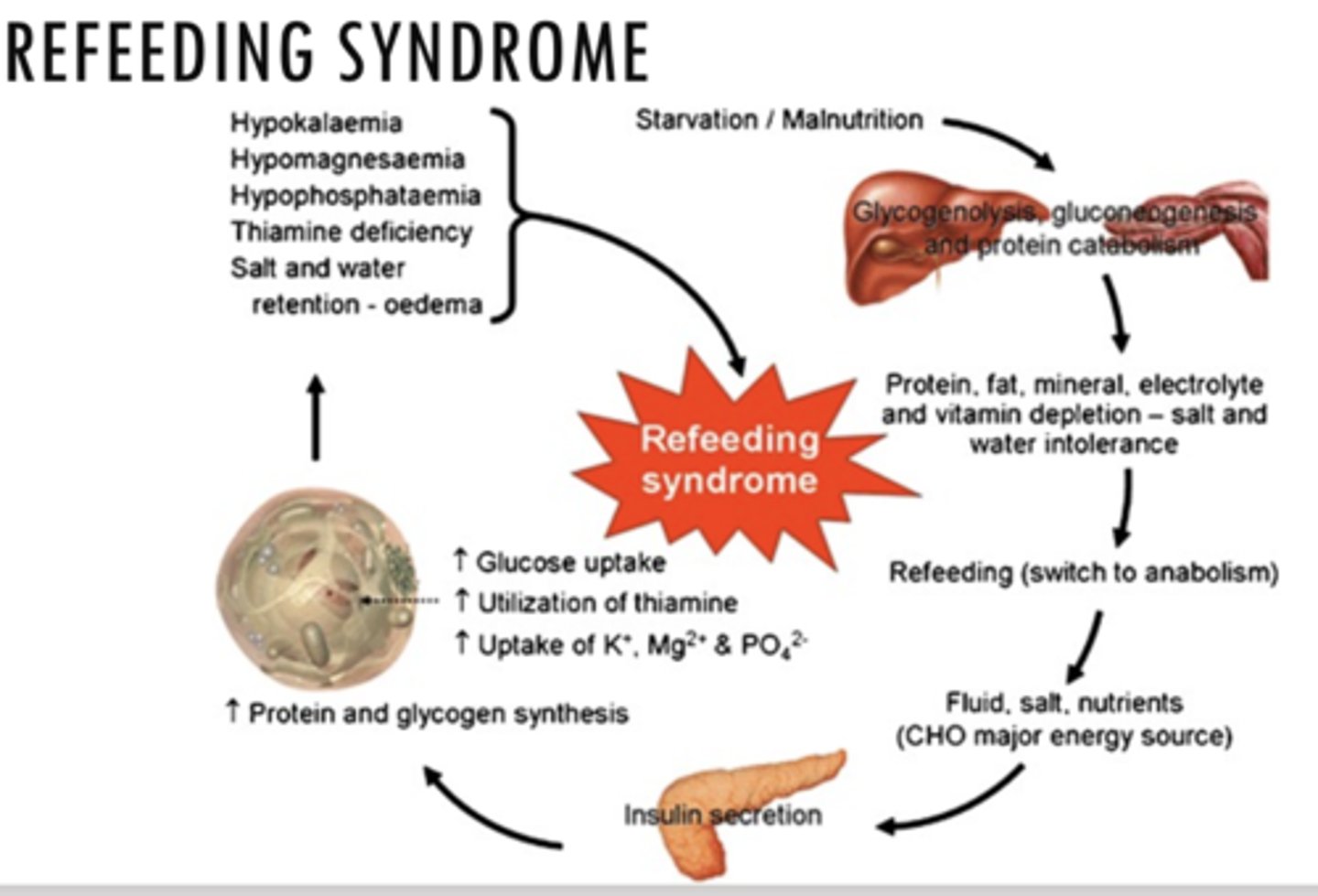
What is refeeding syndrome?
severe electrolyte & fluid shifts associated w/ metabolic abnormalities in malnourished pts undergoing refeeding (whether PO, enterically or parenterally)
- potentially lethal
- electrolyte disturbances
How to prevent refeeding syndrome?
- can take place w/i first few days of refeeding, cardiac complications w/i the first week and delirium
- calorie repletion should be given slowly, particularly the first week at about 20 kcal/kg of body weight per day
Treatment goals of eating disorders
- Reduce distorted body image
- Restore and maintain healthy body weight
- Establish normal eating patterns
- Improve psychological, psychosocial, and physical problems
- Resolve contributory family problems
- Enhance patient compliance
- Prevent relapse
- Weight loss, specifically for BED patients
General approach to treatment
- individualized
- require a team of clinicians
- important to have adequate support system
- CRITICAL first step is ot determine the severity of illness, which drives the intensity & setting for delivery of care
T/F: Medications are part of the comprehensive treatment strategy but are rarely recommended as the sole treatment
TRUE
Nonpharm treatment of anorexia nervosa
- standard therapy consists of nutritional rehabilitation & psychotherapy
- at least 6 months of psychotherapy is preferred; evidence has shown at least 1 yr duration
- CBT, nutritional counseling, family therapy
- Oral feeding, initially w/ liquid formulas most common approach to weight restoration
- in severe cases where pt refuses to eat, nasogastric feeding is preferred over IV bolus dosing
Cognitive Behavioral Therapy (CBT)
- helps pt overcome distorted thinking including self-worth as measured by body image
- teaches pts how to use strategies besides eating to cope
Pharmacologic therapy for anorexia nervosa
- Currently NO FDA-approved medication for AN
- used only for pts who do not respond to initial, standard treatment
If medications are utilized (off-label), start at....
small dose due to low pt weight
What is the primary goal of treatment in medically stable pts?
WEIGHT GAIN --> antipsychotics, specifically Olanzapine 2.5-10 mg daily
Agents used for anorexia nervosa
- if used, SSRI, fluoxetine
- metoclopramide
- benzodiazepines
- estrogen replacement
- supplementation w/ zinc
- olanzapine 2nd gen antipsychotic
T/F: Antidepressants currently have no role in the acute treatment of AN, unless there is another clinical indication present
TRUE, ineffective especially in cases where pt is below their expected weight
If antidepressant is used, what is preferred?
- preferred SSRI
- fluoxetine 20 mg PO QD, increase to 60 mg QD based on response
Metaclopromide in AN
- helpful in reducing bloating, early satiety, & abdominal pain
- does NOT affect weight gain
Benzos in AN
- low dose, short acting
- helpful for severe anxiety, limiting eating
Estrogen replacement in AN
restore mesnes (refeeding typically preferred)
Supplementation w/ zinc in AN
may assist w/ weight restoration
Olanzapine in AN indication (off-label)
- acutely ill pts who receive 1st line treatment w/ nutritional rehab plus psychotherapy but do not gain weight
- no compelling evidence that other antipsychotics (risperidone, quetiapine, or aripiprazole) help restore weight in AN
MOA of olanzapine includes the antagonism of multiple neuronal receptors, including
- dopamine receptors in brain
- serotonin receptors, alpha-1-adrenergic receptors
- histamine receptor H1
- multiple muscarinic receptors
Side effects of olanzapine
- generally well-tolerated
- dizziness
- orthostatic hypotension
- weight gain
- EPS
- dry mouth
US boxed warning for olanzapine
increased mortality in elderly pts w/ dementia-related psychosis
Nonpharm treatment for bulimia nervosa
- Outpatient-based treatment is most often recommended
- nonpharm strategies similar to those used in AN
- CBT consisting of 16-20 sessions over a 4-5 month period
- nutritional counseling, planned meals, self-monitoring
- family therapy in bulimic pt is less critical than w/ AN (pts tend to be older)
What pharmacologic agents are used in bulimia nervosa?
- antidepressants in the acute & maintenance phases of BN adjunctively w/ nonpharm approaches
- opitmal duration of treatment after response is poorly defined, although most clinicians treat for 9 months-1 year then reevaluate
Fluoxetine (SSRI) in BN
- FDA approved for BN (only one)
- inhibits CNS neuron serotonin reuptake, minimal or no effect on reuptake of NE or dopamine
- initial 10-20 mg PO QD, may increase based on response
- also used off-label in BED
Side effects of fluoxetine
- decreased libido
- diarrhea
- nausea
- sexual disorder
- anxiety
- drowsiness
- pharyngitis
Sertraline (SSRI) in BN
- off-label use
- inhibits CNS neuron serotonin reuptake, minimal or no effect on reuptake of NE or dopamine
- inital 50 mg PO QD, may increase
- also used off-label in BED
Side effects of sertraline
- diarrhea
- nausea
- dizziness
- drowsiness
- fatigue
- insomnia
US boxed warning of fluoxetine & sertraline
increased risk of suicidal thoughts & behavior in pts <24 y/o
Nonpharm treatment of Binge-eating disorder
- individual & group CBT, non-pharm treatment of choice
- goal is to reduce number of binge eating episodes, though not likely to significantly improve weight loss
- weight loss focused treatment programs, most effect for weight reduction
Pharmacologic treatment of BED
- stimulants
- antidepressants
- anticonvulsants
Stimulant to treat BED
- lisdexamfetamine, FDA approved for treatment of moderate-severe BED
- reductions in # of binge days per week
- improvement in obsessive-compulsive symptoms
Antidepressants to treat BED
- SSRIs used: citalopram, escitalopram, fluoxetine, sertraline
- SNRIs used: atomoxetine, venlafaxine
- demonstrated efficacy in binge eating, decreasing BMI< and improving depressed mood during acute phases
Anticonvulsants in BED
- Topiramate shown to reduce binge frequency, body weight, BMI
- zonisammide alone & in combo w/ CBT
lisdexamfetamine (Vyvanse) in BED
- FDA-approved for moderate-severe BED (only one)
- prodrug of dextroamphetamine. blocks reuptake of NE and dopamine into presynaptic neuron, increases release of monoamines into the extraneuronal space
- 30 mg PO qAM
Side effects of lisdexamfetamine
- GI sx (NV, stomach/abdominal pain, loss of appetite)
- weight loss
- dry mouth
- HA
- insomnia
SNRIs & SSRIs in BED
- demonstrated efficacy as monotherapy
- reduces binge eating
- decreases BMI
- improves depressed mood during acute phases
- can be used in combo w/ CBT to augment response
topiramate anticonvulsant in BED
- alternative/off-label use for BED
- blocks neuronal voltage-dependent Na+ channels, enhances GABA(A) activity, antagoniszes AMPA/kainite glutamate receptors, & weakly inhibits carbonic anhydrase
- initial 25 mg PO QD, increase incrementally
Side effects of topiramate
- endocrine/metabolic (weight loss)
- GI (abdominal, nausea)
- CNS (dizziness, drowsiness, memory impairment)
Contraindications of topiramate
recent alcohol use w/i 6 hours before or after administration (XR formulation)
Therapeutic outcomes of anorexia nervosa
- Reduction in frequency and severity of abnormal eating habits (recording in diary)
- Normalized exercise patterns and lab tests
- Sustained weight close to age-matched normal values (weekly weigh-ins)
- Quality of life
Therapeutic outcomes of bulimia nervosa
- Reduction in frequency and severity of binge-purge episodes, laxative use
- Normalized exercise patterns and lab tests
- Response to antidepressants usually occurs within 4-8 weeks after initiation; Suicidality assessments
- If pt relapses after medication discontinuation, restart
- Quality of life
Therapeutic BED
- Reduction in frequency and severity of binge-eating episodes
- Weight loss close to age-matched normal values
- Quality of life
T/F: Eating disorder patients in outpatient setting present a challenge. Prescriptions should be limited to small supplies (Impulsivity --> suicide)
TRUE
Which of the following is/are required when considering a diagnosis of anorexia nervosa?
A. Restriction of energy intake leading to low body weight
B. Undue influence of body shape on self-evaluation
C. Behavior that interferes with weight gain
D. All of the above
D. All of the above
Which of the following is an FDA-approved agent for the treatment of binge-eating disorder?
A. Escitalopram
B. Lisdexamfetamine
C. Olanzapine
D. None of the above
B. Lisdexamfetamine
TJ is a 23-year-old female diagnosed with bulimia nervosa. Which characteristic below does not fit with the diagnostic criteria for BN?
A. Average height and weight at presentation, but has periods where she fluctuates between overweight and underweight
B. Presenting symptoms of anxiety, history of substance abuse, and difficulty with personal relationships
C. Several times a month, she eats excessively and feels very guilty about it afterward
D. Lack of concern over her body image
D. Lack of concern over her body image