health psych terms
1/116
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
117 Terms
PHE
Patient Health Engagement Model
PHE model suggests
patient engagement is a developmental process involving a recovered patient’s capacity to plan realistic life projects (ie, meaningful life aims that the patient might generate unless living with the disease condition) and to be goal oriented – even if living with a disease.
four developmental phases PHE model
blackout, arousal, adhesion, and eudaimonic project — NOT SOMETHING LINEAR
blackout phe model
feelings of psychological vulnerability connected to a critical event, such as a disease diagnosis, a new symptomatology, a disease relapse, and the need to assume new lifestyles to manage the health condition
→ To overcome the blackout phase, patients primarily need emotional and psychological support in order to adjust to their new health condition and develop a new sense of agency and control and sense of effectiveness concerning their health management.
arousal phe
arousal have acquired an initial awareness of their health condition, but still have superficial knowledge about how to manage it in an effective way
Adhesion phe
developed a good acceptance of their disease and have overcome the major psychological stress connected to the disease onset. They report being more aware of their health status and of its impact on their lives and life habits. Patients are increasingly knowledgeable about how to effectively manage their disease and treatment. However, patients undergoing the adhesion phase are not fully autonomous in their disease management in terms of medical prescription (both life habits and therapeutic regimens), and they frequently experience trouble when something in their life context changes (ie, going on holiday, working life changes, and so on). This happens because patients in this phase are not totally aware of the reasons behind the medical prescriptions; they appear to be formally compliant with their health providers’ requirements, but risk failing when some variables in their life change. Although patients in this phase still tend to rely frequently on their health care professionals’ advice and support, they also start to perceive the importance of playing an active part in their health care journey.
TLDR; basically managing but not being with it to the longest extent to truly understand like with medications
Eudaimonic project PHE
patients become totally aware of their disease and its implications in terms of changed life habits and therapeutic requirements, they are able to become active agents in reaching a positive and satisfying quality of life, unless living with a disease condition. Patients experiencing the eudaimonic project phase have accepted “patient identity” as one of the many features in a person’s life. In the “eudaimonic project” phase, patients are able to integrate their health and disease management into their life goals. This reframed perspective of patients toward their health condition makes them able to embrace a more positive and satisfactory approach to their life.
transtheoretical model aka
stages-of-change model
The Transtheoretical Model maintains that individuals change their health behaviors in different stages.
They pass from not being concerned to change their behaviors (pre-contemplation stage) to starting to think about them (contemplation) to finally enacting them (action stage) and fully engaging in those behaviors in the long run (maintenance).
THIS IS A STAGE THEORY
CHE model
caregiving health engagment model
CHE model stages
denial, hyper-activation, drowning, balance
denial stage CHE
lots of negative emotions — refuses to acknowledge what happened, avoidance, anger, taking a step back
hyper-activation CHE
super attentive of everything, montoring every single sign, very muchs till leans on clinicians
drowning CHE
insecure and psychologically tired, but able to integrate caregiving into their life, feels as though they can participate in speaking about health and symptoms, UNBALANCED
Balance CHE
full autonomy in responding to loved ones
feels capable
good relationship with care team
cobb ? three health related behaviors
health, illness, and sick role
health behavior
behavior aimed to prevent disease
illness behavior
•behaviour aimed to seek remedy (e.g., going to the doctor)
sick role behavior
was any activity aimed to get well (e.g., taking prescribed medication, resting).
matarazzo health behaviors
health impairing habits and health protective behaviors — Matarazzo distinguished between those behaviours that have a negative effect (the behavioural pathogens, such as smoking, eating foods high in fat, drinking large amounts of alcohol) and those behaviours that may have a positive effect (the behavioural immunogens, such as tooth brushing, wearing seat belts, seeking health information, having regular checkups, sleeping an adequate number of hours per night).
health impairing habits
which he called ‘behavioural pathogens’ (e.g., smoking, eating a high fat diet)
health protective behaviors
which he defined as ‘behavioural immunogens’ (e.g., attending a health check).
adherence in behavior terms
• a person’s ability and willingness to follow recommended health practices. R. Brian Haynes (1979) suggested a broader definition of the term, defining adherence as “the extent to which a person’s behavior (in terms of taking medications, following diets, or executing lifestyle changes) coincides with medical or health advice” (pp. 1–2).
compliance to health behaviors
negative connotation — basically bare minimum like taking drugs
six basic methods of measuring patient adherence are available:
(1)ask the practitioner,
(2)ask the patient,
(3)ask other people,
(4)monitor medication usage,
(5)examine biochemical evidence
(6)use a combination of these procedures
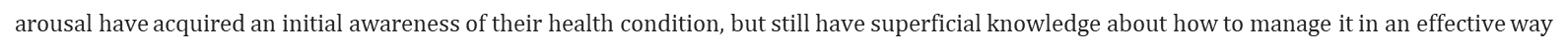
data on non-adherence
More recent reviews confirm the problem of nonadherence, estimating nonadherence to medication regimens at nearly 25% (DiMatteo, 2004b). Adherence rates tend to be higher in more recent studies than in older ones, but many of the factors identified in Sackett and Snow’s (1979) review continued to be significant predictors of adherence. Medication treatments yielded higher adherence rates than recommendations for exercise, diet, or other types of health-related behavior change. However, DiMatteo’s analysis revealed that not all chronic conditions yielded equally low adherence rates. Some chronic conditions, such as HIV, arthritis, gastrointestinal disorders, and cancer, showed high adherences rates, whereas diabetes and pulmonary disease showed lower adherence. Nevertheless, failure to adhere to medical advice is a widespread problem, with one prominent review stating that “effective ways to help people follow medical treatments could have far larger effects on health than any treatment itself” (Haynes et al., 2008; p. 20)
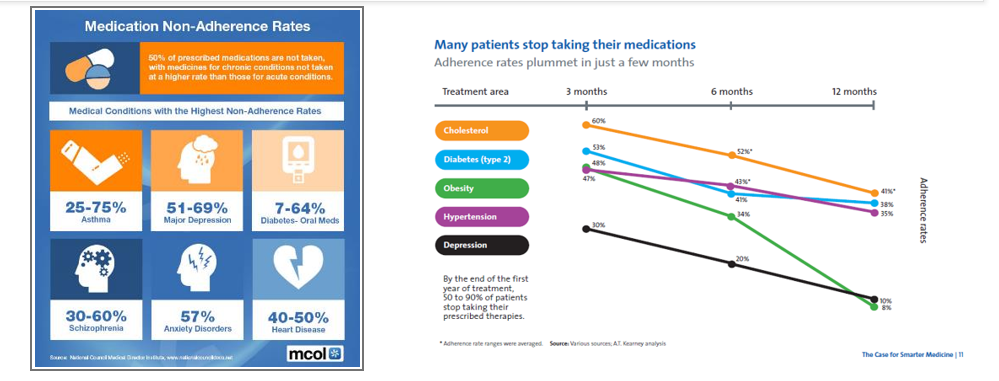
medical adherence factors
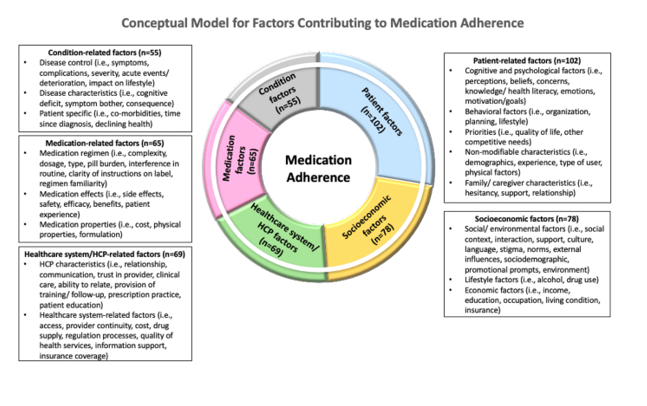
illness cognition
can be described as a patient's perception, interpretation, and understanding of the disease and its treatment. Illness cognitions refer to the common-sense model of illness representations from Levental
patience focuses adherence model
theories of health behaviors categories
continuum theories and stage theories
Continuum theories
the first class of theories developed to understand health behavior and include
●
1.health belief model (Becker & Rosenstock, 1984)
●
2.self-efficacy theory (Bandura, 1986, 1997, 2001)
●
3.theory of planned behavior (Ajzen, 1985, 1991)
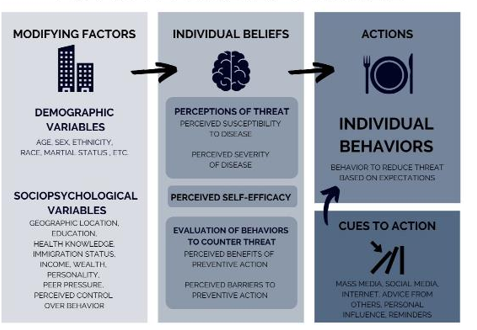
health belief model
continuum — includes the concepts of perceived severity of the disease, personal susceptibility, and perceived benefits of and barriers to health-enhancing behaviors. The health belief model has only limited success in predicting health-related behaviors
theory of planned behavior
continuum — intentional behavior, with the predictors of intentions being attitudes, perceived behavioral control, and subjective norms. Perceived behavioral control and intentions tend to be the strongest predictors of adherence. Subjective norms also predict behavior, but mainly among adolescents and for risk-taking behaviors

self efficacy theory
??? continuum
stage theories of health behavior
•Most importantly, stage models propose that people pass through a series of discrete stages as they attempt to change their behavior. In this way, stage models seem to better describe the processes by which people change their behavior than continuum models.
•Stage models also suggest that different variables will be important depending on what stage a person is in. In this way, stage models differ from continuum models, as people in different stages should benefit from different types of interventions.
•Stage models suggest that interventions should use a tailored, stage-matched approach, by only addressing the variables relevant in the person’s current stage. Thus, the effectiveness of stage-matched interventions depends in part on how well practitioners can classify people into discrete stages. One criticism of the transtheoretical model is that the five stages do not represent discrete stages, and people in different stages may be more similar to each other than the theory suggests. This may explain why there is only mixed support for stage-matched interventions based on the transtheoretical model.
intention - behavior gap
Many people fail to adhere because their intentions do not translate into behavior
behavioral willingness, which represents a person’s willingness to engage in risky behaviors at a given moment
not planning accurately
pro- environemental behavior
defined as all possible actions aimed at avoiding harm to and/or safeguarding the environment (Steg and Vlek, 2009), either performed in public (e.g., participation in environmental movements) or private domains (e.g., recycling; Hadler and Haller, 2011).
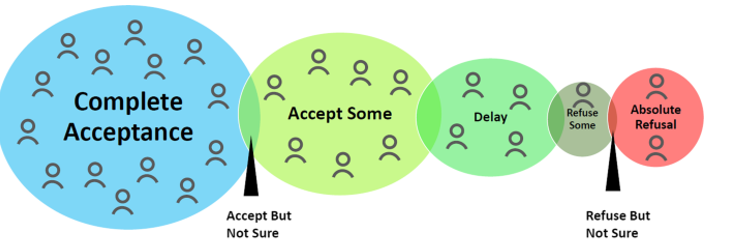
vaccine hesitancy continuum
trends driving change in healthcare landscape

health disparity examples
•Infant mortality: Babies born to Black women in the United States die at more than double the rate of babies born to white women.
•Dementia: Black people also have the highest risk for dementia, and are twice as likely to develop Alzheimer’s disease than whites in the United States.
•Cancer: People with lower incomes and education levels are more likely to get cancer and to die from it compared to their more affluent peers, and that gap appears to be widening.
•Obesity: Even after controlling for family income, rates of obesity in Black women and Mexican-American men are substantially higher than in other races or ethnic groups.
•Smoking: Native American/Alaska Native men and women have disproportionately higher rates of smoking, as do individuals living below the federal poverty level and those who are unemployed.
•Binge drinking: Young white men are more likely than other groups to binge drink (5+ drinks in a two-hour period).
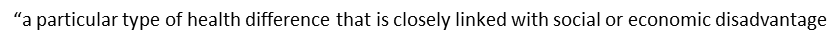
“a particular type of health difference that is closely linked with social or economic disadvantage
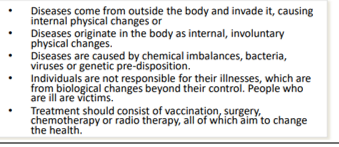
Today, three types of definitions of health seem to be possible and are used.
•The first is that health is the absence of any disease or impairment.
•
•The second is that health is a state that allows the individual to adequately cope with all demands of daily life (implying also the absence of disease and impairment).
•
•The third definition states that health is a state of balance, an equilibrium that an individual has established within himself and between himself and his social and physical environment. This approach to health includes biological, psychological, and social influences. This definition holds that many diseases result from a combination of factors such as genetics, physiology, social support, personal control, stress, compliance, personality, poverty, ethnic background, and cultural be
The Global Wellness Institute (GWI) defines wellness as
active pursuit of activities, choices, and lifestyles that lead to a state of holistic health. •First, wellness is not a passive or static state, but rather an “active pursuit” that is associated with intentions, choices, and actions. Second, wellness is linked to.
the COVID-1holistic health – that is, it extends beyond physical health and incorporates many different dimensions, including physical, mental, emotional, spiritual, social, and environmental dimensions9
people have become more aware of their surroundings etc
shifts in mindset post covid
1.Self-care for self-preservation and survival.
2.Prevention as a lifestyle and a public health priority.
3.Wellness and science must move toward each together.
4.Leaning into nature for nourishment and healing.
5.Balancing physical and virtual connections.
6.Mental well-being takes center stage.
7.A global values reset.
digital health
•mobile health (mHealth), health information technology (IT), wearable devices, telehealth and telemedicine, and personalized medicine.
One Health
approach that recognizes that the health of people is closely connected to the health of animals and our shared environment
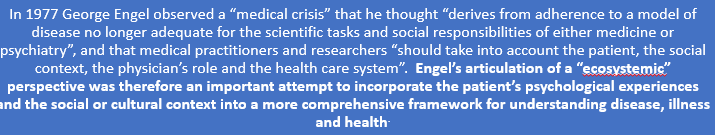
biomedical model
1977 George Engel
shared decision making
SDM — a process in which clinicians and patients work together to select tests, treatments, management or support packages, based on clinical evidence and the patient's informed preferences. It involves the provision of evidence-based information about options, outcomes and uncertainties, together with decision support counselling and a system for recording and implementing patients’ informed preferences
empowered patient
patients take control over their lives — being vocal and making best decisions for themselves
(meaningful) patient involvement
healthcare consumerism
actions to make more informed decisions and proactive behaviors for their health
actions for healthcare consumerism
health consumer
people who use health services, as well as their families and carers.
why not use patients?
•A ‘consumer’ tends to choose and get involved in decision making whereas traditionally a ‘patient’ tends to be a person who receives care without necessarily taking part in decision making.
•Also, the term ‘consumers’ includes carers who often have an important role in health care decision-making and caregiving.
•Finally, many health programs and services don’t use the term ‘patient’ anyway and refer to ‘clients’ or even ‘residents’ (in the case of live-in facilities).
health consumer representative
•health consumer who has taken up a specific role to provide advice on behalf of consumers, with the overall aim of improving health care.
•health consumer representative may be nominated by and accountable to a consumer organization.
•Usually, the role is working with a health service (or patient organization) and is often in a volunteer capacity. Sometimes the role comes with a small payment to cover the consumer’s costs.
expert patient
•has been developed in the last two decades to define a patient who has a significant knowledge of his/her disease and treatment in addition to self-management skills.
, but to also act as educators for other patients and as resources for the last, provide feedback on care delivery, and be involved in the production and implementation of practice guidelines, as well as in the development and conduct of research initiatives.
health psychology four goals
üTo promote and maintain health
üTo prevent and treat illness
üTo determine the causes and diagnostic correlates of health, illness and related dysfunction
üTo improve health care systems and health policy
health psych definition
area of psychology that discovers how consumers’ health and illness behaviors, and decisions are influenced by biological, psychological, and social factors (Cherry, 2020a). This is aimed to discover how people’s attitudes, values, lifestyles and personalities shape healthcare consumers’ motivations for behavior change and communication preferences. Segmenting people by these characteristics allows you to target and deliver communications that resonate more effectively and increase the likelihood of behavior activation. Health psychology emphasizes the role of psychological factors in the cause, progression and consequences of health and illness. The aims of health psychology can be divided into (1) understanding, explaining, developing and testing theory, and (2) putting this theory into practice
The overall focus is on the contributions of behavioral science to the promotion of health and the treatment of illness. Topics covered include determinants of health-related behaviors (e.g., smoking, diet, sustainable behaviors), individual and population approaches to behavior change, stress and coping, and adjustment to illness.
current issues in health psych
•Improving daily nutrition
•Improving recovery
•Preventing illness
•Reducing risky sexual behaviors
•Smoking cessation
•Stress reduction
•Teaching coping skills
•Understanding the effects of illness
•Weight management
•Sustainable behaviors
•Pro-environmental behaviors
•Responsible consumptions
….
summary slide (flip to read)
health as
a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity
life course perspective
the view of life as an integrated continuum of different stages. It explores how different social determinants operate or accumulate as advantages or disadvantages over different stages of the lifecycle. What happens in different stages of life can affect health over the entire lifespan ; however, the recognition of early-life influences on chronic diseases does not imply deterministic processes that negate the utility of later-life intervention.
health across lifespan is influenced by
early life experience
developmental issues that determine health
around biological maturation, including the development of the immune and endocrine systems; cognitive understanding and language development; and attachment and social learning. Influences on these developmental processes, whether biological, psychological or social, and their interactions, can determine the degree to which vulnerability or resilience to ill health emerge.

blues zones
Okinawa, JapanSardinia, ItalyNicoya Peninsula, Costa RicaIkaria, GreeceLoma Linda, California
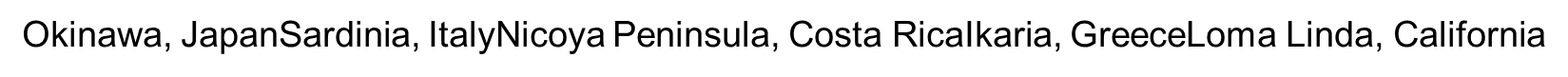
Common Lifestyle Habits ("Power 9"):
•Move Naturally – Engage in regular, low-intensity physical activity.
•Purpose – Maintain a sense of purpose in life.
•Downshift – Incorporate routines to shed stress.
•80% Rule – Stop eating when 80% full.
•Plant Slant – Favor plant-based diets.
•Wine at 5 – Moderate alcohol consumption, especially wine.
•Belong – Participate in faith-based communities.
•Loved Ones First – Prioritize family.
•Right Tribe – Surround oneself with supportive social circles
caregiving health has also
been thought of recently think of the CHE
SDH
The social determinants of health
•are the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies and political systems.

Work, and its associated conditions, is one of the key
key social determinants of health.
Environmental Psychology
examines the reciprocal relations between people and the environment considered at all scales. Emphasis is upon enhancing human-environment relations by improving investment in the sensitive design of built settings
— A number of specific environmental issues can impede human health and wellness. These issues include chemical pollution, air pollution, climate change, disease-causing microbes, lack of access to health care, poor infrastructure, and poor water quality.
Biopsychosocial model
considers the influence of multiple factors on illness or wellness
•
•Biological (genetics, infectious agents, environmental toxins, and immune responses)
•Psychological (personality, attitudes, stress levels, behavioral habits, and coping strategies)
•Social (support systems, medical care, health education, and social roles)
Salutogenic model of health
to an approach to wellness focusing on health and not on disease (pathogenesis).
salutogenic two concepts
the Sense of Coherence and the General Resistance Resources…
Sense of Coherence
Salutogenic model of health —the ability to manage the resources one has in order to cope with the innumerable stressors of life, and a way of viewing or perceiving life as: comprehensible, manageable and meaningful.
— •Comprehensible
Cognitive Component: “The stimuli deriving from one’s internal and external environments in the course of living are structured, predictable and explicable”.
•
•Manageable
Instrumental or Behavioural Component: “The resources are available to one to meet the demands posed by the stimuli”.
•
•Meaningful
Motivational Component: “These demands are challenging, worthy of investment and engagement”.
General Resistance Resources
salutogenic models of health — the biological, material and psychosocial factors that make it easier for people to perceive life as understandable, structured and consistent”
—
of General Resistance Resources include:
•Money
•Knowledge and skills
•Experience
•Self-esteem
•Previous and current Healthy behaviour
•Social support
•Ego / identity
•Commitment and cohesion with one’s cultural roots
•Cultural stability
•Ritualistic activities
•Religion and philosophy (e.g., stable set of answers to life’s perplexities)
•Genetic factors
•Preventive health orientation
If a person has access to these kinds of resources, there is a better chance for them to deal with the challenges of life and to construct coherent life experiences.
Eco-social framework (Krieger, 2012)
sought to integrate social + biological and dynamic + historical + introspective = finding solutions to disease distribution and health discrepancies.
The term “adaptation theories” is used to denote a group of theories and models that try to explain the psychological process of adjustment that takes place whenever people are faced with situations that require them to undertake a major revision of their assumptions about the world and adapt to those situations (eg, the onset of a disease)
In particular, the Transtheoretical Model maintains that individuals change their health behaviors in different stages. They pass from not being concerned to change their behaviors (pre-contemplation stage) to starting to think about them (contemplation) to finally enacting them (action stage) and fully engaging in those behaviors in the long run (maintenance).7
— not as good as a theoru
PHE IN ACTION??
The Relevance of Psychology in global health
•Psychological science contributes to understanding the human dimensions of health behavior, decision-making, and system engagement.
•It provides evidence-based tools to address challenges like vaccine hesitancy, treatment non-adherence, risk communication, and mental health burden.
•Psychology operates at multiple levels: individual (e.g., beliefs, emotions), interpersonal (e.g., trust, stigma), and systemic (e.g., policy design, health literacy).
Psychology contributes to global health not only through understanding behavior but also
through designing and implementing interventions that are culturally informed, ethically grounded, and evidence-based.
Nudging
nudging" refers to a method of influencing people's choices by subtly altering the way options are presented, without forcing them to choose a specific option. This is often done by leveraging cognitive biases and habits to encourage people to make choices that are more beneficial for them or society.
Psychological Theories Guiding Climate Behavior Interventions
. Nudge Theory (Thaler & Sunstein)
•Alters the choice architecture to make sustainable options the easy/default ones.
•Ex: Default vegetarian options in cafeterias → reduced meat consumption.
2. Social Norms Theory
•Leverages what “others like you” are doing to increase compliance.
•Ex: “Most neighbors use less water” → encourages conservation.
3. Self-Determination Theory
•Supports intrinsic motivation by reinforcing autonomy, competence, and relatedness.
•Ex: Climate education programs that build self-efficacy and agency.
4. Dual Process Theory (Kahneman)
•Combines fast, emotional thinking (System 1) with slower, analytical reasoning (System 2).
•Ex: Emotional stories drive action more effectively than data alone.
be concerned about
ethics with nudging etc
Individual voices, collective health: a person-centered cross-sectional study to identify psychological drivers of vaccination attitudes — ARTICLE MAIN IDEAS
Although existing research identifies different profiles of vaccine-hesitant individuals, most studies focus on isolated psychological constructs, neglecting their interplay in shaping vaccination attitudes.
four underlying psychological drivers: Eco-humanism (altruistic/biospheric values and connectedness to nature), Skeptical Perspective (distrust in science, conspiracy mentality, and spirituality), Goal-Driven Positive Mindset (hope and optimism), and Self-Centered Attitude (hedonic/egoistic values).
eco humanism vaccine attitude
more positive vaccination attitudes, particularly lower mistrust in vaccine benefits and reduced concerns about pharmaceutical companies’ profiteering. —
skeptical perspective vaccine attitude
linked to more negative attitudes, including increased mistrust in vaccine benefits, heightened concerns about vaccine safety and pharmaceutical companies’ profiteering, and a greater preference for natural immunity. —
goal driven positive mindset vaccine attitude
although not significantly associated with overall vaccination attitudes, was inversely related to mistrust in vaccine benefits. —
self-centeted attitude vaccines
Self-Centered Attitude was tied to an overall more negative stance, particularly marked by amplified worries about unforeseen long-term effects, heightened concerns about pharmaceutical companies’ profiteering, and an increased preference for natural immunity. — However, unlike the Skeptical Perspective driver, individuals with a strong Self-Centered attitude do not appear to harbor skepticism regarding vaccine efficacy. This suggests that their concerns about vaccines are more focused on personal gain and pleasure rather than a lack of trust in scientific evidence.
how was info collected for vaccine article
BASICALLY QUESTIONAIRE — The questionnaire gathered demographic information (e.g., sex, age, nationality, and residence location) and socioeconomic factors, including marital status, level of education (graduate, undergraduate, etc.), occupation (employed, retired, unemployed, homemaker, student, other), and monthly income. Political orientation was measured on a 10-point Likert scale ranging from “Left” to “Right,” with an additional option for participants who do not identify with any political party or were not interested in politics (coded as [neutral/ignored/separate category]). The questionnaire also encompassed questions assessing participants’ personal values, beliefs, and neuro-biological traits. Spirituality was measured by asking participants to rate the importance of spirituality in their lives on a 10-point Likert scale, with 1 being “not at all important” and 10 being “extremely important”. Similarly, optimism was assessed by prompting participants to rate themselves on a 10-point scale regarding how much they identified as optimists (1 = absolutely pessimist, 10 = absolutely optimist). Furthermore, the questionnaire included validated psychometric scales to assess hope (Hope scale (Snyder et al., 1996)), biospheric, altruistic, hedonic and egoistic values (Environmental Portrait Value Questionnaire, E-PVQ (Bouman et al., 2018)), negative perceptions about the credibility of science (Credibility Of Science Scale (Hartman et al., 2017)), conspiracy mentality (Conspiracy Mentality Questionnaire (Bruder et al., 2013)), sensory-processing sensitivity (HSP scale (Aron and Aron, 1997)), connectedness to nature (Connectedness to nature scale, CNS (Lovati et al., 2023)).
dentification of the psychological drivers of vaccination attitudes
(i) hope, (ii) biospheric, (iii) altruistic, (iv) hedonic and (v) egoistic values, (vi) negative perceptions about the credibility of science, (vii) conspiracy mentality, (viii) optimism, (ix) sensory processing sensitivity, (x) connectedness to nature, and (xi) spirituality.
The VAX scale items are categorized into four sub-domains:
(i) mistrust of vaccine benefits, (ii) concerns about unforeseen future effects, (iii) worries regarding commercial profiteering, and iv) preference for natural immunity.
vaccine study personal values recognized
biospheric, altruistic, hedonic, and egoistic values, are recognized as critical predictors of health behaviors, including vaccination decisions (Pivetti et al., 2023). In particular, biospheric and altruistic values often underpin pro-vaccination attitudes due to their association with concerns for public health and environmental sustainability, which are closely tied to collective well-being (Bouman et al., 2021; Bouman et al., 2018). In contrast, egoistic and hedonic values, which emphasize personal gain and immediate gratification, may correlate with vaccination hesitancy if individuals prioritize perceived risks or discomfort over communal benefits
Sensory processing sensitivity (SPS) in relation to vaccine trust
neurobiological trait characterized by heightened responsiveness to environmental stimuli, may influence vaccination attitudes through increased vulnerability to stress and health-related anxiety (Costa-López et al., 2024). SPS has been shown to affect how individuals perceive health risks and engage with health-related decisions, making it an innovative variable to explore in this context
tools for the climate article
Surveying 973 children (5–11 years) from different regions, findings showed high awareness (93%) and concern (63%) about climate change.
there is a greater concern for climate issues from italian children the
south
factors that influence kids knowledge of climate change
education and regional conditions [2], educational and informational interventions are key in shaping their perceptions of environmental issues.
climate change study thematic clusters
(1) engagement with the climate change challenge (Table 1), (2) concerns about the climate change challenge (Table 2), (3) sense of agency towards the climate change challenge (Table 3), and (4) hopefulness towards the climate change challenge
what does the caregiver study examine
his scoping review aims to comprehensively map the existing literature on the impact of caregiver affiliate stigma of caregivers for individuals with NDDs, on their psychosocial well-being. More specifically this review aimed to: (1) Examine the relationship between affiliate stigma and caregiver psychosocial well-being; (2) Identify and synthesize existing definitions and conceptualizations of caregiver affiliate stigma and related concepts within the context of NDDs through the lenses of Bronfenbrenner’s ecological systems theory; and (3) Identify the knowledge gaps in the existing literature, highlighting areas where further investigation is needed. Finally, using the Bronfenbrenner’s ecological system theory, we discuss the review results to identify possible lines of interventions to prevent caregiver affiliate stigma phenomena.
the word stigma should make you think of
societal labeling, stereotyping, and negative judgments. Caregiver affiliate stigma, the focus of this review, refers to the internalization of these societal biases by caregivers, leading to negative self-perceptions and social withdrawal [30,31]. Various types of stigma, such as public stigma, courtesy stigma (stigma by association), and family stigma, all contribute to caregivers’ psychological burden. Public stigma involves negative societal reactions toward individuals with NDDs, while courtesy stigma extends this discrimination to caregivers due to their association with stigmatized individuals
The majority of articles (n = 16) focused on caregivers of people with various types of dementia. A smaller number of studies specifically examined caregivers of those with AD only (n = 2) and one study included caregivers of patients with ALS or PMA. Notably, despite Parkinson’s disease being the second most common NDD [8], none of the 19 studies included in this review specifically focused on caregivers of individuals with Parkinson’s disease. This represents a significant gap in the current literature on caregiver affiliate stigma in relation to NDDs.