PERIO W8 Classification of Perio: Mucogingival Deformities and Conditions
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
General definition of Mucogingival defects and conditions.
Any defect associated with deviation from normal anatomic/morphologic relationship between gingiva and alveolar mucosa.
all ages are susceptible to the defects and conditions
any tooth or implant can be affected with or without perio disease
Define Normal mucogingival condition.
Define as the absence of a disease state → no disease in gingiva, periodontium or gingival recession.
Define Periodontal Biotypes. What 3 features are considered a periodontal biotype?
Periodontal Biotypes are features of the periodontium influenced by genetic and environmental factors. Includes:
Gingival Biotype
Bone Morphology
Tooth Dimension of any given tooth.
What are the 3 types of Gingival biotypes?
Thin scalloped
Thick scalloped
Thick flat
Describe Thin-scalloped gingival biotype. (4)
Slender, triangular shaped crown
Thin, delicate soft tissue with thin alveolar bone
Narrow zone of keratinized tissue
Accentuated scalloped gingival margin contour.
**greater tendency for onset and progression of mucogingival deformities.

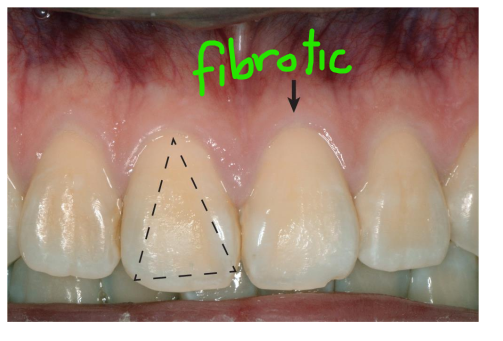
Describe Thick-scalloped Gingival biotype. (4)
Slender, triangular-shaped crown
Thick, fibrotic gingiva
Narrow to moderate zone of keratinized tissue
Accentuated scalloped gingival margin contour
**prone to development of mucogingival deformity
Describe Thick-flat Gingival biotype. (4)
Wide, square-shaped crown
Thick, dense fibrotic tissue
Wide band of keratinized tissue
Flat gingival margin contour
Less pronounced tissue scalloping
Large interproximal contact areas
Thick alveolar bone
**more resilient and less susceptible to inflammation and trauma than thin/thick scalloped biotypes.
Which gingival biotype is the most vulnerable to mucogingival deformities/conditions? Which is the least?
The thin scalloped gingival biotype is generally considered the most vulnerable.
More prone to gingival recession
Less resistant to trauma and inflammation
Thinner underlying bone, increasing risk of defects
Thick-flat gingival biotype is the most resilient
Research shows that plaque-associated inflammation may result in deep periodontal pockets with a ______ biotype and cause gingival recession in __ biotypes.
biofilm-induced inflammation causes:
deep perio pockets for thick-flat biotype
gingival recession for thin-scalloped biotype
What is the most common mucogingival deformity?
Recession of the gingival margin aka gingival recession.
movement of the gingival margin apically towards CEJ.
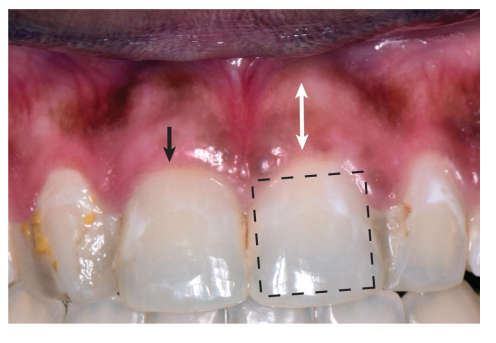
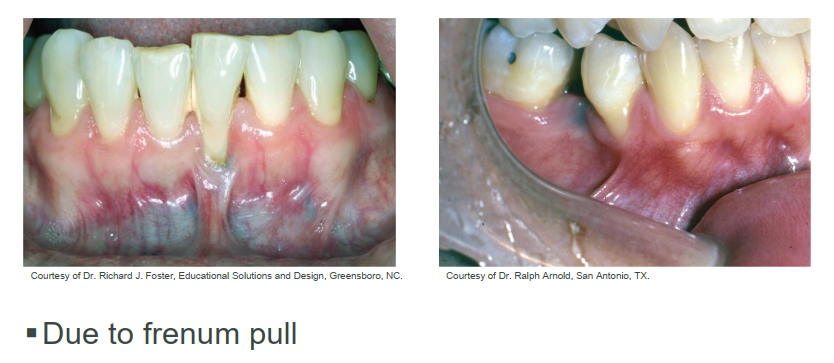
How does the frenum contribute to mucogingival deformities?
frenum pull can cause gingival recession
What are the 3 main risk factors for gingival recession?
Thin tissue biotype
Narrow band/zone of keratinized tissue
Absence of attached gingiva
other risks: reduced thickness of alveolar bone, abnormal teeth position, mechanical trauma, orthodontics
The Miller classification system for Gingival margin recession is was widely used for ~40 years. The system is based on….
Based on level of gingival margin with respect to mucogingival junction and underlying alveolar bone.
has 4 categories
What are some disadvantages to using the Miller classification system? (4)
Difficult to identify exact location of the extent of apical recession with respect to the MGJ
Difficult to differentiate between Class 1 and 2
Not clear in defining amount of interproximal soft/hard tissue loss between Class 3 and 4
Reliability of the system has never been tested
Define the 4 classes of the Miller Classification System for Gingival margin recession.
Class I – Recession does not extend to the mucogingival junction (MGJ). No loss of interdental bone or soft tissue.
Class II – Recession extends to or beyond the MGJ. No loss of interdental bone or soft tissue.
Class III – Recession extends to or beyond the MGJ with some loss of interdental bone and/or soft tissue, or malpositioning of teeth that limits root coverage.
Class IV – Recession extends to or beyond the MGJ with severe loss of interdental bone and/or soft tissue, or severe malpositioning of teeth — root coverage not possible.
Describe how the Cairo classification system categorizes Gingival margin recession.
The Cairo classification is based on clinical attachment loss (CAL) at both the buccal and interproximal sites, rather than just where the gingival margin sits (Miller).
This system is considered more reliable than Miller’s for prognosis and treatment planning because it accounts for interproximal attachment levels.
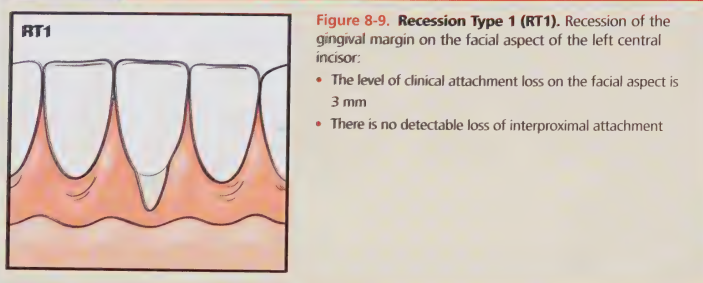
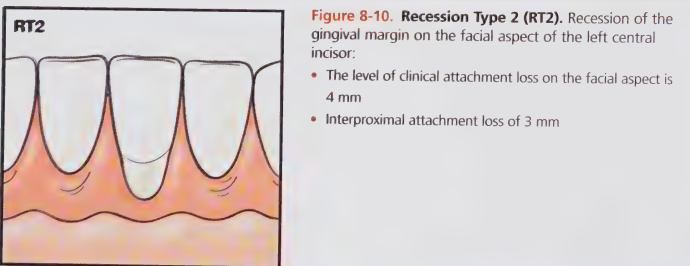
Explain each recession type of Cairo Classification.
RT1 (Recession Type 1) – CAL is present only on the buccal (or lingual) surface, no interproximal attachment loss. Interproximal CEJ is not clinically detectable.
RT2 – CAL is present on the buccal and interproximal surfaces, but interproximal CAL ≤ buccal CAL.
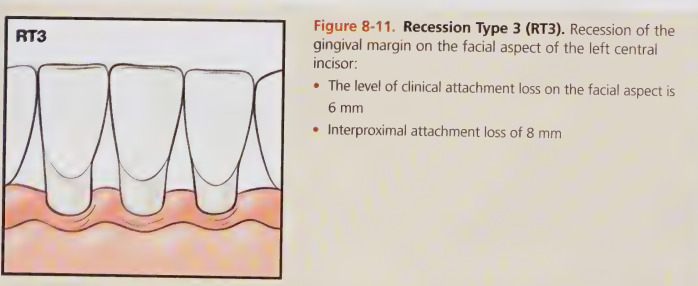
RT3 – CAL is present on the buccal and interproximal surfaces, and interproximal CAL > buccal CAL.
Which Cairo recession type is most likely due to traumatic tooth brushing?
RT1
Which Cairo Recession type is most likely associated with periodontitis-associated horizontal bone loss?
RT 2
Which Cairo recession type is most likely associated with infrabony defects?
RT 3
How is treatment considerations for gingival recession defects assessed?
Considerations for severity of symptoms, tissue biotype, and patient-specific factors
Consider if monitoring with no treatment is sufficient
Restorative/surgical periodontal intervention may be an option if necessary
When might surgical intervention NOT be required?
progression of gingival recession is arrested early on
Gingiva on affected tooth appears stable and clinically healthy
What are some anatomical predisposing factors for gingival recession?
Decreased vestibular depth / lack of attached gingiva
Makes oral hygiene difficult → plaque retention → inflammation → further recession.
Aberrant frenum / high muscle attachment
Pulls on the gingival margin during lip or cheek movement → mechanical tension → recession progression.
Gingival excess
Excess tissue can mask underlying recession or create irregular margins.
gingival excess = pseudo-pocket, inconsistent gingival margin, excessive gingival display (gummy smile), gingival enlargement.
Define non-carious cervical lesions (NCCLs).
Dental tissue loss at or near the CEJ and not relating to tooth decay.
What are 6 Tooth and Prosthesis-related factors that predispose a client to plaque biofilm retention?
Cervical enamel projections
Enamel Pearls
Palatolingual grooves
Tooth malalignment
Orthodontic appliances (braces)
Faulty restorations (overhang on filling)
Define Primary and Secondary occlusal trauma.
Primary occlusal trauma – Too much force on a tooth with healthy gums and bone.
Secondary occlusal trauma – Normal biting force causing damage a tooth with bone loss or gum disease. (ex. occlusal trauma on tooth with periodontitis)
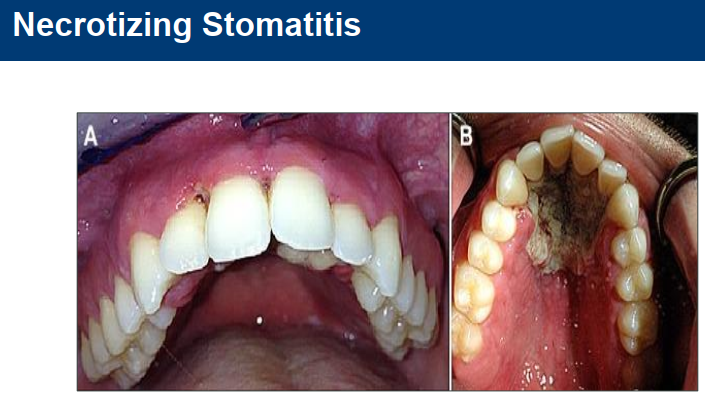
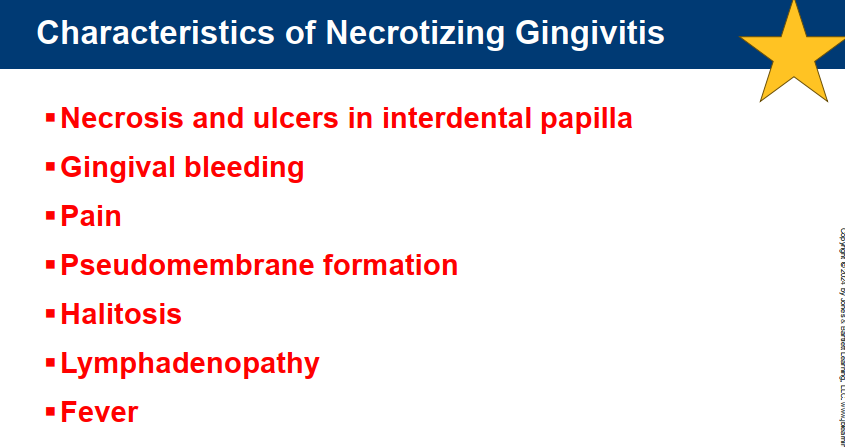
Define necrotizing periodontal disease (NPD). What are some distinct characteristics?
NPD is a inflammatory, destructive infection of the periodontal tissue that involve tissue necrosis (localized tissue death).
Distinct characteristics:
interdental tissue necrosis
intense gingival pain
spontaneous gingival bleeding.
other: very bad breath, pseudomembrane formation, systemic involvement.
NPD is AKA trench mouth, vincent infection, acute necrotizing ulcerative gingivitis (ANUG), necrotizing ulcerative gingivostomatitis
Describe the appearance of Necrotizing Periodontal Disease.
Ulcerated and necrotic papillae and marginal gingiva
Papillae and gingival margin have a “punched out” or “cratered” appearance
Pseudomembrane = gray layer of tissue covering the necrotic areas of the gingiva

What is a systemic sign/symptom of NPD?
Swollen lymph nodes
submandibular
cervical
Other symptoms:
fever
malaise
increase pulse rate
loss of appetite
What are the 3 types of Necrotic Periodontal Diseases? Describe each.
Necrotizing Gingivitis
limited to gingival tissues (interdental and marginal)
Non communicable, destructive, inflammatory disease
most often found in mand anterior region
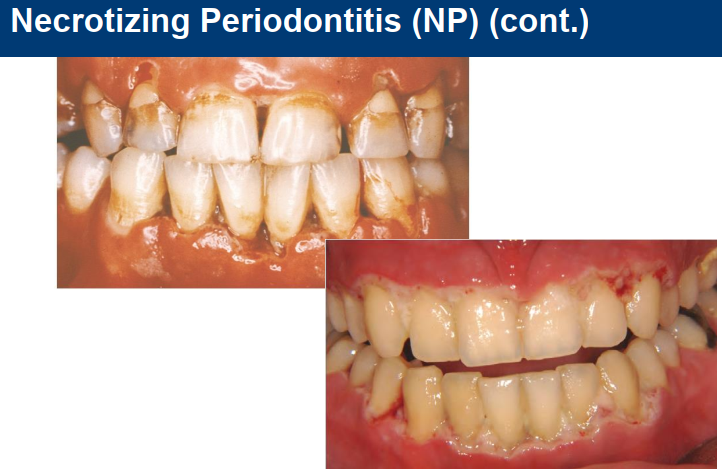
Necrotizing Periodontitis
affects gingival tissue, PDL, and alveolar bone
Necrotizing Stomatitis
severe necrosis extending beyond gingiva to other parts of oral cavity
rarest form of NPD.
What is the progression of necrotizing gingivitis?
Progression is predictable.
Starts with interprox gingiva necroses
spreads to affect marginal gingiva
causes punched out appearance

What is the etiology for Necrotizing gingivitis?
Microbial cause – mainly anaerobic bacteria (bacteria deep within NG lesion); diverse array of MO
95% of cases in North America occur in Caucasians
Predisposing factors:
Poor oral hygiene and plaque accumulation
Stress
Smoking
Immunosuppression (HIV/AIDS, systemic illness, malnutrition)
HIV+ higher risk for NG; NG may be first indicator for HIV infection
Lack of sleep/fatigue
Pre-existing gingivitis or periodontal disease
What age group is the most common/susceptible to Necrotizing Gingivitis?
Can affect all ages but most common is between the ages of 20-30
What are the 4 stages of Treating Necrotizing Periodontal Disease?
Management of Acute Stage
First Treatment: remove pseudomembran, soft and mineralized deposites; provide self care regiment
Second Treatment: Initiate subgingival periodontal instrumentation
Third Treatment: complete subgingival instrumentation; evaluate resolution of symptoms
**severe cases may require antibiotics
Control Pre-existing Condition(s)
Corrective Surgical management (if required)
Maintenance Phase
What is the treatment for Necrotizing Periodontitis?
Similar to NG but more complex due to extensive tissue destruction
Referral to Periodontist
Collaboration with pt GP warranted
What is the typical treatment for Necrotizing Stomatitis?
Treatment for NG and NP + dealing with necrosis progression to deeper tissues beyond mucogingival line
Refer immediately to oral pathologist, oral maxillofacial surgeon and physician (gp)