OT INTRO 4: Clinical Reasoning, Documentations, Team Approach, Safety Precautions
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
82 Terms
Clinical Reasoning
-The process that practitioners use to plan, direct, perform, and reflect on client care.
- a.k.a. professional reasoning, therapeutic reasoning
- Metacognitive analysis: therapists actually think when they actually are engaged in practice
Reasoning In Practice: A Whole-Body Process
It is a different experience to read a case study than to be the practitioner in the situation.
1. Cue acquisition
2. Pattern recognition
3. Limiting the problem Space
4. Problem formulation
5. Problem solution
Cognitive Processes Underlying Professional Reasoning
Professional Self
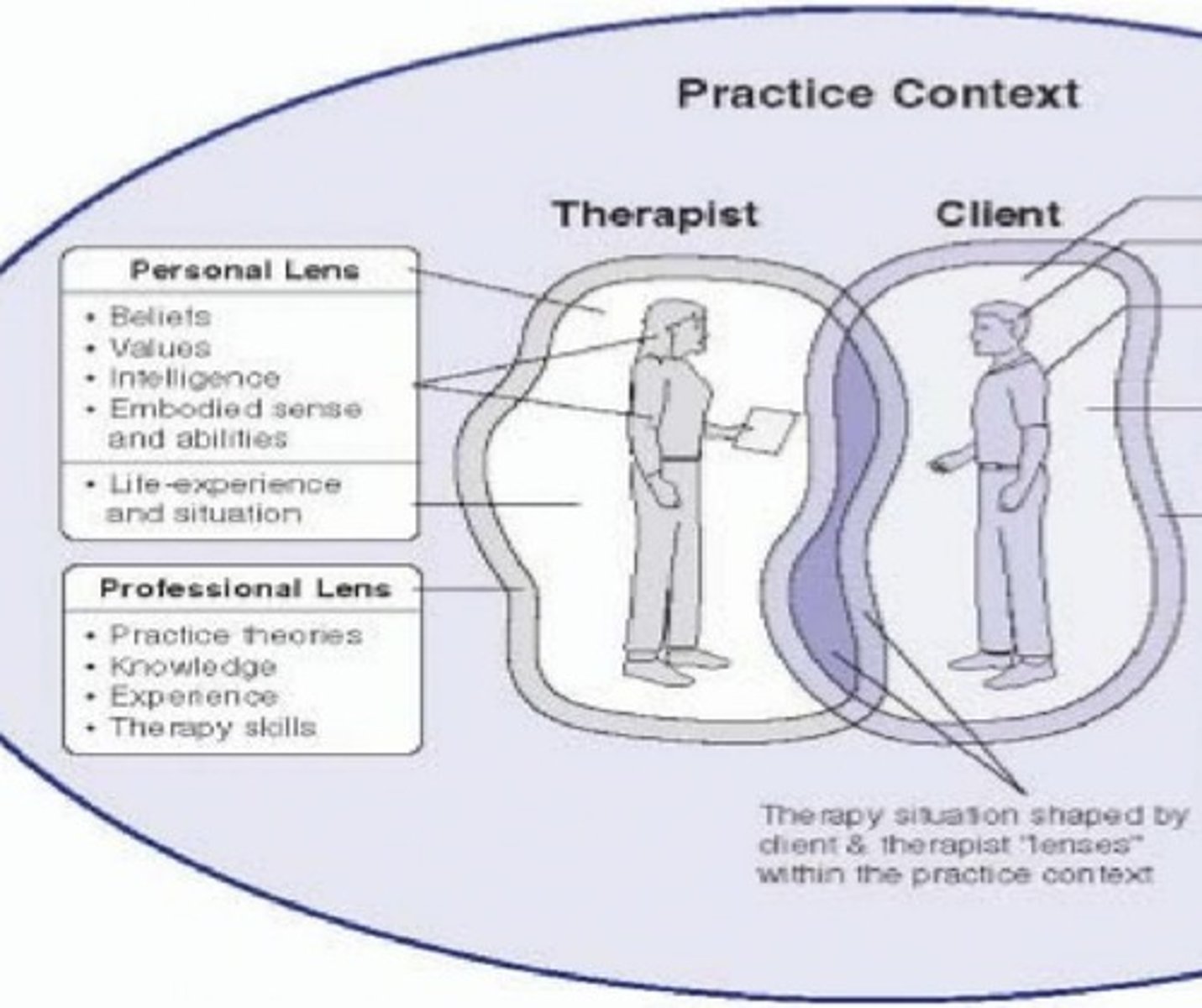
Personal Self
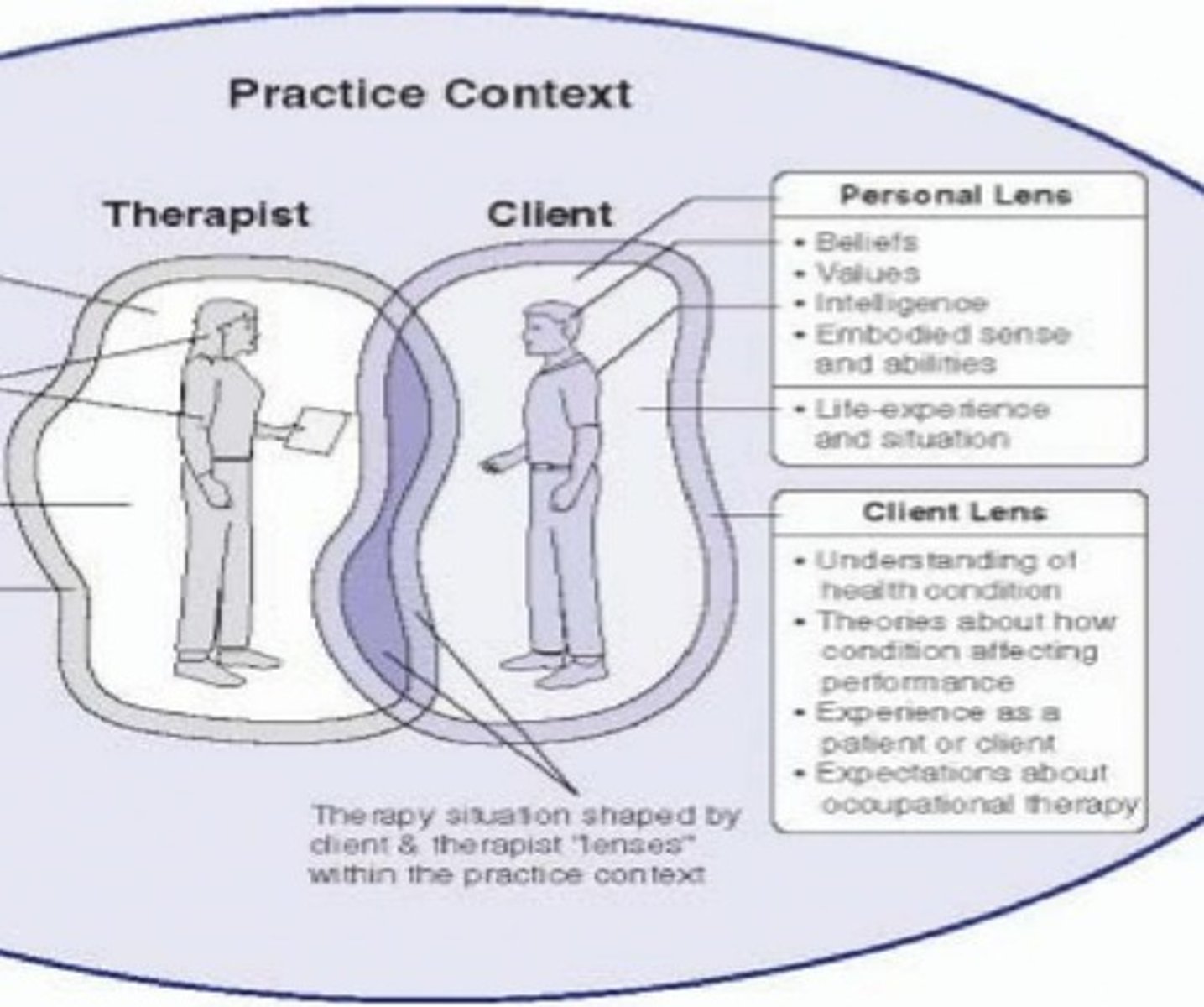
Practice
Reflective practitioner:
term describes how experts think critically about their own experience.
Reflection in action
involves the practitioner's ability to think in the midst of action and adapt to meet the demands of the situation. Reflection in action most often occurs when the usual approaches are not working.
Reflection on action
critical thinking that occurs after the fact. Reflection about practice, identifying what worked and what did not, and being open to alternative conceptions are necessary to support the learning associated with advancing expertise.
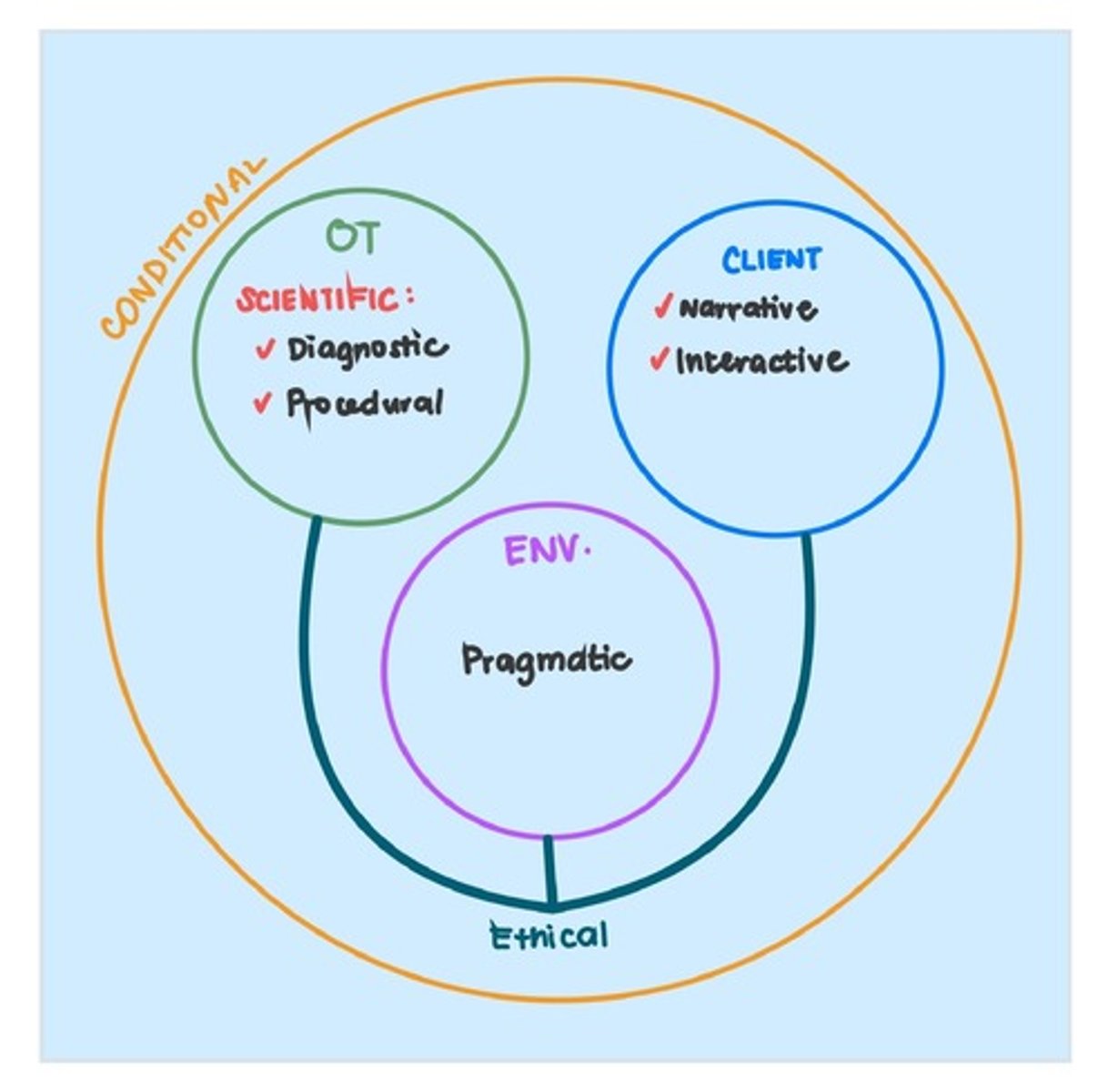
1. Scientific Reasoning
2. Diagnostic Reasoning
3. Procedural Reasoning
4.Narrative Reasoning
5. Pragmatic Reasoning
6. Ethical Reasoning
7. Interactive Reasoning
8. Conditional Reasoning
Types of Reasoning:
Scientific Reasoning
Reasoning:
- Scientific reasoning is used to understand the condition that is affecting an individual and to decide on interventions that are in the client's best interest. It is a logical process that parallels scientific inquiry.
- Scientific reasoning is also referred to as treatment planning in which the therapist uses selected theories both to identify problems and to guide decision making.
Scientific Reasoning
Description and focus:
- Reasoning involving the use of applied logical and scientific methods, such as hypothesis testing, pattern recognition, theory-based decision making and statistical evidence.
Scientific Reasoning
Clues to help ID:
Impersonal, focused on the diagnosis, condition, guiding theory, evidence from research or what "typically" happens with clients like the one being considered.
Diagnostic Reasoning
Reasoning:
is concerned with clinical problem sensing and problem definition.
Diagnostic Reasoning
Description and focus:
- Investigative reasoning and analysis of cause or nature of conditions requiring occupational therapy intervention. Can be considered one component of scientific reasoning.
Diagnostic Reasoning
Clues to help ID:
- Uses both personal and impersonal information. Therapists attempt to explain why client is experiencing problems using a blend of science-based and client-based information.
Procedural Reasoning
Reasoning:
- Occurs when practitioners are "thinking about the disease or disability and deciding which intervention activities (procedures) they might employ to remediate the person's functional performance problems"
Procedural Reasoning
Description and focus:
- Reasoning in which therapist considers and uses intervention routines for identified conditions. May be science-based or may reflect the habits and culture of the intervention setting.
Procedural Reasoning
Clues to help ID:
- Characterized by therapist using therapy regimes or routines thought to be effective with problems identified and that are typically used with clients in that setting. Tends to be more impersonal and diagnostically driven.
Narrative Reasoning
Reasoning:
- Requires that practitioners find a way to understand the meaning of this experience from the client's perspective. Involves thinking in story form and asks "What is the client's story?"
- As Kielhofner noted, it "becomes particularly important for considering how the person's disrupted life story can be constituted or reconstituted"
Narrative Reasoning
Description and focus:
- Reasoning process used to make sense of people's particular circumstances, prospectively imagine the effect of illness, disability, or occupational performance problems on their daily lives, and create a collaborative story that is enacted with clients and families through intervention.
Narrative Reasoning
Clues to help ID:
- Personal, focused on the client, including past, present, and anticipated future. Involves an appreciation of client culture as the basis for understanding client narrative. Relates to the "so what" of the condition for the person's life.
Pragmatic Reasoning
Reasoning:
- is yet another strand of reasoning that goes beyond the practitioner- client relationship and addresses the world in which therapy occurs
- Practice requires that practitioners reason about negotiating their clients' interests within the practice culture.
- Personal context also affects therapy.
Pragmatic Reasoning
Description and focus:
- Practical reasoning which is used to fit therapy possibilities into the current realities of service delivery, such as scheduling options, payment for services, equipment availability, therapists' skills, management directives, and the personal situation of the therapist.
- These include resources for intervention, organizational culture, power relationships among team members, reimbursement practices, and practice trends in the profession
Pragmatic Reasoning
Clues to help ID:
- Generally not focused on client or client's condition, but rather on all the physical and social "stuff" that surrounds the therapy encounter, as well as the therapist's internal sense of what he or she is capable of and has the time and energy to complete.
Ethical Reasoning
Reasoning:
- goes one step further and asks: "What should be done?" The clinical reasoning process terminates in an ethical decision, rather than a scientific one, and the ethical nature of the goal of clinical reasoning projects itself over the entire sequence"
Ethical Reasoning
Description and focus:
- Reasoning directed toward analyzing an ethical dilemma, generating alternative solutions, and determining actions to be taken. Systematic approach to moral conflict.
Ethical Reasoning
Clues to help ID:
- Tension is often evident as therapist attempts to determine what is the "right" thing to do, particularly when faced with dilemmas in therapy, competing principles, risks, and benefits.
Interactive Reasoning
Reasoning:
- The provision of therapy is inherently a communicative process. Practitioners must gain the trust of their clients and of people who are important in the clients' world. This is because occupational therapy involves "doing with" as opposed to "doing to" clients.
Interactive Reasoning
Description and focus:
- Thinking directed toward building positive interpersonal relationships with clients, permitting collaborative problem identification and problem solving.
Interactive Reasoning
Clues to help ID:
- Therapist is concerned with what client likes or does not like. Use of praise, empathetic comments, and nonverbal behaviors to encourage and support client's cooperation.
Conditional ReasoningConditional Reasoning
Reasoning:
- Fleming described the ability of skilled occupational therapy practitioners to "form an image of future life possibilities for the person." The ability to form these images (or schemata, to use a cognitive terms) seems to require a blend of all the forms of clinical reasoning, along with sufficient clinical experience to have seen a variety of different outcomes with former clients.
Conditional Reasoning
Description and focus:
- A blending of all forms of reasoning for the purposes of flexibly responding to changing conditions or predicting possible client futures.
Conditional Reasoning
Clues to help ID:
- Typically found with more experienced therapists who can "see" multiple futures, based on therapists past experiences and current information.
Types of Reasoning
Supervision
It is a process in which two or more individuals collaborate to establish, maintain, promote, or enhance a level of performance and quality of service.
1. Novice
2. Advance Beginner
3. Competent
4. Proficient
5. Expert
Expertise Continuum
Novice
- 0 years
- no experience in situation of practice.
Advance Beginner
- <1 year
- begins to incorporate contextual information into rule-based thinking.
Competent
- 3 years
- automatically performs more therapeutic skills and attends to more issues.
Proficient
- 5 years
- reflects on expanded range of experiences, permitting more focused evaluation and more Proficient flexibility in intervention
Expert
- 10 years
- clinical reasoning becomes a quick intuitive process, which is deeply internalized and embedded in an extensive range of case experiences.
1. Administrative
2. Professional Practice
3. Function
Types of Supervision
Administrative
focused on monitoring performance and making sure that the supervisee's work performance and professional development meet the objectives and standards of the employing organization
Professional Practice
is aimed at providing support, training, and evaluation of a supervisee's professional performance and development
Function
a specific aspect of work or a "function" of clinical practice is delegated to a specified individual to provide training and oversight in that aspect of work
1. Continuous
2. Close
3. Routine
4. General
5. Minimal
Frequency of Supervision
Continuous
required for patient related tasks must be within auditory/visual contact in the immediate area during performance
Close
daily, direct contact at site of work
Routine
direct contact at least every 2 weeks at site of work interim supervision occurring by other methods (telephone/written communication)
General
monthly direct contact with supervision available as needed by other methods
Minimal
provided only on a need basis supervision may be less than monthly
Intermittent
sufficient for non-patient related task; at least a monthly basis; requires periodic discussion, documentation or contact
Team Approach
A team is a group of equally important individuals with common interests collaborating to develop shared goals and build trusting relationship to achieve shared goals.
1. Intradisciplinary
2. Interdisciplinary
3. Multidisciplinary
4. Transdisciplinary
Team Approaches:
Intradisciplinary
- one or more members of one discipline
- evaluate, plan, and implement treatment other disciplines not involved; communication is limited
- potential narrowness of perspective (comprehensive, holistic)
Interdisciplinary
all disciplines collaborate for decision-making independent evaluation and intervention with greater understanding of each discipline's perspective members directed to a common goal and not bound by discipline specific roles uses group process skills
Multidisciplinary
- each member conducts assessments and interventions independent from one another resources and responsibilities are individually allocated between disciplines
- primary allegiance is his/her discipline
Interdisciplinary
- all disciplines collaborate for decision-making independent evaluation and intervention with greater understanding of each discipline's perspective members directed to a common goal and not bound by discipline specific roles
- uses group process skills
Transdiciplinary
- members support and enhance the activities and programs of other disciplines to provide quality, efficient, cost-effective service
- one member may take on multiple responsibilities
- role blurring is accepted
1. Clinical
2. Administrative or departmental
Types of Record
Clinical:
pertains to patient care (OT notes, referral notes)
Administrative or departmental:
(statistical records most important, personnel management record, equipment and supply records, financial records)
Purpose of Documentation
✔ Provide a legal, serial record of client's condition (legal document)
✔ Information resource for client care (facilitate effective intervention)
✓ Communicate information about client from OT perspective (communication) ✔Provide data for use in intervention, evaluation, research, education (reimbursement) except: cover the therapist
Purposes of Record keeping:
✔ For betterment of patient care
✔ Education
✔ Communication
✔ Third party payers, reimbursement
✔ Societal benefits
✔ Legal aspects
✔ Research
✔ Motivational tool
✔Administrative control
Fundamental Elements:
✓ client's full name and case number on each page
✓ date (month, day, year) and type of OT contact
✓ identification of type of documentation, agency, and department name
✓ OT practitioner's signature with a minimum of first name or initial, last name, and professional designation
✓ sign with full signature with no space from content
✓ countersign on documentation written by students and OTA (if required by law)
✓ acceptable terminology defined within the boundaries of setting
✓ standard, well-recognized abbreviations are only used
✔errors must be crossed out with one line and put initials on the correction
✓ adherence to professional standards of technology
✔disposal of records within law or agency requirements (all documents may be subject to subpoena)
✓ comply with confidentiality standards (do not put other client's names)
✓ institutional/program guidelines/reimbursement guidelines must be followed
Guidelines
✓ legible handwriting (illegible is not reimbursable)
✓ correct grammar and spelling (errors detract from professionalism)
✓ be concise, but complete, non-important details should be left out
✓ be objective with clear distinctions between facts vs. behaviors and opinions vs. interpretation
✓ be current and accurate; active rather than passive voice
✓ use person first language at all times (ex. child with autism than autistic child)
Example of documentation
✓ RUMBA (Relevant, Understandable, Measurable, Behavioral, Achievable)
✓ POMR (Problem-Oriented Medical Record)
✓ SOAP (Subjective, Objective, Assessment, Plan)
✓ BIRP (Behavior, Intervention, Response, Plan)
✓ Uniform Terminology (1979, 1989, 1994)
✓ OTPF (2002, 2008, 2013)
✓ SMART (Specific, Measurable, Attainable, Realistic, Time-bound)
✓ABCD (Audience, Behavior, Condition, Degree)
✓ CARE (Clarity, Accuracy, Relevance, Exceptions)
✓ Classification codes set out by WHO/ICF
General First Aid
immediate care given to a person who has been injured or suddenly taken ill. It includes self help and home care when medical assistance is delayed or not available
Roles of First Aid
1. Bridge that fills the gap between the victim and the physician
2. It is not intended to complete with nor to take the place of the services of the physician
3. It ends when medical assistance begins
Objectives of First Aid:
✓ To alleviate suffering
✓ To prevent added or further injury or damage
✓ To prolong life
Injuries/Accidents/Emergencies
✓ Ask for help. Do not leave the client alone.
✓ When emergency is over, document.
✓ Notify supervisor of incident and file incident report
Falls
- Falling forward/backward: Help to stand erect
- Falling too far forward/backward: Assist to floor
Bleeding
- First Aid treatment to preven contamination annd stop bleeding
- Wear gloves, apply direct pressure, elevate, rinse with water/antiseptic
- For arterial bleeding , apply intermittent, direct pressure to the artery above the level of the wound
- Do not apply tourniquet
Seizure
- Place in a safe location. Do not attempt to restrain/ restrict convulsion
- Loosen the clothing. Keep client's airway open
- Do not insert anything on the mouth
- Remove sharp objects from around the person
- Lay the person on the side
- Have the client rest with blanket
Respiratory distress
- High Fowler's Position: lying on bed
- Orthopneic position: sitting or standing
- Pursed-lip breathing
Burns
- Rinse in cold (NOT ICED) water
- Cover with clean dressing
- DO NOT APPLY anything
Shock
- Get medical assistance ASAP; can be life threatening
- Determine cause of shock and correct if possible
- Monitor vital signs
- Place person in supine, head lower than legs
- Do not add heat, apply cold compress
- Do not allow exertion
Insulin-related Illness
- Hypoglycemia: juice or candy (moist, pale skin; agitated/ excited behavior)
- Hyperglycemia: insulin (dry, flushed skin, excessive thirst, drowsy)
Choking or Cardiac arrest
- perform Heimlich maneuver
- perform CPR (perform 30 chest compression/ 2 rescue breaths for 5 cycles)
1. Survey the scene
2. Primary survey of the victim
3. Call for help/ Medical Assistance
4. Secondary survey of the victim (Is patient is conscious)
5. Record Findings
Emergency Activation Principles
Survey the scene
Danger: What happened? Is the scene safe? How many people are injured? Are there bystanders who can help?
Primary survey of the victim
- Responsiveness: Is the victim conscious or unconscious?
- Airway: Is the airway open and clear?
- Breathing: Is the victim breathing? Shallow or deep? Does he appear to be choking? Cyanotic?
- Circulation: Is the victim's heart beating? Assess pulse. Is he severely bleeding?