Unit 2 Exam Study Guide - BIO 1121 - Anatomy & Physiology I
1/180
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
181 Terms
Functions of the skeletal system
support, protection, movement, mineral storage, blood cell production (hematopoiesis)
long bones
bones that are longer than they are wide
These types of bones consist of a shaft with two enlarged ends.
They have a thick layer of superficial compact bone with some deep spongy bone.
The majority of the appendicular skeleton (i.e. arms and legs) is classified as this type of bones. The only exceptions are the patella (kneecap), carpal bones of the wrist, and tarsal bones of the ankle.

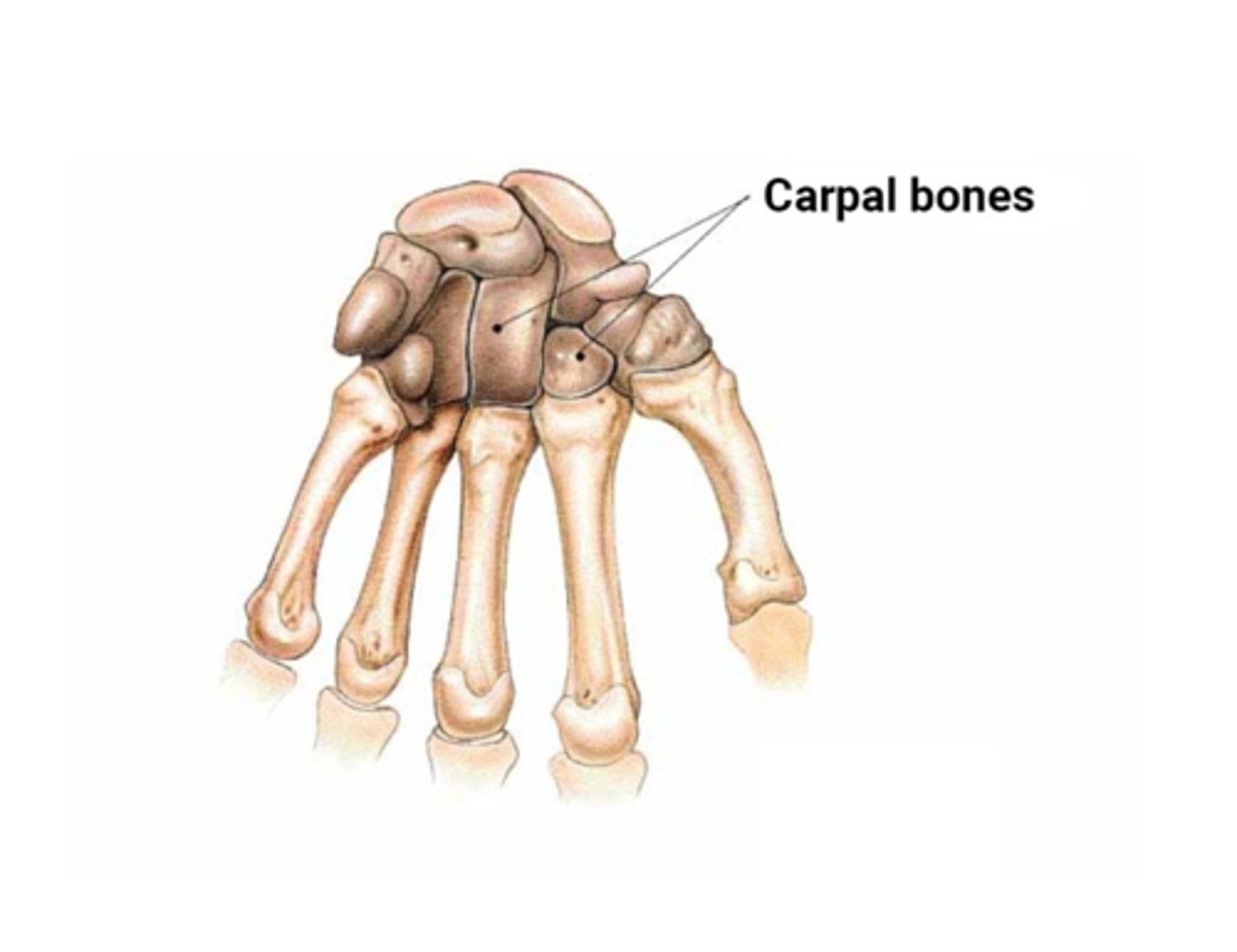
short bones
cube-shaped bones of the wrist and ankle
These bones have a fairly regular square shape.
They have a thin layer of superficial compact bone filled with much deep spongy bone.
The carpal bones and tarsal bones are all examples of this classification of bones.
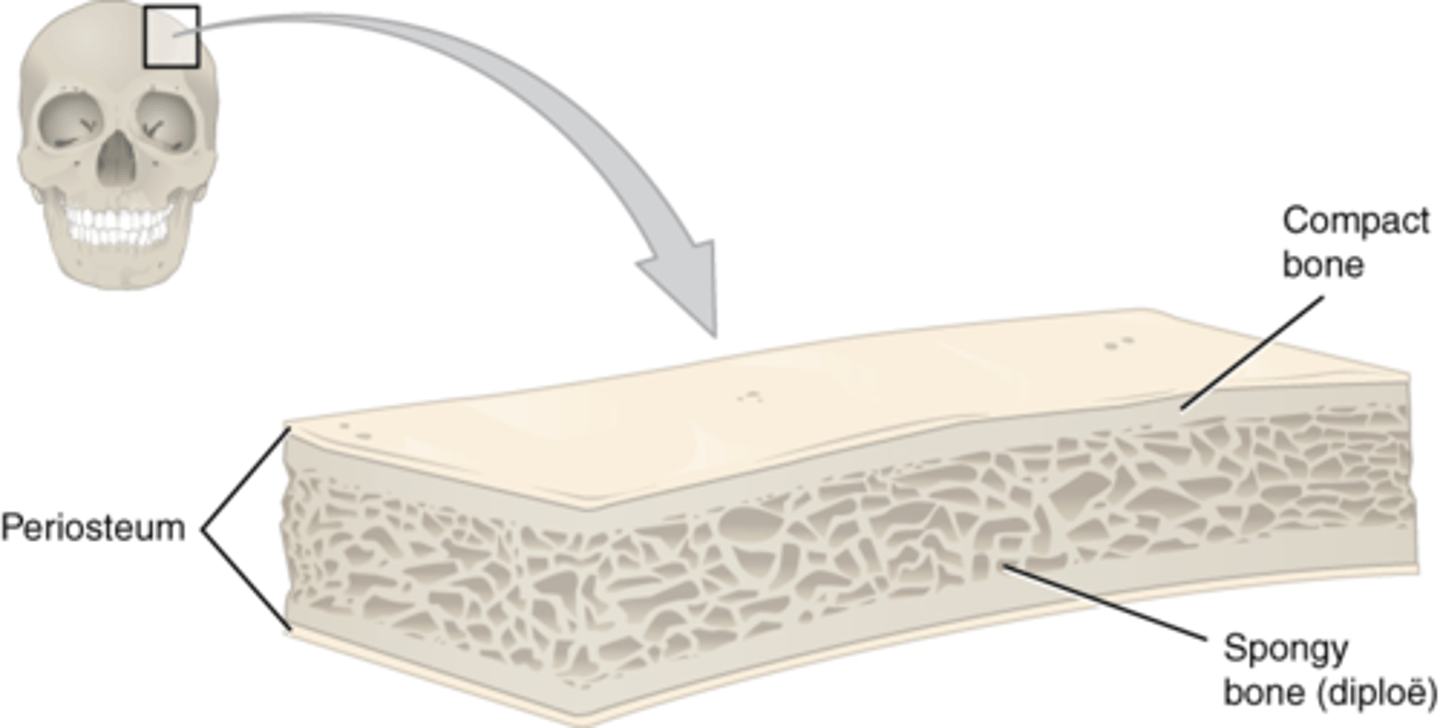
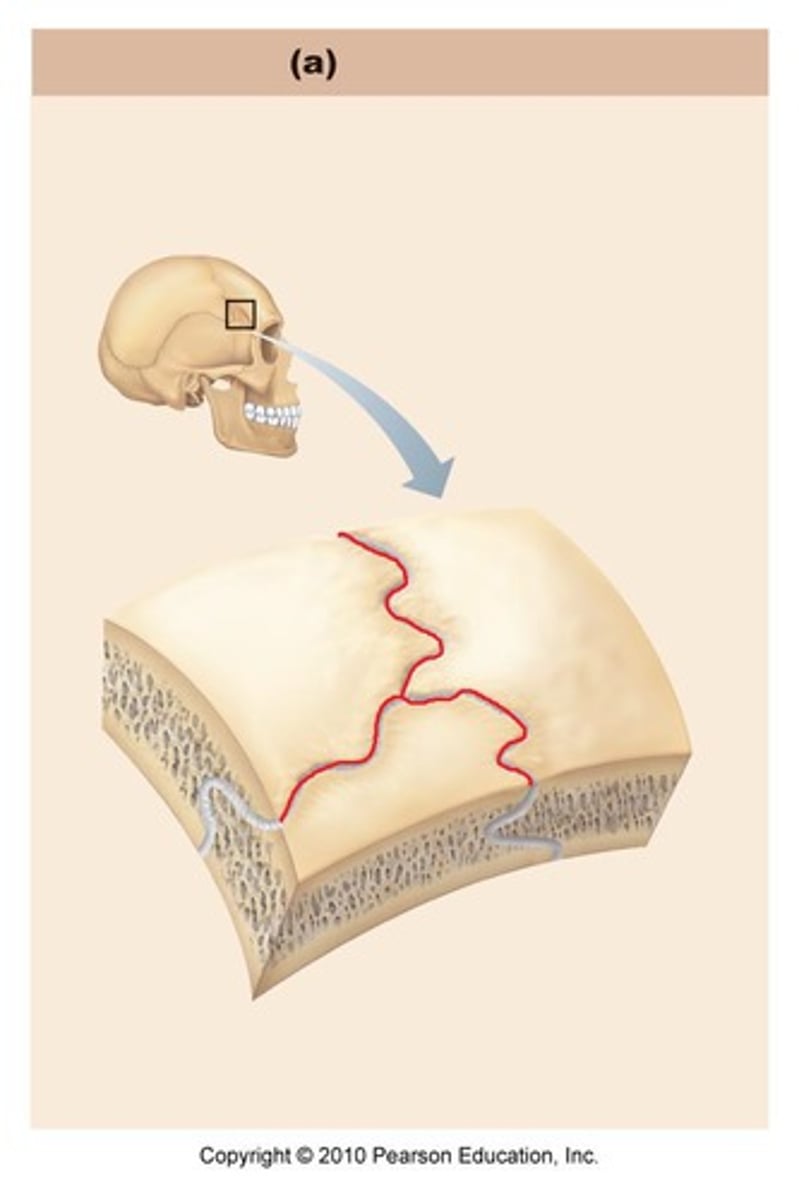
flat bones
These bones have a flattened curved appearance.
They are composed of two surfaces of compact bone enclose a layer of spongy bone.
Examples include the skull, clavicle (collar bone), sternum (breast bone), and ribs.
irregular bones
These bones do not fit in any of the other three classifications due to their unique shape.
- These bones have relatively thin layers of superficial compact bone surrounding much deep spongy bone.
- The scapula (shoulder blade), vertebrae, and pelvis are examples of irregular bones.
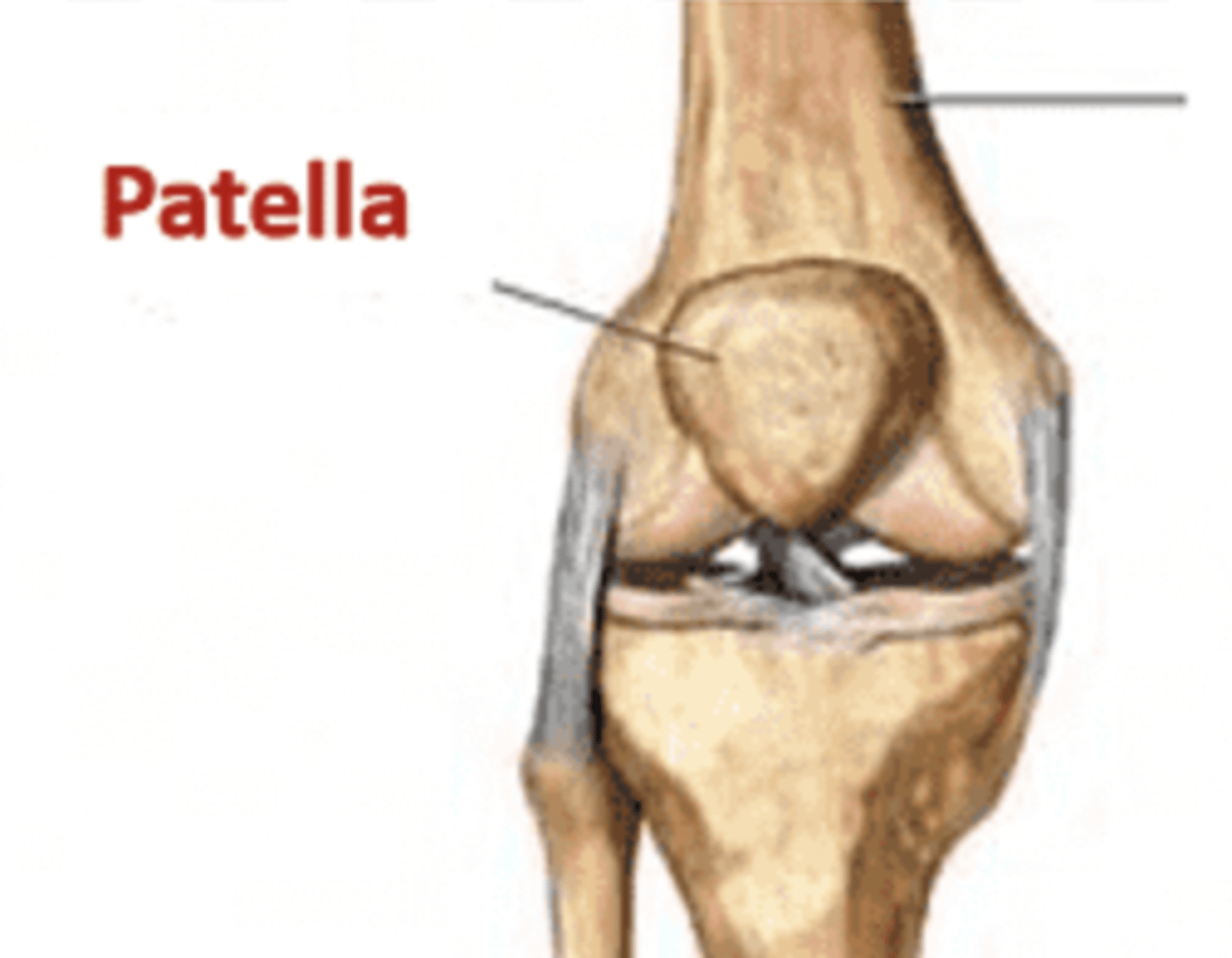
round (sesamoid) bones
The small bones that are found adjacent to joints that assist with motion, and are embedded in tendons.
The patella (kneecap) is classified as this type of bone.
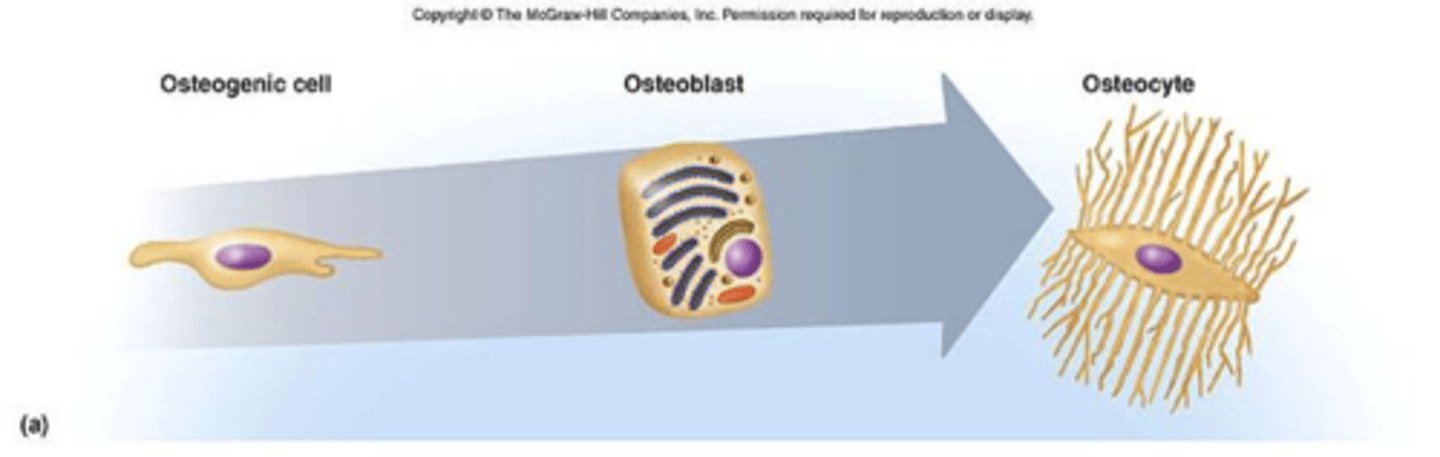
osteoprogenitor cells
Bone stem cells derived from mesenchyme.
Undergo mitosis to become the osteoblasts.
These cells are unspecialized cells that are found in the inner part of the periosteum, the endosteum and within the central canal of compact bone.
They multiply continually and can differentiate into osteoblast cells when needed to form new bone.
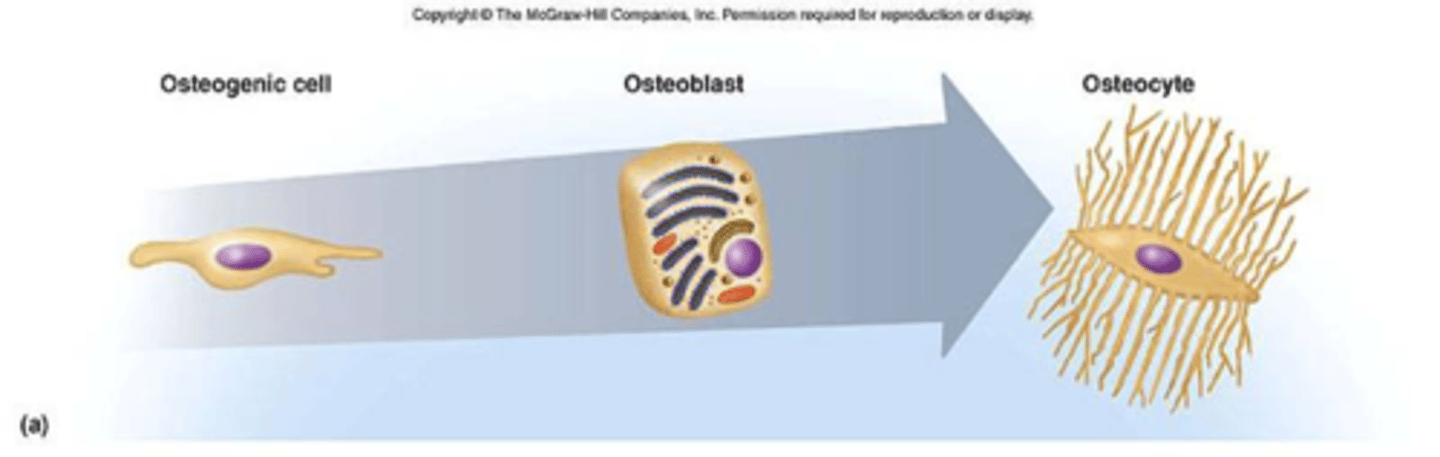
osteoblasts
These cells originate from osteoprogenitor cells and are the bone-forming cells.
They secrete the collagen and other organic components that make up the matrix part of the bone.
They are unable to divide.
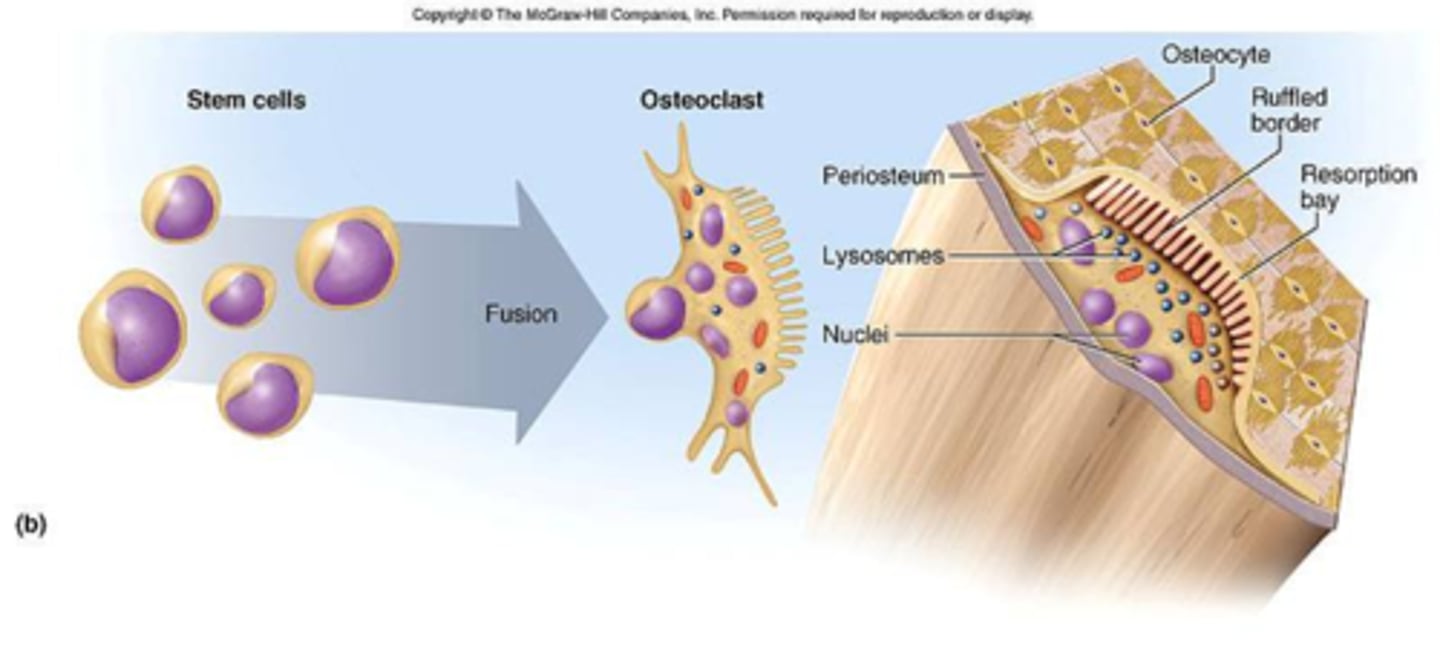
osteoclasts
Large cells that resorb or break down bone matrix
Work to break down bone and thereby add calcium and phosphates to the blood in a process called resorption.
This is an important process for the growth and repair of bone tissue.
They originate from the same bone marrow cells which produce monocytes in the blood.
They fuse together and form large osteoclast cells.
osteocytes
Mature bone cells that come from osteoblasts.
They are former osteoblasts that became trapped in the matrix they secreted.
They are found in tiny cavities called lacunae which are connected by channels or canals called canaliculi.
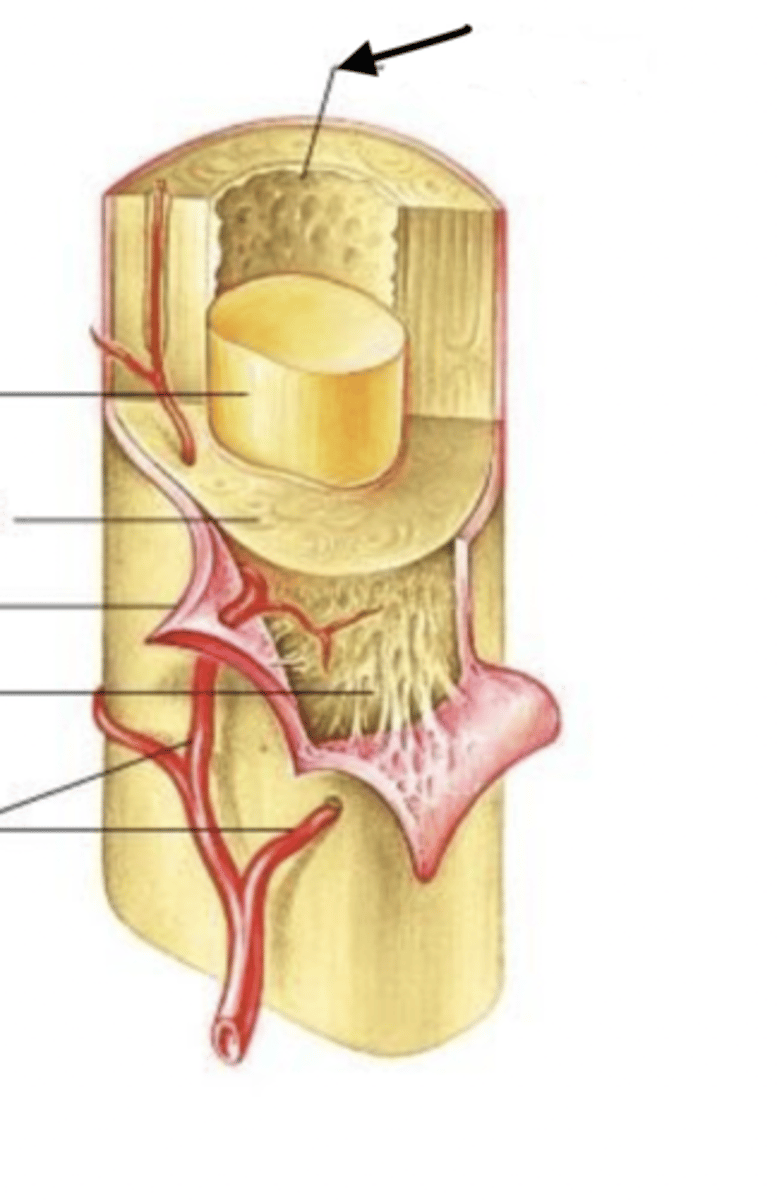
compact bone
Hard, dense bone tissue that is beneath the outer membrane of a bone (the periosteum)
This type of bony tissue is based on a microscopic arrangement of bone called an osteon.
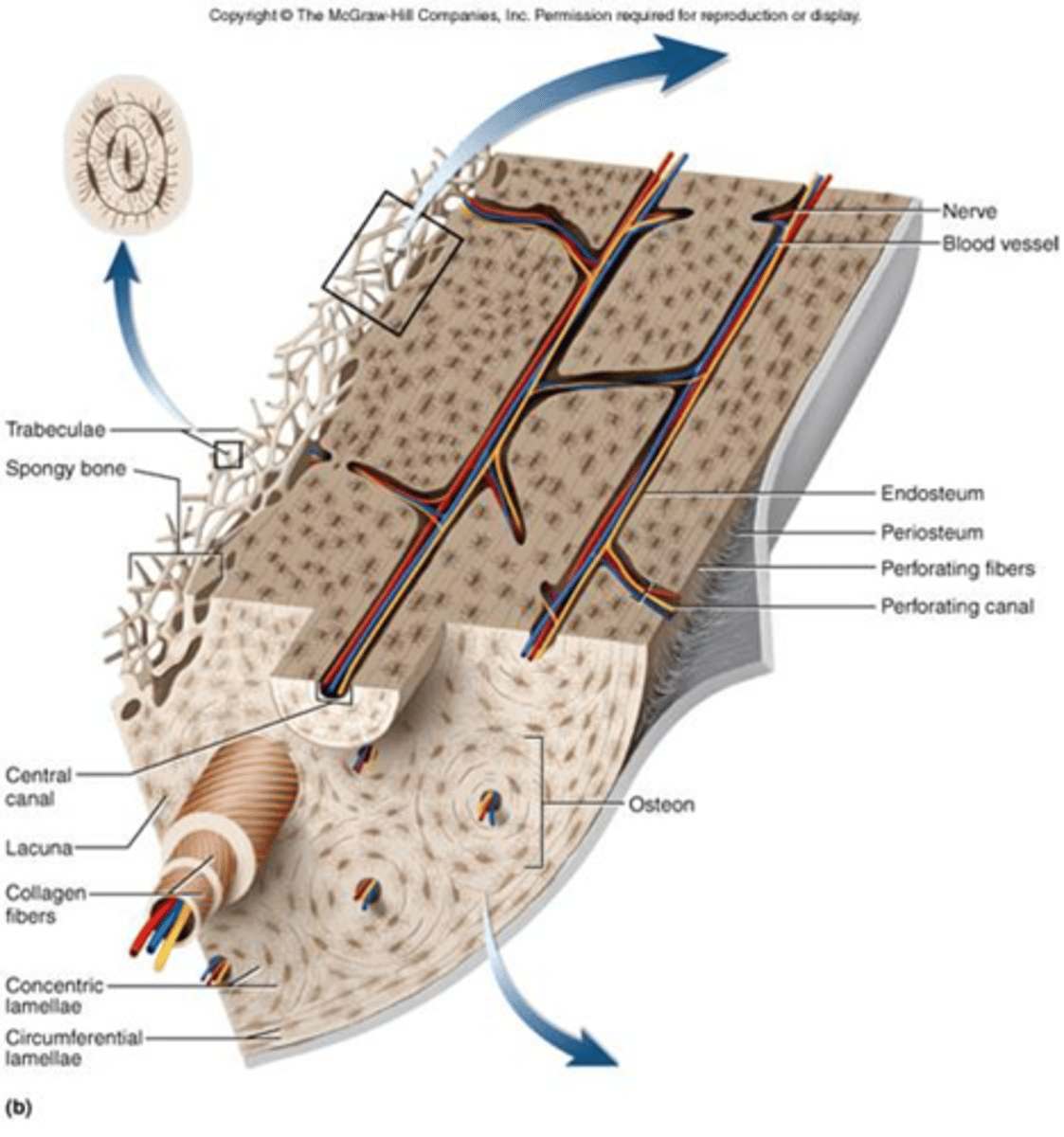
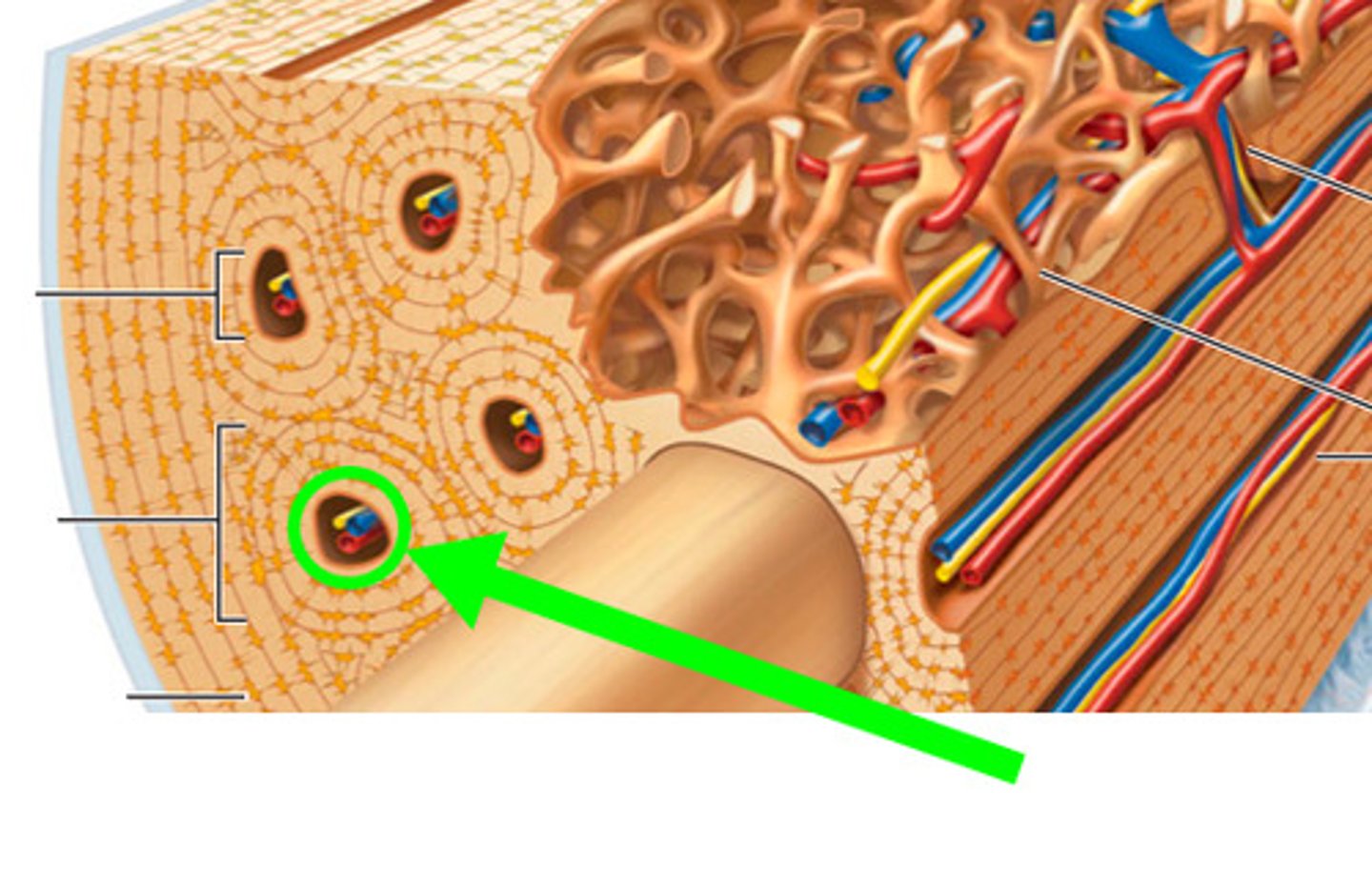
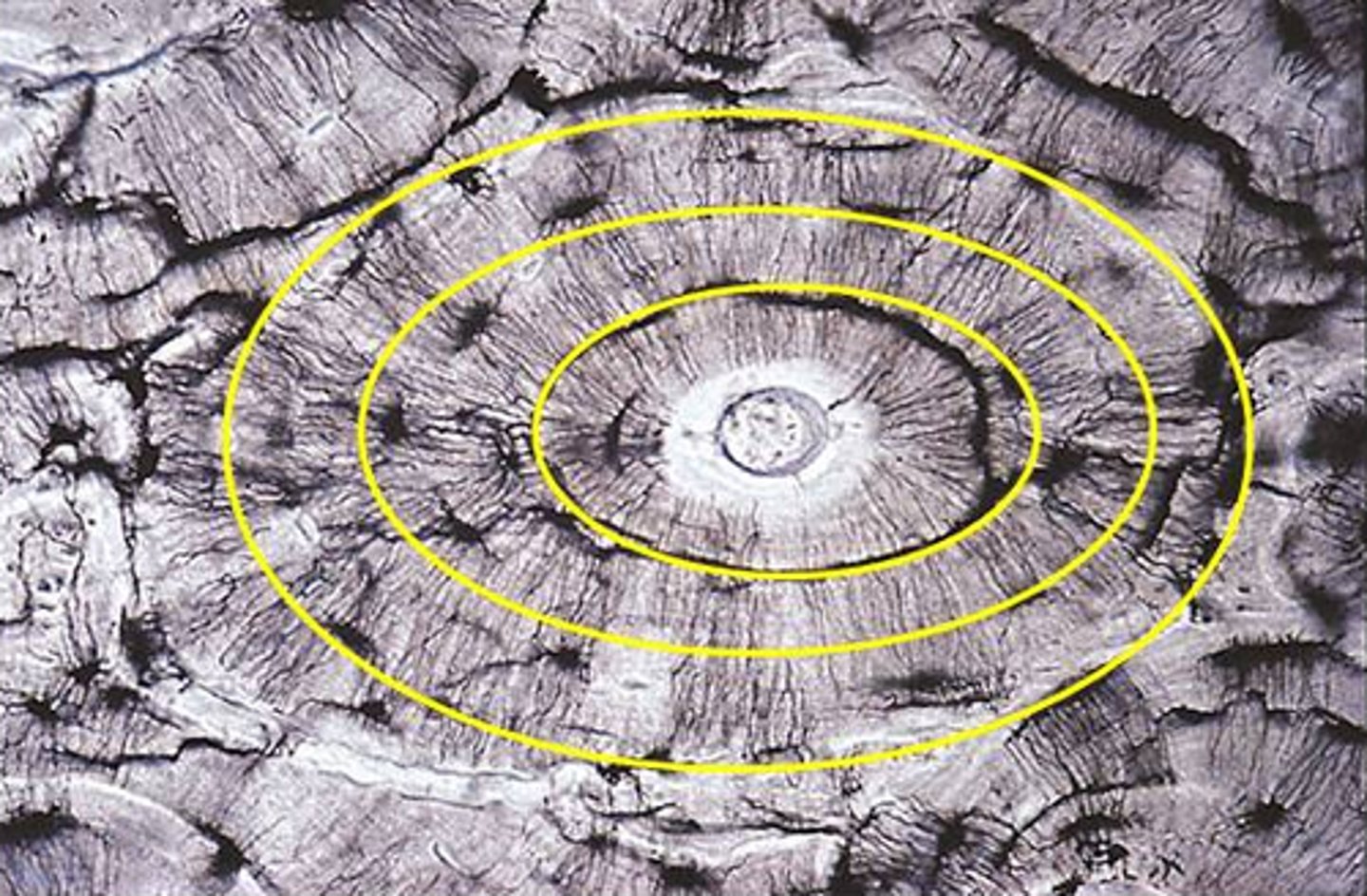
osteon
Columns of bone tissue arranged in a longitudinal pattern.
They give the bone great strength in one direction.
This is the functional unit of compact bone
It is made up of the lamella and the central canal of compact bone.
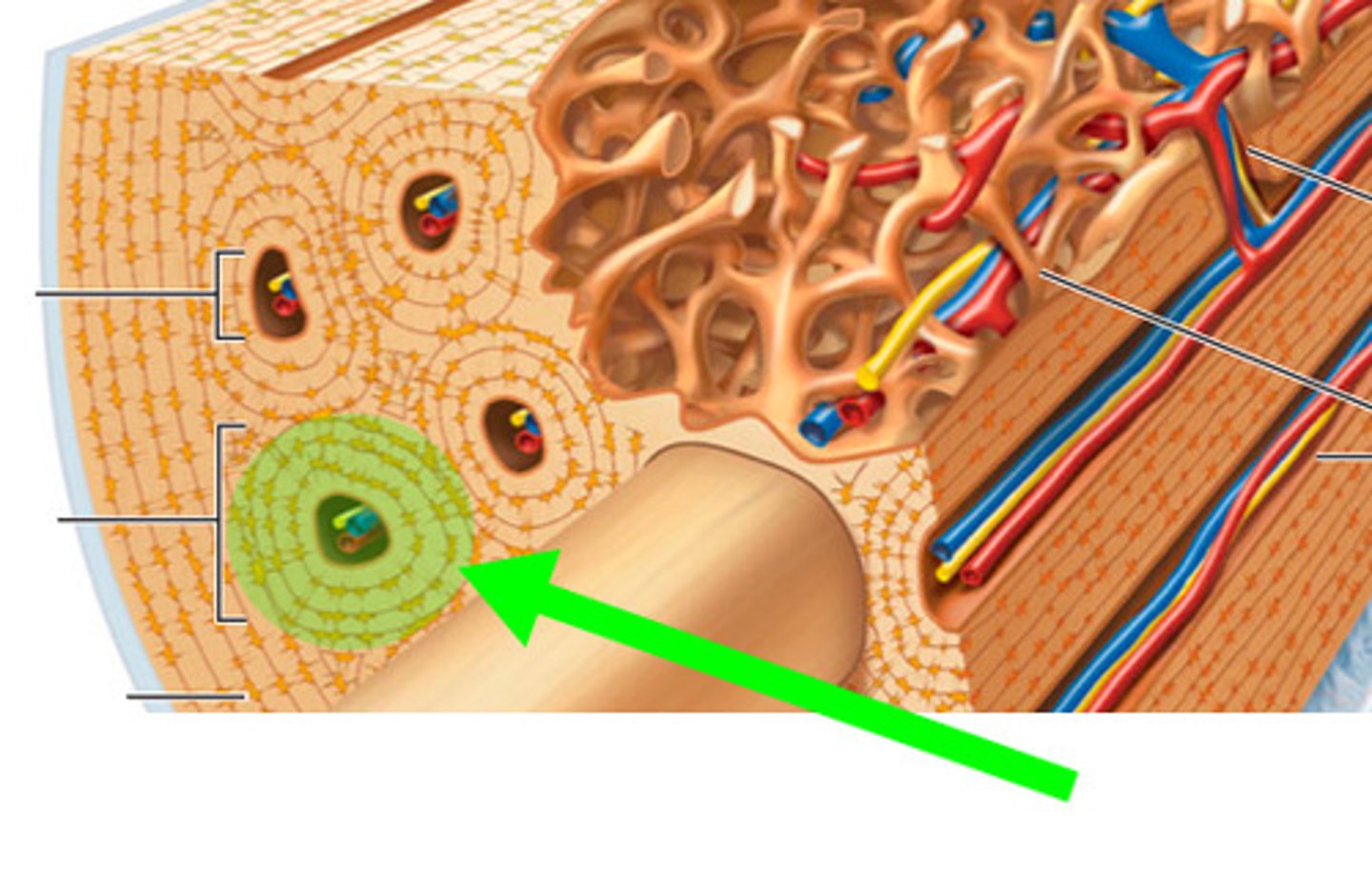
Central (Haversian) Canal
This center area of compact bone is where the blood vessels are found.
canaliculi
The microscopic canals between the lacunae.
Osteocytes project into these canals.
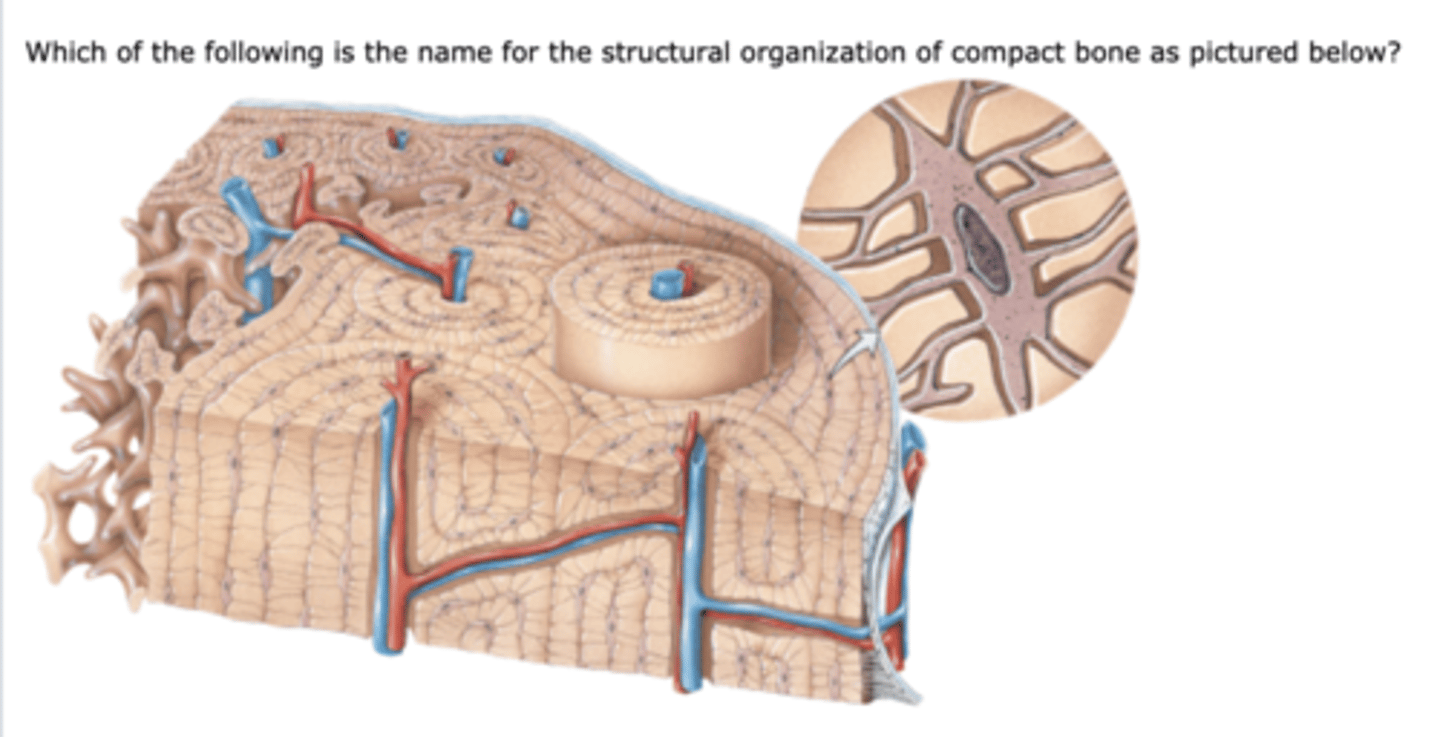
Volkmann's (perforating) canals
Channels lying at right angles to the central canal, connecting blood and nerve supply of the periosteum to that of the Haversian canal
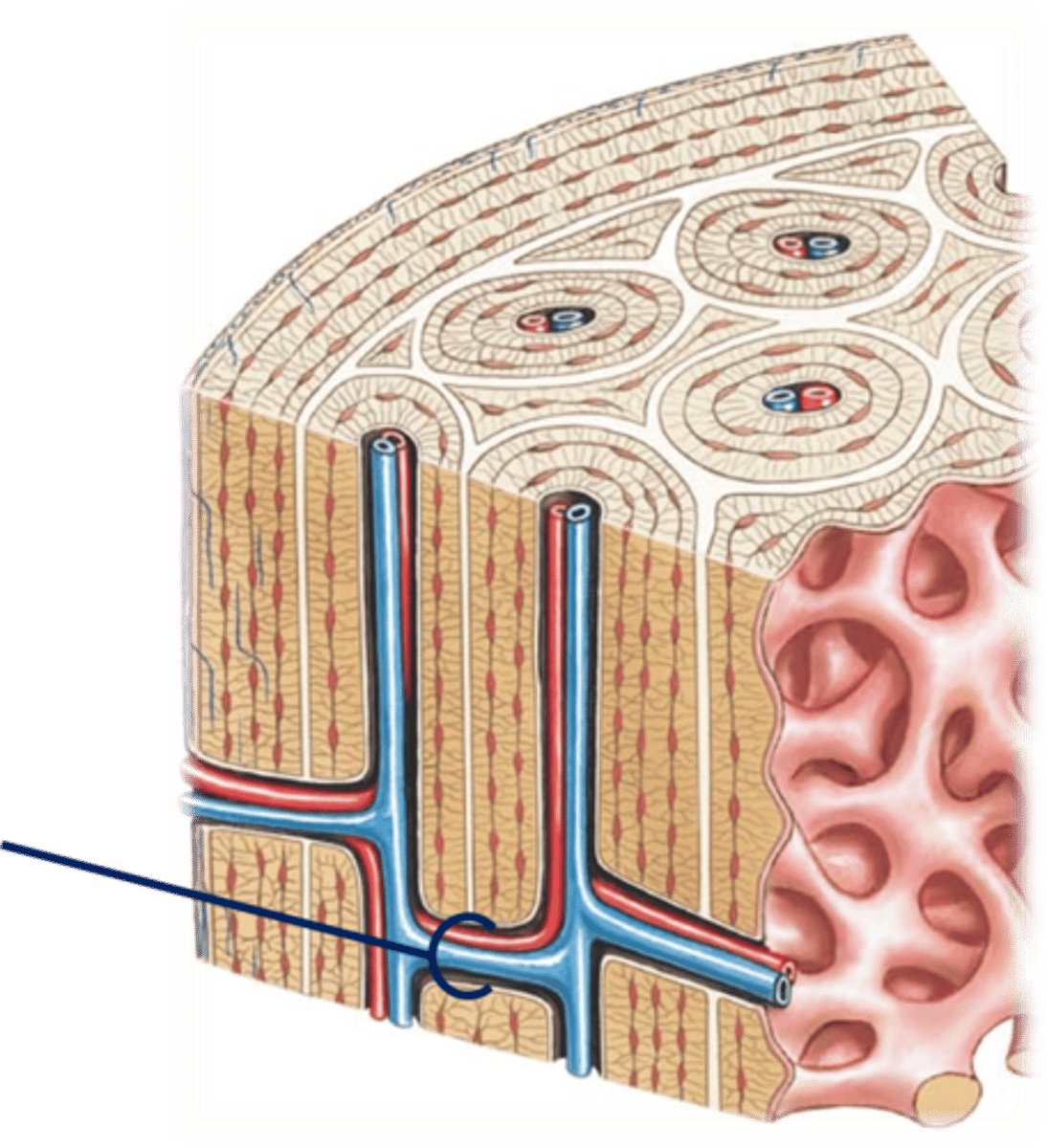
lacunae
Small cavities between the lamellae which contain osteocytes.
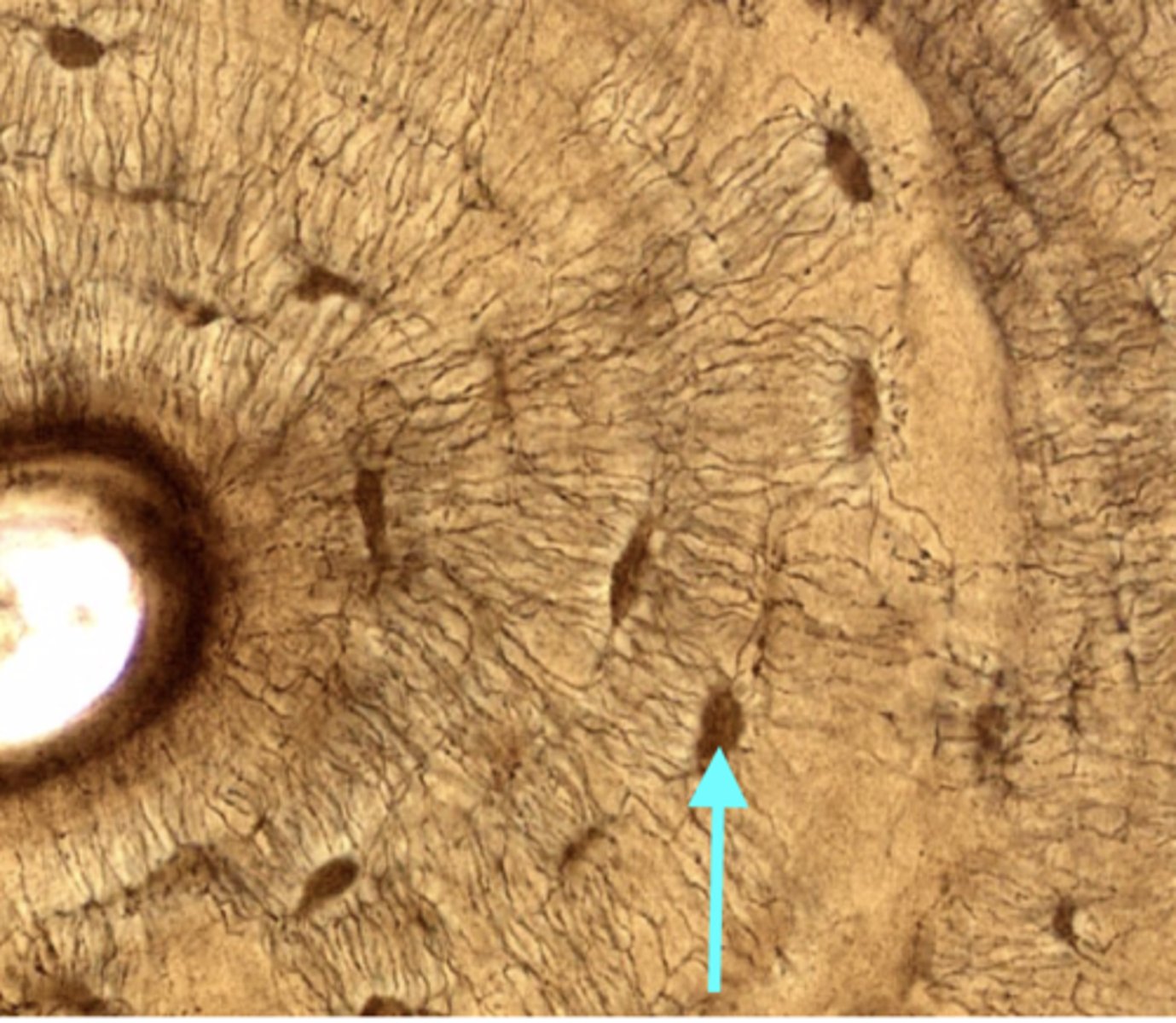
lamellae
The layers of matrix (ground substance), or specifically hydroxyapatite, arranged in concentric rings around the central (Haversian) canal.
Hydroxyapatite
Made of calcium phosphate and calcium hydroxide and provides compressional strength for compact bone.
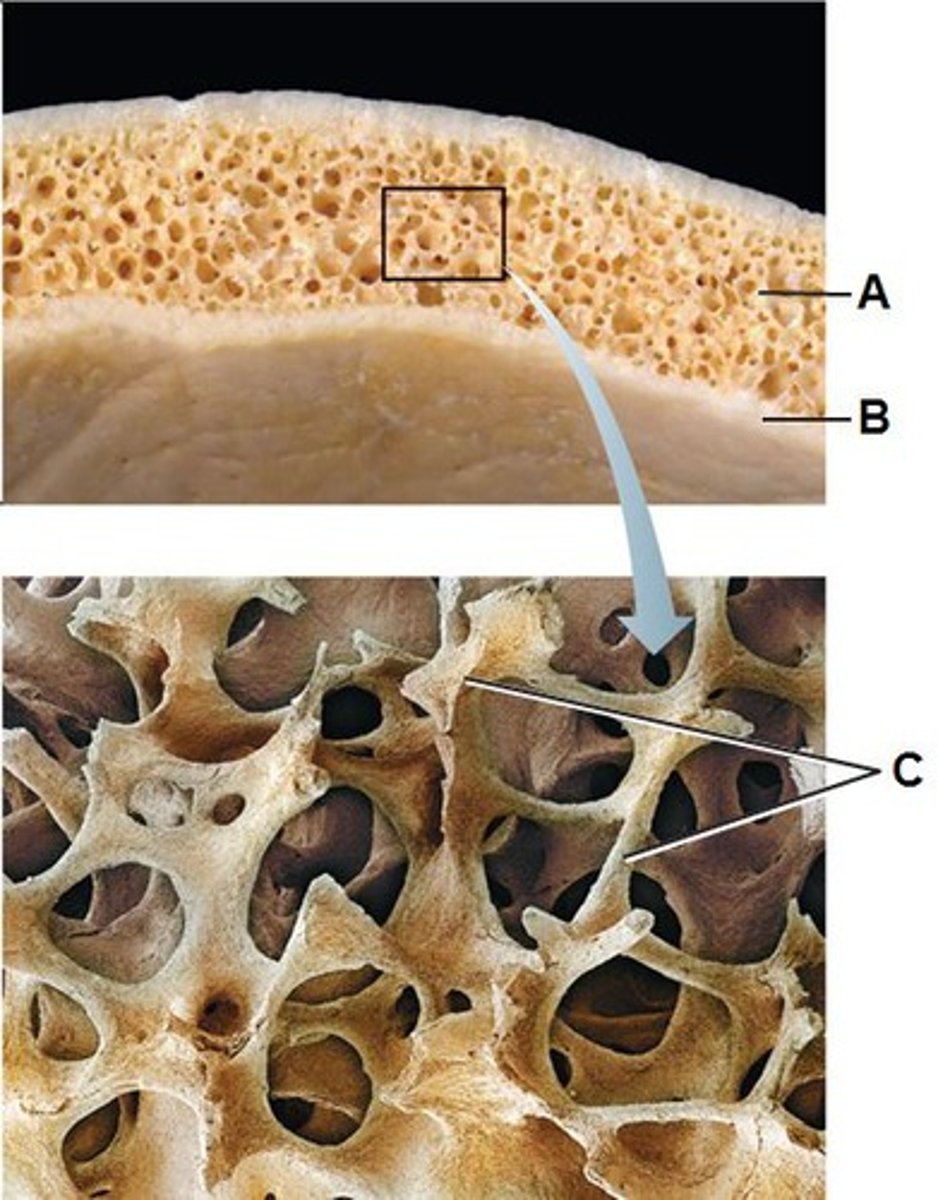
spongy bone
This type of bony tissue is based on a microscopic arrangement of bone called trabeculae.
Looks less organized than the Haversian system, but the trabeculae are arranged for maximum resistance to
stress.
Contains irregularly arranged lamellae and osteocytes interconnected by canaliculi.
No osteons.
Nutrients diffuse through the canaliculi to the osteocytes within the narrow spaces between the trabeculae.
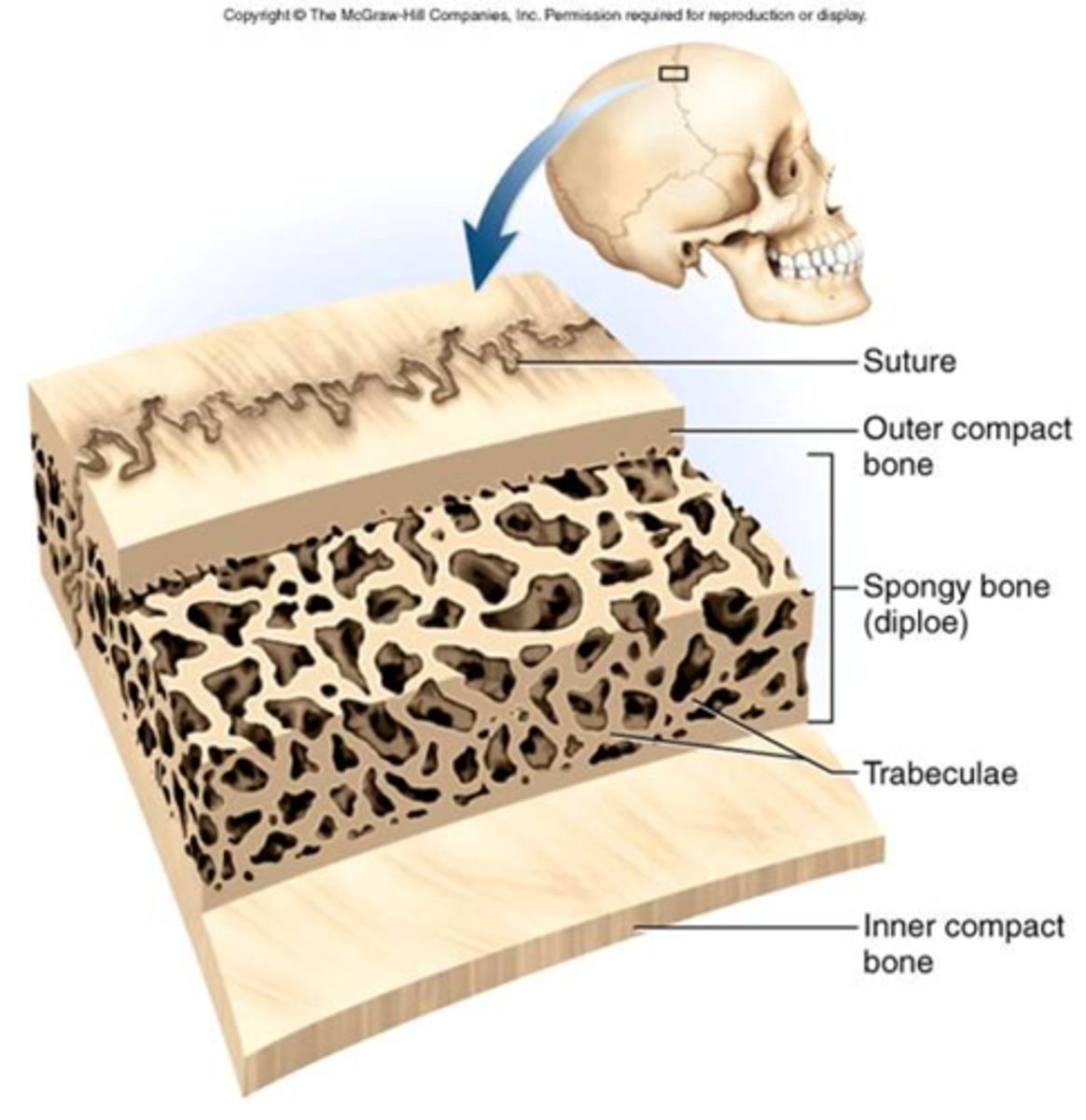
trabeculae
Bony spicules running different directions inside spongy bone.
There are many spaces or holes in it which are filled with bone marrow.
They give bone great strength in many directions.
periosteum
A dense fibrous connective tissue wrapping around bone.
Extensions of this tissue to other bones are called ligaments. When this tissue extends to muscle, it's called a tendon.
Thus, this membrane serves as a way to connect all the bones and muscles together.
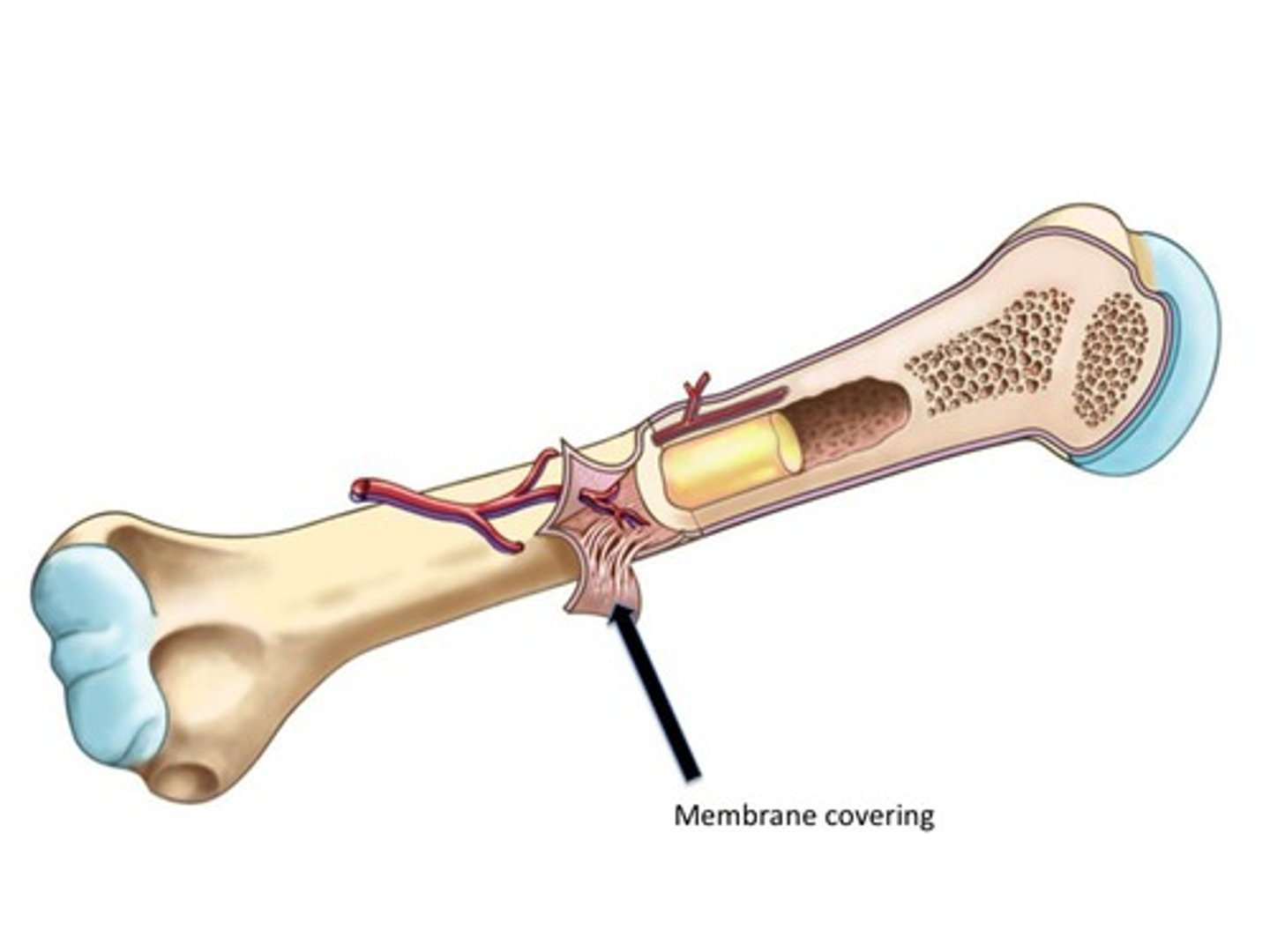
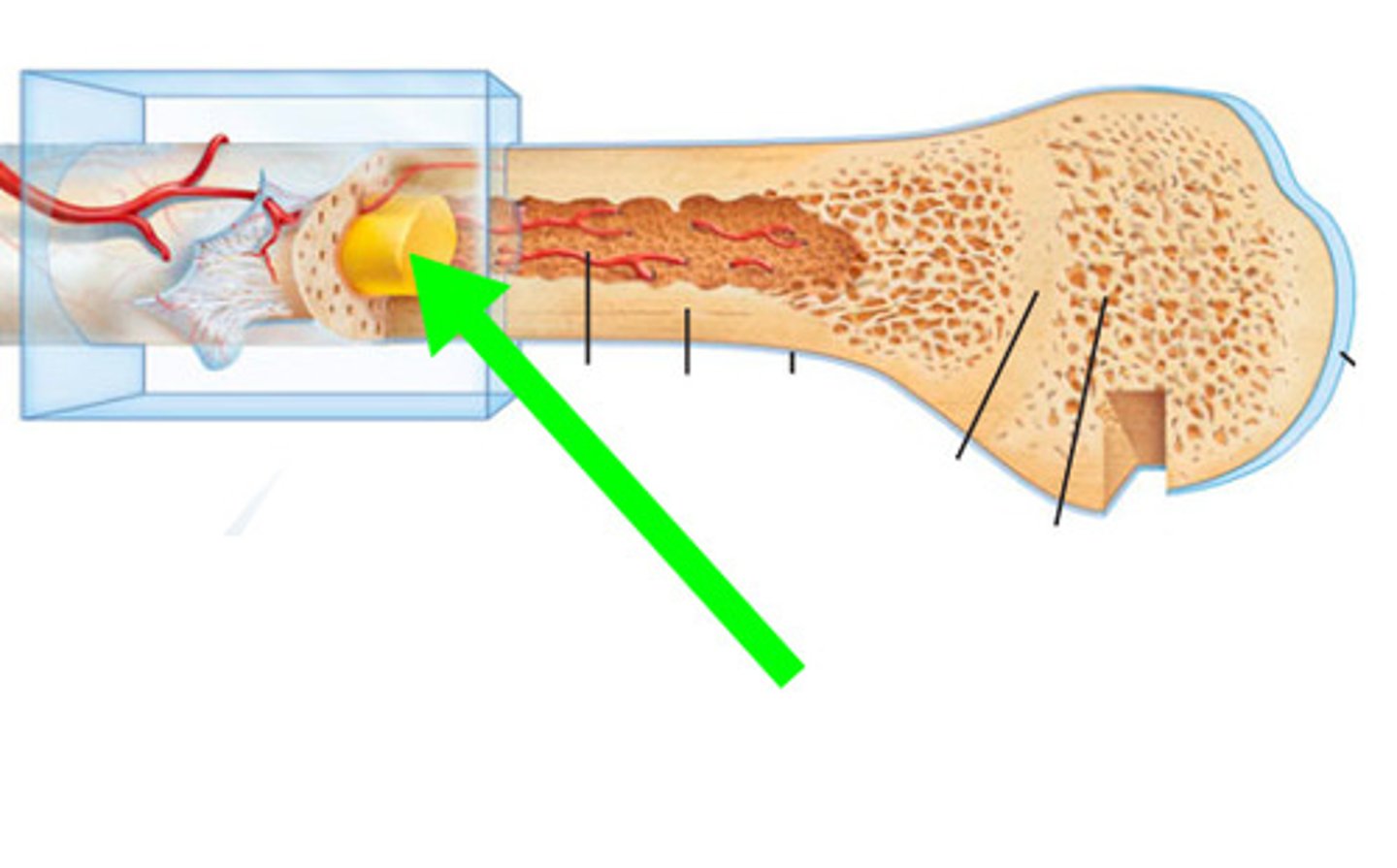
endosteum
A dense fibrous connective tissue lining the inside of bone (medullary cavity). This tissue covers the trabeculae of spongy bone tissue.
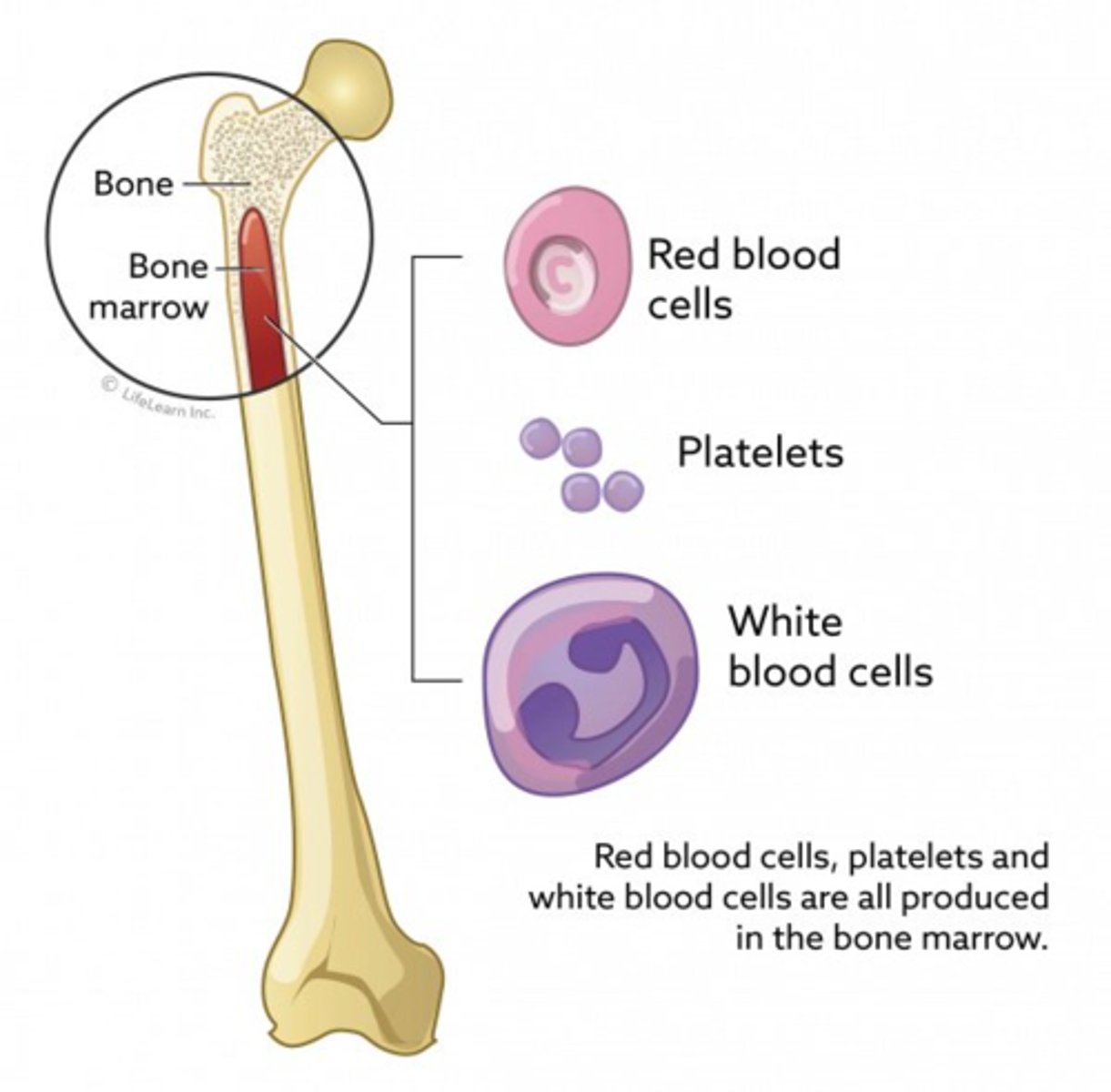
bone marrow
Fills the medullary cavity in the middle of bone.
This is the site of hematopoiesis, blood cell development.
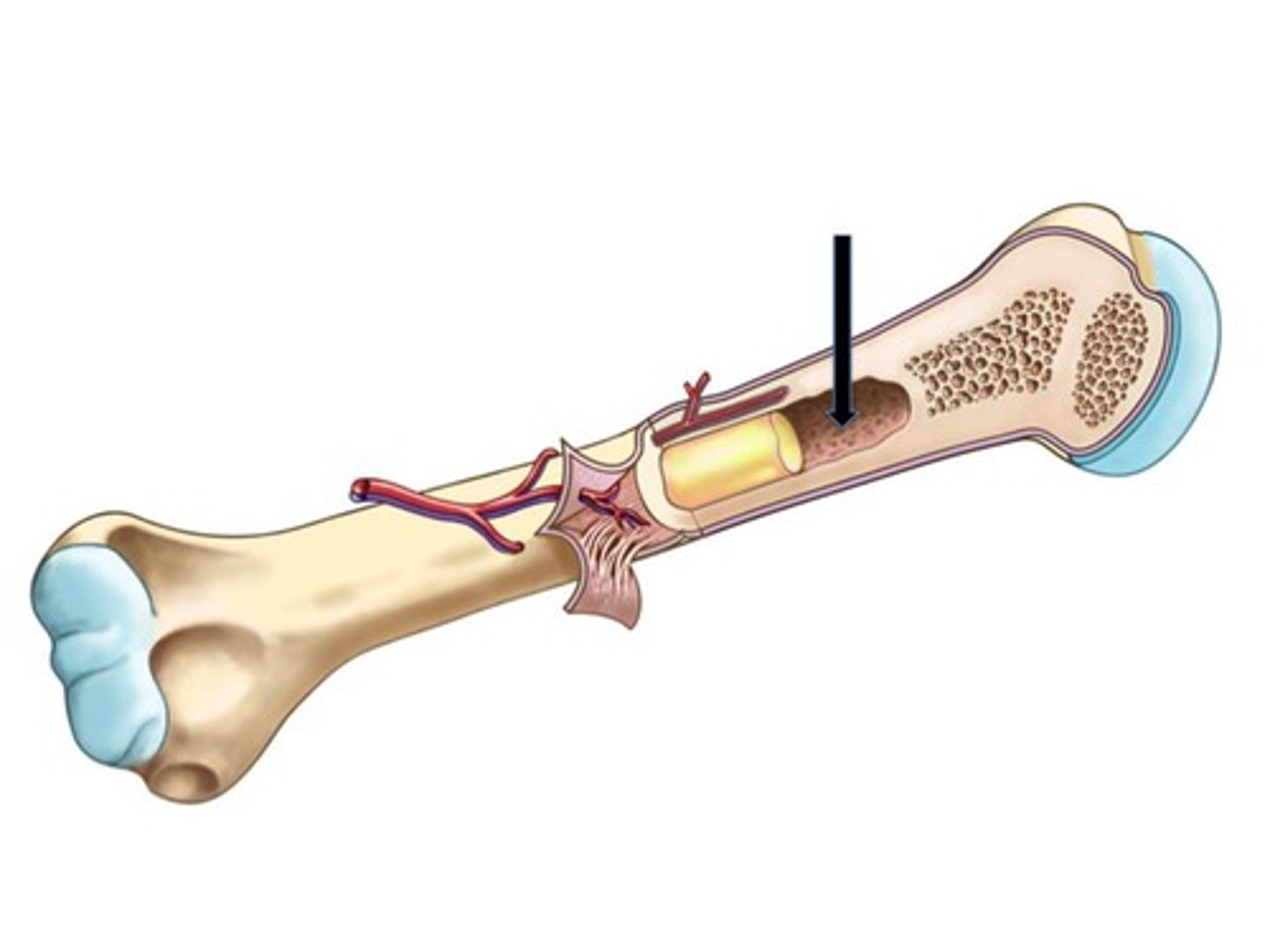
medullary cavity
cavity within the shaft of the long bones filled with bone marrow
red bone marrow
Red marrow is present in children. Red marrow is developing blood cells.
Since the greatest majority of developing blood cells are erythrocytes (red blood cells), this tissue has a reddish color.
Red marrow is present in adults in spongy bone
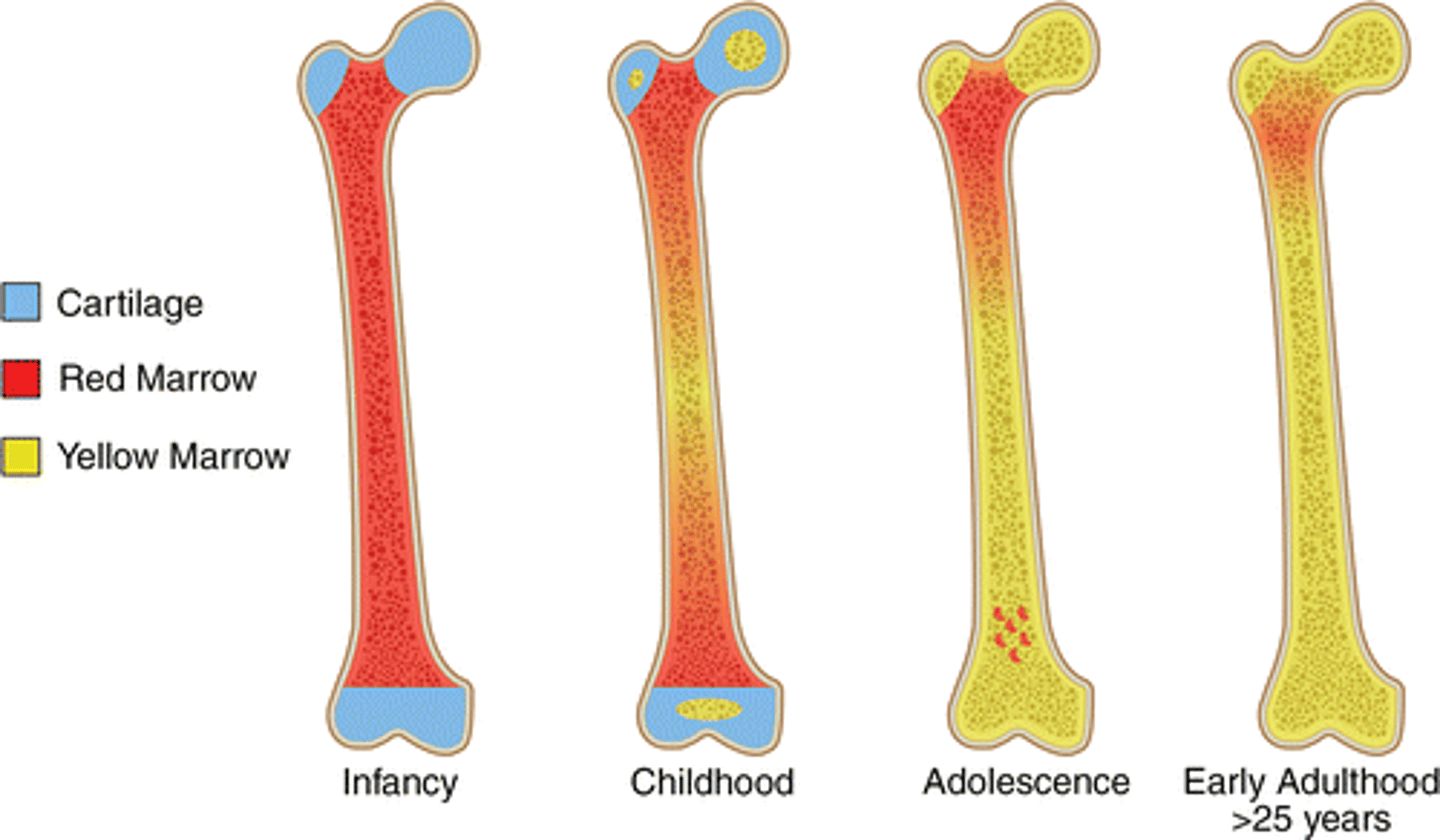
yellow bone marrow
Present in the medullary cavities of long bones in adults.
This tissue is composed of developing blood cells and adipose tissue (fat) which gives the tissue its yellow color.
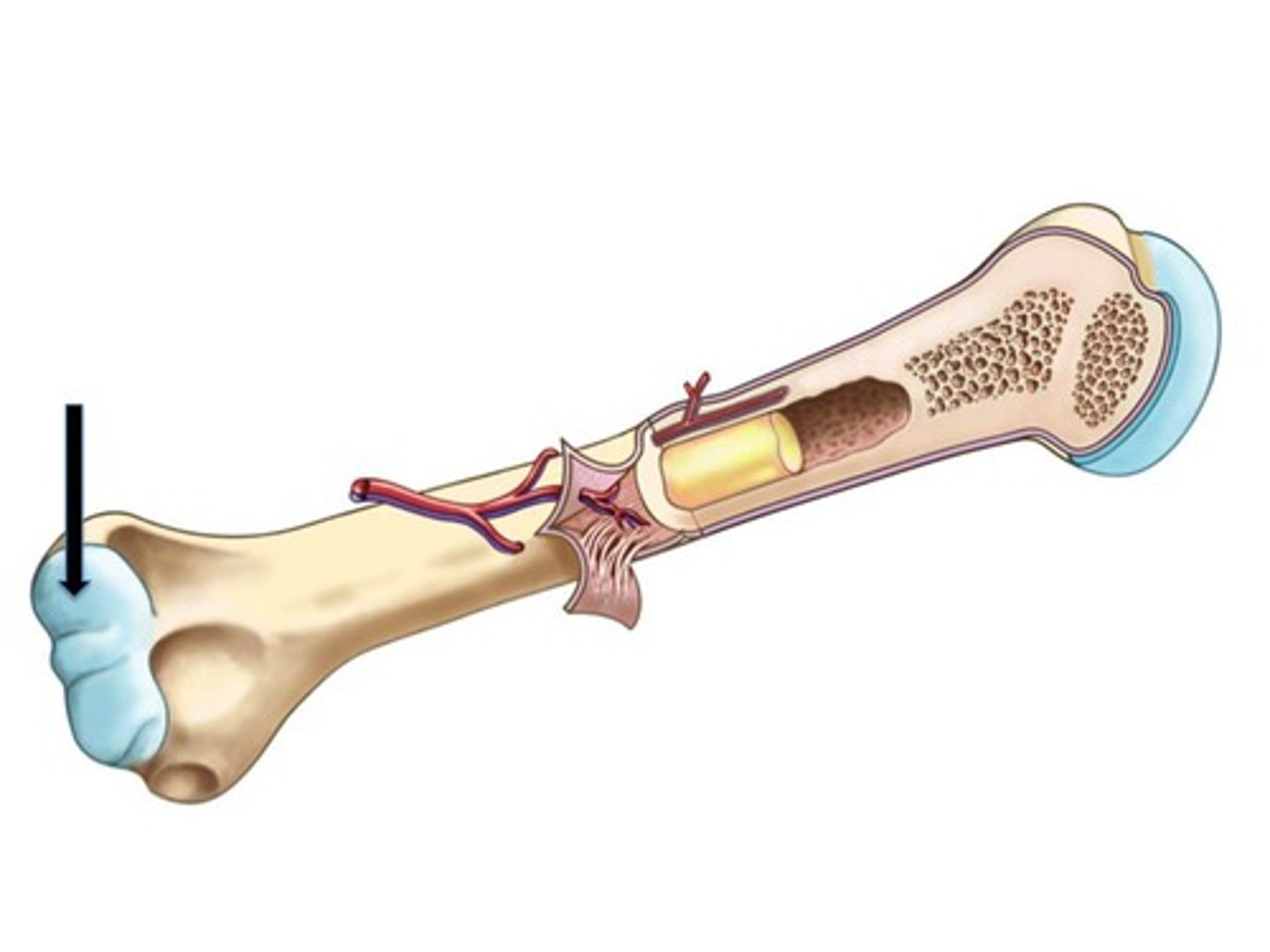
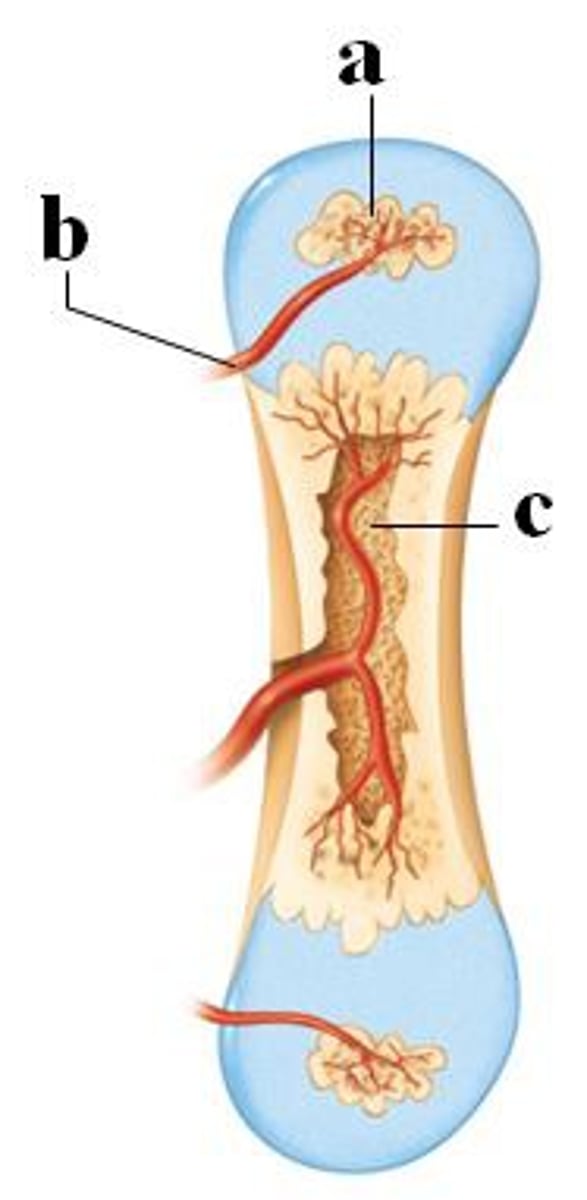
diaphysis
The middle shaft of a long bone consists of a thick layer of superficial compact bone.
The compact bone surrounds a thinner layer of spongy bone tissue.
A space called the medullary cavity is located deep within bone and is filled with yellow bone marrow.
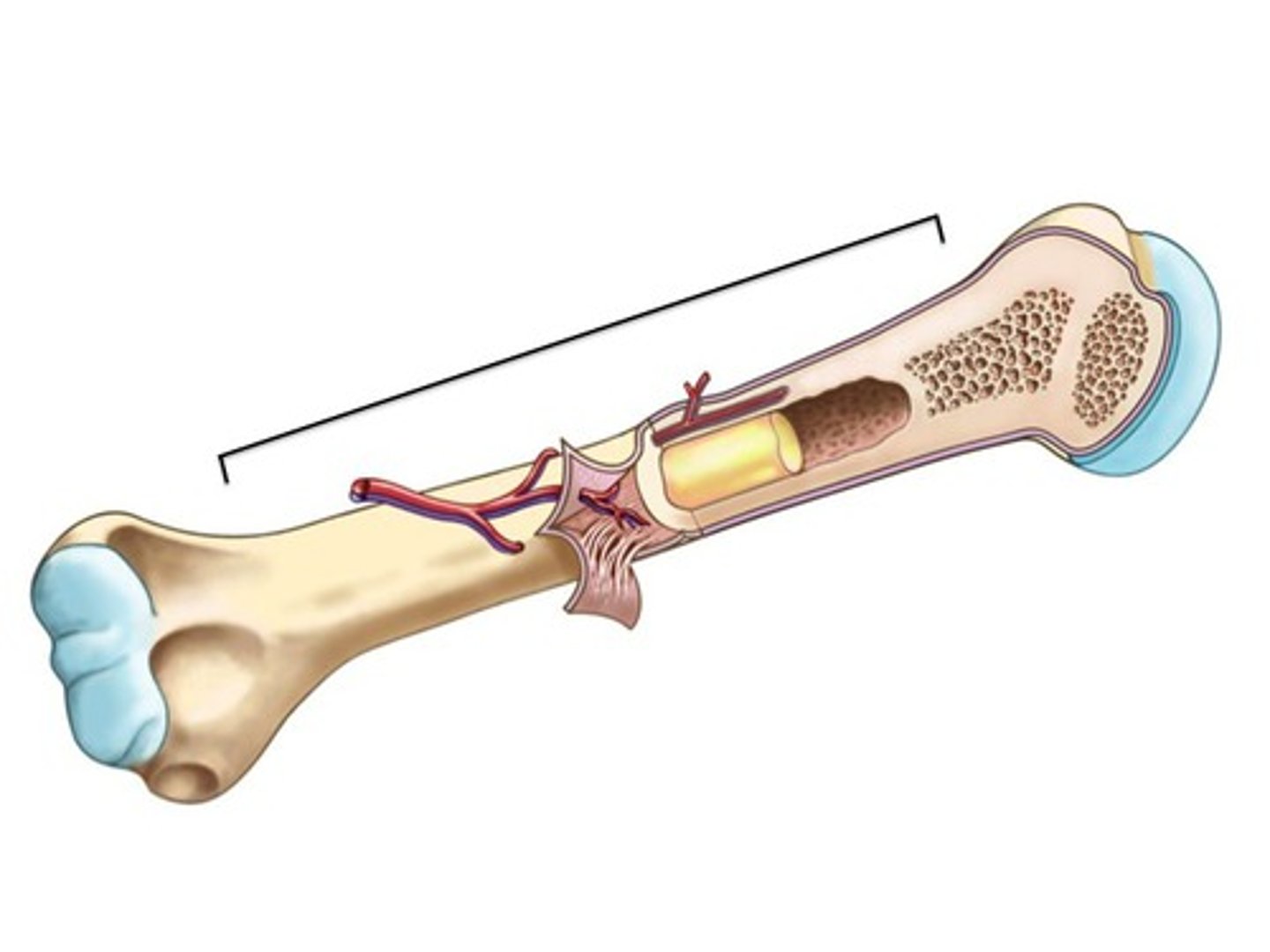
epiphysis
The two ends of a long bone have a greater circumference compared to the diaphysis (shaft).
They are also composed of the same layers of bone tissue present in the diaphysis (compact bone surrounds a thinner layer of spongy bone tissue).
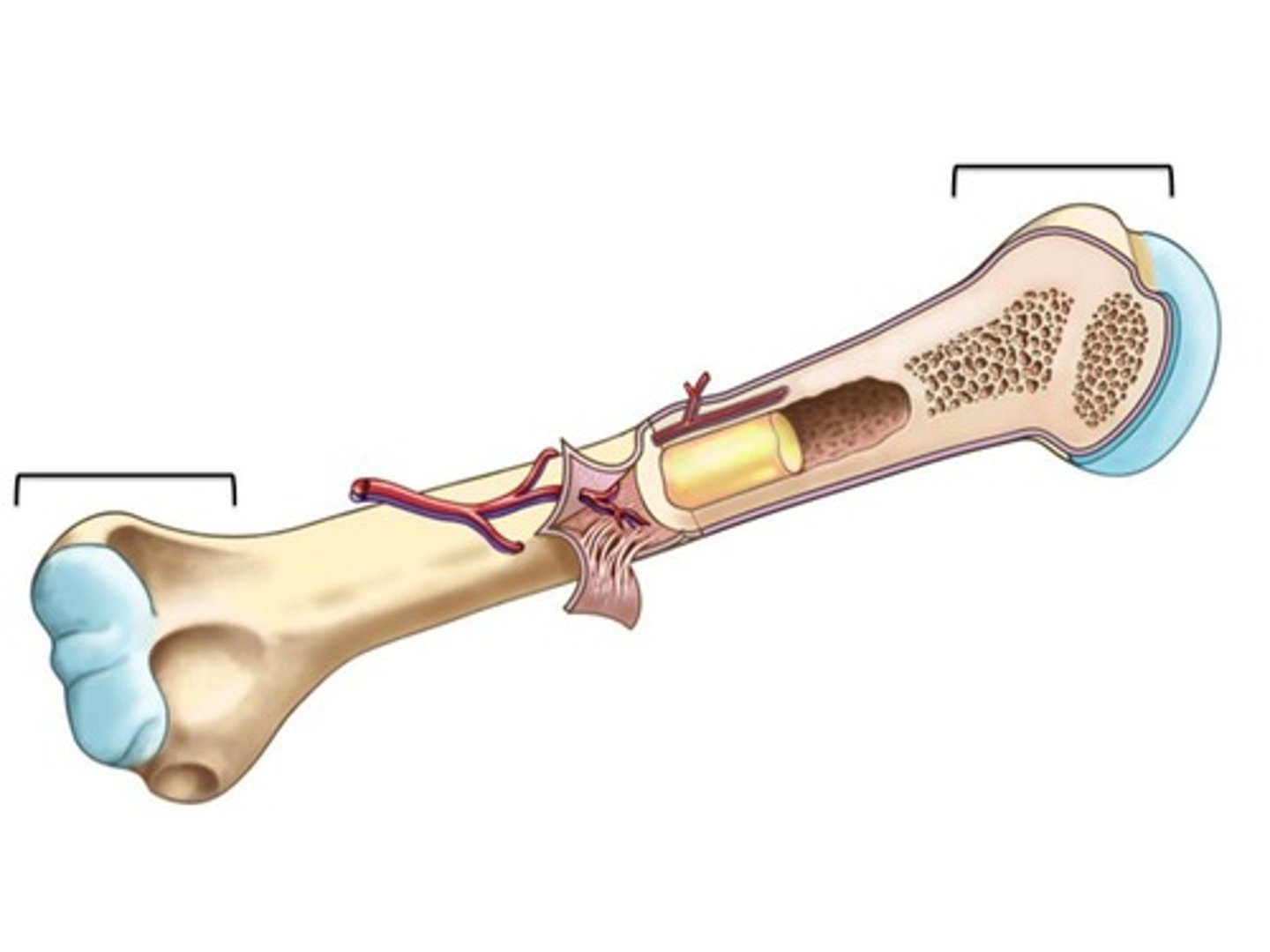
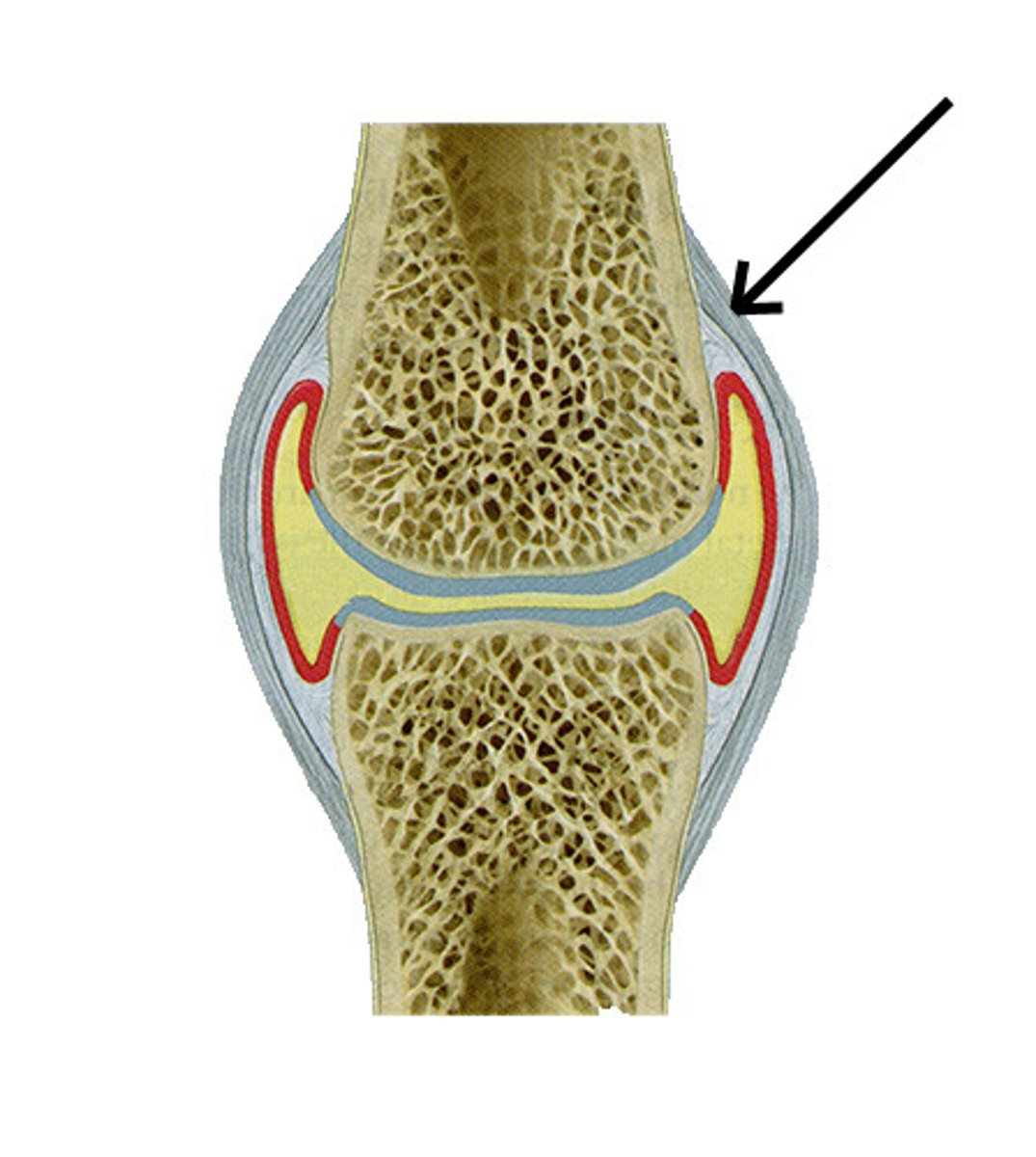
articular cartilage
Hyaline cartilage that covers the ends (epiphyses) of long bones.
It acts as a shock absorber during movement by cushioning the ends of the bones.
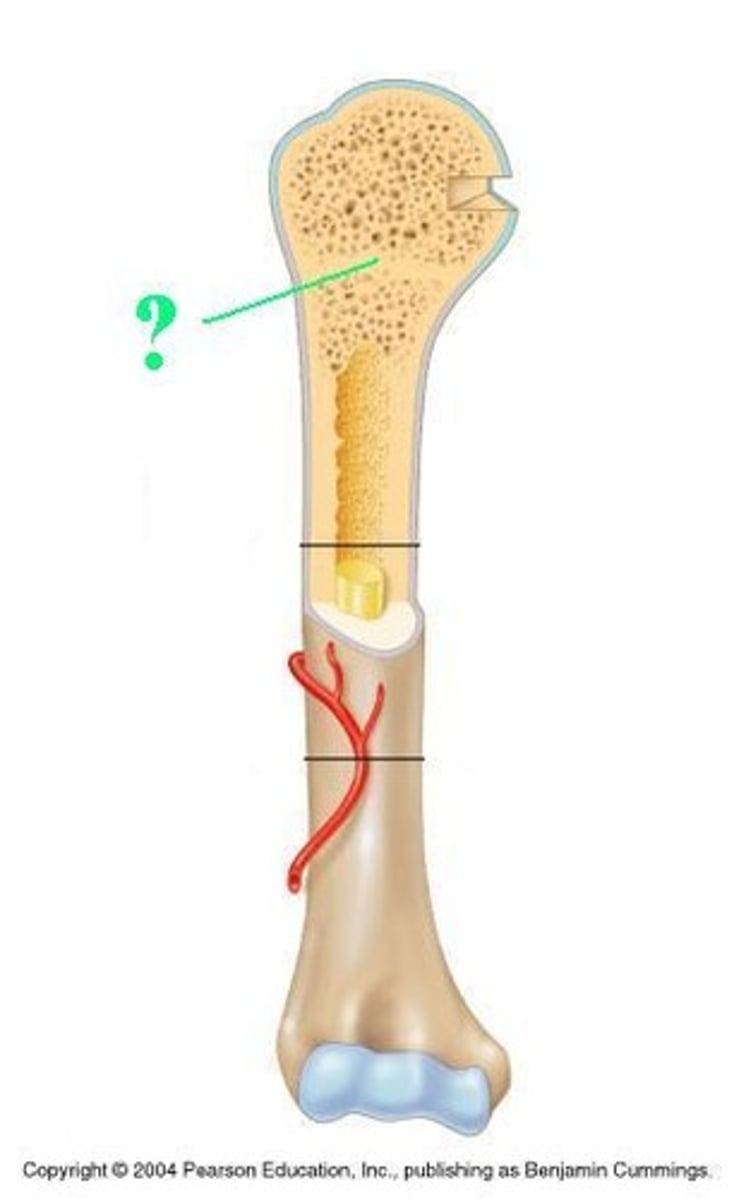
epiphyseal plate
A band of cartilage located between the diaphysis and each epiphysis.
This area is the site of long bone growth in children and is frequently referred to as the "growth plate".
Once the person reaches maturity and adult height, the cartilage ossifies or turns to bone.
This area is referred to as the epiphyseal line in adults.
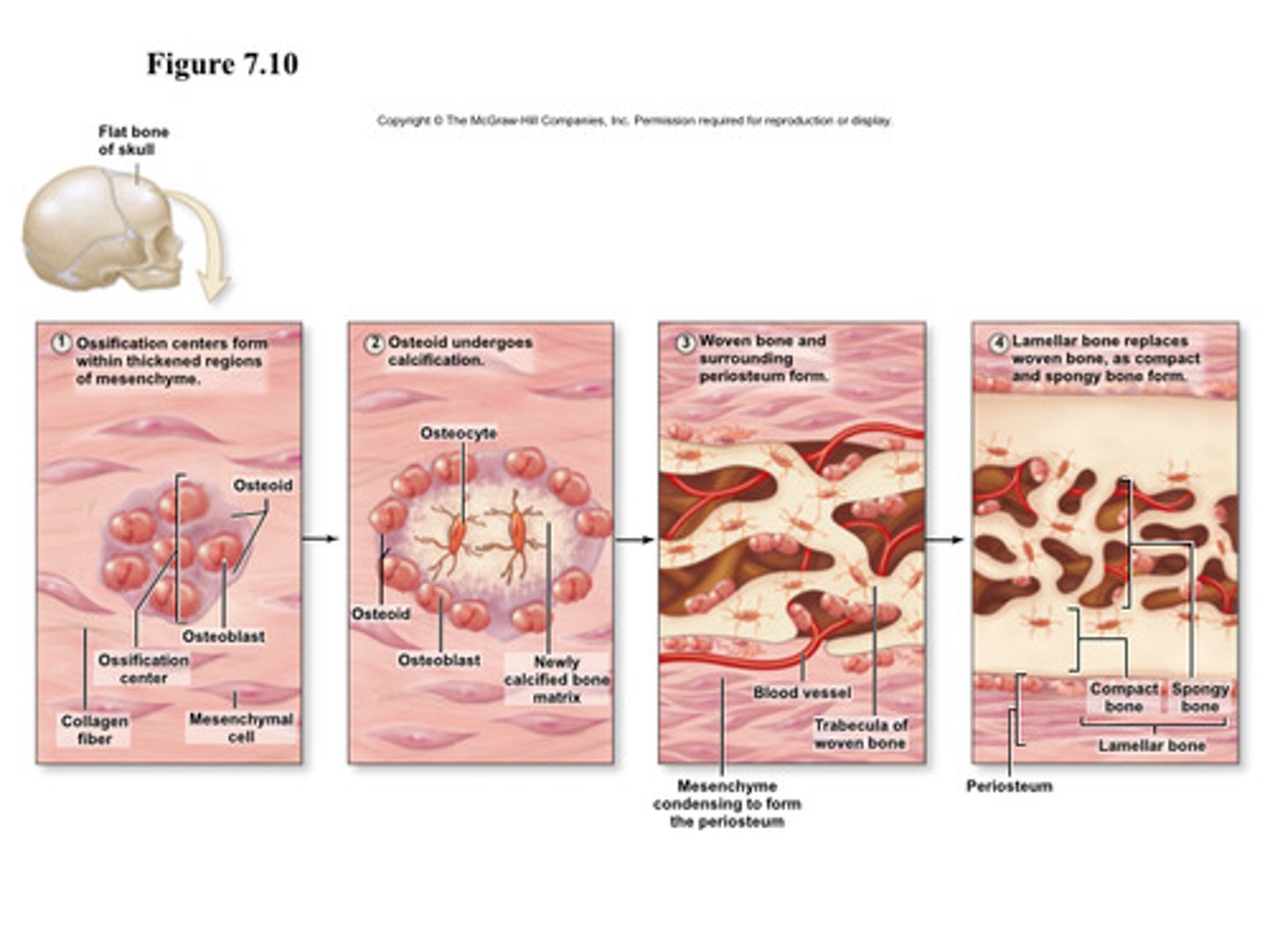
intramembranous ossification
Bone will develop between layers of fibrous connective tissue (i.e. within the membrane).
Cells within this fibrous connective tissue become osteoblasts and form a matrix.
This matrix grows thick and traps more osteoblasts. These osteoblasts become osteocytes.
This is the way the flat bones of the skull and most of the clavicle are formed.
In this process, bones form directly from mesenchymal tissue.
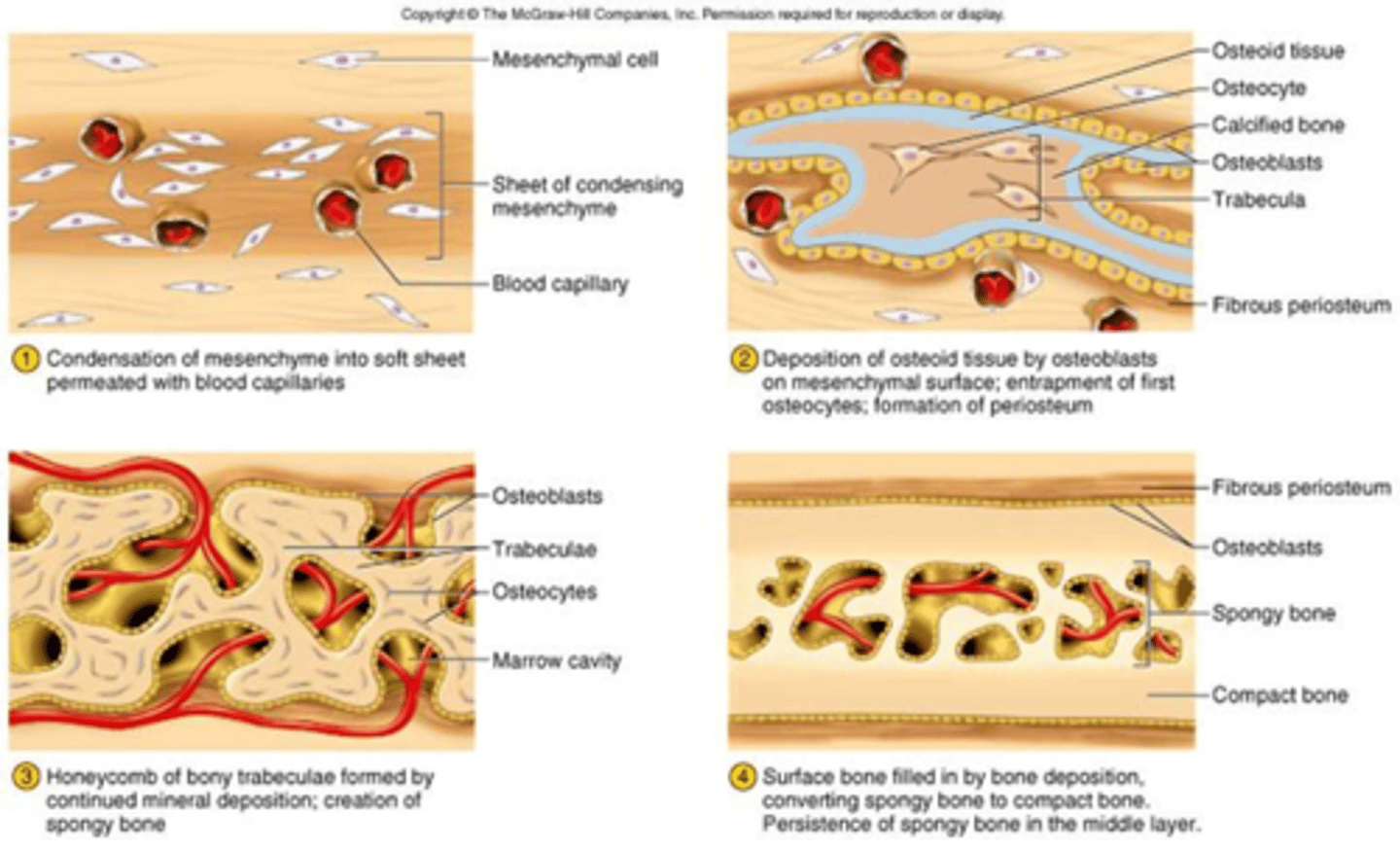
steps of intramembranous ossification
1. Cells in the mesenchyme (the common connective tissue layer) come together and develop into osteoprogenitor cells and then into osteoblasts.
This is the center of ossification. The osteoblasts secrete the organic matrix of the bone until they are completely surrounded by it
2. As the osteoblasts become surrounded by a hard matrix, they form trabeculae which fuse with each other to form the lattice structure of
spongy bone.
3. The internal spaces fill with red bone marrow.
On the outside of the bone, the mesenchyme condenses and eventually becomes the periosteum.
4. The surface of the bone is eventually reconstructed into compact bone
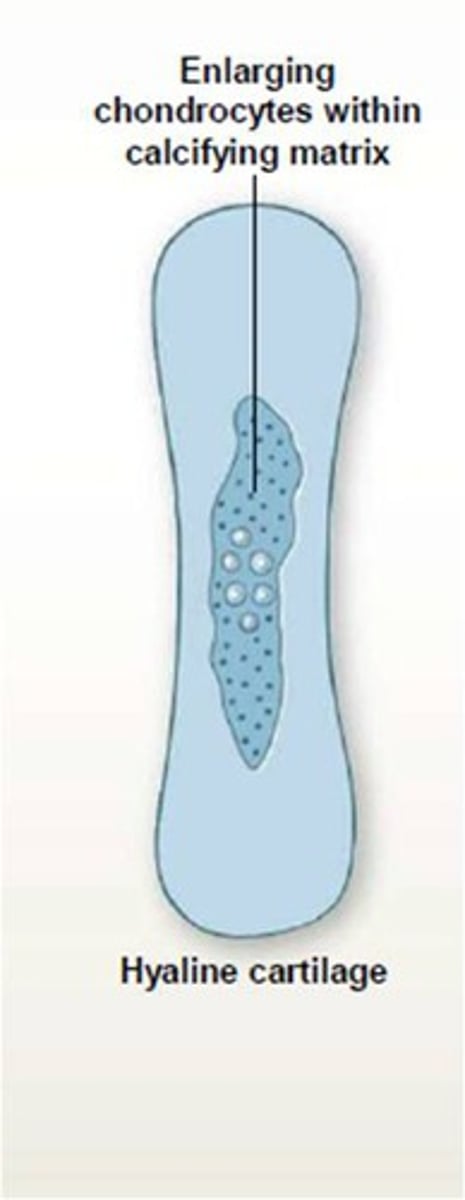
endochodral ossification
Most bones in the skeleton develop by this type of ossification (meaning, ''within cartilage'')
This ossification forms most other bones including the pelvic bones, vertebrae, and bones of the arms and legs.
Cartilage that is formed during fetal development is replaced by bone.
This process of bone formation involves the 3 steps listed below
1. Bony collar formation
2. Primary ossification center formation
3. Secondary ossification centers formation
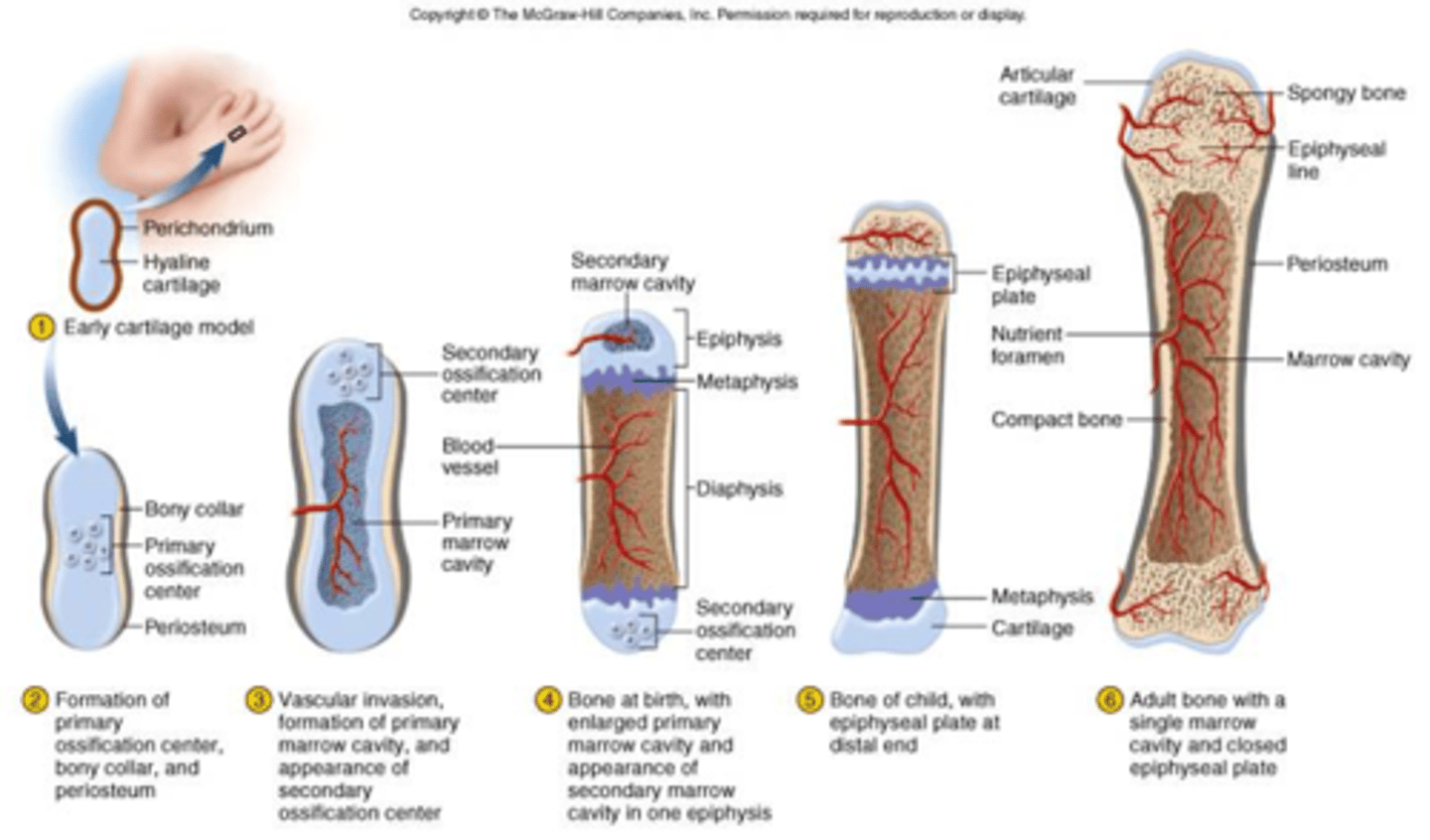
bony collar formation
The bony collar forms on the outside of the cartilage model or the cartilage that will ultimately be replaced with bone.
This provides temporary support for the bone and prevents nutrients from entering (and the subsequent breakdown of the cartilage inside of it.)
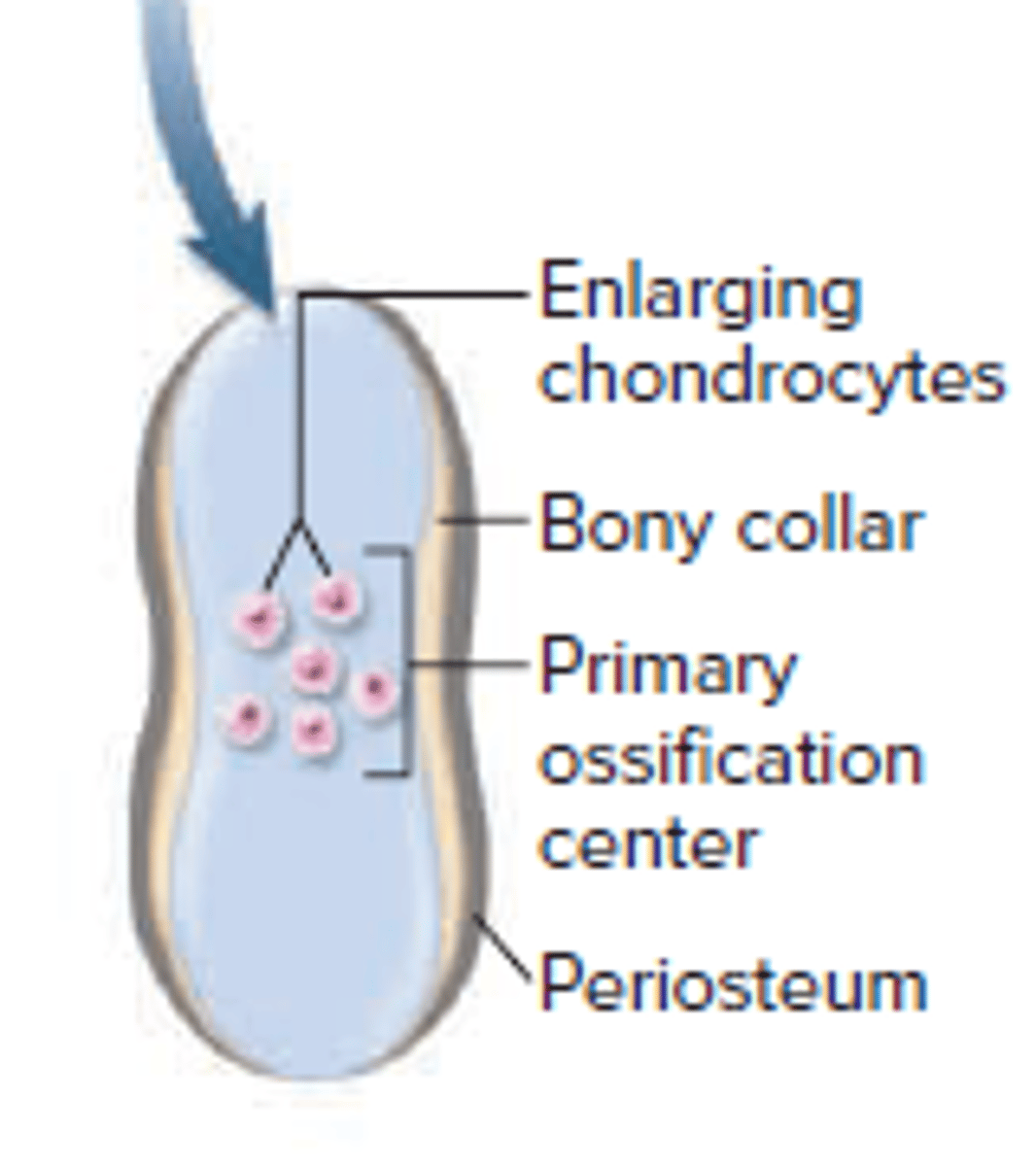
Primary ossification center formation
The cartilage begins to break down in the center or diaphysis of the bone.
This forms the medullary cavity of a long bone
Secondary ossification centers formation
A secondary center forms in the epiphyses of the long bones.
The cartilage will continue to develop into bone during adolescence and early adulthood in this center (epiphyseal plates).
What are the main differences between intramembranous ossification and endochondral ossification?
In intramembranous ossification, bone develops directly from sheets of mesenchymal connective tissue.
In endochondral ossification, bone develops by replacing hyaline cartilage.
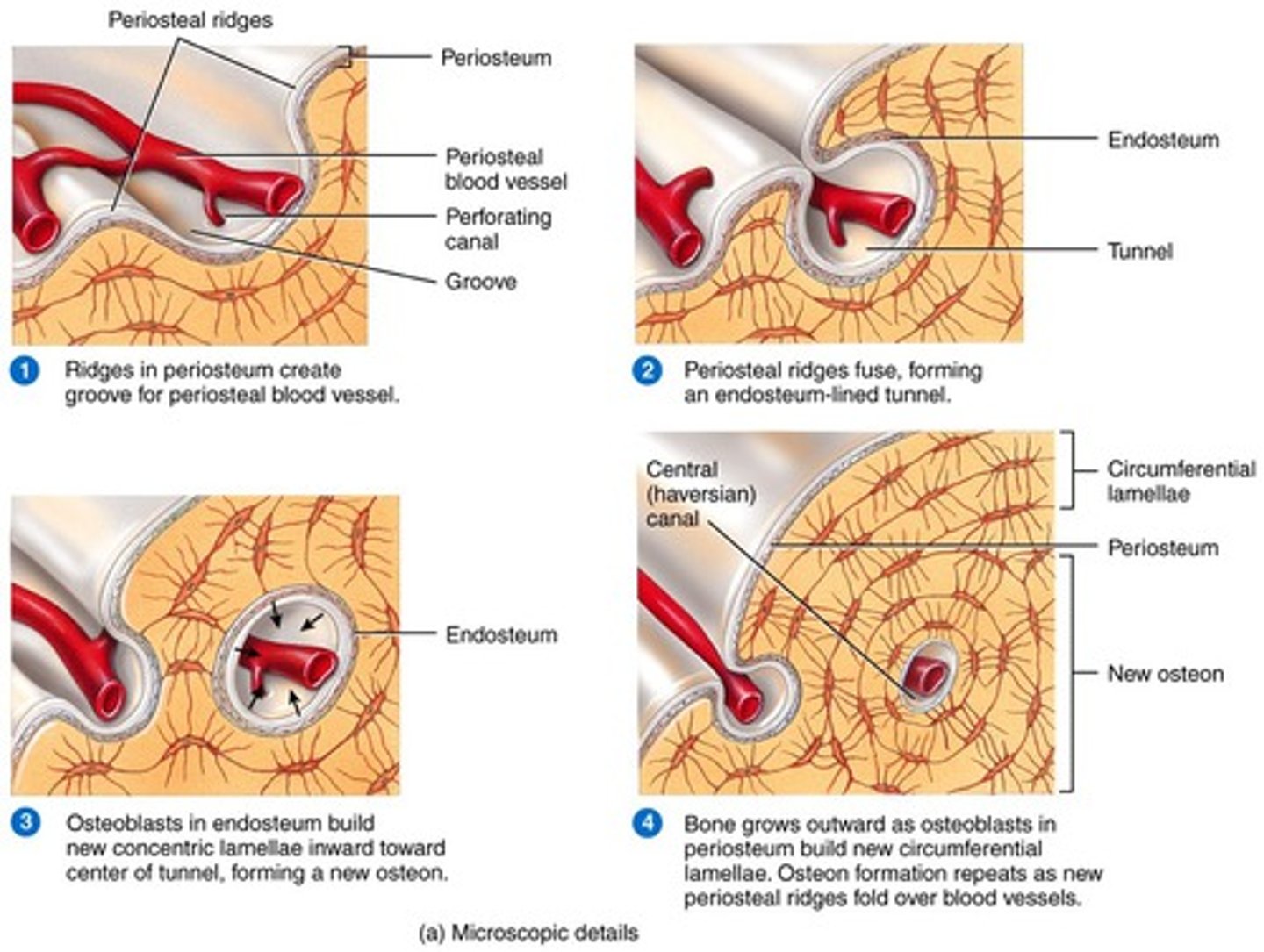
appositional growth
When bone increases in thickness or width. More bone is added to the surface.
It is similar to intramembranous ossification.
The osteoprogenitor cells in the inner periosteum convert to osteoblast cells which in turn add more matrix to the outer surface of the bone.
The osteoblasts become osteocytes when they are trapped in the matrix.
This helps increase the strength of bones and is the only growth that occurs in mature bone.
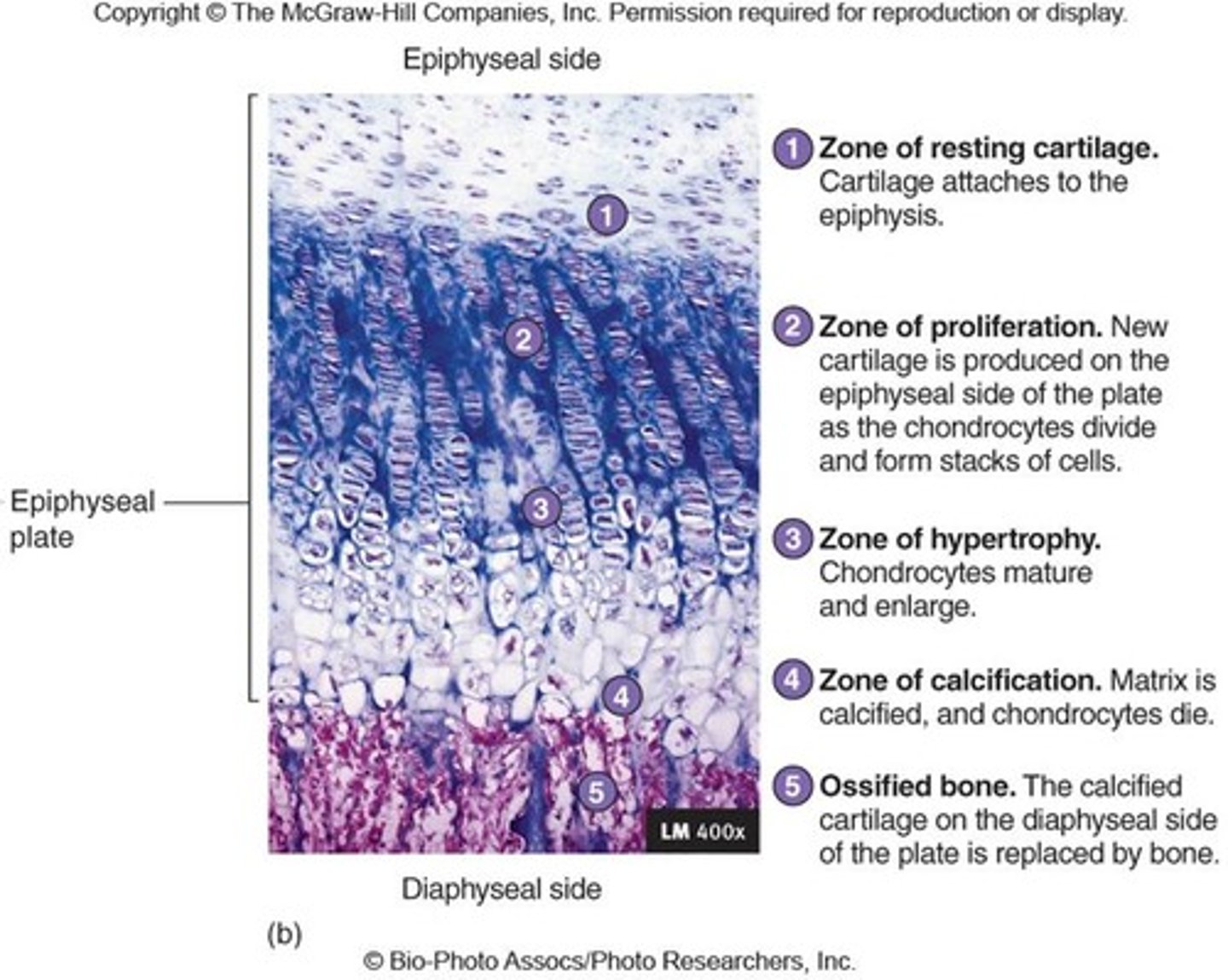
interstitial / endochondral growth
Increases the length of the long bones.
This occurs at the epiphyseal plates that are found between the primary and secondary ossification centers.
Chondrocytes undergo mitosis on epiphyseal side of plate.
Stacks of chondrocyte grow, pushing epiphysis away from diaphysis - stimulated by growth hormone.
Chondrocytes replaced by bone on diaphyseal side of plate.
Growth is complete when all chondrocytes are replaced by bone (ossification) - stimulated by sex hormones (testosterone or estrogen) during puberty.
bone remodeling
The replacement of old bone tissue with new tissue
Significance:
- replaces spongy bone with compact bone during development
- allows for increase in diameter of long bones as internal bone is removed and new bone is added to the outside
- continual renewal of bone tissue during life
replacement of worn and injured bone
- allows bone to act as a calcium storage place
cells involved in bone remodeling
osteoclasts ‑ remove bone matrix
osteoblasts ‑ produce new matrix
What six items are required for bone remodeling to occur?
- Sufficient calcium and phosphorus in the diet
- Vitamin D is required for absorption of calcium from the gastrointestinal tract into the blood and for other calcium processing in the body (rickets and osteomalacia caused by deficiency of vit D)
- Vitamin C is required to maintain the bone matrix
- Vitamin A regulates osteoblasts and osteoclasts
- Human growth hormone is responsible for general bone growth
- Estrogen and testosterone aid in osteoblasts producing matrix and remove cartilage in the epiphyseal plate
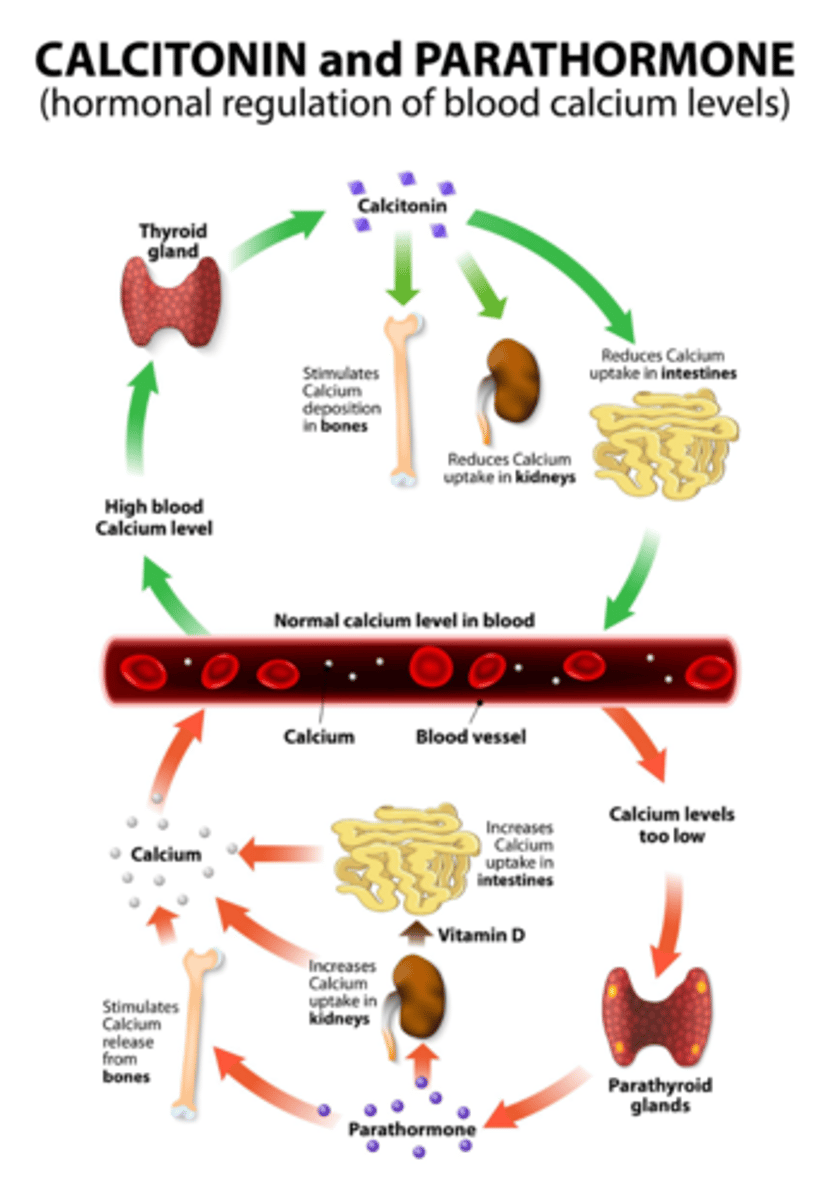
- Calcitonin promotes bone formation and decreases blood calcium levels
- Parathyroid hormone (PTH) promotes bone re-absorption and an increase in blood calcium levels
Calcitonin
Promotes bone formation and decreases blood calcium levels.
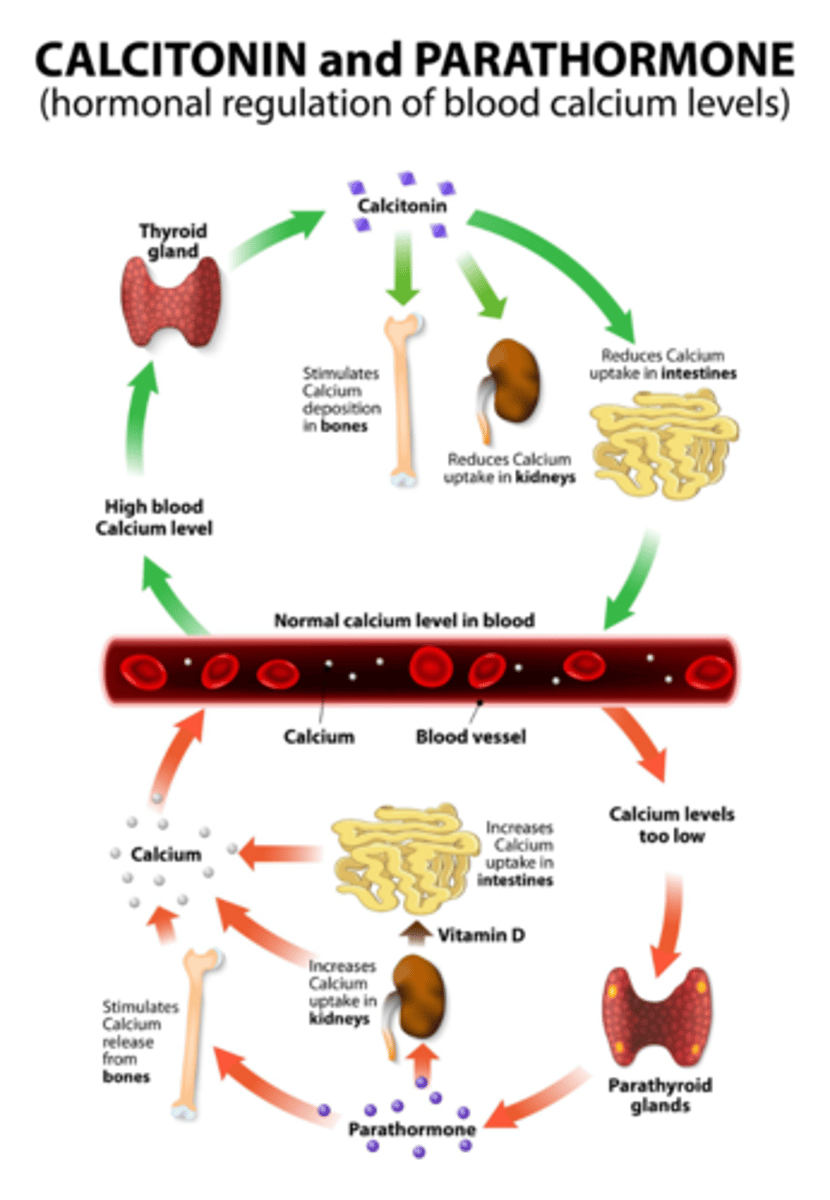
parathyroid hormone (PTH)
Promotes bone re-absorption and an increase in blood calcium levels.
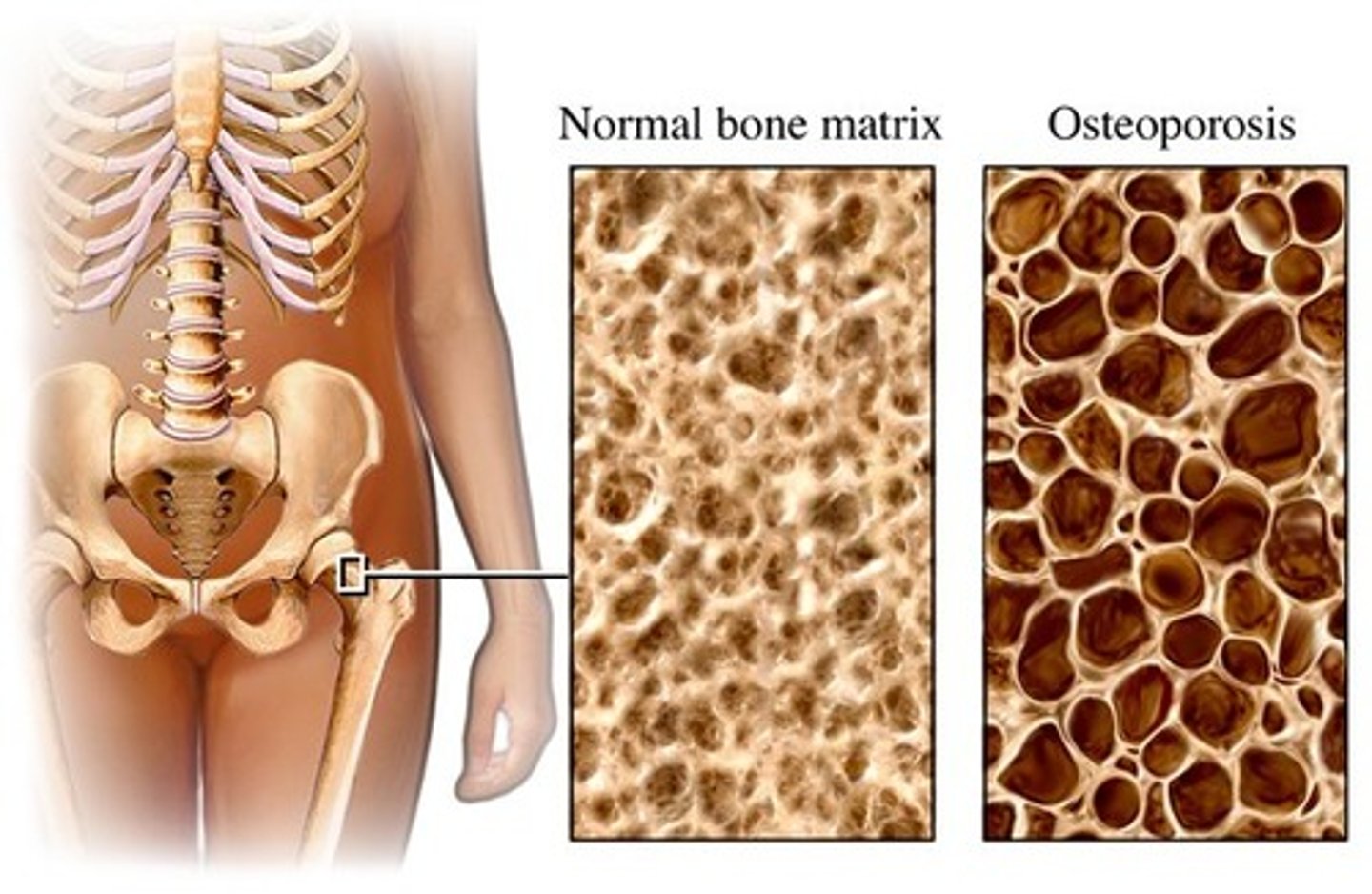
osteoporosis
A decrease in bone mass, usually due to decreased
levels of estrogen and testosterone
Causes fractures and shrinkage of the spine
Osteoblasts become less active
Can also be caused by a calcium deficiency
Alcohol can play a role as it is toxic to osteoblasts
Manifestations include kyphosis and brittle bones due to low bone density.
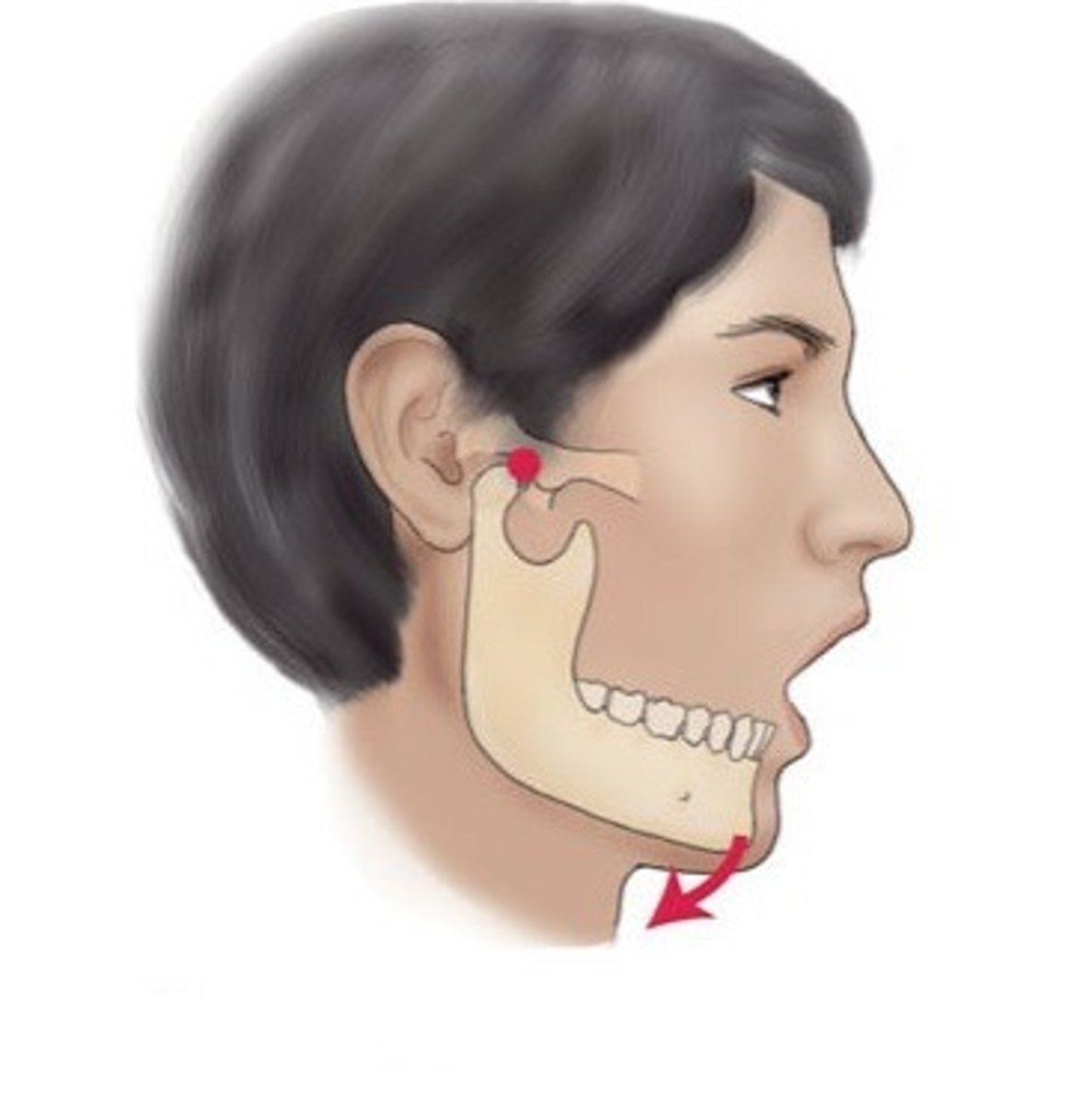
articulation
where two or more bones meet
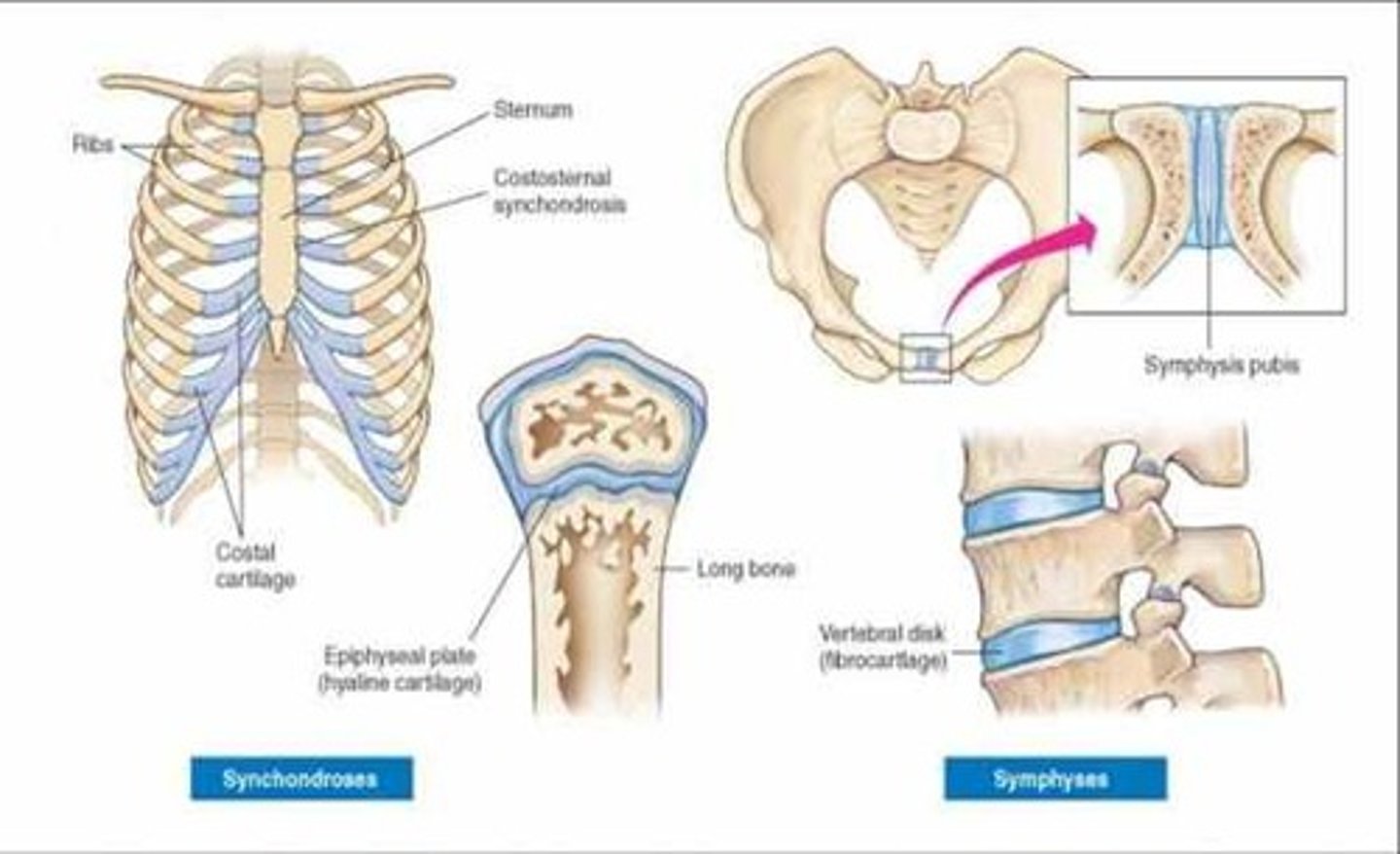
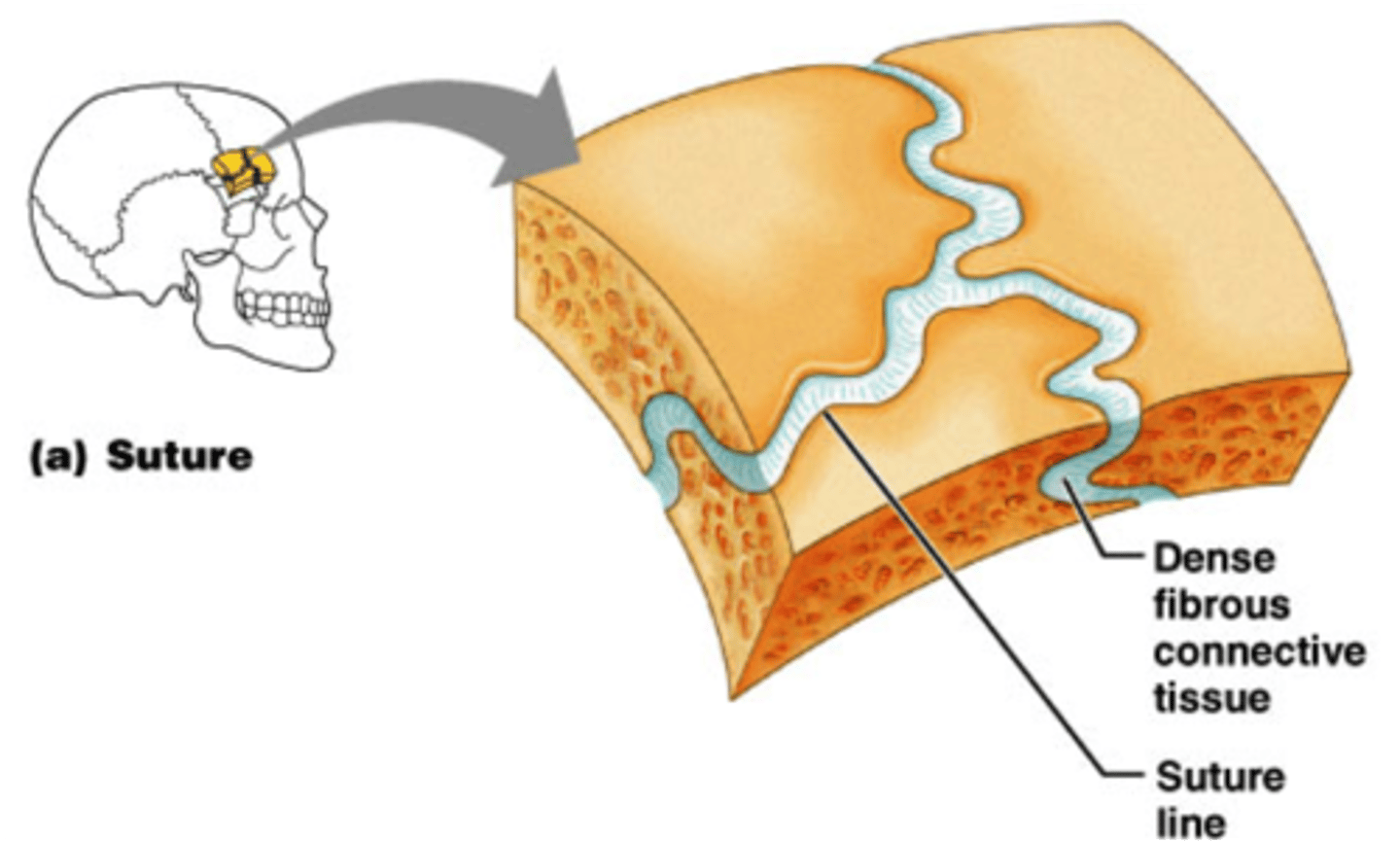
synarthroses
immovable joints
Ex. Skull bones
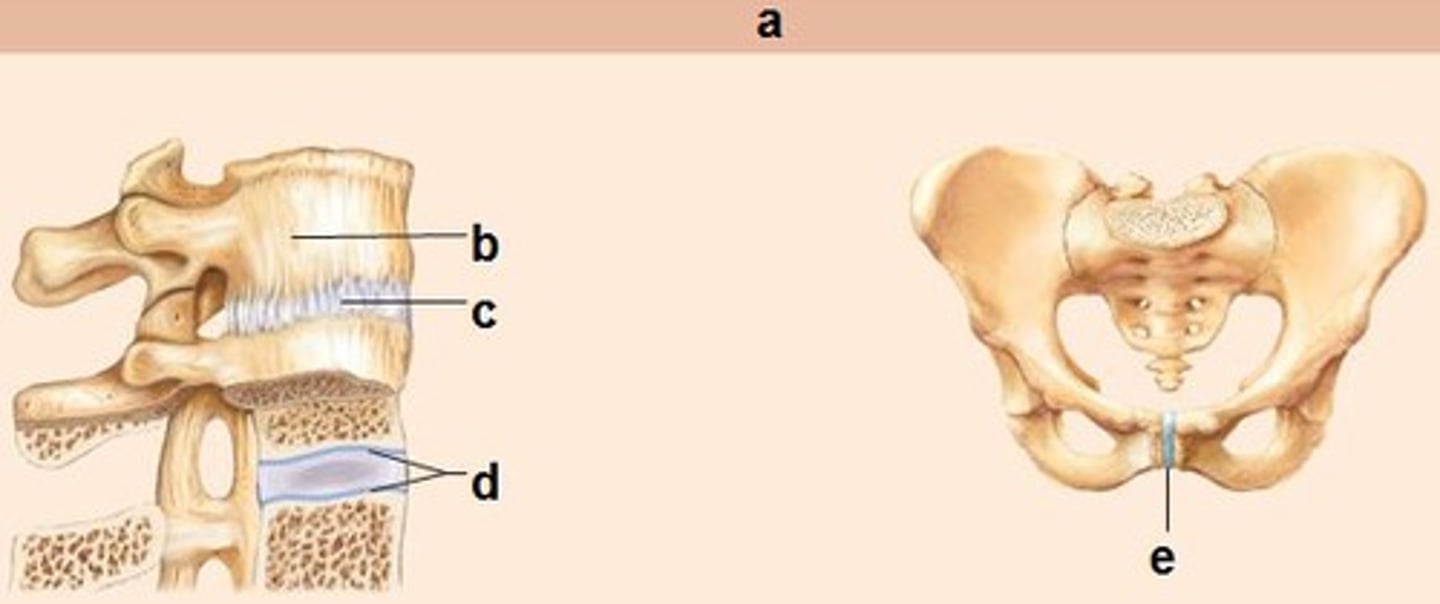
amphiarthroses
slightly movable joints
Ex. Wrist bones, between vertebrae
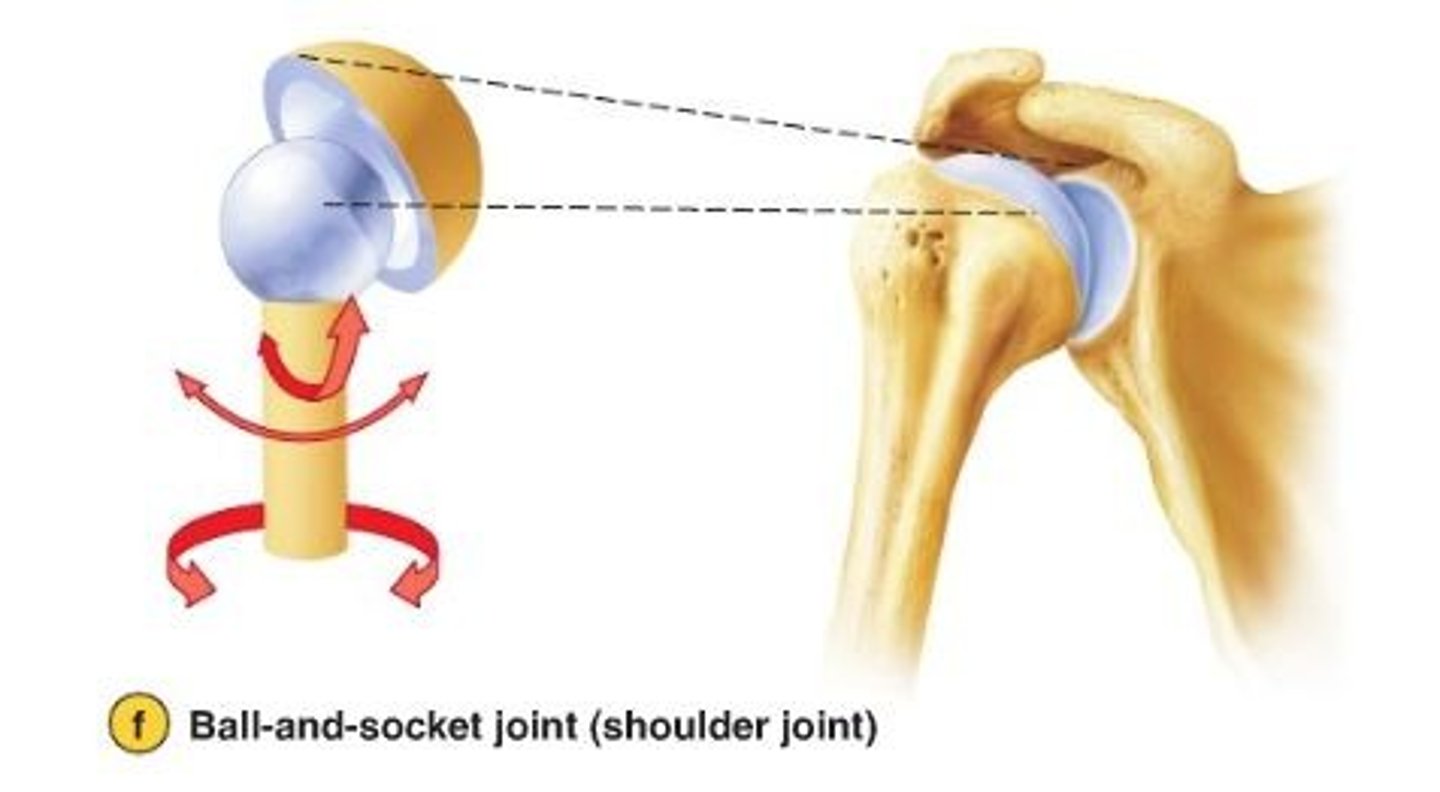
diarthroses
Highly moveable joints
Ex. Shoulder
fibrous joints
Consists of inflexible layers of dense regular connective tissue, holds the bones tightly together.
Ex. skull sutures
cartilaginous joints
Allow only slight movement and consist of bones connected entirely by cartilage
Ex. between vertebrae
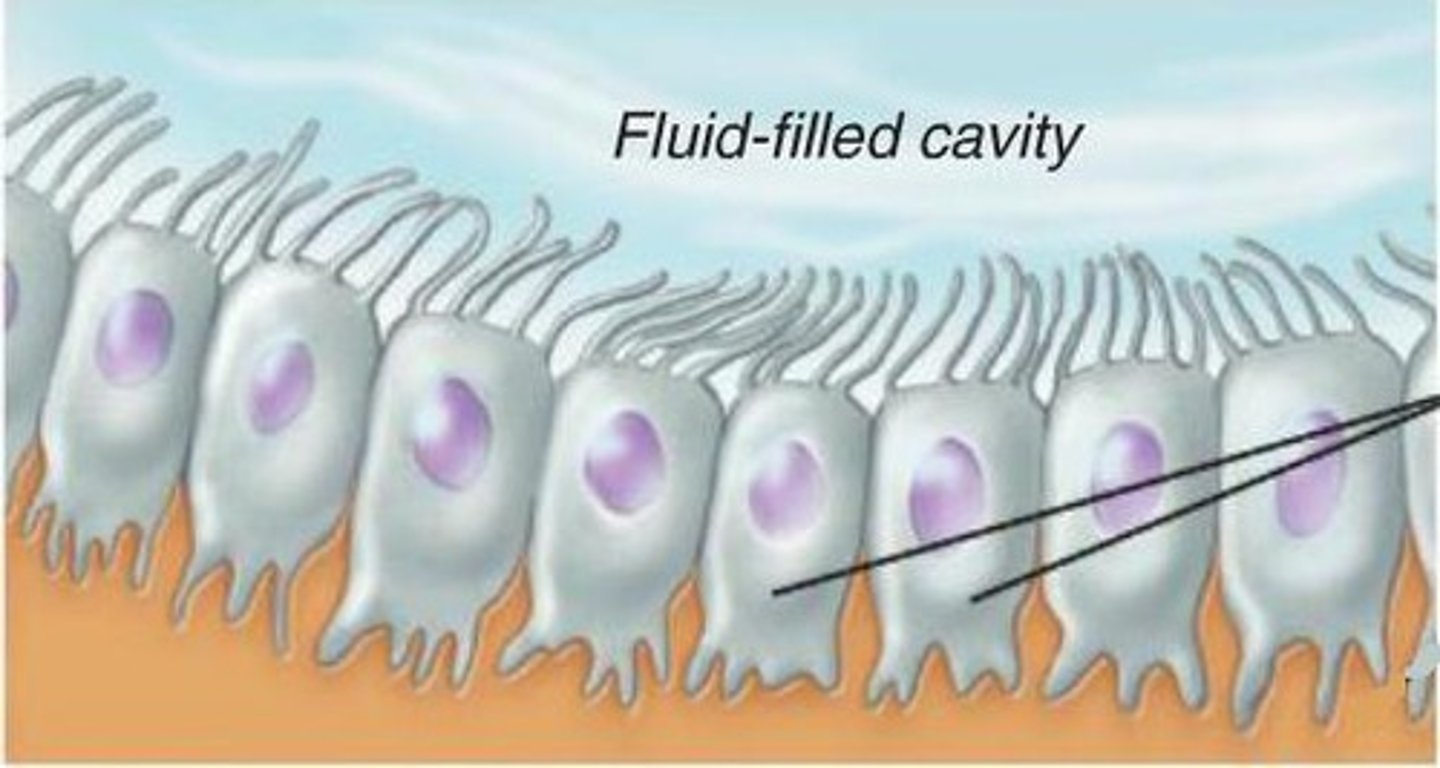
synovial joints
Freely movable joints that contain a fluid-filled joint capsule
Ex. shoulder
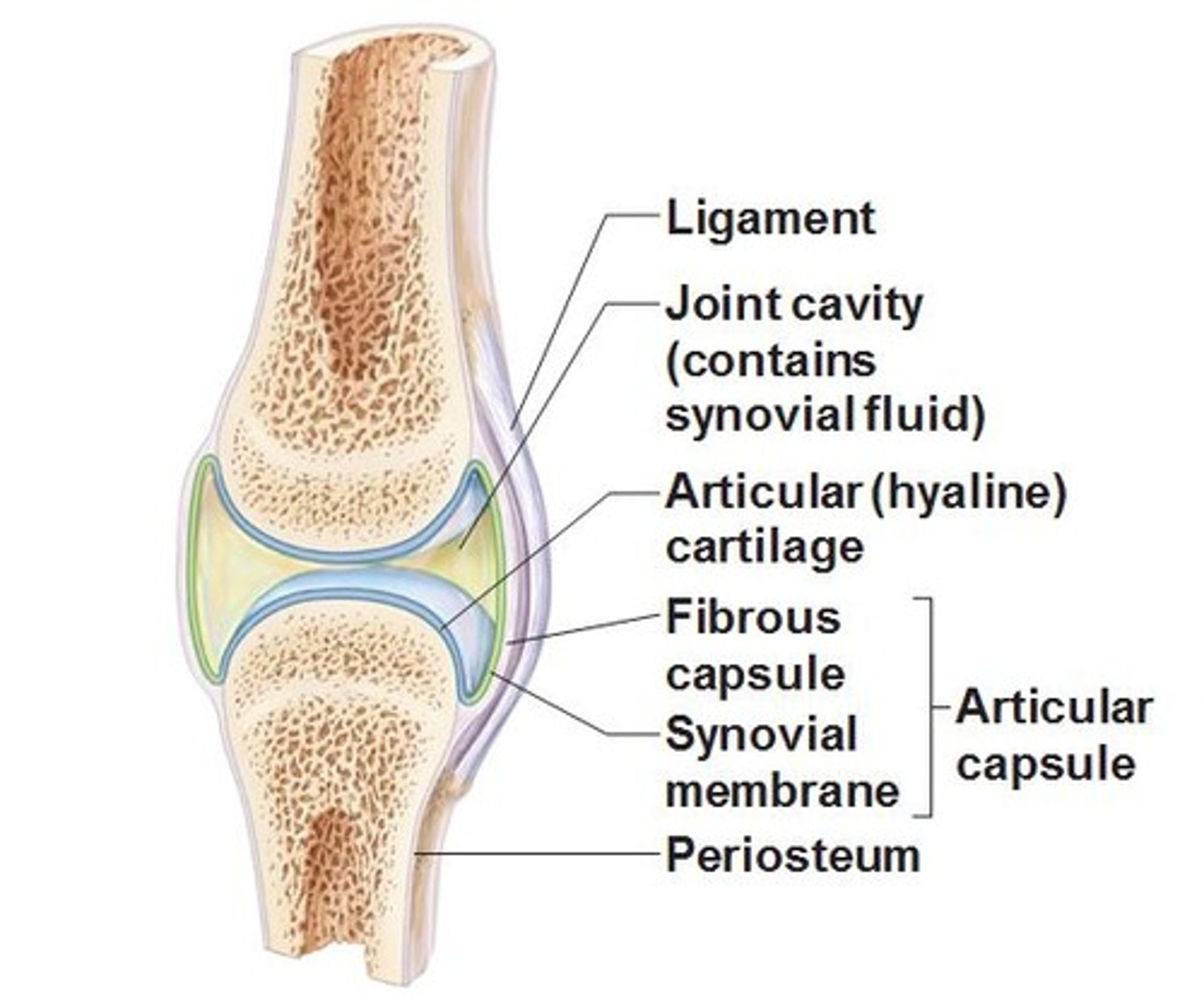
synovial cavity
The space between the articulating bones of a synovial joint, filled with synovial fluid. Also called a joint cavity.
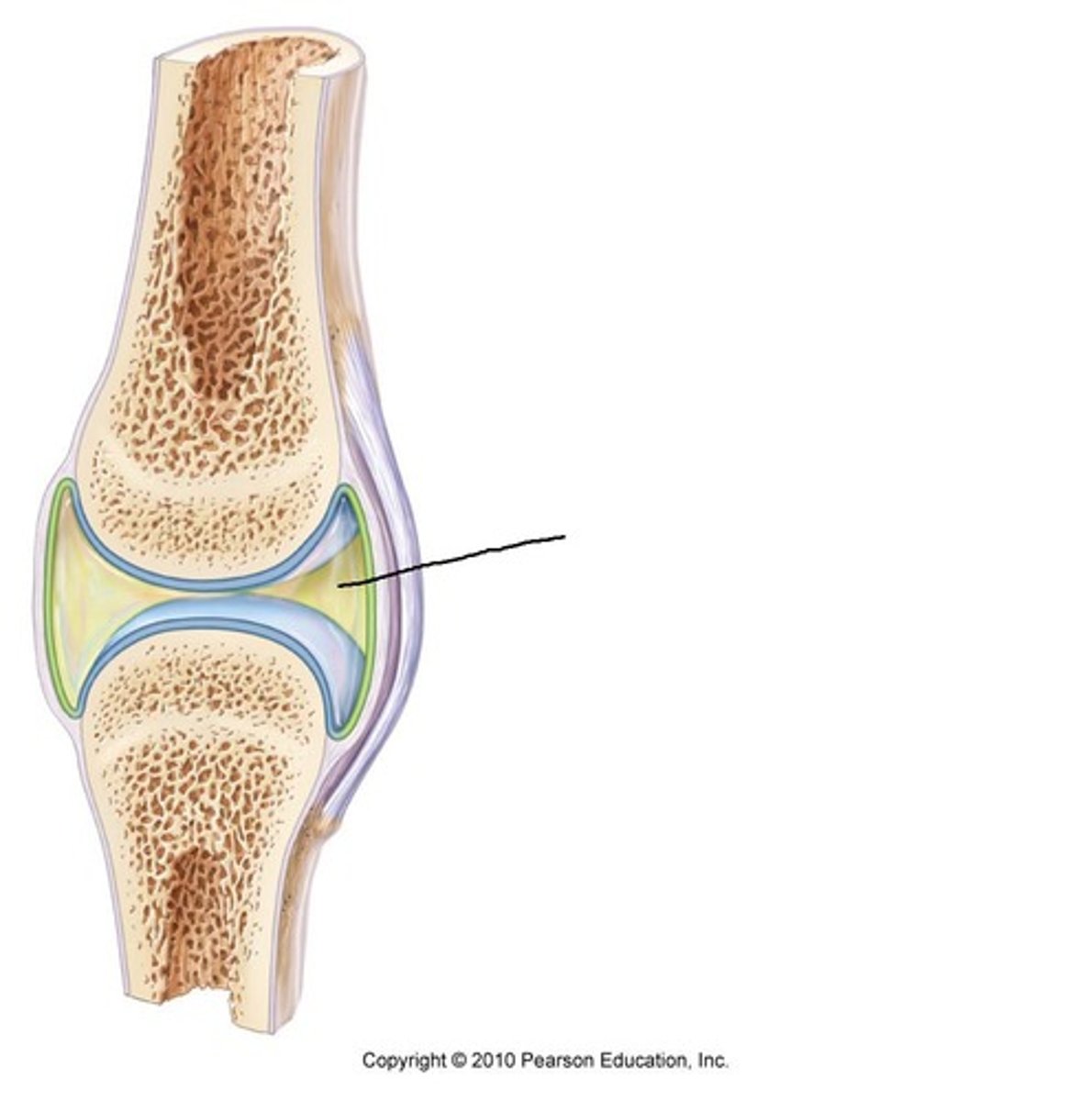
synovial membrane
The lining of a joint that secretes synovial fluid into the joint space.
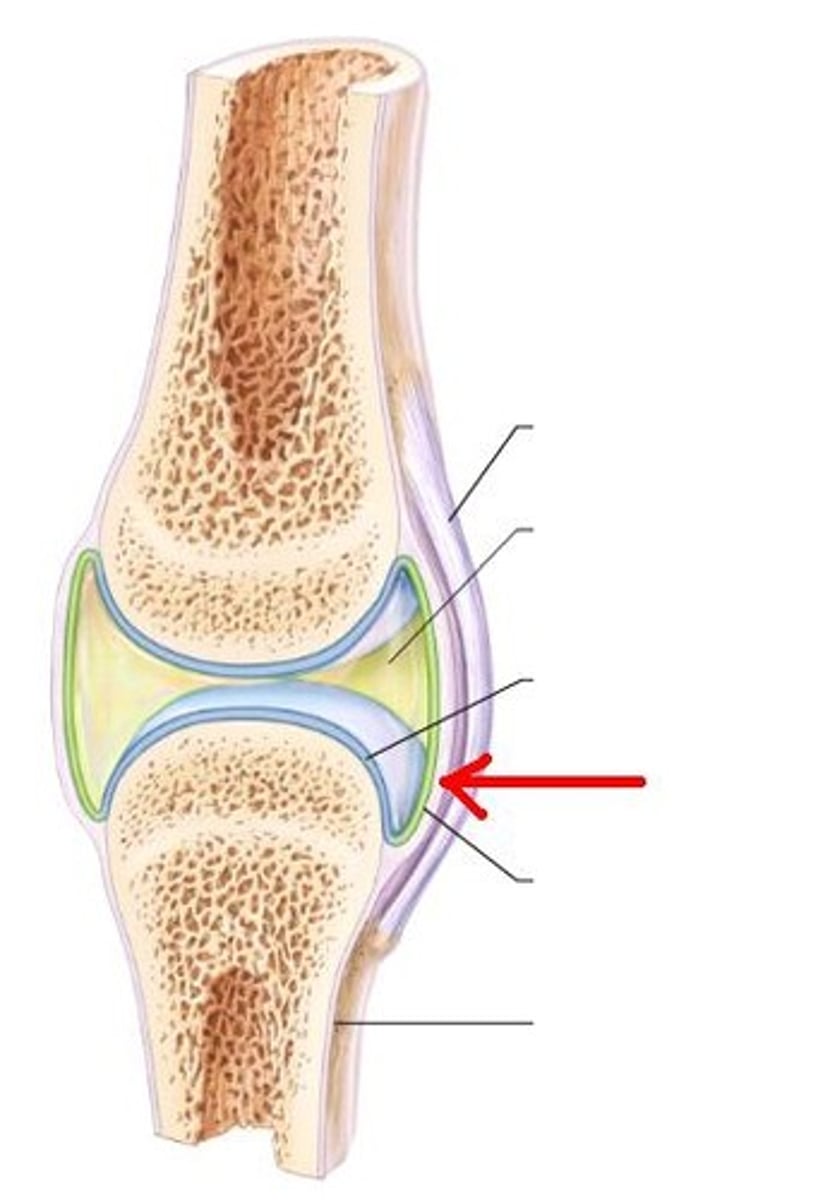
articular cartilage of synovial joint
Hyaline cartilage covers, but doesn't join articular surfaces; reduces friction, absorbs shock
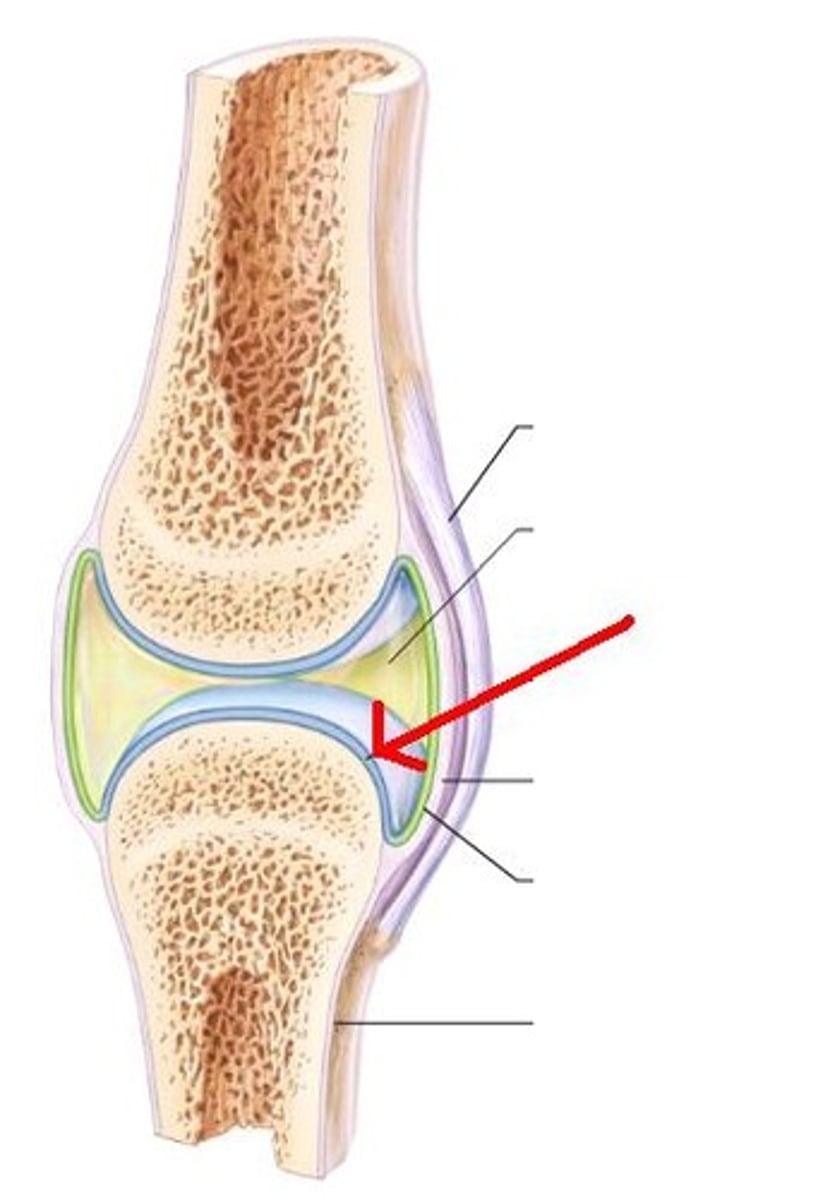
joint capsule
The dense irregular connective tissue sac that encloses a joint.
ligaments
Connect bone to bone. Found inside and outside joint capsule.
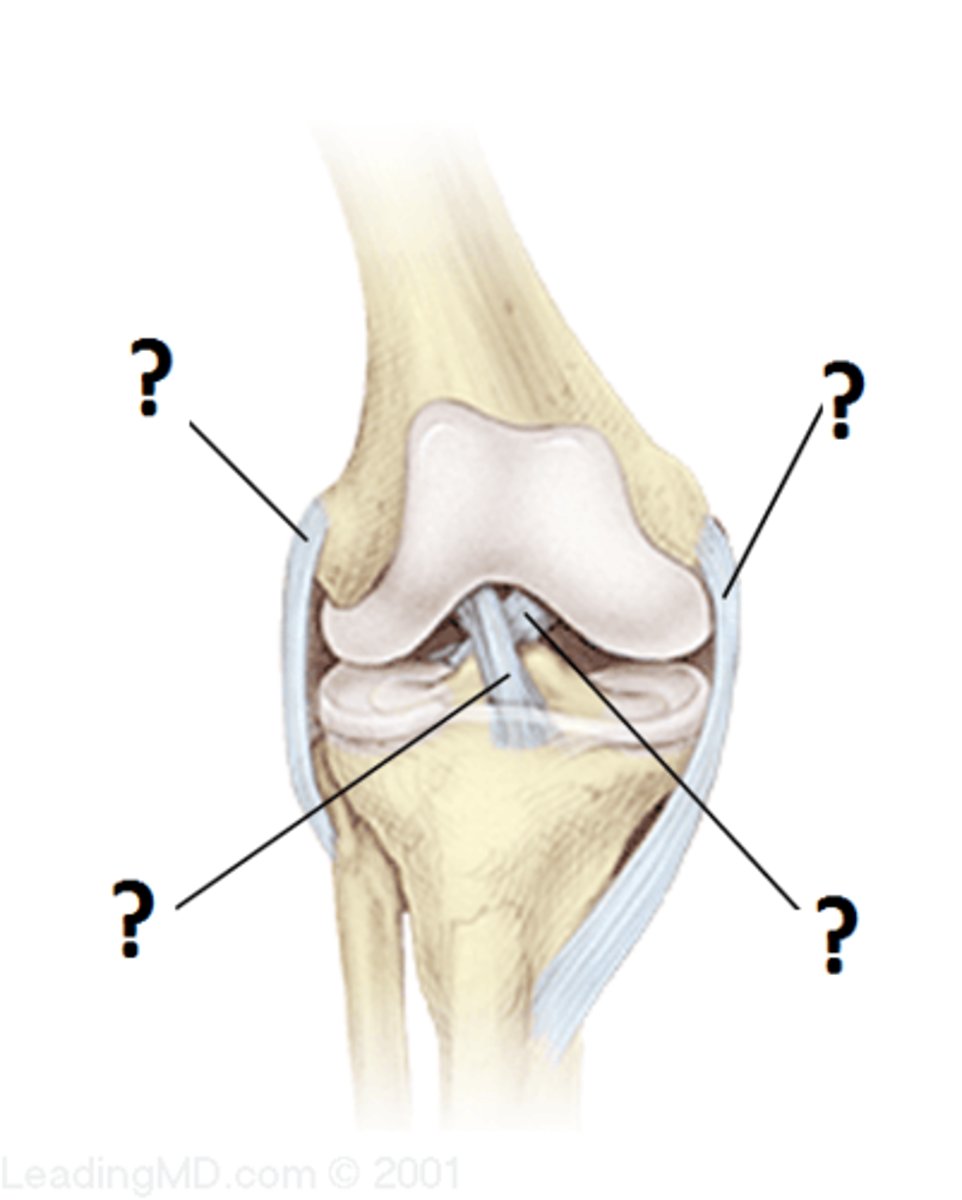
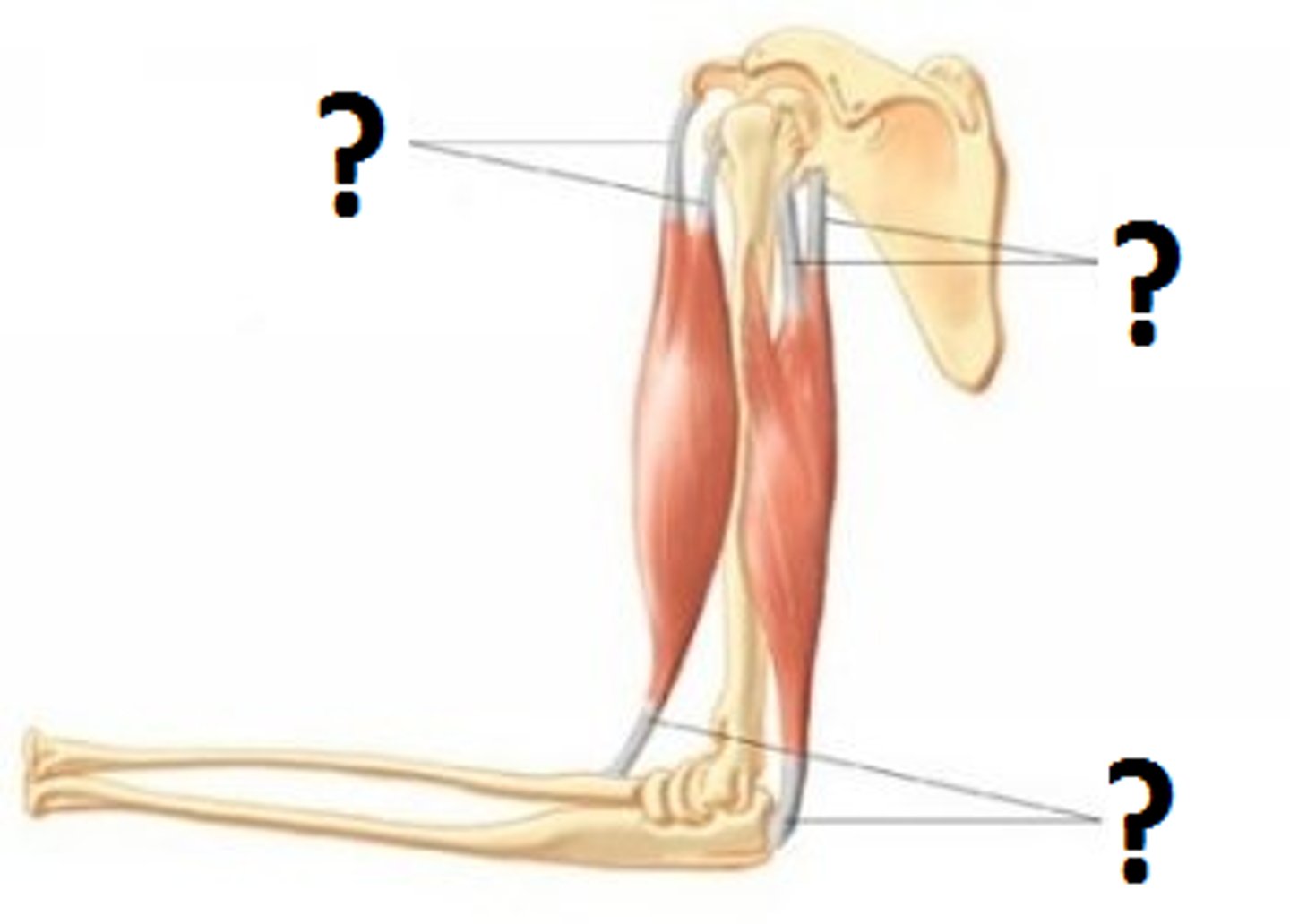
tendons
Connect muscle to bone; provide anchor for muscles to produce force
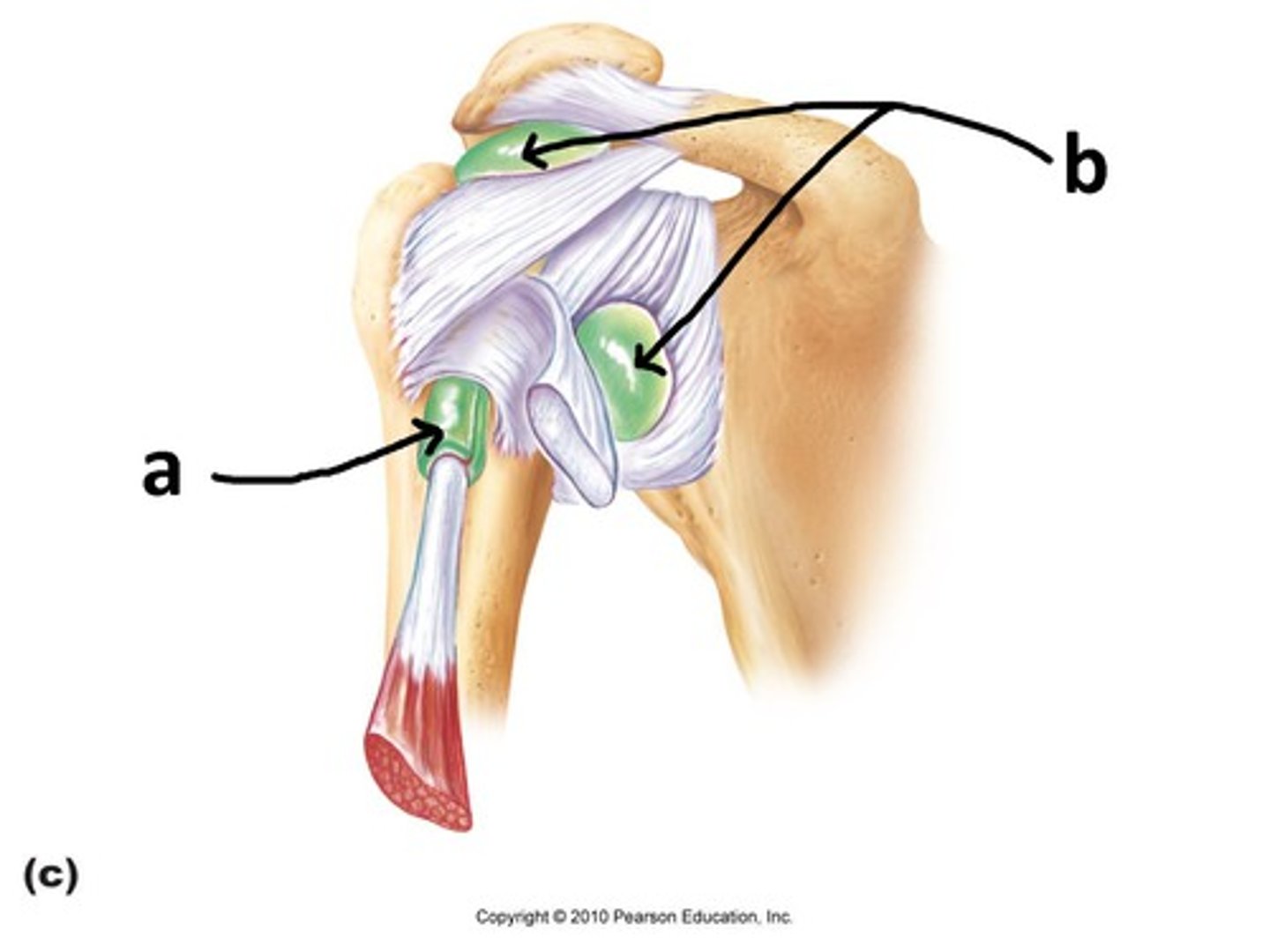
bursae
Fluid-filled sacs that reduce friction at the joint.
Flexion
decreasing the angle of a joint
Extension
Increasing the angle of a joint
Abduction
Movement away from the midline of the body

Adduction
Movement toward the midline of the body

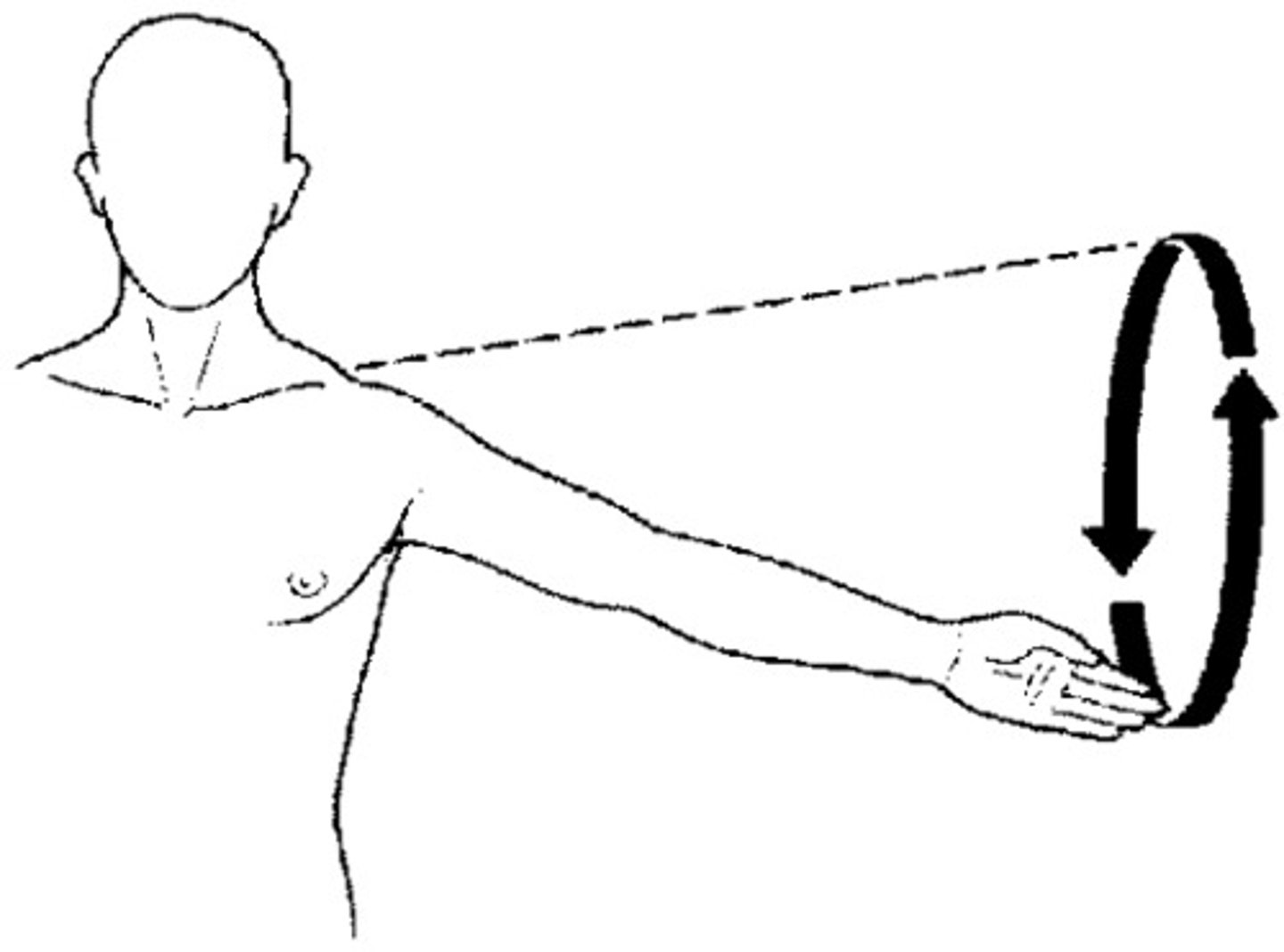
Circumduction
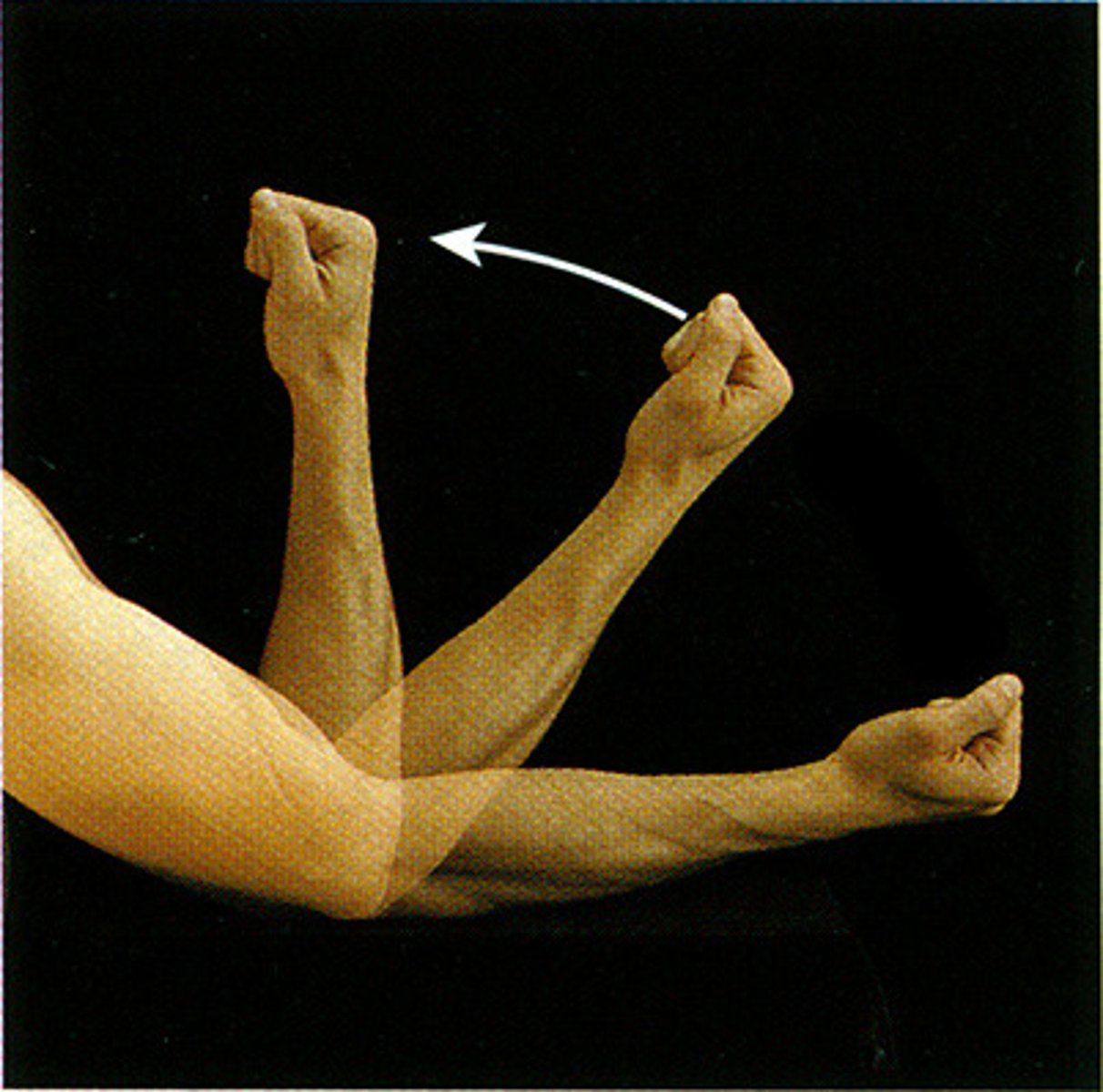
The circular movement at the far end of a limb tracing a cone in space.
Rotation
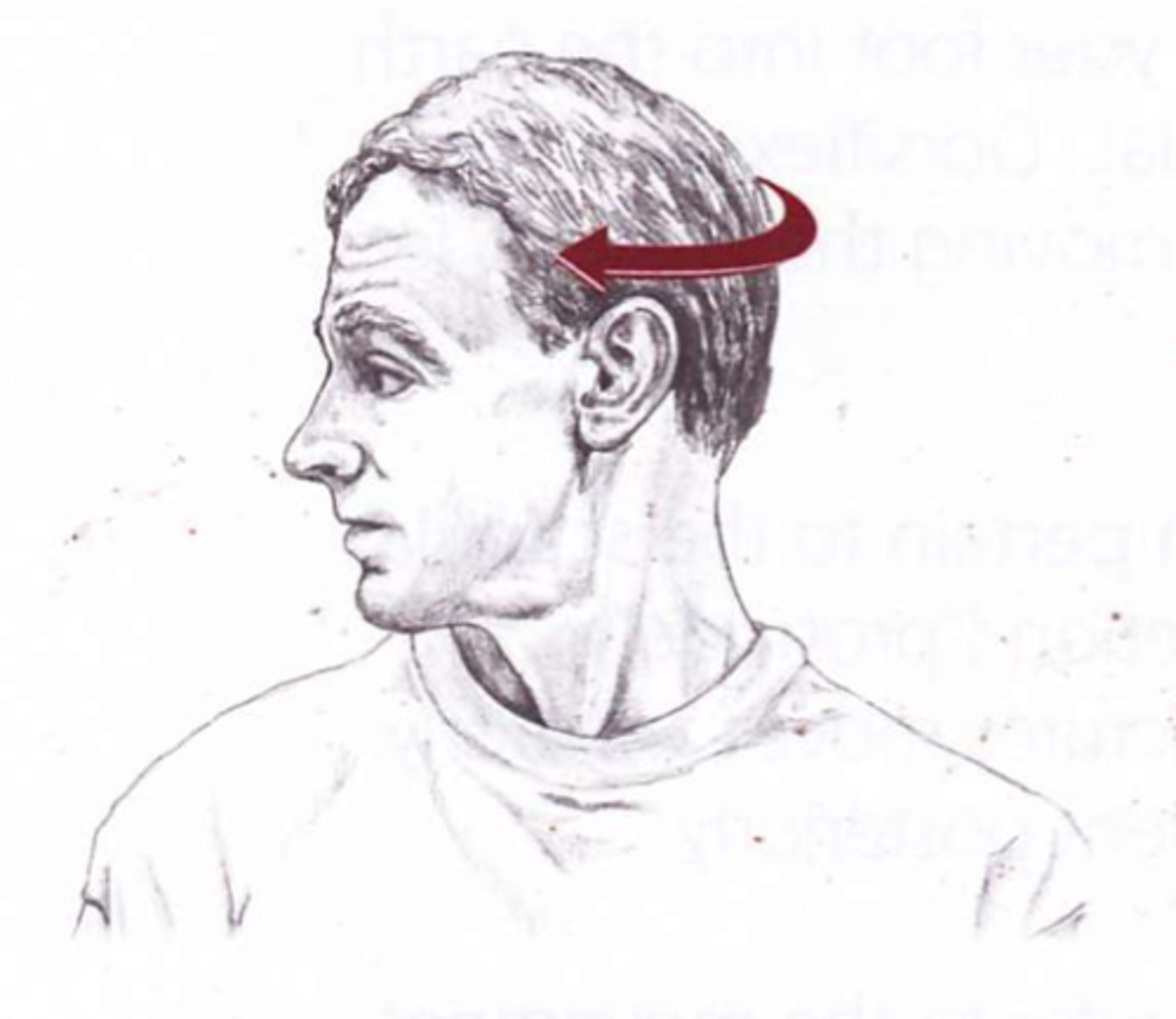
Turning on an axis
Ex. Shaking head "No"
Elevation
raising a body part
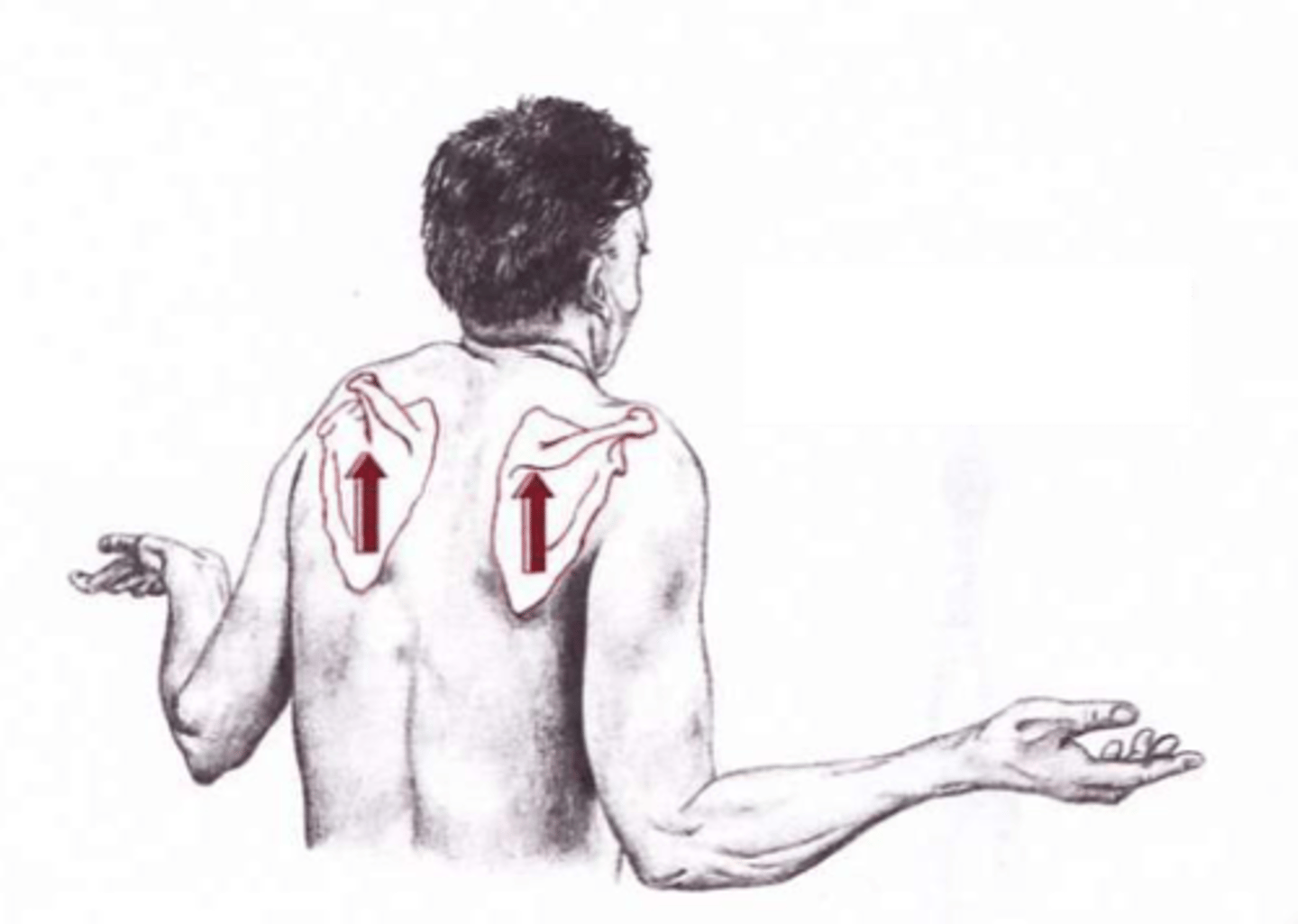
Depression
lowering a body part
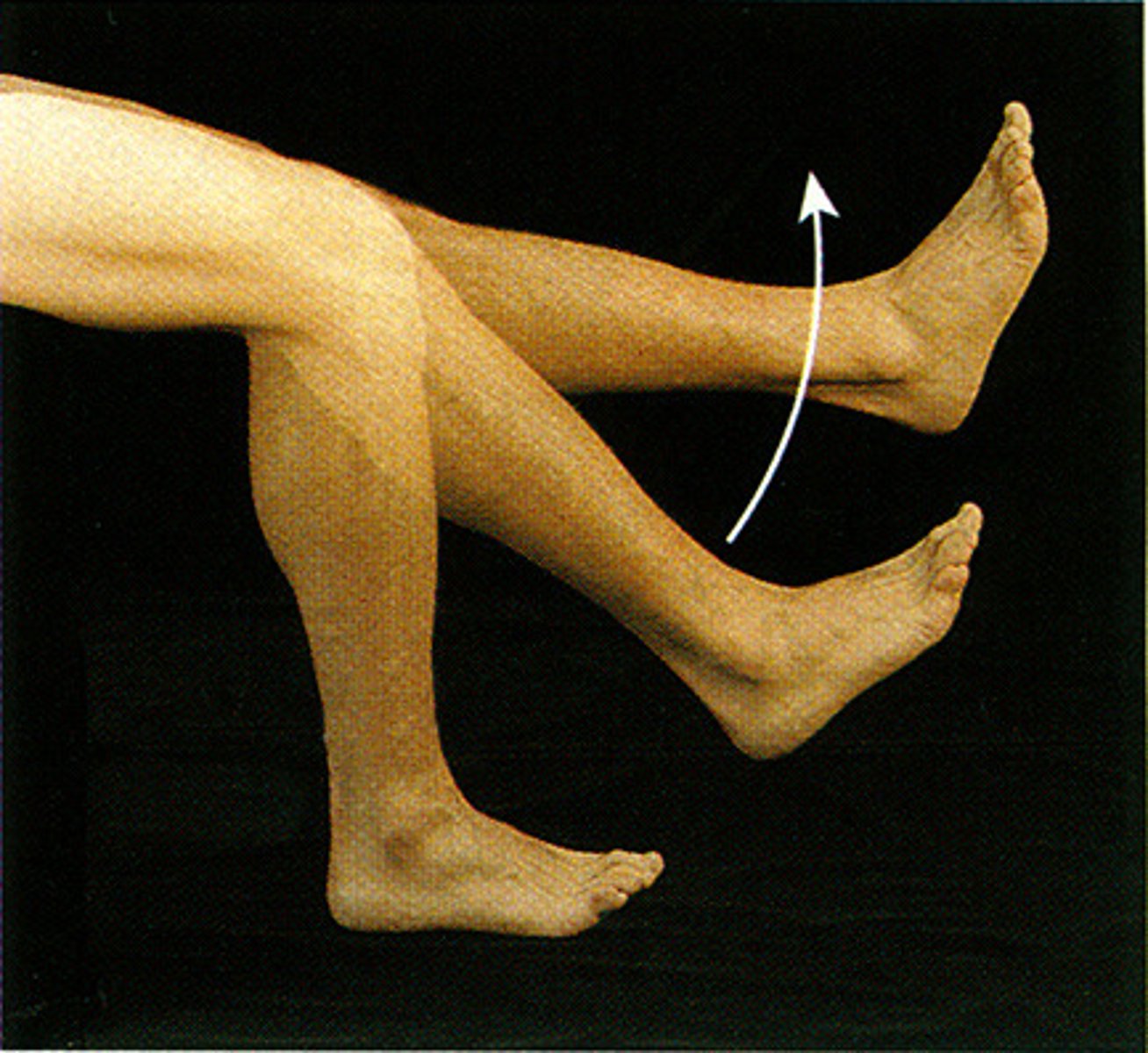
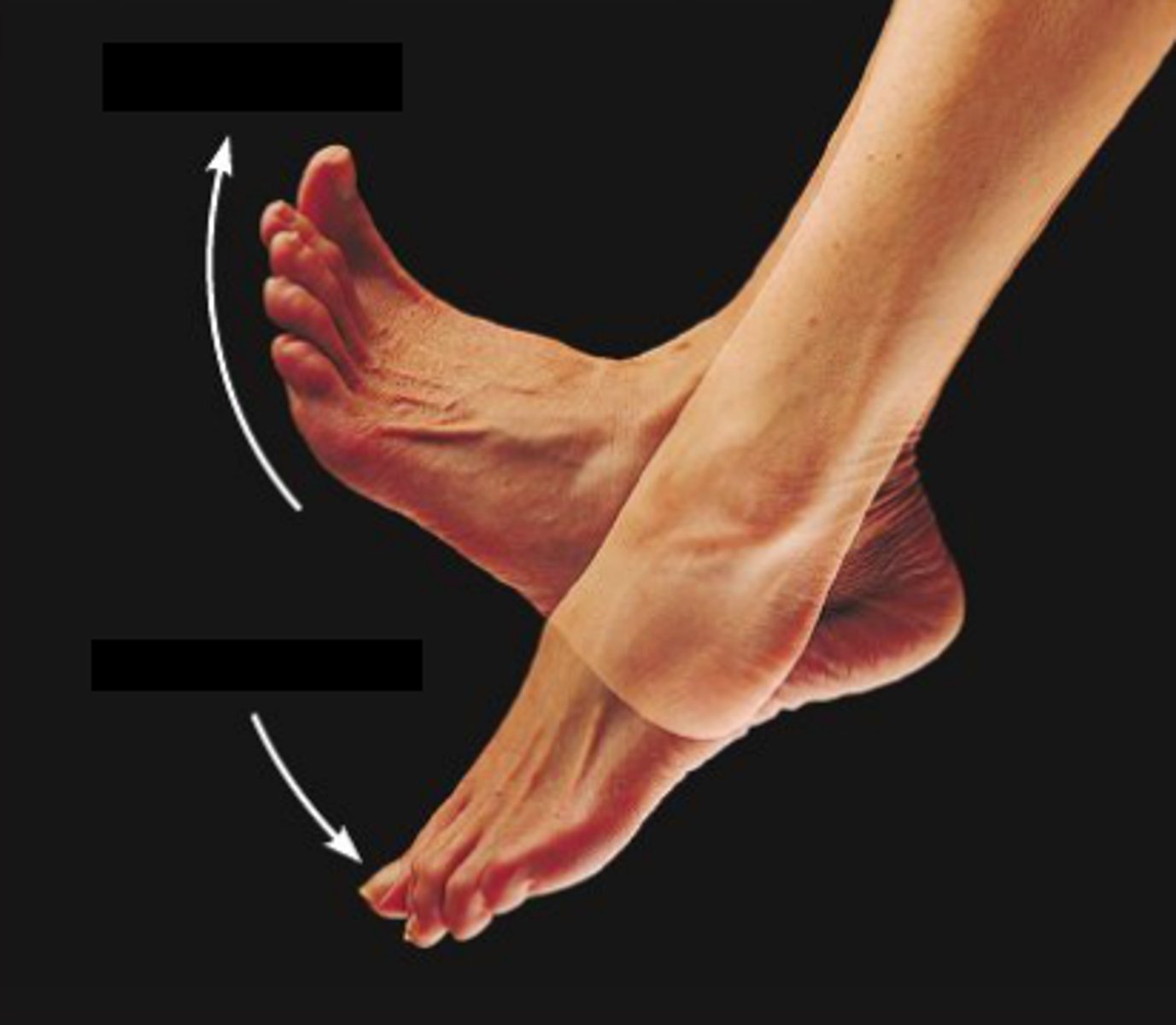
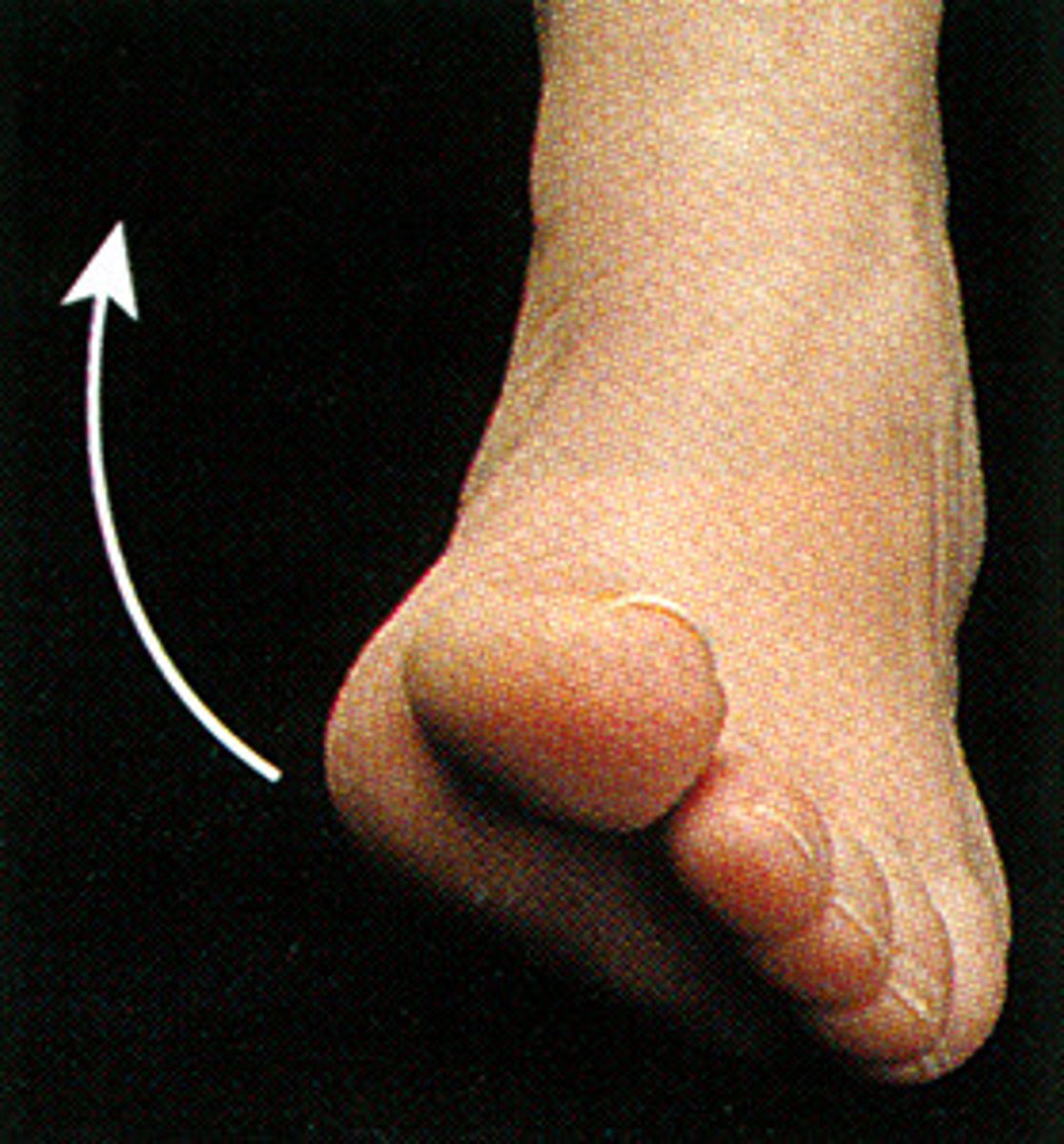
Dorsiflexion
Bending of the foot or the toes upward
Plantar flexion
Pointing toes downward
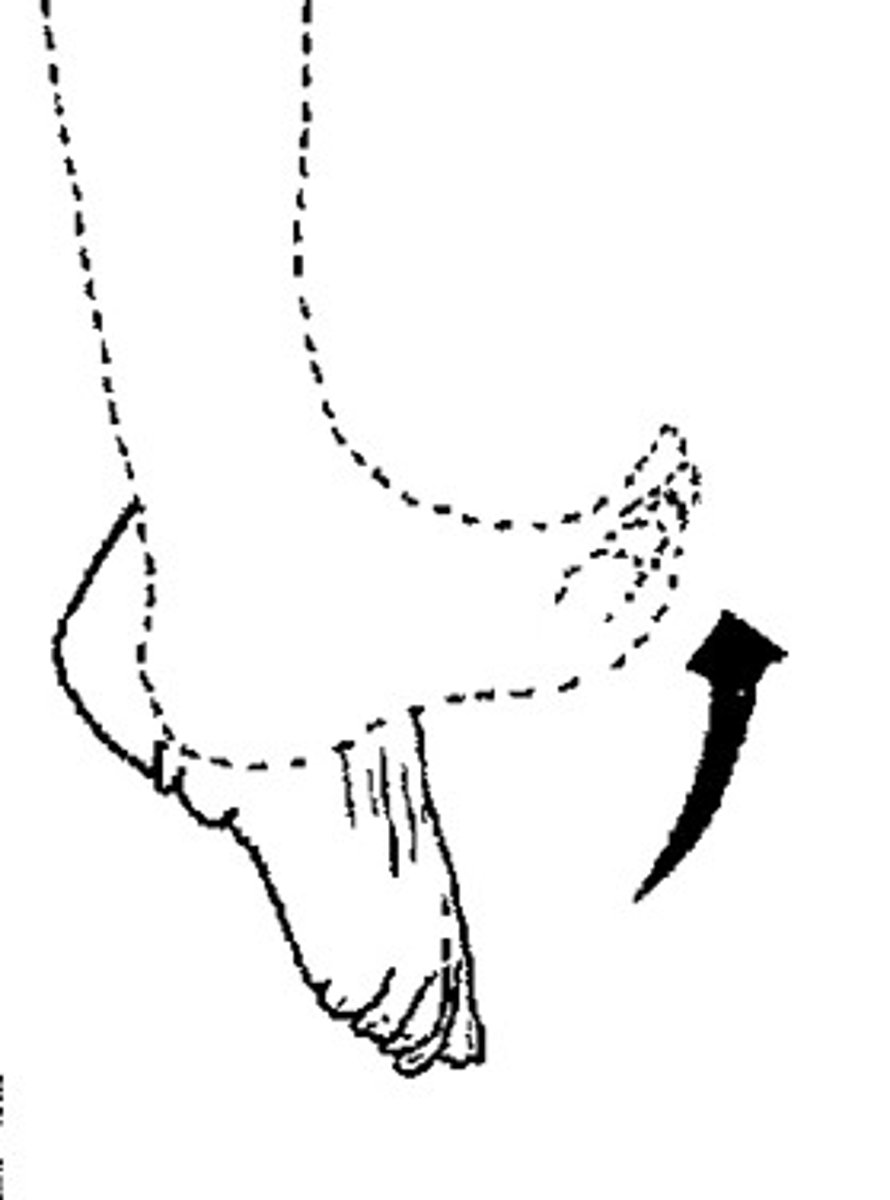
Eversion
turning the sole of the foot outward (laterally)
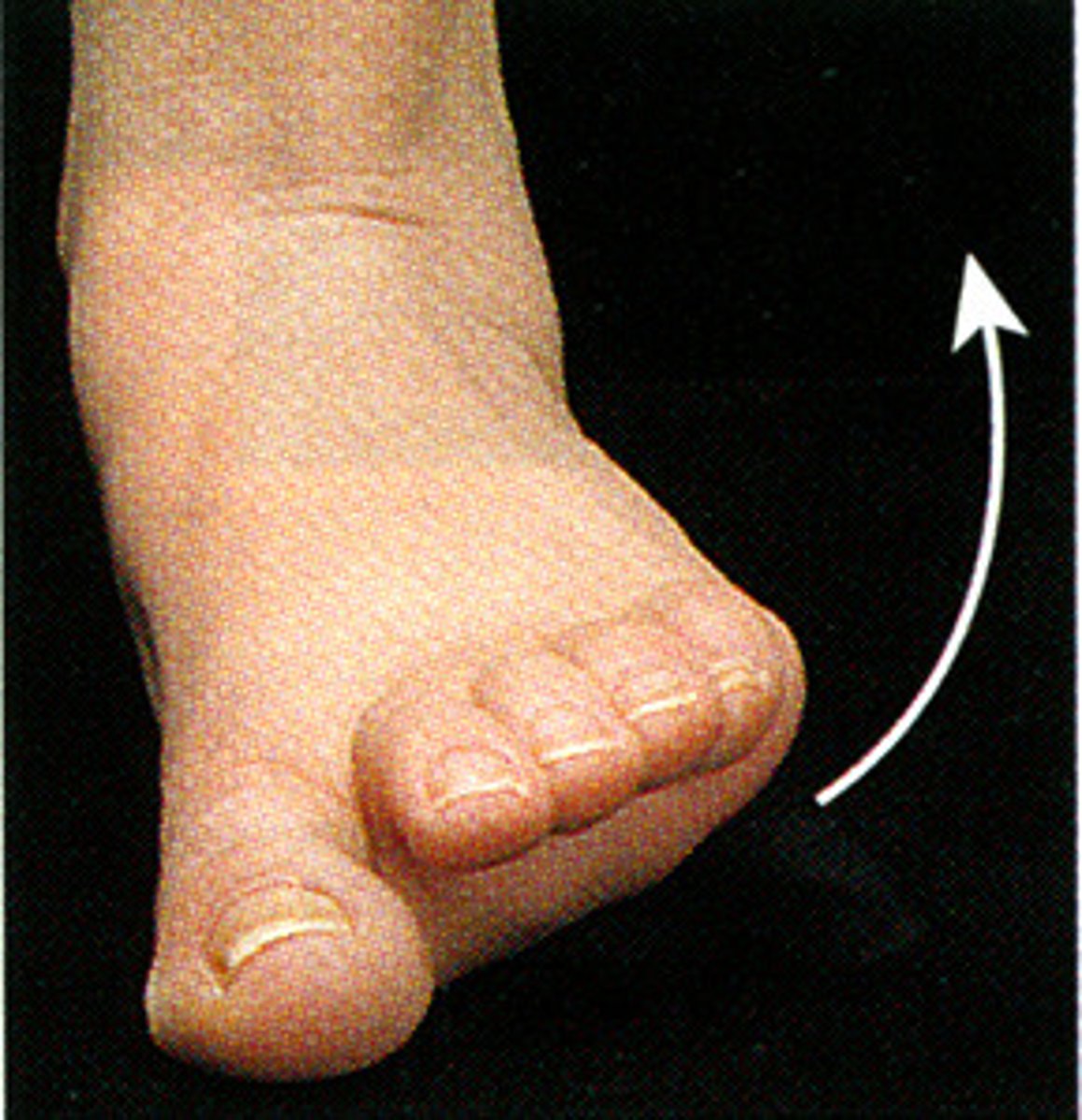
Inversion
Turning the sole of the foot inward (medially)
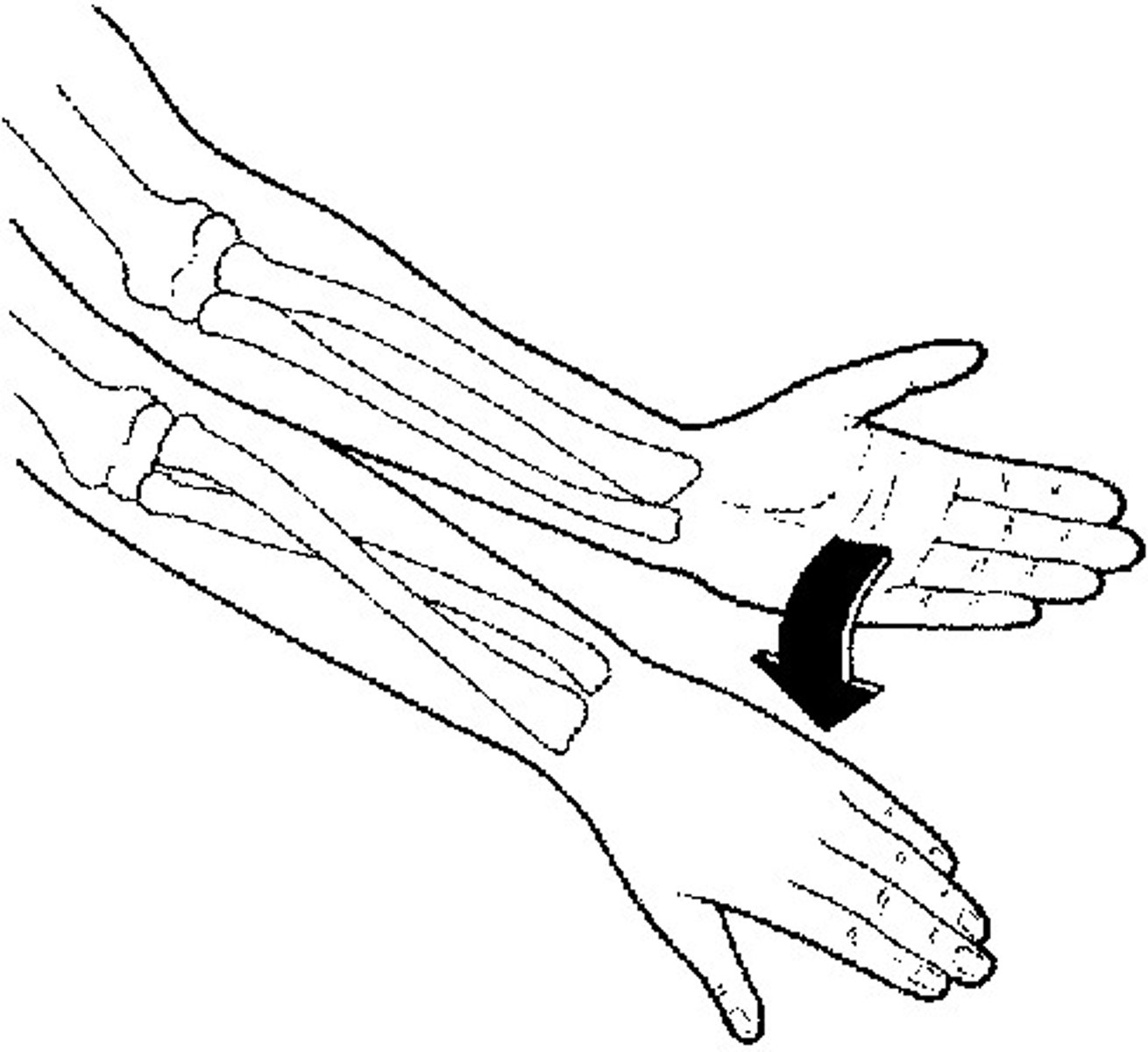
Supination
Rotating forearm so palm faces anteriorly or superiorly (palm up; "hold a bowl of soup")
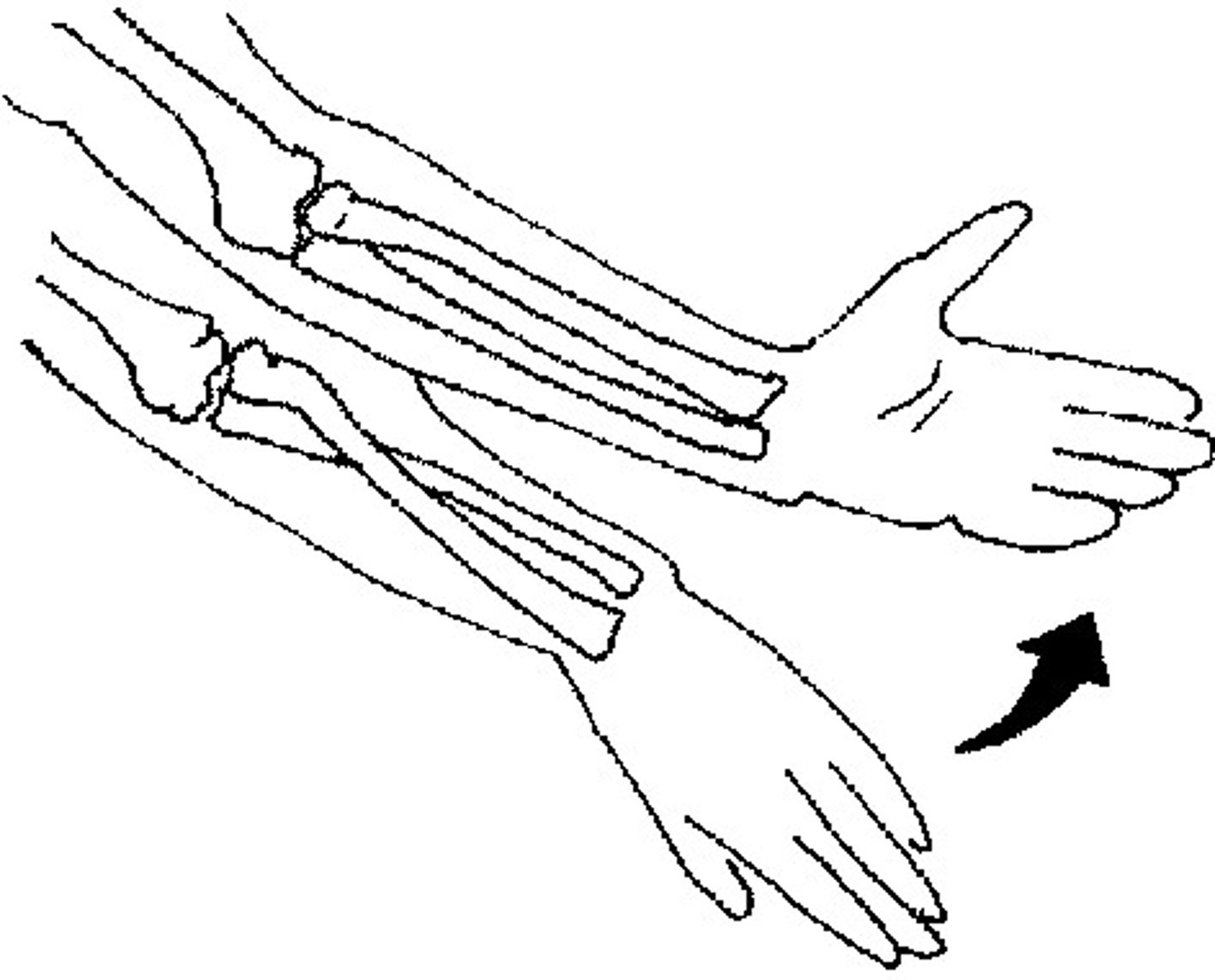
Pronation
Rotating forearm so palm faces posteriorly or inferiorly (palm down; "pour it out")
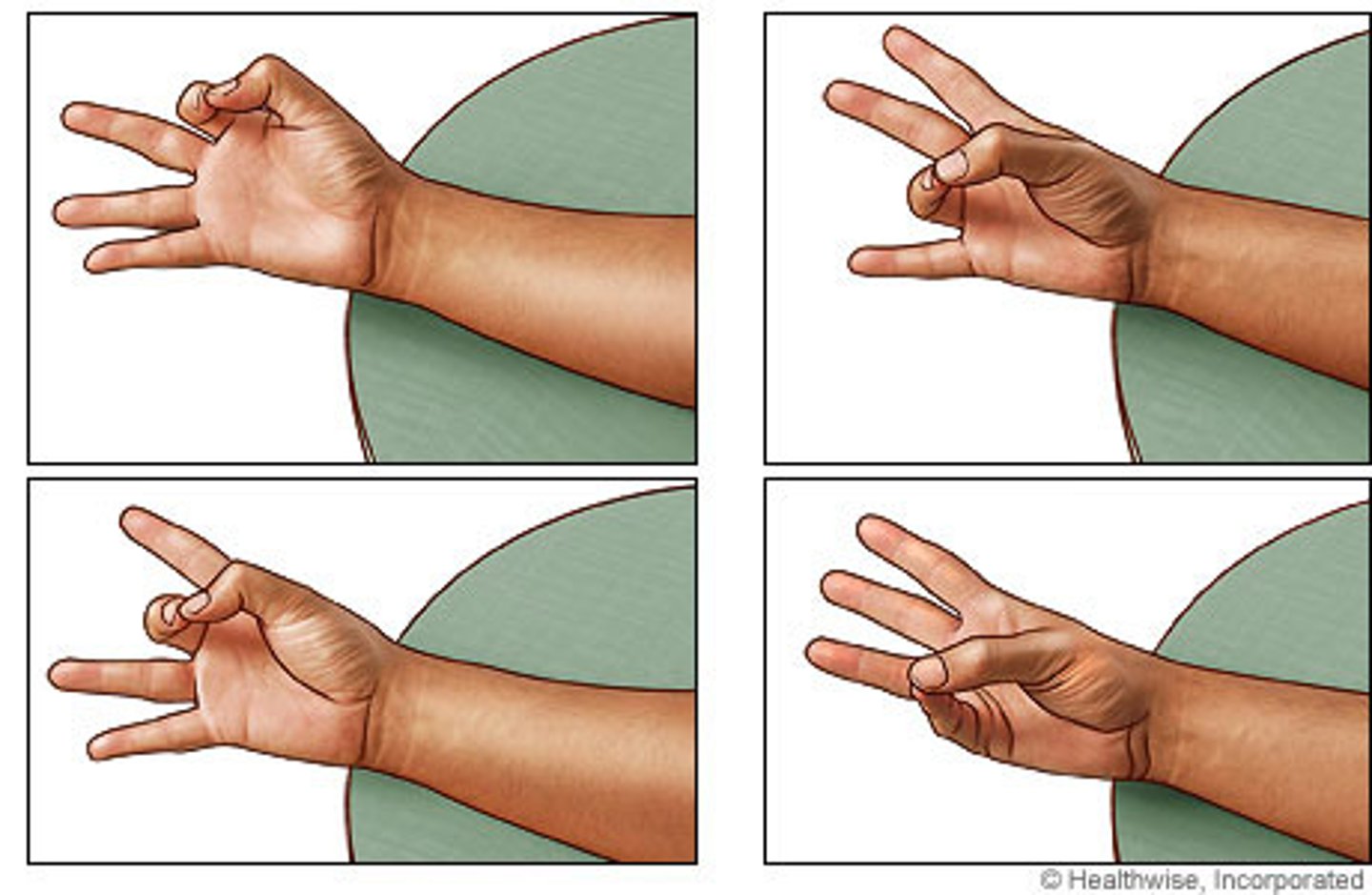
Opposition
Moving the thumb so that it touches the other fingers; for picking things up
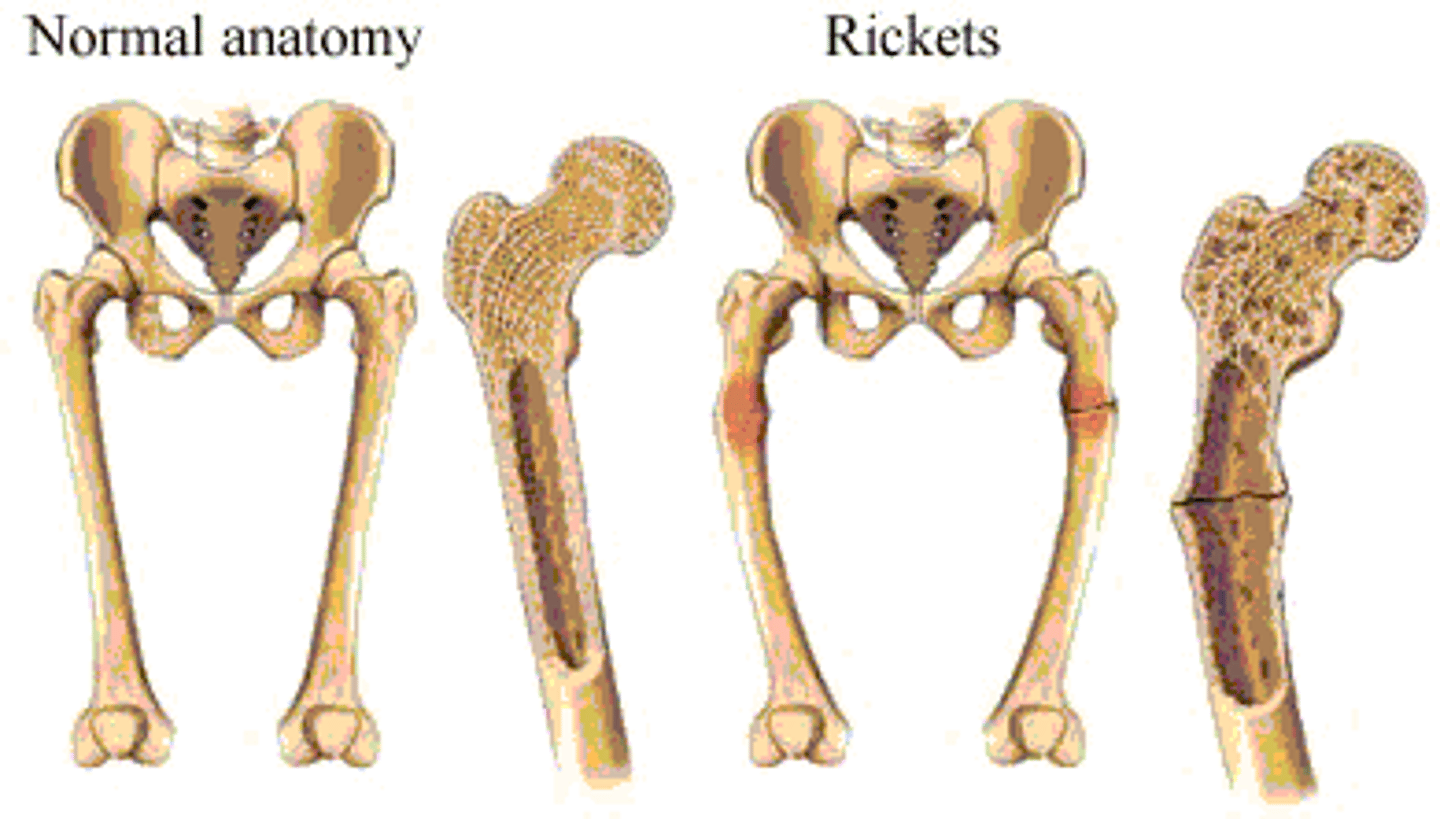
Rickets
Osteomalacia in children caused by a lack of Vitamin D, which produces malabsorption of calcium and phosphate.
Results in malformed bones and bowed legs.

Osteomalacia
A disease marked by softening of the bone caused by calcium and vitamin D deficiency.
The adult form of rickets.
arthritis
Most common joint disorder
Definition: Inflammation of the joint
DAMNIT acronym
What is causing the inflammation?
D - degeneration
A - anomaly
M - Metabolic
N - Neoplasia
I - Immune mediated
T - Trauma
Four examples of how Arthritis can occur.
Rheumatoid Arthritis - immune-mediated - "I"
Osteoarthritis - Wearing and tearing - age and obesity - "D"
Gout - Uric acid deposits - "M"
Bursitis - Sack of fluid associated with the joint - "T"
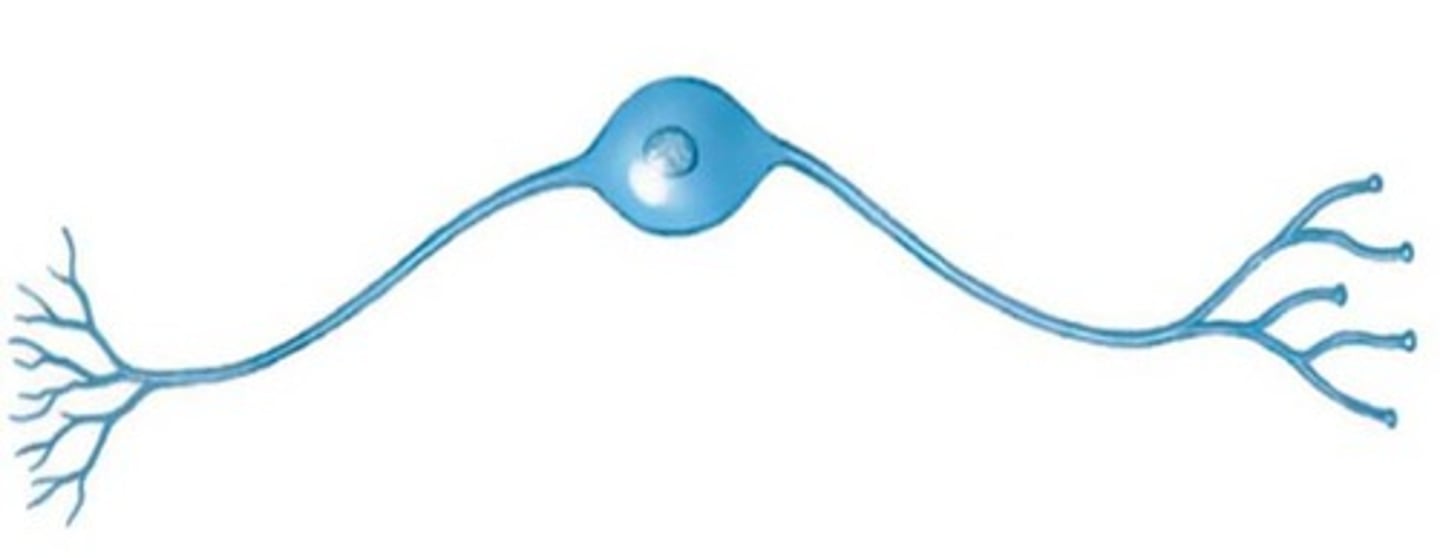
neurons
Nerve cells.
They transmit impulses for communication within the nervous and muscle systems. Therefore, they are the functional units of the nervous system.
neuroglia
Support cells that serve to both support and nourish neurons.
They are capable of cellular division but do not conduct impulses like neurons do.
They are also known as glial cells
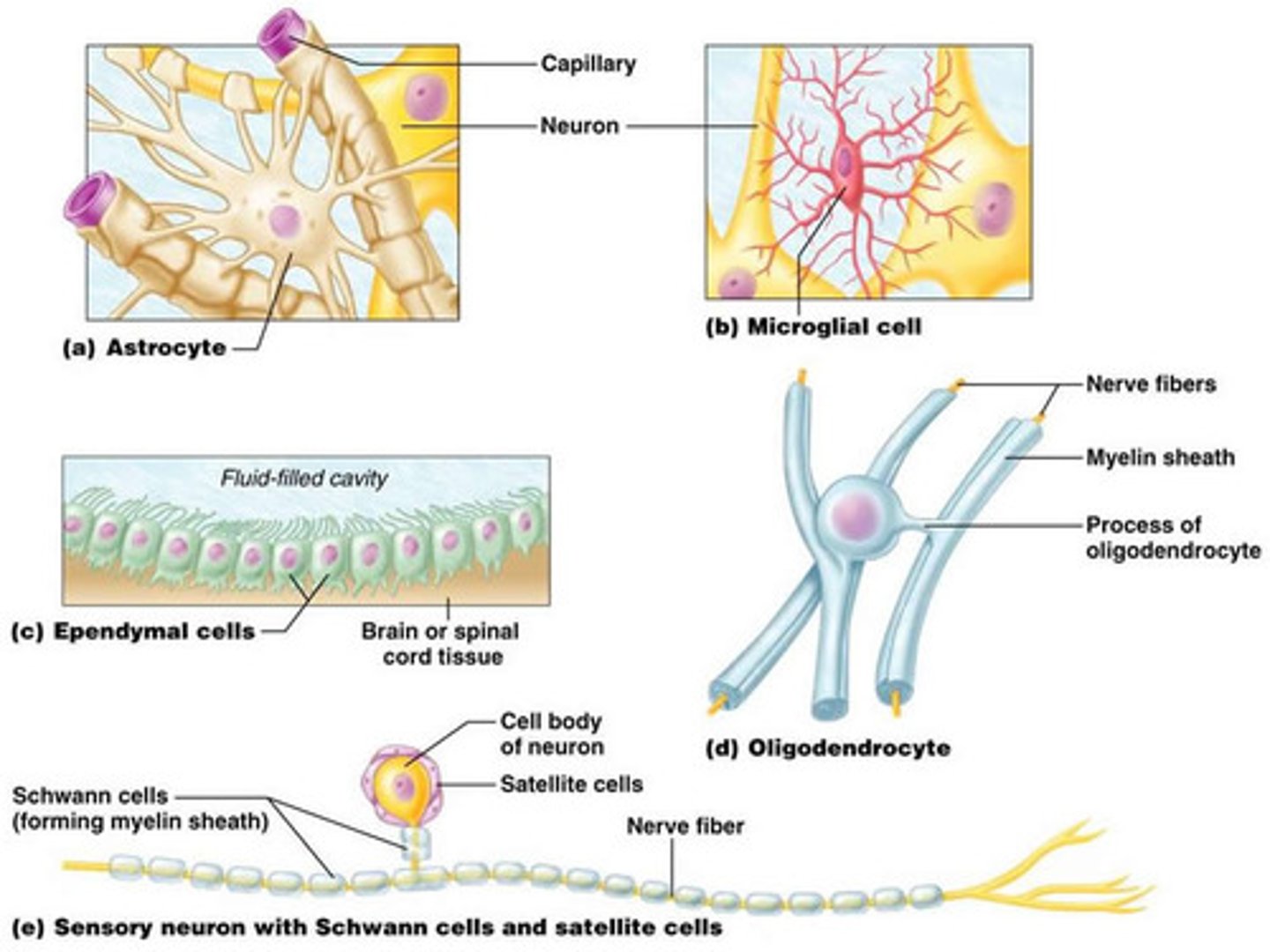
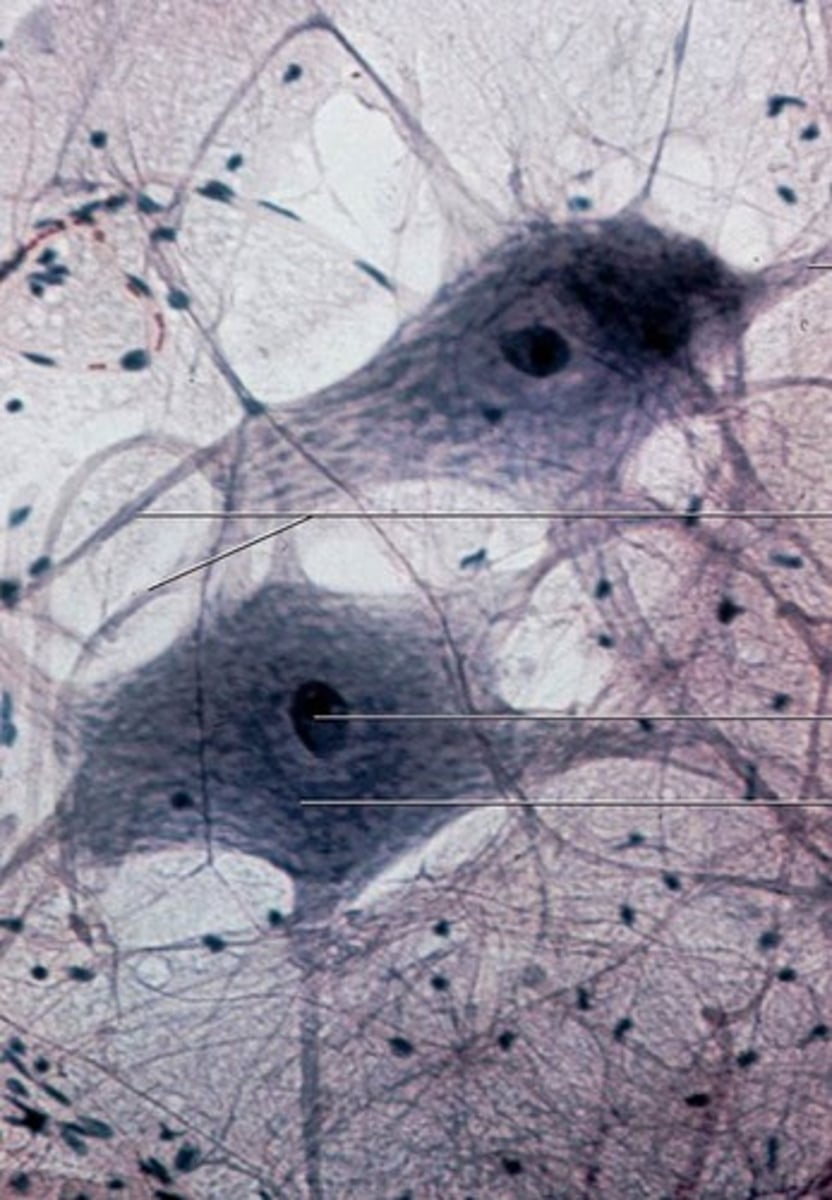
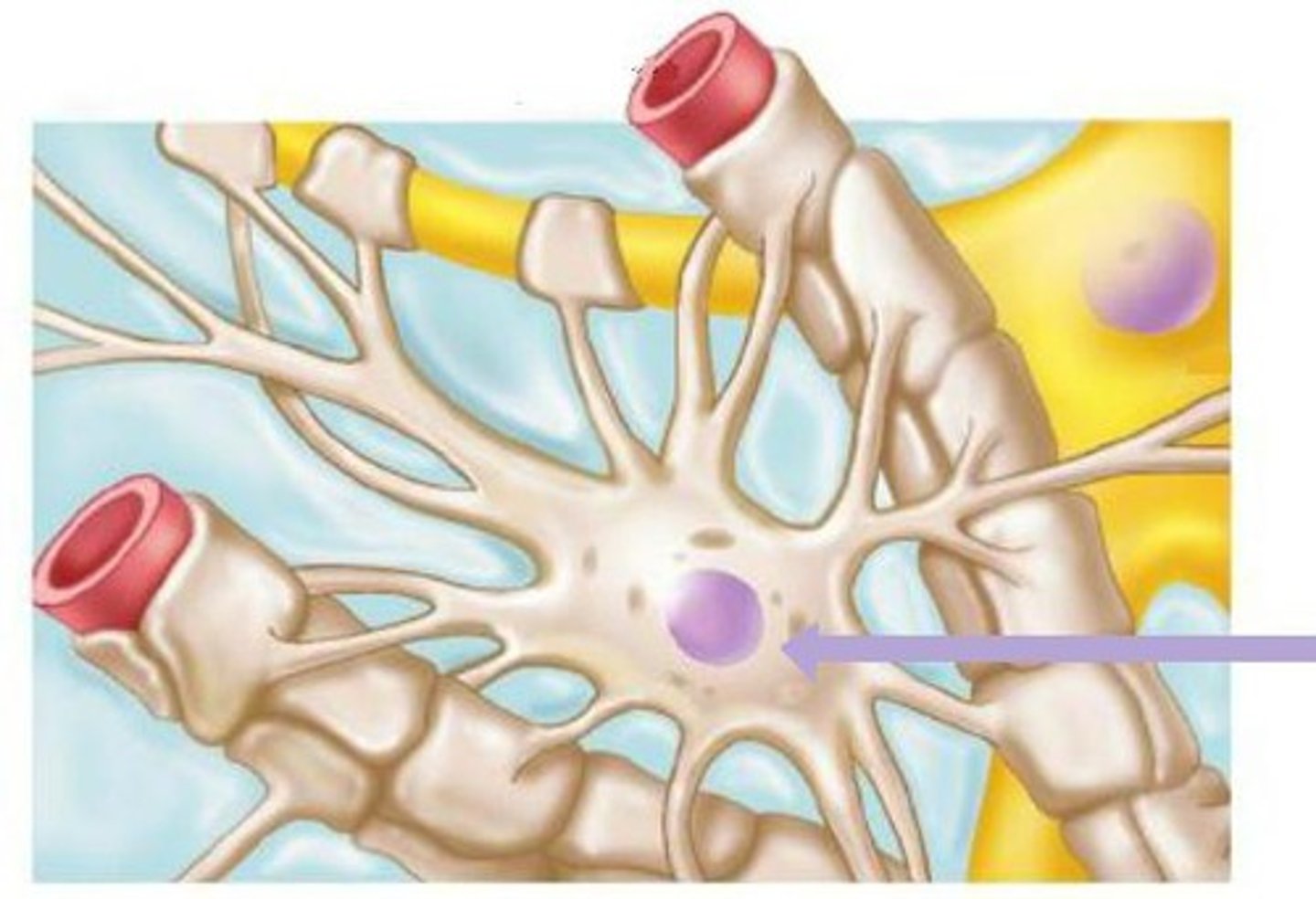
astrocytes
Neuroglia found in the CNS.
They help form the blood-brain barrier (BBB).
The BBB allows certain substances to pass while harmful things are kept out.
They also help maintain the chemical environment by helping clear out neurotransmitters, and they provide nutrients for the neurons.
ependymal cells
Neuroglia found in the CNS that produce cerebral spinal fluid.
They are located in the ventricles of the brain and the central canal in the spinal cord.
microglia
Neuroglial cells found in the CNS that provide protection.
They will engulf invading microbes or clear debris from dead cells.
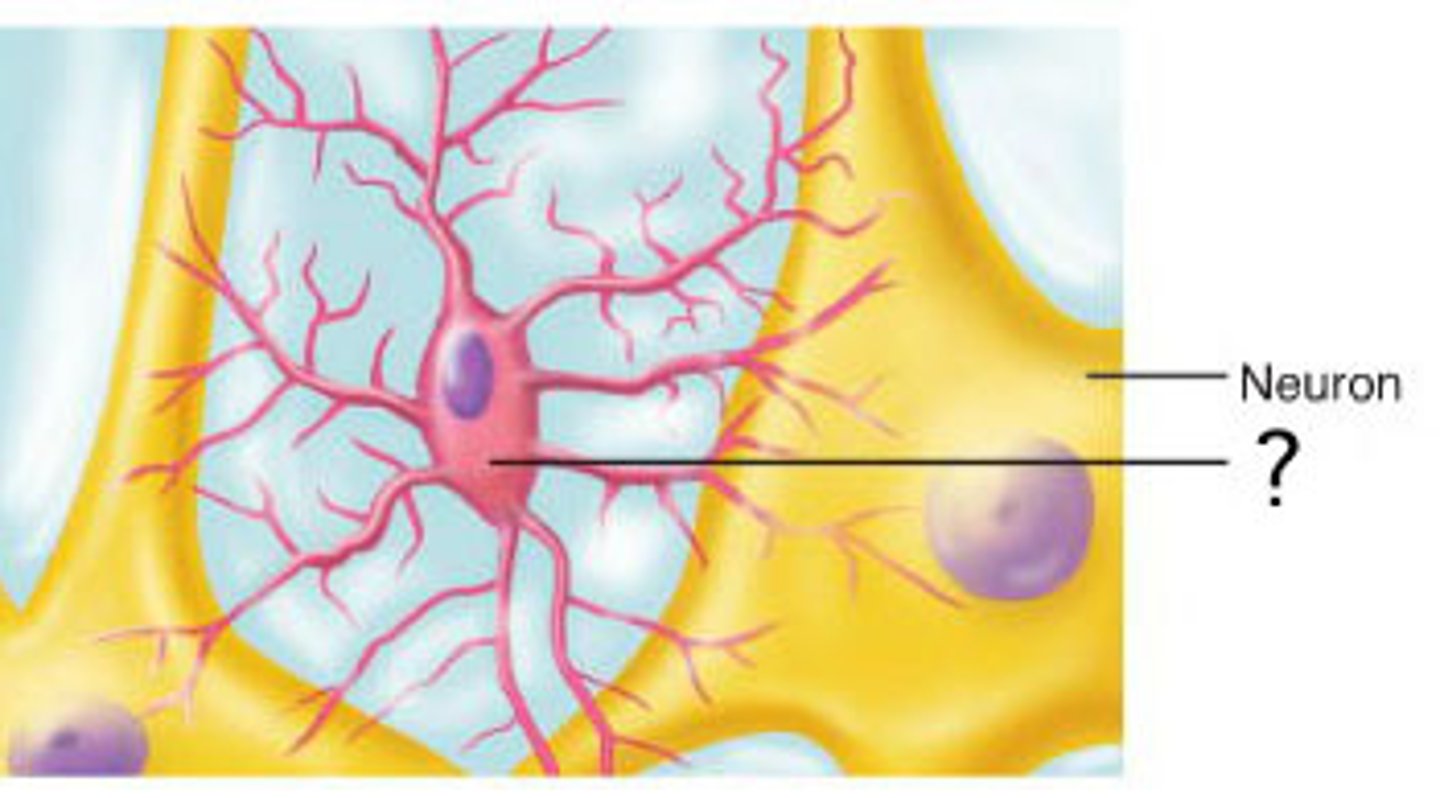
oligodendrocytes
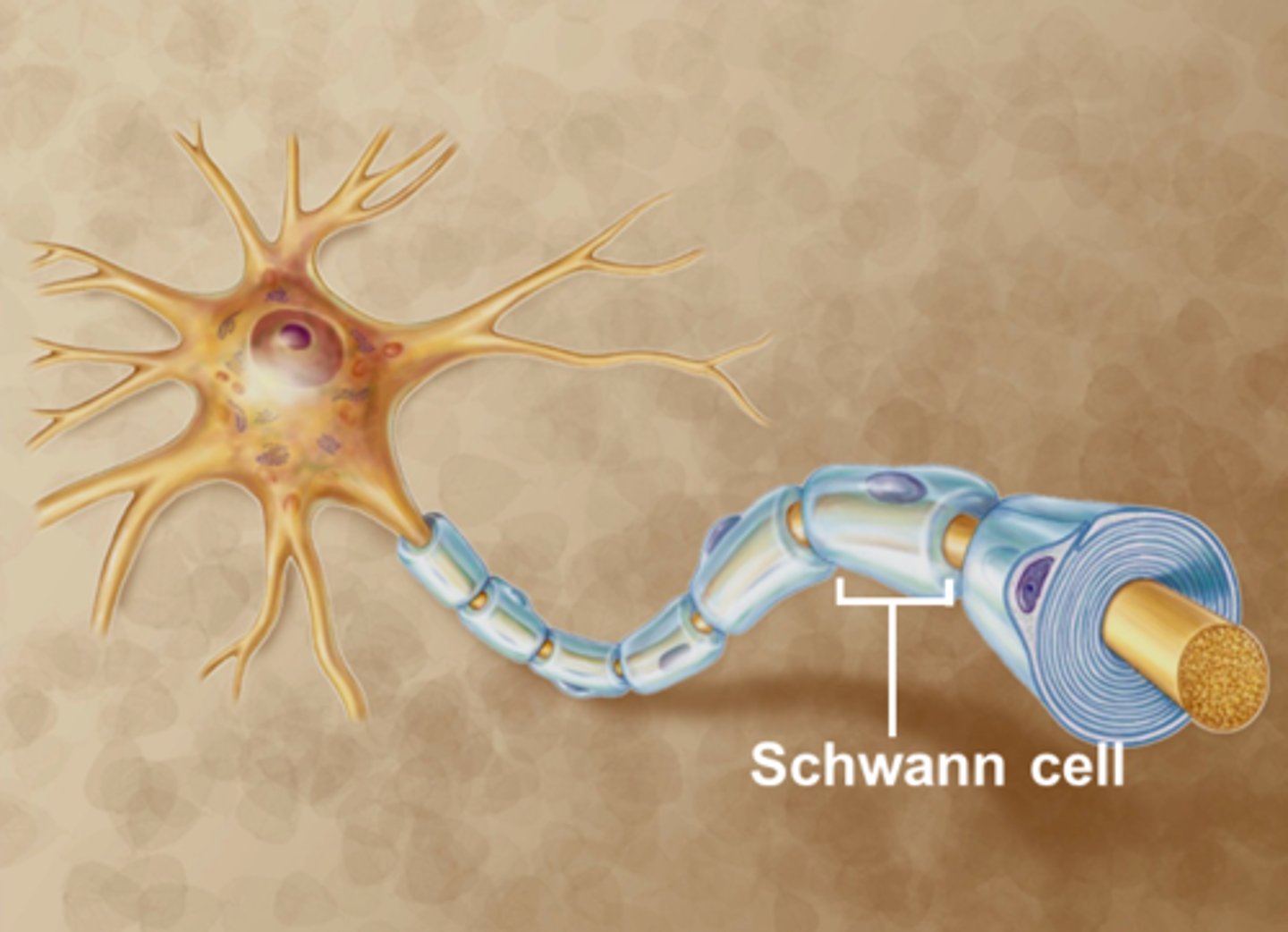
Neuroglial cells that are found in the CNS that produce the myelin sheaths.
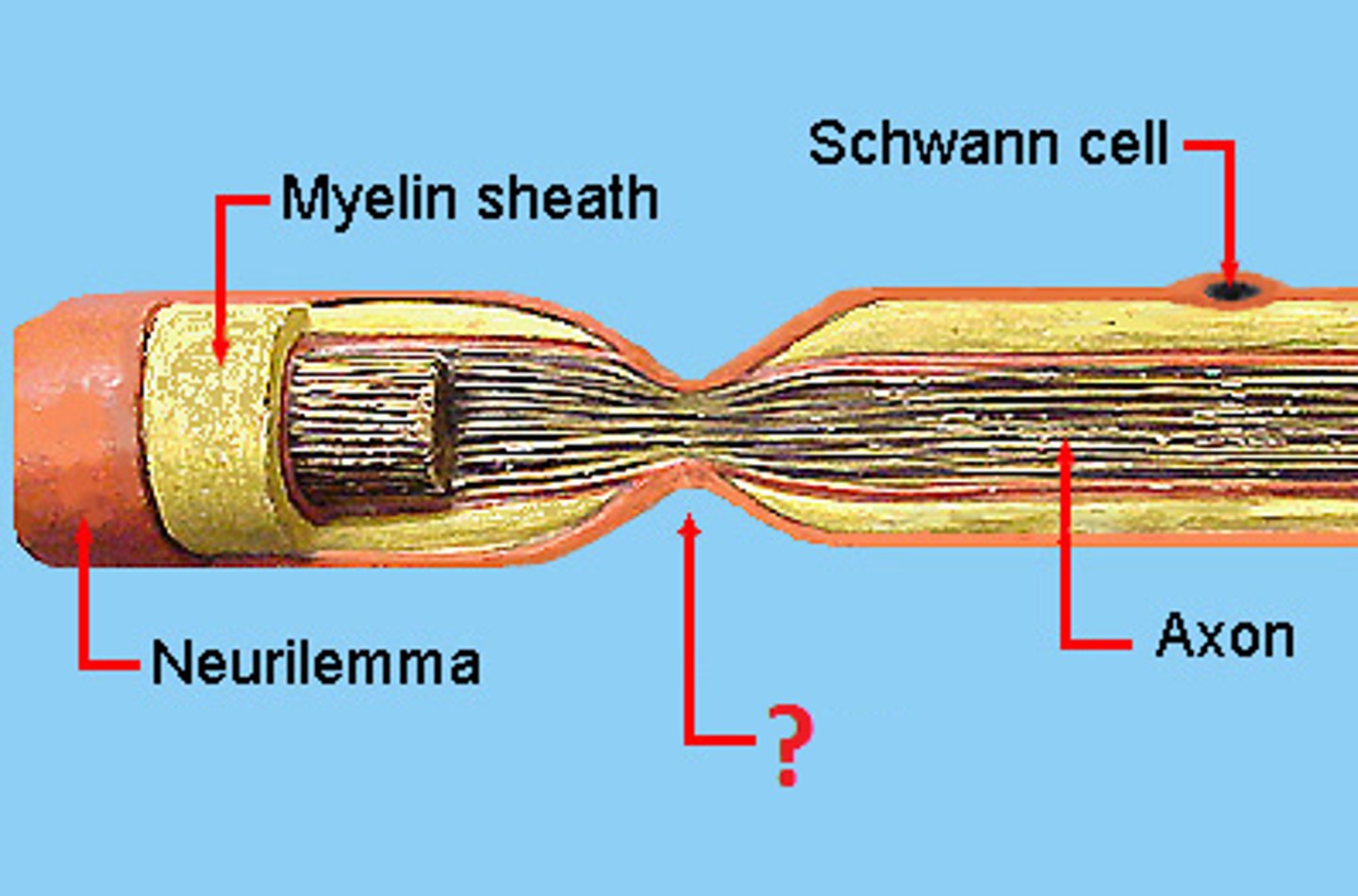
schwann cells
Neuroglia found in the PNS that form the myelin sheaths for PNS neurons.
Four important characteristics of neurons
1. Extreme longevity
Nerve cells are formed during development and have an extreme longevity (meaning, they live a long time).
2. Amitotic
Although some research shows regeneration is possible if the cell body of a neuron remains intact, it is a very slow process and in general they are termed amitotic or not capable of mitotic division.
3. High metabolic rate
Neurons have a very high metabolic rate and a constant need for oxygen and glucose in order to survive
4. Irritability
Irritability means neurons are capable of responding to stimulation.
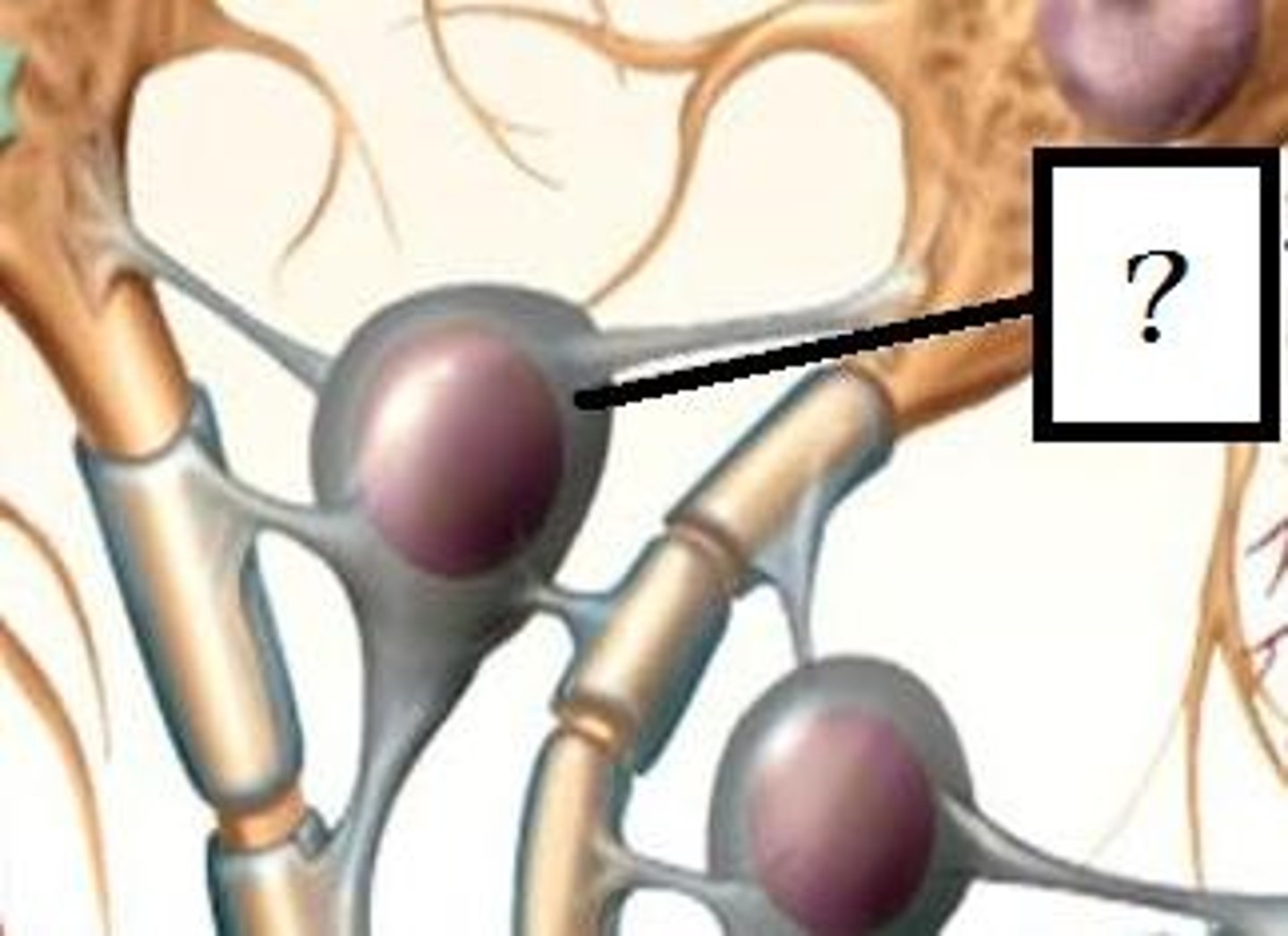
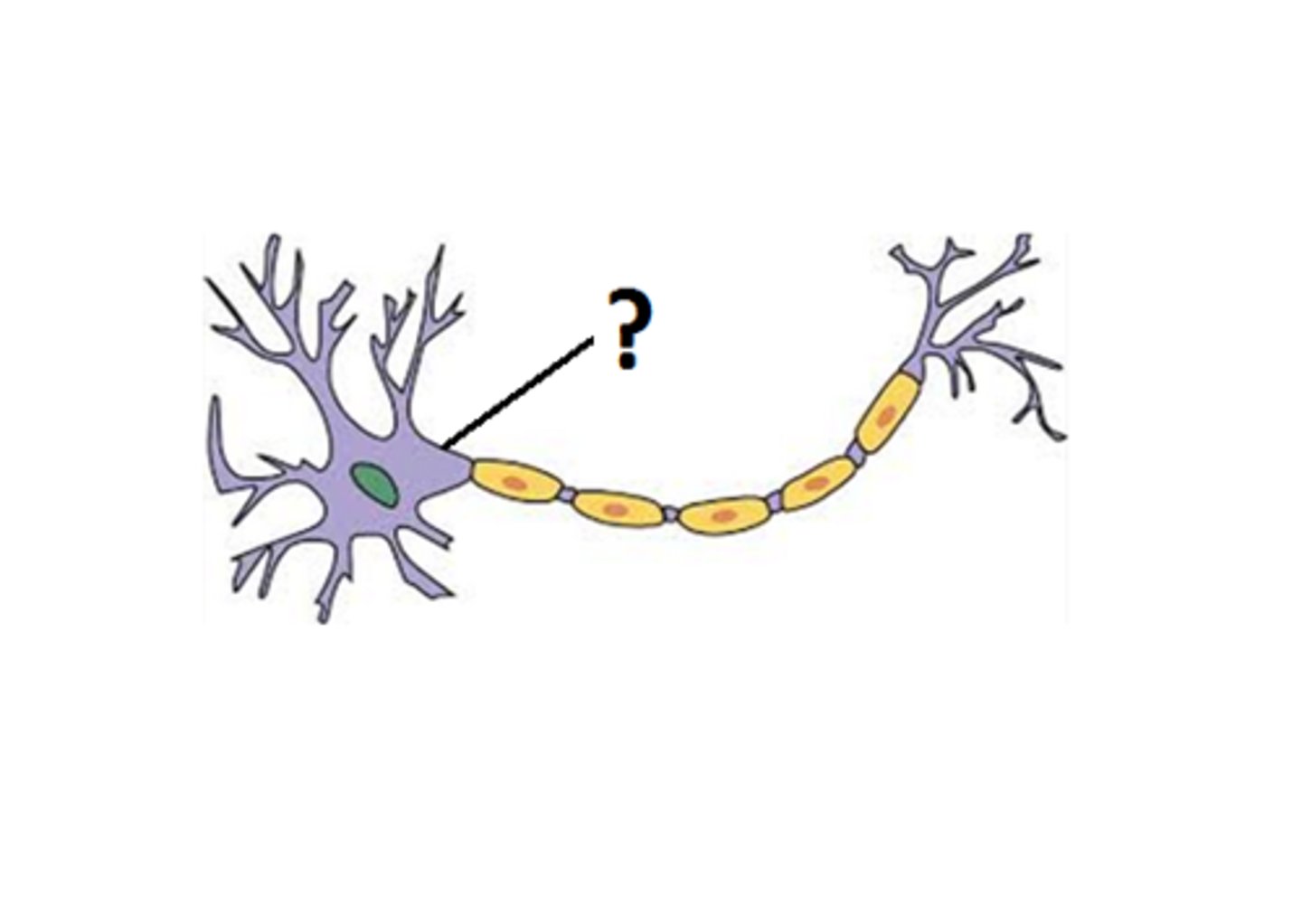
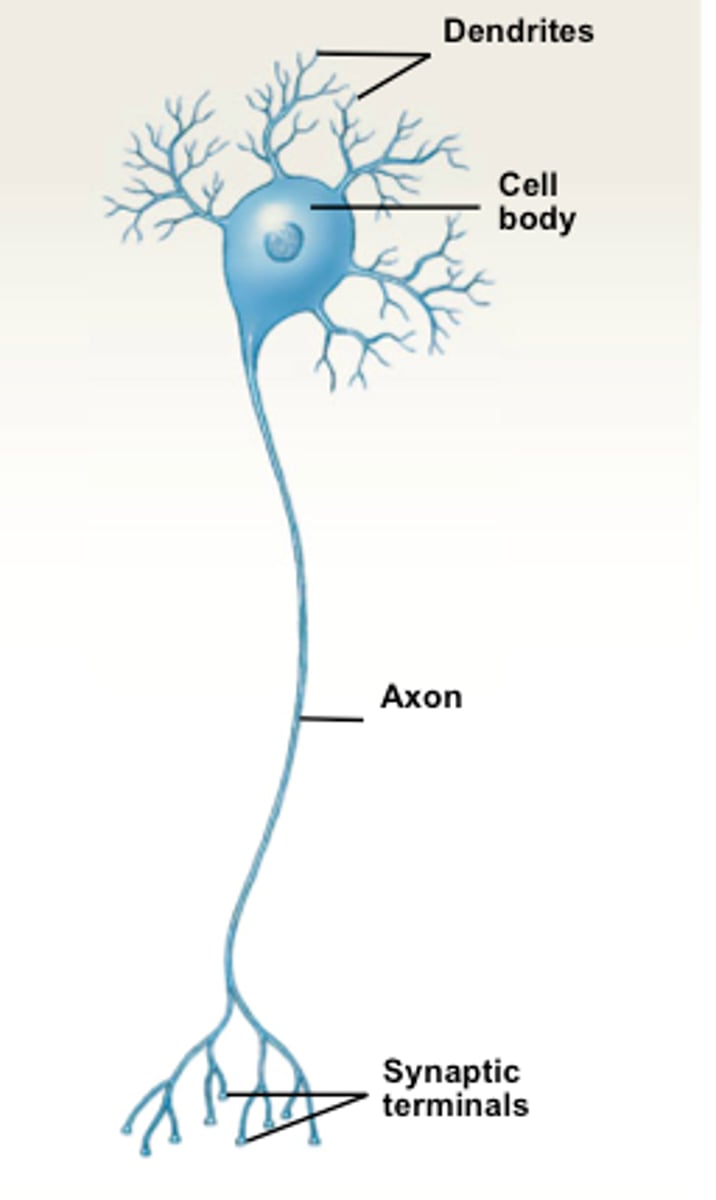
Three parts of a neuron
cell body, dendrites, axon
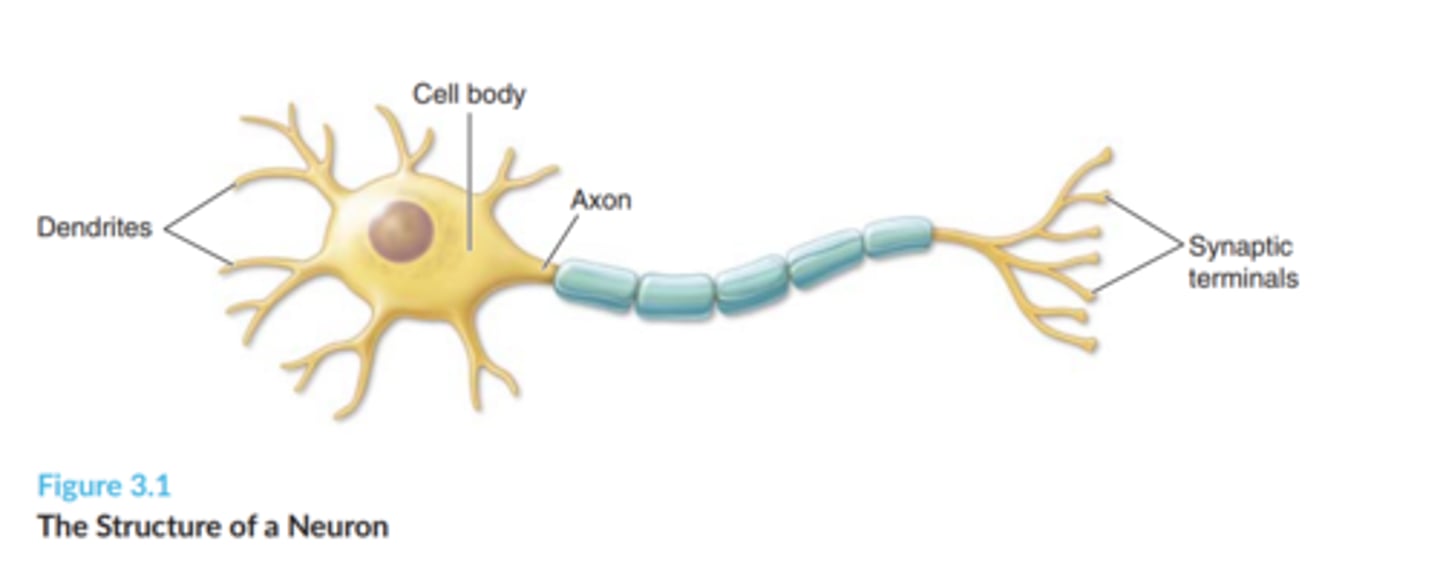
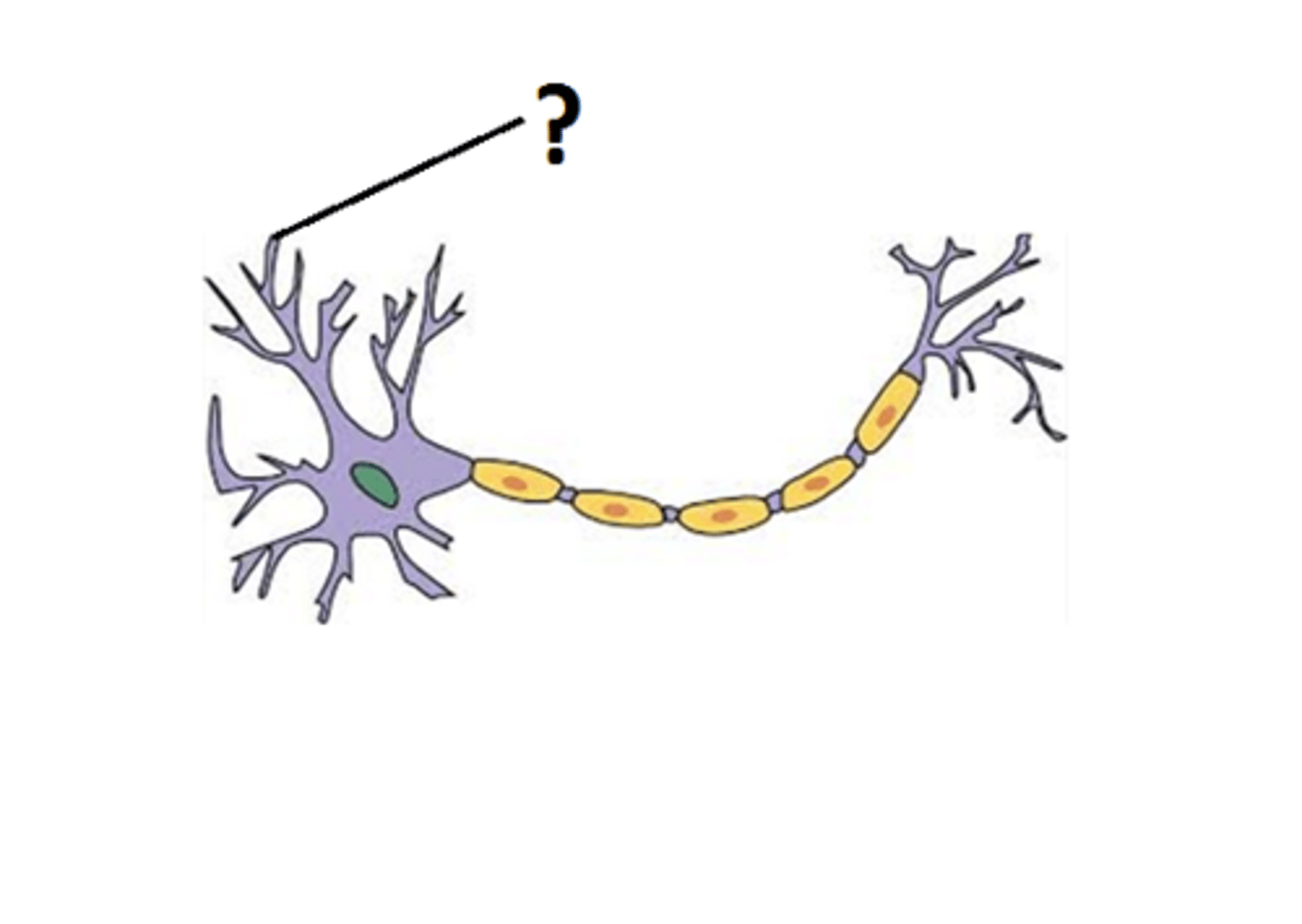
Dendrites
The shorter, branched structures that extend from the cell body.
This is the receptive region of the neuron, or where the neuron receives signals from sensory receptors or other neurons.
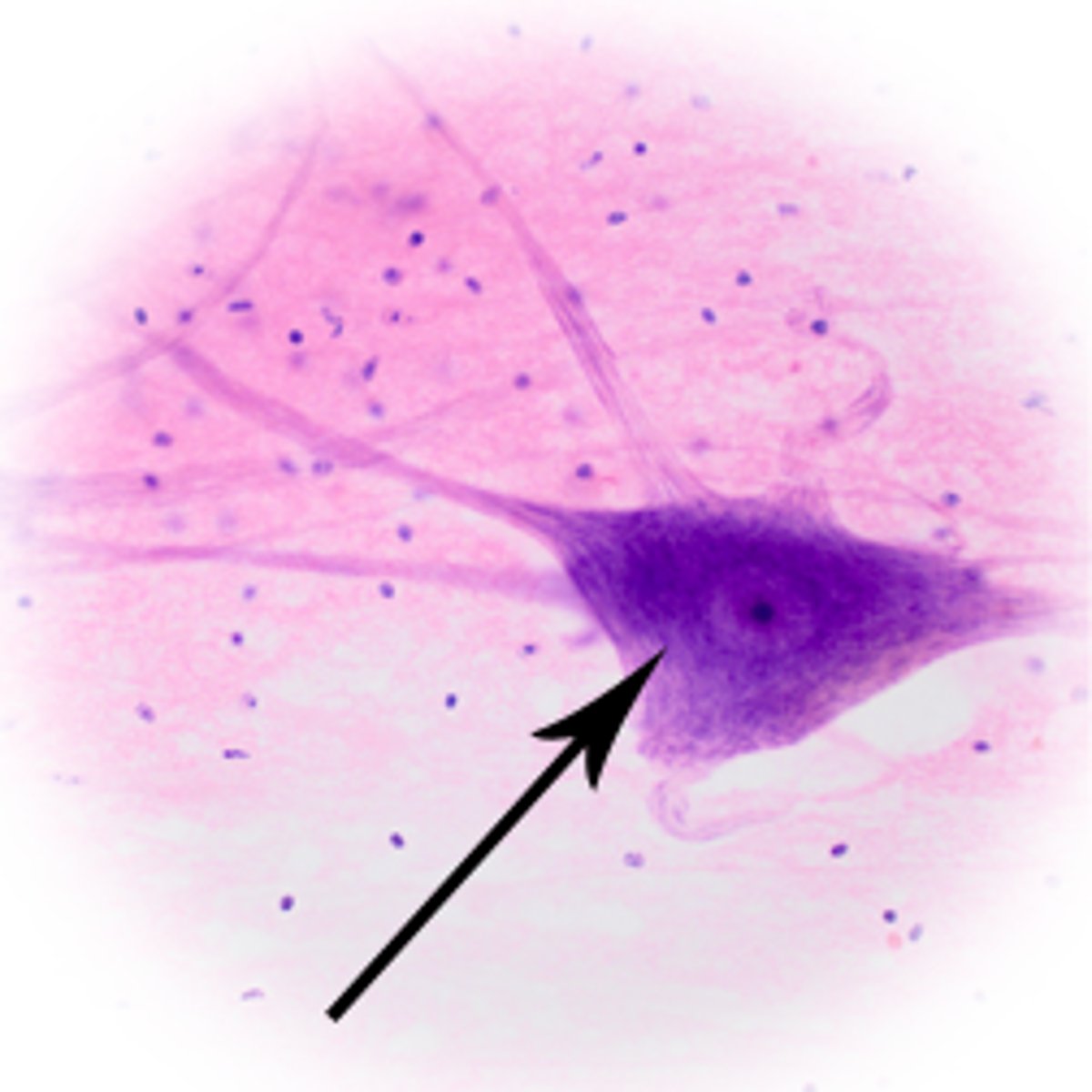
cell body of neuron
The enlarged portion of a neuron that most closely resembles other cells. Also known as the soma.
Contains the nucleus and other organelles such as mitochondria and endoplasmic reticulum.
It coordinates the metabolic activity of the neuron.
It must be intact in order for a neuron to be able to regenerate.
In the CNS they cluster to form nuclei and in the PNS they cluster to form ganglia.
The conductive region of the neuron (along with the axon)
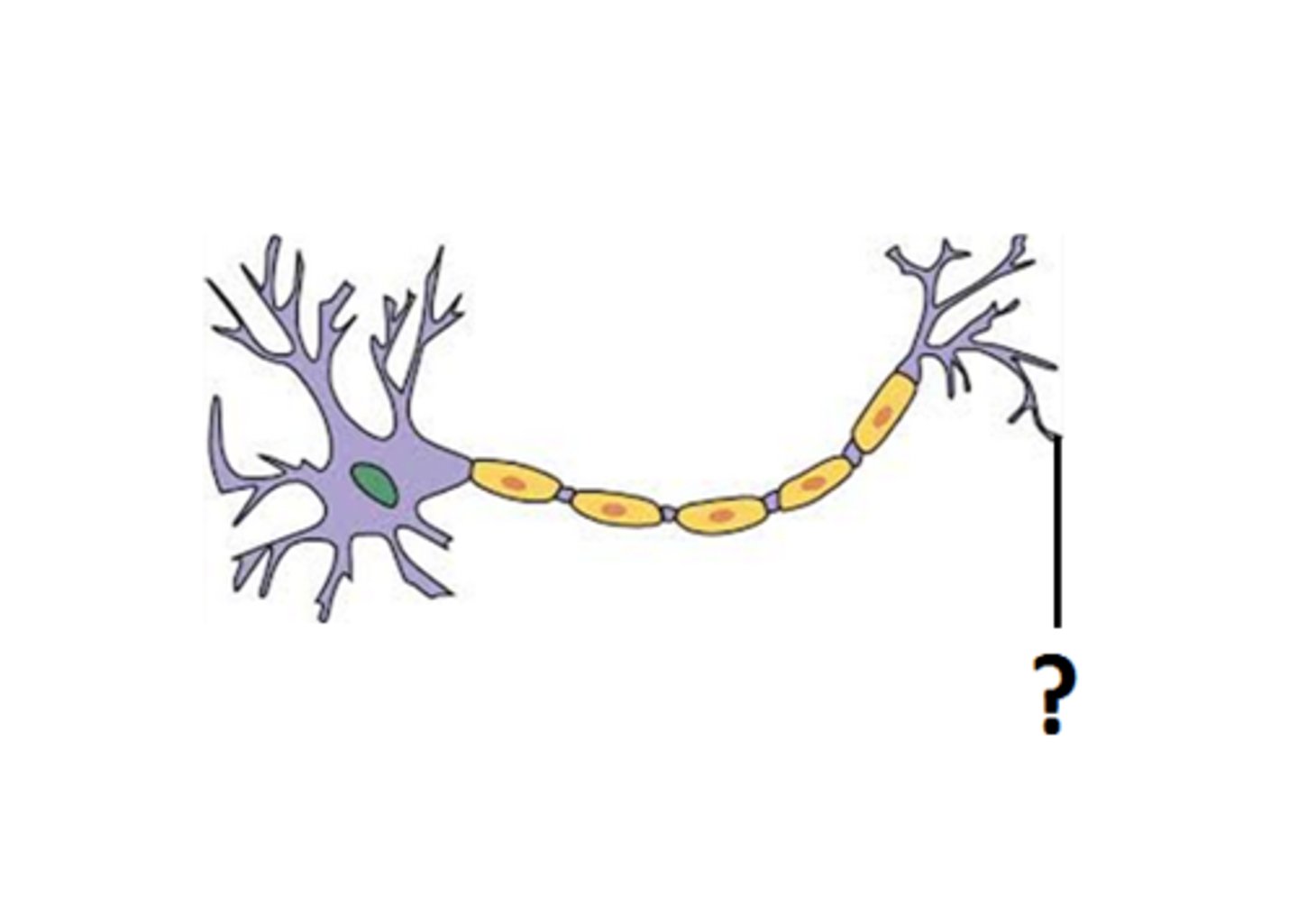
Axon
The extension of a neuron, ending in branching terminal fibers, through which messages pass to other neurons or to muscles or glands
The conductive region of the neuron (along with the neuron body)
axon hillock
The thickened area that connects the cell body and the axon. It is here that an action potential or neural impulse originates
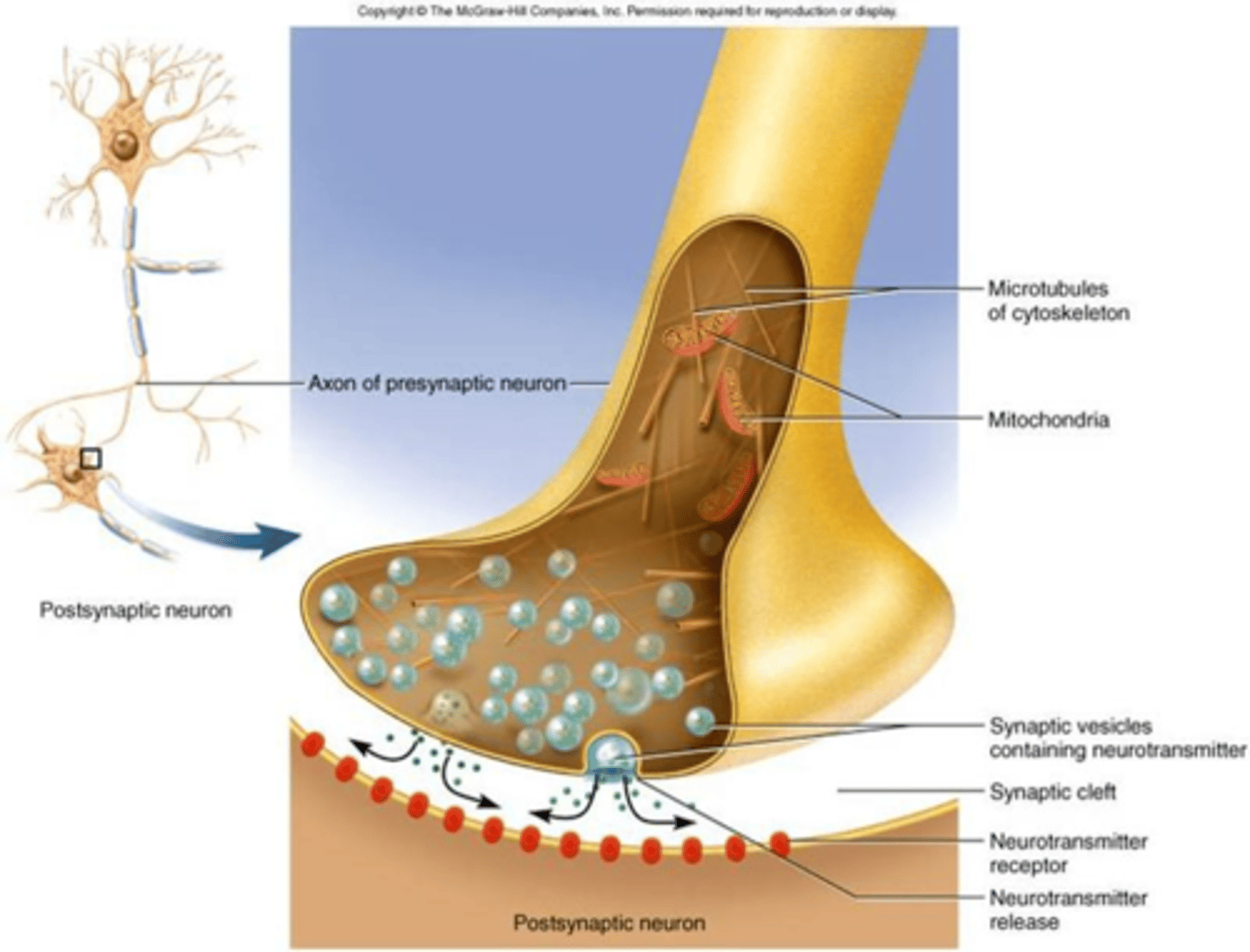
axon terminals
Branches at the end of the axon that are responsible for releasing neurotransmitters into the synapse so that communication can continue between two neurons.
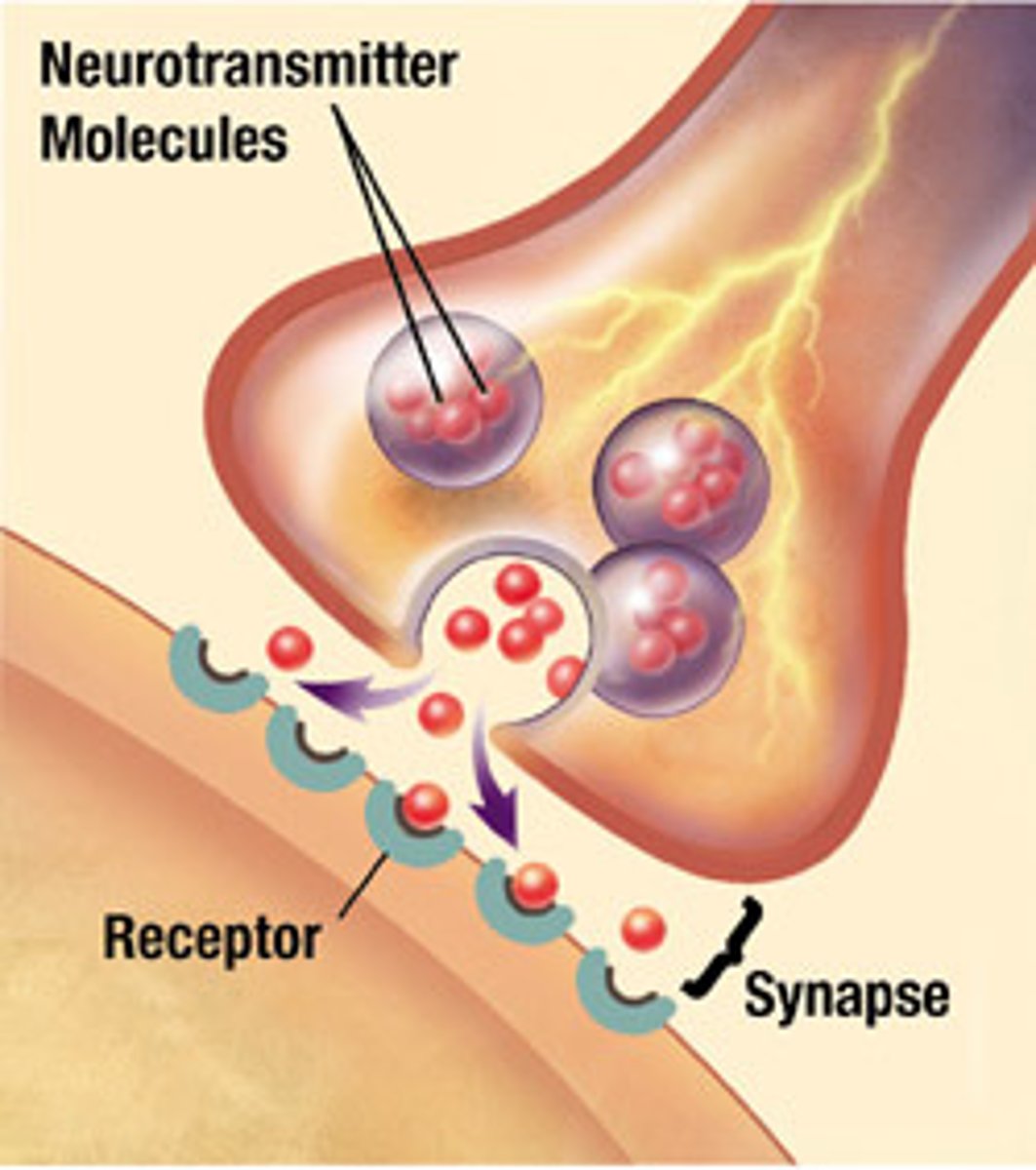
neurotransmitters
Chemicals that carry nerve messages across the synaptic cleft from the presynaptic neuron to the postsynaptic neuron.
myelin sheath
A layer of fatty tissue segmentally encasing the fibers of many neurons; enables vastly greater transmission speed of neural impulses as the impulse hops from one node to the next.
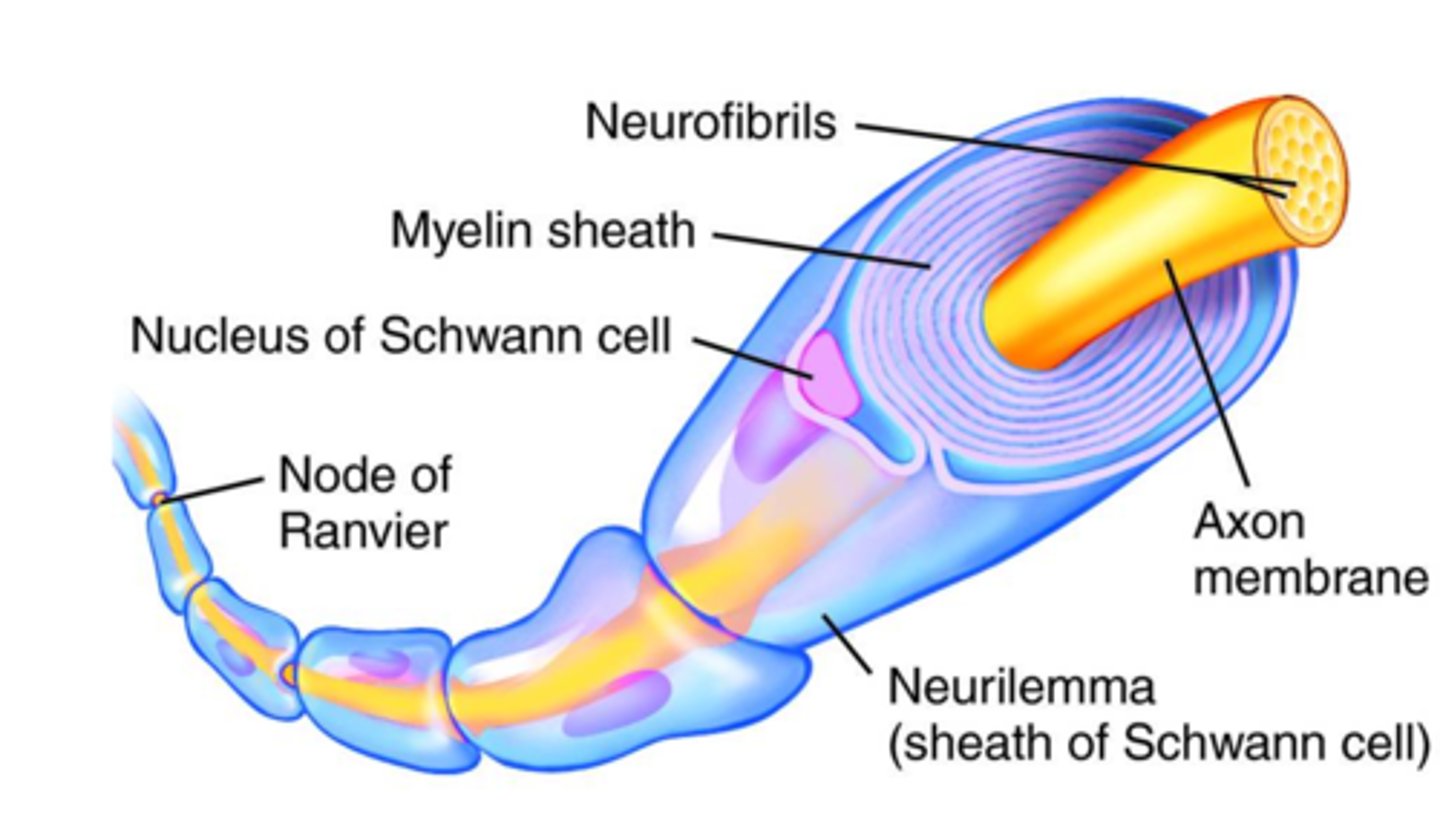
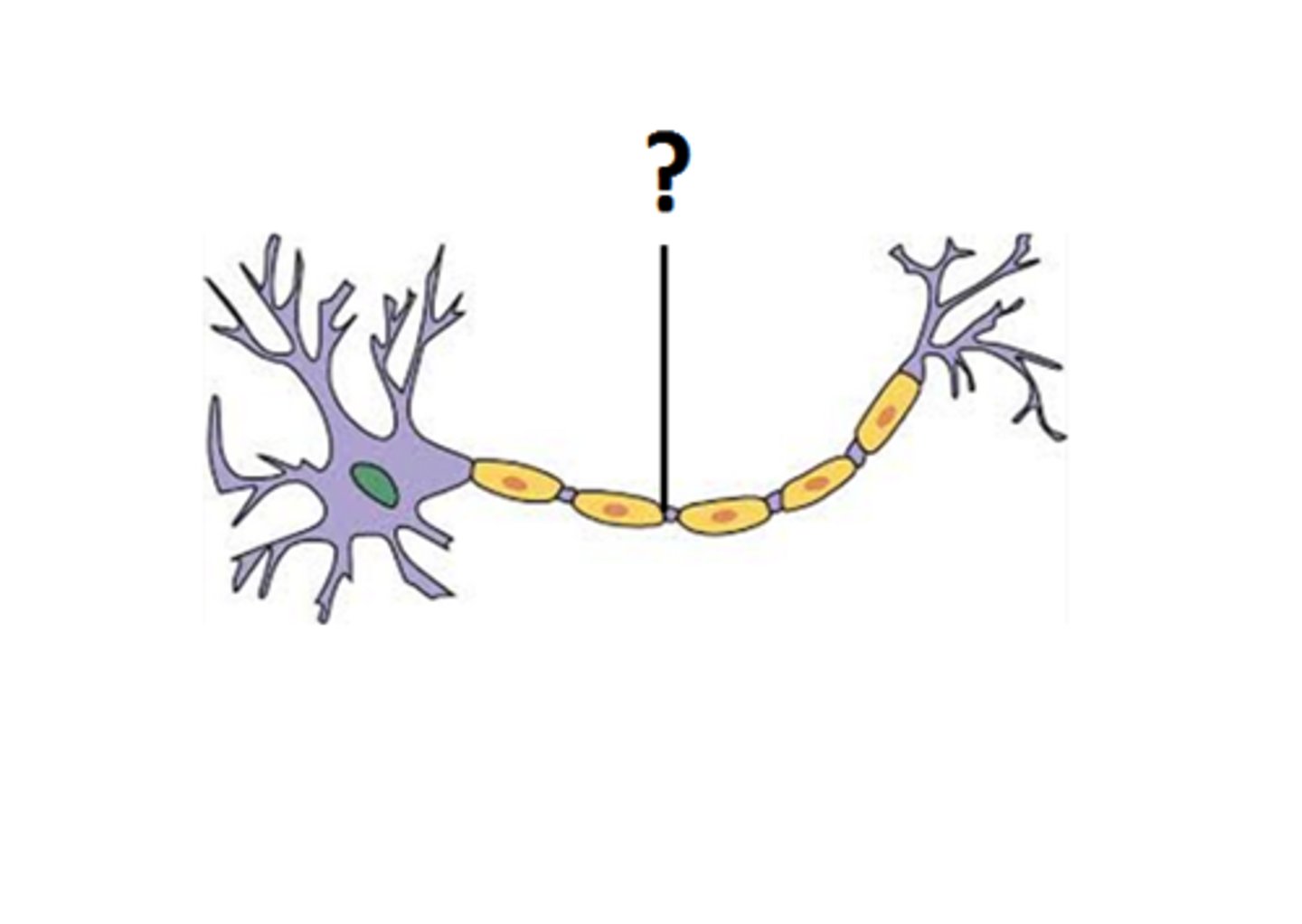
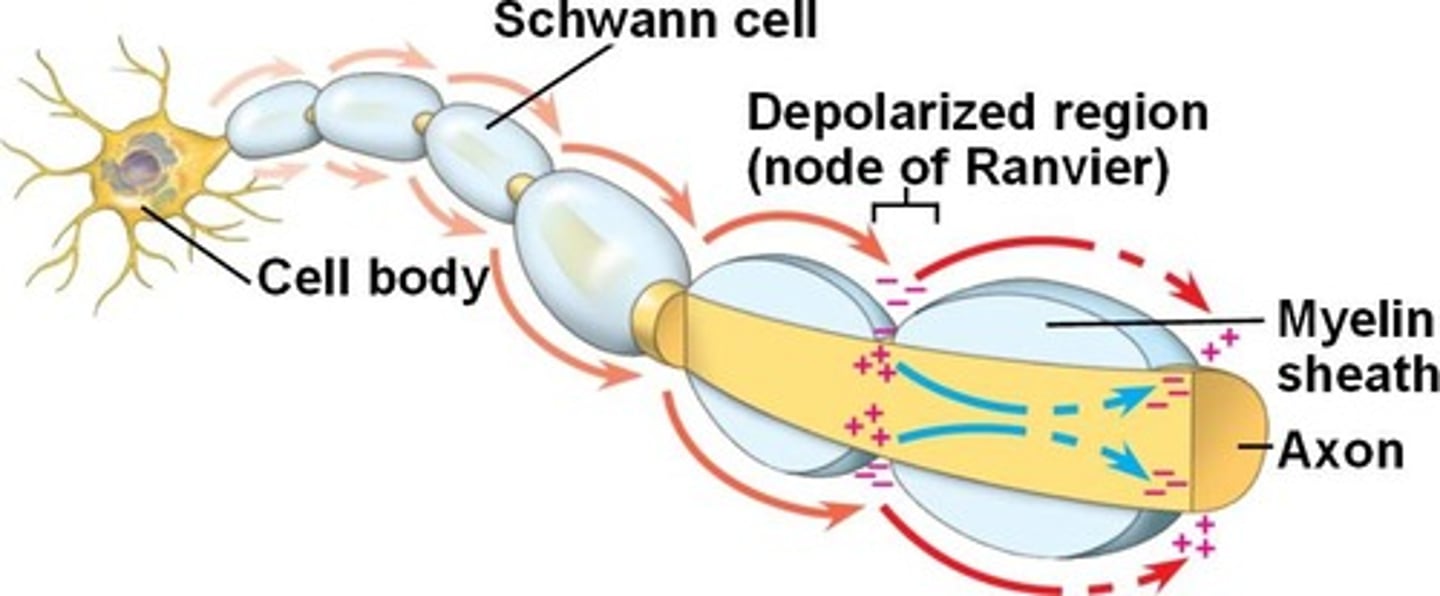
Nodes of Ranvier
The gaps found in myelinated axons.
During saltatory conduction in a myelinated neuron, the electrical signal will jump from one node to the next or travel at a very fast rate (in comparison with unmyelinated axons).
saltatory conduction
The way in which an electrical impulse travels in a myelinated axon.
The electrical impulse "jumps" from one Node of Ranvier to the next.
In contrast, in continuous conduction in an axon without myelin, the impulse must travel the entire length of the axon without "jumping" and therefore travels at a slower rate of speed.
synapse
A space or gap between an axon terminal and another neuron or effector (muscle or gland).
The neurotransmitter is released into this space and then binds to a specialized receptor on the postsynaptic neuron or effector.
The neuromuscular junction is the name for the space between a nerve cell and the skeletal muscle fiber that it supplies.
multipolar neurons
Neurons that have many dendrites and one axon.
This type of neuron is found in the CNS and in motor neurons.
bipolar neurons
Neurons that have one dendrite and one axon.
These are found in the photoreceptor layer of the retina of the eye and in the nasal cavity.