Respiratory Infections
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
what is the most common site for infections?
Respiratory tract
respiratory infections are caused by…?
– Direct contact with the environment
– Constant exposure to infectious agents in the air
Respiratory infections are more common what time of year? why?
winter
1. Proximity to others while confined indoors & poor ventilation
2. Breathing cold air → cough, sneeze, runny nose
3. Cold and dry air → smaller respiratory droplets → stay longer in the air → Increased transmission of pathogens
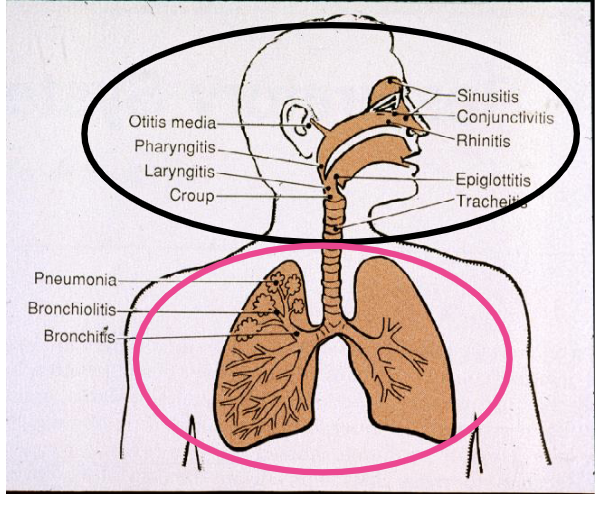
the upper respiratory system consists of?
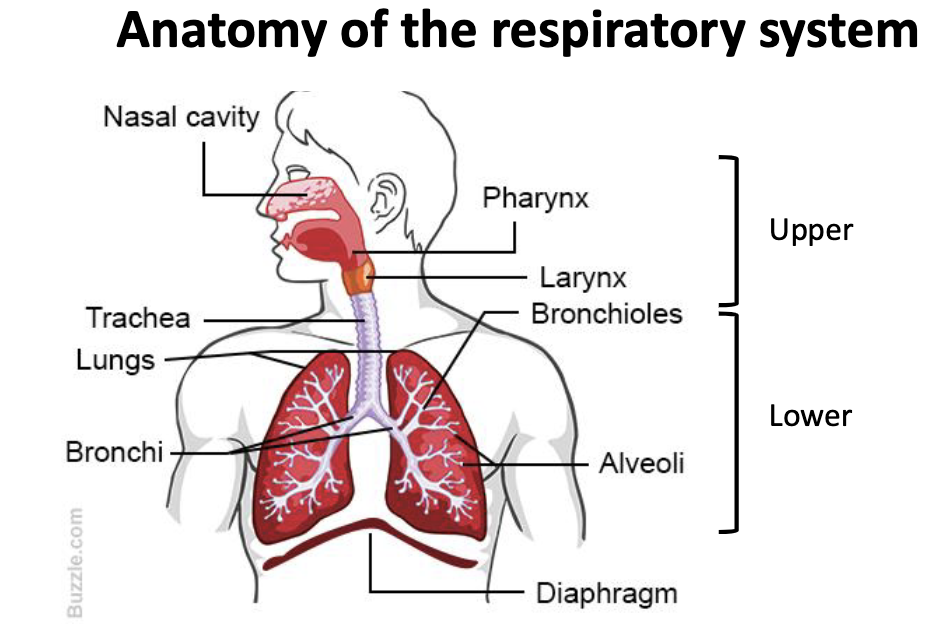
the lower respiratory system consists of?
what defense mechanisms does the nose have (respiratory tract)?
• Nose hairs (filters)
• Nasal turbinates (filters)
• Nasal mucus (sticky, enzymes)
what defense mechanisms does the throat/bronchi have (respiratory tract)?
• Mucociliary escalator
• Coughing reflex
what defense mechanisms does the alveoli have (respiratory tract)?
Alveolar macrophages
Risk factors for respiratory diseases
Anything that impairs the defenses of the respiratory tract:
• Smoking
• Weak immunity
• Serious diseases (lungs, heart, kidney)
• Asthma
• Dry air
• Pollutants
what is the mucociliary escalator (ME)? what are the 2 parts?
major barrier against infection
made of:
goblet cells → produce mucus
ciliated epithelial cells (create upward flow)
how does the mucociliary escalator work to as a barrier against infection?
The cilia are continually beating, pushing mucus up and out into the throat
Microorganisms are caught in the sticky mucus and moved up
how does smoking affect the micociliary escalator?
Smoking paralyzes the cilia
TRUE or FALSE?
A. Alveolar macrophages are a defense mechanism of the nasopharynx.
B. Anything that impairs the function of the mucociliary escalator is a risk factor for respiratory disease.
C. Pathogenic organisms stick to mucus, which helps them penetrate deeper into the respiratory tract.
D. Smoking impairs the expulsion of the mucus from the airways.
F
T
F
T
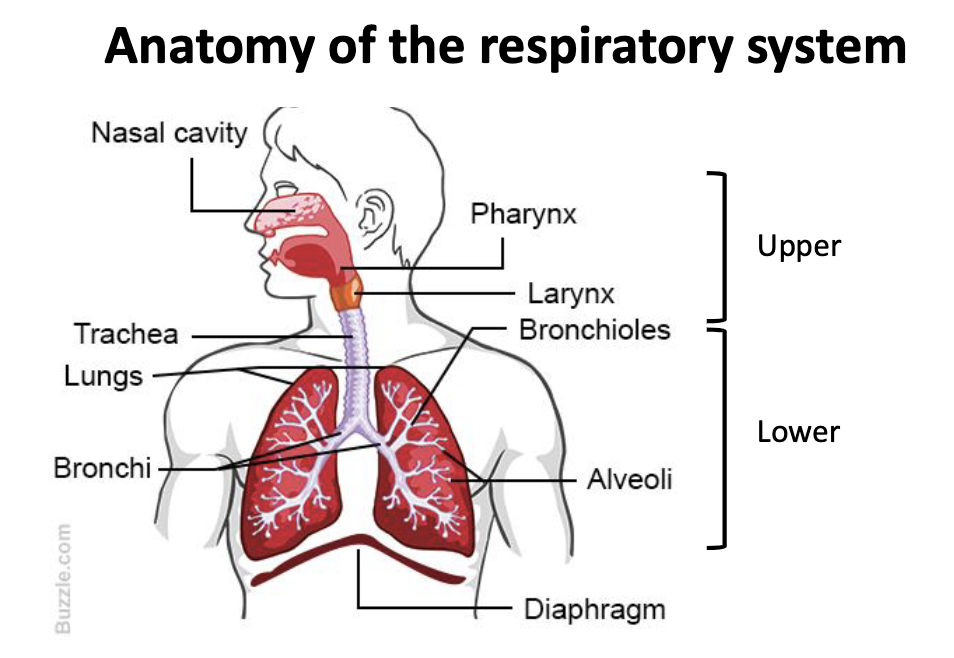
what are the 2 types of respiratory infections?
upper respiratory infections (URIs)
lower respiratory infections (LRIs)
pertussis is also known as
whooping cough
what are the early symptoms of pertussis (1-2 weeks)?
Early, cold-like symptoms (1-2 weeks):
Runny nose
Low-grade fever
Mild, occasional cough
what are the late symptoms of pertussis?
Fits of many, rapid coughs followed by a high-pitched "whoop"
Vomiting during or after coughing fits
Exhaustion after coughing fits
cough caused by pertussis may last how long?
>10 weeks (chinese call is 100-day cough)
pertussis is most dangerous in what demographic? why?
infants
can cause apnea (pause in breathing pattern) + cyanosis
__% of deaths due to B. pertussis infections are in infants under 1 year
~__% of infants under 1 year who get pertussis need hospital care
70%
50%
what type of bacteria is bordetella pertussis?
gram (-)
coccbacillus

bordetella pertussis: encounter
person-to-person (does not survive well in the environment), highly contagious
bordetella pertussis: entry
inhalation
bordetella pertussis: multiplication
obligate aerobe, extracellular, adheres to ciliated bronchial epithelial cells
bordetella pertussis: spread
local infection, no spread
how does bordetella pertussis cause damage?
Produces toxins that immobilize the mucociliary escalator
mucus builds-up
inefficient clearing of bronchial tubes
cough receptors become stimulated
the WHOOP is due to influx of air back into lungs after coughing episode
what is the pertussis vaccine called?
DTaP (for young children)
Tdap (for adults)
pneumonia is infection of the
lung parenchyma (a portion of the lung involved in gas transfer: the alveoli, alveolar ducts and bronchioles)
what is pneumonia caused by?
many different microbes (bacteria, viruses, fungi) which result in different diseases that share a common anatomical location
what characterizes acute penumonia?
sudden onset, symptoms progress over a few days
what are the community acquired vs nosocomial acute pneumonia syndromes?
Community acquired
Streptococcus pneumoniae, person-to-person
Legionella pneumophila, environmental
Nosocomial (hospital acquired)
Pseudomonas aeruginosa
what are the subacute or chronic pneumonia syndromes?
fungal pneumonia (Histoplasma capsulatum)
what type of bacteria is Streptococcus pneumoniae?
gram (+) diplococcus
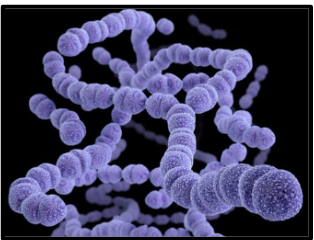
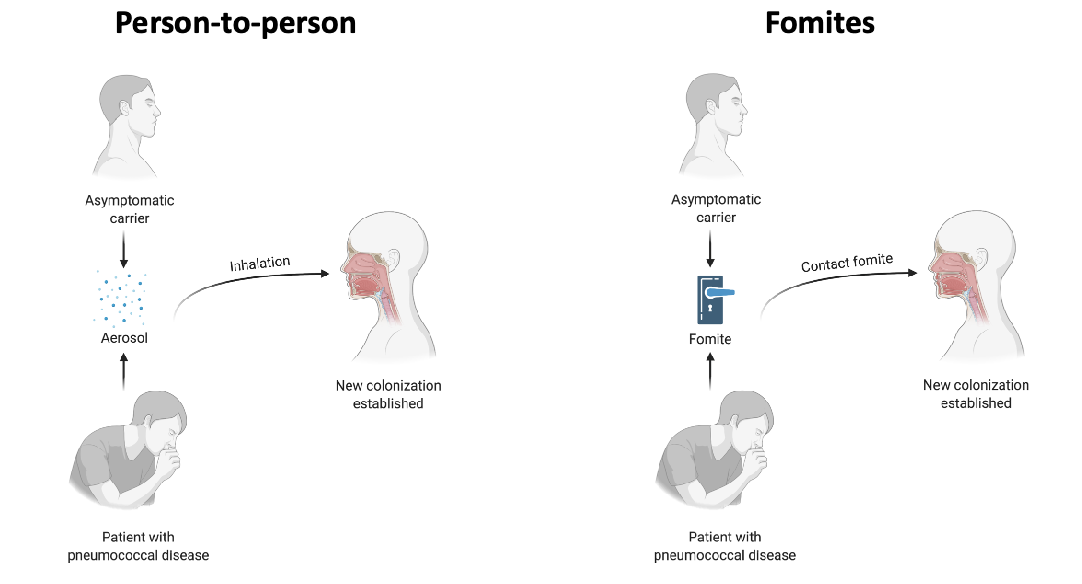
Streptococcus pneumoniae: encounter
asymptomatically colonizes the nasopharynx
–40-70% of children
–5-10% of adults
what is the most common cause of community-acquired pneumonia?
Streptococcus pneumoniae
what patient demographics are most susceptible to community-acquire pneumonia caused by Streptococcus pneumoniae?
– Young children < 2 years old
– Elderly > 65 years old
– Smokers
– Adults with chronic illness, weak immune system
Streptococcus pneumoniae: spread
person-to-person
fomites
spread of Streptococcus pneumoniae out of the nasopharynx can lead to diseases like?
spread to blood → bacteremia, sepsis
spread to other organs
t/f: pneumonia is often fatal before antibiotics but disease responses quickly to antibiotics
true (recovery depends on antibody production)
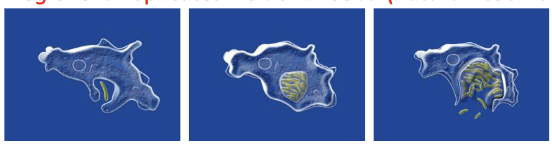
Streptococcus pneumoniae: multiplication
facultative anaerobe, grows extracellularly
capsule allows it to resist phagocytosis by macrophages
Streptococcus pneumoniae: damage (direct)
pneumolysin (pore-forming toxin, virulence factor)
Streptococcus pneumoniae: damage (indirect)
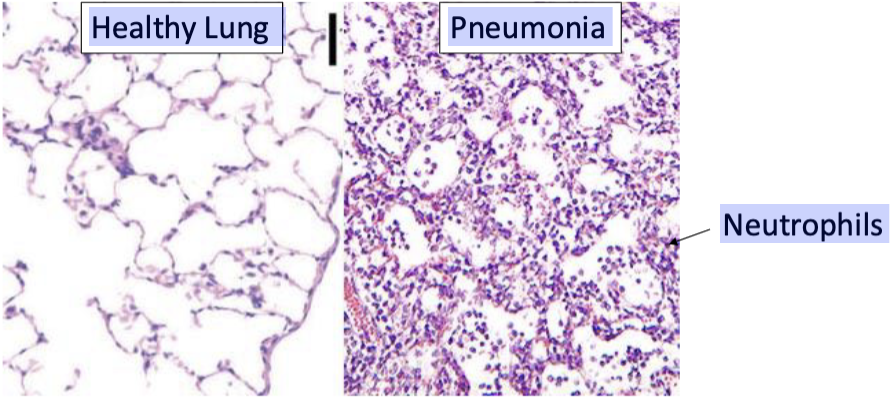
influx of neutrophils (PMNs) -> acute inflammation, tissue damage, fluids in the lung
how does S. pneumoniae cause lung damage?
1. Bacteria get into alveoli -> immune system is activated
2. Neutrophils come in to battle bacteria
3. Cytokines are released (fever, chills, fatigue)
4. Neutrophils, bacteria, exudate, fluid fill the alveoli (poor gas exchange, hard to breathe)
what type of bacteria is Legionella pneumophila?
gram (-) bacillus
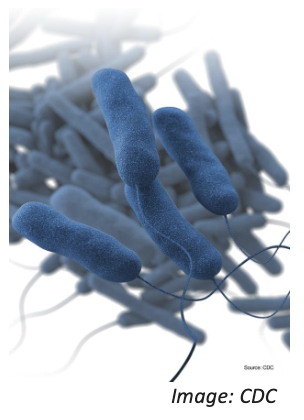
Legionella pneumophila: encounter
environment
• Lakes, streams, ponds
• Plumbing systems: air conditioning units, hot tubs, hot
water tanks and heaters, dental-unit water systems
Legionella pneumophila: entry
mist inhalation, water aspiration
Legionella replicates inside what?
amoebas (natural reservoir)
what disease does Legionella pneumophila cause?
pneumonia (Legionnaire’s disease, Pontiac fever)
Legionella pneumophila: spread
no human-human transmission (humans are dead-end hosts
Legionella pneumophila: multiplication
aerobe, grows intracellularly
No capsule to prevent phagocytosis, so:
The organism is taken up by macrophages but not killed
Legionella grows inside macrophages
Legionella pneumophila: damage is due to?
host inflammatory response
Legionella pneumophila can be found in all of the following EXCEPT one. Which is the EXCEPTION?
A. Air conditioning systems
B. Dental unit water lines
C. Hot tubs
D. Lakes and ponds
E. Healthy human microbiota
E. Healthy human microbiota
what type of bacteria is Pseudomonas aeruginosa?
gram (-) bacillus

Pseudomonas aeruginosa: encounter
• Environment: aquatic reservoirs, cockroaches
• Hospitals, homes
• Person-to-person
Pseudomonas aeruginosa: multiplication
• Facultative anaerobe
• Needs iron
• Biofilms
Pseudomonas aeruginosa: damage is caused by?
• Many extracellular toxins
• Cell lysis (to acquire iron)
Pseudomonas aeruginosa: outcome
• Antibiotic resistance is a problem
• Combination antibiotics are used in treatment
how does Pseudomonas aeruginosa affect healthy, immunocomptenet people?
no or mild disease
– Ears, eyes: contaminated water, contact lens solutions
– Skin: “hot tub rash
how does Pseudomonas aeruginosa affect immunocompromised people?
serious disease
– Cystic fibrosis patients (CF = poor lung function due to thick mucus)
– Patients on ventilators, with catheters, wounds from surgery or burns (nosocomial infections)
what is an opportunistic pathogen?
a microorganism that is normally harmless but can cause disease in people with weakened immune systems
eg. Pseudomonas aeruginosa
TRUE or FALSE?
A. Legionella pneumophila is a frequent cause of pneumonia acquired in nosocomial (hospital) settings.
B. Lung damage during pneumonia is caused both directly by the infectious organism and by the host response to infection.
C. Pseudomonas aeruginosa infections are acquired only from the environment and cannot be transmitted person-to-person.
D. Streptococcus pneumoniae can be transmitted on fomites
F
T
F
T
All of the following are risk factors that increase susceptibility to the disease pneumonia EXCEPT one. Which is the EXCEPTION?
A. Smoking
B. Undergoing chemotherapy
C. Having the disease cystic fibrosis
D. Working at a hospital
D. Working at a hospital
Streptococcus pneumoniae, Legionella pneumophila, Pseudomonas aeruginosa are all examples of…?
acute pneumonia
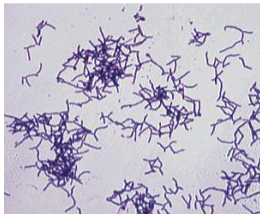
what type of bacteria is Pulmonary Actinomycosis?
gram (+) bacilli) of actinomyces species
Pulmonary Actinomycosis: enounter
• Oral and gut microbiota
• Associated with periodontitis and caries
Pulmonary Actinomycosis: entry
• Aspiration from oropharynx
Pulmonary Actinomycosis: disease
A rare infection of the lung
Pulmonary Actinomycosis: risk factors
Poor dental hygiene
dental abscess
weak immune system
alcohol abuse
emphysema
All of the following are risk factors for the development of pulmonary actinomycosis EXCEPT one. Which is the EXCEPTION?
A. Alcohol abuse
B. Dental abscess
C. Use of broad-spectrum antibiotics
D. Poor dental hygiene
C. Use of broad-spectrum antibiotics
Airborne microorganisms can cause
respiratory diseases
t/f: Although topologically open, the respiratory system is well protected
true
Bacteria have mechanisms to counteract host defenses such as
– capsule, growth within macrophages, attachment factors
– toxins
what makes something a risk factor for respiratory diseae?
Anything that impairs the defenses of the respiratory tract