Glomerular Filtration and Clearance, pt. 2
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
What are the 3 essential functions of the kidneys?
-filtration to remove metabolic products & toxins from the blood & excreting them thru urine
-regulate body fluids, electrolyte balance, & acid-base balance
-produce or activate hormones that are involved in erythrogenesis, Ca2+ metabolism, & regulation of blood pressure & blood flow
Which component of the renal microvasculature controls resistance?
afferent & efferent arterioles
What are the 2 features of renal microvasculature?
-2 major sites of resistance control = afferent & efferent arterioles
-2 capillary beds in series = glomerulus & peritubular capillaries
True or False: The glomerular capillary pressure is relatively high throughout
True
True or False: The peritubular capillary pressure is relatively high throughout
False ==> peritubular capillary pressure is relatively low
How is the hydrostatic pressure of the glomerular capillary controlled?
via constriction or relaxation of the afferent & efferent arterioles
-constriction of afferent + relaxation of efferent = decreased GC hydrostatic pressure
-constriction of efferent + relaxation of afferent = increased GC hydrostatic pressure
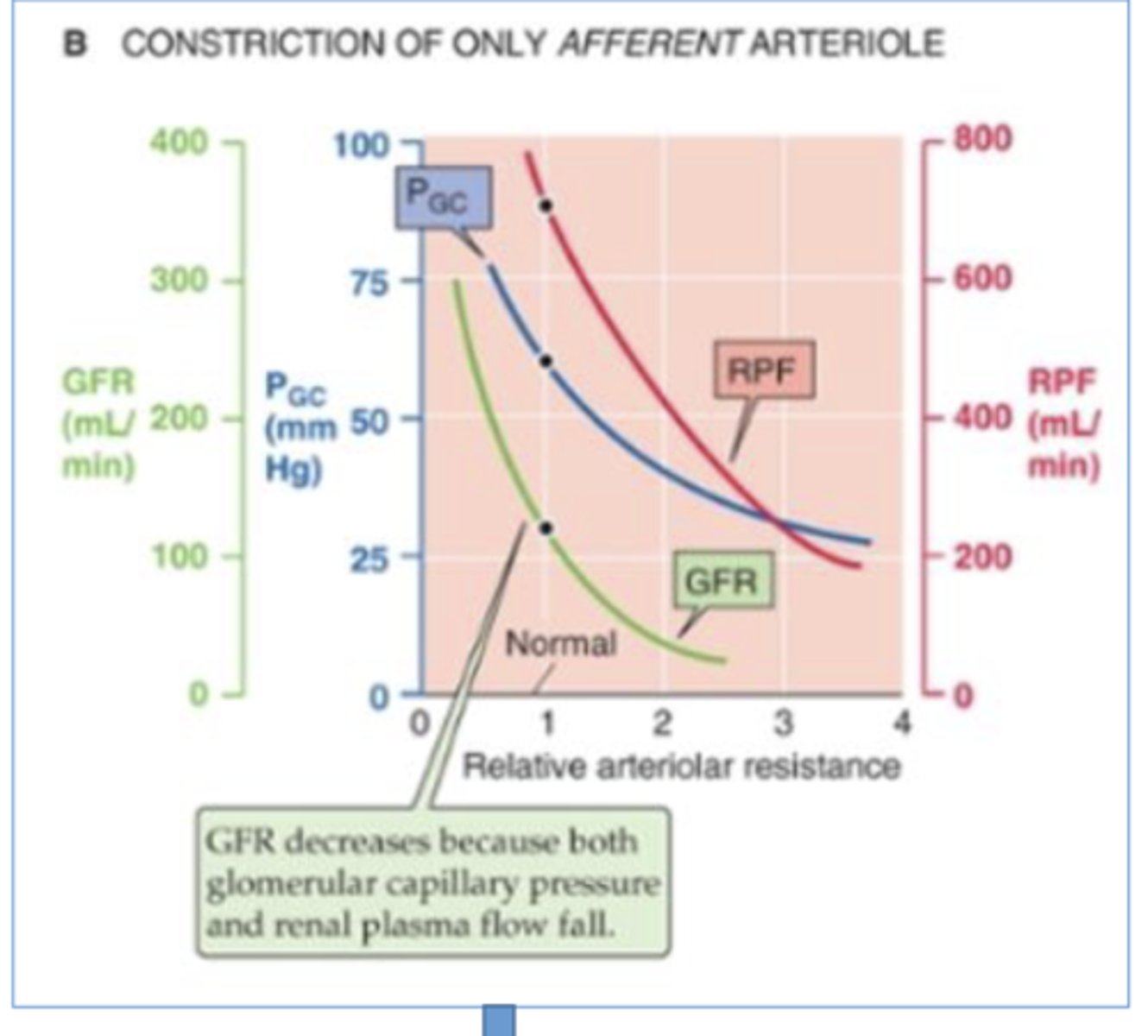
What effect does vasoconstriction of the afferent arteriole have on the renal plasma flow?
decreases RPF ==> less blood entering kidneys, so less plasma flowing thru
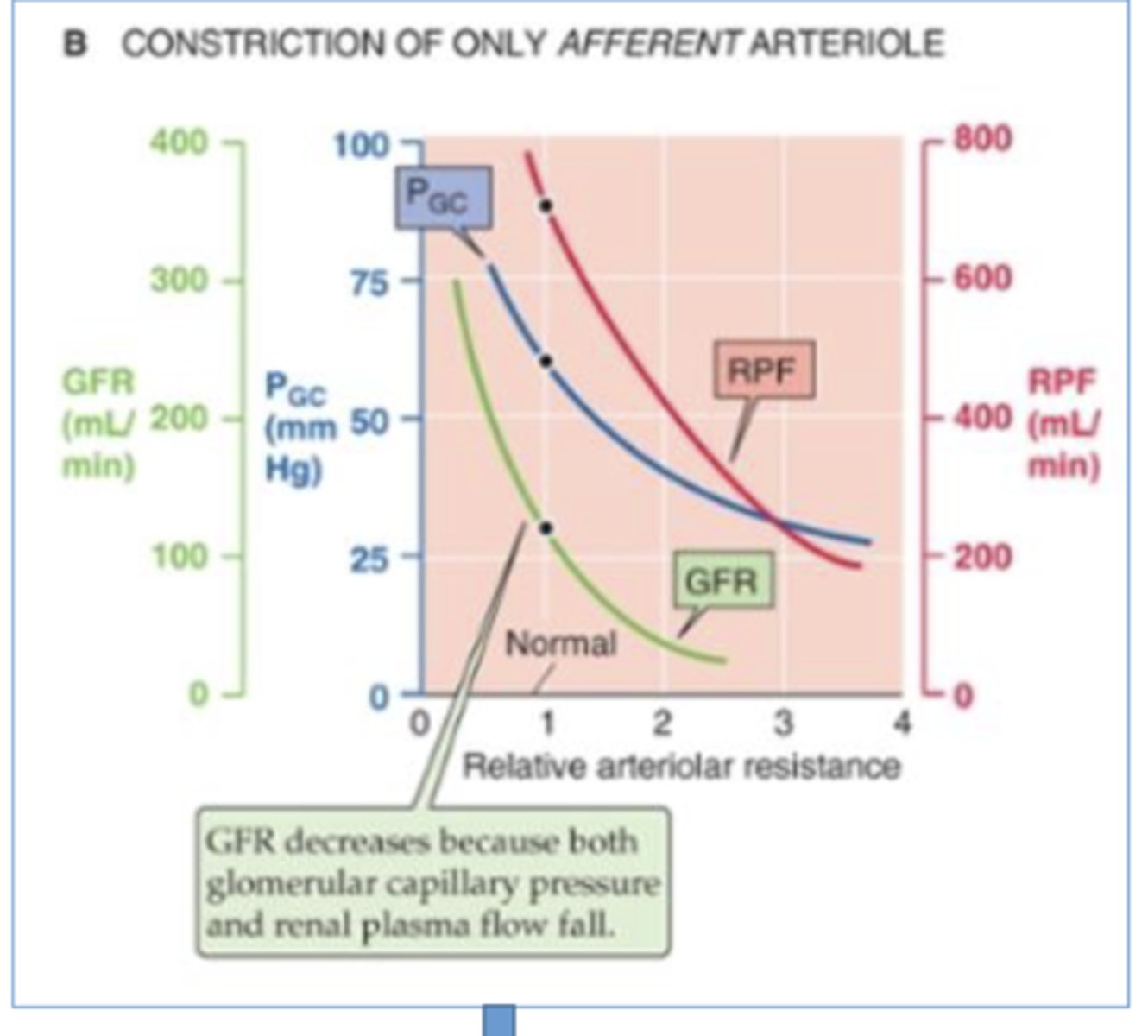
What effect does vasoconstriction of the afferent arteriole have on the hydrostatic pressure of the glomerular capillary?
decreases ==> less blood entering glom, so less hydrostatic pressure
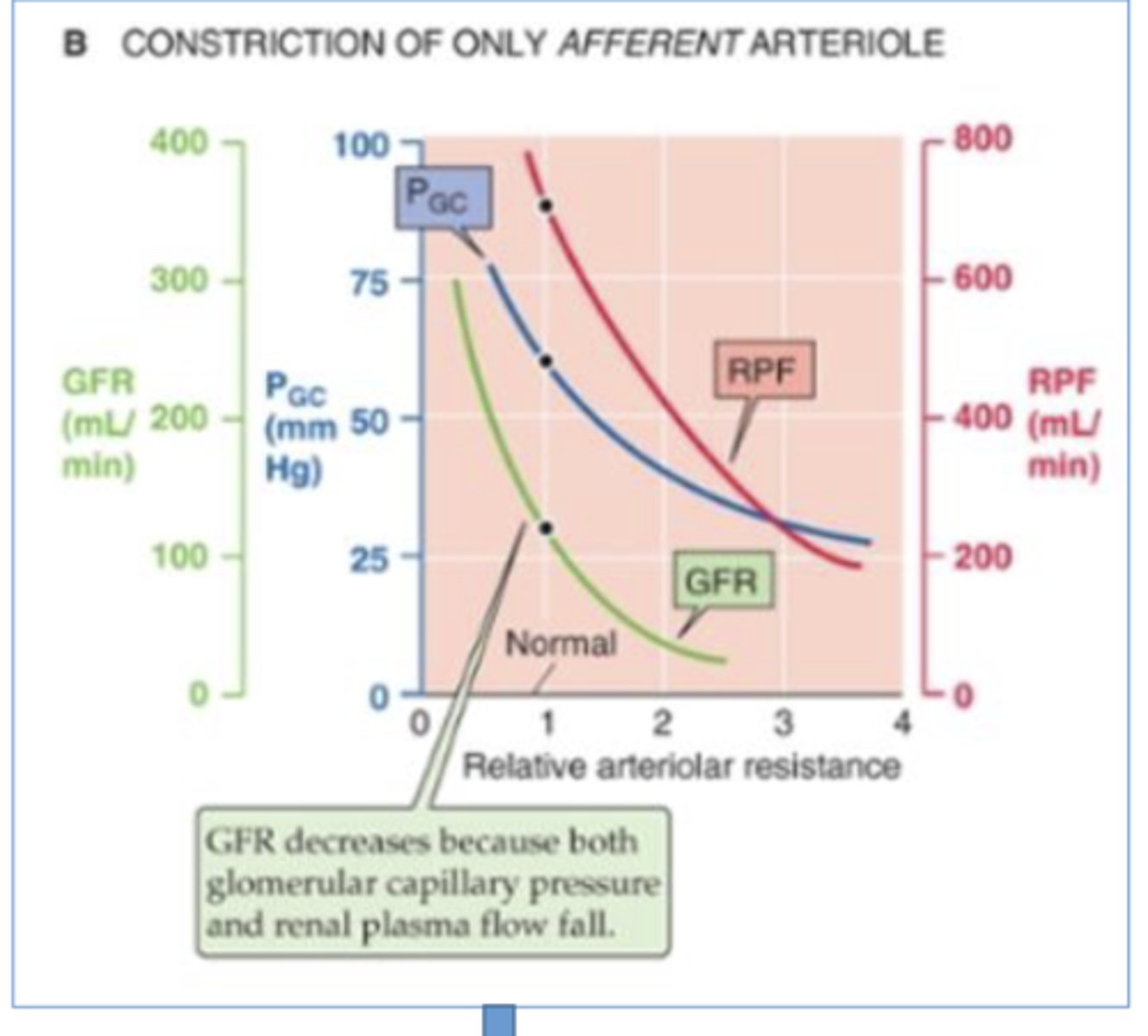
What effect does vasoconstriction of the afferent arteriole have on the glomerular filtration rate?
decreases ==> less blood entering at a time, so less blood filtration at a time
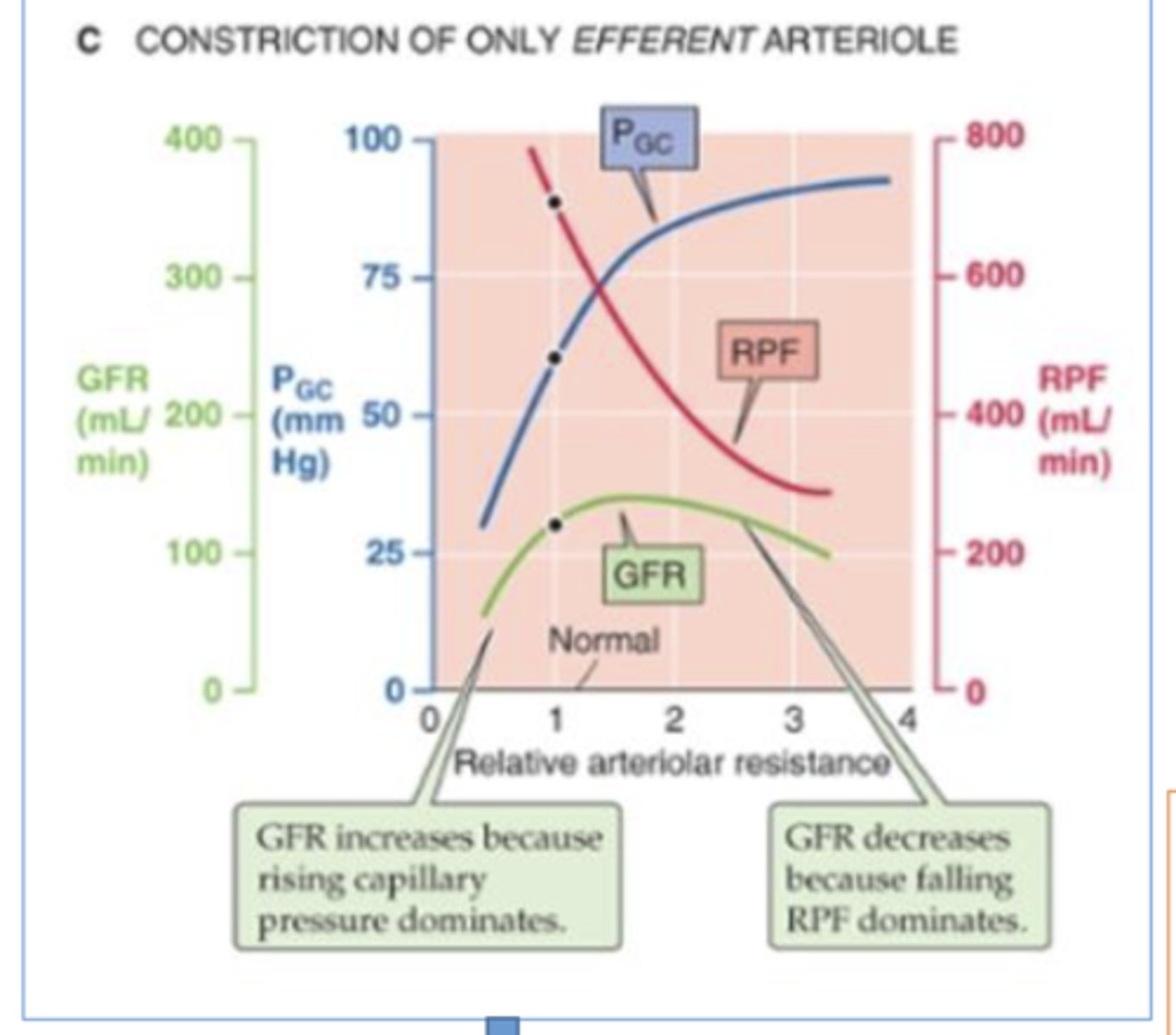
What effect does vasoconstriction of the efferent arteriole have on glomerular filtration rate?
biphasic effect on GFR w/ increased efferent resistance
-initial increase in GFR --> due to increased hydrostatic pressure in glomerulus (back up cuz it can't flow into narrow efferent arteriole as quickly)
-later decrease in GFR --> due to decrease in renal plasma flow (back up stops more blood from afferent arteriole from entering glom)
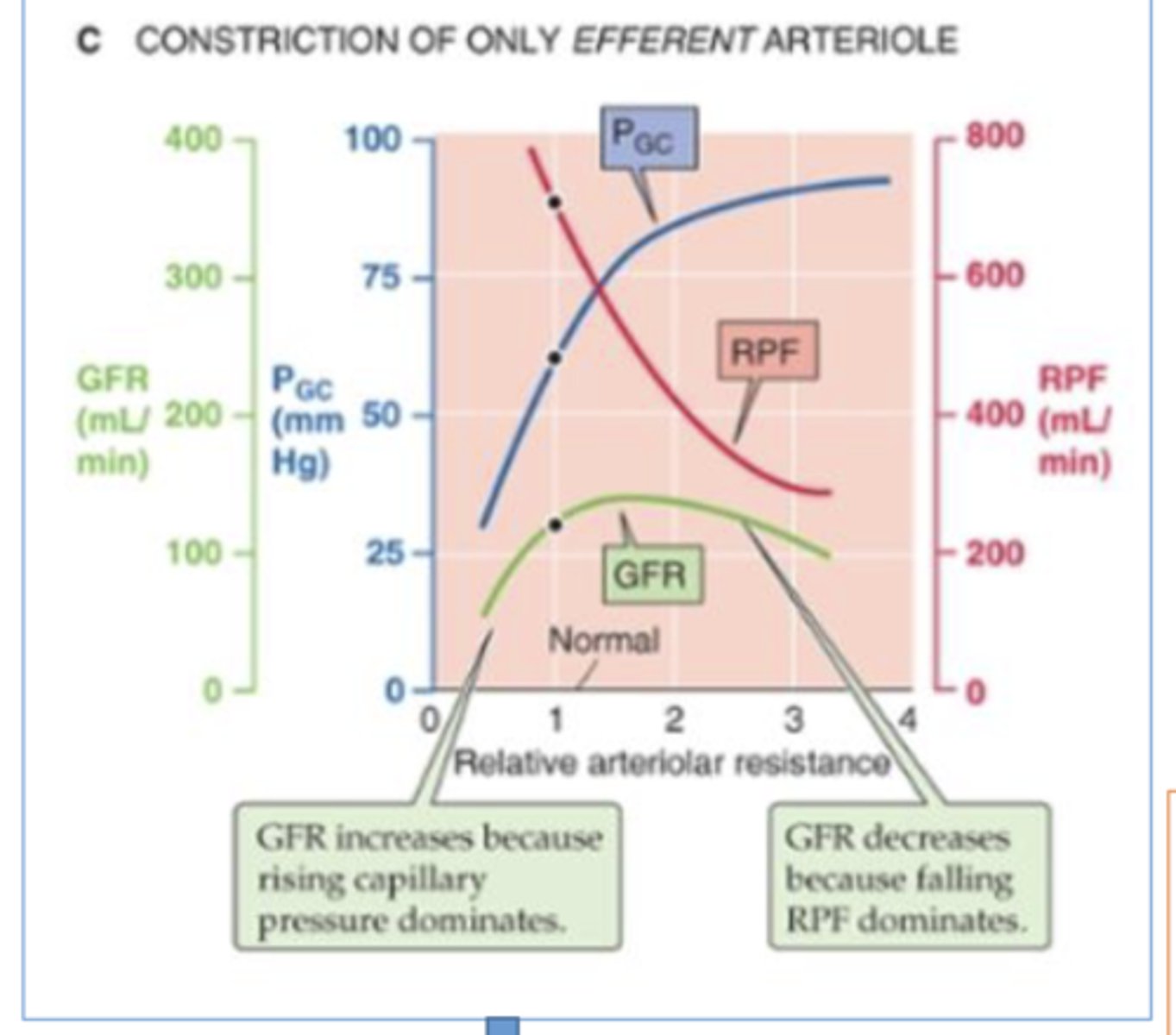
What effect does vasconstriction of the efferent arteriole have on the hydrostatic pressure of the glomerulus?
increases ==> build up of blood in the glomerulus b/c narrow opening of efferent arteriole (narrow exit)
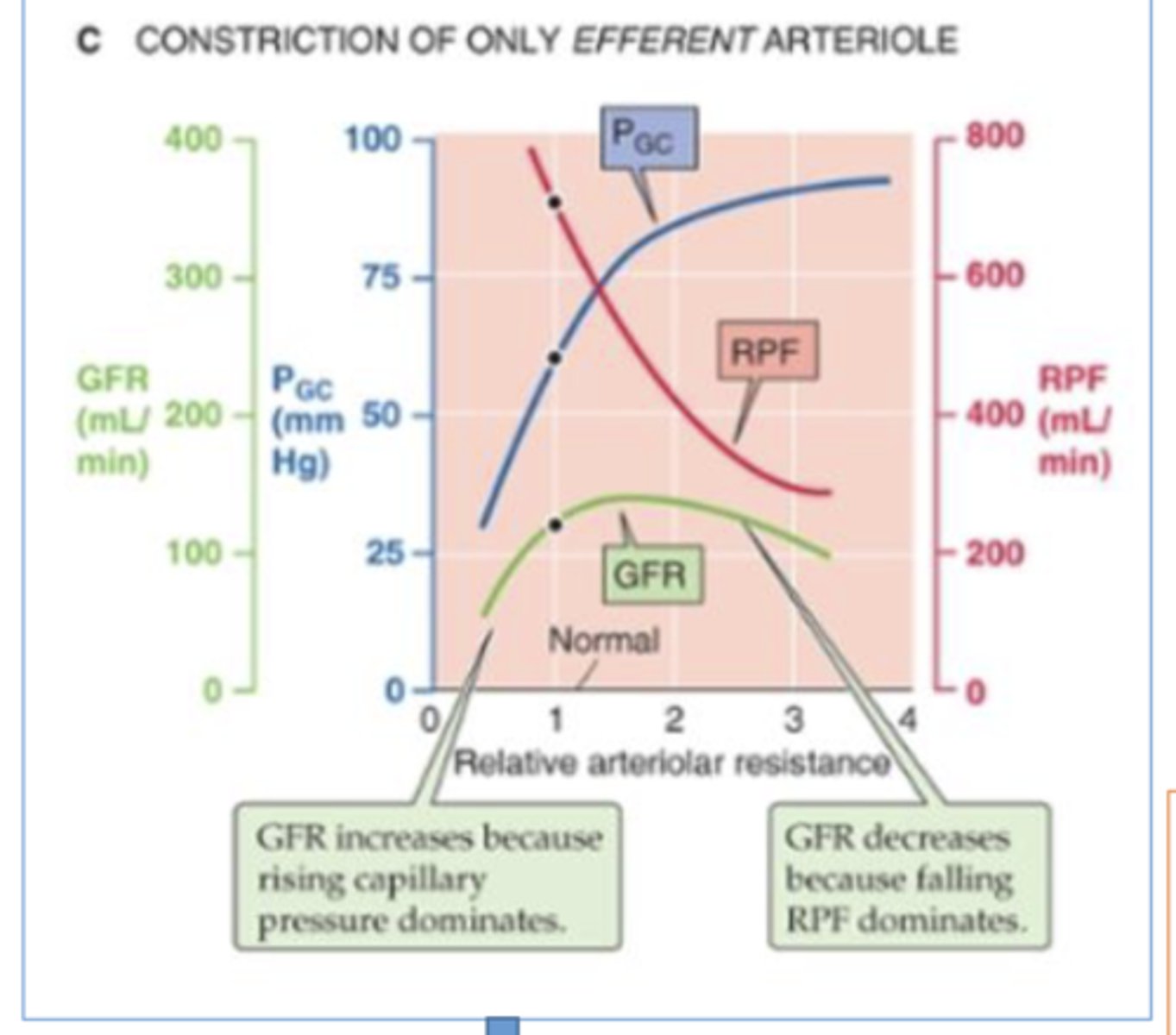
what effect does vasoconstriction of the efferent arteriole have on the renal plasma flow (RPF)?
decreases ==> less blood can flow into kidneys b/c narrow arteriole opening
After nephrectomy in a kidney donor, how is the remaining kidney able to maintain healthy blood filtration (how is it able to still filter the blood enough that the person doesn't die)?
When there's a large increase in renal plasma flow following the loss of renal tissue (like in the case where a kidney is missing so all the blood has to flow to one kidney), the afferent arteriole of remaining kidney dramatically vasodilates to decrease resistance --> increases RPF & GFR enough to sustain life
What is the effect of increased vasodilation of the efferent arteriole?
-significant decrease in GFR --> blood has bigger exit via wide arteriole so it leaves glomerulus quicker
-decreases BP
Angiotensin II inhibitors predominately effects the afferent or efferent arteriole? How is this renal microvessel affected, & how does this effect GFR?
ANGII inhibitors predominately effect efferent arterioles ==> cause vasodilation of efferent arteriole --> significant decrease in GFR (blood has bigger exit via wide arteriole so it leaves glomerulus quicker)
*also decreases BP
Do you expect high or low oncotic pressure in the peritubular capillaries to favor reabsorption?
high (increased) oncotic pressure in peritubular capillaries will favor reabsorption ==> allows more solutes/substances to enter because via being carried by fluid (water wants to flow into highly conc. capillaries and solutes are carried in by water)
Do you expect high or low hydrostatic pressure in the peritubular capillaries to favor reabsorption?
low (decreased) hydrostatic pressure in peritubular capillaries will favor reabsorption ==> allows fluid to enter into capillaries (along with the solutes it's carrying)
True or False: Vasoconstriction of the efferent arteriole promotes reabsorption in the peritubular capillaries.
True ==> allows for increased oncotic pressure & decreased hydrostatic pressure in peritubular capillaries
Why is p-aminohippurate (PAH) a good measure of renal plasma flow (RPF)?
b/c kidneys almost completely clear blood of PAH in a single pass so it's a good measure of RPF ==> filtered in glomerulus & isn't reabsorbed
PAH clearance = RPF
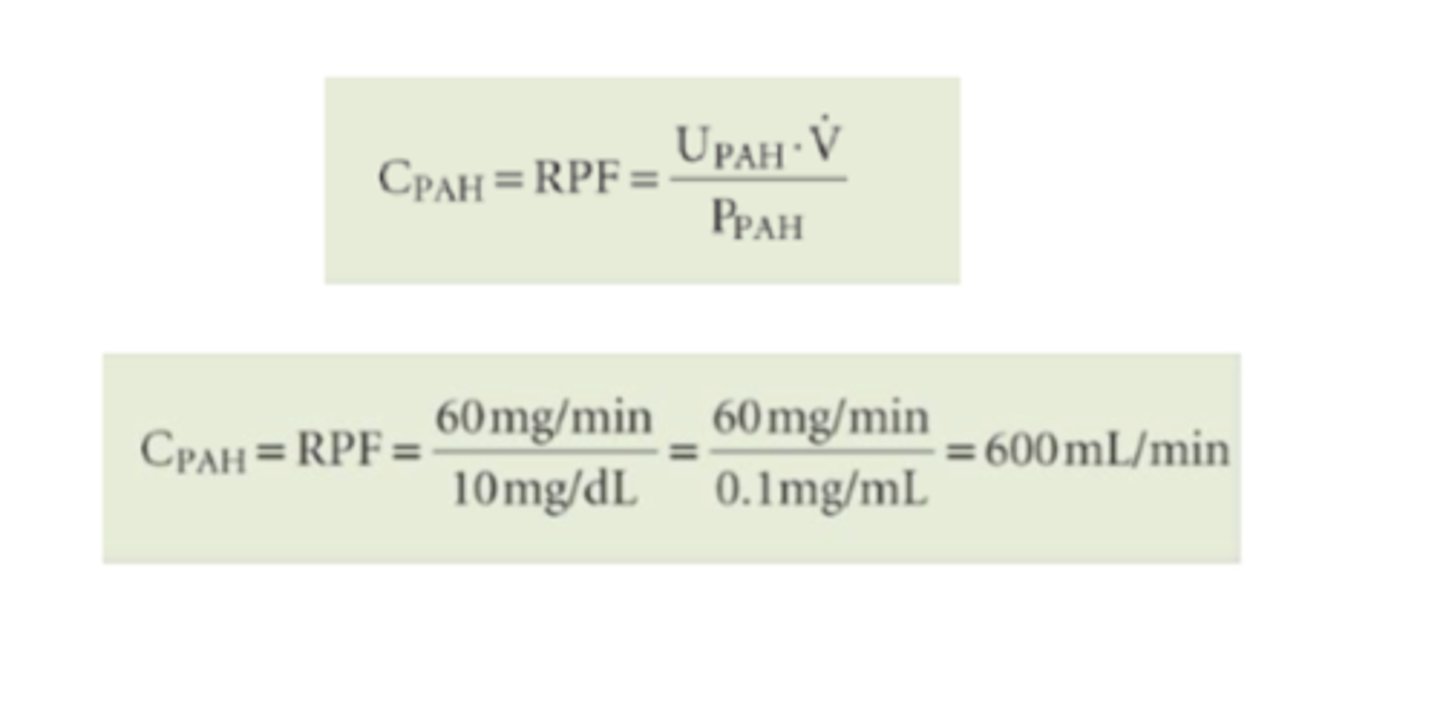
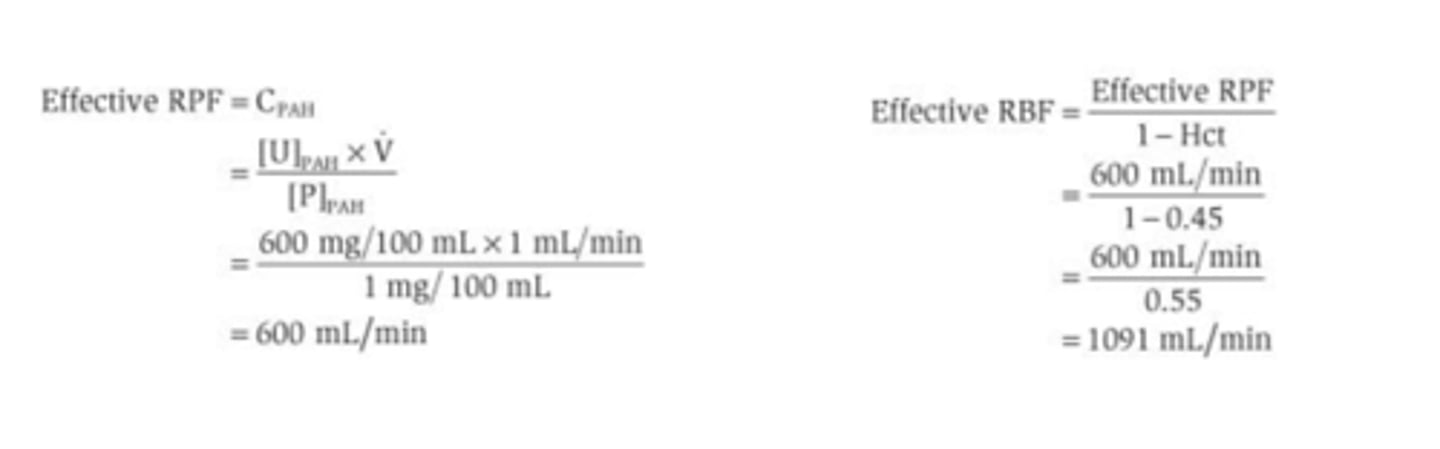
A man with a urine flow of 1 mL/min has a plasma concentration of PAH of 1mg%, a urine concentration of PAH of 600mg%, and a hematocrit of 0.45. What is his RBF (Renal Blood Flow)?
-step1: Since we weren't given values for the renal artery & renal vein concentrations of PAH, calculate clearance of PAH = RPF
-step2: calculate effective RBF using the hematocrit
-remember mg% = mg/100mL
What keeps renal blood flow and GFR relatively constant?
-myogenic control ==> opening of stretch-activated cation channels in vascular smooth muscle of afferent arterioles
-tubuloglomerular feedback = juxtaglomerular apparatus ==> macula densa cells sense an increase in GFR --> stimulate afferent arteriole to contract --> decrease in RPF & hydrostatic pressure --> decrease in GFR
Where does the autoregulatory response occur?
afferent arteriole
Describe Renal Autoregulation via Myogenic Response
opening of stretch-activated cation channels in vascular smooth muscle of afferent arterioles
*the afferent arterioles have the ability to respond to changes in vessel circumference by contracting or relaxing smooth muscle
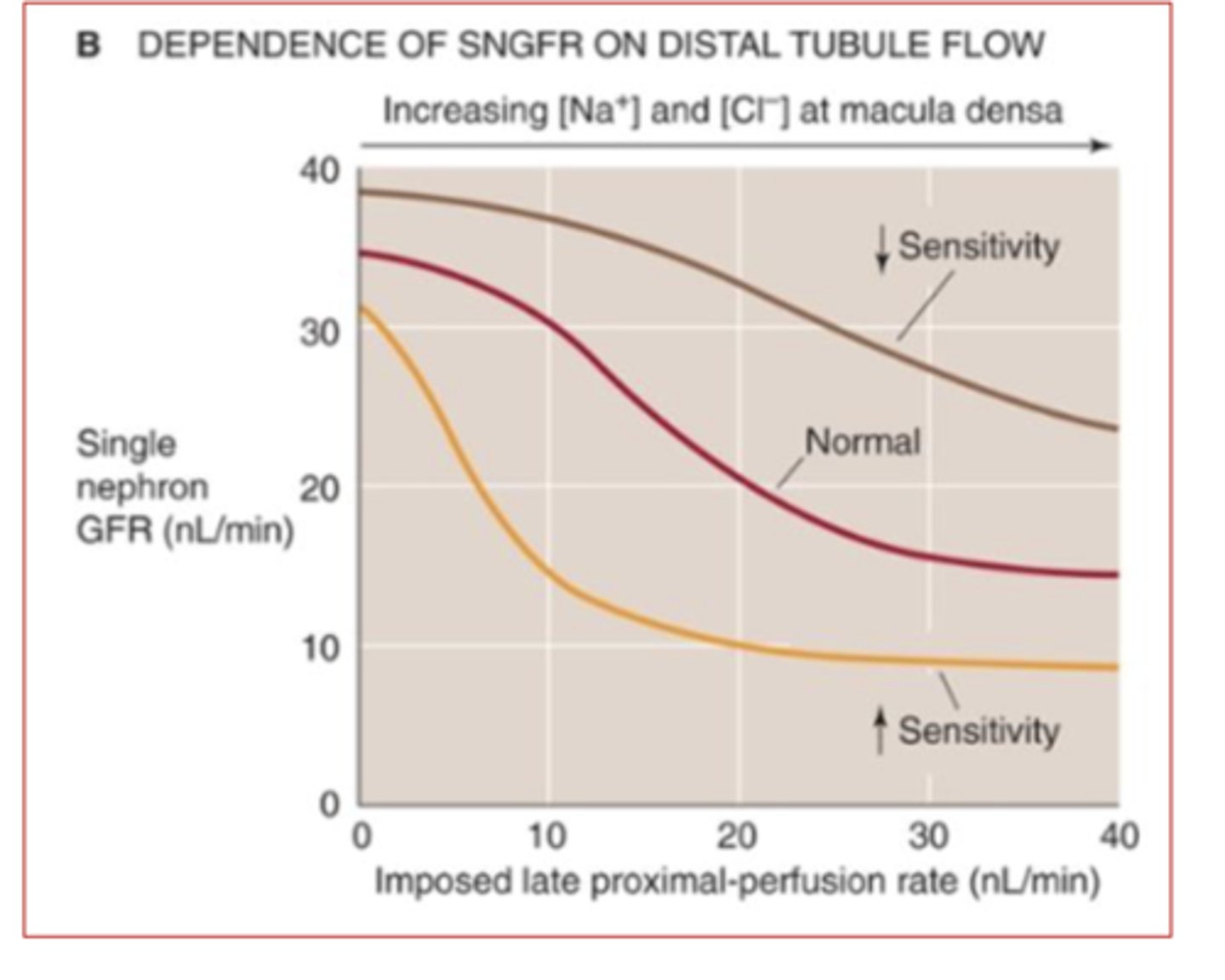
Describe the mechanism of tubuloglomerular renal autoregulation
-increase in afferent arteriole pressure --> increases GFR --> decreases conc of Na+ & Cl- --> detected by macula densa--> increases afferent arteriole vasoconstriction --> decreases GFR
-decrease in afferent arteriole pressure --> decreases GFR --> decreases --> Na+ & Cl- --> detected by macula densa --> decreases afferent arteriole vasoconstriction (increases vasodilation) --> increases GFR
Would you expect the GFR to be increased or decreased if the macula densa has decreased sensitivity to Na+ and Cl- conc. in filtrate?
GFR will be increased ==> less sensitive macula densa won't detect high Na+ or Cl- --> won't stimulate vasoconstriction of afferent arteriole --> GFR will be abnormally increased
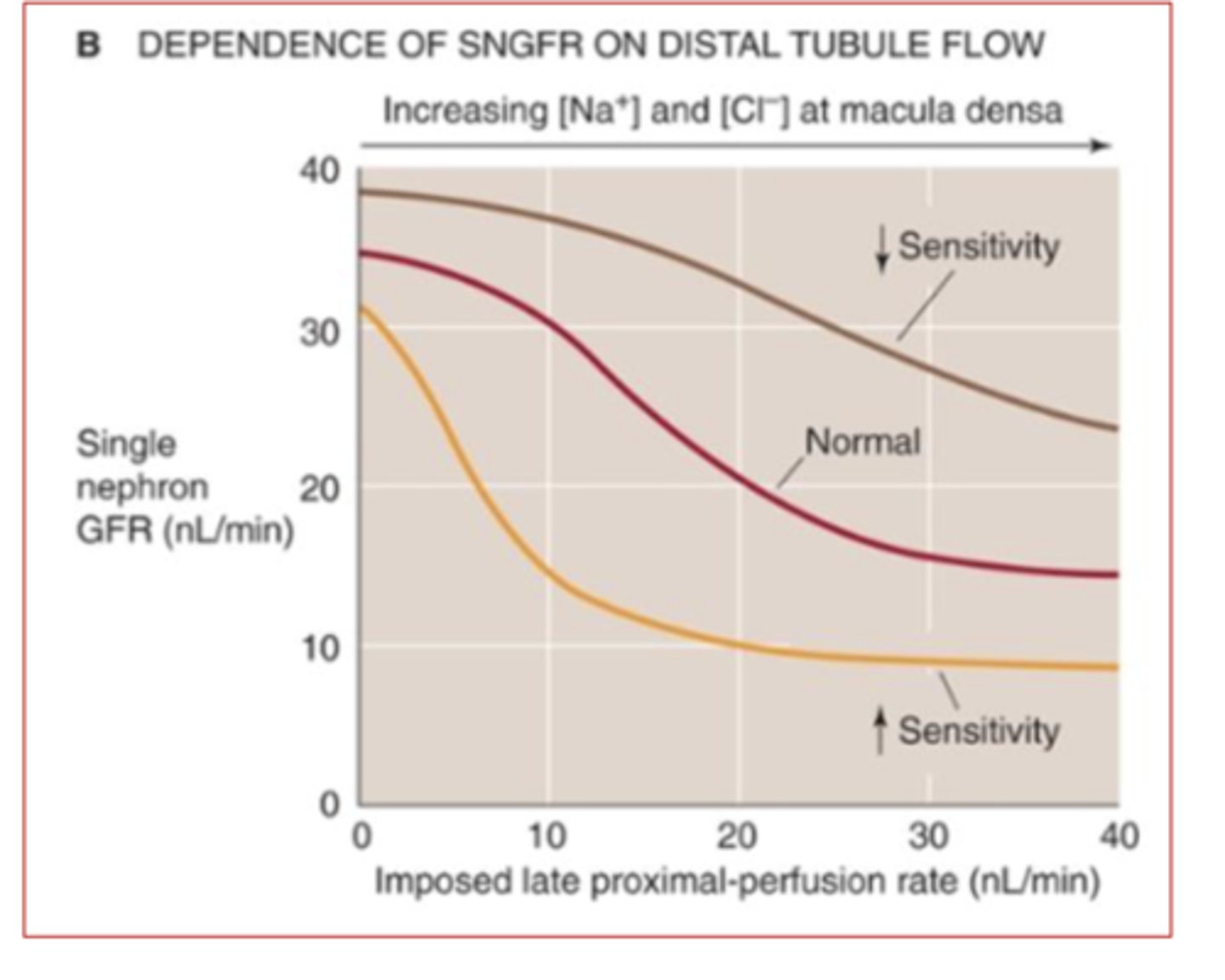
Would you expect the GFR to be increased or decreased if the macula densa has increased sensitivity to Na+ and Cl- conc. in filtrate?
GFR will be decreased ==> more sensitive macula densa will be stimulated by lower levels of Na+ & Cl- than it normally would --> stimulates vasoconstriction of afferent arteriole when it doesn't need to --> GFR will be abnormally increased
What four factors that modulate renal blood flow to regulate effective circulating volume?
-renin-angiotensin-aldosterone axis --> decrease urine to increase blood volume
-the sympathetic nervous system --> decrease urine to maintain preload for heart to power flight or fight
-arginine vasopressin (antidiuretic hormone) --> decrease urine
-atrial natriuretic peptide (ANP) --> increase urine (increased Na+ excretion in urine)
Where is angiotensinogen synthesized?
liver
where is renin synthesized?
synthesized & stored in juxtaglomerular apparatus
where is angiotensin-converting enzyme (ACE) synthesized?
lungs
What is function of aldosterone?
stimulates Na+ reabsorption by the cortical collecting tubules & medullary collecting ducts by increasing activity and number of Na+ channels on the apical tubular cells
*only 2 - 3% of the filtered Na+ load is controlled by aldosterone --> sustained loss of this would exceed the daily Na+ intake significantly
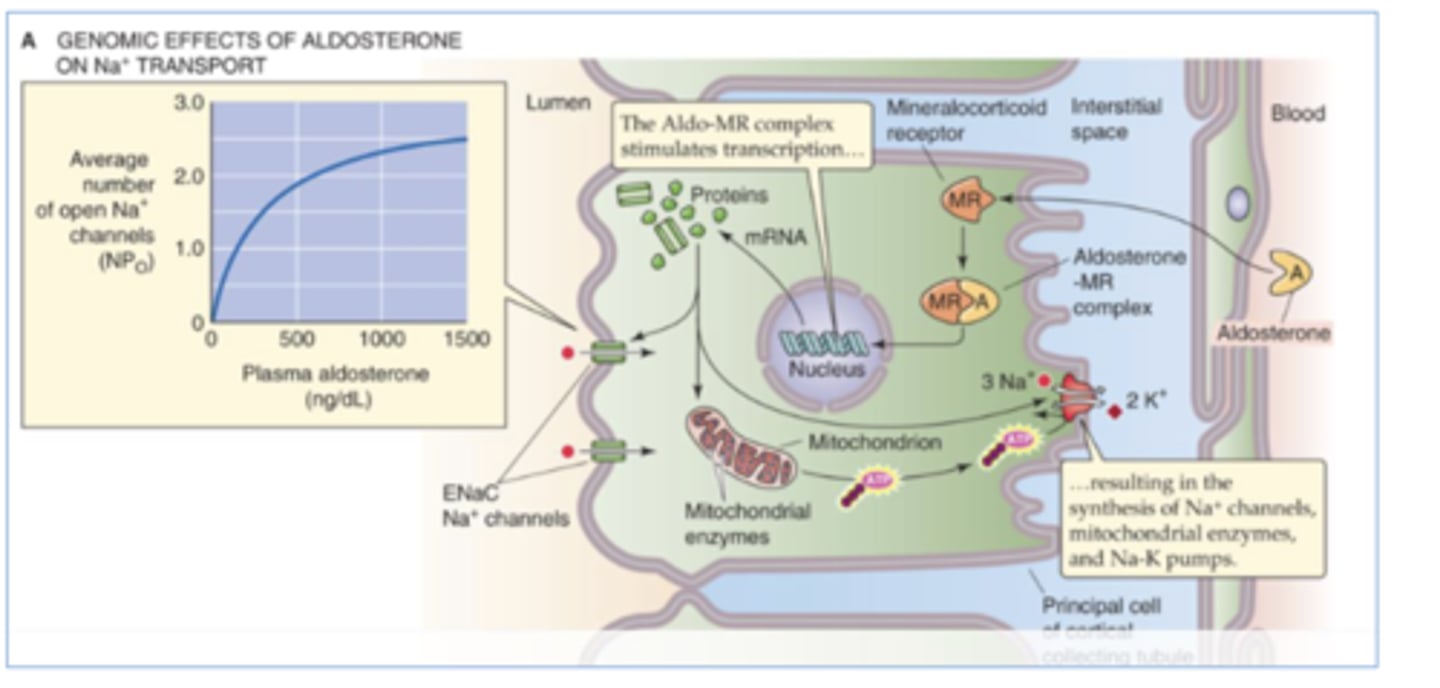
Addison's Disease
adrenal insufficiency that leads to lack of aldosterone--> severe Na+ depletion --> severely decreased ECF --> circulatory insufficiency
What are the functions of Angiotensin II?
-stimulation of aldosterone release from the adrenal cortex
-vasoconstriction of renal vessels
-enhanced tubuloglomerular feedback
-renal hypertrophy --> increase # of pores on cells to allow more entry of aldosterone
-stimulated thirst and AVP release
When does sympathetic tone to the kidney increase?
-general SNS response
-pain, stress, trauma, hemorrhage, or exercise
-selective renal response to decrease in effective circulating volume
*high SNS stimulation--> afferent & efferent arteriolar resistances increase --> decrease RBF & GFR
What effect does sympathetic stimulation have on GFR?
high SNS stimulation--> afferent & efferent arteriolar resistances increase --> decrease RBF & GFR
What effect does sympathetic stimulation have on RBF?
high SNS stimulation--> afferent & efferent arteriolar resistances increase --> decrease RBF & GFR
What effect does maximal SNS stimulation have on the kidneys?
afferent vasoconstriction predominates & leads to drastic reductions in both RBF and GFR
Arginine Vasopressin (AVP)/ Antidiuretic Hormone
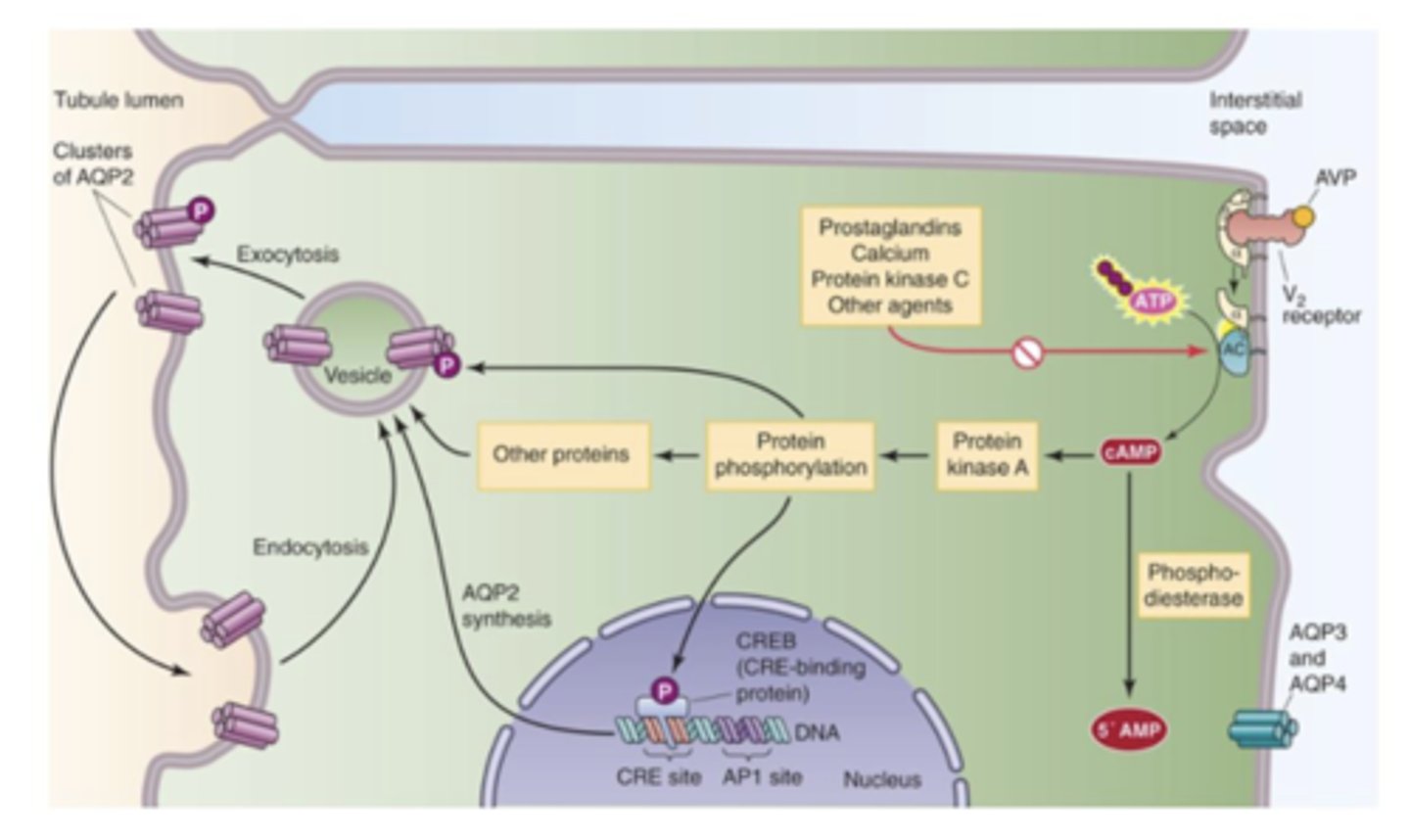
peptide hormone released by pituitary gland in response to increased osmotic pressure of extracellular fluid (triggered by osmoreceptors in the hypothalamus) --> inserts aquaporin channels to apical side of tubular cells of collecting duct--> increases water absorption in collecting ducts to decrease blood osmolarity
*may decrease blood flow to the renal medulla to minimize the washout of the hypertonic medulla ==> hypertonicity of renal medulla is essential for forming concentrated urine
What are some non-osmotic stimuli that modulate secretion of arginine vasopression/antidiuretic?
-reduced effective circulating volume (5-10% loss) --> ex: hemorrhagic shock & hypovolemic shock
-volume expansion--> chronic volume expansion reduces AVP by decreasing the sensitivity of the central osmoreceptors to changes in plasma osmolarity
-pregnancy --> increased blood volume to also circulate blood to the developing fetus
-pain --> stimulates AVP
-nausea --> stimulates AVP
-morphine, nicotine, & high doses of barbituates --> stimulates AVP
-Alcohol --> inhibit AVP secretion
-opiate-antagonists --> inhibit AVP secretion
True or False: Pain stimulates the secretion of vasopressin
True
True or False: Nausea inhibits the secretion of antidiuretic hormone.
False ==> stimulates ADH/AVP secretion
True or False: Morphine stimulates the secretion of arginine vasopressin.
True
What effect does nicotine have on water reabsorption?
increases water reabs ==> nicotine stimulates release of vasopressin/ADH
What effect does barbiturates have on water reabsorption?
increases water reabs ==> high doses of barbiturates stimulates release of vasopressin/ADH
What effect does alcohol have on water reabsorption?
decreases water reabs ==> inhibits secretion of vasopressin/ADH
What effect does opiate-antagonists have on water reabsorption?
decreases water reabs ==> inhibits secretion of vasopressin/ADH
atrial natriuretic peptide (ANP)
hormone released by atrial myocytes in response to increased atrial pressure/circulating volume ==> vasodilates afferent & efferent arterioles --> increases cortical & medullary blood flow & lowers sensitivity of the tubuloglomerular regulatory mechanism --> increases RPF & GFR
*also inhibits secretion of renin & vassopressin/ADH
What are the 4 local vasoactive agents that modulate RBF & GFR?
-dopamine --> vasodilates (opp of epi & norepi)
-prostaglandins --> local vasodilator that provides a buffer against excessive vasoconstriction esp during increased SNS to the kidney or activation of renin-angiotensin system
-nitric oxide --> strong vasodilator
-leukotrienes --> cause local strong vasoconstriction to reduce RBF & GFR
What effect can NSAIDS have on GFR?
-decreases prostaglandins--> decreased glomerulus vasodilation--> decreased GFR
-decreases leukotrienes --> decreases vasoconstriction --> increases RBF & GFR
*NSAIDS can potentially disrupt renal fxn