EMT Chapter 10 Airway management, Artificial Ventilation, and Oxygenation
1/127
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
128 Terms
Respiration
The gas exchange process that occurs between the alveoli or cells and the capillaries
Four distinct components of respiration
1) pulmonary ventilation
2) external respiration
3) internal respiration
4) cellular respiration and metabolism
Pulmonary ventilation
the mechanical process of moving air in and out of the lungs
External respiration
the gas exchange process that occurs between the alveoli and the surrounding pulmonary capillaries; serves to oxygenate the blood and eliminate carbon dioxide in the lungs
Internal respiration
cell/capillary gas exchange; is responsible for delivering oxygen to the cells and removing carbon dioxide from the cell
Cellular respiration and metabolism
Breaks down glucose in the presence of oxygen, produces high amounts of energy in the form of ATP, and releases carbon dioxide and water as a by-product
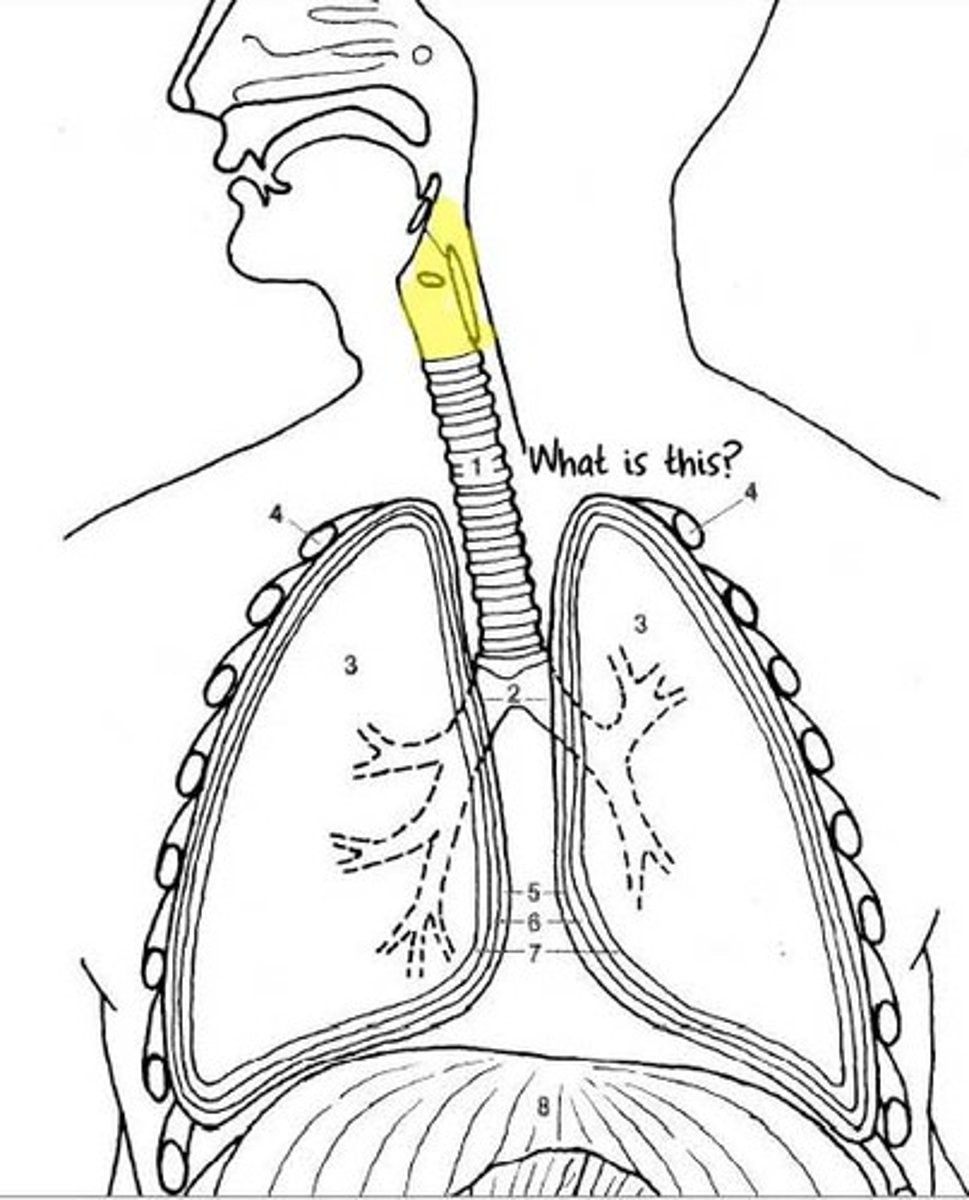
The upper airway
Nasal cavity, Nasopharynx, Oropharynx, Hypopharynx (laryngopharynx), epiglottis, esophagus, trachea, and larynx
Pharynx
Throat
Nasopharynx
Where air from the nasal passages enter
Oropharynx
Where air from the mouth travels to get to the lungs
Importance of keeping a clear pharynx
Obstructions can prevent air from traveling into the lower airways or the substance may be aspirated into the lungs.
The two passageways found at the lower end of the pharynx
The trachea and the esophagus
Larynx
Above the trachea and below the epiglottis; the voice box
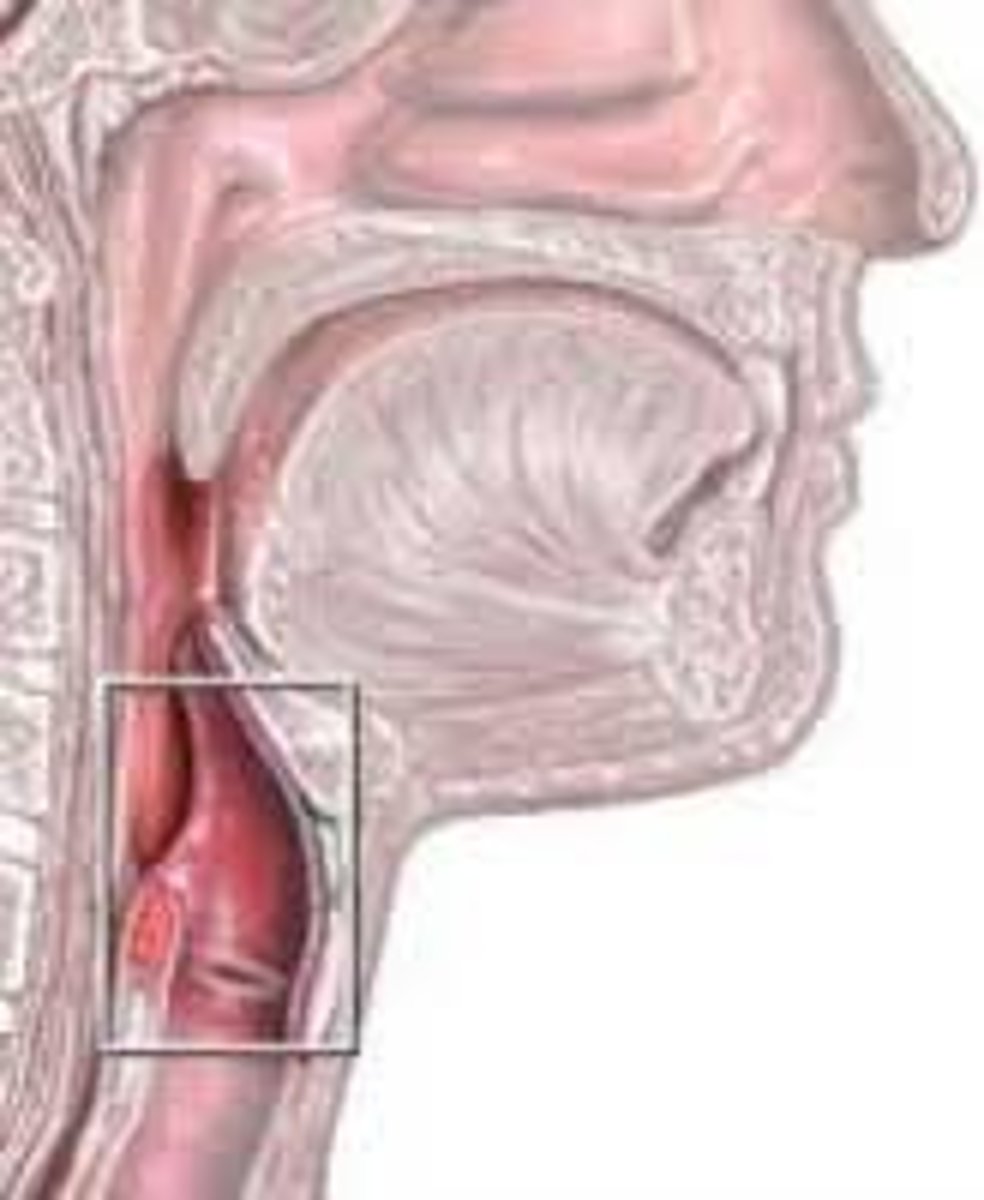
Thyroid cartilage
the anterior portion of the larynx; the adams apple
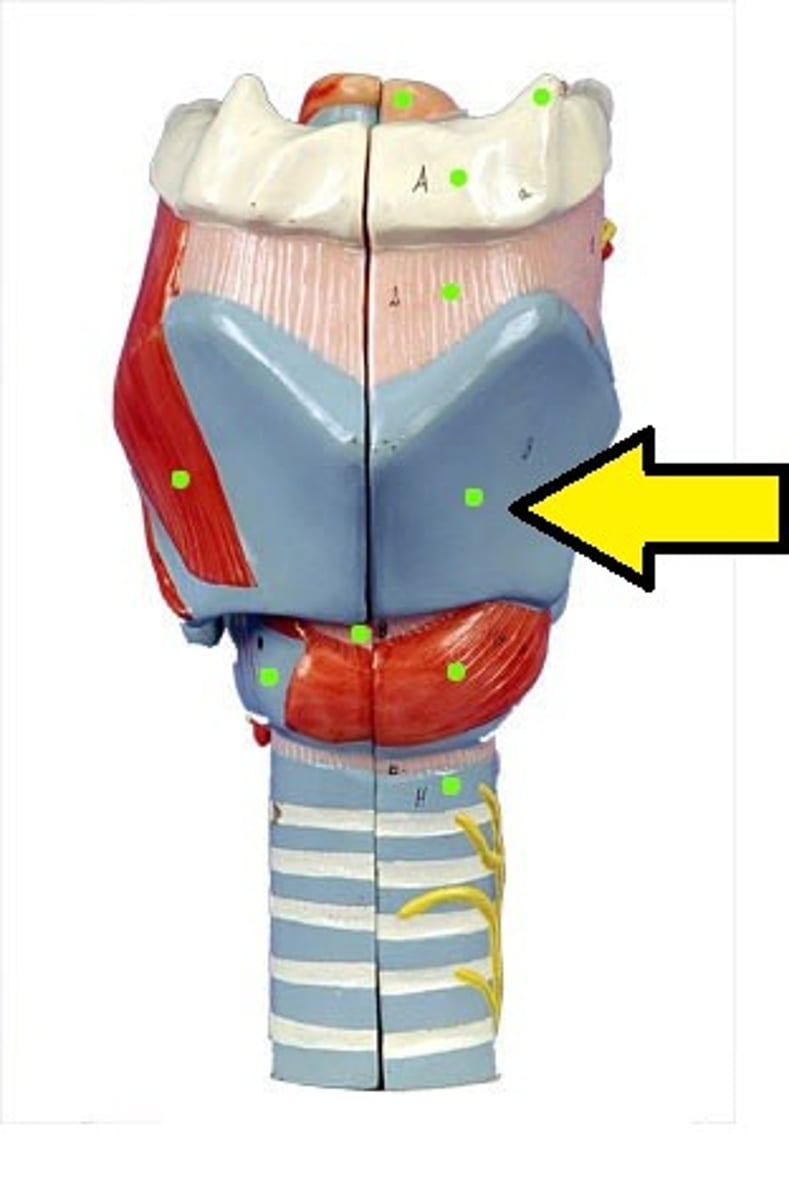
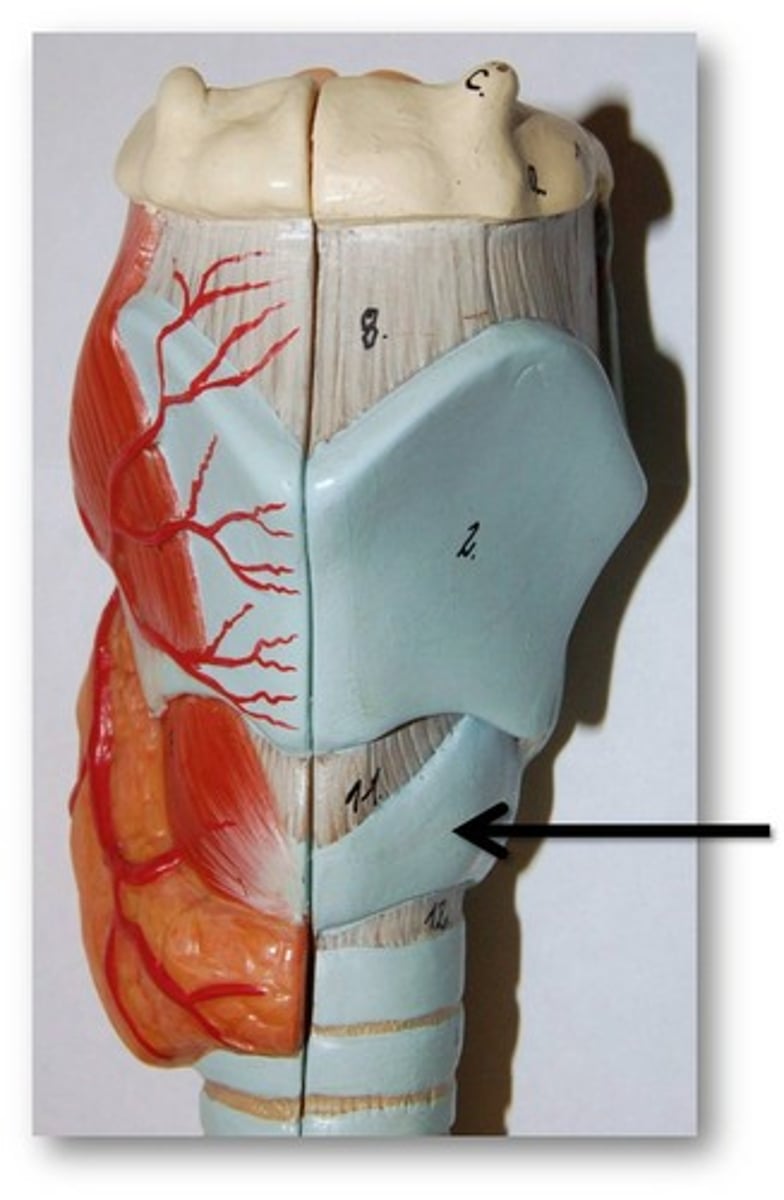
Cricoid cartilage
the inferior portion of the larynx; the only completely circular cartilaginous ring of the upper airway
The lower airway
From the cricoid cartilage to the alveoli
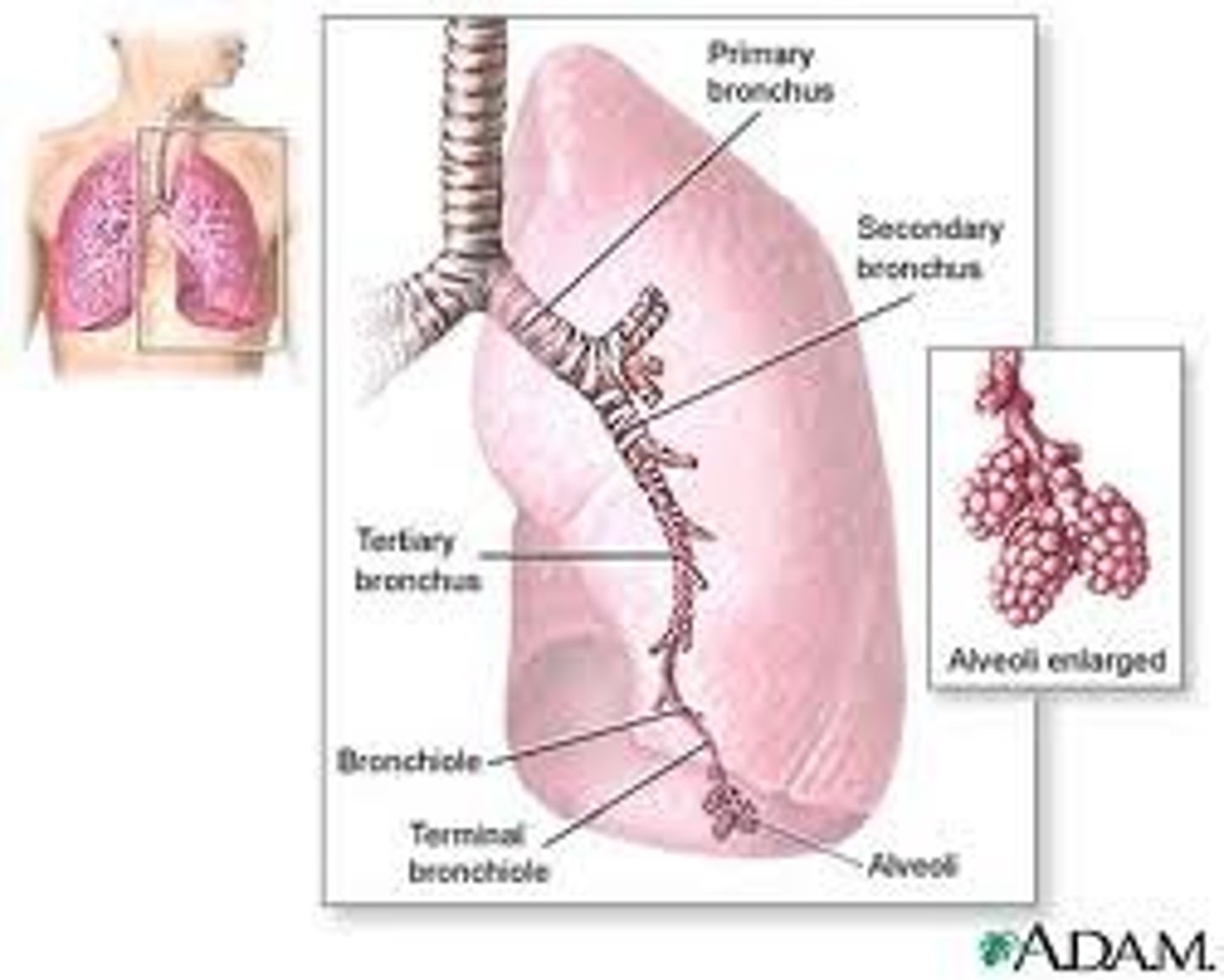
Trachea
The windpipe; the passageway for air entering the lungs
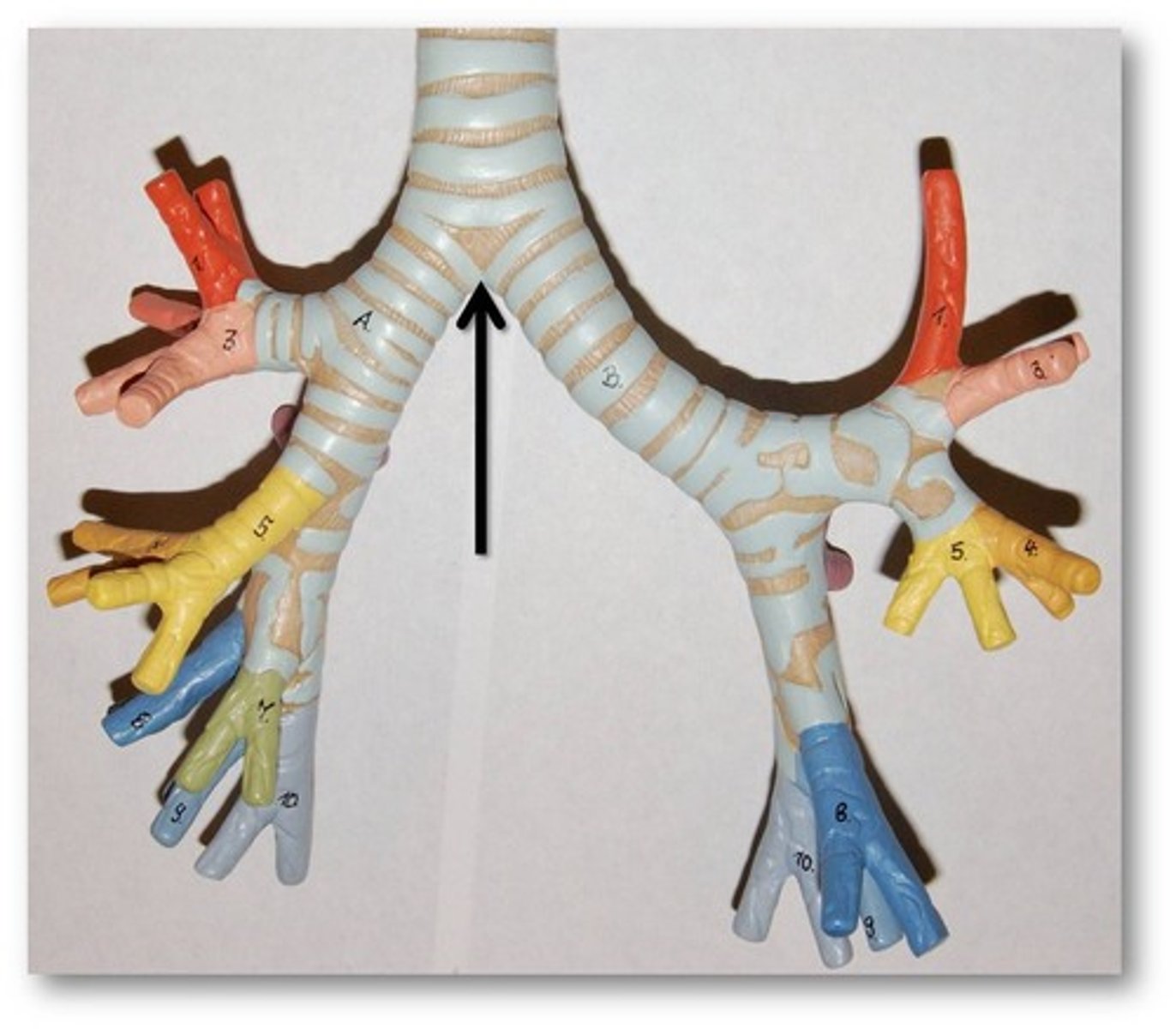
The carina
the point at which the trachea splits into the right and left main stem bronchi
The anterior portion of the trachea
composed of strong C-shaped cartilaginous rings that provide support and structure
The posterior wall of the trachea
Made up of muscle and is not a rigid structure
Bronchi
the two major branches of the trachea; extends from the carina into the lungs
Bronchioles
Smaller sections of the bronchi; lined with smooth muscle and mucous membranes
When the mucous lining of the bronchioles becomes inflamed and swollen
Severely narrows the diameter of the bronchiole and causes lower airway obstruction (as seen in asthma). The narrowing causes an increase in airway resistance inside the bronchiole, which makes it difficult to move air
An increase in airway resistance
Causes the patient to work harder to breathe which may lead to fatigue and failure of the respiratory muscles
Leads to cell hypoxia
ineffective and inadequate ventilation and oxygenation
Alveoli
Tiny air sacs in the lungs
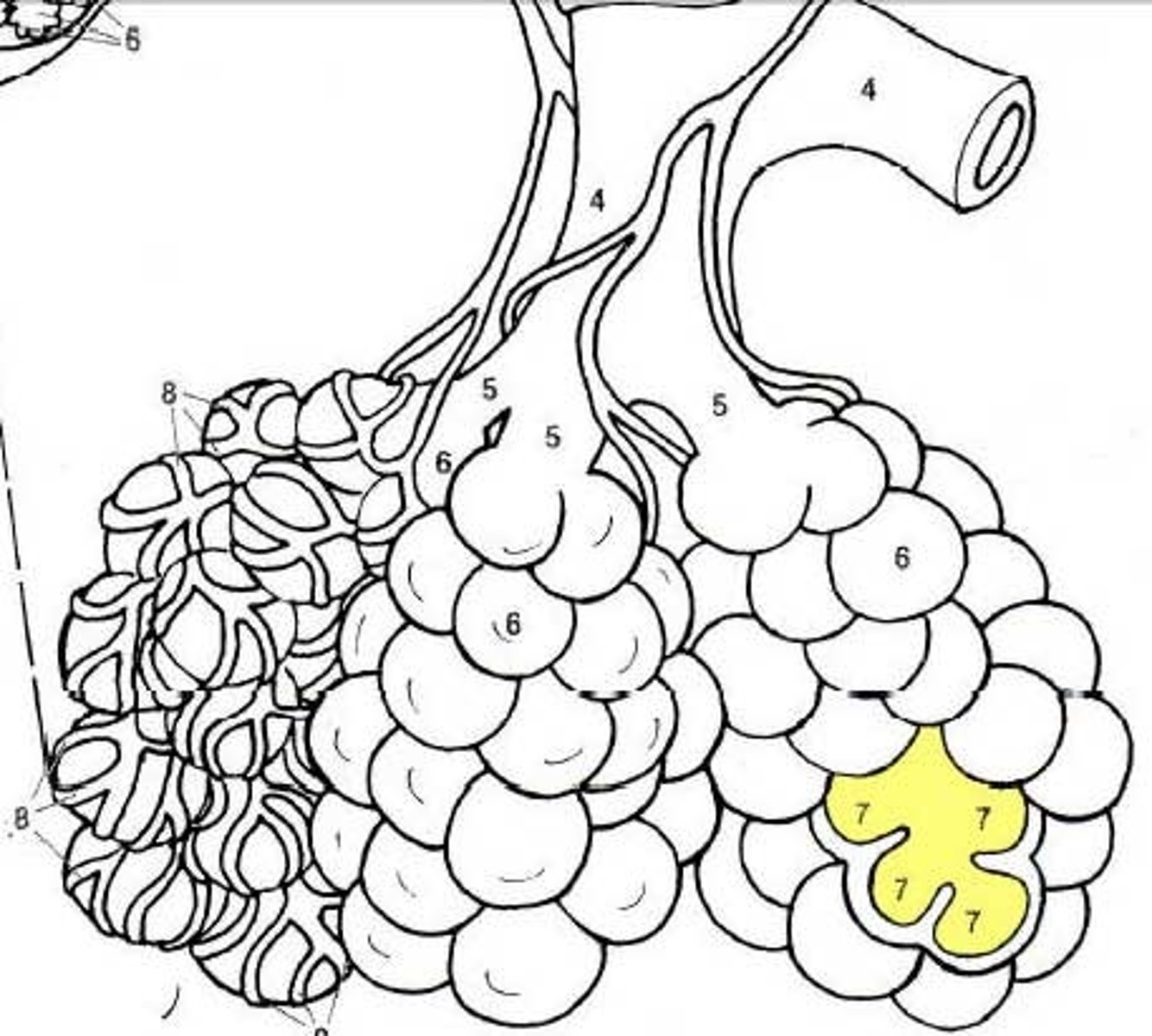
Pulmonary capillaries
a web of thin-walled capillaries that wrap the alveoli; the site of gas exchange
The composition of the lungs
elastic tissue
The pleura
The two layers of connective tissue that surround the lungs
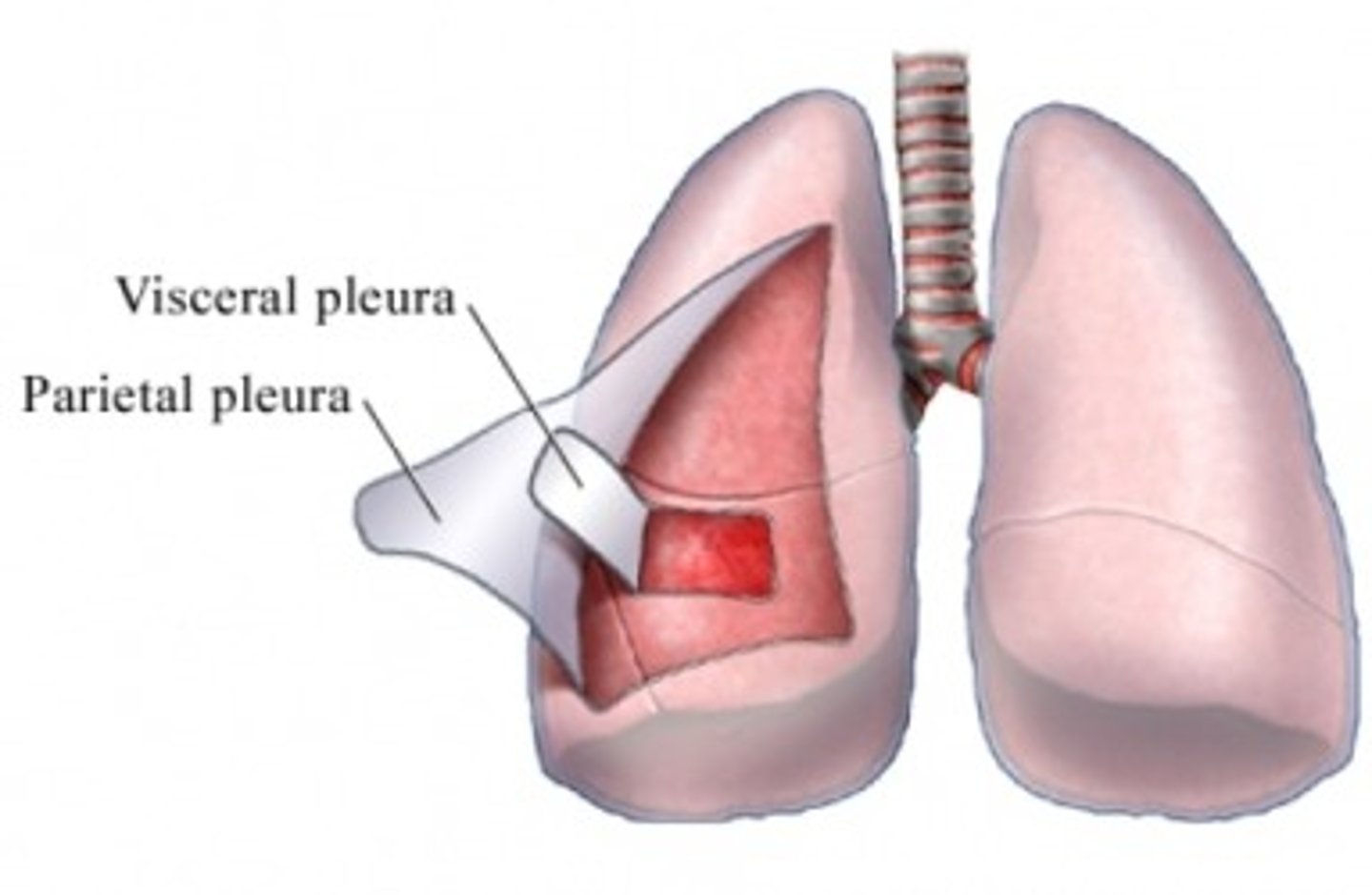
The visceral pleura
the innermost covering of the lung
The parietal pleura
thicker, more elastic layer that adheres to the inner portion of the chest wall
Between the two pleura layer
the pleural space; at negative pressure
Serous fluid
acts as a lubricant to reduce friction in the pleura space
The diaphragm
muscle that separates the chest cavity from the abdominal cavity; major muscle used in breathing; responsible for 60-70% of the effort of ventilation
Ventilation
Passage of air into and out of the lungs; creates pressure changes in the lungs to draw air in and force air out
Inhalation/inspiration
breathing air in
Exhalation/expiration
process of breathing air out
Inhalation mechanics
diaphragm and the external intercostal muscles contract; increases the size of the chest cavity, creating negative pressure inside the chess cavity; active process
Exhalation mechanics
Diaphragm and external intercostal muscles relax; reduced chest cavity size; positive pressure; forces volume of air out of the lungs; passive
Control of Respiration
The respiratory organs do not have the ability to control their function from within the respiratory system; respirations are controlled by the nervous system
The response to an increase level in arterial blood
The chemoreceptors sense the increase and the brainstem sends impulses to the respiratory muscles to increase the rate and depth of respiration
The main stimulus for breathing in healthy people
Carbon dioxide
Hypercarbic drive
What healthy people breath
The difference between COPD people and normal people
In people with COPD the carbon dioxide level in arterial blood is typically chronically elevated as a result of the disease process. Because of the constant high carbon dioxide level the chemoreceptors become relatively insensitive to changes in carbon dioxide. Instead the chemoreceptors in COPD patients tend to rely on oxygen levels in the blood to regulate their breathing.
Why do COPD people breath?
To increase their oxygen levels instead of decrease their Carbon dioxide level
Oxygenation
the process by which the blood and the cells become saturated with oxygen
Internal respiration and external respiration
the process in which fresh oxygen replaces waste carbon dioxide, a gas exchange that takes place between the alveoli and the capillaries in the lungs, and between the capillaries and the cells throughout the body
Hypoxemia
Low oxygen content in arterial blood. Typically occurs from a ventilation-perfusion mismatch
Ventilation-perfusion mismatch
occurs when there is a lack of available oxygenated air in the alveoli even though perfusion (blood flow) to the alveoli is adequate or when the alveoli are adequately oxygenated but perfusion to the alveoli is poor or when there is a combination of both poor ventilation and poor perfusion in the alveolar-capillary structures
Other causes of hypoxemia
inadequate ventilatory drive, anemia, and carbon monoxide poisoning
Hypoxia
inadequacy in the amount of oxygen being delivered to the cells
Different causes of hypoxia
Occluded airway, inadequate breathing, inadequate breathing, inadequate delivery of oxygen to the cells by the blood (hyper fusion or shock), inhalation of toxic gases, lung and airway deceases, etc
Signs of Mild to Moderate Hypoxia
Tachypnea (increased respiratory rate)
Dyspnea (shortness of breath)
Pale, cool, clammy skin (early)
Tachycardia
Elevation in blood pressure
Restlessness and agitation (from hypoxic brain cells)
Disorientation and confusion (from high CO2 levels)
Headache
Signs of Severe Hypoxia
Tachypnea
Dyspnea
Cyanosis
Tachycardia that may lead to dysrhythmias and eventually bradycardia
Severe confusion
Loss of coordination
Sleepy appearance
Head bobbing with droopy eyelids
Slow reaction time
Altered mental status
Seizure
Cyanosis
a bluish gray color, a late sign of hypoxia and may be found in and around several areas including the lips, mouth, nose, fingernail beds
Gas content of the blood entering the capillaries
High oxygen content and a low carbon dioxide content
Causes of disruption in the mechanical process of pulmonary ventilation
•Interruption of the nervous system's control and stimulation of the diaphragm or of the external intercostal muscles
•Structural damage to the thorax may interfere with the bellows action of the chest. This will impede the ability of the thorax to generate pressure changes necessary to draw air into the lungs for inhalation and to allow airflow out of the lungs during exhalation. Pain associated with chest injury, flail chest (two or more ribs fractured in two or more places), rupture or injury to the diaphragm, or compression of the chest wall can reduce the effective bellows action of the chest
•Increased airway resistance will reduce airflow through the respiratory tract and reduce the amount of air in the alveoli. This will make less oxygen available for gas exchange. An increase in airway resistance may occur from bronchoconstriction or from inflammation inside the vessel
•Disruption of airway latency can occur from swell in caused by infection, allergic reaction, or burns; from trauma; from foreign body obstruction; or from loss of muscle tone associated with an altered mental status or unresponsiveness. Reduction or loss of airway latency will reduce the tidal volume, minute ventilation, alveolar ventilation, and volume of gas in the lungs for gas exchange
The mouth and nose of children
The noses and mouths of infants and children are smaller than those of adults; thus it is especially important to keep the nose clear of obstructions
The pharynx of children
The tongue of an infant or child is relatively large in proportion to the size of the mouth.
The trachea and lower airway of children
Narrower, softer, and more flexible than adults. Airway obstructions occur more easily from mucus, pus, blood, secretions, swelling, constriction, and kinking of the trachea with flexion or extension
Chest wall in children
Softer and more pliable than in an adult; leads to greater compliance during ventilation
Patent airway
open airway
Functions and considerations regarding the airway
•the airway and respiratory tract is the conduit that allows air to move from the atmosphere and into the alveoli for gas exchange
•No matter what the patient's condition, the airway must remain patent at all times
•Any obstructions of the airway will result in less air movement, which will lead to some degree of poor gas exchange and potential hypoxia
•The degree of the obstruction will directly affect the amount of air available for gas exchange. The tongue may create only a partial airway obstruction, whereas a piece of food may completely stop airflow
A patient's mental status typically correlates to the status of his airway
An alert, responsive patient who is talking to you in a normal voice has an open airway. A patient with an altered mental status or who is completely unresponsive connote adequately protect his own airway.
Signs of an open airway
1) air can be felt and heard moving in and out of the mouth and nose
2) the patient is speaking in full sentences or with little difficulty
3) the sound of the voice is normal for the patient
Snoring
occurs when the upper airway is partially obstructed by the tongue or by relaxed tissues in the pharynx.
Crowing
sounds like a crow cawing that occurs when the muscles around the larynx spasm and narrow the opening into the trachea, air rushing through the restricted passage causes the sound
Gurgling
sounds like gargling, usually indicates the presence of blood, vomitus, secretions, or other liquid in the airway
Stridor
a harsh, high-pitched sound heard during inspiration, characteristic of a significant upper airway obstruction from swelling in the larynx, may also be heard if a mechanical obstruction by food or other object is presence
Head-tilt, Chin-lift maneuver
no spinal injury
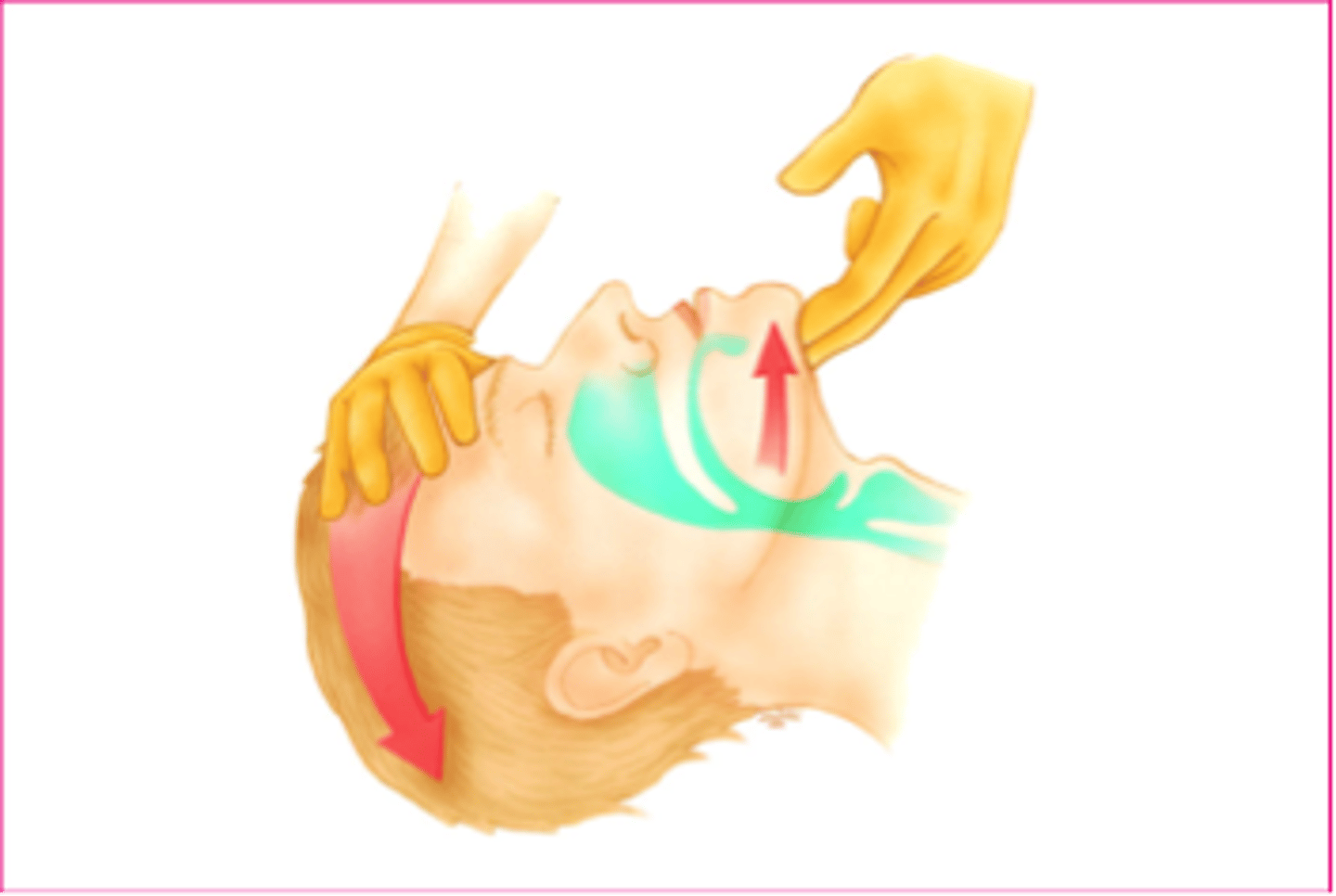
Jaw-thrust maneuver
suspected spinal injury
Standard precaution during suctioning
Protective eyewear, a mask, and gloves. If a patient is known to have TB an N-95 should be worn
Suction Equipment
The device that creates the suction and the catheters
Mounted Suction Devices
On-board the ambulance, should be powerful enough to provide an airflow of >40 lpm and create a vacuum of more than -300 mmHg
Portable Suction Devices
Should be capable of generating -300 mmHg of pressure when the suction hose is clamped. A pressure of -80 to -120 mmHg is generally necessary to provide adequate suction. Can be electric, oxygen, air or hand powered
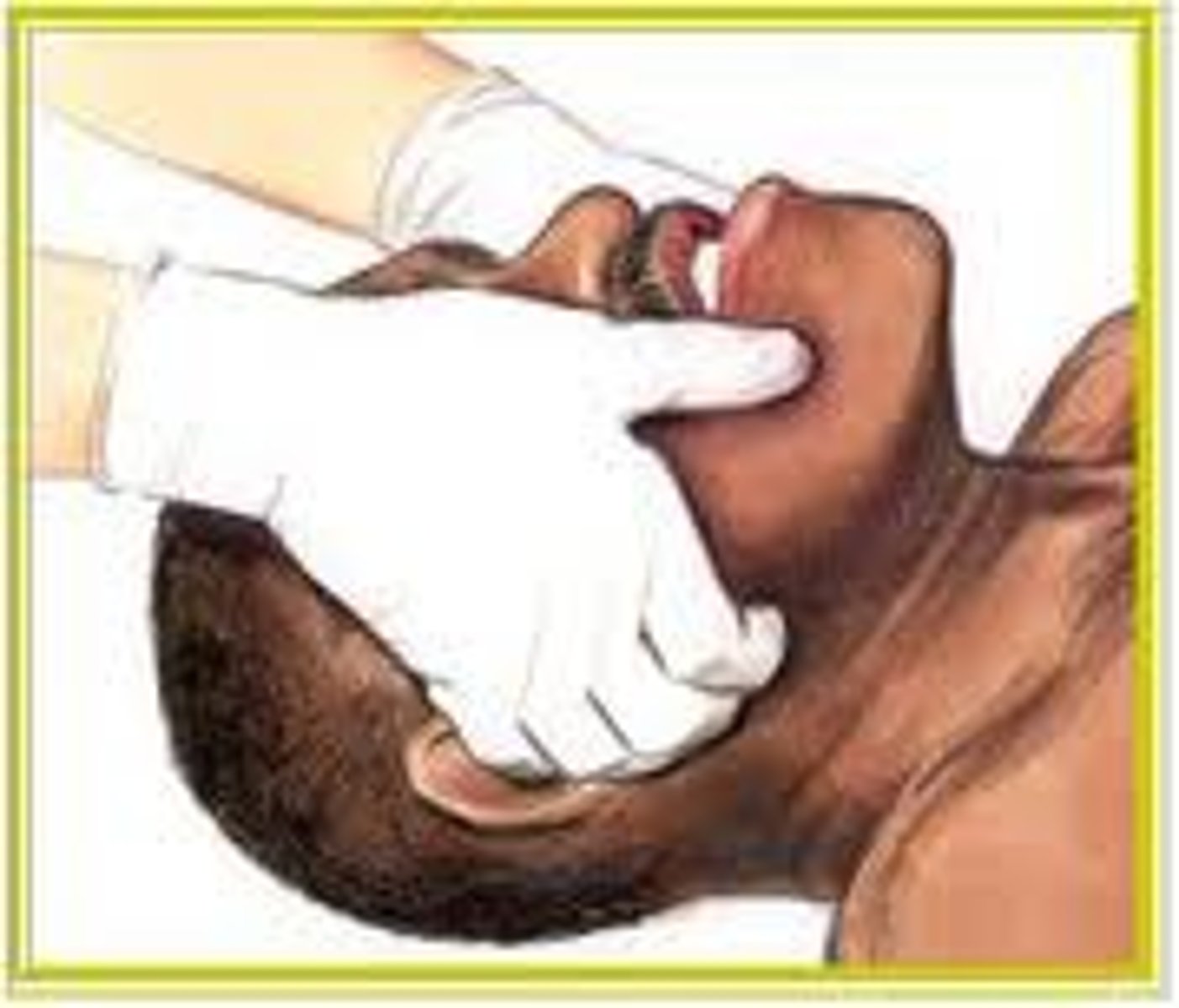
Hard or rigid catheter
Rigid plastic tube; Yankauer catheter or the tonsil tip. Used to suction the mouth and oropharynx of an unresponsive patient. Only be inserted as far as you can see and no farther than the back of the tongue.
Soft catheter
Flexible tubing; also called the "French" catheter. Used in suctioning the nose and nasopharynx and in other situations where the rigid catheter can not be used. Length should be determined by measuring from the tip of the patient's nose to the tip of the ear
Special considerations when suctioning
•If the patient has secretions or vomitus that cannot be removed quickly and easily by suctioning, the patient should be log rolled onto his side and the oropharynx cleared by finger sweeping the foreign material out
•If the patient needs artificial ventilation and is producing frothy secretions as rapidly as suctioning can remove them, apply suction for 10 seconds, provide positive pressure ventilation with supplemental oxygen for 2 minutes, then apply suction for another 10 seconds.
Two types of artificial airways
Oropharyngeal and nasopharyngeal
Points to keep in mind when using artificial airways
1) adjunct must be clean and clear of obstructions
2) proper size must be selected
3) airways adjuncts do not protect the airway from aspirations of secretions, blood, vomitus, or foreign substances
4) the mental status of the patient will determine if an adjunct can be used
The oropharyngeal airway (OPA)
Patient must be completely unresponsive and have no gag or cough reflex. Measure the airway by holding it next to the patient's face, should extend the distance from the corner of the mouth to the tip of the ear

Nasopharyngeal airway (NPA)
Use in patients whom the oral airway cannot be inserted because of clenched teeth, biting, or injuries to the maxilla or face. Can be used in patients who are not fully responsive and have a minimally intact gag reflex. Measure from the nose to the tip of the earlobe

Inadequate breathing leads to
Poor gas exchange in the alveoli and ineffective delivery of oxygen to the cells
Determining the adequacy of breathing
Assets the relationship between the volume and the rate at which a patient is breathing
Minute volume
Dept and rate; typically correlates with how adequately the patient is breathing
Tidal volume
Respiratory rate; amount air breathed in and out in one normal respiration
Alveolar ventilation
Amount of air breathed in that reaches the alveoli
Dead air space
Anatomical areas in the respiratory tract where air collects during inhalation but no gas exchange occurs
Minute volume
Tidal volume multiplied by rate
Amount of dead air
150 mL of the 200 mL breathed in
Assessing for adequate breathing
1) look (inspect) chest rise/fall, general appearance, breathing pattern, nostrils
2) listen
3) feel
4) ausculate
Rate
12-20 adults
15-30 children
25-50 infants
Signs of adequate breathing
Normal respiratory rate
Clear and equal breath sounds bilaterally
Adequate air movement heard and felt from nose and mouth
Good chest rise and fall with each ventilation
Rhythm
The pattern is regular
Quality
Equal and full bilateral breath sounds. No excessive accessory muscle use
Respiratory distress
The patient is working harder to breathe
The effects of inadequate oxygen
Brain death in about 4-6 minutes
Respiratory failure
When the respiratory rate and/or tidal volume is insufficient
Respiratory arrest
Apnea; occurs when the patient completely stops breathing
Causes of respiratory arrest
Stroke
MI
OD
Toxic inhalation
Electrocution and lighting strike
Suffocation
Traumatic injuries to the head, spine, chest or abdomen
Infection to the epiglottis
Away obstruction by a foreign body