2. Ch 23 Alterations of Hematologic Function- Leukocytes and Platelets
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
What factors affect leukocyte function?
Leukocyte function is affected by having too many or too few white cells, or if the cells present are defective.
What happens if phagocytes aren't effective?
If phagocytes aren't effective, the body's ability to fight infections is compromised.
How do defective lymphocytes impact immune response?
Defective lymphocytes result in an inability to respond effectively to antigens, impairing immune function.
What are examples of conditions related to leukocyte dysfunction?
Leukemia and myeloma are examples of conditions where leukocyte function is impaired.
What are quantitative disorders in leukocyte function?
Quantitative disorders involve increases or decreases in leukocyte cell numbers.
What is leukocytosis?
Leukocytosis is a higher-than-expected white blood cell count, often a normal response to stress, surgery, invading organisms, medications, or toxins. It can also be caused by malignancies.
What is leukopenia?
Leukopenia is a lower-than-expected white blood cell count, which is never normal. Causes include radiation, anaphylactic shock, and immune diseases.
What risk does leukopenia pose?
Leukopenia increases the risk of infection as the white blood cell count decreases.
What is granulocytosis/neutrophilia?
Granulocytosis or neutrophilia is an increase in granulocytes (neutrophils, eosinophils, basophils) in the blood.
When is granulocytosis/neutrophilia typically observed?
It is evident in the first stages of infection or inflammation.
What happens if the demand for neutrophils exceeds the supply?
If the demand for neutrophils exceeds the supply, immature neutrophils (banded neutrophils) are released from the bone marrow into the blood.
What is neutropenia?
Neutropenia is a decrease in circulating neutrophils.
What can cause neutropenia?
Neutropenia can be caused by prolonged severe infections, decreased production, reduced survival, or abnormal neutrophil distribution.
What are some conditions where neutropenia is seen?
Neutropenia is seen in leukemias, lymphoma, folate deficiency, B12 deficiency anemia, starvation, and anorexia, all related to decreased nutrients for protein production.
What is granulocytopenia or agranulocytosis?
Granulocytopenia or agranulocytosis is severe neutropenia or the absence of granulocytes.
What causes granulocytopenia/ agranulocytosis?
It is caused by interference with hematopoiesis in the bone marrow or massive cell destruction in circulation (such as from chemotherapy or radiation).
What are the symptoms of granulocytopenia/ agranulocytosis?
Symptoms include severe infection, malaise, ulcers in the mouth and colon (rectal bleeding), fever, and tachycardia.
What is eosinophilia?
Eosinophilia is an increase in the number of eosinophils.
What triggers eosinophilia?
Type I Hypersensitivity reactions trigger the release of eosinophilic chemotactic factors to the mast cell, commonly seen in allergic disorders (seasonal allergies) and parasitic invasions.
What is eosinopenia?
Eosinopenia is a decrease in the circulation of eosinophils.
What causes eosinopenia?
Eosinopenia is often caused by the migration of eosinophils to inflammatory sites and conditions that put the body under stress, such as surgery, shock, trauma, burns, and mental distress.
What is basophilia?
Basophilia is an increase in the number of basophils, which is rare and often a response to inflammation, hypersensitivity reactions, or chronic myelogenous leukemia (CML).
What causes basophilia?
Basophilia is caused by inflammation, hypersensitivity reactions, and conditions like chronic myelogenous leukemia (CML).
What is basopenia?
Basopenia is a decrease in the number of basophils.
What causes basopenia?
Basopenia occurs in acute infections, hyperthyroidism, and long-term steroid therapy.
What is lymphocytosis?
Lymphocytosis is an increase in the number of lymphocytes.
What causes lymphocytosis?
Lymphocytosis is commonly seen in acute viral infections, such as Epstein-Barr virus and infectious mononucleosis.
What is lymphocytopenia?
Lymphocytopenia is a decrease in the number of lymphocytes in the blood.
What causes lymphocytopenia?
Lymphocytopenia can be caused by neoplasia, immune deficiencies, destruction of lymphocytes by drugs, viruses, radiation, or unknown causes.
What is leukemia?
Leukemia is a malignant disorder of the bone marrow and usually also the blood.
What percentage of childhood malignancies is leukemia?
Leukemia accounts for 34% of childhood malignancies.
What are common features of leukemia?
Common features of leukemia include uncontrolled proliferation of malignant leukocytes, overcrowding of the bone marrow, and decreased production and function of normal hematopoietic cells
What causes leukemia at the cellular level?
Leukemia is caused by genetics where cells are unable to mature, and signaling pathways prevent the death of abnormal cells.
What are common chromosomal and genetic factors involved in leukemia?
Leukemia can involve chromosomal malformations and gene mutations.
What results from the accumulation of leukemic cells?
The excessive accumulation of leukemic cells leads to overcrowding in the bone marrow and impaired function of normal blood cells.
What are the manifestations/cues of leukemia?
Manifestations of leukemia include pallor, fatigue, purpura, and fever.
How is leukemia classified?
Leukemia is classified based on the predominant cell of origin (myeloid or lymphoid) and the rate of progression (acute or chronic).
What defines acute leukemia?
Acute leukemia (ALL, AML) is characterized by the presence of undifferentiated or immature cells (blast cells). Its onset is abrupt and rapid.
What defines chronic leukemia?
Chronic leukemia (CLL, CML) involves predominantly mature cells that do not function normally. It progresses slowly.
What is the most common type of leukemia in children?
Acute Lymphoblastic Leukemia (ALL) is more common in children.
Which leukemias are most common in adults?
Chronic Lymphocytic Leukemia (CLL) and Acute Myelogenous Leukemia (AML) are most common in adults.
What leukemia is most commonly seen in adults?
Chronic Myelogenous Leukemia (CML) is seen mostly in adults.
How have remission and survival rates for leukemia improved over the years?
Remission and survival rates have increased, with up to 91% of children with ALL surviving, 81% of CLL, and 24% for AML.
slide 17-19???
??
What happens in leukemia related to bone marrow?
In leukemia, genetic changes cause blast cells to proliferate and crowd out normal marrow, leading to pancytopenia (reduction in all blood components).
What are some risk factors for leukemia?
Risk factors include genetic mutations, environmental factors, radiation, chemotherapy, x-rays, and familial predisposition.
What is a common sign and symptom of leukemia related to bone marrow suppression?
Chronic anemia is often more insidious, progressing slowly. Other signs and symptoms include fatigue, pallor, and increased risk of bleeding.
Common symptoms/cues of leukemia
anemia
bleeding/purpura
petechiae
ecchymosis
thrombosis
DIC/hemorrhage
infection
weight loss
bone pain
elevated uric acid
liver, spleen, and lymph node enlargement
What is lymphadenopathy?
Lymphadenopathy is the enlargement of lymph nodes that become palpable and tender due to proliferation of lymphocytes, monocytes, or malignant cell invasion.
What is local lymphadenopathy?
Local lymphadenopathy occurs when there is drainage of an inflammatory lesion located near the enlarged node, commonly seen with transient illnesses or infections.
What is general lymphadenopathy?
General lymphadenopathy occurs in the presence of malignant or nonmalignant diseases, including endocrine disorders.
What is malignant lymphoma?
Malignant lymphoma is the malignant transformation of a lymphocyte, leading to its uncontrolled and excessive growth in lymphoid tissues, often resulting in tumor masses in lymph nodes.
What are potential causes of malignant lymphoma?
Malignant lymphoma can result from genetic mutations or viral infections.
What happens in malignant lymphoma?
In malignant lymphoma, the affected lymphocyte grows uncontrollably, accumulating in lymph nodes and forming tumor masses.
What are the two major categories of malignant lymphoma?
The two major categories are Hodgkin lymphoma (HL) and Non-Hodgkin lymphoma (NHL).
How have the number of cases of Hodgkin lymphoma (HL) and Non-Hodgkin lymphoma (NHL) changed?
The number of Hodgkin lymphoma cases has decreased over the past few decades, while the number of Non-Hodgkin lymphoma cases has almost doubled in the same period.
How does Hodgkin lymphoma progress?
Hodgkin lymphoma progresses from one group of lymph nodes to another, leading to systemic symptoms.
What are Reed-Sternberg (RS) cells?
Reed-Sternberg (RS) cells are B cells that are the malignant transformed lymphocytes in Hodgkin lymphoma.
What is the triggering mechanism for Reed-Sternberg (RS) cell transformation?
The triggering mechanism for Reed-Sternberg cell transformation remains unknown, but it may be linked to Epstein-Barr virus (EBV).
How does Epstein-Barr virus (EBV) relate to Hodgkin lymphoma?
Some individuals with Hodgkin lymphoma have traces of the EBV genetic code, allowing the malignant cell to evade induced cell death, leading to continued cell division.
What causes many of the local and systemic effects in Hodgkin lymphoma?
The release of cytokines is responsible for many of the local and systemic effects seen in Hodgkin lymphoma.
What are some physical assessment findings in Hodgkin lymphoma?
Painless adenopathy, mediastinal mass, splenomegaly, and abdominal mass.
What are some clinical manifestations of Hodgkin lymphoma?
Intermittent fever, anorexia, malaise, weight loss, night sweats, and pruritus (itchy skin).
What laboratory results might be seen in Hodgkin lymphoma?
Thrombocytosis, leukocytosis, eosinophilia, elevated ESR, and elevated alkaline phosphatase.
What is Non-Hodgkin Lymphoma?
A diverse group of lymphomas not related to Reed-Sternberg (RS) cells—all other types.
What are some risk factors for Non-Hodgkin Lymphoma?
Middle age, male gender, Caucasian, immune disorders, HIV/AIDS, high-fat diet, organ transplant, and H. Pylori infection.
How is Non-Hodgkin Lymphoma classified?
Classified based on cell type (T, B, NK), as they originate from these types of cells.
What factors differentiate Non-Hodgkin Lymphoma?
Differentiated based on etiology, unique features, and response to therapies.
What are some potential causes of Non-Hodgkin Lymphoma?
Chromosome translocations, viral and bacterial infections, environmental agents, immunodeficiencies, and autoimmune disorders.
How do changes in proto-oncogenes and tumor-suppressor genes contribute to Non-Hodgkin Lymphoma?
They contribute to cell immortality, leading to an increase in malignant cells.
What are common manifestations/cues of Non-Hodgkin Lymphoma?
Painless lymphadenopathy, back pain, skin rash, itchy skin, fatigue, fever, night sweats, and leg swelling. Nodes may grow over months or years.
How does Non-Hodgkin Lymphoma usually present compared to Hodgkin Lymphoma?
Non-Hodgkin Lymphoma often starts with localized or generalized lymphadenopathy, and the nodes grow slowly over time.
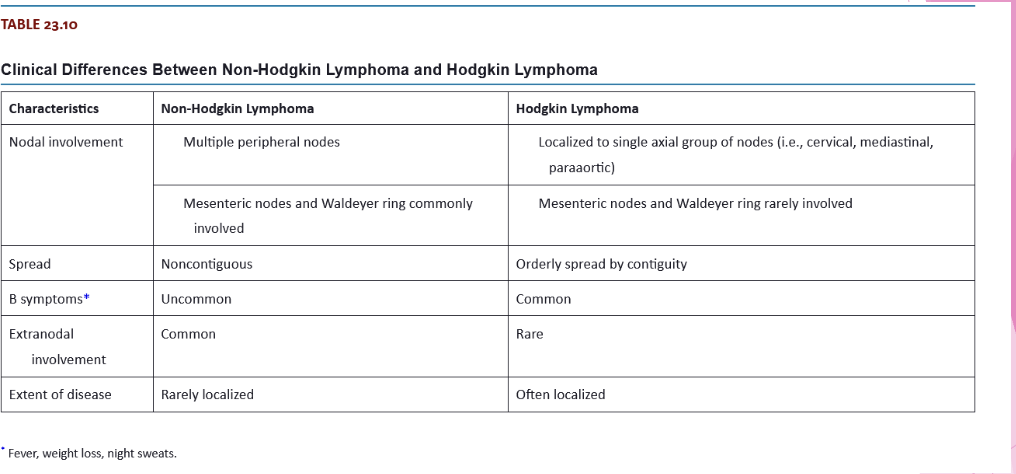
Comparison
What is the most common type of non-Hodgkin lymphoma in children?
Burkitt lymphoma.
What is a key characteristic of Burkitt lymphoma?
It is a very fast-growing tumor, usually seen in the jaw and facial bones.
What virus is commonly found in Burkitt lymphoma patients?
Epstein-Barr virus (EBV).
What genetic alteration is associated with Burkitt lymphoma?
A genetic translocation between chromosome 8 and 14, leading to overexpression of a proto-oncogene and loss of control of cell growth.
What can abnormalities in platelets disrupt?
Coagulation and proper hemostasis.
What problems can arise due to platelet abnormalities?
A decrease or increase in the number of platelets or issues with the structure or function of platelets.
What are the normal platelet values in blood?
145,000-415,000 platelets/uL of blood.
What are some manifestations/cues of alterations in platelet function?
Petechiae, purpura, mucosal bleeding, gingival bleeding, and spontaneous bruising.
What is thrombocytopenia and what are the platelet counts associated with different severity levels?
Thrombocytopenia is when platelet count is <150,000 platelets/uL.
<50,000/uL: Hemorrhage from minor trauma
<15,000/uL: Spontaneous bleeding
<10,000/uL: Severe bleeding
What are some causes of thrombocytopenia?
Thrombocytopenia can be congenital or acquired. Causes include:
Nutritional deficiencies (B12, folic acid)
Medications (chemotherapy, heparin)
Liver disease
Viral illnesses affecting platelet production
Genetic-based syndromes
What happens in immune thrombocytopenic purpura (ITP)?
In ITP, IgG antibodies target platelet glycoproteins. Antibody-coated platelets are sequestered and removed from circulation.
What is a common cause of acute ITP and who is most affected?
Acute ITP often develops after a viral infection and is one of the most common childhood bleeding disorders.
What are the manifestations/cues of immune thrombocytopenic purpura (ITP)?
Symptoms include petechiae, purpura, and progressing to major hemorrhage.
What is the most common cause of acute immune thrombocytopenic purpura (ITP) in children?
Acute ITP is most often secondary to viral infections or conditions like drug allergies, H. pylori infection, or systemic lupus erythematosus (SLE).
How does acute immune thrombocytopenic purpura (ITP) resolve?
Acute ITP resolves when the source of the antigen (e.g., infection or allergy) is eliminated.
What are the characteristics of chronic immune thrombocytopenic purpura (ITP)?
Chronic ITP involves autoantibody-mediated destruction of platelets and is most common in women aged 20-40. It worsens as IgG antibodies target platelet glycoproteins, and platelets are removed by macrophages in the spleen.
How does chronic immune thrombocytopenic purpura (ITP) progress and how is it treated?
Chronic ITP undergoes remissions and exacerbations. Treatment is generally palliative, as the disease progressively worsens.
What are the common manifestations of immune thrombocytopenic purpura (ITP)?
Common manifestations include petechiae, purpura, weight loss, fever, and headache.
What is the rare progression of immune thrombocytopenic purpura (ITP)?
In rare instances, ITP can progress to major hemorrhage.
What is Thrombotic Thrombocytopenic Purpura (TTP)?
TTP is a thrombotic microangiopathy where platelets aggregate, form microthrombi, and cause occlusion of arterioles and capillaries.
What are the two types of Thrombotic Thrombocytopenic Purpura (TTP)?
The two types are chronic relapsing TTP (rare familial) and acute idiopathic TTP.
What is Essential (Primary) Thrombocythemia (Thrombocytosis)?
It is a myeloproliferative disorder of platelet precursor cells, leading to platelet counts >450,000/mm³.
What happens in Essential (Primary) Thrombocythemia (Thrombocytosis)?
Megakaryocytes in the bone marrow are produced in excess, causing microvasculature thrombosis.
What is Vitamin K necessary for in coagulation?
Vitamin K is necessary for the synthesis and regulation of prothrombin, prothrombin factors (II, VII, IX, X), and anticoagulants (proteins C and S).
How does liver disease affect hemostasis?
Liver disease causes defects in coagulation, decreases platelet number, and impairs platelet function.
Do we need to know clotting cascade?